Normal temperature for 10 month old
Fever (0-12 Months)
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections. Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed.
Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears.
- Bacterial Infections. A bladder infection is the most common cause of silent fever in girls.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain. The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.
- Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
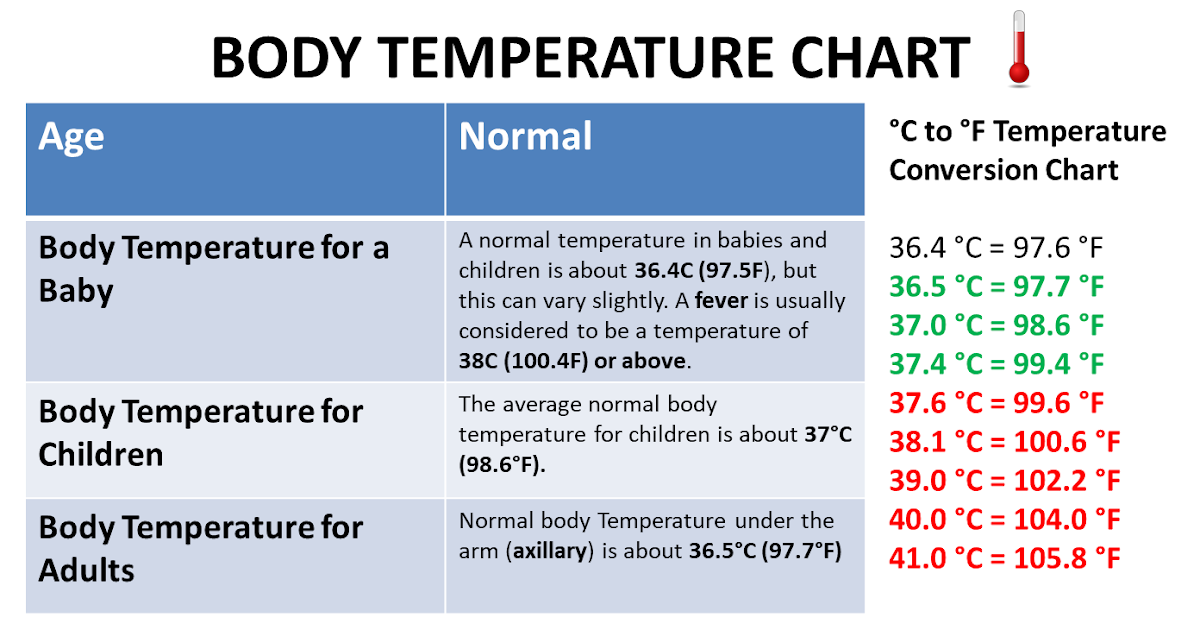
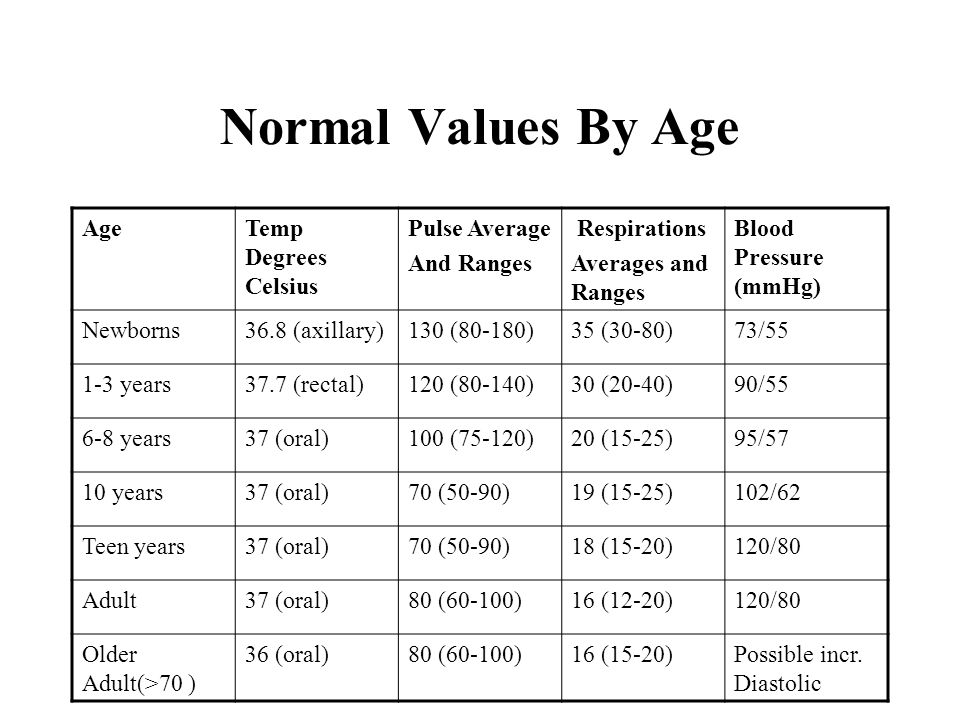
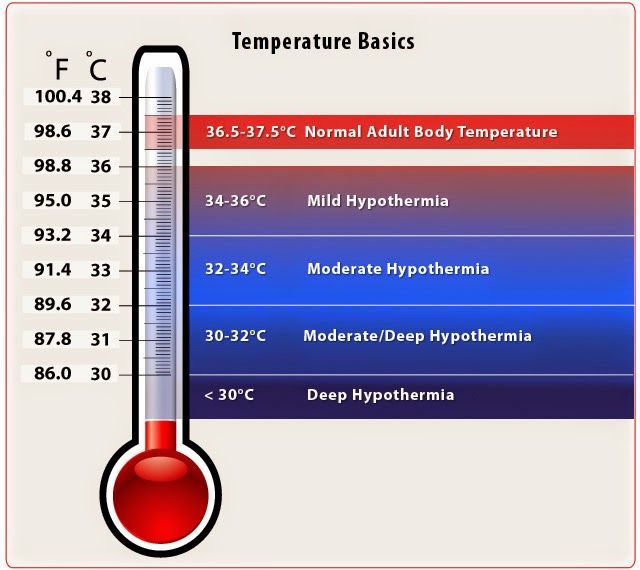
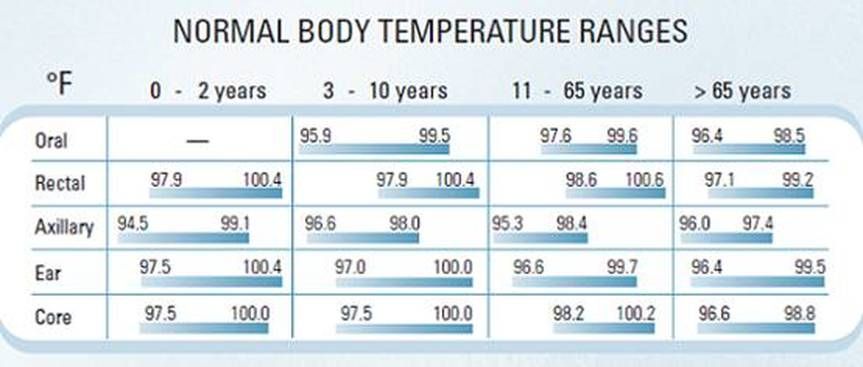
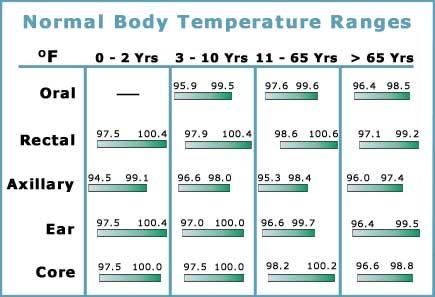
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.3° F (37.9° C) late in the day. This is a normal range.
When to Call for Fever (0-12 Months)
Call 911 Now
- Not moving
- Can't wake up
- Severe trouble breathing (struggling for each breath; can barely speak or cry)
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Fever in baby less than 12 weeks old.
 Caution: Do NOT give your baby any fever medicine before being seen.
Caution: Do NOT give your baby any fever medicine before being seen. - Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-12 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Fever
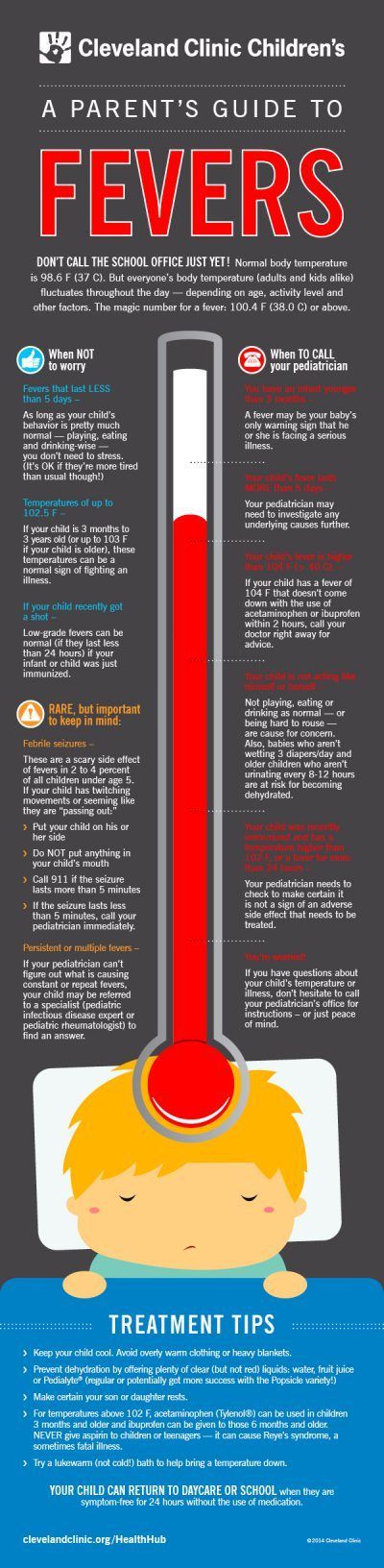
- What You Should Know About Fever:
- Having a fever means your child has a new infection.
- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- For infants more than 3 months old, most fevers are good for sick children. They help the body fight infection.
- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
- Treatment for All Fevers - Extra Fluids:
- Fluids alone can lower the fever. Reason: being well hydrated helps the body give off heat through the skin.
- For shivering (or the chills), give your child a blanket. Make them comfortable.
- Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
- For all children, dress in 1 layer of light weight clothing, unless shivering.
 Reason: also helps heat loss from the skin.
Reason: also helps heat loss from the skin. - For shivering (or the chills), give your child a blanket. Make them comfortable.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: Babies can get over-heated more easily than older children.
- Fever Medicine:
- Caution: Do not give a baby under 3 months any fever medicine. Most of these babies will need to be seen.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are not needed. Reason: fevers in this range help the body fight the infection. Fevers turn on the body's imune system. Fevers don't cause any discomfort. Fever meds are mainly needed for fevers higher than 102° F (39° C).
- Give an acetaminophen product (such as Tylenol).
- Another choice is an ibuprofen product (such as Advil) if over 6 months old.
- Goal of treatment: keep the fever at a helpful level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.
 5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect. - Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
- Pain: fever does not cause pain. If your child also has pain, it's from the infection. It may be a sore throat or muscle pain. Treat the pain, if it's more than mild.
- Return to Child Care:
- Your child can return to child care after the fever is gone. Your child should feel well enough to join in normal activities.
- What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.
- They are not harmful.
- Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/04/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
How to Take a Temperature (0-12 Months)
When Does Your Baby Have a Fever??
- Rectal, Forehead or Ear temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
Where to Take the Temperature
- Rectal temps are the most accurate. Forehead temps are the next most accurate. Ear temps are also accurate if done properly. Temps done in the armpit are the least accurate. Armpit temps are useful for screening at any age.
- Age under 3 months old (90 days old). An armpit temp is the safest and is good for screening.
 If the armpit temp is above 99° F (37.2° C), re-check it. Use a rectal reading. Reason: If young babies have a fever, they need to see a doctor now. New research shows that forehead temps may also be accurate under 3 months of age.
If the armpit temp is above 99° F (37.2° C), re-check it. Use a rectal reading. Reason: If young babies have a fever, they need to see a doctor now. New research shows that forehead temps may also be accurate under 3 months of age. - Age 3 months to 1 year old. Rectal or forehead temps are accurate. An ear thermometer can be used after 6 months old. An armpit temp is good for screening if it is taken right.
- Digital (electronic) thermometers are easily found in stores. They do not cost very much. They can be used for rectal and armpit temps. Most of them give an accurate temp in 10 seconds or less. The AAP suggests you replace any glass thermometer in the house with one of these products.
Rectal Temperature: How to Take
- Age: Birth to 1 year old
- Have your child lie stomach down on your lap. Another way is on the back with the legs pulled up to the chest.
- Put some petroleum jelly on the end of the thermometer and the anus.
- Slide the thermometer gently into the anus no more than 1 inch. If your child is less than 6 months old, put it in no more than ½ inch. That means until you can no longer see the silver tip.
- Be gentle. There should not be any resistance. If there is, stop.
- Hold your child still. Leave a digital thermometer in until it beeps (about 10 seconds).
- Your child has a fever if the rectal temp is above 100.4° F (38° C).
- Warning: do not take rectal temperatures in young children with leukemia or other cancers. Also avoid in other children with weak immune systems such as organ transplant, HIV or sickle cell disease.
Armpit Temperature: How to Take
- Age: Any age for screening
- Put the tip of the thermometer in an armpit. Make sure the armpit is dry.
- Close the armpit by holding the elbow against the chest. Do this until it beeps (about 10 seconds). The tip of the thermometer must stay covered by skin.
- Your child has a fever if the armpit temp is above 99.
 0° F (37.2° C). If you have any doubt, take your child's temp by rectum or forehead.
0° F (37.2° C). If you have any doubt, take your child's temp by rectum or forehead.
Digital Pacifier Temperature: How to Take
- Age: Birth to 1 year. Only good for screening. Requires the baby to suck on it, which is not always possible.
- Have your child suck on the pacifier until it beeps (about 10 seconds).
- Your child has a fever if the pacifier temp is above 100° F (37.8° C).
Ear Temperature: How to Take
- Age: 6 months and older (not accurate before 6 months)
- This thermometer reads the heat waves coming off the eardrum.
- A correct temp depends on pulling the ear backward. Pull back and up if over 1 year old.
- Then aim the tip of the ear probe between the opposite eye and ear.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution. Being outdoors on a cold day will cause a low reading.
 Your child needs to be inside for 15 minutes before taking the temp. Earwax, ear infections and ear tubes do not keep from getting correct readings.
Your child needs to be inside for 15 minutes before taking the temp. Earwax, ear infections and ear tubes do not keep from getting correct readings.
Forehead (Temporal Artery) Temperature: How to Take
- Age: Any age
- This thermometer reads the heat waves coming off the temporal artery. This blood vessel runs across the forehead just below the skin.
- Place the sensor head at the center of the forehead.
- Slowly slide the thermometer across the forehead toward the top of the ear. Keep it in contact with the skin.
- Stop when you reach the hairline.
- Read your child's temp on the display screen.
- Note: some newer forehead thermometers don't need to slide across the forehead. Follow the box directions on how to take the temp.
- Used in more doctor's offices than any other thermometer.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Last Reviewed: 12/04/2022
Last Revised: 03/17/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Normal values of body temperature in children, measurement of the child's body temperature
It is believed that a healthy child should have a body temperature of 36.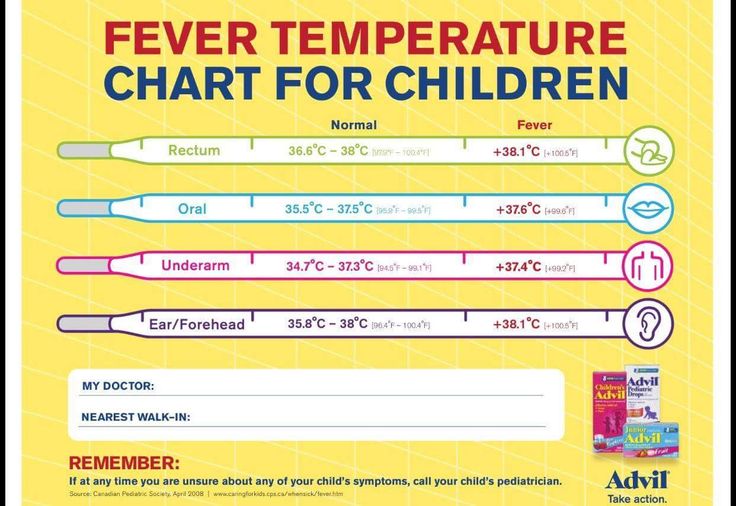 6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
6 °C. And its increase over 37 degrees is regarded as a sign of illness. But it is not so.
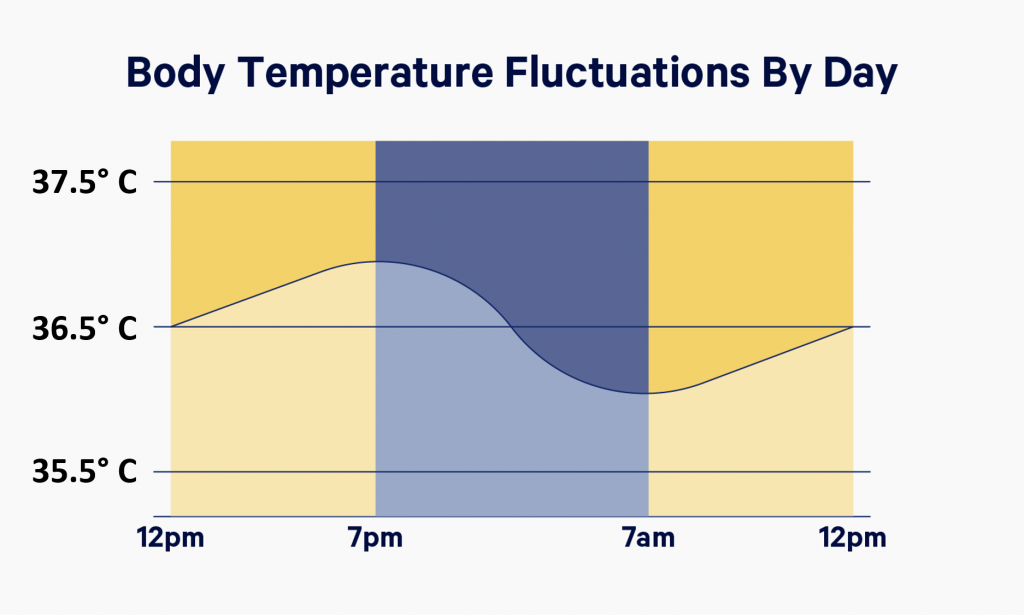
Body temperature depends on age and measurement area. It can increase after physical exertion, emotional arousal and feeding.
Devices and time for measuring body temperature
To determine the temperature, the following types of thermometers are used:
-
digital;
-
mercury;
-
infrared.
The optimal time for thermometry is 7-9 am and 17-19 pm. As prescribed by the doctor, the determination of the temperature during the day in children can be performed 3-4 times.
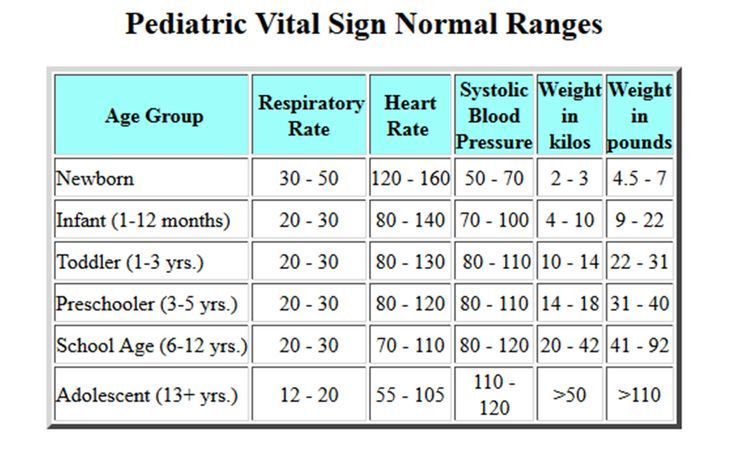
What temperature is considered normal for a child?
Immediately after the birth of a newborn, the temperature of his body decreases by 1-2 ° C, then within 24 hours it rises to 36-37 ° C. In the first 3 months of a baby's life, its indicators are unstable and depend on external factors: air temperature in the room, sleep, food intake. Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm.
Normally, these fluctuations do not exceed 0.6 °C per day. For children of the first year of life, a temperature of 37.7 is the norm.
The average body temperature for a child is 37°C. Usually in the morning - 36.3 ° C, and in the evening it can rise to 37.6 ° C.
In what areas can the temperature of children be taken?
Underarm
The temperature measurement time under the arm is 5-10 minutes and depends on the type of device.
In the rectum
It is used in children under 5 years of age and in debilitated patients. For this method, it is desirable to use medical electronic thermometers with a soft tip. It will take 1-1.5 minutes to determine the rectal temperature.
Oral
The procedure is performed both under the tongue and behind the cheek. Contraindications to the use of this method are: children under 4-5 years of age, increased excitability and impaired nasal breathing.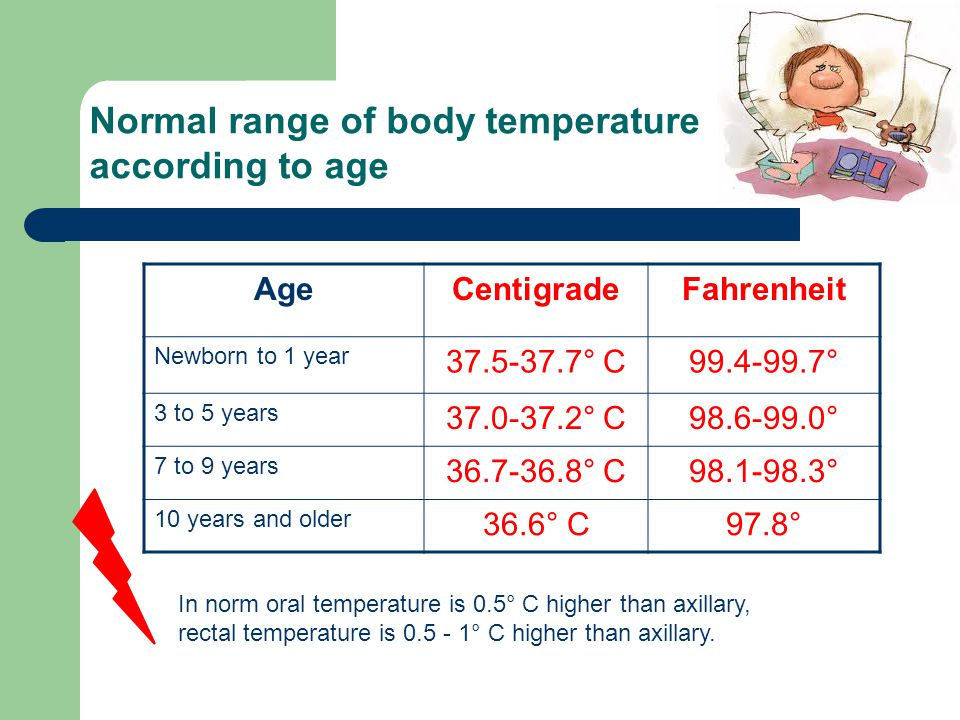 The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
The duration of temperature measurement by the oral method is from 10 seconds to 3 minutes.
In the ear
The temperature in the ear is measured with an infrared sensor. The tip of the thermometer is inserted into the ear canal and the result appears on the display.
On forehead
Forehead temperature can be measured with a contact and non-contact thermometer. It will take 3 to 5 seconds to get the result. If the baby is sleeping or excited, then it is more convenient to use a non-contact method for measuring temperature.
Crotch
Mainly used in infants. The measurement time in the inguinal fold is 5 minutes. The method is inconvenient because the baby is not easy to keep in one position during this time.
Ranges of normal temperature in children depending on age and area of measurement are presented in the following table:
| 0-2 years | 3-10 years | 11-18 years old | |
|---|---|---|---|
| In the armpit | 34.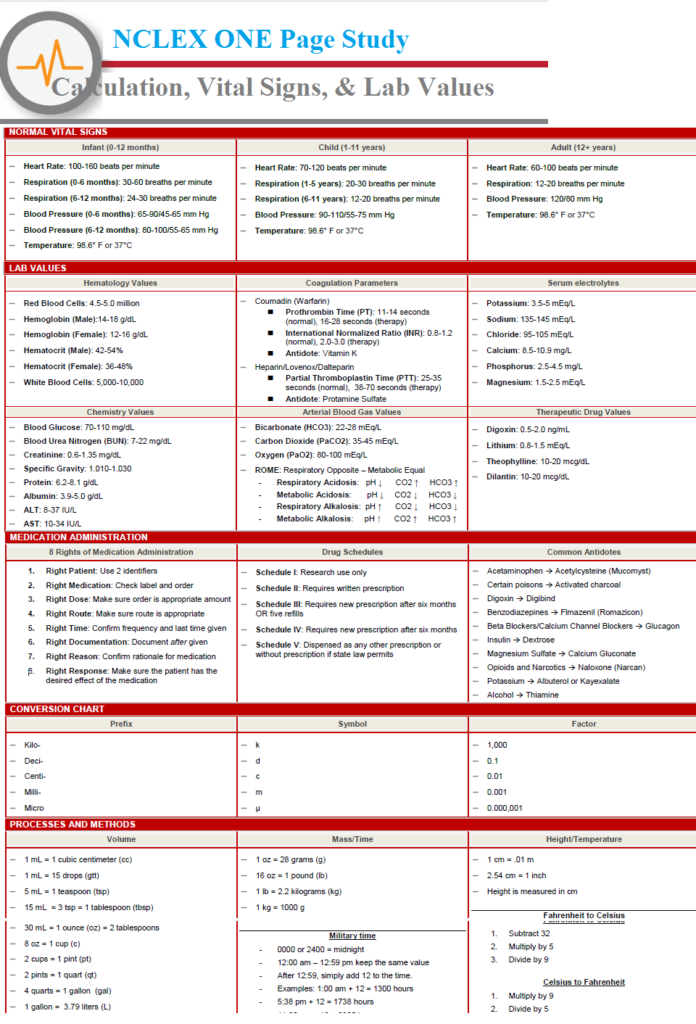 7 - 37.2 7 - 37.2 | 35.8 - 36.6 | 35.1 - 36.8 |
| On the forehead | 36.7 - 37.5 | 36.7 - 37.5 | 36.5 - 37.4 |
| in the ear | 36.3 - 37.7 | 36.3 - 37.7 | 36.7 - 37.8 |
What is the optimal temperature for a room where a newborn baby lives?
What temperature indicators are optimal for a room where a newborn baby lives?
With the birth of a child in any family, troubles increase significantly. Every mother wants to create the most comfortable living conditions for a newly born baby. She must not only provide the baby with the necessary care, but also ensure that the humidity and air temperature in the child’s room correspond to the parameters recommended by pediatricians.
The child doesn't care what brand of bed he sleeps on or what color stroller he is taken out for a walk.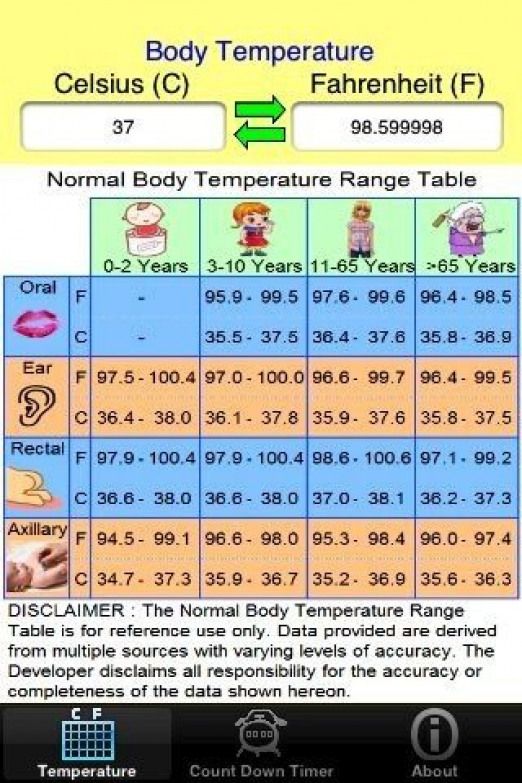 But the temperature and humidity in his room are of great importance, since an uncomfortable environment contributes to the development of most diseases. In addition, failure to comply with the necessary parameters may cause a deterioration in the mood of the infant.
But the temperature and humidity in his room are of great importance, since an uncomfortable environment contributes to the development of most diseases. In addition, failure to comply with the necessary parameters may cause a deterioration in the mood of the infant.
Therefore, for the prevention of diseases in newborns, it is very important to maintain optimal climatic conditions in the room.
Contents
- Comfortable temperature in the baby room
- Bath temperature for baby
- Temperature for premature babies
- Hazards associated with overheating or hypothermia of the infant
- Methods for maintaining the temperature in the newborn room
Comfortable temperature in the baby's room
Most pediatricians agree that the optimal temperature in the room of a newborn baby should range from 18 to 22 C. They consider just such a temperature comfortable for the normal well-being of the crumbs and its further development.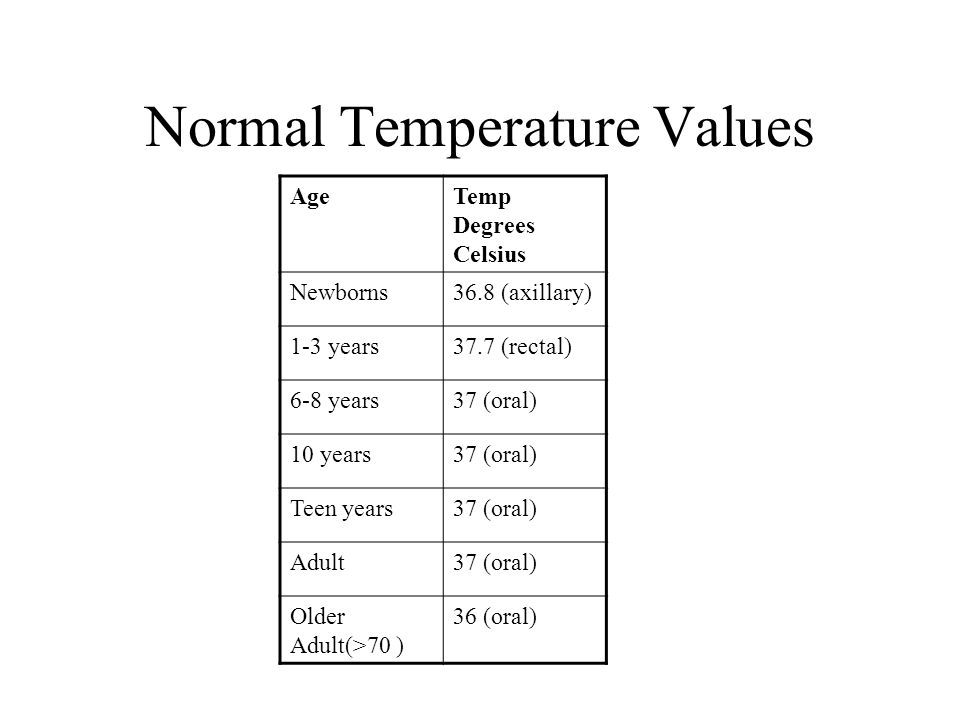
Doctor Komarovsky, widely known today, claims that in the room where a newborn baby is located, the temperature should be within 18-19 degrees. In his opinion, this is the optimal temperature regime for a baby.
Compliance with the indoor temperature in winter becomes much more difficult. This is due to the fact that during the heating period, the supply of heat to the dwellings does not depend on us in any way. Therefore, even in winter, it is necessary to maintain the temperature no higher than 23 degrees.
Another important condition for a baby's well-being is maintaining the necessary temperature indicators at night. If the room is too cold or hot, then the baby’s sleep will be restless, with frequent waking and whims. The ideal temperature for a restful baby's sleep should not exceed 22 degrees.
Please note that normal air circulation is not possible if a canopy is hung over the crib or if the crib is used to decorate the crib.
Temperature control during bathing a baby
During water procedures, it is also necessary to maintain appropriate temperature parameters of the air in the room. Most parents believe that the temperature in the bathing room for a newborn should be maintained at a higher level than usual. However, they are deeply mistaken. If you bathe a baby in a warmer room, then at the end of the water procedures, returning to the usual climatic conditions, he will certainly freeze.
Most parents believe that the temperature in the bathing room for a newborn should be maintained at a higher level than usual. However, they are deeply mistaken. If you bathe a baby in a warmer room, then at the end of the water procedures, returning to the usual climatic conditions, he will certainly freeze.
This means that when you are going to bathe your baby, you do not need to additionally heat the bathroom. The baby should bathe at the usual temperature for him. Just after bathing, you need to briefly wrap the baby in a warm towel. If parents want to harden a child from infancy, then immediately after water procedures, they should arrange air baths for him for several minutes.
Thus, there is no need to additionally heat the room at night and during the bathing period. The air temperature in the room must be maintained constantly at the same level.
Temperature for premature babies
It should be noted that the above room temperature standards apply only to babies born on time.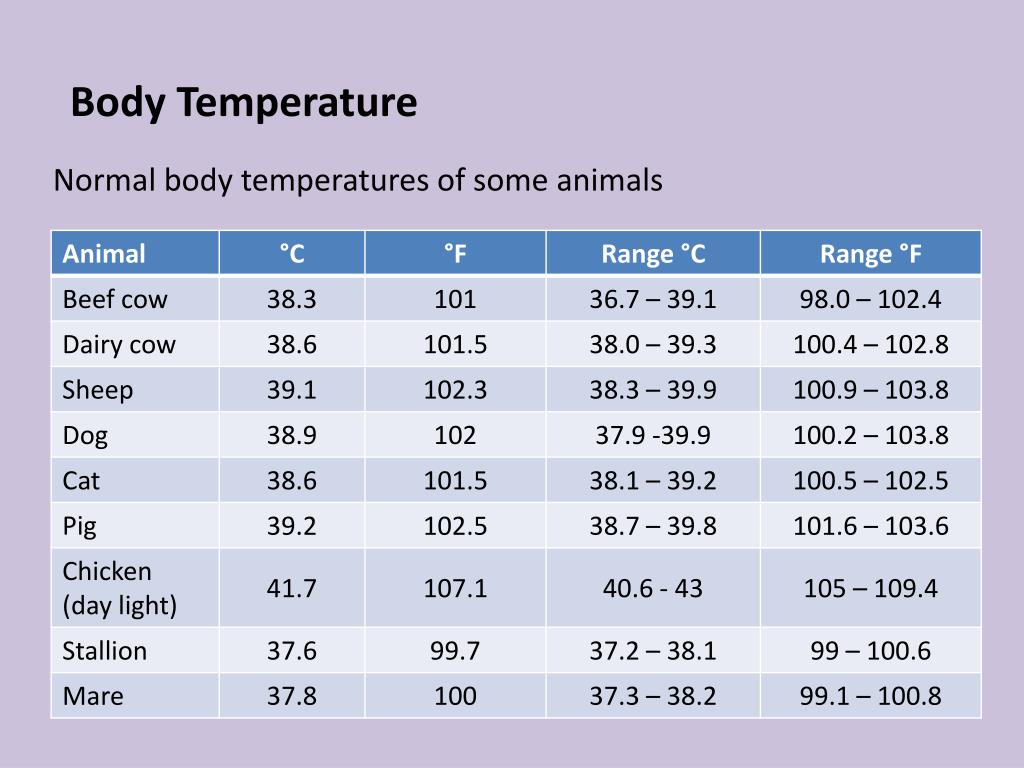 For a premature baby, other conditions of detention must be observed. For him, the temperature regime is optimal, which ranges from 24 - 25 C, since such children's own thermoregulation is often impaired.
For a premature baby, other conditions of detention must be observed. For him, the temperature regime is optimal, which ranges from 24 - 25 C, since such children's own thermoregulation is often impaired.
Infant overheating or hypothermia hazards
Overheating
Specialists in pediatrics have long noticed that overheating of the baby carries more dangers than its hypothermia. During metabolic processes, which are much faster in infants than in adults, a certain amount of heat is accumulated in the body. Excess heat is released either through the surface of the skin or in the process of breathing. The release of excess heat through breathing becomes much more difficult at high room temperatures. Then heat transfer occurs at an accelerated pace through the skin with the help of a sweating system. The baby sweats, redness appears, the pulse becomes more frequent, and breathing is difficult.
All this increases the child's tearfulness, makes him lethargic and deprives him of calmness. It can also cause dermatitis and prickly heat, metabolic processes and heat transfer are disturbed. In this regard, the temperature norm in the children's room must be strictly observed by parents.
Hypothermia
Hypothermia of a newborn baby is no less dangerous. Excessive coolness can provoke the development of colds in a child, which is fraught with the appearance of a number of dangerous complications.
Therefore, the temperature in the newborn room must be strictly observed in accordance with existing norms and recommendations of pediatricians. +
Ways to maintain the temperature in the newborn room
Before setting the optimum room temperature, you need to decide which temperature setting is most comfortable for your child. You can find out the optimal room temperature for the baby quite easily:
- the child feels good and sleeps well;
- the baby does not have redness and prickly heat;
- the so-called "goosebumps" are not observed on the baby's skin, and his legs and arms are warm;
- the child's breathing is not difficult, the pulse is not rapid.
In the event that the room temperature does not meet the standards, some steps should be taken to regulate the air temperature.
If the temperature in the child's room is high, the regulation is carried out by means of an air conditioner or ventilation of the room. It is better to go for a walk with the baby at this time. The air conditioner must be installed in the room next door, or in the same room, but far from the child. Heating radiators should be covered with a thick blanket or blanket.
When the air temperature in the children's room is low, you can maintain the optimal temperature by turning on the heaters.
Room temperature control not possible?
Parents are not always able to maintain the desired temperature in the room where the child is. In this case, it is necessary:
- give the baby more water if the room is stuffy and the air temperature is high;
- the baby should be dressed according to the temperature in the room.