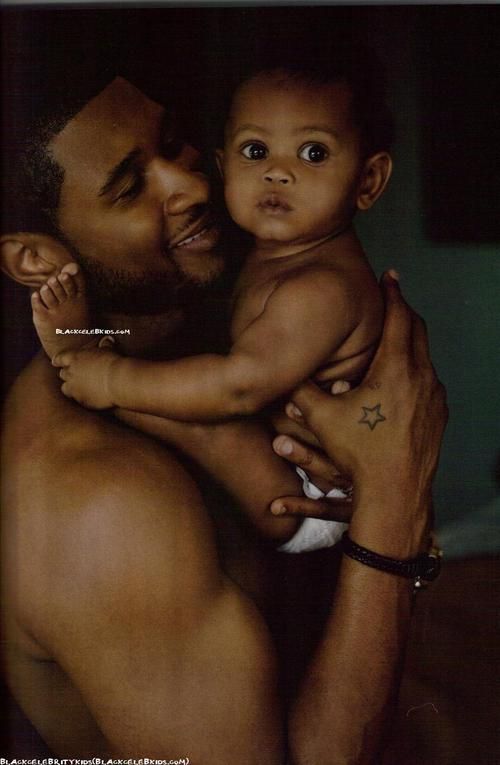
My baby is hot
Signs, Prevention, and Next Steps
From family picnics to vacations to pool parties, summer is full of fun. It can also get pretty hot and sticky depending on where you live, so you might worry about keeping your baby cool as the temperatures climb.
Overheating doesn’t just make your little one uncomfortable. During sleep it can also increase their risk of sudden infant death syndrome (SIDS) and other concerns, like heat rash.
Here’s how to spot overheating in your baby, plus tips to keep cool in summer (and winter) and signs that should prompt you to visit your child’s pediatrician.
Use your senses when evaluating whether your baby is overheating. Touch their skin and look for redness in their face as well as signs of discomfort or distress.
Keep in mind that some signs of overheating overlap with symptoms of fever or dehydration in your baby. Since young infants may not sweat much in general, your little one may be overheated from their environment without appearing to sweat.
To help you figure out whether baby is overheating, pay attention to whether your little one:
- feels hot (with or without a fever).
- looks flushed or red
- is sweating or has damp hair (though keep in mind that babies can be overheated without sweating)
- acts fussy or restless
- has an elevated heart rate (tachycardia)
- seems overly tired, sluggish, or listless
- appears confused, weak, or dizzy
- feels nauseous or is vomiting
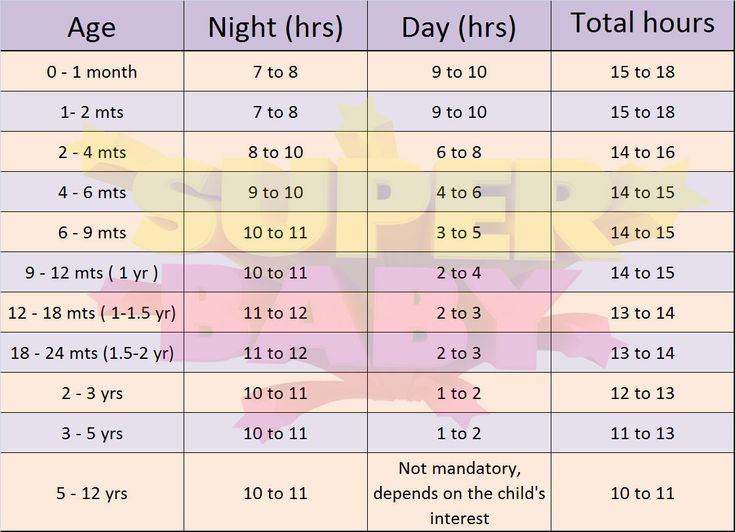
A standard temperature reading for babies is around 97.5°F (36.4°C). Your baby’s temperature can vary depending on:
- the time of the day
- what they’re wearing
- how you take their temperature (in the rectum versus on the forehead)
Unlike adults, babies have trouble regulating their body temperature. So, a reading of 100.4°F (38°C) or above is considered a fever and is particularly concerning in babies under 3 months old.
Keep in mind that overheating and a fever are two different things, though both cause an increase in body temperature.
Ideally, you’ll want to keep your baby’s room temperature to between 68 and 72°F (20 and 22°C) and no higher than 75°F (23.8°C). This temperature range is appropriate in both winter and summer.
When dressing your baby, consider how you might dress yourself to be comfortable while sleeping. Too many layers, even in the winter, can lead to baby overheating in their sleep.
Your house thermostat may not give an accurate reading for the room your child sleeps in, so you might consider using a baby monitor that measures room temperature.
In hot weather
Of course, it can be difficult to maintain ideal temperatures during a heat wave or when you’re outdoors during the summer months. Here are some ways you can keep baby cool:
- Lower your baby’s room temperature to below 75°F (23.8°C). If you don’t have air conditioning, you may use a fan — but don’t point it directly on your baby at full blast. Instead, use an oscillating (moving back-and-forth) feature or point it so it circulates air around the room.

- Keep your baby out of direct sunlight, especially at the peak hours of the day, which are 11 a.m. to 5 p.m. The same applies to sun exposure under windows, which may make the heat more intense.
- If you can’t get the room cool enough, try temporarily moving your baby’s sleep space to a cooler spot in the house. Otherwise, close any curtains to keep out as much heat as possible and dress your baby in fewer layers.
- Consider taking breaks from your home during heat waves if you don’t have air conditioning. You can visit stores, the library, or cooling centers set up by your community if you need a break from the heat.
- Don’t leave your baby inside your vehicle unattended. Even on mild days, heat builds quickly inside cars and can lead to concerns beyond overheating, including heat stroke and even death.
In cold weather
Even well-meaning parents may bundle their babies too much in cold weather. Overheating from too many blankets or clothes in the winter months is one of the leading risk factors for SIDS, according to 2017 research.
Here are a few tips:
- Dress your baby as you would dress yourself for the temperature of the room. At most, add only one more layer or a blanket or swaddle to keep your baby warm.
- The same goes with traveling in the car. Resist bundling your baby with too many blankets, especially when you have the car’s heat running. You should also remove your baby’s jacket before putting them in a car seat. Riding in a car seat in a winter coat can make the car seat less effective if you’re in an accident.
- Ditch the extra blankets and comforters inside the crib. They may contribute to overheating and pose suffocation risks.
- Don’t bump the heat up any higher than 72°F (22°C).
- Avoid having your baby sleep too close to heating vents, portable heaters, or fireplaces.
You can take some steps to help cool down your baby at home, including:
- Move your baby to a cooler space in your home.
- Remove excess layers of clothing and replace with loose-fitting, dry clothing.
- Give your baby a tepid or lukewarm bath, or place a cool washcloth on their skin.
- Breastfeed or give baby extra formula feeds for hydration.
Just be sure to monitor your child’s temperature and watch for other signs of more serious heat-related illness that may warrant medical attention.
Babies who become overheated may risk other health concerns that need prompt attention. At very least, overheating may make your child lose sleep because they’re uncomfortable.
Other risks include:
- Heat rash. Also called prickly heat, this rash is especially common in babies who are overheated. It looks like tiny red bumps in your baby’s skin folds, around the neck, and on their bottom.
- Heat exhaustion or heat stroke. Your baby may sweat heavily, have a rapid or weak pulse, or have very hot or cold, clammy skin. Heat exhaustion and heat stroke are true emergencies. If your child is vomiting or passes out, call 911 right away.
- Dehydration. When your child’s body temperature is elevated, they may sweat excessively and lose fluids and electrolytes, leading to dehydration. Symptoms include lack of tears, decrease in wet diapers, and lethargy.
- SIDS. Along with placing your infant on their back to sleep, you should also pay attention to how you dress them for naps and nighttime rest. Too many layers of clothing, swaddles, or blankets may raise your baby’s body temperature and put them at risk of infant sleep death.
It can be hard to tell if your baby is overheating or has a fever. When in doubt, call your pediatrician. It’s better to play it safe.
If your child is under 3 months old and has a rectal temperature above 100.4°F (38°C), you should call your baby’s doctor or go to the emergency room as soon as possible. While your little one may be overheated, there are other concerns your doctor may want to screen for, including infection.
Also call your doctor if baby:
- is lethargic or difficult to wake
- is very fussy or irritable
- is vomiting or not eating or drinking as usual
- is inconsolable or won’t stop crying
- has a seizure or is not acting like themself
- has a temperature that won’t go down with measures taken at home
Seek emergency medical help
You should also get medical help immediately if overheating was caused by being left in a hot car or some other overly hot environment.
Bottom line: Call your pediatrician if you have concerns, no matter how small they may seem.
Babies cannot regulate their body temperature as efficiently as older kids and adults.
So, it’s important to pay attention to your little one’s environment and other factors, like how they’re dressed, to ensure comfort and safety.
If you have any other questions about safe sleep or signs of overheating, don’t hesitate to contact your baby’s doctor.
Is Your Baby Overheating? Signs Your Baby Is Too Hot – Happiest Baby
By Dr. Harvey Karp, MD, FAAP
On This Page
- Why Babies Overheat Easily
- Normal Infant Temperature
- Signs of Overheating
- Ideal Room Temperature
- How to Prevent Overheating During Sleep
- How to Prevent Overheating in the Winter
- How to Prevent Overheating in The Summer
- How to Cool Down an Overheated Baby
- Overheating & Heat Rash
- Overheating vs.
 Fever
Fever - Final Thoughts on Overheating
You never want your little one to be too hot! If your baby’s overheating, they're likely uncomfortable, their sleep may suffer, and they may get heat rash. But there’s an even more serious concern: Overheating can raise the risk of infant sleep death, also called SIDS.
Studies have shown that thick clothing, too many layers, and high room temperatures increase the risk of SIDS. While it may seem counterintuitive, infants are at higher risk of SIDS during the winter months. That’s because parents worry their baby may get cold and they try to prevent that by overdressing them or cranking up the heat.
Why Babies Overheat EasilyInfants are not great at regulating their core temperature. For one, their body temperature rises much faster than yours. Plus, babies and children sweat less, which greatly reduces their ability to cool down. And it’s not just that babies are more prone to overheating, they’re more likely to be affected by a heat-related illness, too. For instance, because babies’ sweat glands aren’t yet fully developed, they’re more likely to get heat rash or prickly heat.
And it’s not just that babies are more prone to overheating, they’re more likely to be affected by a heat-related illness, too. For instance, because babies’ sweat glands aren’t yet fully developed, they’re more likely to get heat rash or prickly heat.
A normal temperature in babies is around 97.5 degrees Fahrenheit (36.4 degrees Celsius). Overheating and fevers in babies are around 100.4 degrees Fahrenheit (38 degrees Celsius) or above. Keep in mind that normal baby body temperatures can vary in your baby throughout the day.
Luckily, there’s an easy way to tell if your baby is too hot. Touch their ears and neck. If their ears are red and hot—and their neck is sweaty—your baby is too warm. Dress them more lightly or cool the room.
Is your baby overheating? How to check...
Below you’ll find a few signs and symptoms of a baby overheating:
- Warm to the touch
- Red skin
- Rapid heartbeat
- Fever without sweating
- Lethargic or unresponsive
- Vomiting
- Dizzy or confused
No matter the season, keep the room your baby is in between 68 to 72 degrees Fahrenheit (20 to 22..jpg) 2 degrees Celsius). While you can measure the room temperature with a thermometer, in general, the temperature should not be too cool or too warm for an adult.
2 degrees Celsius). While you can measure the room temperature with a thermometer, in general, the temperature should not be too cool or too warm for an adult.
How to Prevent Overheating During Sleep
In addition to setting the thermostat to the ideal sleeping temperature, avoid over-bundling your little bundle for naps or at bedtime with extra layers of clothing or hats. Here are some pointers on dressing your little one for sleep:
-
DON’T use a hat for sleep. Hats are especially problematic because covering their head reduces your baby’s ability to use their head as a little radiator, giving off extra heat. Also, in the middle of the night, a hat might accidentally slip over your little one’s face and cause breathing difficulties.
-
DO wrap Baby in a lightweight swaddle. In hot weather, it’s fine to let your baby sleep in just a short-sleeve bodysuit and light muslin swaddle. (My Sleepea 5-Second Swaddle is made from organic cotton and features breathable mesh at shoulders and legs to keep babies cool and comfy.
 ) In cooler weather, opt for a long-sleeve bodysuit or footie pajamas and a swaddle. (For babies who are rolling, swap the swaddle for a lightweight sleep sack.)
) In cooler weather, opt for a long-sleeve bodysuit or footie pajamas and a swaddle. (For babies who are rolling, swap the swaddle for a lightweight sleep sack.) -
DON’T use loose blankets. Never use loose blankets, which are an overheating risk and a suffocation risk. (A safe crib is a crib free of toys, blankets, and all objects except a pacifier.)
-
DON’T use electric blankets (or heating pads) with your baby. These overheat infants and expose them to electromagnetic radiation.
-
DO place Baby’s bassinet away from the heater. Keep your little one a good distance away from heating vents, radiators, portable heaters, and fireplaces to avoid overheating.
Bundling babies for cold-weather adventures—plus cranking the indoor heat—can easily increase their risk of overheating. Not only are babies terrible at regulating their body temperature, they lack enough body fat to keep themselves insulated and snug. Plus, newborns have yet to develop the shiver reflex, which works to increase body heat in the cold. Here are common-sense steps to avoid your baby overheating in the winter:
Plus, newborns have yet to develop the shiver reflex, which works to increase body heat in the cold. Here are common-sense steps to avoid your baby overheating in the winter:
-
DO dress Baby in layers. Dress your little one in one more layer than you’re wearing. If your bub gets too warm, simply peel off a layer. For outdoors, start with a long-sleeve cotton bodysuit, then add soft pants, socks, and a sweater. If you’ve got a jacket on, your baby should have a jacket or snowsuit on, too—plus a blanket. Finally, don’t forget a hat, mittens, and warm booties to keep their head, hands, and feet warm
-
DON’T dress your baby in a sweater when using a baby carrier. If you’re wearing a baby carrier, your baby likely doesn’t need a sweater or sweatshirt under their jacket. That’s because your body heat will provide just enough extra warmth to keep your little one toasty, without overheating. (Make sure your little one’s face isn’t pressed against your chest or clothing!)
-
DO use a blanket instead of a coat in the car.
 Bulky coats and snowsuits should not be worn in the car seat. They leave too much space under the harness, endangering your baby in the event of a car accident. Instead, secure your little one into their car seat jacket-free, then place a blanket on the lower part of their body. Once the car warms up, remove the blanket.
Bulky coats and snowsuits should not be worn in the car seat. They leave too much space under the harness, endangering your baby in the event of a car accident. Instead, secure your little one into their car seat jacket-free, then place a blanket on the lower part of their body. Once the car warms up, remove the blanket.
It’s no surprise that high outdoor temperatures put babies and children at an elevated risk for becoming overheated. Here are some easy to-dos to keep your little one from overheating in the summer:
-
DON’T go out during peak heat. The day is always at its hottest between around 10am and 2pm. Try to avoid extended outside time during those hours when the temperature is high. And spend time in the shade otherwise!
-
DO seek air conditioning. If you don’t have air conditioning at home and you’re experiencing extreme heat, find a nearby building that has AC, like the library or shopping mall.
 And if you do have AC, never put your baby to sleep next to the unit or they’ll get too cold.
And if you do have AC, never put your baby to sleep next to the unit or they’ll get too cold. -
DON’T cover the stroller. Draping your baby’s stroller with a muslin blanket may shield your bub from the sun, but it traps heat, increasing the temperature of the stroller…and your baby. Instead, use a large canopy or mesh sun shield specially designed for strollers that provide shade and adequate airflow.
-
DO keep hydrated. Babies get all their hydration needs from either breastmilk or formula, so on steamy days, offer more of the same. But you should not give your baby water in the first 6 months of life. From 6 to 12 months, however, 4 to 8 ounces a day is okay.
How to Cool Down an Overheated Baby
If you believe your baby is overheating, then here are some steps that you can try to cool down your little one:
-
Offer your baby fluids. If younger than 6 months, offer breastmilk or formula only.
 If between 6 months and 1 year, offer 4 to 8 ounces of water a day.
If between 6 months and 1 year, offer 4 to 8 ounces of water a day. -
Take your baby to a cooler room. Know that lower floors—and shaded rooms—will be cooler.
-
Dress your baby in light clothing. Cotton and breathable loose-fitting fabrics are ideal.
-
Sponge your baby in lukewarm/cooler water. Don’t use cold water or ice in the bath.
-
Apply a cold compress. Hold it to your baby’s forehead or limbs to help cool them down.
If symptoms do not improve, contact your pediatrician.
Baby Overheating & Heat RashBabies develop heat rash (aka prickly heat) when their salty sweat gets trapped and irritates the skin. It most commonly appears on your baby’s neck, armpits, chest, back, elbows, or thighs. The rash presents as little red dots (irritated hair follicles) and splotchy skin and can be accompanied by fever, chills, and bumps. In most cases, heat rash generally fades on its own within two to three days. But if you think your child has a heat rash, give your doctor a call anyway. They may recommend you sprinkle on a dusting of cornstarch powder—never talcum—to absorb excess sweat and prevent irritation. Applying a cool compress to the heat rash and giving your bub cool baths can help, too.
In most cases, heat rash generally fades on its own within two to three days. But if you think your child has a heat rash, give your doctor a call anyway. They may recommend you sprinkle on a dusting of cornstarch powder—never talcum—to absorb excess sweat and prevent irritation. Applying a cool compress to the heat rash and giving your bub cool baths can help, too.
It’s natural to think that your overheated baby may have a fever. To be sure, take your baby’s temperature and consult your healthcare provider if you have any concern. (For the most accurate temperature reading in babies and toddlers up to 3 years old, use a rectal thermometer.) Additionally, the symptoms below indicate that your baby may have a fever:
- Difficulty sleeping
- Lack of eating
- No interest in playtime
- Lethargic or not as active as usual
Any baby under 3 months with a rectal temperature of 100. 4 degrees Fahrenheit or higher, must be checked by a doctor. And any child with a fever over 104 degrees Fahrenheit needs to be evaluated. So, if you see those numbers, don’t hesitate to give your pediatrician a call!
4 degrees Fahrenheit or higher, must be checked by a doctor. And any child with a fever over 104 degrees Fahrenheit needs to be evaluated. So, if you see those numbers, don’t hesitate to give your pediatrician a call!
The thing to keep in mind is that babies cannot regulate their body temperature well, so you always want to avoid extremes in temperature, whether that’s hot or cold. If you’re ever not sure if your baby is too hot, do the “ear check” to be safe!
More on Baby Safety:
- 6 Winter Care Tips for Newborns
- Flu Shot Need-to-Know
- Dr. Harvey Karp’s Natural Cold Remedies for Babies
- Summer Safety Tips for Babies and Kids
- Smart Sunscreen Advice for Babies and Big Kids
About Dr. Harvey Karp
Dr. Harvey Karp, one of America’s most trusted pediatricians, is the founder of Happiest Baby and the inventor of the groundbreaking SNOO Smart Sleeper. After years of treating patients in Los Angeles, Dr. Karp vaulted to global prominence with the release of the bestselling Happiest Baby on the Block and Happiest Toddler on the Block. His celebrated books and videos have since become standard pediatric practice, translated into more than 20 languages and have helped millions of parents. Dr. Karp’s landmark methods, including the 5 S’s for soothing babies, guide parents to understand and nurture their children and relieve stressful issues, like new-parent exhaustion, infant crying, and toddler tantrums.
After years of treating patients in Los Angeles, Dr. Karp vaulted to global prominence with the release of the bestselling Happiest Baby on the Block and Happiest Toddler on the Block. His celebrated books and videos have since become standard pediatric practice, translated into more than 20 languages and have helped millions of parents. Dr. Karp’s landmark methods, including the 5 S’s for soothing babies, guide parents to understand and nurture their children and relieve stressful issues, like new-parent exhaustion, infant crying, and toddler tantrums.
View more posts tagged, health & safety
Have questions about a Happiest Baby product? Our consultants would be happy to help! Connect with us at [email protected].
Disclaimer: The information on our site is NOT medical advice for any specific person or condition. It is only meant as general information. If you have any medical questions and concerns about your child or yourself, please contact your health provider.
If you have any medical questions and concerns about your child or yourself, please contact your health provider.
What to do if a child has a temperature
October 31, 2017LikbezZdorovye
We answer the main questions about children's fever: when a high temperature becomes dangerous, what medicines to buy in a pharmacy and whether it is worth listening to the advice of grandmothers.
Share
0What is considered a high temperature
To begin with, let's figure out that each of us has a temperature and normally it is not necessarily 36.6 °C. This is the "hospital average" value, because in a healthy person it can range from 36.1 to 37.2 ° C and even change during the day. For example, rise after eating or heavy loads.
When we say “Child has a fever”, we mean fever – a condition in which the body temperature is elevated, that is, the thermometer under the arm shows more than 37.2 °C.
If you put a thermometer rectally (into the rectum) or measure the temperature in the ear, the values are usually higher. Then the fever is more than 38 ° C. When measured orally (in the mouth), it is above 37.8 °C.
Then the fever is more than 38 ° C. When measured orally (in the mouth), it is above 37.8 °C.
How to measure the temperature correctly →
Why the temperature rises
Fever is a protective reaction of the body, usually against various infections. At high temperatures, it is more difficult for bacteria and viruses to survive, so the body starts a process that destroys dangerous microorganisms, and at the same time activates the immune system.
The temperature in children rises more often due to respiratory viral infections, what we call the common cold. But this is not necessary: fever is manifested in many other diseases. In addition to infections, injuries, overheating, oncological, hormonal and autoimmune diseases, and even some drugs that have such side effects can be to blame for the temperature.
How to understand that a child has a temperature
Adults notice a high temperature by special symptoms:
- Weakness.
- Headache.

- Feeling chilly and trembling.
- Loss of appetite.
- Muscle pain.
- Sweating.
Children who can already talk may complain of discomfort. But the temperature rises in infants who do not know how to describe their condition.
The reason for taking the temperature is unusual behavior of the child:
- Refusal to eat or breastfeed.
- Tearfulness, irritability.
- Drowsiness, fatigue, passivity.
One cannot speak of a fever based on a kiss on the forehead. Only the thermometer shows high temperature.
When and why to reduce the temperature
An elevated temperature is a sign of the correct immune response when it comes to infections. Therefore, it should not be reduced so as not to delay recovery. It usually makes sense to give antipyretics after the temperature has risen to 39°C is a rectal measurement. When the temperature is checked under the arm, doctors recommend lowering it after 38. 5 ° C, but not before. Don't worry, the fever itself isn't that bad.
5 ° C, but not before. Don't worry, the fever itself isn't that bad.
Many people are afraid that high temperatures will damage brain cells. But according to the WHO, it is safe for children until it reaches 42°C.
Fever is not an independent disease, but only its symptom. When the temperature is reduced with drugs, the external manifestations of the disease are removed, but they do not cure it.
In rare cases, too high a temperature in children leads to febrile convulsions - involuntary muscle contractions. It looks creepy and brings parents to fainting, but basically the attacks stop by themselves and have no consequences. Call the doctors and make sure that the child does not injure himself: put him on his side, hold him, open tight clothes. Do not put anything in your mouth, it only increases the risk of injury.
But everyone endures a fever differently: someone even at 39°C on the thermometer can read and play, someone lies at 37. 5 °C and cannot move. Therefore, it is necessary to reduce the temperature for the sake of convenience and improve the well-being of the child.
5 °C and cannot move. Therefore, it is necessary to reduce the temperature for the sake of convenience and improve the well-being of the child.
If the child feels normal, then nothing needs to be done about the high temperature.
How to reduce fever
The easiest, fastest and most effective way is to give your child an antipyretic based on ibuprofen or paracetamol. They are produced in forms that are convenient for children to use: sweet syrups or candles. Be careful if you give your child syrup: flavors and dyes can cause allergies.
Never exceed the dosage of the medicine. It is usually calculated based on the weight of the child. Children, especially preschoolers, can vary greatly in weight even at the same age, so focus on the number of kilograms, not years.
Remember that drugs take time to work: from 0.5 to 1.5 hours. So do not rush to measure the temperature 10 minutes after taking the pill.
Use the measuring cups, spoons and syringes that come with your medicine. Do not collect medicine in the dark or in a teaspoon by eye: you always need to know how much and what medicines you gave your child.
Do not collect medicine in the dark or in a teaspoon by eye: you always need to know how much and what medicines you gave your child.
To avoid overdosing, do not give babies combination medicines for cold symptoms. They already have paracetamol or another antipyretic in them, so it's easy not to notice that you overdose if you give several drugs at the same time.
Paracetamol and ibuprofen can be taken on the same day, but don't get carried away and don't give your child all at once. If, for example, you gave paracetamol and it didn't help much, then when it's time for a new dose of antipyretic, give ibuprofen (or vice versa).
Do not give aspirin and analgin: they can cause serious side effects in children.
There are also physical methods, though ineffective: wipe the child's hands and feet with a damp towel, put a cool compress on the forehead. Just do not take ice for this, it is enough to soak the towel with water at room temperature.
When to call a doctor
Experienced parents know that mild SARS can be dealt with on their own, at home. In such cases, a doctor is needed only to write out a certificate or sick leave for parents. But still, you need to see a pediatrician if:
- You need a doctor's advice, calm down. Or you just think that the child needs medical help.
- A child with fever is less than three months old.
- The child is less than six months old and has a temperature above 38 °C for more than 1 day.
- The child is less than a year old and has a temperature above 39°C for more than 1 day.
- The child developed a rash.
- Along with fever there are severe symptoms: uncontrollable cough, vomiting, severe pain, photophobia.
When to call an ambulance
Urgently seek help if:
- The temperature has reached high values (more than 39 °C) and continues to rise after taking antipyretics.
- The child has a confused mind: he is too sleepy, he cannot be woken up, he does not react well to the environment.

- Difficulty with breathing or swallowing.
- Vomiting added to the temperature.
- A rash has appeared in the form of small bruises that does not disappear when the skin is pressed.
- Convulsions started.
- There are signs of dehydration: the child rarely goes to the toilet, he has a dry mouth with a red tongue, he cries without tears. In infants, the fontanel may sink.
How to help a child with a fever
The main way we can help in the fight against fever is to eliminate its cause. If it's a bacterial infection, antibiotics are needed (only as prescribed by a doctor). If other diseases are to blame, they must be treated. And only viruses pass by themselves, you just need to support the body, which will destroy these viruses.
Give warm drinks
At high temperatures, the moisture that is in the human body evaporates faster, so there is a risk of dehydration. This is especially true for children: they are small and they need very little to lose 10% of the liquid. With a lack of water, the mucous membranes dry up, it becomes more difficult to breathe, the child has nothing to sweat with, that is, he cannot dump heat on his own. Therefore, a warm drink at a temperature is very, very important.
With a lack of water, the mucous membranes dry up, it becomes more difficult to breathe, the child has nothing to sweat with, that is, he cannot dump heat on his own. Therefore, a warm drink at a temperature is very, very important.
Give your child juices, compotes, tea, water more often, persuade him to drink at least a few sips. Babies need to be offered breasts more often, but if the baby refuses, it is better to give him water or a special drink than to wait until he returns to breast milk.
Buy a humidifier
In order not to increase the loss of fluid with breathing (and we exhale steam, in which there is a lot of moisture from the mucous membranes), humidify the air in the room. To keep the relative humidity at 40-60%, it is best to buy a special humidifier. But you can try other methods as well.
Clean up
Every day, wet the room: mop the floors and collect dust. This is again necessary to facilitate breathing. Do not be afraid to open the windows and ventilate. Fresh air is especially necessary for a person whose body is fighting a disease, because ventilation is one of the ways to disinfect a room. From an open window it will not get worse, but from hot, dry and full of microbes air it will.
Fresh air is especially necessary for a person whose body is fighting a disease, because ventilation is one of the ways to disinfect a room. From an open window it will not get worse, but from hot, dry and full of microbes air it will.
By the way, you can bathe your child if they have a fever.
Of course, when the baby wants to sleep and lie down, you don't have to drag him to the bathroom. But if the general condition is normal, the child moves and plays, you can wash.
Keep a diet
Feed your child healthy: do not give kilos of sweets just because he is sick. If the baby does not have an appetite, do not force him to eat. Lunch eaten through force will not help to cope with the infection. It is better to boil chicken broth and give it to your child: it is liquid, food, and help in the fight against inflammation.
What not to do when a child has a temperature
The best way to survive an unpleasant period of illness without problems and losses is to provide a child with good care. For some reason (according to tradition, on the advice of grandmothers, on advice from the forums), many harmful actions are considered mandatory in the treatment of temperature. How not to make mistakes:
For some reason (according to tradition, on the advice of grandmothers, on advice from the forums), many harmful actions are considered mandatory in the treatment of temperature. How not to make mistakes:
- Do not wrap your child . If the temperature is high, then warm clothes and two blankets will only aggravate the process. It is better to persuade him to drink another cup of warm compote.
- Do not place the heater near the child. In general, if the temperature in the room is above 22 ° C, it is necessary to reduce it. For a child with a fever, it will be better if the room is 18-20 ° C: inhalation of such air will not dry out the mucous membranes.
- Don't steam your feet, don't make you breathe over a pot of something hot, don't put mustard plasters : these procedures have no proven effectiveness, and the risk of burning and overheating is greater than any possible benefit. In addition, these are unpleasant activities, and the child is already bad.
 If you really want to help the baby, it is better to figure out how to entertain him when he is having a hard time.
If you really want to help the baby, it is better to figure out how to entertain him when he is having a hard time. - Do not rub your child with vinegar and vodka . These methods help little, but they are very toxic to children.
- Do not put your child to bed if he does not want to go there . The patient himself prescribes bed rest. If he has the strength to play, then it's good.
What to do if you have a fever after vaccination
Some vaccines cause temporary reactions in the body - redness at the injection site, irritability, a slight increase in temperature. These are not complications, everything will pass by itself in 1-3 days.
You can eliminate unpleasant symptoms in the same way as in the case of any other temperature: antipyretics and a suitable regimen.
The usual temperature after vaccination is not higher than 37.5 °C. But if the fever rises, see a doctor.
Read also:
- Why a child needs to be vaccinated →
- Measles: why they are so afraid of it and is it better to get sick →
- 10 amazing discoveries that I made after the birth of a child →
- For which symptoms of pneumonia call a doctor and for which an ambulance →
Payment for food and information about the child's attendance at school, kindergarten or college.
 Moscow State Services
Moscow State Services Conditions for obtaining services on the website
The service allows you to get information about when a child is at school, kindergarten or college, how they eat in the school cafeteria and canteen, as well as plan an order for a child's hot meals, replenish his personal account and control his expenses and purchases in the canteen.-
Who can apply for the service
Parents (legal guardians) whose children attend school, college or kindergarten.
Proxies added by the parent (legal guardian) to the number of representatives of the child.
Data of legal representatives of children (full name and mobile phone number) must be previously entered into the information system "Access and Meals" at school, college or kindergarten when connecting the information service.
-
Service cost and payment procedure
The service is provided free of charge.
 Connection to it occurs automatically when the following conditions are met:
Connection to it occurs automatically when the following conditions are met: 1. Registration by a legal representative (principal) at a school, college, kindergarten Application for information connection.
2. Availability of a personal account on mos.ru.
3. The phone number indicated in the application for informing connection coincides with the phone number recorded in the personal account.
Other authorized persons will gain access to the service if: a) the principal issues an electronic power of attorney on the mos.ru portal and b) the authorized person has a personal account on the mos.ru portal. -
Terms of service provision
Constantly throughout the school year
-
The result of the service
After linking the child's personal account to your personal account on the mos.ru portal, you will have access to the "Attendance and meals" page of the "View information about attendance and meals at school, kindergarten, college" service, where you can view the information:
1.
 About all the facts of your child's passage to school, college.
About all the facts of your child's passage to school, college.
2. Who and when from the legal representatives of the child brought to the kindergarten and took him away from the kindergarten.
3. About a set of free food rations at school (if he has this benefit).
4. On the composition of hot meal rations in the school canteen and buffet products for a fee
5. About the history of operations on the personal account of the child and the current balance of funds.
In addition, you can set up a set of events and reports that are convenient for you, for which you would like to receive notifications (on a visit, on a child’s purchases, on replenishment of a personal account, reports on events for a day, a week), as well as ways to receive them: push and/or email.You can also use the range of services provided:
1. Top up the child's personal account for non-cash payment for meals at school.
2. Set the auto payment amount from the parent's bank card to the child's personal account.