Miscarriage four weeks
4 Weeks Pregnant: Symptoms, Tips, and More
4 Weeks Pregnant: Symptoms, Tips, and MoreMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Ashley Marcin on October 18, 2017
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Overview
By the time you’re 4 weeks pregnant, you can usually get a clear positive on a urine pregnancy test.
It’s a funny thing, but your egg may have only been fertilized in the last two weeks. Still, the dating for pregnancy begins with the start of your last menstrual period.
By entering this date into a due date calculator, you can estimate the day your little one might enter the world. Try this pregnancy quiz to learn more.
Changes in your body
Your baby has just implanted into your uterine lining. Your body is now beginning the incredible series of changes that will take place over the next 36 weeks, give or take a few.
One of the earliest physical signs you’ll experience is a missed period. This indicates that your progesterone levels are taking over your hormonal balance to sustain your pregnancy.
As your baby develops, your body will produce more and more human chorionic gonadotropin (hCG) as well. This hormone is present in your blood as soon as 7 to 11 days after conception. It comes from the cells that eventually turn into the placenta.
At 4 weeks, normal levels should range between 5 and 426 mIU/mL.
Your baby
Share on Pinterest
Your baby is currently a collection of cells called a blastocyst. Development this week is rapid. Around half of these cells will become an embryo the size of a poppy seed by the week’s end. The other half of the cells work to keep your baby safe and nourish its growth.
The size may sound impossibly small, but what’s even wilder is that many of your child’s characteristics, such as eye color, hair color, sex, and more, have already been determined through its chromosomes.
Twin development at week 4
Your first trimester symptoms may be amplified if you’re carrying twins. After all, you have two bundles of joy, so you’re more likely to have higher hormone levels. You may even suspect you’re pregnant sooner than if you were carrying one baby. You can take a pregnancy test this week to find out, but you won’t know the number of babies until your first doctor’s appointment, which is usually around week 8. Your first appointment might happen sooner if you had fertility treatment.
If you’ve had fertility treatments for pregnancy, you may also have your human chorionic gonadotropin (hCG) and progesterone levels confirmed with a blood test. There’s nothing to see on an ultrasound yet, but high hCG and progesterone levels may give you a clue that you’re carrying multiples.
4 weeks pregnant symptoms
At this early stage, you might not notice much going on with your body. In fact, some women don’t know that they’re pregnant for weeks if they aren’t keeping close track of their menstrual cycles or if their cycles tend to be irregular.
On the other hand, by week 4 of your pregnancy you may experience the following:
- breast tenderness
- exhaustion
- frequent urination
- nausea
- heightened sense of taste or smell
- food cravings or aversions
Overall, the symptoms in week 4 often mimic your normal premenstrual symptoms. So much so that many women swear their periods will start at any moment.
Here are some home remedies for common early pregnancy symptoms:
- To relieve sore breasts, wear a supportive bra during the day and to bed if it helps.
- If you feel sluggish, try taking a catnap in the afternoon. Exercise can also give you a much-needed boost of energy.
- You may want to moderate your liquid consumption if you’re finding yourself in the bathroom too often. Don’t cut back too much, though, because you need the hydration now more than ever.
- Nausea is uncommon this early, but if you do experience it, try eating small, frequent meals and avoiding foods that trigger sickness.
 Many women find relief while snacking on carbohydrates and tart foods.
Many women find relief while snacking on carbohydrates and tart foods.
Read more about the best nausea remedies for morning sickness.
Things to do this week for a healthy pregnancy
Once your pregnancy test turns positive, you’ll want to call your doctor or midwife to set up your first prenatal appointment. Don’t worry if the due date is far in the future. Most women are seen for the first time around week 8.
Depending on your healthcare provider’s protocol, you may also need to head into the office to have some preliminary blood work. This will confirm your pregnancy and check your hormone levels. One test will check your hCG. This number should double about every 48 to 72 hours. The other will check your progesterone levels.
Both tests are repeated at least once to assess the increase in numbers.
Even at week 4, it’s never too early to start healthy habits. Try eating whole foods, avoiding smoking and alcohol, and, if you aren’t already, start taking a prenatal vitamin.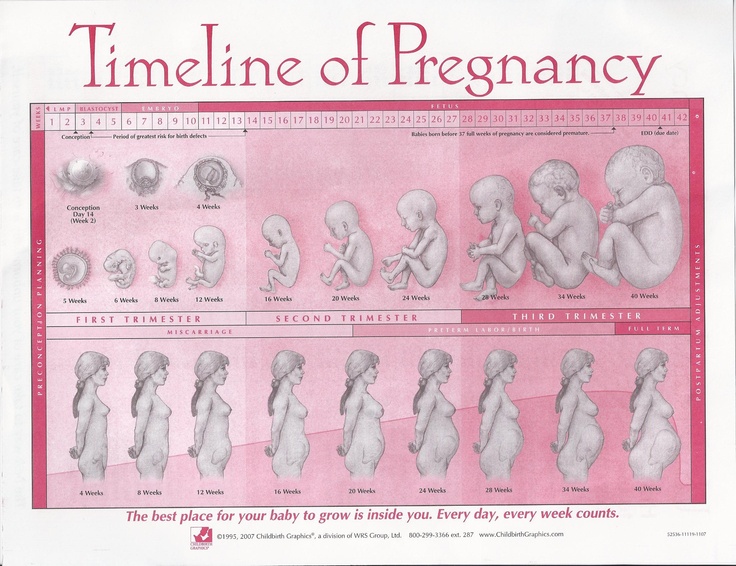
Exercise is also a great way to ease pregnancy symptoms and keep your body and baby healthy. Typically any activity you were doing before pregnancy is safe to continue in the first trimester. For vigorous exercise, you may want to speak with your doctor about certain changes that might be necessary.
Shop for prenatal vitamins.
When to call the doctor
While you shouldn’t worry, it’s important to know that miscarriage rates are high in early pregnancy. Researchers estimate that up to 20 percent of known pregnancies end in miscarriage, many of which happen around the time a woman expects her period to start.
At week 4, miscarriage is called a chemical pregnancy since the embryo cannot be detected on ultrasound, only through blood and urine testing.
Signs of miscarriage include cramping, spotting, and heavy bleeding. If you experience these symptoms, don’t necessarily fear the worst. As the blastocyst buries deeper into your lining, you may have spotting and discomfort. In other words, not all blood means miscarriage is imminent.
In other words, not all blood means miscarriage is imminent.
The best way to gauge what’s going on is to keep an eye on yourself and speak with your doctor about the symptoms you’re experiencing. If you don’t already have a provider, our Healthline FindCare tool can help you connect to physicians in your area.
The waiting game
The first weeks can seem like a difficult waiting game. It’s easy to compare notes with friends and family. Keep in mind that each pregnancy and each woman is unique. What may have worked or been a problem for someone else might not apply in your situation.
If you ever have questions or concerns during pregnancy, your first resource should be your healthcare provider. They’re used to frequent calls and even silly questions, so ask away!
Last medically reviewed on October 19, 2017
- Parenthood
- Pregnancy
- 1st Trimester
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Ashley Marcin on October 18, 2017
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Ashley Marcin on October 18, 2017
related stories
Weird Early Pregnancy Symptoms No One Tells You About
The Pregnancy Quiz: Am I Pregnant?
9 Ways to Tell Your Parents You’re Pregnant
11 Best Prenatal Vitamins for a Healthy Pregnancy, According to a Dietitian
Your First Prenatal Visit
Read this next
Weird Early Pregnancy Symptoms No One Tells You About
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
You might be surprised by certain symptoms that the first trimester of pregnancy can bring. Get the facts on 10 unusual symptoms, such as tasting…
READ MORE
The Pregnancy Quiz: Am I Pregnant?
Medically reviewed by George Krucik, MD, MBA
There are certain signs and symptoms that indicate pregnancy.
 Are you experiencing any of them?
Are you experiencing any of them?READ MORE
9 Ways to Tell Your Parents You’re Pregnant
Trying to find a cute, creative way to tell your parents you’re pregnant? Try one of these!
READ MORE
11 Best Prenatal Vitamins for a Healthy Pregnancy, According to a Dietitian
Medically reviewed by Kathy W. Warwick, R.D., CDE
Taking a daily prenatal multivitamin is essential to support a healthy pregnancy. These 11 dietitian-recommended brands are excellent options for both…
READ MORE
Your First Prenatal Visit
Medically reviewed by Fernando Mariz, MD
Learn what to expect during your first prenatal visit.
READ MORE
7 Tips for Coping with Anxiety During Pregnancy
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
Many women experience anxiety during pregnancy.
 If it starts to interfere with your daily life, here’s how to cope.
If it starts to interfere with your daily life, here’s how to cope. READ MORE
14 Recipes to Ease Morning Sickness
Medically reviewed by Natalie Butler, R.D., L.D.
Morning sickness got you down? Get over your nausea with one of these 14 delicious, easy recipes.
READ MORE
6 Questions Everyone Should Ask Themselves About Their Fertility, Right NowREAD MORE
Why We Need to Talk About Depression During Pregnancy
Perinatal depression is depression during pregnancy, and it's a very real and serious illness many women experience — often alone.
READ MORE
7 Books That Shine a Light on Pregnancy
For everything from what to eat during pregnancy to how to plan for birth and what comes after, check out these best pregnancy books!
READ MORE
Signs of Early Miscarriage | Obstetrics & Gynecology
Skip to main content
Department of Obstetrics and Gynecology
News | Careers | Giving | UC Davis Health
- UC Davis Health
- Obstetrics and Gynecology
- Miscarriage Management
- Signs of Early Miscarriage
Early miscarriage refers to loss of a pregnancy in the first trimester.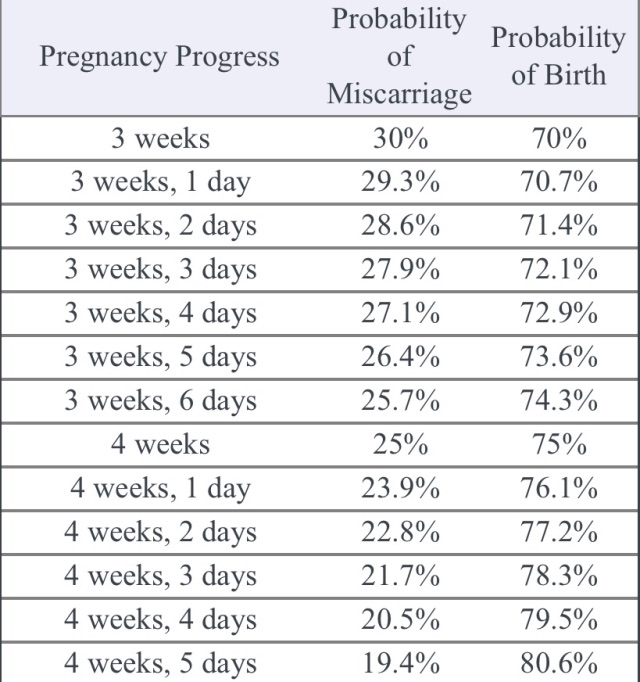 The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
Miscarriage is more common than many people realize. About 10 to 20% of women who learn they are pregnant will have an early miscarriage. The rates of early miscarriage are even higher when women are checking home pregnancy tests very close to the time of their period and are finding a positive test VERY early. By chance alone, 1% to 4% of women will have two miscarriages in a row. However, it is very rare to have 3 or more miscarriages in a row, which is recurrent miscarriage.
In medical terms, early miscarriage is called an early pregnancy failure. This means that the pregnancy failed to develop. Almost all early miscarriages are due to circumstances beyond anyone’s control, and were destined to happen before the woman even knows she is pregnant.
What are the symptoms of early miscarriage?
- Bleeding – light bleeding early in pregnancy is fairly common, and does not mean you will have a miscarriage.
- Brown discharge: This may look like coffee grounds. This “discharge” is actually old blood that has been in the uterus for a while and is just coming out slowly.
- Spotting, bright red bleeding or clots
- Passage of tissue through the vagina
- A gush of clear or pink vaginal fluid
- Abdominal pain or cramping
- Pregnancy symptoms, such as breast tenderness and nausea, begin to go away
- Dizziness, lightheadedness, or feeling faint
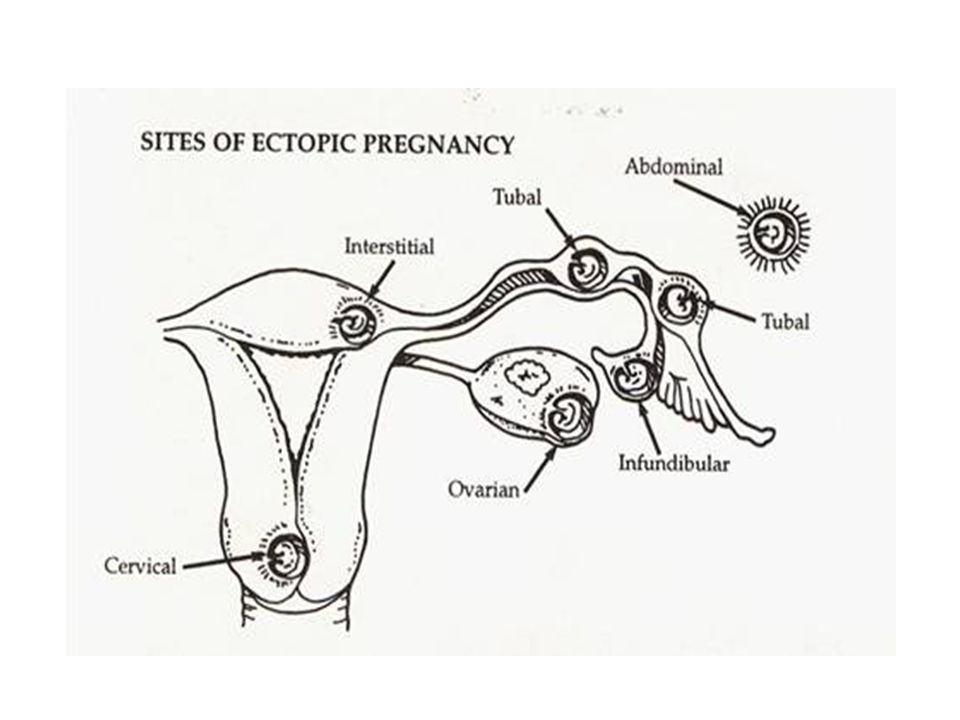
If you have any symptoms of a miscarriage, you should contact a doctor right away to have an evaluation. It will be important to have an ultrasound exam to look into the uterus to see if the pregnancy is normal or you are having a miscarriage. Even if you think you passed the entire pregnancy and are feeling better, you should see a doctor. Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Types of early miscarriage
Early miscarriage is a non-medical term for lots of different types of events that might or might not actually result in pregnancy loss. The types of miscarriage include the following:
Spotting or bleeding in the first trimester in which the patient and the doctor are not yet sure if the pregnancy will miscarry or not. About 1/3 of all women will bleed in the first trimester, but only about half of those women will have a miscarriage.
The entire pregnancy is passed from the uterus, most commonly with bleeding and cramping, and no additional treatment or observation is needed.
The pregnancy is definitely miscarrying, but only some of the pregnancy tissue has passed. The tissue that is still in the uterus will eventually pass on its own. Some women may need emergency treatment if there is also heavy vaginal bleeding. Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
With this type of miscarriage, the pregnancy implanted but the embryonic tissue (the part of the pregnancy that will develop into a fetus) never developed, or started to develop and then stopped.
With this type of miscarriage, the early embryo (or fetus once 10 weeks pregnant) stops developing and growing.
This is an uncommon type of miscarriage today. With a missed abortion, the pregnancy stops developing but the pregnancy tissue does not pass out of the uterus for at least 4 weeks. Sometimes, dark brown spotting or bleeding occurs, but there is no heavy bleeding.
Some miscarriages occur with an infection in the uterus. This is a serious condition that requires urgent treatment to prevent shock and death. With septic miscarriage, the patient usually develops fever and abdominal pain and may have bleeding and discharge with a foul odor. Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
What causes early miscarriage?
Almost nothing you can do will cause an early miscarriage. Avoiding sex or heavy work will not impact an early pregnancy. There are a lot of changes that need to occur with the cells and genes in a developing pregnancy, and sometimes those changes do not happen perfectly. There are some health conditions or habits that can increase the chance that an early miscarriage will occur, including:
- Heavy smoking
- Use of illicit drugs, especially cocaine
- Poorly controlled diabetes
- Hyperthyroidism or hypothyroidism
- Physical problems with the uterus, including fibroids or abnormalities of development of the uterus
Why see our specialists at UC Davis Health?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently. We perform our own ultrasound examination in the office and can share the results with you immediately.
We perform our own ultrasound examination in the office and can share the results with you immediately.
If we do confirm you have a miscarriage, we can discuss expectant management or treatment options with you immediately. Should you need blood testing to evaluate the pregnancy, the laboratory is in the same building as our office.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Treatment of early miscarriage
Not all miscarriages “need” treatment. The choice of whether to wait for the pregnancy to completely pass without any treatment is up to you. Our doctors are committed to providing options for all patients, including the pros and cons of all available options when miscarriage is diagnosed. All patients with Rh-negative blood, regardless of which option they choose, need treatment with Rh-immune globulin, an injection that prevents a woman from forming substances in her blood that may attack the baby during a future pregnancy.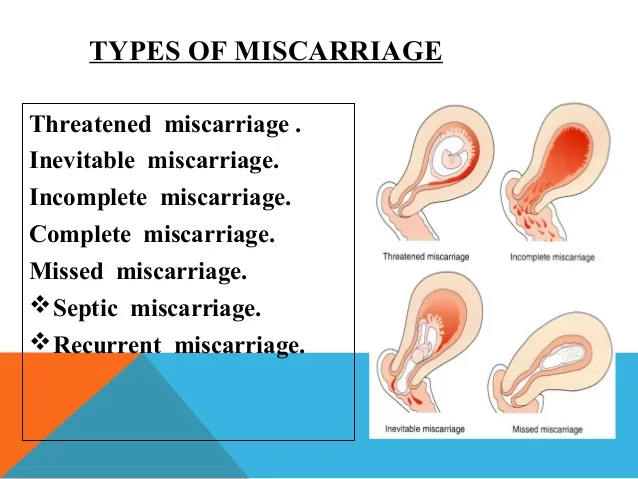
When a diagnosis of miscarriage is made, options include:
This means that you will not receive any treatment; just continued follow-up. In an early miscarriage, with time, most women will pass the pregnancy completely. The main issue is time – there is no way to predict exactly when this will occur. You will typically have heavy bleeding and severe abdominal cramping when the pregnancy does pass. Should you want this option, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications can be used once the pregnancy begins to pass from the uterus.
This treatment uses medicines to cause the pregnancy tissue to pass from the uterus. The medicines cause cramping and bleeding, just like what will occur with natural passing of the pregnancy tissue. Using the medicines is like expectant management, except that you know when the pregnancy is going to pass. Most women will pass the pregnancy within 24 hours of taking the medication.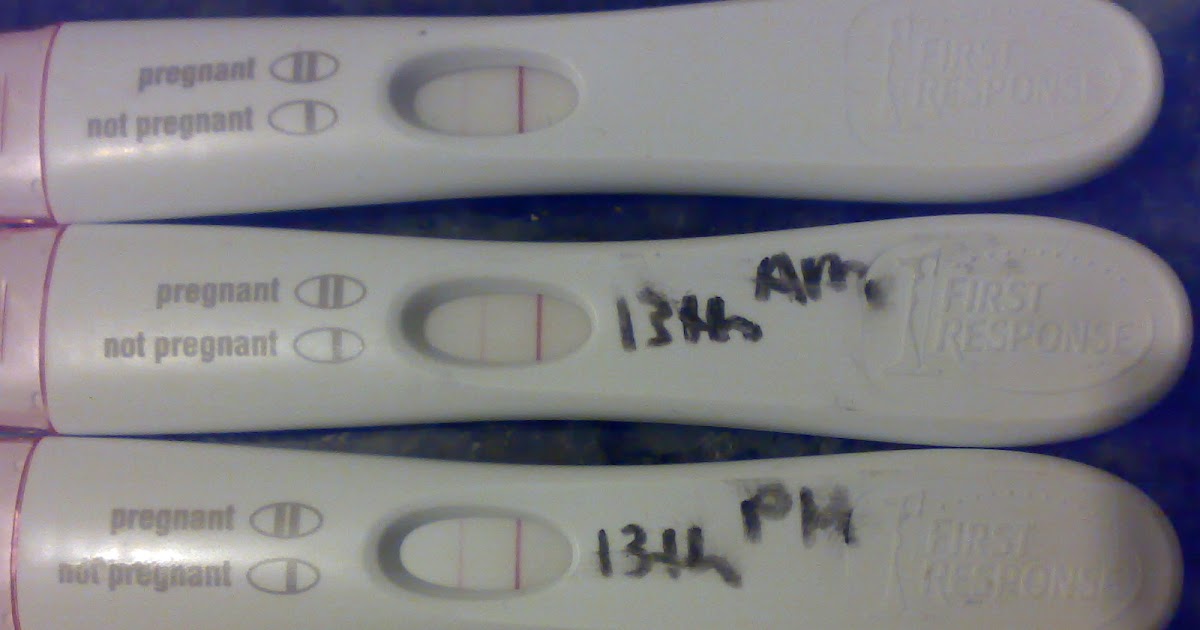 Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
- This brief procedure can be done in the office or the operating room. The following steps occur regardless of the location:
- The woman is in the same position as during a regular pelvic exam, like when a Pap test is done.
- A speculum is placed in the vagina
- A cleansing antibacterial solution is applied to the cervix and vagina
- Numbing medicine is applied to the cervix to decrease cramping
- The cervix is dilated (opened) with thin rods; with early miscarriage, the cervix does not need to be opened much to complete the procedure
- A thin straw-like tube is placed through the open cervixThe pregnancy is removed using a mechanical suction pump attached to the tube
- Everything is removed from the vagina when the procedure is done
You may choose to have the procedure in the office or operating room based on your preferences – different women have different needs.
Office procedure:
- A spouse, partner, friend or relative can be in the room with you
- If desired, oral medications can be taken before the procedure to help you feel more relaxed
- You can eat or drink anything you want before the procedure
- The suction used in the office is most commonly a syringe that creates the suction so no noisy machine is used
- You will usually goes home 15-30 minutes after the procedure and can resume relatively normal activities
- Operating room procedure
- The procedure is done in an outpatient operating suite or in the main hospital
- You will be asleep during the procedure
- You cannot eat or drink anything after midnight on the night before the procedure because you will be receiving anesthesia
- You will feel sleepy for the whole day after the procedure and will need someone to be able to drive you home and be with you for the whole day after the procedure
- The operating room is more appropriate for women with certain medical conditions
After treatment for a miscarriage
Bleeding may continue for several weeks after a miscarriage but tends to be much lighter with a suction aspiration.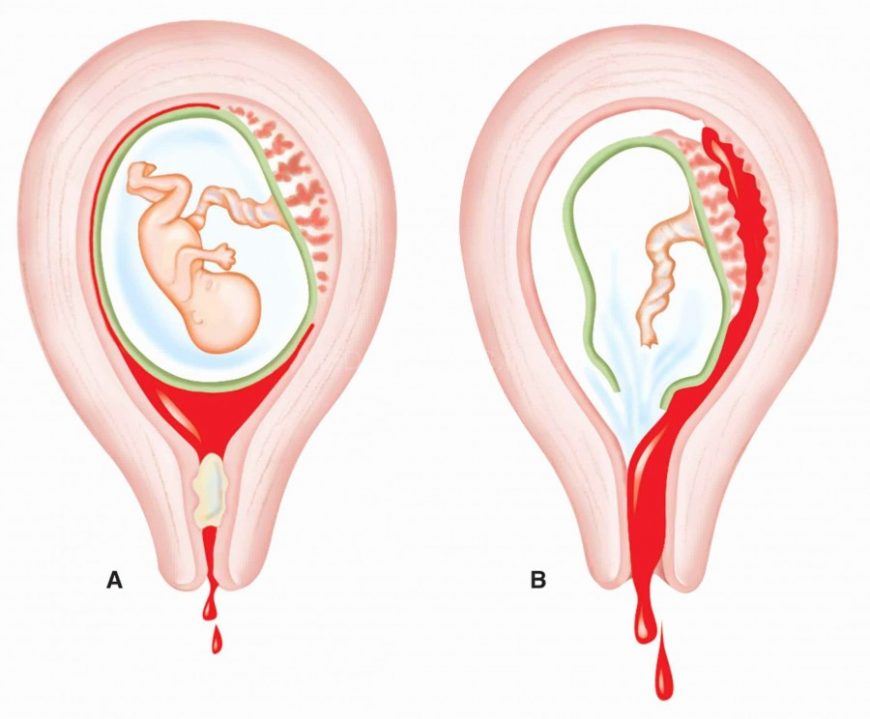 Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Frequently asked questions about miscarriage
Having one miscarriage does not increase your chances of having another. If you have had only one prior miscarriage, the rate of miscarriage in the next pregnancy is similar to the overall rate in the general population.
No. Working, exercise and sexual activity do not increase the risk of miscarriage.
Patients were told years ago to wait one or two menstrual cycles to wait to get pregnant. We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
Since most early miscarriages are caused by problems specific to that fertilized egg, and miscarriage overall is relatively common, most experts do not recommend special testing until you have had three early miscarriages (or two miscarriages in women 40 years and older). At that point it is termed "recurrent" miscarriage and further testing may be needed. Studies have shown that even after a woman has experienced three consecutive miscarriages, her chance of the next pregnancy being normal is still about 70%. All women who have a pregnancy loss later in pregnancy should have further testing.
Tips to help support parents after pregnancy loss
UC Davis Health social worker Brenna Rizan, who works within the Department of Obstetrics/Gynecology provides supportive tips and advice for grieving parents, family and friends after pregnancy loss.
Related stories
Miscarriages are more common than people think - KCRA (Interview with Brenna Rizan)
Facebook Live: Discussing miscarriages with Dr. Mitch Creinin
UC Davis Early Pregnancy and Miscarriage Center
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be initiated.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
The International Histological Classification Organization (FIGO) has declared an epidemic of the situation with an increase in the frequency of miscarriages.
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.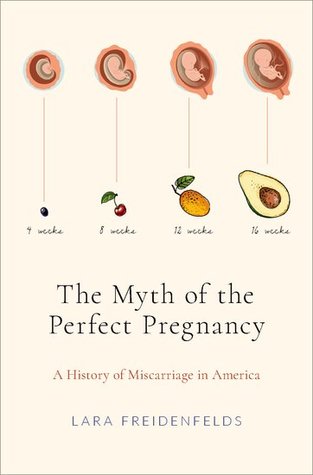
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis.
- antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption.
- use of caffeine (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes per day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).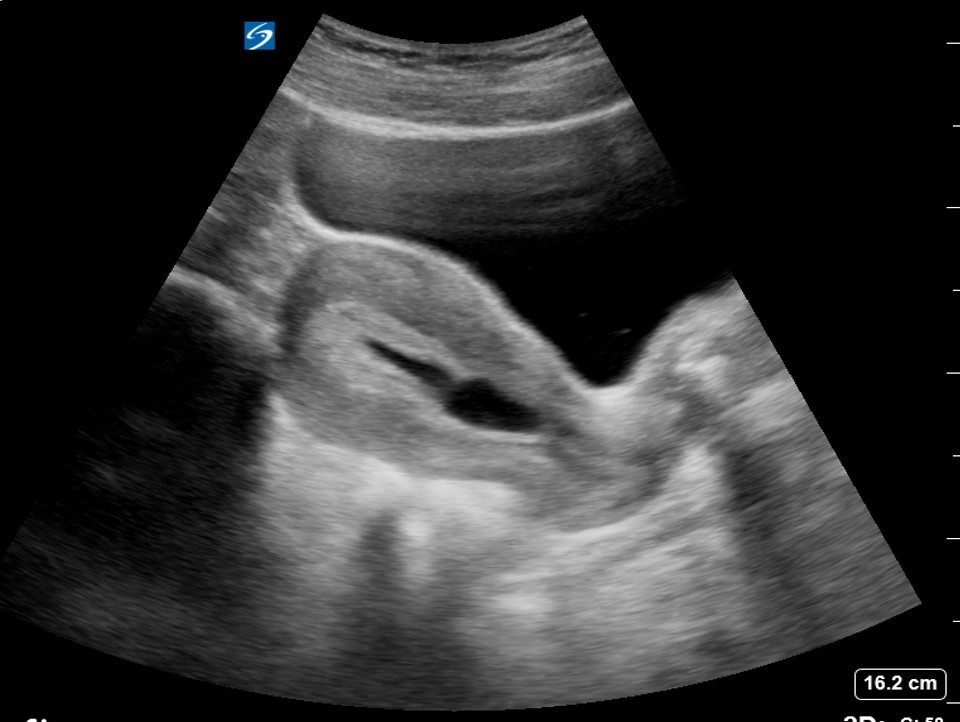
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss?
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repetition of a gynecologist's examination, ultrasound, tests after 7-10 days. If a the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital. A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed.
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis.
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy.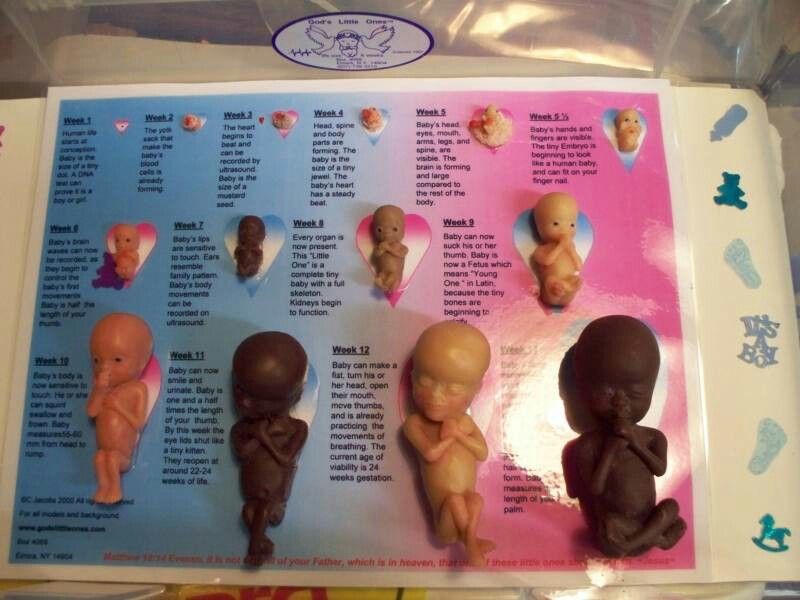 Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy.
If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome).
In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities of a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).