How do i know if my child has dyspraxia
Developmental co-ordination disorder (dyspraxia) in children - Symptoms
Developmental co-ordination disorder (DCD) can cause a wide range of problems. Some of these may be noticeable at an early age, while others may only become obvious as your child gets older.
Problems in infants
Delays in reaching normal developmental milestones can be an early sign of DCD in young children. For example, your child may take slightly longer than expected to roll over, sit, crawl or walk.
You may also notice that your child:
- shows unusual body positions (postures) during their 1st year
- has difficulty playing with toys that involve good co-ordination, such as stacking bricks
- has some difficulty learning to eat with cutlery
These signs might come and go.
Problems in older children
As your child gets older, they may develop more noticeable physical difficulties, plus problems in other areas.
Movement and co-ordination problems
Problems with movement and co-ordination are the main symptoms of DCD.
Children may have difficulty with:
- playground activities such as hopping, jumping, running, and catching or kicking a ball. They often avoid joining in because of their lack of co-ordination and may find physical education difficult
- walking up and down stairs
- writing, drawing and using scissors – their handwriting and drawings may appear scribbled and less developed compared to other children their age
- getting dressed, doing up buttons and tying shoelaces
- keeping still – they may swing or move their arms and legs a lot
A child with DCD may appear awkward and clumsy as they may bump into objects, drop things and fall over a lot.
But this in itself isn't necessarily a sign of DCD, as many children who appear clumsy actually have all the normal movement (motor) skills for their age.
Some children with DCD may also become less fit than other children as their poor performance in sport may result in them being reluctant to exercise.
Additional problems
As well as difficulties related to movement and co-ordination, children with DCD can also have other problems such as:
- difficulty concentrating – they may have a poor attention span and find it difficult to focus on 1 thing for more than a few minutes
- difficulty following instructions and copying information – they may do better at school in a 1-to-1 situation than in a group, so they can be guided through work
- being poor at organising themselves and getting things done
- being slow to pick up new skills – they need encouragement and repetition to help them learn
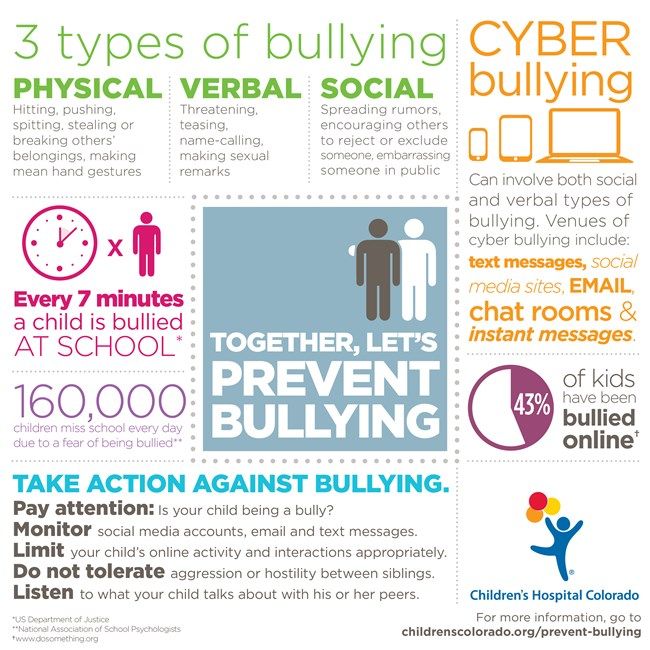
- difficulty making friends – they may avoid taking part in team games and may be bullied for being "different" or clumsy
- behaviour problems – often stemming from a child's frustration with their symptoms
- low self-esteem
Although children with DCD may have poor co-ordination and some additional problems, other aspects of development – for example, thinking and talking – are usually unaffected.
Related conditions
Children with DCD may also have other conditions, such as:
- attention deficit hyperactivity disorder (ADHD) – a group of behavioural symptoms that include inattentiveness, hyperactivity and impulsiveness
- dyslexia – a common learning difficulty that mainly affects the way people read and spell words
- autism – a condition that affects social interaction, communication, interests and behaviour
Some children with DCD have difficulty co-ordinating the movements required to produce clear speech.
Help us to improve our website today
If you have dyspraxia, please do you have a few moments to help us today?
Take our survey
Page last reviewed: 28 August 2019
Next review due: 28 August 2022
What It Is, Causes, Symptoms, Diagnosis & Treatment
Overview
What is dyspraxia?
Dyspraxia, also known as developmental coordination disorder (DCD), is a chronic condition that begins in childhood that causes difficulties with motor (movement) skills and coordination.
Dyspraxia can cause a wide range of issues with movement and coordination. Some of these may be noticeable at an early age, while others may only become obvious as your child gets older. Dyspraxia can affect your child’s coordination skills, which can make riding a bicycle or playing sports difficult. It can also affect their fine motor skills, such as writing or fastening buttons.
In the latest edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), developmental coordination disorder is subcategorized as a motor disorder within the broader category of neurodevelopmental disorders. It was previously listed as a learning disorder.
Dyspraxia in adults
When it’s not used in the context of childhood developmental coordination disorder, the term “dyspraxia” has a broader meaning.
Healthcare providers may also use the term “dyspraxia” to describe movement difficulties that happen later in life because of damage to your brain, such as from a stroke or brain injury.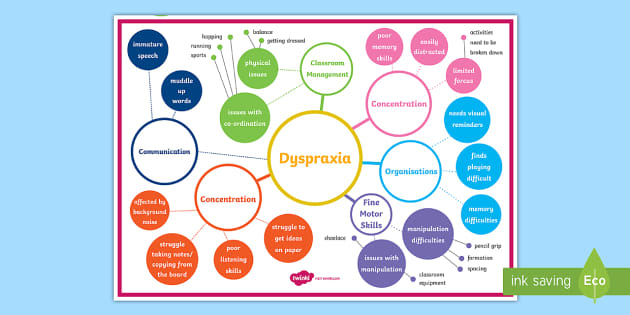 Providers may refer to this as acquired dyspraxia.
Providers may refer to this as acquired dyspraxia.
What is the difference between dyspraxia and apraxia?
Healthcare providers sometimes use the terms “apraxia” and “dyspraxia” interchangeably. However, apraxia is often more severe than dyspraxia. Apraxia means that you completely lose the ability to do something even though you understand the command and have a willingness to perform the movement. Dyspraxia means that you partially lose the ability to do something with accuracy.
Apraxia also has several different subtypes, including childhood apraxia of speech, limb-kinetic apraxia (the inability to make precise movements with your finger, arm or leg) and constructional apraxia (the inability to draw or copy simple diagrams or to construct simple figures).
Who does dyspraxia affect?
The first signs of dyspraxia (developmental coordination disorder) begin in childhood during the developmental period. As it’s a chronic condition, dyspraxia can persist into adulthood as well.
Dyspraxia more commonly affects men and people assigned male at birth than women and people assigned female at birth.
Your child may be more likely to have dyspraxia if:
- They were born prematurely before the 37th week of pregnancy, especially if they were born before the 32nd week of pregnancy.
- They were born with a very low birth weight (less than 4 pounds).
- They have a family history of developmental coordination disorder.
How common is dyspraxia?
Dyspraxia (developmental coordination disorder) is relatively common. It affects approximately 6% of school-aged children.
Symptoms and Causes
What are the signs and symptoms of dyspraxia (developmental coordination disorder)?
Dyspraxia (developmental coordination disorder) can cause a wide range of issues with coordination and motor skills. While most people with dyspraxia show signs of the condition by the time they start school, some people have mild forms of the condition that are more difficult to detect.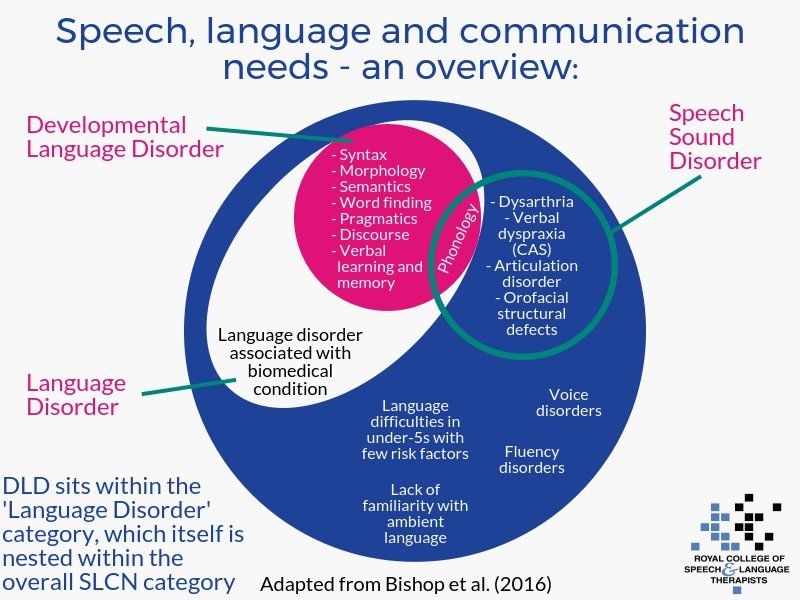
Signs of dyspraxia in babies and toddlers
Delays in reaching expected developmental milestones can be an early sign of dyspraxia in babies and toddlers. For example, your child may take longer than expected to roll over, sit, crawl or walk.
You may also notice that your child:
- Has difficulty playing with toys that involve good coordination, such as stacking cups.
- Has some difficulty learning to eat with spoons and forks.
Signs of dyspraxia in older children
Signs of dyspraxia in older children include:
- Difficulty with walking up and down stairs.
- Difficulty with balance — they may bump into objects, fall frequently or seem clumsy.
- Difficulty with sports and activities, such as riding a bike; jumping; and catching, throwing or kicking a ball. They may avoid participating in activities because of their lack of coordination.
- Difficulty with writing, drawing/coloring and using scissors compared to other children their age.

- Difficulty getting dressed, fastening buttons, brushing their teeth and tying shoelaces.
- Restlessness — they may swing or move their arms and legs frequently.
Your child may become frustrated when trying to perform these tasks.
Children with dyspraxia are also more likely to develop overweight or obesity since they may be reluctant to exercise due to difficulties and frustration with coordination.
What causes dyspraxia?
Performing coordinated movements and motor skills is a complex process that involves many different nerves and parts of your brain. Any issue in this process could potentially lead to difficulties with movement and coordination (dyspraxia).
Researchers aren’t sure of the exact cause of dyspraxia. But being born pre-term (before 37 weeks of pregnancy) and having a low birth weight put children at higher risk for having dyspraxia.
Diagnosis and Tests
How is dyspraxia diagnosed?
Although signs of dyspraxia (developmental coordination disorder) are present from an early age, they can be easy to miss, as children vary widely in their rate of development. Because of this, a definite diagnosis of DCD doesn’t usually happen until a child is 5 years old or older.
Because of this, a definite diagnosis of DCD doesn’t usually happen until a child is 5 years old or older.
Dyspraxia should be diagnosed by a team of professionals qualified to examine the specific criteria for the condition, which may include a:
- Pediatrician.
- Occupational or physical therapist.
- Child psychologist.
- Pediatric neurologist.
There are no medical tests that can definitively diagnose dyspraxia. Instead, your child’s team of healthcare providers will ask detailed questions about your child’s medical history, development and symptoms. They’ll assess your child’s gross and fine motor skills, coordination and balance. They’ll also assess your child’s mental ability to see if it’s within the expected range for their age.
Healthcare providers will also need to rule out other possible causes of your child’s motor difficulties, such as cerebral palsy or muscular dystrophy.
For a child to be diagnosed with dyspraxia (developmental coordination disorder), they typically need to meet all of the following criteria:
- Their motor skills are significantly below the level expected.

- Their lack of motor skills and coordination affects their daily activities and achievements at school.
- Symptoms of dyspraxia first developed during an early stage of their development.
- Their difficulty with motor skills isn’t better explained by other medical conditions.
Management and Treatment
How is dyspraxia managed and treated?
There’s no cure for dyspraxia (developmental coordination disorder), but different types of therapies, such as occupational therapy and physical therapy, can help children and adults with dyspraxia improve their motor skills and coordination.
As dyspraxia affects everyone differently, your child will benefit most from an individualized treatment plan to manage their physical difficulties and improve their confidence.
One of the main types of therapies providers use to help children with dyspraxia is called task-oriented intervention. It involves working with your child to identify specific tasks that cause difficulties and finding ways to overcome them.
For example, an occupational therapist can help your child improve difficulties with specific tasks by breaking down the movements into smaller steps. They then teach your child to use these individual movements and practice them regularly.
Your child may also benefit from adapting certain tasks to make them easier to perform. For example, adding special grips to pens and pencils can make them easier to hold.
Outlook / Prognosis
What can I expect if my child has dyspraxia?
It’s important to remember that no two children with dyspraxia (developmental coordination disorder) are affected in the same way. The best way to know what to expect is to talk to healthcare providers who specialize in diagnosing and treating dyspraxia.
Other conditions that often co-occur or share symptoms with dyspraxia include:
- Attention deficit hyperactivity disorder (ADHD). About half of children with dyspraxia also have ADHD.
- Language difficulties.
- Dysgraphia.

- Mental health conditions, such as anxiety and depression.
- Autism spectrum disorder.
If your child has symptoms of any of these conditions, it’s important to make sure they’re properly diagnosed and receive treatment.
Living With
How can I take care of my child with dyspraxia?
One of the most important things you can do to help your child is to be an advocate for them, which involves understanding the challenges and letting your child know you’re going to support them no matter what — at home, at school and as they grow.
If your child is eligible for special education, you’ll work with professionals to develop an Individualized Education Program (IEP) that will help your child in school.
When should my child see their healthcare provider about dyspraxia?
Your child may need support to help them learn ways to overcome difficulties with motor skills and coordination throughout their life. If you notice that your child is having difficulties with a new movement task, such as writing or learning to drive a car, talk to their healthcare provider and/or occupational therapist.
A note from Cleveland Clinic
If your child has dyspraxia (developmental coordination disorder), they may experience frustration when they understand how to perform a certain action, such as throwing a ball, but are unable to accurately perform the movement. Your child’s care management will likely be long-term to help them better perform tasks and improve coordination. Offer support and encouragement as your child reaches new milestones for motor skills and coordination each day.
Developmental Delays and Disabilities - Speech Development Center in Moscow
We help children cope with movement disorders, improve coordination and learn to perform complex movements. We accept children of any age. We are developing a comprehensive correction program, which includes classes with a neurologist, a game therapist and an osteopath, and homework. We help patients outside the clinic: we will consult by phone on any issue.
Symptoms of dyspraxia
Dyspraxia is a type of developmental delay in which the child has problems coordinating and performing complex actions, but there are no disturbances in muscle tone and paralysis. There are no physical pathologies in dyspraxia, so dyspraxia cannot be detected at an early age. As the child develops, the following symptoms appear:
There are no physical pathologies in dyspraxia, so dyspraxia cannot be detected at an early age. As the child develops, the following symptoms appear:
- Clumsiness, clumsiness;
- Inaccuracy while eating: food falls off cutlery, drinks spill while drinking;
- Bad posture;
- Falls out of the blue;
- Motility problems;
- Frequent stumbling while walking;
- Increased fatigue due to the fact that you have to make a lot of effort to perform daily activities;
- Problems with active games: the child cannot catch and throw a ball, ride a bicycle, it is difficult for him to jump and run; nine0010
- Poor memory: the child forgets the learned material during the day.
A child with dyspraxia, even at primary school age, often cannot dress himself: he confuses front and back, left and right shoes. Cannot fasten a button and tie shoelaces. Each time he thinks about which hand to hold the spoon and pencil. Sometimes these children do not have a sense of the direction of movement: the child can move chaotically if an adult does not lead him somewhere purposefully. This behavior is typical only for children 2-3 years old. nine0003
Dyspraxia does not go away on its own. Adolescents and adults are characterized by poor, unset "childish" handwriting, problems with drawing (a person cannot draw a straight line). Awkwardness also increases with age: people with dyspraxia have an awkward gait and everything “falls out of hand”. It takes several times more time to complete everyday activities than for ordinary people. People are inattentive and distracted, often forget about important things.
If you notice these symptoms in your child, be sure to consult a specialist. One of the main problems for people with dyspraxia is loneliness. Children ignore peers with “special features”, which is why people grow up isolated and unsociable from childhood, cannot work in a team, and suffer from depressive and anxiety disorders. nine0003
Correction methods of the Akme Center
Physical development. The main tool of our methodology is play therapy. Classes are held in a specially equipped room with the participation of parents and one or two specialists of the center: a neurologist, a play therapist and an osteopath. To prevent children from getting hurt during the game, the walls, floor and game elements in the room are soft.
We mainly use active games aimed at the comprehensive development of the musculoskeletal system. Classes help the child to feel his body and understand how to control it. We build the correction plan in such a way that at each lesson the weak areas of the child are tightened and the strong ones are strengthened. Thanks to this, the result becomes noticeable after the first sessions. nine0003
Working with parents. Parents must participate in every lesson of the center, because with the participation of parents, the child trusts doctors more and shows better results. The specialist explains to parents his actions during the lesson, helps to understand the child and develop his own approach to him. We do not give template methods, we teach how to find a way out of difficult situations, choose the right words to support the child. Mutual understanding and skills of working with a child remain with parents forever. Thanks to this, the treatment does not end with several weekly sessions, but continues at home. nine0003
If parents have any questions when doing homework, we will consult by phone.
Hardware methods. We use safe hardware techniques: electrocardiography and micropolarization. The Varicard electrocardiograph helps to assess the child's fatigue by the end of the session. This is important, because the same exercises exhaust one child and are insufficient in terms of load for others. By monitoring the condition of the child, we increase or decrease the load, so that it matches the possibilities. nine0003
Micropolarization - stimulation of the spinal cord and brain with weak currents. The device normalizes muscle tone, breathing, stimulates mental and motor activity.
Appointment
To consult with a specialist of the center and start treatment, order a call back or write to us through a special form on the site. We will respond as soon as possible and select a convenient appointment time for you.
Dyspraxia in children: what is it
- Home >
- About clinic >
- Publications >
- "Clumsy child" or dyspraxia syndrome in children
All children go through a stage of clumsiness as they grow and develop. If complaints of coordination difficulties and fine motor deficits persist after 7 years, it is necessary to find out if this child has dyspraxia.
nine0067
Dyspraxia (clumsy child syndrome, coordination awkwardness, difficulties in motor reactions) is such a disorder of the motor system when a child has difficulty coordinating his actions while performing complex and purposeful movements, but at the same time he has neither paralysis nor impaired muscle tone .
Between 6 and 20% of children suffer from dyspraxia. According to the results of recent studies, a violation of the development of motor functions is detected in approximately 50% of children with the consequences of hypoxic-ischemic brain damage during the perinatal period. nine0003
Up to 10% of Brits have symptoms of dyspraxia, with men suffering 4 times more often than women. English actor Daniel Radcliffe admitted in 2008 that he suffers from this disorder, but his illness is mild, and the biggest difficulty for him is to tie his shoelaces.
Causes of dyspraxia
The causes of dyspraxia are not completely known, but recent neurophysiological studies indicate that the disease may be caused by the underdevelopment or immaturity of brain neurons, rather than their damage. A special role in the development of this disease is played by hypoxic-ischemic brain damage in the perinatal period. nine0003
Violation of praxis (the ability to perform purposeful movements) can only be diagnosed after the seventh year of life, when it can be distinguished from disorders of coordination and movement disorders.
The diagnosis of "dyspraxia" can only be made by a pediatrician or a pediatric neurologist, psychoneurologist.
Manifestations of the "clumsy child" syndrome:
- Delays in physical development. nine0010
- The child slowly learns to dress and eat independently.
- The child is sloppy while eating, does not use a knife or fork well
- Awkwardness in performing any purposeful action
- The child cannot or does not jump well, does not ride a bicycle well, often falls on level ground and stumbles when walking.
- The child does not play ball well.
- There are difficulties in writing and drawing. nine0010
- Various psycho-emotional and behavioral complexes.
- Unstable and sluggish posture.
Children with this diagnosis experience certain difficulties in social relationships, often peers refuse to contact them. It is not easy for an "inept" child to match healthy children in everyday life. Such children are characterized by increased fatigue, because the energy costs for performing ordinary daily tasks are much higher for them than for healthy peers. nine0003
Treatment of dyspraxia
Treatment of dyspraxia should be comprehensive. Depending on the type and severity of the disease, neurologists, psychologists and speech therapists should be involved in the treatment.
Tips for parents:
- Encourage the child and help him acquire special skills.
- Praise the child for any attempt to perform the action, not paying attention to the result. nine0010
- Be sure to follow the daily routine.
- Set clear and understandable goals for your child.
- It is better to start with those activities that the child himself likes.
- Be patient with your child.
Games for the development of coordination abilities in children with dyspraxia:
"To the touch".
(develops fine motor skills of hands, touch, tactile sensitivity). nine0003
Up to 10 small items are put into an opaque fabric bag, having previously shown them to the child: a pen, a bottle cap, a notepad, a remote control, etc. The child identifies the items in the bag by touch.
"Lock".
(develops motor skills of small muscles of the hand, oral coherent speech, memory and imagination).
While pronouncing the text: “There is a lock on the door.
Who could open it? nine0067 Pulled, twisted,
They knocked and opened!”,
there are rhythmic quick connections of the fingers into the lock, then the handles stretch in different directions, the hands with clasped fingers move away from themselves - towards themselves, the bases of the palms tap against each other, the fingers disengage, the palms spread apart. Repeated several times.
Whose horse is faster?
(develops coordination and speed of movements of large and small muscle groups, forms the correct posture, trains attention, improves vision and hearing, coordinates the movements of the trunk and limbs). nine0003
Sticks 20 cm long, shoelaces or pieces of rope, toys or any other toys are needed.
Children sit on chairs and hold sticks in their hands, to which toys (or other toys) are tied by laces at a distance of 15-20 steps. On a signal, the children begin to wind the string around the stick, bringing the toy closer to them.
"Catch the ball."
(develops attention, memory, ball game skills are acquired). nine0003
The players stand in a circle. The driver in the center throws the ball up and calls the name of the player. The named player must catch the ball. If the ball is not caught, the player changes place with the driver. The winner is the one who was the least leading.
The diagnosis of "dyspraxia" can only be made by a pediatrician or a pediatric neurologist, psychoneurologist. Make an appointment by calling the unified contact center in Moscow +7 (495) 775 75 66, use the online appointment service for a doctor or contact the clinic reception.