Nitrous and pregnancy
Nitrous Oxide for Labor and Delivery
Nitrous oxide use during labor and delivery is a great option for pain relief. Nitrous oxide is safe for use for most women, offers minimal side effects, and is also safe for babies with no effect on baby alertness or breastfeeding.
Moreland OB-GYN is the first medical provider in Southeastern Wisconsin to offer nitrous oxide during labor and is a premiere gynecology and obstetric practice with services in Waukesha, Oconomowoc, Brookfield, Hartland, Sussex, Mukwonago, and Watertown.
What Is Nitrous Oxide?
Nitrous oxide is a flavorless, odorless gas that can be administered to patients to help alleviate pain and anxiety, and promote relaxation.
Nitrous oxide is safe for use during pregnancy, labor, and delivery.
How Does Nitrous Oxide Work During Labor?
Nitrous oxide is a unique pain-relief option during labor and delivery because it can be used at any time.
Patients are in control of administering nitrous oxide by either putting on or removing a mask. Breathing with the mask in place allows the effects of nitrous oxide to be felt in 30 seconds or less, allowing patients to experience pain relief and reduced feelings of anxiety almost immediately. Upon removal of the mask, within three breaths, the effects of nitrous oxide can no longer be felt.
- Many women choose nitrous oxide to help reduce anxiety during early labor and then choose to use alternative options during active labor, like an epidural injection.
- Some women choose to use nitrous oxide throughout labor, putting the mask in place before contractions, and breathing freely without the mask between contractions.
Learn more about nitrous oxide vs. other pain relief options in this informative article.
Benefits of Nitrous Oxide During Labor
The use of nitrous oxide in labor and delivery is beneficial for many reasons.
- It is a fast-acting pain relief option that allows you to feel the effects in 30 seconds or less.

- When using nitrous oxide, you can get up, move around, re-position, or use a birthing device, such as a birthing ball.
- Between contractions you can remove the mask, reducing or eliminating the effects of the gas; you can feel like yourself, without any grogginess.
- Nitrous oxide wears off quickly, and the full effects only last as long as the mask is in place on your face.
In a recent New York Times article written by Sarah Baird, “The Rise of Laughing Gas in the Delivery Room,” healthcare professionals from around the country weigh in on the benefits of nitrous oxide and its rising popularity in the U.S. The article states, “The increased interest in nitrous dovetails with a growing number of women searching for ways to avoid additional medical interventions during birth.” Read more.
Nitrous Oxide Side Effects
There are very few risks associated with the use of nitrous oxide. In fact, it is one of the safest pain relief options for women during labor and delivery.
Nitrous oxide side effects include:
- Mild nausea (experienced by about 20-percent of women)
- Vomiting
- Dizziness
You can be given anti-nausea medication to help reduce these symptoms.
The nitrous oxide used by obstetricians during labor and delivery is 50-percent nitrous gas and 50-percent oxygen. Unlike the side effects of much higher concentrations used in dentistry and other medical fields, the side effects of a 50/50 gas are minimized substantially. In fact, all side effects of nitrous oxide wear off in as little as 10-15 minutes.
Who Is a Good Candidate for Nitrous Oxide Use?
Almost everyone is a good candidate for using nitrous oxide in labor and delivery. The only disqualifying factor is if you currently have a B12 deficiency or if you’ve had one in the past.
If you are interested in the use of nitrous oxide during labor, our staff will draw blood in your third trimester to confirm it is a safe option for you.
Nitrous oxide can also be used successfully to help patients who experience pain with cervical checks or other procedures during pregnancy.
Pregnancy | American Dental Association
- Preventive, diagnostic and restorative dental treatment is safe throughout pregnancy.
- Local anesthetics with epinephrine (e.g., bupivacaine, lidocaine, mepivacaine) may be used during pregnancy.
- Special considerations should be given to pregnant dental personnel whose job duties can involve direct exposure to nitrous oxide and radiation.
Oral health care, including having dental radiographs taken and being given local anesthesia, is safe at any point during pregnancy.1, 2 Further, the American Dental Association and the American College of Obstetricians and Gynecologists (ACOG) agree that emergency treatments, such as extractions, root canals or restorations can be safely performed during pregnancy and that delaying treatment may result in more complex problems.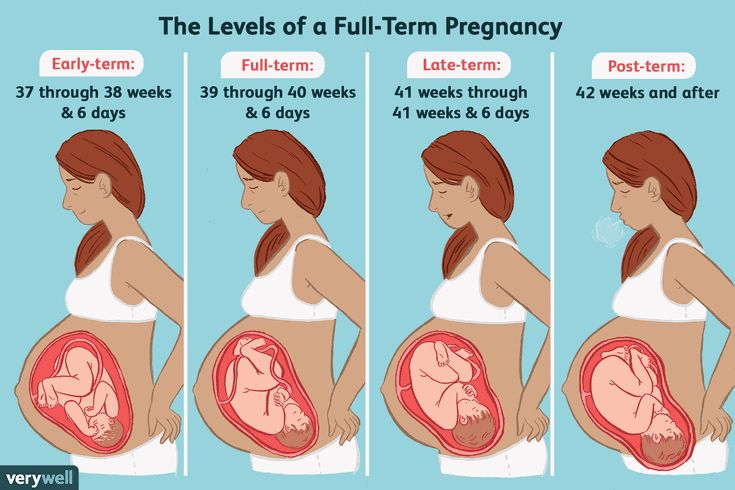 1, 2 Although ACOG has a statement regarding postponing elective nonobstetric general surgery and some invasive procedures (e.g., cardiac catheterization or colonoscopy) until after delivery,3 their statement on oral care during pregnancy and through the lifespan1 states that oral conditions requiring immediate treatment, such as periodontal or endodontic treatment, extractions, or restoration of untreated caries can be managed at any time during pregnancy.
1, 2 Although ACOG has a statement regarding postponing elective nonobstetric general surgery and some invasive procedures (e.g., cardiac catheterization or colonoscopy) until after delivery,3 their statement on oral care during pregnancy and through the lifespan1 states that oral conditions requiring immediate treatment, such as periodontal or endodontic treatment, extractions, or restoration of untreated caries can be managed at any time during pregnancy.
When treating pregnant patients, it might be helpful to reach out to the obstetrician to develop a working relationship should consultation be needed later. Questions to ask might include:4
- When is the expected delivery date?
- Is this a high-risk pregnancy? If so, are there any special concerns or contraindications?
- Is there a recommended medication for pain control?
During pregnancy, several oral health conditions are more common:
- Gingivitis may result from hormonal changes that exaggerate the response to bacteria in the gum tissue4
- Dental caries may occur due to changes in diet such as increased snacking due to cravings, increased acidity in the mouth due to vomiting, dry mouth or poor oral hygiene stemming from nausea and vomiting.
 1, 4
1, 4 - Pyogenic granuloma (also known as granuloma gravidarum) is a round growth, usually connected to the gingivae by a thin cord of tissue, that may develop due to hormonal changes.5,6
- Erosion stemming from vomiting as a result of morning sickness may be detected.5 Patients should be encouraged to avoid toothbrushing immediately after vomiting, which exposes the teeth to stomach acids. Instead, they should opt for rinsing with a diluted solution of 1 cup water and 1 teaspoon of baking soda to neutralize the acid.5
Due to the increased risk of gingivitis and caries, the importance of good daily oral hygiene should be emphasized to these patients. Brushing twice a day with a soft-bristled brush for two minutes, using a fluoride-containing toothpaste, and cleaning between the teeth once a day should be encouraged. If it is determined that a topical fluoride treatment is needed to minimize the effects of erosion, fluoride varnish may be preferred over gel treatments due to nausea. 7
7
Periodontitis and Adverse Pregnancy Outcomes
Much has been written in recent years about the relationship between maternal periodontitis and pregnancy outcomes. While findings of individual studies have been mixed, an overview of 23 systematic reviews conducted through 2016 concluded that associations exist between periodontitis and pre-term birth, low birthweight babies, low birthweight babies born prematurely and the development of pre-eclampsia. 8
More research is needed to determine the relationship between periodontitis and pregnancy outcomes, however, should periodontitis develop during pregnancy, scaling and root planing is recognized as safe to perform.1, 4 The ACOG statement on oral care during pregnancy and through the lifespan1 states that “despite the lack of evidence for a causal relationship between periodontal disease and adverse pregnancy outcomes, the treatment of maternal periodontal disease during pregnancy is not associated with any adverse maternal or birth outcomes,” and “prenatal periodontal therapy is associated with the improvement of maternal oral health. ”
”
Medication Safety Labeling
Historically, manufacturers have relied on an alphabetical system to communicate the safety of medications for use with pregnant patients. In 2015, the U.S. Food & Drug Administration began phasing out that system for prescription drugs, replacing it with a narrative section in the package insert that discusses the benefits and risks of using a particular medication with this population.9, 10 The new system will be phased-in, with a full compliance date of 2020.
The alphabetical system (Table) will continue to be used for over-the-counter (OTC) medications.11
Medication Selection
Questions about use of local anesthetics or antibiotics in pregnant individuals are common. Options considered safe for use in these situations include:
- Local anesthesia (with or without epinephrine)1, 13, 14
- Antibiotics13-15
- Penicillin
- Amoxicillin
- Cephalosporins
- Clindamycin
- Metronidazole
Use of other medications calls for consultation with the patient’s obstetrician to weigh risks and benefits. An example of a situation that may benefit from consultation is pain relief. Several analgesics have been placed in pregnancy Category B, which indicates that they are typically safe to use; however, in 2015, the U.S. Food & Drug Administration backed off that classification, stating that the published research is “too limited to make any recommendations” on pain reliever use in this population.16 This suggests that decisions made about medications for pain relief should be arrived at after consultation with the obstetrician. That said, emergencies call for immediate implementation of standard emergency protocols.
An example of a situation that may benefit from consultation is pain relief. Several analgesics have been placed in pregnancy Category B, which indicates that they are typically safe to use; however, in 2015, the U.S. Food & Drug Administration backed off that classification, stating that the published research is “too limited to make any recommendations” on pain reliever use in this population.16 This suggests that decisions made about medications for pain relief should be arrived at after consultation with the obstetrician. That said, emergencies call for immediate implementation of standard emergency protocols.
Lactation
Questions often arise about medication use by patients who are lactating. Most medication product inserts have information related to use during lactation. The National Library of Medicine also provides a searchable database (LactMed) on this topic.
Nitrous Oxide
Nitrous oxide is classified as a pregnancy risk group Category C medication, meaning that there is a risk of fetal harm if administered during pregnancy. It is recommended that pregnant individuals, both patients and staff, avoid exposure to nitrous oxide.17 The National Institute of Occupational Safety and Health (NIOSH), a federal agency affiliated with the Centers for Disease Control and Prevention, recommends use of a scavenging system and exposure limits of N2O concentrations in dental operations to approximately 25 ppm during analgesia administration.18
It is recommended that pregnant individuals, both patients and staff, avoid exposure to nitrous oxide.17 The National Institute of Occupational Safety and Health (NIOSH), a federal agency affiliated with the Centers for Disease Control and Prevention, recommends use of a scavenging system and exposure limits of N2O concentrations in dental operations to approximately 25 ppm during analgesia administration.18
Dental offices that use nitrous oxide-oxygen can review best management practices on the Nitrous Oxide Oral Health Topic page.
Radiographs are considered safe for the pregnant patient, at any stage during pregnancy, when abdominal and thyroid shielding is used.1
Dental professionals who take radiographs should inform their employer in writing that they are pregnant as soon as they are aware of the pregnancy. The employee should be provided with a personal dosimetry badge and the manufacturer’s instructions should be followed to ensure that the occupational radiation exposure does not exceed 0. 5 millisieverts (mSv) per month.19 Provision of dosimetry badges and limiting exposure to 0.5 mSv/month are recommendations for good practice; to determine whether there are related regulations in your state, contact your radiation protection program.
5 millisieverts (mSv) per month.19 Provision of dosimetry badges and limiting exposure to 0.5 mSv/month are recommendations for good practice; to determine whether there are related regulations in your state, contact your radiation protection program.
During pregnancy, individuals may be at increased risk for oral conditions such as gingivitis and dental caries, and should be counseled by both their obstetrician and dentist on the importance of good oral hygiene throughout the pregnancy. Regular and emergency dental care, including the use of local anesthetics and radiographs, is safe at any stage during pregnancy.
Statement on Alcohol and Other Substance Use by Pregnant and Postpartum Patients
(Trans.2005:330)
Resolved, that the following ADA Statement on Alcohol and Other Substance Use by Pregnant and Postpartum Patients be adopted.
Statement on Alcohol and Other Substance Use by Pregnant and Postpartum Patients
1. Dentists are encouraged to inquire about pregnant or postpartum patients’ history of alcohol and other drug use, including nicotine.
Dentists are encouraged to inquire about pregnant or postpartum patients’ history of alcohol and other drug use, including nicotine.
2. As healthcare professionals, dentists are encouraged to advise these patients to avoid the use of these substances and to urge them to disclose any such use to their primary care providers.
3. Dentists who become aware of postpartum patients’ resumption of tobacco or illegal drug use, or excessive alcohol intake, are encouraged to recommend that the patient stop these behaviors. The dentist is encouraged to be prepared to inform the woman of treatment resources, if indicated.
American Dental Association
Adopted 2005; Reviewed 2017
Dental Examinations for Pregnant Women and Women of Child-Bearing Age
(Trans.2014:508)
Resolved, that the ADA urge all pregnant women and women of child-bearing age to have a regular dental examination.
American Dental Association
Adopted 2014
Dental Treatment During Pregnancy
(Trans. 2014:508)
2014:508)
Resolved, that the ADA acknowledges that preventive, diagnostic and restorative dental treatment to promote health and eliminate disease is safe throughout pregnancy and is effective in improving and maintaining the oral health of the mother and her child.
American Dental Association
Adopted 2014
- American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women. Oral Health Care During Pregnancy and Through the Lifespan (Number 569). 2013; Reaffirmed 2017. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2013/08/oral-health-care-during-pregnancy-and-through-the-lifespan. Accessed May 4, 2021.
- American Dental Association. ADA Current Policies, 1954-2020. 2021. https://www.ada.org/~/media/ADA/Member%20Center/Members/current_policies.pdf. Accessed May 4, 2021.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice and the American Society of Anesthesiologists.
 Nonobstetric Surgery During Pregnancy (Number 775). 2017; Reaffirmed 2021. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/04/nonobstetric-surgery-during-pregnancy.
Nonobstetric Surgery During Pregnancy (Number 775). 2017; Reaffirmed 2021. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/04/nonobstetric-surgery-during-pregnancy. - Niessen LC. Women's Health. In: Patton LL, Glick M, editors. The ADA Practical Guide to Patients with Medical Conditions. Second ed. Hoboken NJ: John Wiley & Sons; 2016. p. 423-34.
- Steinberg BJ, Hilton IV, Iida H, Samelson R. Oral health and dental care during pregnancy. Dent Clin North Am 2013;57(2):195-210.
- Silva de Araujo Figueiredo C, Goncalves Carvalho Rosalem C, Costa Cantanhede AL, Abreu Fonseca Thomaz EB, Fontoura Nogueira da Cruz MC. Systemic alterations and their oral manifestations in pregnant women. J Obstet Gynaecol Res 2017;43(1):16-22.
- Giglio JA, Lanni SM, Laskin DM, Giglio NW. Oral health care for the pregnant patient. J Can Dent Assoc 2009;75(1):43-8.
- Daalderop LA, Wieland BV, Tomsin K, et al.
 Periodontal Disease and Pregnancy Outcomes: Overview of Systematic Reviews. JDR Clin Trans Res 2018;3(1):10-27.
Periodontal Disease and Pregnancy Outcomes: Overview of Systematic Reviews. JDR Clin Trans Res 2018;3(1):10-27. - U.S. Food and Drug Administration. Pregnancy & Lactation: Improved Benefit-Risk Information. 2015. https://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/SmallBusinessAssistance/UCM431132.pdf. Accessed May 4, 2021.
- U.S. Food and Drug Administration. Pregnancy and Lactation Labeling (Drugs) Final Rule. https://www.fda.gov/drugs/labeling-information-drug-products/pregnancy-and-lactation-labeling-drugs-final-rule. Accessed May 3, 2021.
- U.S. Food and Drug Administration. Questions and Answers on the Pregnancy and Lactation Labeling Rule. https://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093311.htm. Accessed May 4, 2021.
- Mendia J, Cuddy MA, Moore PA. Drug therapy for the pregnant dental patient. Compend Contin Educ Dent 2012;33(8):568-70, 72, 74-6 passim; quiz 79, 96.

- Oral Healthcare During Pregnancy Expert Workgroup. Oral Health Care During Pregnancy: A National Consensus Statement. Washington, DC: National Maternal and Child Oral Health Resource Center; 2012.
- Bassiur JP, Boyd BC, Burrell KH, et al. ADA/PDR Guide to Dental Therapeutics. Fifth ed. Montvale NJ: Physicians' Desk Reference, Inc.; 2009.
- California Dental Association Foundation; American College of Obstetricians and Gynecologists, District IX.
- U.S. Food & Drug Administration. FDA Drug Safety Communication: FDA has Reviewed Possible Risks of Pain Medicine During Pregnancy. 2015. https://www.fda.gov/Drugs/DrugSafety/ucm429117.htm. Accessed May 4, 2021.
- National Institute for Occupational Safety and Health. International Chemical Safety Cards: Nitrous Oxide. https://www.cdc.gov/niosh/docs/hazardcontrol/hc3.html. Accessed May 4, 2021.
- The National Institute for Occupational Safety and Health (NIOSH).
 Control of Nitrous Oxide in Dental Operatories (DHHS/NIOSH Publication No. 96-107). U.S. Department of Health & Human Services. https://www.cdc.gov/niosh/docs/hazardcontrol/hc3.html. Accessed May 4, 2021.
Control of Nitrous Oxide in Dental Operatories (DHHS/NIOSH Publication No. 96-107). U.S. Department of Health & Human Services. https://www.cdc.gov/niosh/docs/hazardcontrol/hc3.html. Accessed May 4, 2021. - National Council for Radiation Protection & Measurements. NCRP Report No. 145 - Radiation Protection in Dentistry. Bethesda: National Council on Radiation Protection and Measurement; 2003.
Professional Resources
- X-rays: Dental Radiography and Pregnancy
- Nitrous Oxide
Patient Resources
JADA “For the Patient” page:
- Pregnancy and oral health (March 2021)
ADA MouthHealthy:
- X-rays
- Pregnancy
- U.S. Centers for Disease Control and Prevention: Radiation and Pregnancy: A Fact Sheet for the Public
- Oral Healthcare During Pregnancy: A National Consensus Statement
- Recommendations on Oral Health Care for the Pregnant Adolescent
- Guideline on Oral Health Care for the Pregnant Adolescent
- LactMed (U.
 S. National Library of Medicine Toxicology Data Network drugs and lactation database)
S. National Library of Medicine Toxicology Data Network drugs and lactation database) - American Academy of Pediatrics: Oral Health Toolkit for Providers
Reviewed by: ADA Council on Advocacy for Access and Prevention and the ADA Center for Dental Practice.
Last Updated: May 4, 2021
Prepared by:
Department of Scientific Information, Evidence Synthesis & Translation Research, ADA Science & Research Institute, LLC.
Ozone therapy during pregnancy
Ozone therapy during pregnancy can be useful in many diseases: preeclampsia, toxicosis, fetal hypoxia, intrauterine growth retardation, infections, anemia. In addition, it can be indicated for gestational diabetes mellitus, obesity, stretch marks (stretch marks) of pregnant women. However, caution is needed in connection with the need to be responsible for the life of both the patient and the child. Only after examination and consultation with an experienced doctor, you can start ozone therapy during pregnancy. nine0013
nine0013
Sign
Sign
Sign up0013
Sign
Sign
Sign up
Sign up
Sign
Sign
Sign up
Book an appointment
Features of procedure
Pregnant women are most commonly treated intravenously. Intravenous injections are usually painless and well tolerated without any anesthesia.
Intravenous injections are usually painless and well tolerated without any anesthesia.
In order to achieve a noticeable therapeutic effect, ozone therapy during pregnancy is carried out in courses of five or more sessions. The therapeutic effect may appear earlier, especially with toxicosis and gestosis. nine0015 Ozone therapy for pregnant women is carried out strictly according to indications. Only after a preliminary examination and consultation with a doctor, by appointment.
Preparation and process
How to prepare for the procedure
An initial consultation with a doctor who performs ozone therapy is necessary to identify possible contraindications. After the consultation, it is possible to prescribe additional examinations of the mother and fetus.
Process description
Prenatal ozone therapy is most often limited to intravenous administration of saline saturated with ozone. Less often, the patient's blood is used, which is first taken, then ozonized and injected back intravenously (autohemotherapy). For the treatment of stretch marks, irrigation with nitrogen water and massage with ozonated oil are used. Subcutaneous and intradermal administration of ozone in pregnant women is rarely practiced. nine0003
What to do after removal
The first procedures of ozone therapy in pregnant women are carried out with caution, under the supervision of a physician. This is necessary in order to immediately detect side effects or individual intolerance not only in the mother, but also in the unborn child.
Why are diseases associated with pregnancy dangerous?
Pathology of pregnancy leads to the birth of premature babies, increases the risk of abortion, leads to an increase in the likelihood of congenital malformations and diseases. Modern treatment of many diseases of pregnant women (preeclampsia, fetal hypoxia, delayed development) is rather modestly presented and not as effective as we would like. In many cases, it is better to start ozone therapy at the first signs of disease. In the future, this can prevent stillbirth and reduce the likelihood of congenital diseases and malformations. nine0015 sign up
Sign
Sign up
Sign
Sign
sign up
oxygen mixture (area of one joint)
Sign up
Sign up
Show all prices
Equipment
As with other types of ozone therapy for the treatment of pregnant women, the main equipment is an ozonizer. From the air in this apparatus, ozone is synthesized using discharges of electricity. The resulting ozone dissolves almost immediately in saline or other liquids to avoid toxic effects on humans when inhaled. Other instruments, including droppers and intravenous needles, are standard medical equipment. nine0003
From the air in this apparatus, ozone is synthesized using discharges of electricity. The resulting ozone dissolves almost immediately in saline or other liquids to avoid toxic effects on humans when inhaled. Other instruments, including droppers and intravenous needles, are standard medical equipment. nine0003
FAQ
What are the reviews for ozone therapy for pregnant women?
In most cases, reviews are good due to the effectiveness of ozone therapy against nausea and vomiting that occurs in the first trimester in pregnant women. Favorable reviews are more common if ozone therapy is carried out by an experienced doctor who has fully examined the pregnant patient.
liquid nitrogen during pregnancy - 25 recommendations on Babyblog.ru
Periodically I write articles for various magazines and portals. I want to share one of them with you. nine0003
Published in My Baby and Me
Mothers spend hours looking at newborns and usually find something interesting. For example, moles and spots. Are these just cute “good luck kisses” or do you need to run to the doctor already?
For example, moles and spots. Are these just cute “good luck kisses” or do you need to run to the doctor already?
Causes of occurrence
There is no clear answer to the question of where moles come from in a newborn child. Some experts believe that their appearance is associated with the course of pregnancy and childbirth, others see “marks” of hormonal failure here, others are sure that moles can be transmitted genetically from parents: it is not so rare that a birthmark (nevus) or its location the baby and one of the parents match. nine0003
Maria, 30
My daughter was born with two marks. One is a convex mole under the knee, the other is a pink spot on the back of the head. A convex mole under the knee is family and is passed down through the female line from generation to generation. All the relatives insisted that we cauterize the spot on the back of the head. But my husband and I, after consulting with an endocrinologist, decided that we would wait and observe. Now my daughter is 4 years old, the spot on the back of her head has turned pale and almost merged with her skin color. It does not cause any psychological discomfort - it is not visible at all under the hair, and it seems that the daughter does not even realize that it is there. nine0321
Now my daughter is 4 years old, the spot on the back of her head has turned pale and almost merged with her skin color. It does not cause any psychological discomfort - it is not visible at all under the hair, and it seems that the daughter does not even realize that it is there. nine0321
Risk groups
According to statistics, birthmarks appear more often in premature babies. Babies with fair skin are also more likely to develop moles. If we talk about gender, then girls are born with nevi more often than boys.
Types of birthmarks
Neoplasms on the body of babies can be divided into two groups: pigmented spots that appear from cells that contain melanin and vascular skin defects. nine0003
Pigmented patches vary in color from light brown to black, raised and flat. Pigmentation almost never disappears; and, if there are more than six such spots on the baby’s body, you should definitely consult a specialist.
Vascular defects are bright burgundy or purple in color, are not considered dangerous and usually disappear without any intervention.
The most common vascular defects:
- Hemangioma . May appear during the first year of a child's life. This defect occurs on any part of the body. Usually after a year and a half it turns pale and merges with the color of the skin. In the vast majority of children, hemangiomas go away by the age of 10.
- "Stork bites" - the popular name for such a defect as telangiectasia. H most often appears on the back of the head, bridge of the nose and eyelids as a large spot or cluster of small pink spots. In most cases, such spots fade over time, but become brighter during stress and crying of the child. "Stork bites" do not carry any negative consequences for children. The main disadvantage of this stain is considered unaesthetic appearance. nine0346
- Wine stain or flaming nevus . These moles usually appear on the face or scalp and grow as the child grows. They appear due to the expansion of capillaries and do not carry any oncological risks.
Superstitions
According to folk signs, newborns with moles will have a happy life. Also among the people there are signs that explain the presence of moles in babies. For example, according to superstition, a pregnant woman should not darn clothes, because. the baby will be born with a patch. So that the child does not have a mole, folk rumor forbids the expectant mother from touching black animals. Another sign suggests that a woman who has experienced a strong fright during pregnancy will certainly give birth to a baby with a birthmark. nine0003
How to care for moles
- Do not cover moles with plaster. The created greenhouse effect can become a favorable environment for the development of melanoma.
- Keep your child out of direct sunlight. Don't forget sunscreen, hats, umbrellas, etc.
- Dry your baby with a dry towel after bathing. This is important because water droplets can create a magnifying glass effect, which can cause your baby to get burned.
 nine0015
nine0015 - If a child has abraded or damaged a mole, do not treat the wound with antiseptics. Apply a sterile bandage and seek medical advice.
- Do not remove hairs growing on a mole or in close proximity to a growth. This can not only damage the hair follicle, but also serve as a favorable factor in the accelerated growth of new birthmarks. Remember: any injury to a mole can provoke its rebirth!
Treatment and removal of moles
Most birthmarks do not need to be treated. Doctors advise parents to simply watch the birthmarks and wait until the child grows up - over the years, many birthmarks disappear or brighten.
But there are marks that are not just an aesthetically ugly skin defect, but also interfere with the child's normal life and threaten health. The latter include moles located in the eye area, bulging spots on the face, marks that can degenerate into melanoma, nevi in an area that is amenable to constant friction and contact with other parts of the body or clothing. nine0003
nine0003
In this case, the mole is completely removed by surgery. The decision to operate is usually made by the oncologist.
Today there are the following treatment options for birthmarks:
- Laser therapy . The most modern and painless method that does not leave scars behind. Laser therapy is not suitable for all types of spots.
- Cryotherapy , or cauterization with liquid nitrogen. The most painful way to remove moles. After the procedure, small scars may form. nine0015
- Prescribing hormonal preparations that slow down the growth of spots.
Olga, 35 years old
The eldest son was born with a port-wine stain on his face. After consultation with an oncologist, we were convinced that the neoplasm does not pose any danger. But the son is very complex because of the appearance, so we decided to remove the stain with a laser.
This is important!
The probability of the appearance of malignant formations from moles is low.