Nt scan normal range
Normal reference range of fetal nuchal translucency thickness in pregnant women in the first trimester, one center study
J Res Med Sci. 2015 Oct; 20(10): 969–973.
doi: 10.4103/1735-1995.172786
,,,1 and 2
Author information Article notes Copyright and License information Disclaimer
Background:
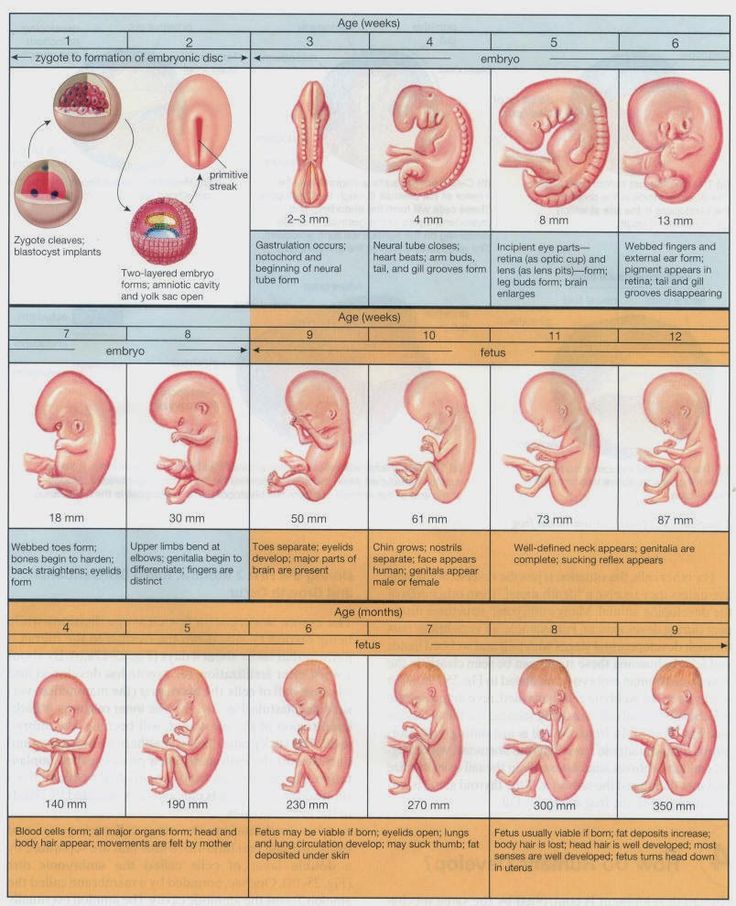
Considering that establishment of reference value of nuchal translucency (NT)-related to the crown rump length (CRL) during the first trimester will be helpful for determining an appropriate cutoff level for screening of increased NT thickness-related abnormalities, we determined the NT thickness and investigated its relation with different chromosomal and nonchromosomal abnormalities among a large sample size of pregnant Iranian women.
Materials and Methods:
In this analytic cross-sectional study, pregnant women who were in their first trimester were enrolled at their antenatal visit. Using an abdominal ultrasonography, the fetal NT thickness of the studied population was measured. Those with increased NT thickness were determined. The reference value of NT thickness (5th, 25th, 50th, 75th, and 95th percentiles) within each 5-mm range of CRL and during the 11th, 12th, and 13th gestational weeks were determined. The presences of the different chromosomal and nonchromosomal abnormalities were compared in women with different percentiles of NT thickness who underwent amniocentesis and those who did not.
Results:
1,614 pregnant women were evaluated. The mean NT thickness was 1.30 ± 0.54 mm. Increased NT thickness >2 mm and >95th percentile according to their gestational age (GA) was detected in 89 (5.5%) and 58 (3.6%) pregnant women. The reference 95th percentile value range for NT was 1.8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
Conclusion:
The obtained reference range in our studied population was different from that reported for other ethnic groups and it is suggested that using this values are more favorable for screening of chromosomal abnormalities during the first trimester of pregnancy than the recommended single cutoff value.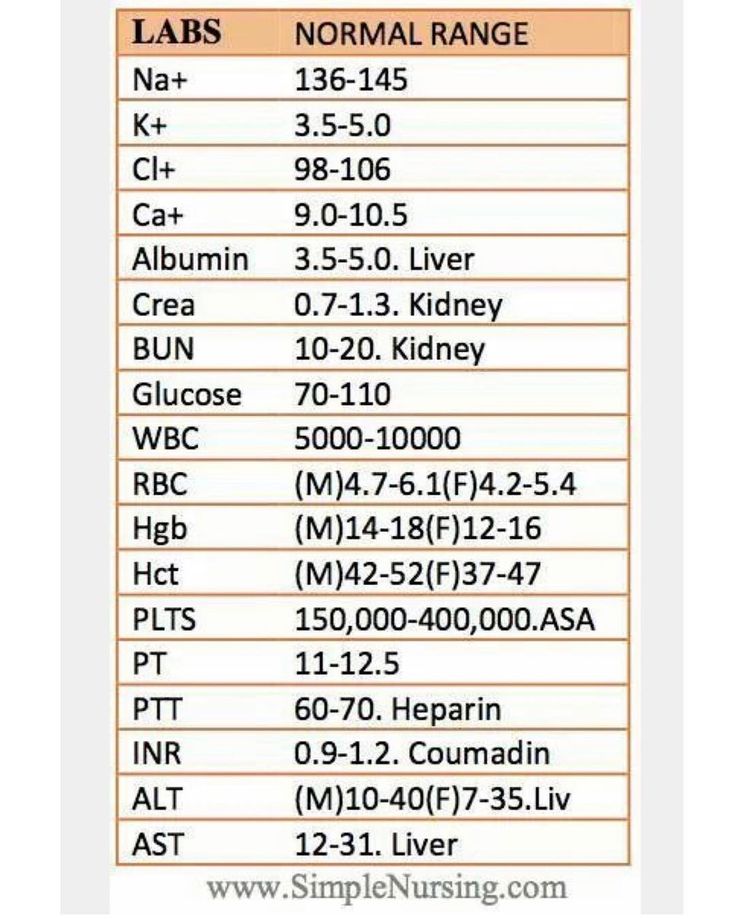
Keywords: Crown rump length (CRL), nuchal translucency (NL), reference values
Nuchal translucency (NT) is the normal fluid-filled subcutaneous space between the back of the fetal skin and the overlying skin.[1] NT is visible and can be measured by ultrasonographic imaging between 11 weeks and 14 weeks gestation.[2] Increased NT is associated with different fetal chromosomal and nonchromosomal abnormalities. There is growing evidence that increased NT thickness during the first trimester of pregnancy in a chromosomally normal fetus is associated with numerous fetal structural abnormalities, genetic syndromes, heart defects, and poor perinatal outcomes such as miscarriage and intrauterine death.[3,4,5]
The first definition for increased NT was a measure >95th percentile for a given crown rump length (CRL) and a NT value of 2.5-3 mm, which was reported as a normal range for the marker. Recently, some studies indicated that NT >99th percentile or NT value that exceeds of 3. 5 mm are associated with the most common adverse outcomes.[6,7]
5 mm are associated with the most common adverse outcomes.[6,7]
The utility of NT as a sensitive and noninvasive ultrasonographic marker for screening and detection of aneuploidies and major structural anomalies in modern obstetrical practice has been demonstrated recently. Its use as a new screening method for the mentioned purposes has been developed in many developed countries.[8,9,10]
Since the introduction of NT thickness, several studies worldwide have determined the normal range of NT in different populations. The results were different regarding the normative value of NT. One of the explanations for the reported great variety of NT thickness range is ethnic variation.[11,12,13,14,15] However, there are still controversies regarding the role of ethnicity on the value of NT. Some reported a significant role of ethnicity in this regard, whereas others did not support the association.[16,17] However, recently the establishment of reference value for NT in different populations was performed. It is suggested that ethnic and region-specific reference value of NT could have a significant impact on its screening efficacy and using a single cutoff for fetal NT could not be an appropriate tool in this field.[18]
It is suggested that ethnic and region-specific reference value of NT could have a significant impact on its screening efficacy and using a single cutoff for fetal NT could not be an appropriate tool in this field.[18]
So considering that establishment of reference value of NT related to the CRL during the first trimester will be helpful for determining an appropriate cutoff level for screening of increased NT thickness-related abnormalities and the presence of few reports in this field among the Iranian population, in this study we determined the reference values of NT thickness among Isfahani pregnant women to evaluate the role of ethnicity on the normative value of NT as well as the association of increased NT thickness with chromosomal and nonchromosomal abnormalities during the first trimester.
In this analytic cross-sectional study, pregnant women referred to a private radiology center for ultrsonographic assessment during the antenatal visit in their first trimester were enrolled. The study was performed from January 2013 to December 2013 in Isfahan, Isfahan Province, Iran.
The study was performed from January 2013 to December 2013 in Isfahan, Isfahan Province, Iran.
The protocol of the study was approved by the Regional Ethics Committee of Isfahan University of Medical Sciences.
Pregnant women with gestational age (GA) of 11-13 weeks and 6 days and/or CRL 45-84 mm were included.
The pregnant women were selected by the consecutive method. Those who did not agree to have the ultrasonography performed, with multiple pregnancies, fetal malformation, and those with inappropriate cooperation were excluded. Written informed consent was obtained from all the selected participants. The selected pregnant women underwent abdominal ultrasonography. The sonography was performed by an expert radiologist. The fetal NT thickness of the studied population was measured.
Those with NT thickness of 2 mm were considered as women with increased NT thickness.[19]
The mean of CRL and GA were compared in women with and without increased NT thickness.
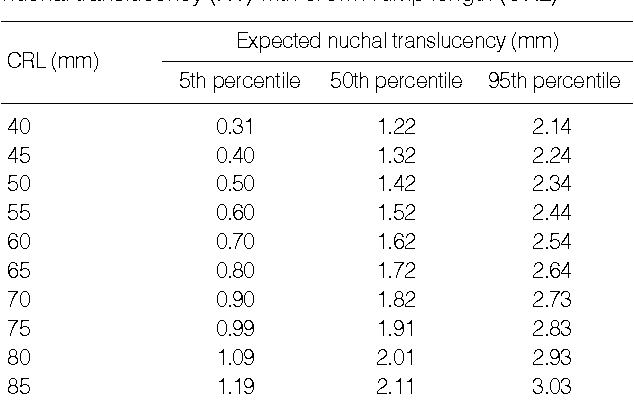
The reference value of NT thickness (5th, 25th, 50th, 75th, and 95th percentiles) within each 5-mm range of CRL and during the 11th, 12th, and 13th gestational weeks were determined.
Women with NT thickness of >95th percentile were determined. The women were followed up and fetal outcomes were evaluated by the neonatologists at birth. The presence of different chromosomal abnormalities as well as nonchromosomal abnormalities including cardiac malformation, genitourinary or renal abnormalities, diaphragmatic hernia, spontaneous miscarriage, and intrauterine fetal death (IUFD) were compared in women with different percentiles of NT thickness who underwent amniocentesis and those who did not.
Ultrasonographic measurements
The ultrasonographic measurements were performed in pregnant women in a supine position.
Fetal CRL and NT thickness measurements were performed by transabdominal ultrsonography using a multi fz: 3. 5 MHz tranduser (GE Volusun 730). The measurement was performed based on the criteria recommended by the Fetal Medicine Foundation (FMF).[20] According to the criteria, the fetus should be in a neutral position, with the head aligned with the spine in a way that fetus occupied at least 75% of the image. NT was defined as the black area between the inner skin outlines echo and the outer border of the soft tissue overlying the cervical spine.
5 MHz tranduser (GE Volusun 730). The measurement was performed based on the criteria recommended by the Fetal Medicine Foundation (FMF).[20] According to the criteria, the fetus should be in a neutral position, with the head aligned with the spine in a way that fetus occupied at least 75% of the image. NT was defined as the black area between the inner skin outlines echo and the outer border of the soft tissue overlying the cervical spine.
The maximal thickness of the black area was measured with caliper placed on the inner borders of the NT space, perpendicular to the long axis of the fetus when a sagittal section with a neutral position of the fetus was obtained. The measurements were recorded to the nearest 0.1-mm interval. At least three NK measurements were taken and the largest was recorded.
CRL was measured at the same time and recorded.
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 21 (SPSS Inc. , Chicago, IL, USA). Using regression equation, the expected 5th, 25th, 50th, 75th, and 5th percentile values of NT thickness according to the CRL categories of CRL (5-mm interval) and GA (11th, 12th, and 13th weeks) were obtained. Quantitive and qualitative values were compared using the t-test and chi-square test, respectively. P value of <0.05 was considered to be statistically significant.
, Chicago, IL, USA). Using regression equation, the expected 5th, 25th, 50th, 75th, and 5th percentile values of NT thickness according to the CRL categories of CRL (5-mm interval) and GA (11th, 12th, and 13th weeks) were obtained. Quantitive and qualitative values were compared using the t-test and chi-square test, respectively. P value of <0.05 was considered to be statistically significant.
During this study, 1,614 pregnant women were evaluated. Among the studied pregnant women 382 (23.7%), 871 (54.0%), and 361 (22.4) were in the 11th, 12th, and 13th gestational week. The mean of GA, CRL, and NT thickness in the studied population were 12.46 ± 0.62 weeks, 59.35 ± 8.35 mm, and 1.30 ± 0.54 mm, respectively. Pearson correlation test indicated that there was a significant positive correlation between NT and CRL (r = 0.238, P < 0.001), NT and GA (r = 0. 24, P < 0.001 and GA) and CRL (r = 0.8, P < 0.001).
24, P < 0.001 and GA) and CRL (r = 0.8, P < 0.001).
Increased NT thickness (NT >2 mm) was detected in 89 (5.5%) pregnant women. The mean of CRL and GA in pregnant women with normal and increased NT thickness are presented in .
Table 1
Mean ± SD of CRL and GA in pregnant women with normal and increased NT thickness
Open in a separate window
The expected 5th, 25th, 50th, 75th, and 95th percentile values of NT thickness to CRL and GA are listed in Tables and . Using the obtained reference value of NT, 58 (3.6%) pregnant women were determined as those with NT thickness >95th percentile according to their GA. During follow-up, 31/58 (53.4%) underwent amniocentesis. Distribution of chromosomal and nonchromosomal abnormalities in pregnant women with NT thickness >95th percentile according to their GA in total and among those with and without amniocentesis are presented in . Frequency of chromosomal abnormalities were significantly higher in those pregnant women with increased NT thickness who underwent the amniocentesis procedure (P = 0.001). The frequency of different nonchromosomal abnormalities were not significantly different between the two studied groups (P > 0.05).
Frequency of chromosomal abnormalities were significantly higher in those pregnant women with increased NT thickness who underwent the amniocentesis procedure (P = 0.001). The frequency of different nonchromosomal abnormalities were not significantly different between the two studied groups (P > 0.05).
Table 2
The expected 5th, 25th, 50th, 75th, and 95th percentile values of NT thickness (mm) to CRL
Open in a separate window
Table 3
The expected 5th, 25th, 50th, 75th, and 95th percentile values of NT thickness (mm) to gestational age (GA)
Open in a separate window
Table 4
Distribution of chromosomal and nonchromosomal abnormalities in pregnant women with NT thickness >95th percentile according to their GA in total and among those with and without amniocentesis
Open in a separate window
In this study, we determined the reference values of NT thickness among pregnant Isfahani women to evaluate the role of ethnicity on the normative value of NT as well as the association of increased NT thickness with chromosomal and nonchromosomal abnormalities during the first trimester. The results indicated that the reference 95th percentile value range for NT was 1.8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
The results indicated that the reference 95th percentile value range for NT was 1.8-2.35 and increased NT thickness according to our obtained values was associated significantly with chromosomal abnormalities.
Several reports from different parts of the worlds and Iran have demonstrated the utility of NK measurement for screening different chromosomal and nonchromosomal abnormalities.[20,21,22,23]
Most of the studies have used the recommended definition for NT thickness by the FMF (i.e., 2.5-3 mm),[6] whereas recent studies reported that using NT thickness as a continuous variable was more appropriate than using a single cutoff value for the fetal NT and consequently, the outcomes of its increased values and screening programs.[18] So, establishment of reference values of NT have been developed in different regions and ethnic groups worldwide.
Though there were studies in Iran, which investigated the association between increased NT value and Down syndrome[22] and adverse pregnancy outcome including miscarriage, fetal loss, and fetal abnormalities,[23] there was not any study, which reported the normative value of NT thickness for the Iranian population. So, this study was designed to determine the ethnic specific reference value of NT thickness for pregnant Iranian women. Our results indicated that the median NT thicknesses for a CRL between 45 mm and 80 mm ranged from 1.00 to 1.65 mm, and the 95th percentiles ranged from 1.8 to 2.35 mm. The median NT thickness for GA were 1.0 mm, 1.2 mm, and 1.4 mm for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively, and the 95th percentiles of NT thickness were 1.8, 1.9, and 2.2 for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively.
So, this study was designed to determine the ethnic specific reference value of NT thickness for pregnant Iranian women. Our results indicated that the median NT thicknesses for a CRL between 45 mm and 80 mm ranged from 1.00 to 1.65 mm, and the 95th percentiles ranged from 1.8 to 2.35 mm. The median NT thickness for GA were 1.0 mm, 1.2 mm, and 1.4 mm for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively, and the 95th percentiles of NT thickness were 1.8, 1.9, and 2.2 for gestational age of 11 weeks, 12 weeks, and 13 weeks, respectively.
The distribution of the NT thickness for CRL has been reported in many studies. The median NT thicknesses has been reported to be 1.2-1.9 mm, 1.22-2.10 mm, and 1.19-1.73 mm for a CRL between 45 mm and 80 mm in Japan, Korea, and Brazil, respectively.[11,12,13] Our reported median value was lower than the other reports.
The 95th NT thickness percentiles have been reported to be 2.1-3.2 mm, 2.14-2.3 mm, 1.57-2. 10 mm, 1.00-2.90 mm, and 1.84-2.35 mm for a CRL between 45 mm and 80 mm in Japan, Korea, Brazil, Thailand, and China, respectively.[11,12,13,14,15] Our results were similar to the reported reference value range of Brazil.[13] Although there was no report from the Eastern Mediterranean region in this field, the values were not similar to the values reported from the Asian countries.
10 mm, 1.00-2.90 mm, and 1.84-2.35 mm for a CRL between 45 mm and 80 mm in Japan, Korea, Brazil, Thailand, and China, respectively.[11,12,13,14,15] Our results were similar to the reported reference value range of Brazil.[13] Although there was no report from the Eastern Mediterranean region in this field, the values were not similar to the values reported from the Asian countries.
Reported variations in the index measurements in the different studies might have been due to factors such as radiologist experience, quality of the ultrasound, method of measurement, and an inappropriate fetal and nuchal cord position. In addition, as mentioned by Kor-anantaku et al. in Thailand some investigators have considered the average of two or three measurements of NT thickness, whereas others considered the largest measurement.[14]
There are controversial reports regarding the impact of ethnicity on NT thickness values and its utility for screening. Thilaganathan et al. have investigated the possible role of ethnicity on NT screening and concluded that the reported differences could not have a significant impact in this regard.[24] Many other studies have also showed that ethnic differences in NT measurements are not clinically significant, especially when it used for screening of Down syndrome.[17,24,25] However, it seems that using ethnic-specific reference values of NT thickness could help us in the first trimester screening programs mainly for chromosomal abnormality, especially when they are integrated with other ultrasonographic and biochemical measurements.
have investigated the possible role of ethnicity on NT screening and concluded that the reported differences could not have a significant impact in this regard.[24] Many other studies have also showed that ethnic differences in NT measurements are not clinically significant, especially when it used for screening of Down syndrome.[17,24,25] However, it seems that using ethnic-specific reference values of NT thickness could help us in the first trimester screening programs mainly for chromosomal abnormality, especially when they are integrated with other ultrasonographic and biochemical measurements.
In this study using the single cutoff value of 2 mm, 5.5% of the studied pregnant women were considered to have high-risk pregnancy and after using our obtained reference value the rate decreased to 3.6%. Thus, it seems that using normative values of NT thickness is more useful for the first trimester screening and it could optimize the screening results by reducing false positive cases.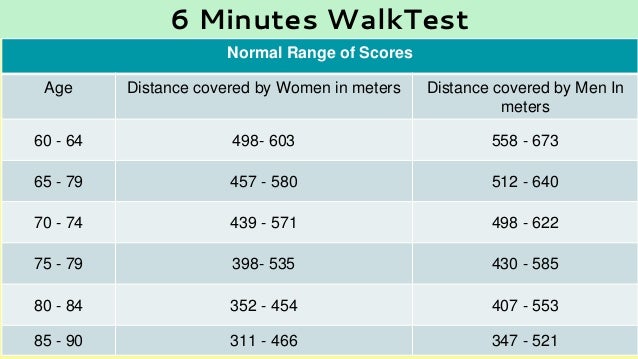
In addition, there was significant association between performing the amniocentesis procedure and detection of chromosomal abnormalities among women with increased NT thickness.
The advantage of the current study was a larger sample size of enrolled pregnant women.
The limitation of the current study was that we did not determine the sex-specific reference value of 95th percentiles of NT and its association with both chromosomal and nonchromosomal abnormalities. We followed up only pregnant women with increased NT thickness and did not determine the frequency of the mentioned abnormalities in pregnant women with normal NT. It was due to the reason that follow-up of that large a sample size was not assessable in the framework of the current study. In addition, we enrolled the patients who were referred to a single referral radiologic center, which could not be a representative sample of the whole population. It is suggested that the large sample size of the studied population could partially alleviate the abovementioned limitation.
Further, the planning of further studies that also determine the 99th percentile values of NT thickness is recommended because recent studies demonstrated that chromosomal and nonchromosomal abnormalities are mainly associated with the 99th percentile value of NT thickness.[7]
The results of our study indicated the reference value of NT thickness in a large sample size of Isfahani pregnant women. The obtained reference range in our studied population was different from that reported for other ethnic groups and it is suggested that using this values are more favorable for screening of chromosomal abnormalities during the first trimester of pregnancy than the recommended single cutoff value. The relation between increased NT thicknesses with chromosomal abnormalities also confirms its utility. The results of the current study could be used as baseline information for other follow-up studies and designing first trimester screening programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
All authors contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
The study was supported by Isfahan University of Medical Sciences (research project number; 393486).
1. Nicolaides KH, Azar G, Byrne D, Mansur C, Marks K. Fetal nuchal translucency: Ultrasound screening for chromosomal defects in first trimester of pregnancy. BMJ. 1992;304:867–9. [PMC free article] [PubMed] [Google Scholar]
2. Szabó J, Gellén J. Nuchal fluid accumulation in trisomy-21 detected by vaginosonography in first trimester. Lancet. 1990;336:1133. [PubMed] [Google Scholar]
3. Vogel M, Sharland GK, McElhinney DB, Zidere V, Simpson JM, Miller OI, et al. Prevalence of increased nuchal translucency in fetuses with congenital cardiac disease and a normal karyotype. Cardiol Young. 2009;19:441–5. [PubMed] [Google Scholar]
4. Bilardo CM, Müller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: Time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30:11–8. [PubMed] [Google Scholar]
Bilardo CM, Müller MA, Pajkrt E, Clur SA, van Zalen MM, Bijlsma EK. Increased nuchal translucency thickness and normal karyotype: Time for parental reassurance. Ultrasound Obstet Gynecol. 2007;30:11–8. [PubMed] [Google Scholar]
5. Saldanha FA, Brizot Mde L, Moraes EA, Lopes LM, Zugaib M. Increased fetal nuchal translucency thickness and normal karyotype: Prenatal and postnatal follow-up. Rev Assoc Med Bras. 2009;55:575–80. [PubMed] [Google Scholar]
6. Salman Guraya S. The associations of nuchal translucency and fetal abnormalities; significance and implications. J Clin Diagn Res. 2013;7:936–41. [PMC free article] [PubMed] [Google Scholar]
7. Souka AP, Von Kaisenberg CS, Hyett JA, Sonek JD, Nicolaides KH. Increased nuchal translucency with normal karyotype. Am J Obstet Gynecol. 2005;192:1005–21. [PubMed] [Google Scholar]
8. Stefanovic V, Äyräs O, Eronen M, Paavonen1 J, Tikkanen M. Clinical utility of nuchal translucency screening. Res Rep Neonatol. 2014;4:169–76. [Google Scholar]
[Google Scholar]
9. Snijders RJ, Noble P, Sebire N, Souka A, Nicolaides KH. UK Multicentre Project on assessment of risk of trisomy 21 by maternal age and fetal nuchal-translucency thickness at 10-14 weeks of gestation. Fetal Medicine Foundation First Trimester Screening Group. Lancet. 1998;352:343–6. [PubMed] [Google Scholar]
10. Miron P, Côté YP, Lambert J. Nuchal translucency thresholds in prenatal screening for down syndrome and trisomy 18. J Obstet Gynaecol Can. 2009;31:227–35. [PubMed] [Google Scholar]
11. Hasegawa J, Nakamura M, Hamada S, Matsuoka R, Ichizuka K, Sekizawa A, et al. Distribution of nuchal translucency thickness in Japanese fetuses. J Obstet Gynaecol Res. 2013;39:766–9. [PubMed] [Google Scholar]
12. Chung JH, Yang JH, Song MJ, Cho JY, Lee YH, Park SY, et al. The distribution of fetal nuchal translucency thickness in normal Korean fetuses. J Korean Med Sci. 2004;19:32–6. [PMC free article] [PubMed] [Google Scholar]
13. Araujo Júnior E, Pires CR, Martins WP, Nardozza LM, Filho SM. Reference values of nuchal translucency thickness in a Brazilian population sample: Experience from a single center. J Perinat Med. 2014;42:255–9. [PubMed] [Google Scholar]
Reference values of nuchal translucency thickness in a Brazilian population sample: Experience from a single center. J Perinat Med. 2014;42:255–9. [PubMed] [Google Scholar]
14. Kor-Anantakul O, Suntharasaj T, Suwanrath C, Chanprapaph P, Sirichotiyakul S, Ratanasiri T, et al. Distribution of normal nuchal translucency thickness: A multicenter study in Thailand. Gynecol Obstet Invest. 2011;71:124–8. [PubMed] [Google Scholar]
15. Sun Q, Xu J, Hu SQ, Chen M, Ma RM, Lau TK, et al. Distribution and normal reference range of fetal nuchal translucency thickness in Kunming pregnant women in the first trimester. Zhonghua Fu Chan Ke Za Zhi. 2012;47:514–7. [PubMed] [Google Scholar]
16. Huang T, Wang F, Boucher K, O’Donnell A, Rashid S, Summers AM. Racial differences in first trimester nuchal translucency. Prenat Diagn. 2007;27:1174–6. [PubMed] [Google Scholar]
17. Chen M, Lam YH, Tang MH, Lee CP, Sin SY, Tang R, et al. The effect of ethnic origin on nuchal translucency at 10-14 weeks of gestation. Prenat Diagn. 2002;22:576–8. [PubMed] [Google Scholar]
Prenat Diagn. 2002;22:576–8. [PubMed] [Google Scholar]
18. Taipale P, Hiilesmaa V, Salonen R, Ylöstalo P. Increased nuchal translacency as a marker for fetal chromosomal defects. N Engl J Med. 1997;337:1654–8. [PubMed] [Google Scholar]
19. Kim SM, Jun JK. Simplified protocol of nuchal translucency measurement: Is it still effective? Obstet Gynecol Sci. 2013;56:307–11. [PMC free article] [PubMed] [Google Scholar]
20. Kagan KO, Avgidou K, Molina FS, Gajewska K, Nicolaides KH. Relation between increased fetal nuchal translucency thickness and chromosomal defects. Obstet Gynecol. 2006;107:6–10. [PubMed] [Google Scholar]
21. Barati M, Zargar M, Masihi S, Taherpour S. Evaluation of nuchal translucency measurement in first trimester pregnancy. Int J Fertil Steril. 2011;5:35–8. [PMC free article] [PubMed] [Google Scholar]
22. Elahifar MA, Hasanzadeh M, Dahmardeh H, Elahifar A. The relationship between thickness of nuchal translucency and Down syndrome in the first trimester of pregnancy.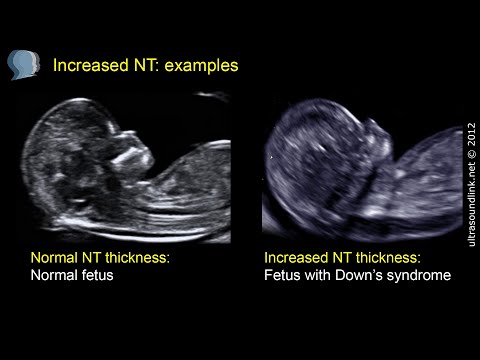 Zahedan J Res Med Sci. 2012;14:26–8. [Google Scholar]
Zahedan J Res Med Sci. 2012;14:26–8. [Google Scholar]
23. Tahmasebpour A, Rafiee NB, Ghaffari S, Jamal A. Increased nuchal translucency and pregnancy outcome. Iran J Public Health. 2012;41:92–7. [PMC free article] [PubMed] [Google Scholar]
24. Thilaganathan B, Khare M, Williams B, Wathen NC. Influence of ethnic origin on nuchal translucency screening for Down's syndrome. Ultrasound Obstet Gynecol. 1998;12:112–4. [PubMed] [Google Scholar]
25. Hsu JJ, Hsieh CC, Chiang CH, Lo LM, Hsieh TT. Preliminary normal reference values of nuchal translucency thickness in Taiwanese fetuses at 11-14 weeks of gestation. Chang Gung Med J. 2003;26:12–9. [PubMed] [Google Scholar]
Nuchal translucency test
Medical Tests
Definition
The nuchal translucency test measures the nuchal fold thickness. This is an area of tissue at the back of an unborn baby's neck. Measuring this thickness helps assess the risk for Down syndrome and other genetic problems in the baby.
Alternative Names
Nuchal translucency screening; NT; Nuchal fold test; Nuchal fold scan; Prenatal genetic screening; Down syndrome - nuchal translucency
How the Test is Performed
Your health care provider uses abdominal ultrasound (not vaginal) to measure the nuchal fold. All unborn babies have some fluid at the back of their neck. In a baby with Down syndrome or other genetic disorders, there is more fluid than normal. This makes the space look thicker.
A blood test of the mother is also done. Together, these two tests will tell if the baby could have Down syndrome or another genetic disorder.
How to Prepare for the Test
Having a full bladder will give the best ultrasound picture. You may be asked to drink 2 to 3 glasses of liquid an hour before the test. DO NOT urinate before your ultrasound.
How the Test will Feel
You may have some discomfort from pressure on your bladder during the ultrasound. The gel used during the test may feel slightly cold and wet. You will not feel the ultrasound waves.
Why the Test is Performed
Your provider may advise this test to screen your baby for Down syndrome. Many pregnant women decide to have this test.
Nuchal translucency is usually done between the 11th and 14th week of pregnancy. It can be done earlier in pregnancy than amniocentesis. This is another test that checks for birth defects.
Normal Results
A normal amount of fluid in the back of the neck during ultrasound means it is very unlikely your baby has Down syndrome or another genetic disorder.
Nuchal translucency measurement increases with gestational age. This is the period between conception and birth. The higher the measurement compared to babies the same gestational age, the higher the risk is for certain genetic disorders.
The measurements below are considered low risk for genetic disorders:
- At 11 weeks -- up to 2 mm
- At 13 weeks, 6 days -- up to 2.8 mm
What Abnormal Results Mean
More fluid than normal in the back of the neck means there is a higher risk for Down syndrome, trisomy 18, trisomy 13, Turner syndrome, or congenital heart disease. But it does not tell for certain that the baby has Down syndrome or another genetic disorder.
If the result is abnormal, other tests can be done. Most of the time, the other test done is amniocentesis.
Risks
There are no known risks from ultrasound.
References
Chaveeva P, Agathokleous M, Nicolaides KH. Fetal aneuploidies. In: Coady AM, Bower S, eds. Twining's Textbook of Fetal Abnormalities. 3rd ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2015:chap 2.
Walsh JM, D'Alton ME. Nuchal translucency. In: Copel JA, D'Alton ME, Feltovich H, et al, eds. Obstetric Imaging: Fetal Diagnosis and Care. 2nd ed. Philadelphia, PA: Elsevier; 2018:chap 45.
Review Date: 04/19/2018
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright ©2019 A.D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
Information developed by A.D.A.M., Inc. regarding tests and test results may not directly correspond with information provided by UCSF Health. Please discuss with your doctor any questions or concerns you may have.
When should I do an NT Scan?
nt screening is usually performed between weeks 11 1/2 and 13 1/2, but must be performed between 10 and 13 weeks of pregnancy . After that, the fabric becomes thicker and is no longer translucent, so the test results become inconclusive.
What is the best week for NT?
This data suggests that when only the last menstrual period is known, the optimal time to schedule a Nuchal translucency measurement is 12 to 13 weeks .
Can I get a scan after 15 weeks?
nt-scan is considered safe . It does not harm your child. But make sure you only get an NT scan in the first trimester. The reason why NT scans in the first trimester is because the space behind the neck may disappear by the 15th week of pregnancy.
Do you see any abnormalities on the 12 week scan?
Some major abnormalities may be visible after 12 weeks, but it is much better to have an ultrasound at 20-22 weeks to rule out structural abnormalities as much as possible.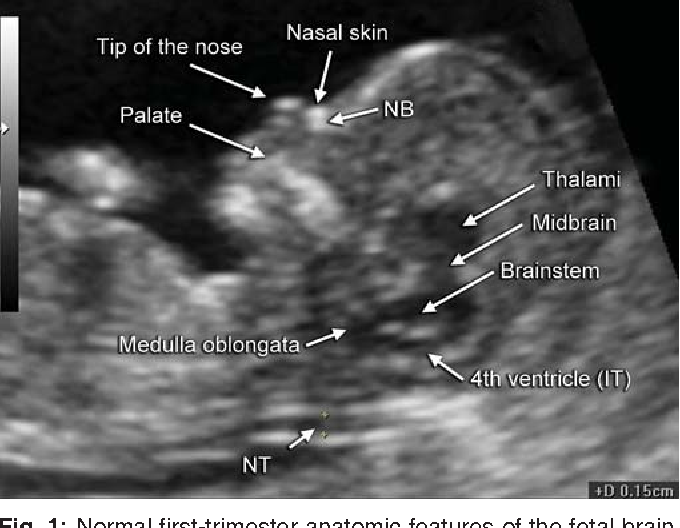 Assess the risk of Down syndrome and other chromosomal abnormalities.
Assess the risk of Down syndrome and other chromosomal abnormalities.
13 weeks late for NT scan?
Too late to do NT Scan at 14 weeks as any excess Nuchal fluid may be absorbed by your baby's developing body. You will be offered a verified second trimester test if for any reason your scan does not occur before 14 weeks. nine0005
What is the normal NT scan range?
The normal NT range for this age is 1.6-2.4 mm . Nuchal skin (NF) skin measurements and prenatal follow-up ultrasound findings were normal.
Is the transparency of Nuchal going away?
Studies have shown that in normal fetuses, fluid collection, known as NT, increases with gestational age until about 13 weeks of gestation3 and usually disappears after 14 weeks3 , 4.
What is an abnormal NT measurement?
Fetal NT increases with gestational age/crown - tear length. Because of this, the NT measurement may be considered abnormal when it is above 3. 0 mm or above the 99th percentile for gestational age. In pooled data from 30 studies, only NT screen has a sensitivity for trisomy 21 of 77% with a 6% false positive rate.
0 mm or above the 99th percentile for gestational age. In pooled data from 30 studies, only NT screen has a sensitivity for trisomy 21 of 77% with a 6% false positive rate.
What makes you at high risk for Down syndrome, baby? nine0023
One of the factors that increases the risk of having a child with Down syndrome is the age of the mother . Women who are 35 or older when they become pregnant are more likely to be affected by Down syndrome than women who become pregnant at a younger age.
When is it too late for a NIPT test?
NIPT is performed with one blood test in the first or second trimester. This can be done any time after the 10th week of pregnancy . What can NIPT tell me? The NIPT can tell you if your pregnancy is at low or high risk for common chromosome disorders including: Down syndrome (Trisomy 21), Trisomy 18, Trisomy 13.
What happens if you test positive for Down syndrome?
If the test is positive, you will be offered a diagnostic test, usually CVS or possibly an amniocentesis. A diagnostic test will determine if the pregnancy is actually affected. CVS is offered early in pregnancy (usually 10 to 13 weeks). nine0005
A diagnostic test will determine if the pregnancy is actually affected. CVS is offered early in pregnancy (usually 10 to 13 weeks). nine0005
How accurate is the 12-week scan for Down syndrome?
First trimester screening results are given as positive or negative and as a probability, eg 1 in 250 risk of transporting a child with Down syndrome. Proper first trimester screening will identify 90,007 about 85 percent of women who are carrying a baby with Down syndrome.
Do I need to drink water before an NT scan? nine0023
You must have a full bladder. You must drink 600-800 ml of water two hours before the scan and refrain from going to the toilet before the scan.
How often is NT wrong?
This test is not perfect. There is 5% false crease . In other words, 5 percent of the women tested get positive results, but the baby is fine. After a positive result, your doctor may suggest another blood test called a cell-free prenatal DNA screen. nine0005
nine0005
can a thick nuchal fold be normal?
Many healthy children have thick folds with the knife. However, there is a higher chance of Down syndrome or other chromosome conditions when the Nuchal fold is thick. There may also be a higher chance for rare genetic conditions.
can increased translucency be normal?
Our study shows that increased NT thickness in first trimester ultrasound screening is associated with poor pregnancy outcome even when the karyotype is normal. However, in euploid pregnancies with normal second trimester ultrasound results, a beneficial outcome occurs in 74.1% of cases.
What happens if the translucency is too high?
Elevated NT has also been associated with a high risk of miscarriage or fetal death. This risk increases with increasing NT thickness, and miscarriage or fetal death may be preceded by symptoms of heart failure such as fetal hydrops. nine0005
2 mm Translucency OK?
Conclusion. In euploid, anatomically normal fruits.
In euploid, anatomically normal fruits.
What is Nuchal translucency off?
Objectives: Link between isolated, elevated translucency thickness (NT) and pathogenic data by chromosomal microarray analysis (CMA). A recent meta-analysis reported that most studies use a limited NT value of 3.5 mm .
What causes extra fluid behind the neck in the fetus? nine0023
In fetal fluid, collects behind the neck, just as it does in dependent ankle edema later in life. This is partly due to the tendency of the fetus to lie on its back and partly due to laxity of the neck skin.
.
Is NT Scan Painful?
You should not feel pain during the procedure. You may feel some discomfort as the doctor or ultrasound technician draws into your abdomen. This feeling usually passes quickly. If you are having a blood test as part of your first trimester, you may feel a small pinch from the needle. nine0005
Where is the baby in your belly in 12 weeks?
Your body at 12 weeks pregnant
it rises to the abdomen as shown in the image.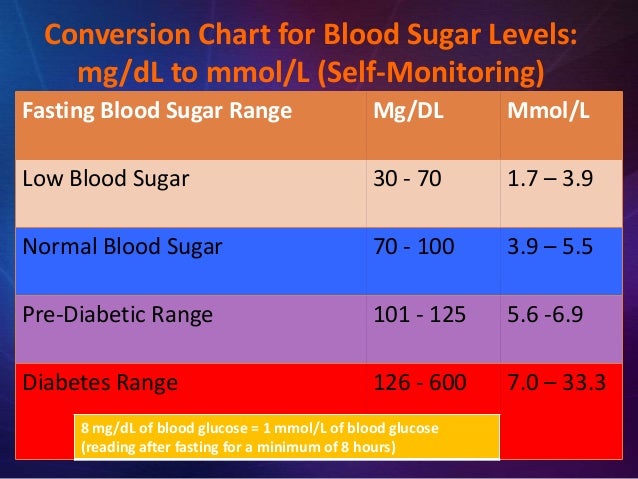 The glans, the upper part of the uterus, is just above the apex of the symphysis, where the pubic bones come together.
The glans, the upper part of the uterus, is just above the apex of the symphysis, where the pubic bones come together.
How long does it take for 12-week scan results?
Normal results will be confirmed in writing within 7 business days. If the result determines pregnancy as a higher risk for any of the conditions, you will be contacted by phone within three days from the midwife. nine0005
Who scans the Internet and whether Australia exists / Sudo Null IT News
Anyone who has raised sites knows that as soon as a web server is launched, requests begin to come to it. Also, DNS doesn’t really know about it, and the httpd error log file is already full of entries like these:
So I became interested, and I decided to study this issue in more depth.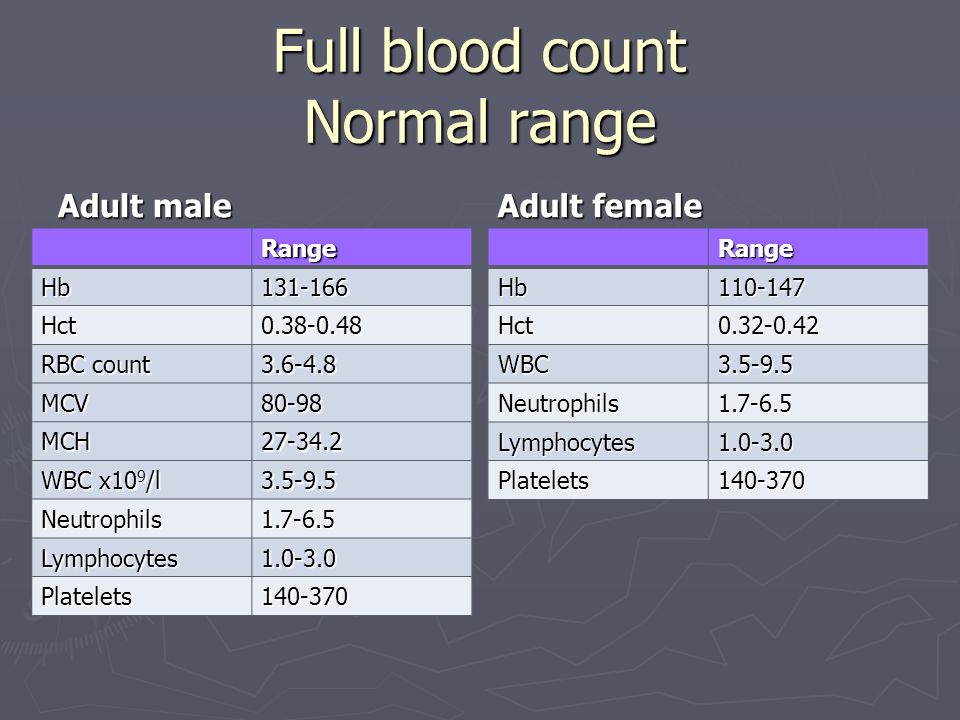 As soon as I had time, I wrote a web server log parser. Since I love visibility, I put the results on the map. nine0147 And here's the picture:
As soon as I had time, I wrote a web server log parser. Since I love visibility, I put the results on the map. nine0147 And here's the picture:
On the map, markers mark the locations determined by the IP addresses of the scanning sources. The free offline SxGeo library was used to obtain information, and the 2GIS API was used to display. Of course, due to the fact that the SxGeo library is free, it does not have high accuracy, and some addresses fall into the ocean. However, over time (at the moment I have accumulated statistics for 2 months), the picture becomes quite clear. nine0005
Surely some of the addresses are proxies. At the same time, scanning sources almost evenly cover the most IT-developed regions of the world.
However, as our beloved Mikhail Sergeevich Boyarsky would say - "A thousand devils", what is wrong with Australia?
In addition to the distribution of scan sources, I was also interested in collecting the target paths that scanners check. There were quite a few of those. Below I will give only a small part of the targets for example:
There were quite a few of those. Below I will give only a small part of the targets for example:
var/www/html/RPC2
/var/www/html/SQLite
/var/www/html/SQLiteManager
/var/www/html/SQLiteManager-1.2.4
/var/www/html/SQLite
/var/www/html/Snom
/var/www/html/Version.html
/var/www/html/Yealink
/var/www/html/\xd1\x86\xd1\x80\xd1\x89\xd1\x8b\xd1\x81\xd1\x84\xd1\x82\xd1\x8c\xd1\x83
/var/www/html/_PHPMYADMIN
/var/www/html/_pHpMyAdMiN
/var/www/html/_phpMyAdmin
/var/www/html/_phpmyadmin
/var/www/html/_query.php
/var/www/html/_whatsnew.html
/var/www/html/adm
/var/www/html/admin
/var/www/html/admin.php
/var/www/html/admin888
/var/www/html/admin_area
/var/www/html/admin_manage
/var/www/html/admin_manage_access
/var/www/html/admindb
/var/www/html/administrator
/var/www/html/administrator.php
/var/www/html/adminzone
Case game often seen:
/var/www/html/_PHPMYADMIN
/var/www/html/_pHpMyAdMiN
/var/www/html/_phpMyAdmin
/var/www/html/_phpmyadmin
There are also exotic targets that I certainly can't get anywhere:
/var/www/html/nmaplowercheck1523152976
/var/www/html/elastix_warning_authentication.php
You can get the full list of targets from the link in the footer. The trapping system now works in automatic mode and therefore is constantly replenished. nine0005
Okay, but what to do about it? The information we receive, like any other, can be used in different ways.
For example:
- When creating sites, especially based on standard CMS and using standard DBMS, it is desirable to change the standard names of directories and files. Do not leave installation directories after installation is complete. Do not place configuration files in the root directory or folder named "configuration", "config", etc. nine0210 Can be blocked at the iptables level from addresses that are being scanned. Of course, this is an extreme case, but there is such a possibility and it can be automated.
- Using the dictionary of caught targets, you can check the site structure for matches. For this, a simple script is used.
And another way to use "cool hackers" for their own purposes is to increase website traffic. This is both a joke and not.
It really works if you create files on your site based on the dictionary of caught targets, and place arbitrary text and counter code inside. This will only work, of course, if the scanner can execute JS (apapacy's plugin). nine0005
And this is a joke, because there are not so many really unique IP addresses of scanners. I caught 275 of them in 2 months. I didn’t count how many “smart” bots and browsers there are among them. Maybe not at all.
It should be noted that scanning was observed once from some addresses, while from others it was performed daily. But this process is constant. I wonder what share of traffic on the Web is occupied by scan traffic. Apparently not very big times no one is struggling with this.
Question: is it necessary to pay attention to scanning and what should be done in order not to become the prey of scanners? nine0005
P.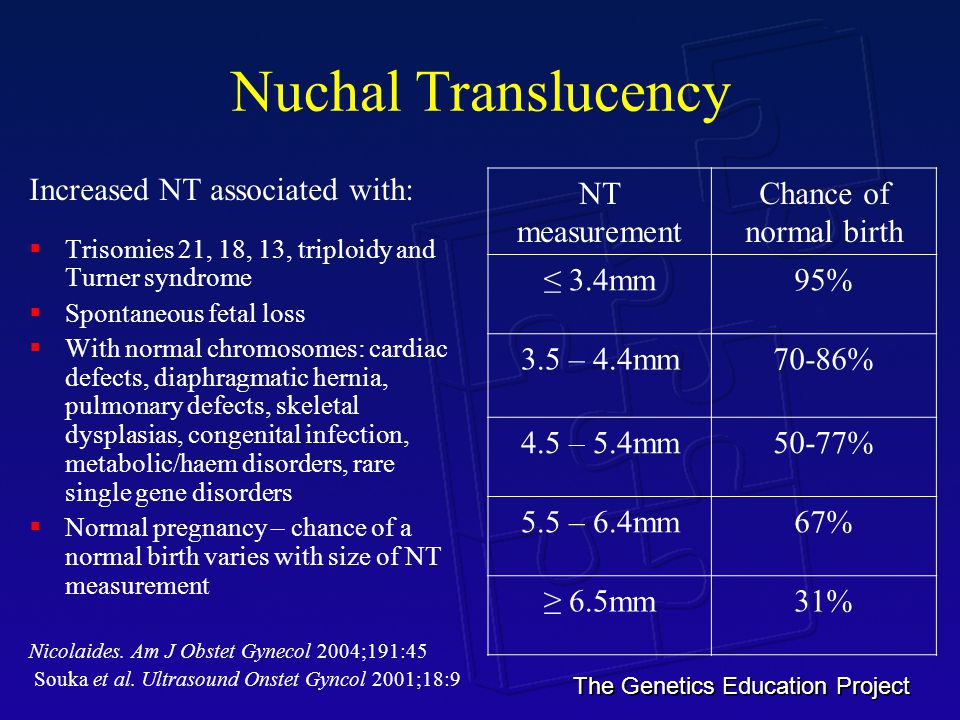 S.
S.
The phenomenon of scanning, although man-made, seems to have become a natural process for the Internet. It was and will be as long as the Network exists. This is a harmful factor from which you can protect yourself like glasses from solar ultraviolet radiation.
To sum up some of the discussion:
1. Australia does exist, but the Internet is expensive and scarce there. Same with NZ. But there is the ocean, beaches and kangaroos.
2. Scanning web resources is a special case of scanning real addresses on the Internet in general. Almost all standard ports and standard software serve as targets, and the geography of scanning sources coincides with the geography of the availability of "fast" Internet access. nine0005
3. Scanners work for a reason. Scanning is the first stage of hacking. Scanners are looking for possible vulnerabilities. The presence of such vulnerabilities can be used to infect servers with malware and/or to gain access to personal information.