Nipple stings after breastfeeding
Nipple Vasospasm and Breastfeeding - Breastfeeding Support
A vasospasm is a sudden narrowing (or constriction) of blood vessels. If the blood vessels in the nipple have a vasospasm this can cause nipple pain and sometimes deeper breast pain. A breastfeeding baby can trigger a nipple vasospasm if they are not attached (latched) to the breast comfortably ie with a big mouthful of breast tissue as well as the nipple. A nipple vasospasm can also be connected with Raynaud’s phenomenon (a condition affecting blood supply). This article looks at the symptoms, causes and possible treatments for easing nipple vasospasm.
Search Articles
Need to look something up?
Nipple vasospasm and breastfeeding
If a nipple is flattened or compressed because a baby is pinching the nipple during a breastfeed, this may trigger a nipple vasospasm. The nipple may look pointed or slanted like the top of a new lipstick straight after a feed and, since the blood vessels in the nipple are narrowed, less blood can flow and the nipple can temporarily turn white. When the blood flows back to the nipple after each breastfeed, mothers may feel a painful burning or throbbing sensation.
What are the symptoms of nipple vasospasm?
Symptoms of nipple vasospasm include:
- Painful nipples—the pain is often described as burning, stabbing or itching and may be felt a short time after breastfeeding and/or in between feeds.
- Sore nipples—nipple vasospasm is associated with misshapen nipples and sore nipples or previously damaged nipples that are healing.1
- White nipples—nipple tips may look white (blanched) after a feed or mothers may notice other colour changes in their nipples e.g. blue or dark red (also associated with Raynaud’s Phenomenon—see below)
- Deep breast pain—some mothers may feel deep breast pain or shooting pains deep in the breast sometimes referred to as Mammary Constriction Syndrome.

- Cold temperatures and stress may worsen the pain or trigger it.
Not vasospasm? Other causes of pain
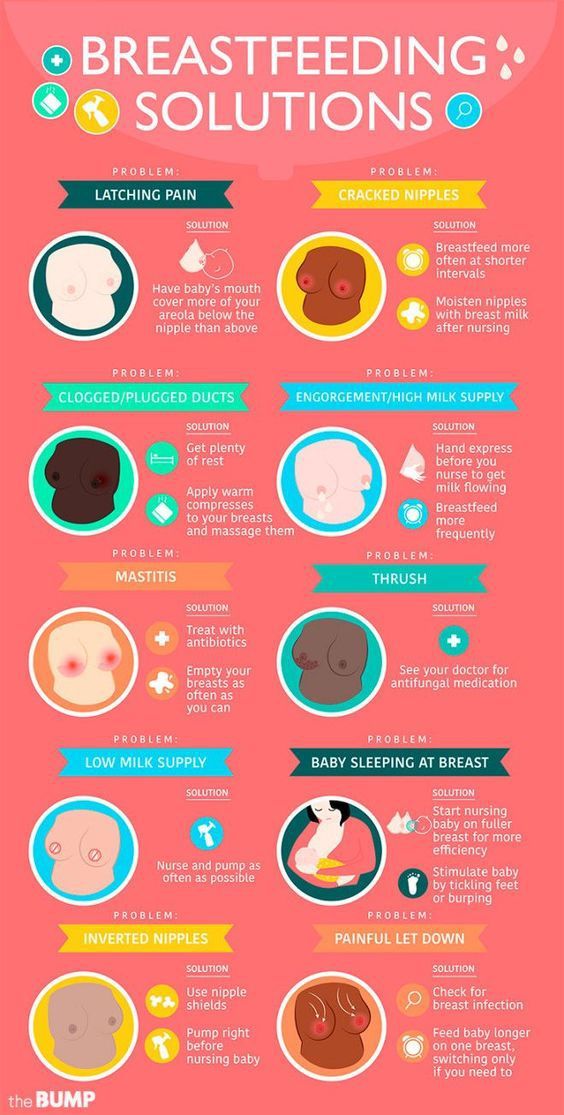
There are many causes of sore nipples or pain during breastfeeding and for a complete overview see Causes of Sore Nipples and Why Does Breastfeeding Hurt? Vasospasm symptoms such as burning pain and soreness can be very similar to those of a bacterial infection (e.g. a Staph infection) or a fungal infection (e.g. thrush). Note that a misdiagnosis of thrush and resulting unnecessary prescription medication, may make vasospasm symptoms worse.2
What causes nipple vasospasm?
There are a number of risk factors that seem to make nipple vasospasm more likely:
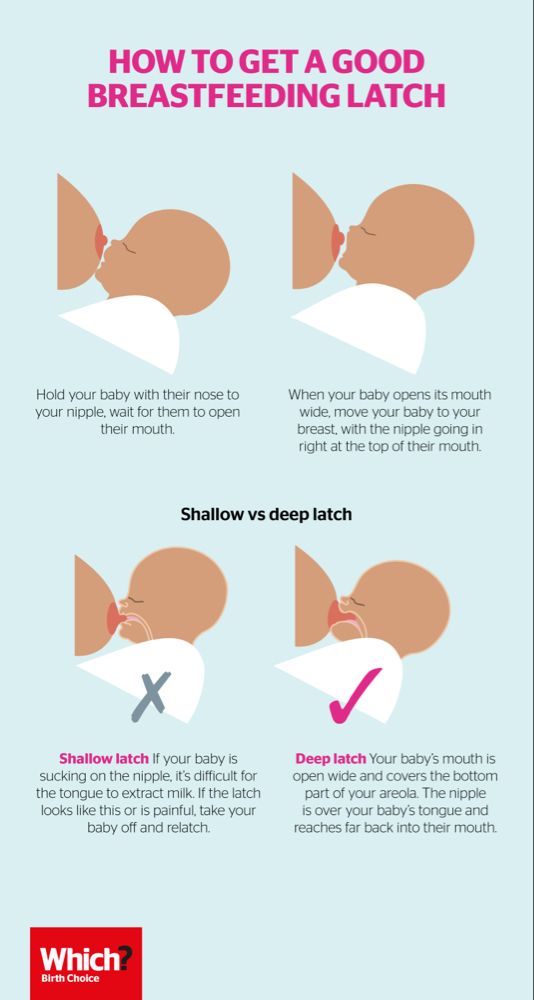
- A shallow latch. In breastfeeding mothers, the main trigger for nipple vasospasm is likely to be a poor latch (the way a baby attaches to the breast).
 If a baby breastfeeds with mostly only the nipple in their mouth and not a good deep mouthful of breast tissue as well, this is often called a shallow latch. In a shallow latch the nipple is more likely to get pinched between baby’s tongue and the roof of their mouth and trigger the vasospasm. Some babies also learn that pinching the nipples is a good way to slow the milk flow in a fast let-down.
If a baby breastfeeds with mostly only the nipple in their mouth and not a good deep mouthful of breast tissue as well, this is often called a shallow latch. In a shallow latch the nipple is more likely to get pinched between baby’s tongue and the roof of their mouth and trigger the vasospasm. Some babies also learn that pinching the nipples is a good way to slow the milk flow in a fast let-down. - Sore nipples. Sore nipples, damaged or cracked nipples, and nipples that are healing are associated with poor positioning at the breast and are risk factors for vasospasm (Thomas, 2013).
- Cold temperatures. Exposure to cold temperatures and climates, or the sudden drop in temperature when a baby lets go of the nipple is a risk factor for a nipple vasospasm.3
- Severe stress. Severe emotional stress is a risk factor for nipple vasospasm and a history of migraines may be a risk factor (Goldfarb, 2019).
- Medical conditions. An existing history of autoimmune disease eg lupus, rheumatoid arthritis, thyroid dysfunction, scleroderma, or previous diagnosis of Raynaud’s syndrome increases the likelihood of nipple vasospasm.4
- Cigarette smoking. Exposure to cigarette smoke, second-hand smoke or nicotine can be triggers for nipple vasospasm (Goldfarb, 2013).5
- Medications. Certain medications including fluconazole (prescribed for thrush), some decongestants, or birth control medication are risk factors for nipple vasospasm (Goldfarb, 2019; Breastfeeding Network, 2019) also beta-blockers, or vasoconstrictor medications which narrow blood vessels (Douglas, Vol 18: 1–29 2022).
- Caffeine may be a trigger for vasospasm (Goldfarb, 2019; Breastfeeding Network, 2019) however Douglas says there is no clear evidence linking caffeine intake to secondary Raynaud’s syndrome (vasospasm without existing Raynaud’s) (Douglas, Vol 18: 1–29 2022).

How can I avoid vasospasm symptoms?
Minimising the risk factors can work very well to help prevent symptoms of nipple vasospasm, namely:
- Get help with positioning from an International Board Certified Lactation Consultant so that your baby’s latch is not triggering vasospasm. A poorly latched baby, an ineffective suck or the baby clamping on the nipple can all cause nipple blanching. Babies with high muscle tone or those with tummy ache (e.g. from a food allergy) may seem to “bite” at the breast and can cause a nipple vasospasm. A baby needs to attach to the breast deeply with a big mouthful of breast as well as the nipple. See Breastfeeding Positioning for Newborns, Latching Tips and Why Does Breastfeeding Hurt? for more information and see your breastfeeding specialist for one to one help.
- Check pumping equipment. A poorly fitted pump flange could cause nipple damage and vasospasm symptoms, conversely pumping with a well fitted pump may offer relief to symptoms compared to breastfeeding for some women until they can get help with positioning.

- Keep warm; breastfeed in a warm room and cover the nipple as soon as a breastfeed ends. Don’t leave nipples to air dry as they will get colder that way. Keep breastpads dry, some mothers use woollen or fleecy breastpads for warmth. Try to avoid sudden temperature changes.6
- Avoid latching a baby while the nipple is having a vasospasm, as this may cause damage to the nipple, try warming the breast and repeatedly squeezing the nipple to help blood flow back into this area before latching (Hills, accessed Oct 2022).
- Gentle massage. Try massaging the nipples with warm olive oil after a breastfeed to stop a nipple vasospasm.78 Repeatedly squeezing the nipple during a vasospasm helps blood flow return to the nipple and can improve recovery time.
 9
9 - Rule out a bacterial infection or thrush—check with your health professional that you don’t have any other causes of burning pain and sore nipples.
- Avoid potential triggers: cigarette smoke and smoking, nicotine, caffeine, or any medications that promote vasoconstriction e.g. some decongestants10 and avoid stress where possible.
- Keep active with aerobic exercise.
Raynaud’s phenomenon
Raynaud’s is a disorder of the tiny blood vessels of the extremities which reduces blood flow. Cold temperatures or strong emotions cause the blood vessels in the extremities to go into spasms, which may cause pain, numbness, throbbing and tingling. Some women who have Raynaud’s in the fingers and toes may find they get Raynaud’s of the nipple when they breastfeed. This might be because breastfeeding affords lots of opportunities for nipples to get cold e.g. just before and after latching. Painful breastfeeding can also be stressful. Raynaud’s is often misdiagnosed as thrush or a poor latch .11
This might be because breastfeeding affords lots of opportunities for nipples to get cold e.g. just before and after latching. Painful breastfeeding can also be stressful. Raynaud’s is often misdiagnosed as thrush or a poor latch .11
Diagnosis of Raynaud’s
Raynaud’s symptoms affecting the nipple may be difficult to distinguish from nipple vasospasm caused by a poor latch:
- Symptoms can be triggered by cold and may still occur in spite of a good latch.
- Colour changes of the nipples e.g. from white to blue to red/purple may be seen with lighter skin tones.
- Raynaud’s may be linked with a history of migraines or a history of poor circulation 12.
- May be associated with previous breast surgery and nipple damage1314
Treatments for nipple vasospasm
In addition to using the above ideas to avoid getting vasospasm symptoms, there are a number of treatment options for nipple vasospasm that still persists after a poor latch has been corrected and other infections ruled out. Treatments options are discussed in the following patient information handout from the Goldfarb Breastfeeding Clinic and include pain relief, dietary supplements (calcium, magnesium and vitamin B6), omega fatty acids and prescription medication:
Excerpt from
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
- The use of Advil™ or Motrin™ (ibuprofen) and/or Tylenol™ (acetaminophen) may be very useful to treat the pain of nipple vasospasm. These medications are safe during breastfeeding.
- Your health professional may suggest high doses of calcium and magnesium, and vitamin B6.
Please consult your health professionals for doses specific to your case.
- Omega fatty acids may also help. Evening primrose oil (up to 12 capsules a day) and fish oil capsules are rich sources of omega fatty acids.
- Nifedipine (Adalat™) […] normally used for high blood pressure, can also be used for nipple vasospasm, and is safe for breastfeeding mothers and infants.
Nifedipine
Refer to the full Goldfarb article online for precautions regarding nifedipine and share this with your health care professional. The Breastfeeding Network discusses doses and side effects of nifedipine in their fact sheet Raynaud’s Phenomenon in Breastfeeding Mothers and for more places to find information about the safety of nifedipine online see Medications and Breastfeeding. Always discuss medications or medicinal doses of supplements with your health care provider.
Treatment tips from Dr Jack Newman
Jack Newman, a Canadian paediatrician and breastfeeding expert, has a protocol for treating vasospasm; see Vasospasm on his website. In addition to a discussion of certain vitamin and mineral supplements (also referred to in the patient handout quoted above), Dr Newman advocates:
In addition to a discussion of certain vitamin and mineral supplements (also referred to in the patient handout quoted above), Dr Newman advocates:
- All Purpose Nipple Ointment (APNO), a topical cream with antibacterial, antifungal and anti-inflammatory ingredients to help with soreness.
- Massaging olive oil into the nipples as an alternative to APNO.
- Pectoral muscle massage see Mammary Constriction Syndrome.
Complementary medicine
Scleroderma and Raynaud’s UK (SRUD) discuss natural and over the counter complementary medicine for scleroderma and Raynaud’s in Natural Therapies. They discuss how vitamin C, vitamin E, gamolenic acid (GLA), ginkgo bilboa and ginger may help symptoms in the general population but note this article is not specific to breastfeeding mothers. For the latest recommendations on the compatibility of individual supplements with breastfeeding check online at e-Lactancia or LactMed. Always discuss taking therapeutic doses of supplements with your qualified health professional to make sure they are compatible with your medical history and existing medication.
Always discuss taking therapeutic doses of supplements with your qualified health professional to make sure they are compatible with your medical history and existing medication.
The Breastfeeding Network fact sheet for Raynaud’s adds that it may be helpful to include ginger in the mother’s diet e.g. drink ginger tea, or even add a spoonful of ground ginger to bath water.
Summary
Nipple vasospasm is a narrowing of blood vessels in the nipple. It can be triggered by a baby breastfeeding in a shallow latch and can cause burning, stabbing or itching pain in the nipples after a breastfeed. Nipple vasospasm can also be associated with Raynaud’s phenomenon and can also cause Mammary Constriction Syndrome or deep breast pain. Treatment involves improving a baby’s latch and positioning at the breast, and avoiding the triggers of nipple vasospasm. Some medications and natural remedies may help symptoms.
Footnotes & References
-
Thomas.
 The problem with yeast. Too much diagnosis. Too little data. Adapted from Dr Jen’s Guide to Breastfeeding p98. 2012 [accessed 21 October 2022]
The problem with yeast. Too much diagnosis. Too little data. Adapted from Dr Jen’s Guide to Breastfeeding p98. 2012 [accessed 21 October 2022] -
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
-
Nipple Vasospasm Patient Handout, Herzl Family Practice Centre, Goldfarb Breastfeeding Clinic, 2019
-
Douglas. Re-thinking lactation-related nipple pain and damage. Women’s Health Volume 18: 1–29 2022
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Hills. Raynaud’s of the Nipple: Help for Pregnant & Breastfeeding Moms. Raynauds.org [accessed 20 October 2022]
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Newman. Vasospasm.
 2019
2019 -
Raynaud’s Information. Summerwarmth.co.nz [accessed 20 October 2022]
-
Raynaud’s Syndrome, Breastfeeding Network, 2019
-
Anderson et al, Raynaud’s Phenomenon of the Nipple: A Treatable Cause of Painful Breastfeeding, Pediatrics, 2004
-
Raynaud’s Phenomenon in Breastfeeding Mothers, Breastfeeding Network, 2019
-
Anderson et al, Raynaud’s Phenomenon of the Nipple: A Treatable Cause of Painful Breastfeeding, Pediatrics, 2004
-
Hills. Raynaud’s of the Nipple: Help for Pregnant & Breastfeeding Moms. Raynauds.org [accessed 20 October 2022]
Breast & nipple thrush | The Royal Women's Hospital
Breast and nipple thrush can cause strong nipple and breast pain. The pain may be severe enough to lead to early weaning if the condition is not treated.
Thrush is a fungal infection caused by the organism Candida albicans, which can occur in the nipples or breast tissue (as well as other places in the body).
If you have nipple pain that doesn’t go away when you adjust your breastfeeding attachment, you may need to talk with a lactation consultant or other health care professional. Early diagnosis and treatment of nipple and breast thrush will help to improve your breastfeeding experience.
Causes
Breast and nipple thrush may be linked to a history of vaginal thrush, recent use of antibiotics or nipple damage. However, sometimes the cause is not known.
Symptoms
The most common symptom is nipple pain or breast pain, or both.
Nipple thrush pain is often described as burning, itching, or stinging and may be mild to severe. The pain is usually ongoing and doesn’t go away with improved positioning and attachment of your baby to the breast. Your nipples may be tender to touch and even light clothing can cause pain.
Breast thrush pain can vary. It has been described as a stabbing or shooting pain, a deep ache or a burning sensation that radiates through the breast. It may be in one or both breasts.
Often this pain is experienced immediately after, as well as in between, feeds.
Signs of nipple and breast thrush
There are usually no obvious signs of thrush on your nipples. However some signs may be present and include:
- your nipples may appear bright pink; the areola may be reddened, dry or flaky. Rarely a fine white rash may be seen
- nipple damage (e.g. a crack) that is slow to heal
- signs of thrush may be present in your baby's mouth or on your baby's bottom, or both. Thrush in the mouth appears as a thick white coating on the tongue or white spots on the inside of the cheeks, or both. Thrush on a baby's bottom appears as a bright red rash with spots around it which does not clear without antifungal cream.
If you or your baby have been diagnosed with thrush you will be both need to be treated.
Management and treatment
Breast or nipple thrush is treated with antifungal tablets and creams. You also need to treat thrush in your baby and any other fungal infection in you or your family members.
- Thrush in your baby’s mouth is treated using an oral gel or drops.
- Breast and nipple thrush is treated with antifungal medicine and antifungal nipple gel/creams.
- Treat any other site of fungal infection in the whole family, i.e. vagina, nappy rash, feet.
- Keep your nipples dry by frequently changing breast pads as thrush grows well in a moist and warm environment.
- Clean teats and dummies thoroughly after use and boil for five minutes. Replace weekly if possible.
- To prevent the spread of thrush, wash your hands thoroughly after nappy changes and before and after applying any creams/lotions.
- Wash towels, bras, cloth nursing pads etc. in hot soapy water and air dry outside.
Related Health Topics
-
- Breast and nipple thrush
Breast and nipple thrush can cause strong nipple and breast pain.
 This pain may be severe enough to lead to early stopping of breastfeeding if not appropriately treated.
This pain may be severe enough to lead to early stopping of breastfeeding if not appropriately treated. -
- (English) PDF (387 KB)
- Breast and nipple thrush
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Why nipples itch and how to get rid of itching
October 14, 2021 Likbez Health
If you notice that your nipples have also changed shape, contact your doctor immediately.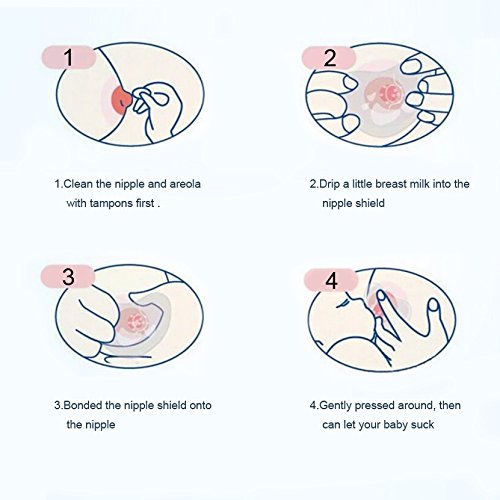
You can also listen to this article. If it's more convenient for you, turn on the podcast:
Mild short-term itching in the chest is most often a safe and easily eliminated phenomenon. But exceptions are possible.
Here are the most common causes of itchy nipples in both women and men. nine0003
1. Dry air
Itching and irritation are the first signs that the skin lacks moisture. The skin on the nipples is thinner than on most other parts of the body, so it reacts to dehydration earlier.
What to do about it
- Keep an eye on the humidity in the room where you spend time.
- Don't forget to use moisturizers and gels after you shower.
- Drink enough water.
2. Atopic dermatitis
Or eczema. This skin inflammation sometimes occurs on the nipple or areola, the flat, pink area around it. It is not always possible to establish the causes of dermatitis: it can be associated with allergies, hormonal changes, pregnancy, breastfeeding.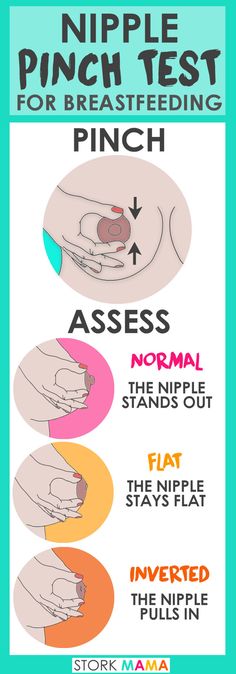
Eczema can be recognized by a mild, sometimes itchy rash on the nipple and areola. These pimples are both dry and weeping.
What to do about it
The best option is to consult a general practitioner or dermatologist. As a rule, moisturizing creams with ceramides (they are also called ceramides) help with eczema on the nipples, a waxy substance that is part of the stratum corneum of the skin and can help restore it. Sometimes hydrocortisone ointments and creams are used to reduce itching and swelling. Perhaps, heavy artillery will also be required - drugs that are sold in pharmacies only by prescription. nine0003
3. Unsuitable detergent
Soap, shower gel or powder that you have washed on a T-shirt or dress - the chemicals in them can sometimes cause contact dermatitis. As a rule, it manifests itself as itchy reddened spots all over the body or in areas with increased skin sensitivity. The nipples are those areas.
What to do about it
If your nipples itch for no reason at first glance, remember if you have used a new shower gel or washing powder. Give it up for a while and monitor your condition. If the itching goes away, then your skin just doesn't like the particular product. Try not to use it. nine0003
Give it up for a while and monitor your condition. If the itching goes away, then your skin just doesn't like the particular product. Try not to use it. nine0003
4. Unsuitable laundry
Dermatitis can also occur due to contact with the fabric. Often this is the fault of woolen and synthetic fibers, microfiber, fabrics with the addition of bright dyes and a high content of elastane.
What to do about it
Think about the situations in which your nipples itch and whether this is due to the fact that you are wearing a particular bra or T-shirt. If the reason seems likely to you, give up suspicious underwear for a while and observe your condition. nine0003
5. Friction
A tight bra, hard T-shirt or tank top can rub on the nipples. Those in response are irritated and itchy.
How to deal with it
Rethink your wardrobe for softer, looser bottoms. If you're talking about a sports bra that needs to be tight, use nipple shields or apply Vaseline to your skin before training to help reduce friction.
6. Pregnancy and lactation
During these periods, the breasts increase in size, the skin stretches, and in the thinnest areas - on the nipples and areola - it sometimes begins to itch. Unpleasant sensations enhance hormonal changes in the body. nine0003
What to do about it
You can lubricate your nipples with natural cocoa butter, coconut oil or lanolin ointment. But it is better to consult a gynecologist or therapist.
7. Excess weight
The same as during pregnancy: an increase in breast volume leads to itching and irritation. In addition, excess body fat affects the hormonal background, which contributes its five cents.
What to do about it
The strategically correct option is to get rid of excess weight. To reduce itching here and now, use a moisturizer, coconut or cocoa butter, and if the discomfort is severe, then a pharmacy hydrocortisone ointment. nine0003
8. Fungal and bacterial infections
They are more common in breastfeeding women. But men can also pick up an infection: harmful microbes and fungi enter the body through injured skin. If this happens, itching will be the least of the problems - with such an infection, the nipples also hurt.
But men can also pick up an infection: harmful microbes and fungi enter the body through injured skin. If this happens, itching will be the least of the problems - with such an infection, the nipples also hurt.
What to do about it
Be sure to consult a general practitioner, mammologist, gynecologist. The specialist will figure out what kind of infection we are talking about and prescribe the necessary medicines for you. nine0003
9. Menopause in women
During menopause, the skin becomes thinner, dry, irritated. And the nipples are the first to react.
What to do about it
Avoid hot showers or baths, use mild cleansers, and moisturize your skin more often to retain moisture.
10. Tumors
Itching may be one of the first symptoms of their development. And both benign and malignant. Other signs:
- change in the shape of the nipple; nine0023
- rash or crust on the nipple;
- discharge from the nipples;
- pits and irregularities on the skin of the chest.

What to do about it
Go to a general practitioner or mammologist as soon as possible. The earlier the tumor is detected, the higher the chances of recovery.
Read also 👩⚕️👍💊
- 10 reasons not to wear a bra
- How not to catch scabies and how to treat it
- 9 facts about breasts and nipples
- Why breasts hurt: 11 harmless and frightening reasons
- Why the head itches and how to get rid of itching
ᐈ Breast thrush • How candidiasis of the skin of the nipples manifests itself in breastfeeding
Breast pain during lactation: a norm or a symptom
You must have heard other mothers complain about pain and severe discomfort during breastfeeding. Such stories could be told by a mother, aunt or grandmother, adding: “at first it’s always like that, you need to endure it.” Therefore, you think that discomfort in the mammary gland is normal and should be so. nine0003
But things are not so simple. Yes, discomfort in some cases may appear immediately after you start breastfeeding. It will be a response to new sensations. But also chest pain indicates diseases that need to be recognized and cured. In this case, you need to answer yourself the following questions:
Yes, discomfort in some cases may appear immediately after you start breastfeeding. It will be a response to new sensations. But also chest pain indicates diseases that need to be recognized and cured. In this case, you need to answer yourself the following questions:
- What is the nature of the pain?
- Does it hurt in one nipple or two?
- Is the pain localized only in the nipples or does it spread to the whole breast? nine0023
- When exactly does the discomfort occur - at the beginning or at the end of feeding?
- How does the breast look, is there any redness or swelling?
- How long does the pain last?
- Do your nipples hurt between feedings?
- When did the pain - start from the first days of feeding or later?
Often the cause of pain in the mammary gland is an inflammatory process caused by a fungus of the genus Candida. This is thrush of the breasts - a fairly common disease. nine0003
Photo 1. Any pain is a reason to see a doctor.
Any pain is a reason to see a doctor.
Symptoms thrush on the nipples
It is not necessary to self-diagnose. And "Doctor Google" is not the best assistant in the treatment of a nursing mother. Similar or similar symptoms are typical for dermatitis of the skin of the nipples, eczema and psoriasis, damage to the epidermis of the breast with improper attachment or pumping.
If you have any complaints, see a dermatologist or mammologist. The doctor takes into account the symptoms and predisposing factors, makes an accurate diagnosis. nine0003
Make an appointment for an examination
Make an appointment at the center
Treatment of thrush in 7 steps
- Provide air to the affected nipples. During treatment, do not use breast pads or, if this is not possible, change them as often as possible.
- Maintain personal hygiene: wash your hands thoroughly after changing a diaper and washing your baby, after going to the toilet, before every feeding.

- Wash your nipples with baking soda (1 teaspoon per glass of water) after each breastfeed to relieve symptoms. nine0023
- Thoroughly sterilize everything that comes into contact with the breast (pads, breast pump) and change your bra as often as possible.
- Choose underwear made from natural materials (cotton, linen, silk), as synthetics cause additional irritation.
- Temporarily eliminate sweets, baked goods, alcoholic and sugary carbonated drinks from your diet.
- Take medications that are compatible with breastfeeding as prescribed by your doctor at your appointment. nine0023
Photo 2. Your comfort is key when breastfeeding
Rules for feeding your baby with candidiasis
Follow the basics of personal hygiene, and also:
9002 feed your baby more often.