Not gaining weight in pregnancy
How to Know If You're Not Gaining Enough
Many women struggle with gaining too much weight during pregnancy. But what happens when the opposite is true, and you’re not gaining enough weight during pregnancy? Here’s what you need to know about weight gain during pregnancy.
If you’d like to learn more about this topic in a visual way, check out my Google web stories for 6 tips to help you gain weight during pregnancy.
There may be several reasons that you’re not gaining enough weight during pregnancy—it could be due to excessive nausea, loss of appetite, food aversions, or other digestive concerns. If you’re concerned that you’re not gaining enough weigh, don’t worry. I’ve got you covered. Plus, check this out if you’re looking for the ultimate guide to pregnancy nutrition.
In this post you’ll learn:
- How to figure out how much weight you should gain
- Calorie intake during pregnancy (how do I know how much to eat?)
- How to choose calorie and nutrient-dense foods
- Why Smaller more frequent meals might help
- Why you might want to skip the salad
- Why you shouldn’t turn towards junk food for extra calories
- How to combat nausea
- How to notice food aversions
How to know whether you’re gaining the right amount of weight during pregnancy
First of all, it’s important to understand what healthy pregnancy weight gain looks like. A common way to calculate your target weight gain during pregnancy is by using your pre-pregnancy Body Mass Index (BMI).
Now, I really don’t want to get stuck on the numbers here—especially when it comes to your body mass index (BMI)—because what’s defined as “healthy” according to BMI charts can be a little deceiving or unfair. For example, someone who has lots of muscle may have a higher BMI than what’s considered “healthy,” but may be in great shape and very healthy. Or someone who has a “healthy” BMI due to their genetics may have an unvaried diet and never move their body. BMI is just one assessment tool you can use, but it’s imperfect. Don’t get stuck on it! But for those of you who like numbers, here they are:
To calculate your pre-pregnancy BMI, multiply your weight in kilograms by your height in meters squared. Or if you want a shortcut, just google “BMI calculator” and plug your numbers in. The recommended weight gain during pregnancy depends on which category the pre-pregnancy BMI lands in.
Pregnancy Weight Gain
| Prepregnancy BMI | Weight category | Weight gain for full-term pregnancy | Weight gain for full-term pregnancy with twins |
| Below 18.5 | Underweight | 28 to 40 pounds | No set guidelines |
| 18.5 to 24.9 | Normal weight | 25 to 35 pounds | 37 to 54 pounds |
| 25.0 to 29.9 | Overweight | 15 to 25 pounds | 31 to 50 pounds |
| 30.0 and above | Obese | 11 to 20 pounds | 25 to 42 pounds |
Calorie intake during pregnancy
I’m not keen on overemphasizing calorie goals or ranges because I really want to encourage you to listen to your body when it comes to the amount of food you eat at any given meal or snack. And quite frankly, counting calories sucks and takes the enjoyment out of eating! But here’s what I will tell you:
- During your first trimester, it’s not necessary to eat any more than normal.
 So just eat like you normally would!
So just eat like you normally would! - During the second trimester, it makes sense that you’re hungrier than normal, because your energy and nutrient needs are rising. It’s good to eat a little more: about 300 to 350 extra calories. That’s like an extra snack each day.
- During the third trimester is when your nutrient and energy needs are the highest throughout your pregnancy, and it’s advised to eat an extra 400 to 450 calories per day. That could be an extra snack (Greek yogurt, berries, and granola) or maybe a little more at each meal.
How many extra calories do I need (assuming that you’re starting out at a healthy BMI)?
| Stage of pregnancy | Calorie intake |
| First trimester | No additional calories |
| Second trimester | Add 300 to 350 calories per day |
| Third trimester | Add 400 to 450 calories per day |
Any additional calories that you take in should come from nutrient-dense foods such as lean protein, vegetables, fruits, and whole grains. Limit foods that are overly processed with a lot of added sugar, salt, or fat to only once in a while. But do give yourself permission to indulge once a day on something that you absolutely love and can’t live without.
Limit foods that are overly processed with a lot of added sugar, salt, or fat to only once in a while. But do give yourself permission to indulge once a day on something that you absolutely love and can’t live without.
I’m having trouble gaining enough
If you’re having trouble gaining enough weight during pregnancy, know that you’re not alone. This is a common concern and something that can be managed with a little bit of extra knowledge and even some help from a registered dietitian if you and/or your doctor are concerned. Lack of weight gain can happen because of many reasons, including:
- excessive nausea
- loss of appetite
- food aversions
- other digestive concerns
- you might be a small or particular eater to begin with, and may need to pay a little bit more attention to what and how much you’re eating.
To help ensure that you are gaining enough weight throughout your pregnancy, and in a healthy way, here are my top 6 tips:
1.
 Choose calorie-dense (and nutrient-dense) foods
Choose calorie-dense (and nutrient-dense) foodsIf you have a small appetite, it’s crucial to make every bite count! That means you want to get the most nutrition (protein, vitamins, minerals etc.)in the foods you choose. Even if you get full quickly or have a small appetite, you know you took in some great nutrition. Foods that are high in calories and chock-full of nutrients are:
- Nuts, seeds, and nut butters
- Avocados
- Olive oil as a topping or dressing
- Whole grain pasta, oats, brown rice, and other whole grains
- Legumes like lentils, chickpeas, and beans
- Fatty fish like salmon
If you’re needing some recipe inspiration for nutrient-dense meals and snacks, check out one of my fave cookbooks, Nourish. On top of this, you should be making sure that you’re taking a prenatal multivitamin, vitamin D and perhaps even an Omega-3 supplement too. Here are some nutrients (and foods) that you should be paying extra attention to during pregnancy.
2. Try smaller, more frequent meals
You may be turned off of larger portion sizes of foods, and eating might feel overwhelming if your plate is too full (which can actually decrease your appetite). Instead, try having five or six smaller more snack-sized, lighter meals that aren’t so overwhelming. For example, instead of having a big spaghetti dinner, have a piece of French toast with greek yogurt and berries. Or make a batch of homemade protein-rich muffins or energy bites that you can snack on throughout the day or on-the-go. These snack-sized meals can still pack a nutritional punch and provide the calories that you need, but might be less overwhelming and more appealing (meaning, you’ll eat more!).
3. Salads are great but may be too low in calories
Wait, what? Did a dietitian just advise you to skip a salad? While vegetables are super-healthy, they are not calorically-dense and high in fiber. A big bowl of lettuce with cucumber can make you feel full quickly, but is too low in calories. That’s not enough to meet your needs! If you really have a low appetite and can eat only a small amount, it’s better to have more calories with every bite. For example, try whole grain toast with peanut butter and banana slices (yes, you CAN and SHOULD eat peanuts when you’re pregnant), or a pasta salad with avocado, nuts, meat and cooked veggies which would have more calories than a light green salad.
That’s not enough to meet your needs! If you really have a low appetite and can eat only a small amount, it’s better to have more calories with every bite. For example, try whole grain toast with peanut butter and banana slices (yes, you CAN and SHOULD eat peanuts when you’re pregnant), or a pasta salad with avocado, nuts, meat and cooked veggies which would have more calories than a light green salad.
Look at the numbers to see what I mean:
- Whole grain toast with 1 tablespoon peanut butter and a banana: 220 calories
- 1½ cups romaine lettuce and cucumbers: 20 calories
- 1½ cups romaine lettuce, cucumbers, and 1 teaspoon dressing: 60 calories
If you ARE craving salad, what can you add to it? Maybe it means adding a tablespoon of dressing to your lettuce, and topping it with nuts, seeds, chickpeas, quinoa, avocado, or any other calorie-dense foods.
4. Energy dense foods are fine in moderation
We know what you’re thinking: “I need to eat more calories! I can have all of the ice cream I’ve ever wanted!” If only it were that easy! Yes, you need more calories.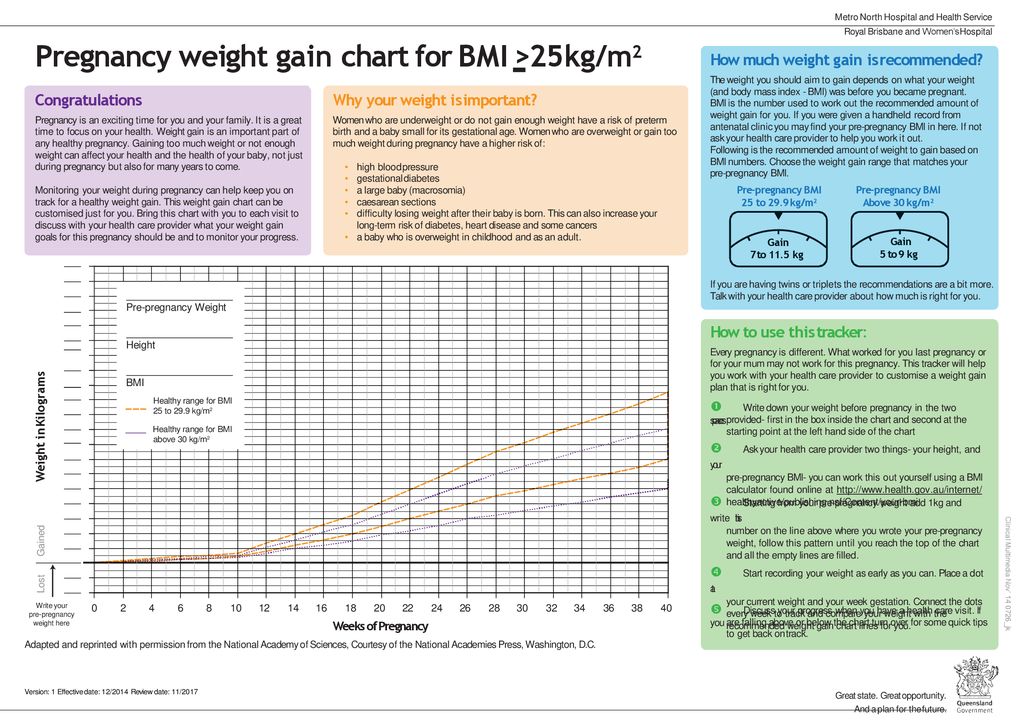 BUT. You also don’t need tons of sugar and fat. You want the calories to come from nutritious foods (see list above). Of course, you can enjoy ice cream mindfully, but please don’t get your day’s worth of calories from pint after pint of creamy goodness.
BUT. You also don’t need tons of sugar and fat. You want the calories to come from nutritious foods (see list above). Of course, you can enjoy ice cream mindfully, but please don’t get your day’s worth of calories from pint after pint of creamy goodness.
5. Combat nausea in pregnancy
Morning sickness can sometimes turn into all-day-sickness. Luckily, by the time you enter your second trimester, when weight gain starts to ramp up, nausea usually starts to wind down. If you’re one of the unlucky (approximately half of all pregnant women) who feels pregnancy-related nausea, here are some tricks that may help:
- Keep a snack on your night table. Have a bite before bed and in the morning. Soda crackers are a popular option!
- Avoid getting too hungry – that can lead to nausea. It might be your first instinct to avoid food when you feel nauseous, but that is the opposite of what you should do. Eating every two to three hours will help keep nausea at bay! Keep high calorie snack options (like nuts) with you throughout the day.

- Don’t take your nutrition supplements on an empty stomach–make sure you combine with a meal or snack.
- Try ginger. This age old-remedy is backed by science too. Try making tea with fresh ginger. You can use ginger in cooking and baking. Ginger snaps anyone?
- Stay hydrated, especially if nausea is accompanied by vomiting. Try drinking your fluids before or after meals, as opposed to with your meal. This is my favourite water bottle (that I carry around always!) to help me remember to stay hydrated.
If none of these tips help and you really can’t keep any food down, you may have hyperemesis gravidarum, and should discuss it with your doctor. They can prescribe medication to help.
6. Notice food aversions in pregnancy
There may be certain smells or flavors that turn your stomach when you’re pregnant – and often they are foods you used to love. Common food aversions are to strong flavors, such as garlic, onion, spice and coffee. If you can’t stand the taste or smell of certain foods, simply avoid them. Know that it’s totally normal, it’s common, and it will pass!
Know that it’s totally normal, it’s common, and it will pass!
Commonly Asked Questions About Pregnancy Weight Gain
How much weight should you gain while pregnant?
The weight gain ranges below are for a full-term pregnancy:
• Underweight: 28 to 40 pounds
• Normal: 25 to 35 pounds
• Overweight: 15 to 25 pounds
• “Obese”: 11 to 20 pounds
How fast do you gain weight when pregnant?
On average, people gain 1 to 4 pounds in the first trimester — but it can vary. Expect to gain ½ a pound to one pound (. 23 to . 45 kg) per week during the rest of your pregnancy. Ultimate guide to pregnancy nutrition.
How soon do you gain weight when pregnant?
Some initial weight gain will happen in the first 12 weeks of pregnancy. The majority of weight gain will occur during the second and third trimester. How much is too much?
How much is too much?
If you need some personalized guidance on your nutrition during pregnancy, contact us to book an appointment with our dietitian team (most people have coverage for our services through their health benefits plan).
Food to Grow On
Food to Grow On is the definitive guide to childhood nutrition, packed with practical advice to support you through pregnancy, and up until your little one starts school.
Laid out in an easy-to-navigate question and answer style, this book provides practical advice and support from Sarah Remmer and Cara Rosenbloom, two trusted registered dietitians (and moms). Food to Grow On is packed with hard-earned parenting wisdom and the very latest research in pediatric nutrition, so you will feel supported, understood, and ready to help your child thrive.
Buy Food to Grow On Now!
Not Gaining Weight During Pregnancy? What's Normal & What's Not
Pregnancy
Shutterstock
Experts *weigh* in.
by Jessica Booth
It only makes sense that being pregnant means packing on some extra pounds — your body is literally growing another human being. For most pregnant people, some weight gain isn’t just expected, it’s encouraged. But, for some, the number on the scale doesn’t really go up, and they might start to wonder if it’s normal to not gain weight during pregnancy, or if something could be wrong. When you hear some pregnant people talk about gaining 30, 50, or 100 pounds, meanwhile you’re pregnant but not gaining weight, it can be unnerving. Before you freak out, take a deep breath and remember that your weight during pregnancy — gain or or lack thereof — doesn’t always mean that something is wrong with the baby.
Is it normal to not gain weight during pregnancy?
Only about one-third (32%) of women gain the recommended amount of weight during pregnancy. Most women (48%) gain more than the recommendations, and some women (21%) gain less, per the Centers of Disease Control and Prevention (CDC).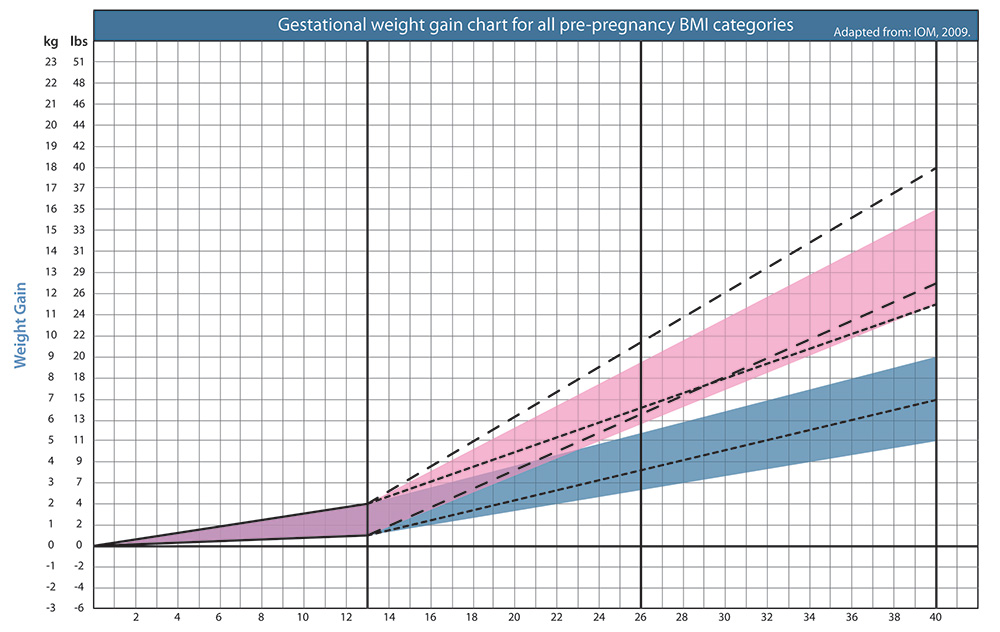 The amount of weight your doctor or health care professional will usually suggest that you gain during pregnancy depends on your body mass index (BMI). That means that it suggested average weight gain recommendations will varies from person to person. This makes it hard to say what is really “normal” and what isn’t, explains Dr. Mary Jacobson, M.D., OB-GYN and chief medical advisor for Alpha Medical. The reason obstetricians care about your the number on the scale — and might be concerned if you’re not gaining weight during pregnancy — is because gaining less than the recommended amount can be associated with birthing smaller babies, which can come with its own set of risks, like difficulty breastfeeding and increased risk of illness.
The amount of weight your doctor or health care professional will usually suggest that you gain during pregnancy depends on your body mass index (BMI). That means that it suggested average weight gain recommendations will varies from person to person. This makes it hard to say what is really “normal” and what isn’t, explains Dr. Mary Jacobson, M.D., OB-GYN and chief medical advisor for Alpha Medical. The reason obstetricians care about your the number on the scale — and might be concerned if you’re not gaining weight during pregnancy — is because gaining less than the recommended amount can be associated with birthing smaller babies, which can come with its own set of risks, like difficulty breastfeeding and increased risk of illness.
Still, sometimes it can be difficult for a pregnant woman to gain weight. Jacobson notes that the below reasons can contribute to no or very little weight gain during pregnancy:
- Calorie restriction
- Hyperemesis gravidarum, a condition that causes severe nausea and vomiting during pregnancy
- Autoimmune disorders such as rheumatoid arthritis and systemic lupus erythematosus
- Cancer
Keep in mind that weight gain doesn’t always happen during the first few weeks of pregnancy, especially if you’re experiencing a lot of nausea or morning sickness and having trouble keeping food down. If you’re not gaining weight in the first trimester of pregnancy, rest assured that you’re in good company. For many pregnant people, pregnancy weight gain doesn’t begin until the second trimester. In fact, some women with morning sickness will actually lose weight in the first trimester, Dr. Jill Purdie, M.D., OB-GYN and medical director at Northside Women’s Specialists in Atlanta, Georgia, tells Romper. The weight is often re-gained once the nausea and vomiting stops. If you’re struggling to maintain weight in the first trimester, don’t stress. Just be sure to drink plenty of water, reminds Purdie, because it is easy to become dehydrated when pregnant.
If you’re not gaining weight in the first trimester of pregnancy, rest assured that you’re in good company. For many pregnant people, pregnancy weight gain doesn’t begin until the second trimester. In fact, some women with morning sickness will actually lose weight in the first trimester, Dr. Jill Purdie, M.D., OB-GYN and medical director at Northside Women’s Specialists in Atlanta, Georgia, tells Romper. The weight is often re-gained once the nausea and vomiting stops. If you’re struggling to maintain weight in the first trimester, don’t stress. Just be sure to drink plenty of water, reminds Purdie, because it is easy to become dehydrated when pregnant.
How much weight gain in pregnancy is considered normal?
There is no one ideal weight you should aspire to when you’re pregnant, as the “normal” amount varies for each person. “How much weight a person should gain in pregnancy is dependent on their body mass index,” explains Jacobson. “BMI is a measurement of body fat based on height and weight. It can be calculated using pounds and inches: BMI = (weight in pounds x 703) / (height in inches x height in inches). It is also dependent on if they have a singleton or multiple gestation (more than one fetus in utero) pregnancy.”
It can be calculated using pounds and inches: BMI = (weight in pounds x 703) / (height in inches x height in inches). It is also dependent on if they have a singleton or multiple gestation (more than one fetus in utero) pregnancy.”
The Institute of Medicine offers a chart of expected weight gain during a single or twin pregnancy, which Jacobson recommends looking at and following. For a single pregnancy:
- If before getting pregnant you had a BMI under 18.5, you should gain 28-40 pounds.
- If before getting pregnant you had a BMI between 18.5 and 24.9, you should gain 25-35 pounds.
- If before getting pregnant you had a BMI between 25 and 29.9, you should gain 15-25 pounds.
- If before getting pregnant you had a BMI over 30, you should gain 11-20 pounds.
Remember, these are general recommendations. If you are not gaining weight during pregnancy so far, talk to your health care provider. If they aren’t concerned, then you likely don’t need to be either.
When to be concerned about your weight in pregnancy
Everyone’s body is different, which means that not everyone will gain the recommended amount of weight during pregnancy — and sometimes that’s totally fine. Sometimes, though, not gaining weight during pregnancy is cause for concern. Your medical provider will probably check your weight at each appointment. If they notice something they’re worried about, they will look into it. Or, if you’re worried, you should feel empowered to ask them for more information.
“If the size of your uterus, measured as fundal height from your pubic bone to the top of your uterus, is not progressively increasing after 20 weeks gestation, your obstetric clinician will recommend a ‘growth scan’ or abdominal ultrasound to measure different aspects of the fetus, like head circumference, abdominal circumference, and femur length, as well as pockets of amniotic fluid around the fetus in order to make a treatment plan,” Jacobson says.
ShutterstockHow to gain weight with severe morning sickness
Again, it’s extremely normal to not gain much weight during the first trimester of pregnancy, and those who struggle with morning sickness may even lose weight. If you’re worried, though, try eating small, frequent meals. The food you do eat should be high in carbohydrates and low in fat. If you know certain foods make you feel more sick, avoid them at all costs. Eat foods with higher levels of protein and calories, like protein shakes or supplement shakes, advises Purdie.
If you’re worried, though, try eating small, frequent meals. The food you do eat should be high in carbohydrates and low in fat. If you know certain foods make you feel more sick, avoid them at all costs. Eat foods with higher levels of protein and calories, like protein shakes or supplement shakes, advises Purdie.
Other popular nausea remedies for the first trimester include drinking ginger tea, acupressure devices like Sea-Bands, or a combination of vitamin B6 and Unisom at bedtime. Be sure to clear this — and any new medications — with your OB-GYN before trying them.
Experts:
Dr. Mary Jacobson, M.D., OB-GYN and chief medical advisor for Alpha Medical
Dr. Jill Purdie, M.D., OB-GYN and medical director at Northside Women’s Specialists
Weight gain during pregnancy - how not to gain weight?
Contents:
- What are the optimal weight limits?
- Pregnancy Weight Chart
- How to weigh yourself correctly during pregnancy
- Why does weight gain occur?
During pregnancy, it is important for a woman to eat a varied diet so as not to deprive the unborn baby of essential minerals and nutrients. Both excessive weight gain and weight loss are equally dangerous. But evidence suggests that more than half of European and American women gain more weight during pregnancy than recommended 1 . So now is the time to give up what does not bring any benefit, but only extra pounds: sweet, fatty, fast food. Being overweight can cause problems during pregnancy and childbirth.
Both excessive weight gain and weight loss are equally dangerous. But evidence suggests that more than half of European and American women gain more weight during pregnancy than recommended 1 . So now is the time to give up what does not bring any benefit, but only extra pounds: sweet, fatty, fast food. Being overweight can cause problems during pregnancy and childbirth.
What are the optimal weight limits?
The average weight gain during pregnancy is about 10-12.5 kilograms 2 . But a child is born weighing 3-4 kilograms, where does everything else come from and when does the excess go away?
In addition to the fetus itself, the uterus and breasts become larger in preparation for feeding. Muscle and fat increase - the body stores energy.
This is how the weight gained by a woman during pregnancy is distributed on the eve of feeding,
0.9 kg - amniotic fluid,
1.4–1.8 kg - blood and organic fluids, thanks to which the child receives the necessary oxygen,
0. 9 kg - uterus (20 times more than normal weight),
9 kg - uterus (20 times more than normal weight),
0.7 kg - placenta, the main element through which the fetus receives nutrients.
Add the weight of the unborn baby, and you will get the approximate weight that a woman gains in nine months.
Doctors say that everything is individual and there are no uniform standards for how many kilograms to gain during pregnancy. But let things take their course, there is something horrible and you can’t completely forget about the scales. Watch your weight - you will avoid many problems during pregnancy and childbirth and easily return to your previous weight. You will have "strategic reserves" for feeding the baby. Don't worry, those extra pounds will go away as quickly as they appeared. But only on the condition that you eat right during pregnancy and lactation.
Pregnancy weight chart
The recommended weight gain during pregnancy for women with a normal body mass index is 11.5-16 kilograms. Those who are overweight during pregnancy are advised to gain a little less - from 7 to 11. 5 kilograms. Those who are expecting twins or triplets, on the contrary, should score more. For example, in a multiple pregnancy with twins for a woman of normal weight, the recommended weight gain is from 16.8 to 24.5 kilograms 3 .
5 kilograms. Those who are expecting twins or triplets, on the contrary, should score more. For example, in a multiple pregnancy with twins for a woman of normal weight, the recommended weight gain is from 16.8 to 24.5 kilograms 3 .
Trimester weight gain during pregnancy varies 3 . A woman gains the least during the first trimester - from 1.6 to 2.3 kg. Nausea in the first trimester usually causes loss of appetite and some weight loss may occur.
In the second and third trimesters, a woman gains an average of 200 to 500 g per week.
Pregnancy weight gain: weekly chart, weight in kilograms
| Week | Minimum | Average weight | Maximum |
|---|---|---|---|
| 14 | 1.1 | 1.5 | 1.9 |
| 15 | 1.6 | 2 | 2. 4 4 |
| 16 | 1.9 | 2.3 | 2.8 |
| 17 | 2.2 | 2.8 | 3.4 |
| 18 | 2.5 | 2.8 | 3.4 |
| 19 | 3 | 3.7 | 4.5 |
| 20 | 3.5 | 4.2 | 5 |
| 21 | 3.9 | 4.7 | 5.6 |
| 22 | 4.2 | 5.2 | 6.2 |
| 23 | 4.6 | 5.7 | 6.9 |
| 24 | 4.9 | 6.1 | 7.4 |
| 25 | 5.3 | 6.6 | 8 |
| 26 | 5.6 | 7 | 8.5 |
| 27 | 6 | 7.5 | 9 |
| 28 | 6.3 | 7.9 | 9.5 |
| 29 | 6.7 | 8.3 | 9.9 |
| 30 | 7 | 8. 7 7 | 10.4 |
| 31 | 7.3 | 9 | 10.8 |
| 32 | 7.5 | 9.4 | 11.3 |
| 33 | 7.8 | 9.7 | 11.7 |
| 34 | 8.1 | 10.1 | 12.1 |
| 35 | 8.4 | 10.5 | 12.6 |
| 36 | 8.6 | 10.8 | 13 |
| 37 | 9 | 11.2 | 13.5 |
| 38 | 9.3 | 11.6 | 14 |
| 39 | 9.4 | 11.7 | 14.1 |
| 40 | 9.5 | 11.8 | 14.2 |
How to weigh yourself correctly during pregnancy
Doctors do not recommend weighing yourself daily, it is not always informative, fluctuations are not always noticeable, the error is large, and in general this can lead to unnecessary worries.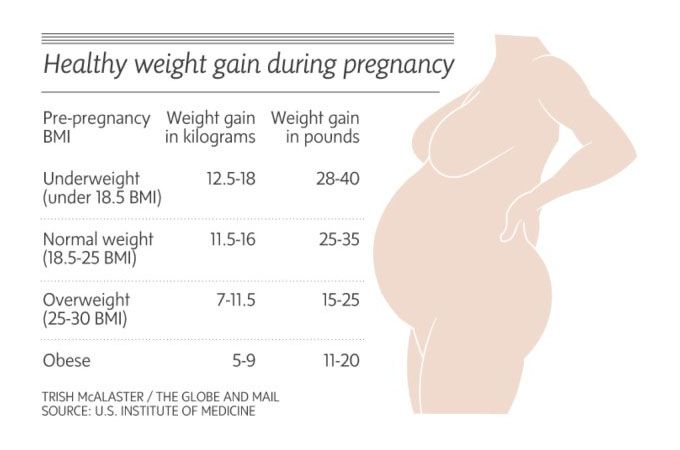 The correct option: control the weight once a week, in the morning, on an empty stomach. It is important to use the same scales, now the priority is “dynamics”. Weigh yourself only at home or in the office of your gynecologist.
The correct option: control the weight once a week, in the morning, on an empty stomach. It is important to use the same scales, now the priority is “dynamics”. Weigh yourself only at home or in the office of your gynecologist.
Why does weight gain occur?
Excess weight is caused by hormonal changes in the body, which makes the expectant mother constantly feel hungry. Many pregnant women decide that now they need to eat for two. No need. Just eat twice as good - more varied, more correct, but not more.
Sources:
* Not a drug. dietary supplement. There are contraindications. ** Estimated period of use within the Elevit line of vitamin and mineral complexes. According to the instructions, Elevit Pronatal can be used at the stage of pregnancy planning, during pregnancy, after childbirth and during breastfeeding.
- Healthy maternal nutrition: a better start to life report WHO, Regional Office for Europe 2016.
- https://www.nhs.uk/common-health-questions/pregnancy/how-much-weight-will-i-put-on-during-my-pregnancy/
- Poston L.
 Gestational weight gain // https://www.uptodate.com/contents/gestational-weight-gain, accessed 07.10.2018.
Gestational weight gain // https://www.uptodate.com/contents/gestational-weight-gain, accessed 07.10.2018.
CH-20220504-32
Fetal growth restriction (FGR)
Gynecology
It happens that expectant mothers hear a frighteningly incomprehensible abbreviation - ZRP at the appointment with the attending physician or in the ultrasound room. Its decoding is even more frightening: "delayed fetal development." A pregnant woman faced with a similar diagnosis is tormented by many questions. How dangerous is this condition? How will it affect the health of the baby? Will he be able to catch up?
Adult people are not alike, and among the many external differences they differ in height and weight. Even the same person at different periods of his life can lose weight or gain weight, and this does not cause alarm in anyone. Very young children are another matter: clear criteria are calculated for them, a deviation from which indicates that something is wrong with the baby. And the smaller the child, the more important is the correspondence of his physical development to certain norms. And to assess the state of intrauterine development of the fetus, its size is the most objective criterion.
And the smaller the child, the more important is the correspondence of his physical development to certain norms. And to assess the state of intrauterine development of the fetus, its size is the most objective criterion.
The weight of a child at birth is very important for his development, especially in the first year of life, and affects his health in the future. Children born with low body weight (up to 2500 grams) are more prone to obstetric complications: they tolerate childbirth worse, they develop hypoxia and even asphyxia more often than children with normal weight, and neurological disorders also occur.
As a result, these babies do not adapt well to a new life. In infancy, they suffer from hyperexcitability, increased or, conversely, decreased muscle tone, sluggishly suck and often spit up food, gain weight poorly, and may lag behind their peers in psychomotor development. Even at the age of 7-8 years, such children are hyperactive, clumsy and do not know how to concentrate on the necessary subject for a long time. The difference between healthy babies and small babies only blurs by 9-10 years, although in height and weight they catch up with their peers by the age of two. However, the consequences of the transferred condition can “come around” already in adulthood. Recent studies have shown an association between low birth weight and an increased risk of developing cardiovascular disease, obesity, diabetes mellitus and elevated blood lipids, all of which are associated with congenital endocrine disorders seen in low birth weight infants. Therefore, such a pathology as Fetal growth retardation (FGR or fetal malnutrition) deserves special attention.
The difference between healthy babies and small babies only blurs by 9-10 years, although in height and weight they catch up with their peers by the age of two. However, the consequences of the transferred condition can “come around” already in adulthood. Recent studies have shown an association between low birth weight and an increased risk of developing cardiovascular disease, obesity, diabetes mellitus and elevated blood lipids, all of which are associated with congenital endocrine disorders seen in low birth weight infants. Therefore, such a pathology as Fetal growth retardation (FGR or fetal malnutrition) deserves special attention.
FGR can be symmetrical, when all organs are evenly reduced, and asymmetric, when the brain and skeleton correspond to the gestational age, and the internal organs lag behind in development. The reasons for this are smoking, alcohol consumption, chromosomal abnormalities, infections, but most often - fetoplacental insufficiency and other conditions that lead to circulatory disorders: high or low blood pressure, toxicosis of the second half of pregnancy, diabetes mellitus with vascular damage, kidney disease, etc.
The development of fetal malnutrition is influenced by the age of the mother . The fact is that the body of very young mothers (16-18 years old) is simply not yet ready for the upcoming stresses, while older mothers (32-40 years old) most often already have a “baggage” of chronic diseases. Smoking, addiction to alcohol and any drugs clearly contribute to the development of malnutrition, as they cause pronounced vasoconstriction and reduce uteroplacental blood flow. Alas, quite often, malnutrition is observed in multiple pregnancies, since two or even three twins have to share, literally brotherly, the nutrients received from the mother.
One of the simplest methods of monitoring fetal development is to measure the size of the uterus. As soon as it can be easily felt above the womb - approximately at the fourth month of pregnancy, at each visit, the doctor will measure the height of the fundus of the uterus, and in the second half of pregnancy, the circumference of the abdomen at the level of the navel. This will allow the doctor to roughly judge the size of the fetus. Obviously, these indicators are not objective enough, because their value is influenced by the thickness of the anterior abdominal wall, the amount of amniotic fluid, and the physique of the woman.
This will allow the doctor to roughly judge the size of the fetus. Obviously, these indicators are not objective enough, because their value is influenced by the thickness of the anterior abdominal wall, the amount of amniotic fluid, and the physique of the woman.
The most accurate diagnostic method is the ultrasound biometry used in our Clinic , which measures and evaluates several fetal parameters. The most traditional is the measurement of the head, tummy and femur, but if the doctor has doubts, he will also take additional measurements. The accuracy of the diagnosis is ensured by the high qualification of the doctor conducting the study, the excellent resolution of our Sonix OP ultrasound scanner and the possibility of conducting a Doppler study. Ultrasound also controls the amount of amniotic fluid, reveals signs of placental dysfunction, as well as changes in blood flow in it, which helps the doctor to accurately make a preliminary diagnosis and begin treatment. To clarify the diagnosis, we carry out Doppler study of vessels of the placenta, umbilical cord and large vessels of the fetus, as well as cardiotocography (CTG), which allows you to register the fetal heartbeat and the nature of changes in the frequency of its heart rate in response to movements or contractions of the uterus. It is important that normal Doppler and CTG data - even in the presence of low weight, indicate the well-being of the baby. If the examination did not reveal any deviations, then it becomes clear that we are talking about a healthy, low-weight fetus. In this case, we simply observe the woman without any therapy.
To clarify the diagnosis, we carry out Doppler study of vessels of the placenta, umbilical cord and large vessels of the fetus, as well as cardiotocography (CTG), which allows you to register the fetal heartbeat and the nature of changes in the frequency of its heart rate in response to movements or contractions of the uterus. It is important that normal Doppler and CTG data - even in the presence of low weight, indicate the well-being of the baby. If the examination did not reveal any deviations, then it becomes clear that we are talking about a healthy, low-weight fetus. In this case, we simply observe the woman without any therapy.
The first signs of IGR can be detected in such a study as early as 24-26 weeks, and its symmetrical form is more often noted. The occurrence of malnutrition after 32 weeks is more typical for the asymmetric form, and fetal hypoxia usually also joins it.
Identified fetal growth retardation should be treated.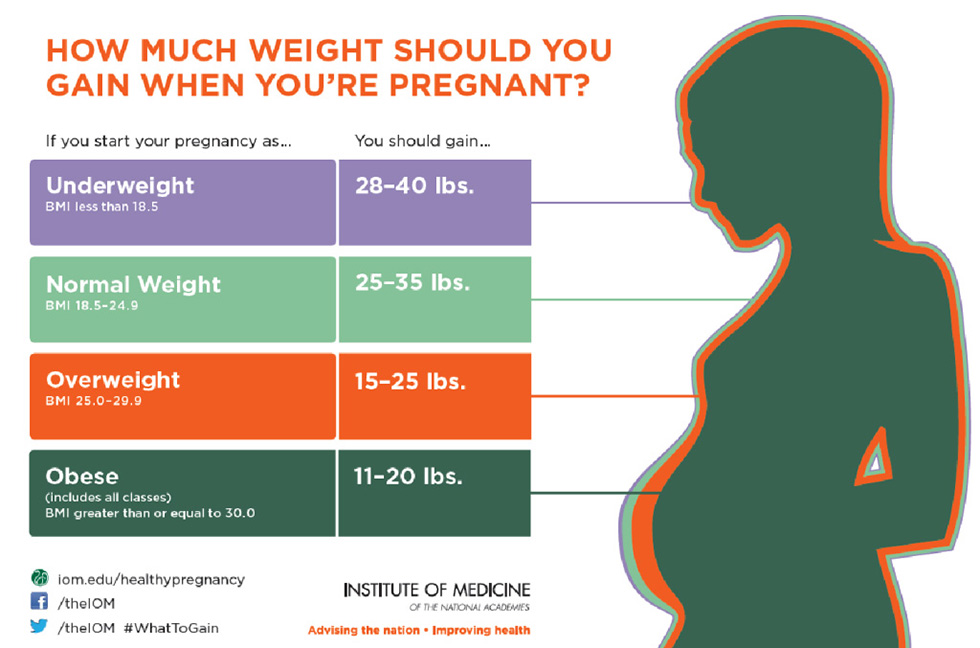 The goal of treatment in this case is not to “fatten the baby”, but to normalize metabolic processes and support the vital functions of the fetus. Of course, the success of treatment largely depends on how timely it is started. A large arsenal of medicines is used to treat malnutrition. It should be individual, taking into account the cause that caused IGR in this particular case and aimed at treating both the woman's diseases and pregnancy complications. For expectant mothers who are carrying a small child, it is very important to have a good diet rich in vitamins and animal proteins, as well as a regimen with limited physical activity. Although you should not overeat, remembering that excesses in the diet do not at all lead to a proportional increase in the amount of nutrients taken by the placenta for the fetus.
The goal of treatment in this case is not to “fatten the baby”, but to normalize metabolic processes and support the vital functions of the fetus. Of course, the success of treatment largely depends on how timely it is started. A large arsenal of medicines is used to treat malnutrition. It should be individual, taking into account the cause that caused IGR in this particular case and aimed at treating both the woman's diseases and pregnancy complications. For expectant mothers who are carrying a small child, it is very important to have a good diet rich in vitamins and animal proteins, as well as a regimen with limited physical activity. Although you should not overeat, remembering that excesses in the diet do not at all lead to a proportional increase in the amount of nutrients taken by the placenta for the fetus.
Depending on the severity of the condition of the fetus, the treatment is carried out on an outpatient basis, for example, in our day hospital, or in the maternity hospital.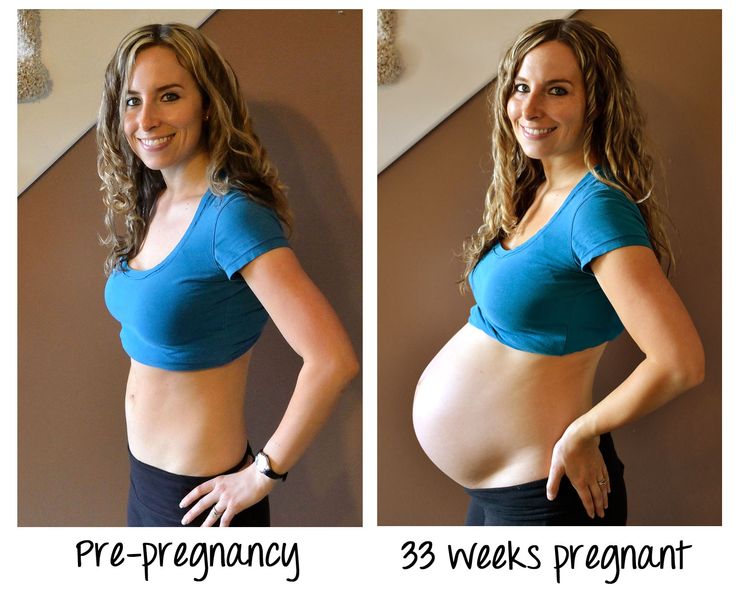 Although, as you know, houses and walls help, but in severe cases it is better not to refuse hospitalization. In the hospital, it is easier to monitor the condition of the mother and baby, and therefore provide more effective assistance. The effect of therapeutic measures must be constantly monitored using ultrasound and CTG, which are usually prescribed at intervals of 2 weeks, and if necessary, more often. FGR treatment almost always produces good results. In most cases, it is possible to observe adequate fetal growth: for example, in 7-10 days, the size of the fetus increases accordingly, and does not lag even further, which is considered a completely satisfactory result.
Although, as you know, houses and walls help, but in severe cases it is better not to refuse hospitalization. In the hospital, it is easier to monitor the condition of the mother and baby, and therefore provide more effective assistance. The effect of therapeutic measures must be constantly monitored using ultrasound and CTG, which are usually prescribed at intervals of 2 weeks, and if necessary, more often. FGR treatment almost always produces good results. In most cases, it is possible to observe adequate fetal growth: for example, in 7-10 days, the size of the fetus increases accordingly, and does not lag even further, which is considered a completely satisfactory result.
The method and timing of delivery largely depend on the condition of the fetus. If the treatment of FGR is successful and the baby is growing, then it makes no sense to rush things, because by the end of pregnancy it can reach quite a decent size. If, despite all efforts, the child does not gain weight or has any other problems, then they resort to early delivery.