Nt scan for pregnancy
NT Scan: What You’ll Find Out
If you recently found out you’re pregnant, you’ll have several doctor appointments and screenings from now until the birth of your baby. Prenatal screenings can identify problems with your health, such as anemia or gestational diabetes. Screenings also can monitor your baby-to-be’s health, and help identify chromosomal abnormalities.
Pregnancy screenings take place during the first, second, and third trimesters. The first trimester screening is a type of prenatal testing that provides your doctor with early information about your baby’s health — namely your baby’s risk for chromosome abnormalities.
A nuchal translucency (NT) scan screens your baby for these abnormalities. This test is typically scheduled between weeks 11 and 13 of pregnancy.
An NT scan is a common screening test that occurs during the first trimester of pregnancy. This test measures the size of the clear tissue, called the nuchal translucency, at the back of your baby’s neck.
It’s not unusual for a fetus to have fluid or clear space at the back of their neck. But too much clear space can indicate Down syndrome, or might show another chromosome abnormality like Patau syndrome or Edwards syndrome.
Our body cells have many parts, including a nucleus. The nucleus holds our genetic material. In most cases, the nucleus has 23 pairs of chromosomes, which are equally inherited from both parents.
Individuals born with Down syndrome have an extra copy of chromosome 21. Down syndrome, which can’t be cured, causes developmental delays and distinct physical characteristics.
These include:
- a small stature
- eyes with an upward slant
- low muscle tone
This condition affects 1 in every 700 babies born in the United States. It’s one of the most common genetic conditions.
Patau syndrome and Edwards syndrome are rare and often fatal chromosome abnormalities. Unfortunately, most babies born with these abnormalities die within the first year of life.
The clear space in the back of a developing baby’s neck can disappear by week 15, so an NT scan should be completed in the first trimester.
This test can also include blood work to measure your levels of plasma protein and human chorionic gonadotropin (HCG), a maternal hormone. Abnormal levels of either may indicate a chromosome problem.
During the screening, your doctor or a technician will take an abdominal ultrasound. You could alternatively have a transvaginal test, where an ultrasound probe is inserted through your vagina.
An ultrasound uses high frequency sound waves to create an image from inside your body. From this image, your doctor or technician measures the translucency, or clear space, at the back of your baby’s neck. They can then enter your age or date of birth in a computer program to calculate the risk of your baby having an abnormality.
An NT scan cannot diagnose Down syndrome or any other chromosome abnormality. The test only predicts the risk. Talk to your doctor about available blood tests. They also can help assess your baby’s risk.
Talk to your doctor about available blood tests. They also can help assess your baby’s risk.
As with any prediction, the accuracy rate varies. If you combine an NT scan with blood testing, the screening is about 85 percent accurate for predicting the risk of Down syndrome. If you don’t combine blood testing with the scan, the accuracy rate drops to 75 percent.
No special preparation is required for an NT scan. In most cases, testing is completed in about 30 minutes. During the scan, you’ll lie down on an exam table as the technician moves an ultrasound wand over your stomach.
The ultrasound pictures may be easier to read if you have a full bladder, so your doctor may recommend drinking water about one hour before your appointment. The ultrasound tech needs access to your lower abdomen, so make sure you wear comfortable clothing that makes it accessible.
Results from the scan may be available on the same day of testing, and your doctor may discuss the findings with you before you leave.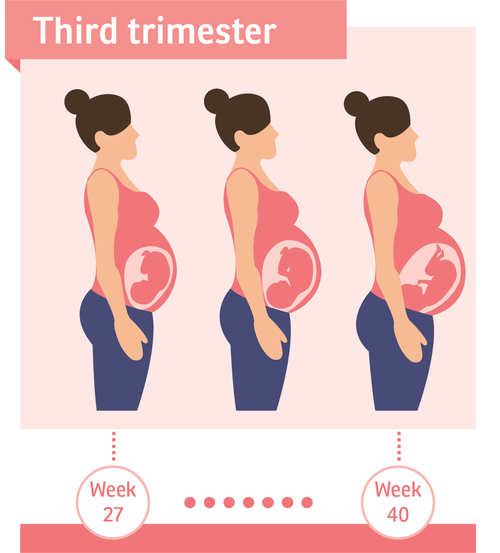 It’s important to remember that receiving an abnormal result from an NT scan doesn’t necessarily mean that your baby has a chromosome problem. Similarly, normal test results can’t guarantee that your baby won’t be born with Down syndrome.
It’s important to remember that receiving an abnormal result from an NT scan doesn’t necessarily mean that your baby has a chromosome problem. Similarly, normal test results can’t guarantee that your baby won’t be born with Down syndrome.
This test isn’t perfect. There’s a 5 percent false-positive rate. In other words, 5 percent of women tested receive positive results, but the baby is fine. After a positive result, your doctor may suggest another blood test called prenatal cell-free DNA screening. This test examines fetal DNA in your bloodstream to assess your baby’s risk for Down syndrome and other chromosome abnormalities.
It can be frightening to receive inconclusive or positive results from an NT scan. Keep in mind that an NT scan can only predict your baby’s risk: It doesn’t offer a definitive answer about chromosomal abnormalities. An NT scan is a screening test, not a diagnostic test.
There are differences between screening and diagnostic testing. The purpose of a screening test is to identify risk factors for a particular disease or condition. Diagnostic testing, on the other hand, confirms the presence of a disease or condition.
Diagnostic testing, on the other hand, confirms the presence of a disease or condition.
To diagnosis a chromosome abnormality, ask your doctor about diagnostic testing. Options include an amniocentesis, which is when a needle is inserted through your stomach into the amniotic sac to retrieve a fluid sample. Amniotic fluid contains cells that provide genetic information about your baby.
Another option is chorionic villus sampling. A sample of your placental tissue is removed and tested for chromosome abnormalities and genetic problems. There’s a small risk of miscarriage with both tests.
An NT scan is a safe, noninvasive test that doesn’t cause any harm to you or your baby. Keep in mind that this first trimester screening is recommended, but it’s optional. Some women skip this particular test because they don’t want to know their risk. Talk to your doctor if you experience anxiety, or are worried about how the results might affect you.
Nuchal translucency test (NT scan)
- Pregnancy
- Health & Safety
By Kate Marple
|
|
August 9, 2021
The NT scan is an ultrasound done in the first trimester to determine your baby's risk of having Down syndrome and some other chromosomal abnormalities. It's usually done along with a blood test. If the nuchal translucency test indicates that your baby may have a health condition, you can decide whether to have a diagnostic test to find out for certain.
It's usually done along with a blood test. If the nuchal translucency test indicates that your baby may have a health condition, you can decide whether to have a diagnostic test to find out for certain.
Photo credit: Thinkstock
- What is the nuchal translucency test?
- How is the nuchal translucency test done?
- How are NT scan results calculated?
- What do NT scan results mean?
- How accurate is the nuchal translucency test?
- What happens if my NT scan indicates a problem?
What is the nuchal translucency test?
The nuchal translucency test (also called the NT scan) uses ultrasound to assess your developing baby's risk of having Down syndrome (DS) and some other chromosomal abnormalities, as well as major congenital heart problems. It's offered to all pregnant women, along with a blood test, in first-trimester combined screening options.
The NT scan measures the clear (translucent) space in the tissue at the back of your baby's neck. (This is the "nuchal translucency.") Babies with abnormalities tend to accumulate more fluid at the back of their neck during the first trimester, causing this clear space to be larger than average.
(This is the "nuchal translucency.") Babies with abnormalities tend to accumulate more fluid at the back of their neck during the first trimester, causing this clear space to be larger than average.
The NT scan must be done when you're between 11 and 14 weeks pregnant, because this is when the base of your baby's neck is still transparent. (The last day you can have it is the day you turn 13 weeks and 6 days pregnant.)
Some practitioners also look for the presence of the fetal nasal bone during the NT scan. If no nasal bone is seen in the developing baby, some experts believe this increases the likelihood of chromosomal abnormalities. In some very specialized testing centers, other major abnormalities may be detected during the scan.
The NT scan is not invasive, and it's not conclusive. Diagnostic testing such as CVS or amniocentesis are necessary to confirm a positive screen result.
In addition to testing for Down syndrome (trisomy 21), the NT scan will also screen for:
- Trisomy 18 (Edward's syndrome)
- Trisomy 13 (Patau syndrome)
- Some other chromosomal abnormalities
- Some structural problems, such as heart, abdominal wall, and skeletal defects
If your baby's nuchal translucency measurement indicates that they are at increased risk for structural defects, you'll be given a special ultrasound (also called an advanced level or level II ultrasound) and a special test called a fetal echocardiogram, both in the second trimester.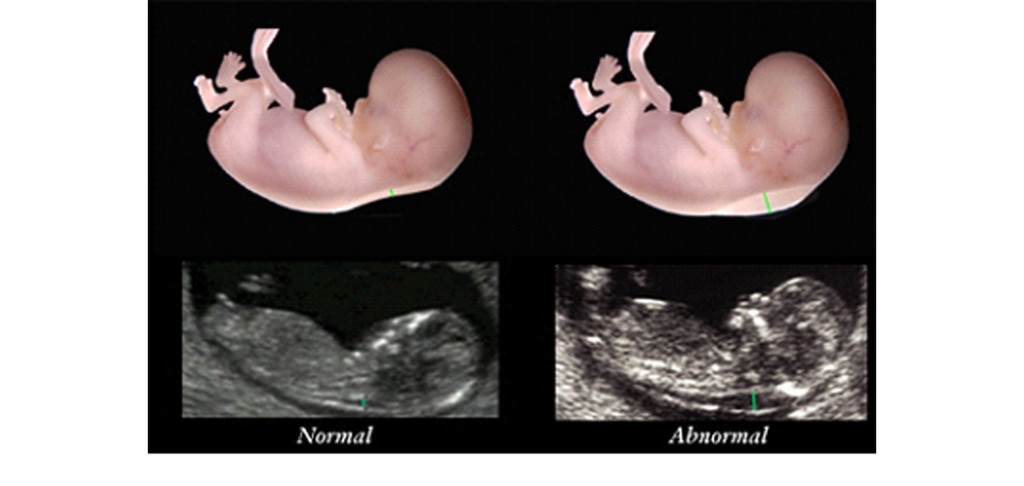 If your baby has a structural defect, they'll need to be monitored with regular ultrasounds and delivered at a medical center equipped to handle the condition.
If your baby has a structural defect, they'll need to be monitored with regular ultrasounds and delivered at a medical center equipped to handle the condition.
How is the nuchal translucency test done?
The sonographer first confirms your baby's gestational age by measuring them from crown to rump to see whether they're about the size they should be for their age. Then the sonographer positions the sensor, called the transducer, over your abdomen so that your baby's nuchal translucency shows up on the monitor and measures the thickness of it on the screen with calipers.
How are NT scan results calculated?
Your baby's chances of having a chromosomal abnormality are determined by the nuchal translucency measurement, your age, your baby's gestational age, and the blood test results.
Your age is factored in because although anyone can have a baby with a chromosomal abnormality, the risk increases as you age. For example, your likelihood of carrying a baby with Down syndrome ranges from approximately 1 in 1,200 at age 25 to 1 in 100 at age 40.
Because a baby's nuchal translucency normally gets a bit thicker with each day of gestation, researchers have been able to establish how large the translucent area should be each day during the three weeks the screening can be performed.
They've also calculated the statistical relationship between this measurement, the baby's age, the mother's age, and the likelihood that the baby will be born with certain abnormalities. In general, the thicker the nuchal translucency at a given gestational age, the higher the chance of a chromosomal problem.
You may get the results right away, or you may have to wait up to 10 days if the doctor has to send the data to a processing center.
What do NT scan results mean?
You'll want to talk with your practitioner or a genetic counselor about how to interpret the results, which can be confusing. Many centers will report each individual lab result as well as the final calculated result using a special formula.
The ratio
You'll get your results in the form of a ratio that expresses your baby's chances of having a chromosomal defect.
For example, a risk of 1 in 100 means that for every 100 women with this result, one baby will have Down syndrome and 99 will not. A risk of 1 in 1,200 means that for every 1,200 women with this result, one baby will have it and 1,199 will not. The higher the second number, the lower the risk.
Normal or abnormal results
You may also be told that your results are "normal" or "abnormal" for a particular condition, depending on whether the ratio is below or above a specified cutoff. For example, some tests use a cutoff of 1 in 250. So a result of 1 in 1,200 would be considered normal because the risk that there's a problem is lower than 1 in 250. A ratio of 1 in 100 would be considered abnormal because that risk is higher than 1 in 250.
Remember that a normal screening result (screen negative) isn't a guarantee that your baby has normal chromosomes, but it does suggest that a problem is unlikely. Likewise, an abnormal screening result (screen positive) doesn't mean that your baby has a chromosomal problem – just that your baby is more likely to have one. Most screen-positive babies turn out not to have a problem: Only about a third of babies with an increased nuchal translucency measurement turn out to have chromosomal defects.
Most screen-positive babies turn out not to have a problem: Only about a third of babies with an increased nuchal translucency measurement turn out to have chromosomal defects.
How accurate is the nuchal translucency test?
The NT scan alone will detect about 70 to 80 percent of babies with DS (depending on which study you look at). The detection rate for the NT scan plus a first-trimester blood test ranges from 79 to 90 percent. (Most tests will include both the NT scan and the blood test.)
This does not mean that a screen-positive baby has a 79 to 90 percent chance of having DS. It just means that 79 to 90 percent of babies who have DS will have screening results that are suspicious enough to recommend diagnostic testing. And 5 to 21 percent of babies who have DS will be determined to be at normal risk — that is, the results will be misleading.
False negative result
Screening tests aren't perfect. They don't detect all cases of DS, so they may identify your baby as being at low risk when they really do have DS.
In other words, if you're carrying a baby with DS, there's a 79 to 90 percent chance that the combined screening will detect the abnormality and give you what's called a screen-positive result indicating that further testing is recommended. But it also means there's a 5 to 21 percent chance that the tests will miss the DS and give you a screen-negative result.
This is called a false negative result, and it might lead you to decide against diagnostic testing that would have revealed a problem.
False positive result
These tests also have a 5 percent false-positive rate. A false-positive result is one that suggests that your baby is at increased risk for DS or another condition when, in fact, there's no problem.
What happens if my NT scan indicates a problem?
With the help of your practitioner or a genetic counselor, you'll want to decide whether the results indicate a high enough risk that you want to have CVS or amniocentesis to get a definitive diagnosis.
In making your decision, you'll need to weigh your need to know about your baby's condition against the small chance that diagnostic testing could cause a miscarriage.
If you decide not to have diagnostic testing, you can get more information about your baby's health and development by following up with NIPT (a blood test that's available to all pregnant women beginning at 10 weeks of pregnancy), the quad screen (a blood test in the second trimester), and a detailed ultrasound at 18 to 20 weeks.
This ultrasound can detect "soft markers" of chromosome disorders, such as short limbs, a bright dot in the heart, a bright bowel, and certain problems in the kidneys. It can also look for anatomical defects, such as spina bifida.
Sources
BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies.
We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies.
ACOG. 2020. Prenatal genetic screening tests. American College of Obstetricians and Gynecologists. https://www.acog.org/patient-resources/faqs/pregnancy/prenatal-genetic-screening-tests [Accessed August 2021]
March of Dimes. 2020. Down syndrome. https://www.marchofdimes.org/complications/down-syndrome.aspx [Accessed August 2021]
MedlinePlus. 2021. Nuchal translucency test. https://medlineplus.gov/ency/article/007561.htm [Accessed August 2021]
Nemours. 2015. Down syndrome. https://kidshealth.org/en/parents/down-syndrome.html?ref=search [Accessed August 2021]
NIH. 2017. What tests might I need during pregnancy? National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/preconceptioncare/conditioninfo/tests-needed [Accessed August 2021]
UptoDate. 2021. Should I have a screening test for Down syndrome during pregnancy? https://www. uptodate.com/contents/should-i-have-a-screening-test-for-down-syndrome-during-pregnancy-beyond-the-basics?topicRef=422&source=see_link [Accessed August 2021]
Show more
advertisement | page continues below
advertisement
Featured video
All pregnancy, parenting, and birth videos >
What you will learn from an NT scan during pregnancy
If you have recently found out that you are pregnant, you will have several visits to the doctor and check-ups before the baby is born. Prenatal screenings can reveal health problems such as anemia or gestational diabetes. Screening can also monitor the health of your unborn child and help identify chromosomal abnormalities.
Pregnancy screening is done in the first, second and third trimesters. First trimester screening is a type of prenatal testing that gives your doctor early information about your baby's health, namely your baby's risk of chromosomal abnormalities.
An occipital translucency (NT) scan checks your child for these abnormalities. This test is usually given between 11 and 13 weeks of pregnancy.
What is the purpose of an NT scan?
The NT scan is a common screening test done during the first trimester of pregnancy. This test measures the size of the transparent tissue, called the nuchal space, at the back of your child's neck.
It is not unusual for a fetus to have fluid or a clear space in the back of the neck. But too much free space can indicate Down syndrome or another chromosomal abnormality such as Patau syndrome or Edwards syndrome.
The cells in our body are made up of many parts, including the nucleus. The nucleus contains our genetic material. In most cases, the nucleus has 23 pairs of chromosomes, which are equally inherited from both parents.
People born with Down syndrome have an extra copy of chromosome 21. Down syndrome, which cannot be cured, causes developmental delay and various physical characteristics.
They include:
- short
- eyes tilted up
- low muscle tone
This condition affects 1 in every 700 babies born in the United States. This is one of the most common genetic conditions.
Patau syndrome and Edwards syndrome are rare and often fatal chromosomal abnormalities. Unfortunately, most children born with these anomalies die within the first year of life.
When is an NT scan scheduled during pregnancy?
The space at the back of the neck of a developing baby may disappear by 15 weeks, so an NT scan should be done in the first trimester.
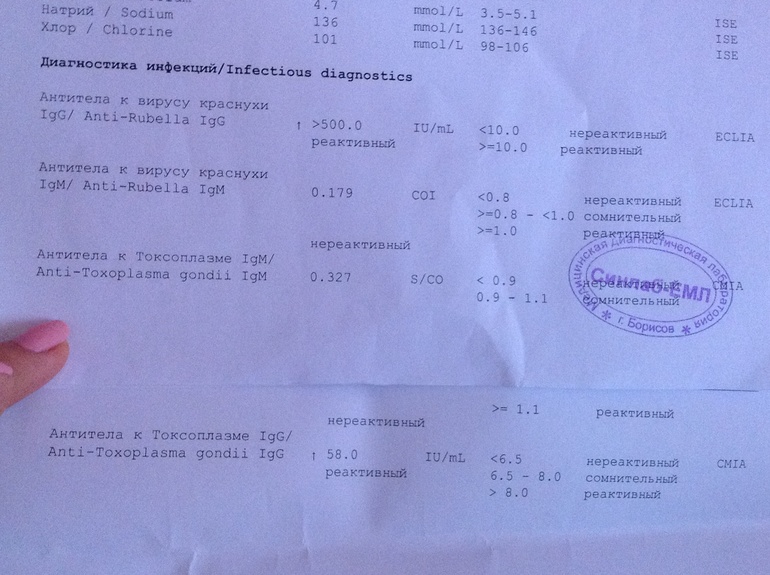
This test may also include a blood test to measure plasma protein and human chorionic gonadotropin (hCG), a maternal hormone. Abnormal levels of any of these may indicate a problem with the chromosome.
How does NT scanning work?
During the screening, your doctor or technician will perform an abdominal ultrasound. Alternatively, you can have a transvaginal test, in which an ultrasound probe is inserted through the vagina.
Ultrasound uses high frequency sound waves to create an image inside your body. From this image, your doctor or technician measures the transparency, or open space, in the back of your child's neck. They can then enter your age or date of birth into a computer program to calculate the risk of your child having an anomaly.
The NT scan cannot diagnose Down syndrome or any other chromosomal abnormality. The test only predicts risk. Talk to your doctor about available blood tests. They can also help assess the risk to your child.
As with any forecast, the degree of accuracy varies. If you combine an NT scan with a blood test, the screening is about 85 percent accurate in predicting the risk of Down syndrome. If you do not combine a blood test with a scan, the accuracy drops to 75 percent.
How to prepare for the test
NT scanning does not require special training. In most cases, testing is completed in about 30 minutes. During the scan, you will lie on the examination table while the technician passes the ultrasound probe over your abdomen.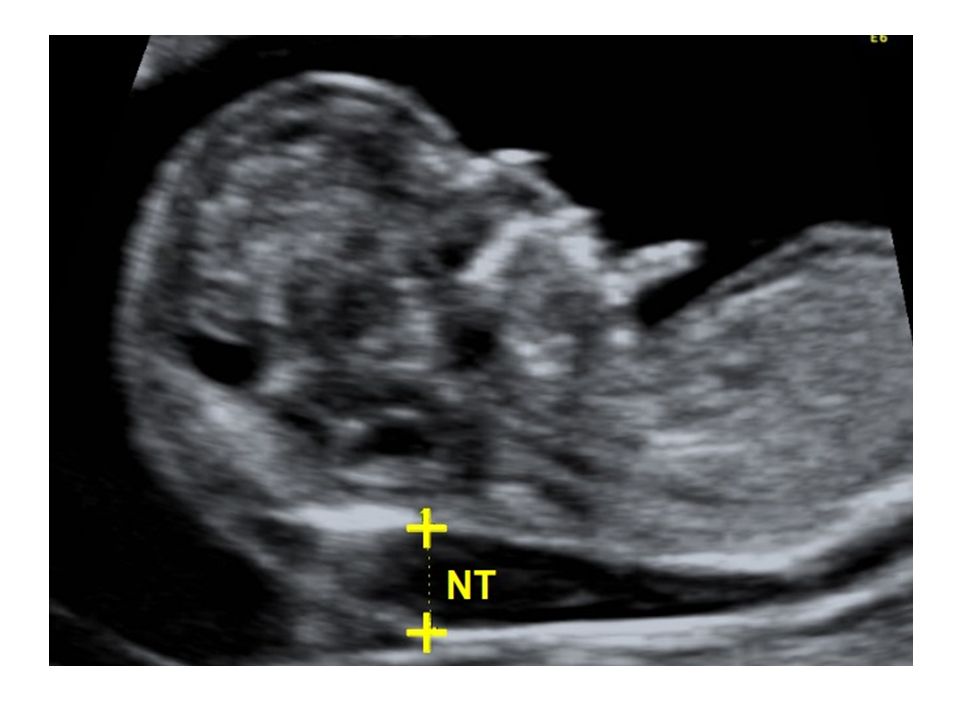
Ultrasound images may be easier to read if you have a full bladder, so your doctor may recommend drinking water about an hour before your appointment. The ultrasound technician needs access to the lower abdomen, so make sure you wear comfortable clothing that makes it accessible.
Scan results may be available on the day of the test and your doctor can discuss them with you before you leave. It is important to remember that getting an abnormal NT scan result does not necessarily mean that your child has chromosome problems. Similarly, normal test results cannot guarantee that your baby will not be born with Down syndrome.
This test isn't perfect. There's a 5 percent false-positive rate. In other words, 5 percent of women tested receive positive results, but the baby is fine. After a positive result, your doctor may suggest another blood test called prenatal cell-free DNA screening. This test examines fetal DNA in your bloodstream to assess your baby’s risk for Down syndrome and other chromosome abnormalities.
Screening versus diagnostic testing
Getting inconclusive or positive NT scan results can be scary. Keep in mind that an NT scan can only predict your child's risk: it does not give a definitive answer about chromosomal abnormalities. The NT scan is a screening test, not a diagnostic test.
There are differences between screening and diagnostic testing. The purpose of a screening test is to identify risk factors for a particular disease or condition. Diagnostic testing, on the other hand, confirms the presence of a disease or condition.
How to diagnose an abnormality
To diagnose a chromosomal abnormality, ask your doctor about diagnostic testing. Options include amniocentesis, where a needle is inserted through the stomach into the amniotic sac to obtain a fluid sample. The amniotic fluid contains cells that provide genetic information about your baby.
Another option is chorionic villus sampling. A sample of your placental tissue is taken and tested for chromosomal abnormalities and genetic problems. With both tests, there is a small risk of miscarriage.
With both tests, there is a small risk of miscarriage.
Conclusion
The NT scan is a safe, non-invasive test that does not harm you or your baby in any way. Keep in mind that this first trimester screening is recommended but not required. Some women skip this particular test because they don't want to know their risk. Talk to your doctor if you are worried or worried about how the results might affect you.
Transvaginal ultrasound | #06/98
When is it advisable to perform an ultrasound examination during pregnancy?
Is transvaginal scanning useful for postmenopausal bleeding?
How accurate is the method for examining ovarian pathology?
Transvaginal scanning has been carried out since 1986, when high-frequency 7-MHz probes first appeared. Since then, transvaginal scanning has been used in many areas of obstetrics and gynecology and currently serves as one of the main research methods.
- Obstetrics
With the help of a transvaginal scan, pregnancy is determined starting from five weeks, and from the sixth week, the fetal heartbeat is detected. Therefore, the method is used to confirm early pregnancy and determine the viability of the fetus. Also, multiple pregnancies can be detected in the early stages.
Therefore, the method is used to confirm early pregnancy and determine the viability of the fetus. Also, multiple pregnancies can be detected in the early stages.
| Figure 1. Cross section of the uterus with a 7.5-week-old fetus. Easily detectable fetal heartbeat |
With a positive pregnancy test result (increased HCG level) and the absence of a fetal bladder inside the uterus during scanning, you should immediately think about a possible ectopic pregnancy. In the case of bleeding from the implantation site during an ectopic pregnancy, blood is detected in the Douglas space using a scan. Sometimes, on the side of the uterus, closer to the ovaries, a volumetric formation is determined, and occasionally the embryo sac can also be seen.
Transvaginal scanning is a mandatory part of the examination of women referred to the hospital with bleeding and / or pain in early pregnancy. Thus, transvaginal scanning is the most important way to determine ectopic pregnancy.
Thus, transvaginal scanning is the most important way to determine ectopic pregnancy.
In addition to transvaginal scanning, it is advisable to assess quantitative HCG levels.
Bubble skid has inherent ultrasonic features. The large number of small bubbles that appear during the hydatidiform drift form many echoes, while the appearance of the scan is described by some as a snow storm.
| Figure 2 Dermoid ovarian cyst later histologically confirmed |
Later, at 16-20 weeks of pregnancy, a transvaginal scan is used to assess the length of the cervix, which helps to resolve the issue of possible cervical insufficiency and recommend that the woman put stitches on the cervix. With the help of transvaginal scanning, cervical dilatation can be detected and the integrity of the internal axis can be assessed.
In the process of managing a patient, transvaginal scanning can detect placenta previa and measure the distance between the edge of the placenta and the cervical canal in types I and II placenta previa.
- Menstrual disorders
Transvaginal scanning allows you to deal with a number of gynecological problems. In women with menstrual irregularities and abnormal uterine bleeding, transvaginal scanning assesses the size of the uterus, including the thickness of the endometrium.
| Figure 3 Endometrial cancer subsequently histologically confirmed |
You can also determine the size and number of myoma nodes. As a rule, it is visible whether or not there is a curvature of the uterine cavity. Thickening of the endometrium and absence of signal from the midline suggest the presence of an endometrial polyp.
Transvaginal scanning allows you to establish the exact localization of intrauterine devices, while the image quality is such that you can find out exactly which contraceptive device was used.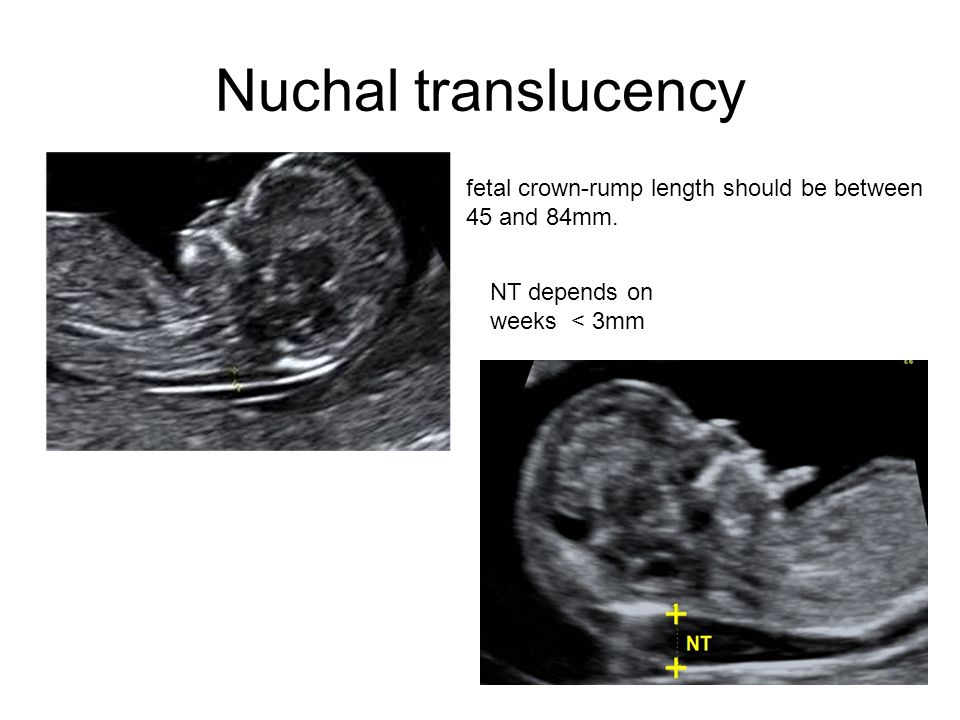 The benefit of this is obvious in cases where a woman has lost all information regarding the IUD.
The benefit of this is obvious in cases where a woman has lost all information regarding the IUD.
Transvaginal scanning is indicated when examining women presenting with postmenopausal bleeding. If the endometrium is thin, 3 mm or less, with the preservation of the subendometrial layer, serious pathological changes can be excluded. To finally verify this, hysteroscopy and / or endometrial biopsy is performed. With an endometrial thickness of more than 3 mm, biopsy analysis is mandatory.
Table 1. Transvaginal scanning in obstetricsEarly diagnosis of pregnancy
|
- Infertility
It is highly advisable to prescribe a transvaginal ultrasound scan as a baseline study for women suffering from infertility.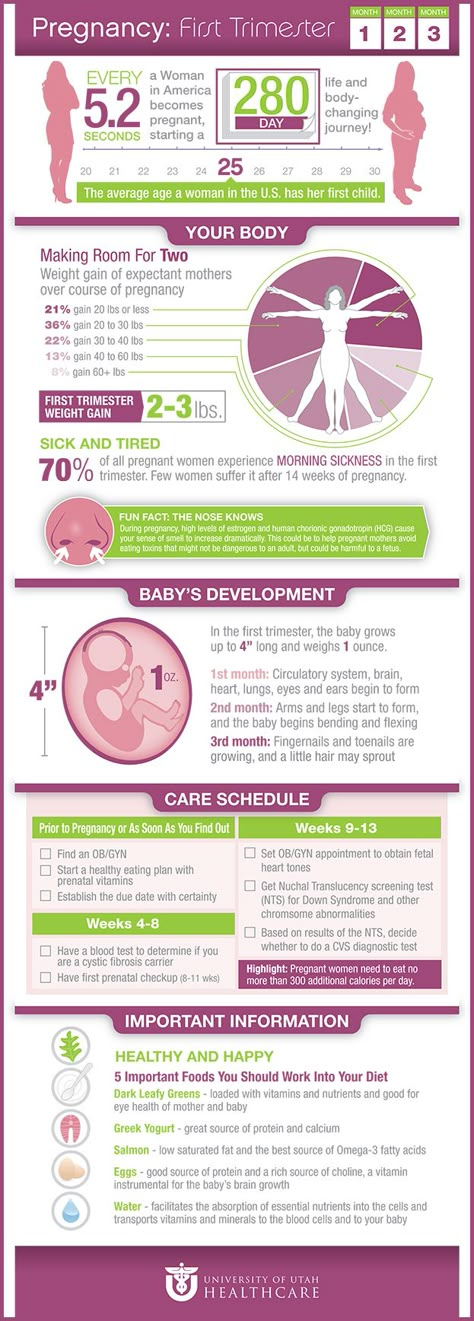
Determination of the size and morphological characteristics of the ovaries can reveal various anomalies, such as polycystic and multiple follicles. Sometimes it is possible to detect a previously unmanifested cyst, for example, a dermoid one.
When evaluating the uterus, it is possible to identify myomatous nodes, congenital malformations, for example, a bicornuate uterus. The hydrosalpinx appears as a fluid-filled structure, usually in the pouch of Douglas. Unlike ovarian cysts, hydrosalpinx tend to form septa extending two-thirds along the cyst.
Transvaginal ultrasound is used to monitor follicle growth during the natural cycle to determine if a woman is ovulating normally. It can also be used to monitor stimulated cycles, including ovulation induction with clomiphene, parenteral ovulation induction with FSH.
| Figure 4 Ovary with five follicles. |
Table 2. Transvaginal scanning in gynecologyMenstrual irregularities
|
Most often, transvaginal aspiration of the follicle under ultrasound control is used to extract the oocyte. This is the simplest technique, in addition, its advantage over laparoscopic extraction is the clear visibility of the oocyte even in the presence of pelvic adhesions. The same device is used for transvaginal drainage of ovarian cysts under ultrasound control.
The same device is used for transvaginal drainage of ovarian cysts under ultrasound control.
- Differential diagnosis of pelvic masses
Transvaginal ultrasound allows you to determine the nature of the formation, as well as to differentiate between malignant and benign formation.
In the group of young patients among benign formations, dermoid cysts are most common. Typically, these cysts are filled with highly reflective, echogenic fatty material that appears white on scans. These cysts are often bilateral, so the other ovary must be carefully examined.
Endometrioid cysts have a lower reflectivity and appear gray on the scan. Ultrasound methods cannot distinguish them from corpus luteum cysts, but the latter disappear within one to four weeks, while endometrioid cysts do not change in size during this time.
Benign cystic adenomas are usually single-chamber, in the presence of several chambers the partitions between them are thin - less than 3 mm.
Cystic adenocarcinomas are multilocular, with septa more than 3 mm thick. In addition, there may be solid germination in one or more chambers. If there is even the slightest suspicion of a malignant cyst, it is necessary to carefully look for free fluid in the abdominal cavity; it is advisable to take a blood sample to detect CA125, a non-specific marker of malignant neoplasms in the ovaries.
Other causes of masses in the pelvic cavity can be pelvic abscesses and diverticula. Abscesses appear gray on sonography; they can be confused with a pedunculated fibroid. The appearance of the diverticulum is complex and resembles an ovarian neoplasm.
Ultrasound becomes widely available
Ultrasound is the most important imaging modality in the first trimester of pregnancy, especially for early detection of abnormalities and early diagnosis of ectopic pregnancy.
The ideal location for first trimester ultrasound is in the early pregnancy ward, which is now taken into account in many hospitals.