Fetal distress c-section
Fetal distress | Pregnancy Birth and Baby
beginning of content4-minute read
Listen
Fetal distress is a sign your baby isn’t coping with labour. It might mean they need closer monitoring and possibly a caesarean to speed up the birth.
What is fetal distress?
Fetal distress is a sign that your baby is not well. It happens when the baby isn’t receiving enough oxygen through the placenta.
If it’s not treated, fetal distress can lead to the baby breathing in amniotic fluid containing meconium (poo). This can make it difficult for them to breathe after birth, or they may even stop breathing.
Fetal distress can sometimes happen during pregnancy, but it’s more common during labour.
What causes fetal distress?
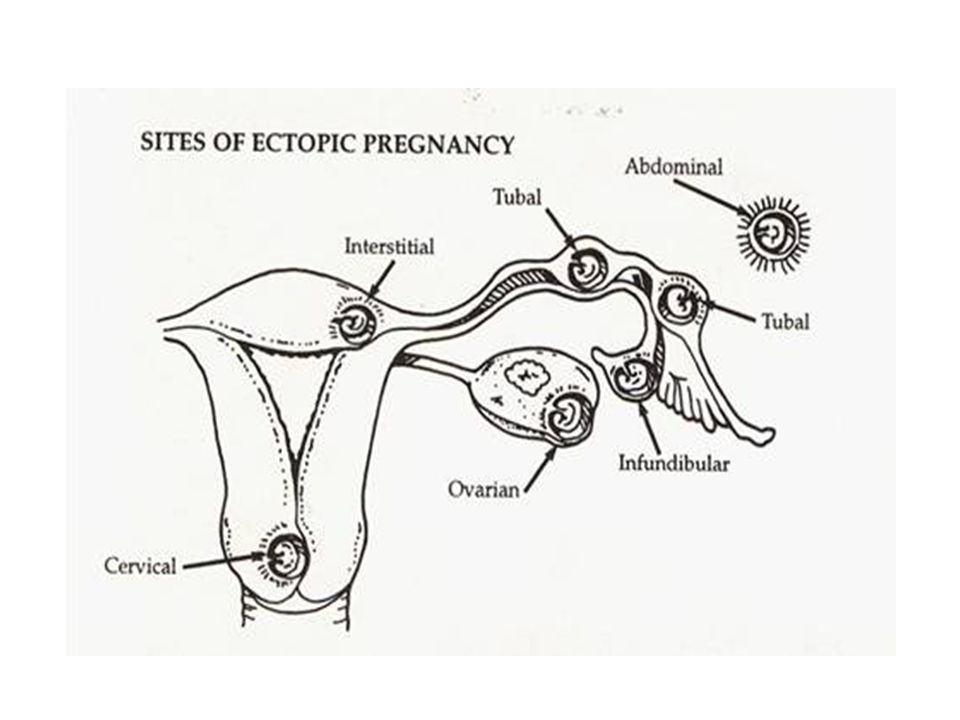
The most common cause of fetal distress is when the baby doesn’t receive enough oxygen because of problems with the placenta (including placental abruption or placental insufficiency) or problems with the umbilical cord (for example, if the cord gets compressed because it comes out of the cervix first).
Fetal distress can also occur because the mother has a health condition such as diabetes, kidney disease or cholestasis (a condition that affects the liver in pregnancy).
It is more common when pregnancy lasts too long, or when there are other complications during labour. Sometimes it happens because the contractions are too strong or too close together.
You are more at risk of your baby experiencing fetal distress if:
- you are obese
- you smoke
- you have high blood pressure in pregnancy or pre-eclampsia
- you have a chronic disease, such as diabetes or kidney disease
- you have a multiple pregnancy
- your baby has intrauterine growth restriction
- you have had a stillbirth before
How is fetal distress diagnosed?
Fetal distress is diagnosed by reading the baby’s heart rate. A slow heart rate, or unusual patterns in the heart rate, may signal fetal distress.
Sometimes fetal distress is picked up when a doctor or midwife listens to the baby’s heart during pregnancy. The baby’s heart rate is usually monitored throughout the labour to check for signs of fetal distress.
The baby’s heart rate is usually monitored throughout the labour to check for signs of fetal distress.
Another sign is if there is meconium in the amniotic fluid. Let your doctor or midwife know right away if your notice the amniotic fluid is green or brown since this could signal the presence of meconium.
How is fetal distress managed?
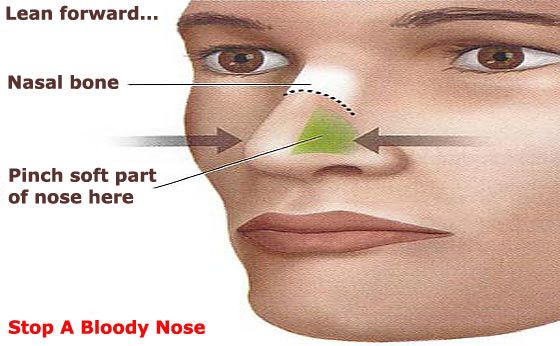
The first step is usually to give the mother oxygen and fluids. Sometimes, moving position, such as turning onto one side, can reduce the baby’s distress.
If you had drugs to speed up labour, these may be stopped if there are signs of fetal distress. If it’s a natural labour, then you may be given medication to slow down the contractions.
Sometimes a baby in fetal distress needs to be born quickly. This may be achieved by an assisted (or instrumental) delivery which is when the doctor uses either forceps or ventouse (vacuum extractor) to help you deliver the baby, or you might need to have an emergency caesarean.
Does fetal distress have any lasting effects?
Babies who experience fetal distress, such as having an usual heart rate or passing meconium during labour, are at greater risk of complications after birth.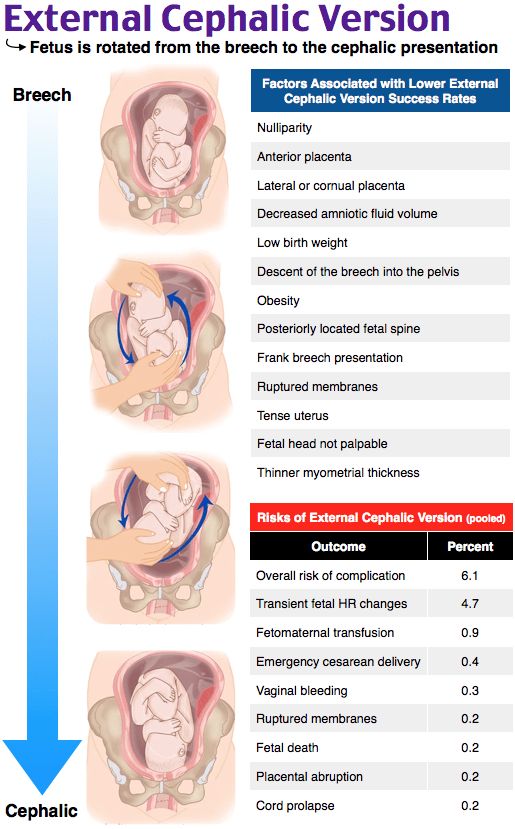 Lack of oxygen during birth can lead to very serious complications for the baby, including a brain injury, cerebral palsy and even stillbirth.
Lack of oxygen during birth can lead to very serious complications for the baby, including a brain injury, cerebral palsy and even stillbirth.
Fetal distress often requires birth by caesarean section. While this is a safe operation, it carries extra risks to both the mother and baby, including blood loss, infections and possible birth injuries.
Babies born with an assisted delivery can also be at greater risk of short-term problems such as jaundice, and may have some difficulty feeding. Having lots of skin-to-skin contact with your baby after the birth and breastfeeding can help reduce these risks.
You won’t necessarily experience fetal distress in your next pregnancy. Every pregnancy is different. If you’re worried about future pregnancies, it can help to talk to your doctor or midwife so they can explain what happened before and during the birth.
Women whose labour didn’t go to plan often feel quite negative about their birth experience.
If you feel sad or disappointed or traumatised about what happened, it is important to talk to someone.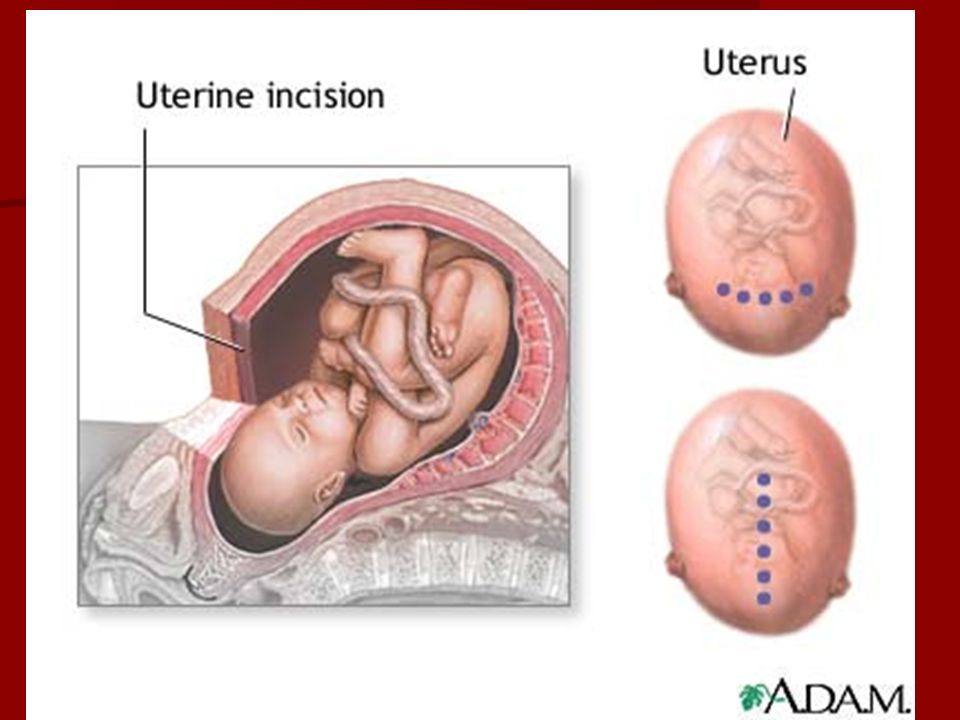 You can contact or talk to a range of people and organisations, including:
You can contact or talk to a range of people and organisations, including:
- Your doctor
- PANDA on 1300 726 306
- Australasian Birth Trauma Association
- Beyond Blue on 1300 22 4636
- Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436
Sources:
Australian Family Physician (Decreased fetal movements: a practical approach in primary care setting), Australasian Birth Trauma Association (What is birth trauma?), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Provision of routine intrapartum care in the absence of pregnancy complications), Birth (The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age), MSD Manual (Fetal distress), Kidspot (All about foetal distress), King Edward Memorial Hospital (Fetal compromise), Journal of Translational Medicine (Reducing the risk of fetal distress with sildenafil study)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2020
Back To Top
Related pages
- Labour complications
- Interventions during labour
- Induced labour
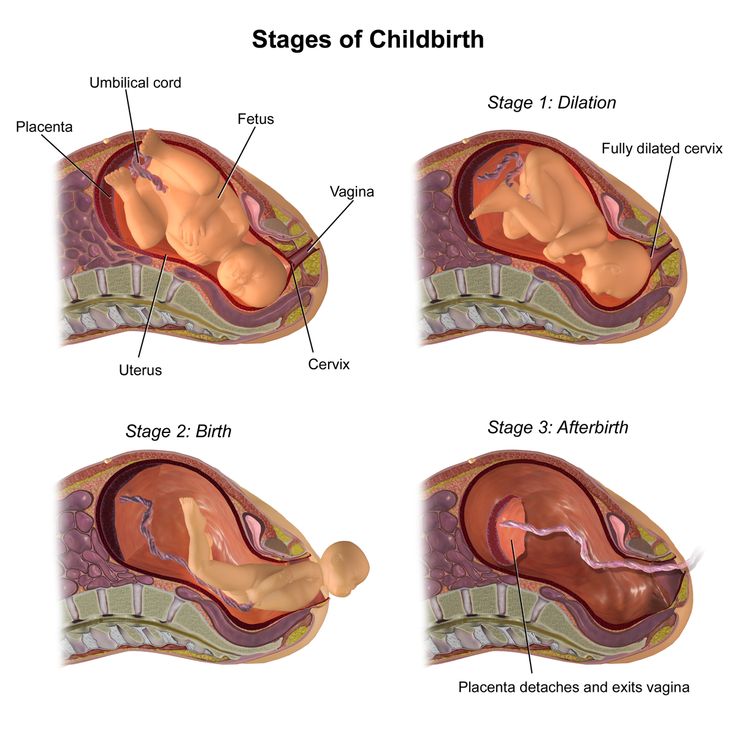
- Giving birth - stages of labour
- Fetal heart rate monitoring
- Baby movements during pregnancy
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Fetal distress and delayed emergency C-section cause baby to be born with brain damage and resultant cerebral palsy
Rebecca Fielding went into labor on March, 25th, 2010 in her home. Fielding was 10 days past her due date and was in labor for 14.5 hours during the first stage of labor, and at least 5 hours during the second stage.![]() She had decided to have a natural birth with a woman who was registered as a nurse / midwife. During labor, the midwife discovered that the baby was not in the proper position, which was making it difficult for the baby to progress through the birth canal. The baby was in the occiput posterior (OP) position, which means his head was down, but unlike a normal position, the baby was facing forward, with his back to his mother’s spine. This position makes it very difficult to progress through the birth canal because it prevents the baby from tucking in his chin. At 12:30 a.m., in an attempt to speed up delivery, the midwife injected Fielding with Pitocin multiple times. Pitocin (oxytocin) is a drug used to expedite delivery by increasing the strength and frequency of contractions. Misjudging the stage of labor, the midwife performed an episiotomy, which is a procedure performed upon immediate delivery in which the perineum is cut in order to enlarge the vaginal opening. Finally, the midwife directed Fielding to cleanse herself with a probiotic treatment, as an alternative to taking antibiotics, in order to prevent the potentially fatal transmission of Group B Strep (for which Fielding had tested positive) to the baby during delivery.
She had decided to have a natural birth with a woman who was registered as a nurse / midwife. During labor, the midwife discovered that the baby was not in the proper position, which was making it difficult for the baby to progress through the birth canal. The baby was in the occiput posterior (OP) position, which means his head was down, but unlike a normal position, the baby was facing forward, with his back to his mother’s spine. This position makes it very difficult to progress through the birth canal because it prevents the baby from tucking in his chin. At 12:30 a.m., in an attempt to speed up delivery, the midwife injected Fielding with Pitocin multiple times. Pitocin (oxytocin) is a drug used to expedite delivery by increasing the strength and frequency of contractions. Misjudging the stage of labor, the midwife performed an episiotomy, which is a procedure performed upon immediate delivery in which the perineum is cut in order to enlarge the vaginal opening. Finally, the midwife directed Fielding to cleanse herself with a probiotic treatment, as an alternative to taking antibiotics, in order to prevent the potentially fatal transmission of Group B Strep (for which Fielding had tested positive) to the baby during delivery.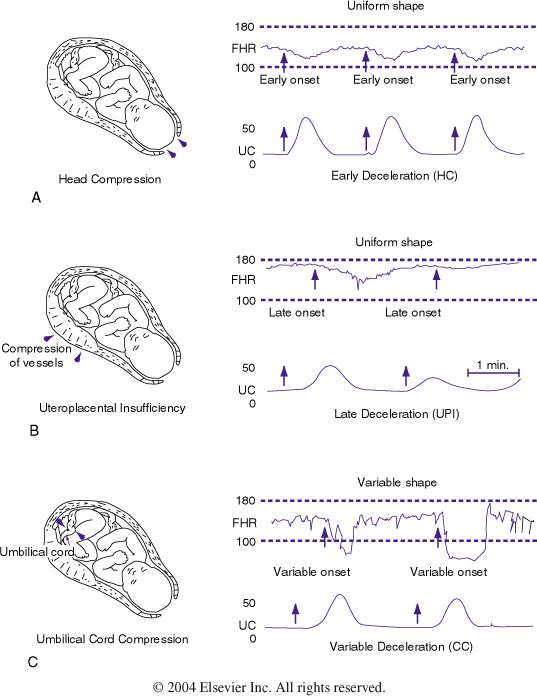 None of these interventions worked, and the midwife “decided it was time to go to the hospital.” The midwife sutured the episiotomy and called an ambulance, which took Fielding to Johns Hopkins Hospital.
None of these interventions worked, and the midwife “decided it was time to go to the hospital.” The midwife sutured the episiotomy and called an ambulance, which took Fielding to Johns Hopkins Hospital.
Fielding arrived at the hospital at 3:30 a.m. on March 26th. The hospital team evaluated Fielding and applied a fetal heart monitor. The medical records indicate that the baby was at a +1 station, which means that the baby’s head was engaged (at a 0 station, the baby’s head is even with a certain part of the mother’s pelvic bone, and at +5 station, the baby’s head crowns and emerges from the vagina). The baby remained at a +1 after the physicians gave Fielding a chance to push a few times. At 3:45 a.m., the physicians decided that she would not be able to deliver vaginally and that an “urgent” rather than an “emergency” C-section was required. One reason for this decision, the physicians stated, was because the fetal heart rate monitor indicated that the baby was adequately oxygenated.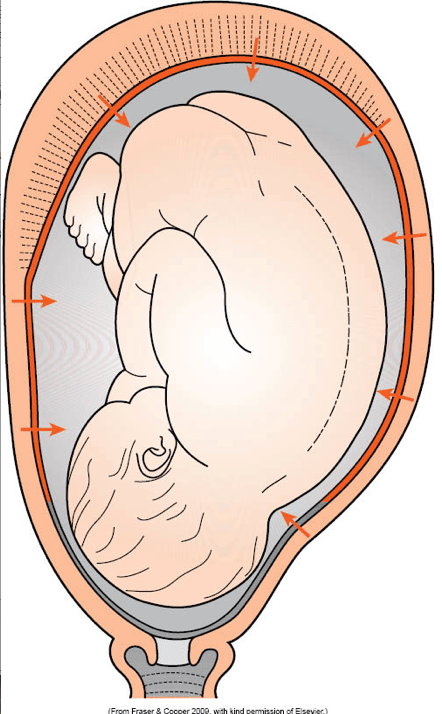 An urgent C-section is one that must be performed as soon as possible, but there is time to have the mother’s blood tested, etc. An emergency C-section is one that must be completed immediately; no blood or other tests are performed.
An urgent C-section is one that must be performed as soon as possible, but there is time to have the mother’s blood tested, etc. An emergency C-section is one that must be completed immediately; no blood or other tests are performed.
The physicians received all the test results they wanted at 4:57 a.m. One of the drugs they wanted to administer to Fielding was penicillin to reduce the risk transmitting GBS to her baby. The medical team made other pre-delivery preparations, and baby Enzo Martinez was delivered at 5:40 a.m. (almost 2 hours after an urgent C-section was ordered) in very poor condition. He was later diagnosed with cerebral palsy, intellectual disabilities and other disorders.
A lawsuit was filed against Johns Hopkins Hospital alleging that the hospital negligently failed to perform a timely C-section. Baby Enzo’s lawyer argued that, had the baby been delivered earlier, as the standard of care required, Enzo would not have suffered injury. In addition, Enzo’s lawyers argued that Johns Hopkins failed to recognize the signs of fetal distress.
Prior to the case going to trial, Enzo’s attorneys filed a motion seeking to exclude testimony regarding the standard of care applicable to the midwife and her alleged breach of that standard while treating Fielding. In response to this, Johns Hopkins argued that the presentation of both were relevant to the hospital’s defense that it was not negligent and that the hospital was not the cause of baby Enzo’s injuries. In support of these assertions, Johns Hopkins attached an order from the Maryland Board of Nursing, which had suspended the midwife’s certification and license to practice as a nurse / midwife. The order stated that the Board had never authorized the midwife to perform deliveries in the home and concluded that she had violated the Nurse Practice Act based upon the care she provided to Fielding and other patients. In fact, the midwife was linked to five other cases, including one that resulted in the death of a newborn. Johns Hopkins attached deposition testimony from physicians indicating that actions taken by the midwife were no longer used during labor and deliveries and that the actions may have contributed to the baby Enzo’s injuries.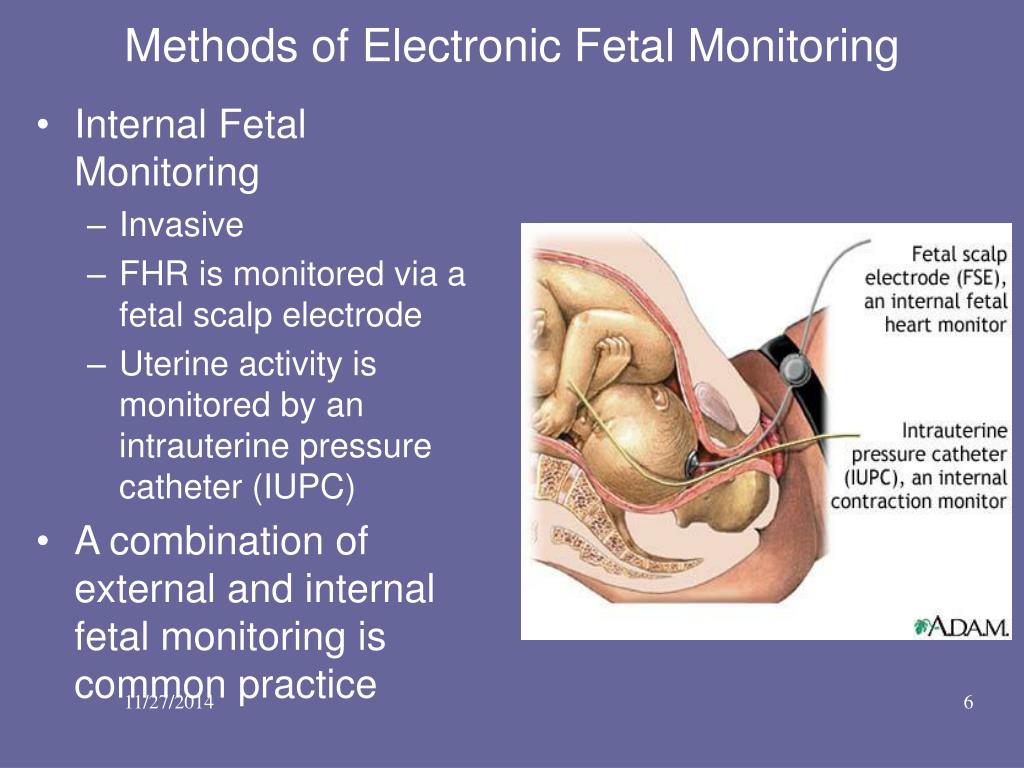
The trial court granted the motion to exclude the testimony.
The trial lasted two weeks and the jury awarded baby Enzo and her family $4 million for lost wages, $25 million for future medical expenses and $26 million for non-economic damages.
Johns Hopkins and baby Enzo both appealed.
On appeal, Johns Hopkins argued that the evidence regarding the standard of care for a midwife and the midwife’s alleged breach of this standard were relevant to its defense that the midwife’s negligence was the sole cause of baby Enzo’s brain damage prior to Fielding arriving at the hospital. Johns Hopkins also argued that the evidence was relevant to explaining why the C-section took place when it did. Johns Hopkins stated that it had to perform additional evaluations to determine the effect the midwife’s negligence had on the baby and mother before performing the C-section.
Baby Enzo’s attorneys argued, among other things, that the trial court acted properly in excluding the evidence, and that Johns Hopkins defense was not contingent upon a finding that the midwife violated the standard of care.
The Court of Special Appeals reversed, holding that the trial court made a mistake when it forbade evidence of the nurse / midwife standard of care and when it forbade evidence of a breach of that standard by a nurse / midwife while treating Fielding. The appellate court also ordered a new trial.
The trial judge had reasoned that the standard of care pertaining to the midwife was irrelevant. “While the trial judge’s inferences are reasonable, his rationale does not recognize the other obvious possibility; namely, that Midwife Muhlhan breached her standard of care, and that the breach was the sole cause of Martinez’s injuries. This was precisely the defense advanced by the Hospital at trial. Thus, the relevant inquiry on appeal is whether evidence of a non-party’s negligence is relevant to a defendant’s complete denial of liability,” the appeals court said.
The appeals court further stated that Johns Hopkins was entitled to try to convince the jury that, not only was it not negligent and not the cause of baby Enzo’s injuries, but that the midwife was negligent and caused the injuries. By precluding such evidence, the jury was given a materially incomplete picture of the facts, which denied the hospital a fair trial.
By precluding such evidence, the jury was given a materially incomplete picture of the facts, which denied the hospital a fair trial.
There are many complex issues – including evidentiary issues – in birth injury malpractice litigation. It therefore is important to hire an attorney who is very experienced in going to trial.
Another reason it is important for a birth injury attorney to be experienced is due to the fact that oftentimes, birth injury cases involve numerous complex medical issues. Medical records can be extremely lengthy and difficult to read; they contain formats, abbreviations and symbols that are usually understood only by medical personnel. An experienced birth injury attorney is familiar with these records and knows how to find evidence of negligence. A skilled and experienced attorney is also familiar with standards of care applicable to the wide array of disorders and complications that can cause birth injuries.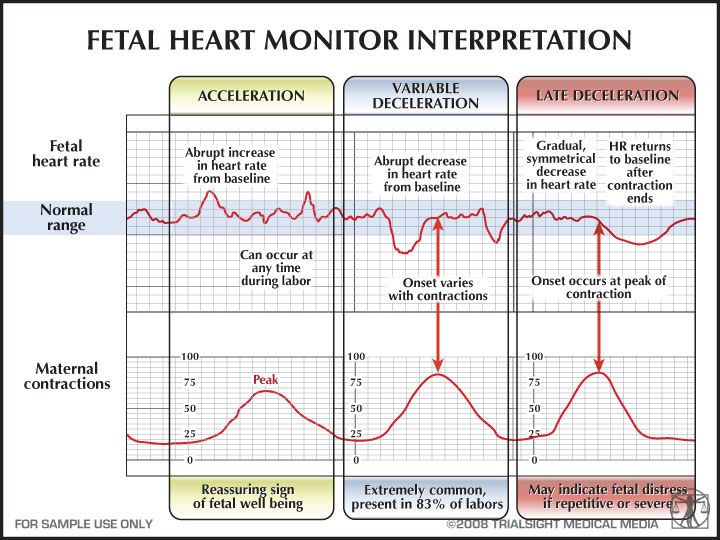
Failure to appropriately manage a baby who is malpositioned
When a baby is not in the normal, head first position, and is malpositioned, as in breech or face presentation, delivery can difficult. OP is another position that can make delivery very difficult. Expectant management (allowing labor to progress naturally) of a baby in OP position is only appropriate when there is a reassuring fetal heart rate, favorable clinical pelvimetry (the mother’s pelvis is large enough to allow the baby to progress through the birth canal), and continued progress in the second stage of labor. OP position is associated with labor abnormalities and a variety of neonatal complications, such as a low Apgar score, acidic blood in the baby (which means the baby is not oxygenating well), meconium stained amniotic fluid (the baby is likely to have inhaled stool into his lungs), birth trauma (head injury and brain bleeds), and the need to be in an intensive care unit after birth. Thus, delivery should occur in a timely fashion, especially if the fetal heart rate is not known or is nonreassuring.
Thus, delivery should occur in a timely fashion, especially if the fetal heart rate is not known or is nonreassuring.
Manual rotation (internal rotation of the baby by the physician’s hand) of a baby in the first stage of labor is not recommended because it could lead to disengagement of the head or umbilical cord prolapse. Sometimes forceps are used for rotation, but experts state that this intervention, which involves insertion of a delivery instrument that looks like salad tongs, should be reserved only to those experienced and skilled in forceps use due to the high risk of complications.
Use of forceps and another delivery device, called a vacuum extractor, to assist with vaginal delivery can be used if the baby is in direct OP position. But again, the physician must have skill and experience in using the delivery device chosen, and the mother must meet certain criteria before delivery instrument use can occur.
In baby Enzo’s case there was no fetal heart monitor used when the midwife first discovered him to be in OP position.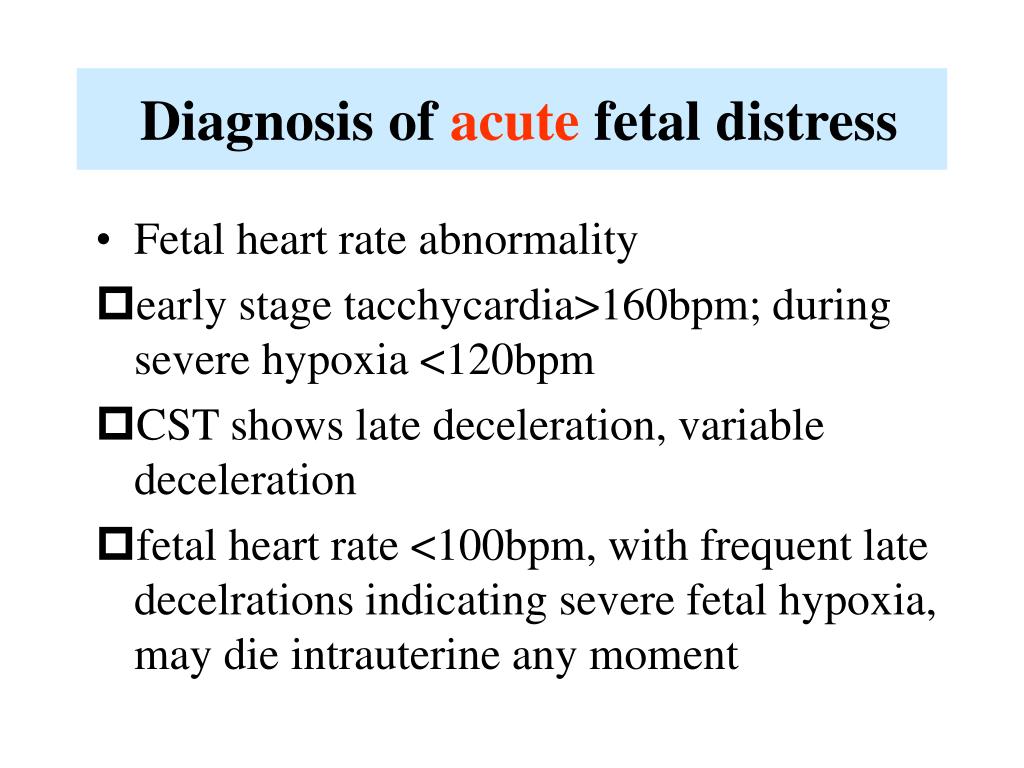 Furthermore, there was dispute about whether Enzo’s heart rate was reassuring at the hospital; experts presented by Enzo’s attorneys contended that the baby’s heartbeat had become nonreassuring by 4:00 a.m., just 30 minutes after arriving at the hospital. Since no fetal heart monitoring was done from the time the midwife discovered that Enzo was in OP position (sometime before 12:30 a.m.) until sometime around 3:30 a.m., baby Enzo could have had numerous episodes of non-reassuring heart tracings before arriving at the hospital.
Furthermore, there was dispute about whether Enzo’s heart rate was reassuring at the hospital; experts presented by Enzo’s attorneys contended that the baby’s heartbeat had become nonreassuring by 4:00 a.m., just 30 minutes after arriving at the hospital. Since no fetal heart monitoring was done from the time the midwife discovered that Enzo was in OP position (sometime before 12:30 a.m.) until sometime around 3:30 a.m., baby Enzo could have had numerous episodes of non-reassuring heart tracings before arriving at the hospital.
Indeed, a non-reassuring heart rate means that the baby must be delivered immediately. Another indication that baby Enzo should have been delivered emergently by C-section is the fact that the second stage of labor was not progressing.
Failure to properly monitor a baby during labor and quickly perform an emergency C-section
An electronic fetal monitor records the mother’s contractions and the baby’s heart beat in response to contractions. When a fetal heart monitor is nonreassuring, it means that the baby is in distress and is not getting enough oxygen (called hypoxia), and prompt and appropriate actions must be taken. In fact, a nonreassuring fetal heart tracing is often the only indication that a baby is in distress. In many cases, an emergency C-section is indicated when this occurs. An emergency C-section is required when a baby has a nonreassuring heart tracing and is in OP position. The baby must be removed from the conditions causing the hypoxia.
In fact, a nonreassuring fetal heart tracing is often the only indication that a baby is in distress. In many cases, an emergency C-section is indicated when this occurs. An emergency C-section is required when a baby has a nonreassuring heart tracing and is in OP position. The baby must be removed from the conditions causing the hypoxia.
When required, an emergency C-section should be performed as quickly as possible, and many times it should be performed within 10 – 18 minutes or less.
Tragically, Enzo was left in stressful, oxygen-depriving conditions and he was born in poor condition and suffered permanent brain damage. When a baby is oxygen-deprived, the hypoxia can get progressively worse. Mere minutes can make a difference in how much damage hypoxia inflicts on the brain. When distress occurs, there is no room for physicians to gamble that a baby will be okay inside the womb.
Indeed, small amounts of time can make a difference during birth when fetal distress and other complications are occurring, which is why it is imperative that hospitals with be fully prepared to timely deliver a baby by C-section.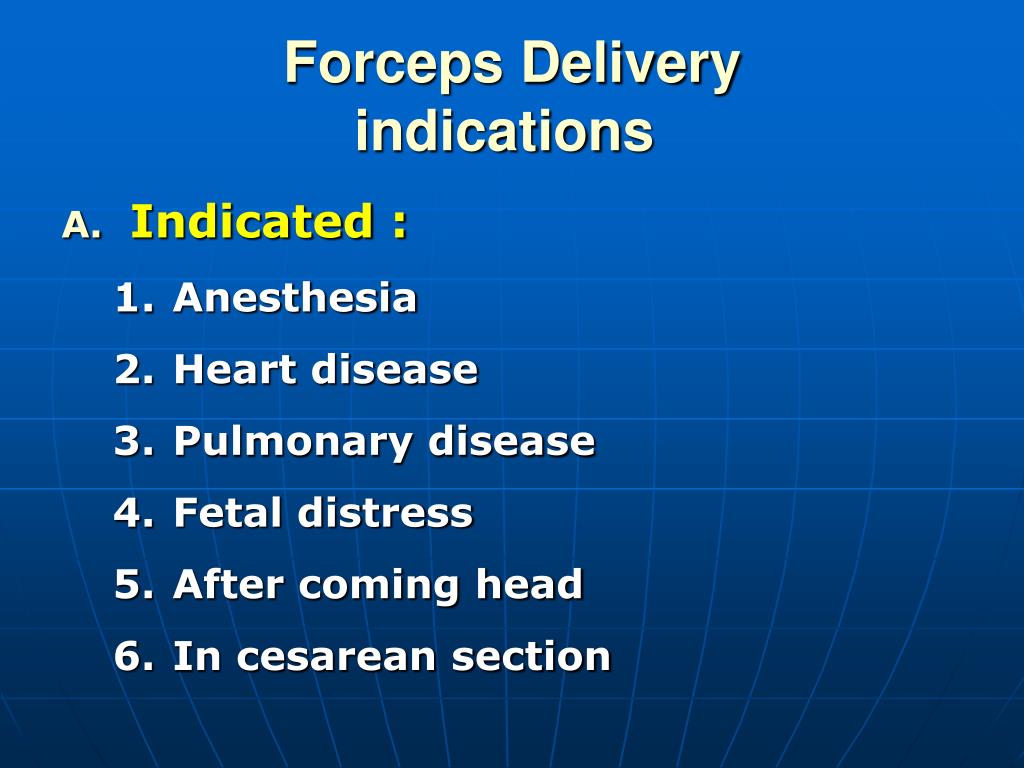 This means that the facility must have proper anesthesia and surgical personnel to permit the start of C-section delivery within 30 minutes of the decision to perform the procedure, according to guidelines set forth by the American Congress of Obstetrics and Gynecology (ACOG) and the American Society of Anesthesiologists (ASA). Furthermore, experts state that in certain cases, a C-section must be performed in a matter of minutes, and in more serious conditions, such as when a baby is OP position and has a nonreassuring heart rate, delivery must occur as soon as possible.
This means that the facility must have proper anesthesia and surgical personnel to permit the start of C-section delivery within 30 minutes of the decision to perform the procedure, according to guidelines set forth by the American Congress of Obstetrics and Gynecology (ACOG) and the American Society of Anesthesiologists (ASA). Furthermore, experts state that in certain cases, a C-section must be performed in a matter of minutes, and in more serious conditions, such as when a baby is OP position and has a nonreassuring heart rate, delivery must occur as soon as possible.
Use of Pitocin
Pitocin causes frequent and strong contractions and because of this, a condition called hyperstimulation can occur. Hyperstimulation means that the contractions are so fast and strong that it is essentially as if the uterus is in a constant state of contraction. When the uterus (womb) contracts, blood vessels are impinged upon and this impingement hinders that ability of oxygen-rich blood to be transported to the baby.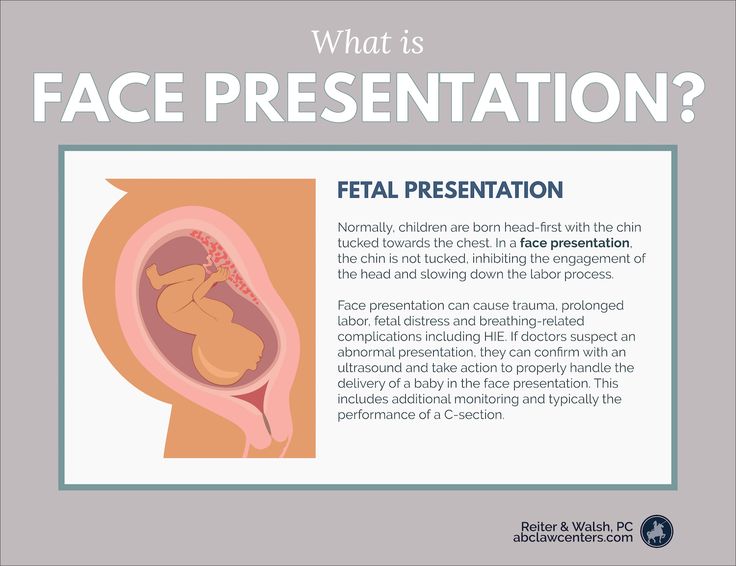 In a state of contraction with almost no breaks, a baby could be receiving very little oxygen or almost no oxygen at all. In fact, Pitocin has been labeled a high risk drug by the Food and Drug Administration (FDA). Due to this, it is critical that a baby’s heart rate be continuously monitored and closely watched when Pitocin is administered.
In a state of contraction with almost no breaks, a baby could be receiving very little oxygen or almost no oxygen at all. In fact, Pitocin has been labeled a high risk drug by the Food and Drug Administration (FDA). Due to this, it is critical that a baby’s heart rate be continuously monitored and closely watched when Pitocin is administered.
Baby Enzo had no fetal monitoring for at least 3 hours after Pitocin was administered. This violates standards of care and is considered negligence.
Group B Strep (GBS)
GBS is a bacterium that is part of the normal flora of the gut and genital tract. When a GBS infection occurs, it means there is too much GBS present, and this infection can cause servere illness and death in newborns who are exposed to it. Babies can be exposed to the bacteria during delivery if they come into contact with it in the birth canal. When a mother has a GBS infection, the rate of transmission to the baby is approximately 50% during vaginal delivery.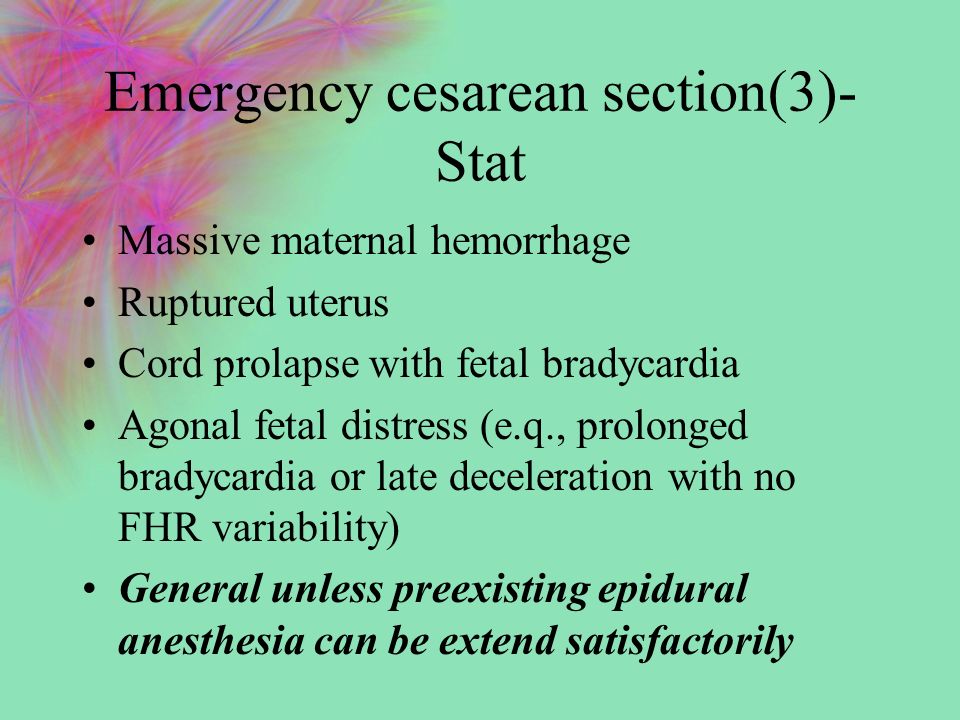 It therefore is crucial that a mother be given appropriate antibiotics to prevent the baby from GBS infection. Antibiotics such as penicillin are typically given during labor to prevent transmission of the infection.
It therefore is crucial that a mother be given appropriate antibiotics to prevent the baby from GBS infection. Antibiotics such as penicillin are typically given during labor to prevent transmission of the infection.
Generally, the type of birth (C-section versus vaginal delivery) does not affect how a physician will proceed with regards to GBS prophylactic treatment. What is most important is whether the baby is exposed to the bacteria and how best to protect him or her from possible infection. If the water remains intact, the baby is not exposed to the bacteria. And if it is broken, the baby is exposed. The antibiotics will wipe out the bacteria in the vagina, and they will transfer to the baby to help him or her fight a possible infection.
The midwife treated the GBS by using a probiotic, which is not the standard of care for treatment. Fielding was in labor for at least 3 hours (probably a lot more, given the timeline of events) before the proper treatment, penicillin, was administered. This constitutes negligence. In addition, it appears as though the hospital may have waited for test results before administering the penicillin. The physicians were aware that Fielding had GBS. If a baby is about to be born, treatment of GBS should be administered immediately. In fact, even if a mother is suspected of having GBS, the standard of care is to quickly administer an appropriate antibiotic. GBS is very serious, and a medical team should not risk exposure to the baby.
This constitutes negligence. In addition, it appears as though the hospital may have waited for test results before administering the penicillin. The physicians were aware that Fielding had GBS. If a baby is about to be born, treatment of GBS should be administered immediately. In fact, even if a mother is suspected of having GBS, the standard of care is to quickly administer an appropriate antibiotic. GBS is very serious, and a medical team should not risk exposure to the baby.
When a baby suffers from permanent brain damage as is the case with baby Enzo, it is devastating. When negligence on the part of trusted medical personnel causes the damage, it is especially tragic.
Failure to properly monitor a baby who is in a high risk situation is considered negligence. In addition, failure to properly interpret the fetal heart tracings and recognize distress also constitutes negligence.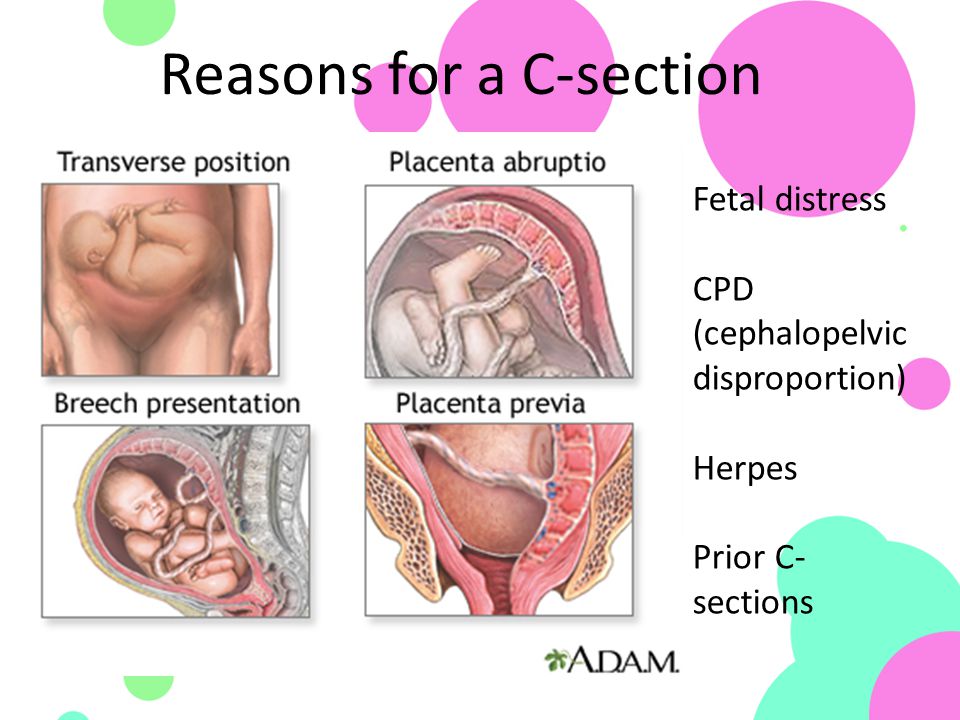 Failure to properly treat a maternal infection and failure to quickly deliver a baby by ermegency C-section when indicated is negligent behavior. When this negligence causes injury in the baby, it is medical malpractice.
Failure to properly treat a maternal infection and failure to quickly deliver a baby by ermegency C-section when indicated is negligent behavior. When this negligence causes injury in the baby, it is medical malpractice.
Due to the complex nature of birth injury cases, it is imperative to have skilled and experienced attorneys. At Reiter & Walsh ABC Law Centers, our attorneys will research your case, find the cause of injury and determine if negligence occurred. For decades, we have been helping families in Michigan and throughout the nation, and we have numerous multi-million dollar verdicts that attest to our success. We will fight to obtain the compensation you and your family deserve for lifelong care, treatment and therapy of your child, and you never pay any money until we win your case. Call us at 888-419-2229.
Cesarean section - Clinic 29
Modern technique caesarean section is that the incision of the skin and subcutaneous tissue is made along the lower fold of the abdomen in the transverse direction (according to Pfannenstiel) up to 15 cm long, or a transverse incision is made (according to Joel-Kohan ) 2-3 cm below the middle of the distance between the womb and the navel, 10-12 cm long.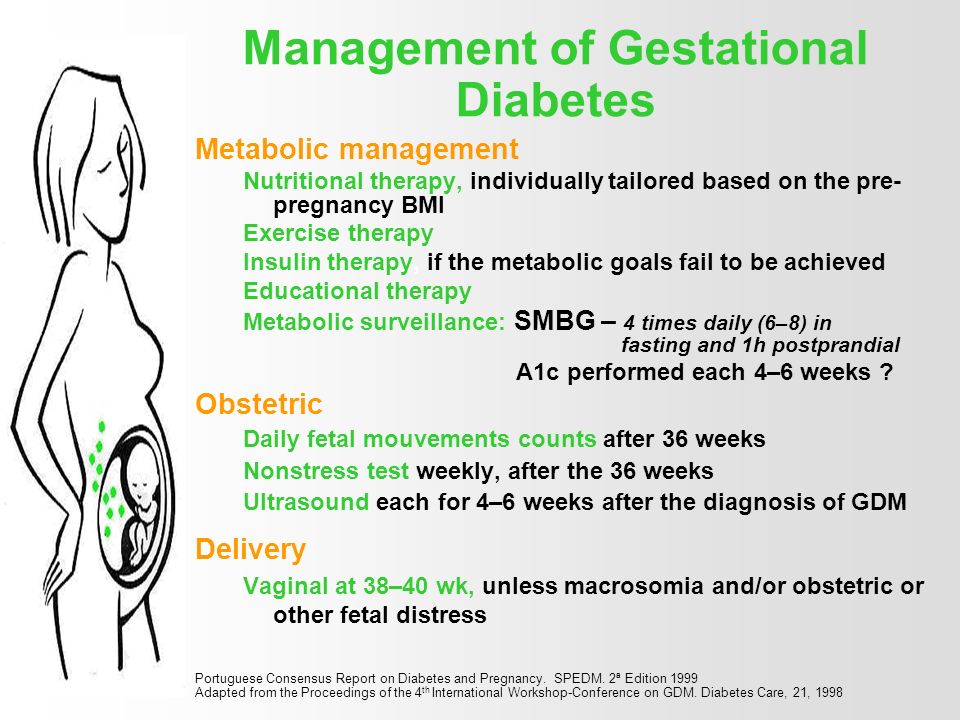 This is a convenient and fairly quick operative access for caesarean section. Such an incision has its advantages: it has a good cosmetic effect, which explains the widespread use of this type of intervention, because both of these incisions create favorable conditions for intradermal suture. It is noteworthy that during a repeated caesarean section, an incision on the skin is made at the site of the previous scar with excision of the latter. Such an incision of the anterior abdominal wall allows for a more active postoperative period compared to a longitudinal (lower median) incision. The puerperal woman is allowed to get out of bed during the first day after the operation, which is the prevention of subinvolution of the uterus, intestinal paresis, the formation of adhesions and reduces the risk of thrombosis in the postoperative period.
This is a convenient and fairly quick operative access for caesarean section. Such an incision has its advantages: it has a good cosmetic effect, which explains the widespread use of this type of intervention, because both of these incisions create favorable conditions for intradermal suture. It is noteworthy that during a repeated caesarean section, an incision on the skin is made at the site of the previous scar with excision of the latter. Such an incision of the anterior abdominal wall allows for a more active postoperative period compared to a longitudinal (lower median) incision. The puerperal woman is allowed to get out of bed during the first day after the operation, which is the prevention of subinvolution of the uterus, intestinal paresis, the formation of adhesions and reduces the risk of thrombosis in the postoperative period.
Over the past 10 years, the technique of caesarean section has progressively changed. A prerequisite for this was the work proving that the unsutured visceral and parietal peritoneum does not entail any additional postoperative complications and even significantly reduces the likelihood of adhesions in the abdominal cavity.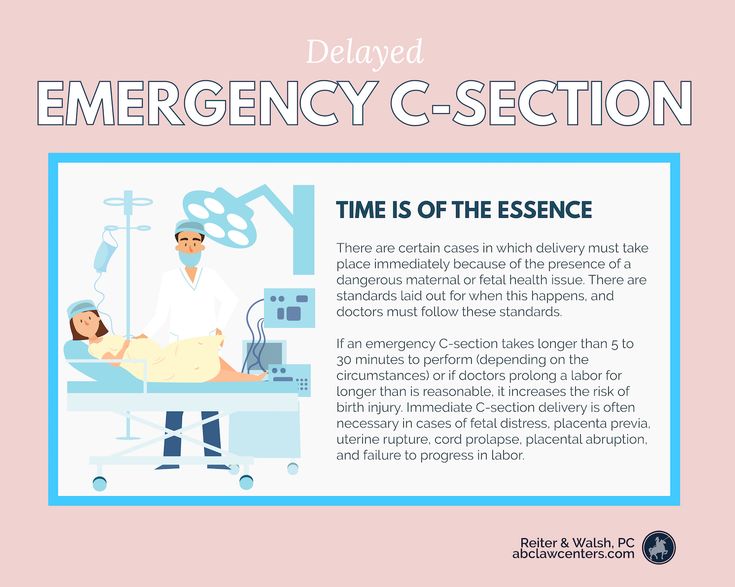 Another prerequisite was the widespread use in surgical practice of synthetic (vicryl, polyglycolide) absorbable suture material, and therefore, when suturing an incision on the uterus, a single-row continuous suture is more often used. In patients with a single-row suture on the uterus (according to ultrasound data), edema in the area of the postoperative suture is observed 4 times less often than with a double-row suture. The suture on the uterus and aponeurosis is treated using argon plasma coagulation (APC). A feature of the APC is that the active electrode is blown with argon, ionized, and a torch is formed between the electrode and the tissue. In an environment of inert argon gas at a temperature of 120°C, tissue coagulation occurs to a depth of no more than 3 mm. In this case, there is no effect of carbonization-charring, since there is no direct combustion of the tissue, and there is also a direct thermal effect on the microbial agent. Due to APC, the healing processes are activated - as a result of deep tissue heating: myometrium in the suture area (to a depth of 10-15 mm) and reduction of collagen fibers due to tissue heat treatment.
Another prerequisite was the widespread use in surgical practice of synthetic (vicryl, polyglycolide) absorbable suture material, and therefore, when suturing an incision on the uterus, a single-row continuous suture is more often used. In patients with a single-row suture on the uterus (according to ultrasound data), edema in the area of the postoperative suture is observed 4 times less often than with a double-row suture. The suture on the uterus and aponeurosis is treated using argon plasma coagulation (APC). A feature of the APC is that the active electrode is blown with argon, ionized, and a torch is formed between the electrode and the tissue. In an environment of inert argon gas at a temperature of 120°C, tissue coagulation occurs to a depth of no more than 3 mm. In this case, there is no effect of carbonization-charring, since there is no direct combustion of the tissue, and there is also a direct thermal effect on the microbial agent. Due to APC, the healing processes are activated - as a result of deep tissue heating: myometrium in the suture area (to a depth of 10-15 mm) and reduction of collagen fibers due to tissue heat treatment.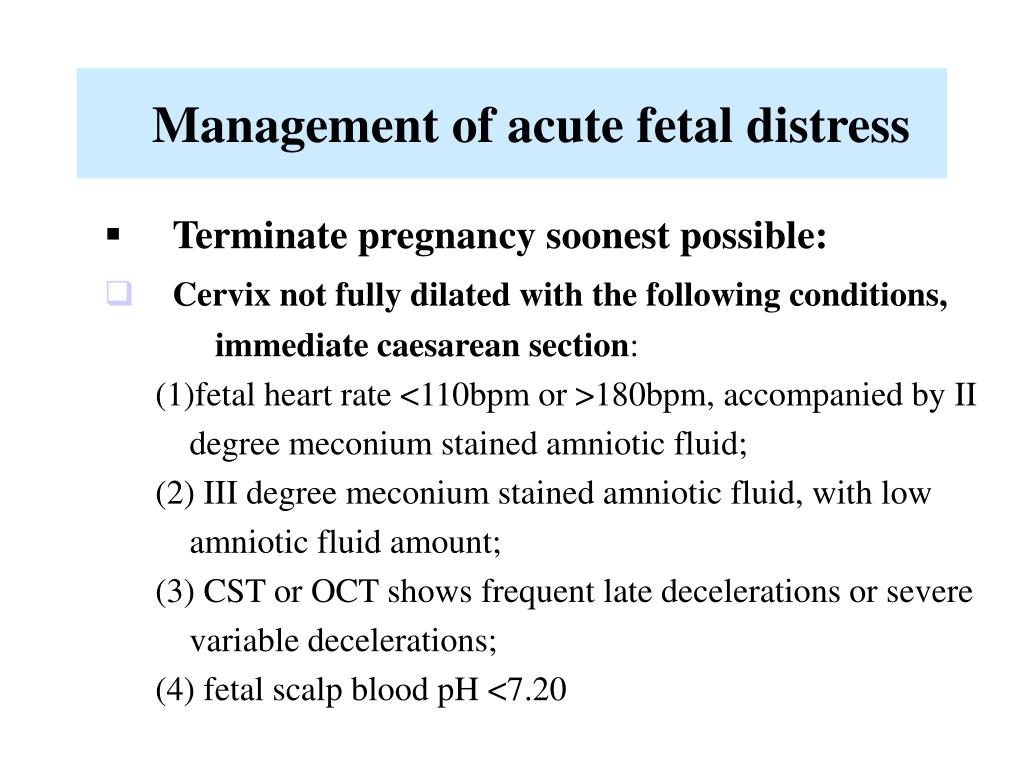 The use of APC for caesarean section can reduce blood loss during surgery, improve the quality of life in the postoperative period by reducing pain and reducing the length of stay in the hospital. Direct antibacterial action makes it possible to refuse preventive course antibiotic therapy, promotes the healing of the surgical wound, and reduces the risk of purulent-inflammatory diseases in the postoperative period. In addition, the consistency of the scar on the uterus is achieved, which allows you to increase the percentage of subsequent spontaneous births.
The use of APC for caesarean section can reduce blood loss during surgery, improve the quality of life in the postoperative period by reducing pain and reducing the length of stay in the hospital. Direct antibacterial action makes it possible to refuse preventive course antibiotic therapy, promotes the healing of the surgical wound, and reduces the risk of purulent-inflammatory diseases in the postoperative period. In addition, the consistency of the scar on the uterus is achieved, which allows you to increase the percentage of subsequent spontaneous births.
The combination of several well-known techniques and the elimination of a number of optional steps make it possible to speak of Stark caesarean section as a new modification that has a number of advantages over conventional methods. These include rapid retrieval; a significant reduction in the duration of the operation; reduction of blood loss; reducing the need for postoperative use of painkillers; reduction in the incidence of intestinal paresis and other postoperative complications; earlier discharge for 3-4 days after birth.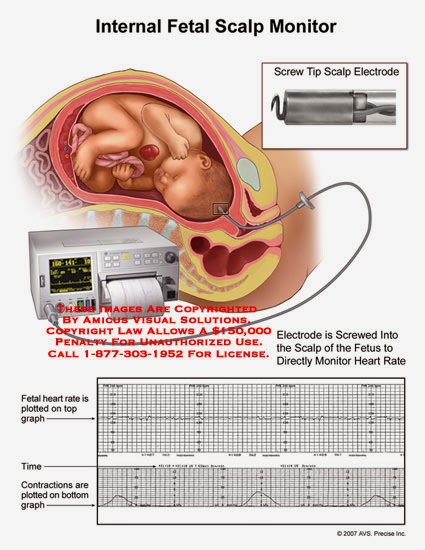
The duration of a traditional surgical intervention is on average 40 minutes, and in the Stark modification - 22 minutes. Due to these advantages, as well as the simplicity of the method itself, this operation is quickly gaining popularity. Babies removed after a cesarean section according to Stark have a more stable adaptation, which allows them to be breastfed during the first minutes of life.
Our Maternity Hospital uses a new technique of "slow" caesarean section. A unique, gentle way of delivery "slow" caesarean section at 29maternity hospital! The method of "natural" or "slow" caesarean section, for patients with a contraindication for natural childbirth, was developed by English specialists in elite clinics in London. Its essence is as follows: the woman in labor is conscious, as in a conventional cesarean, the doctor makes a small incision and removes the baby's head. Unlike a standard cesarean section, when the baby is quickly taken out, not giving the opportunity to adapt to environmental conditions, with a “slow” cesarean section, the child is given the opportunity to get out of the uterus on his own. The mother is actively involved in the delivery process, she can watch how the baby is born. This method of operative delivery is safe for mother and baby, and it is gaining more and more supporters among women abroad, especially in the UK. Maternity Hospital at City Clinical Hospital No. 29is the only state maternity hospital in Moscow where this unique technique is used.
The mother is actively involved in the delivery process, she can watch how the baby is born. This method of operative delivery is safe for mother and baby, and it is gaining more and more supporters among women abroad, especially in the UK. Maternity Hospital at City Clinical Hospital No. 29is the only state maternity hospital in Moscow where this unique technique is used.
Maternity hospital at City Clinical Hospital No. 29 — we will answer your questions!
Childbirth:
- How to improve conditions?
- How to give birth calmly?
- Will my doctor be there?
Pregnancy:
- How to avoid queues?
- How to be observed individually?
- Will everything be all right?
Get the answer by phone right now!
Call us:
Record in the maternity hospital
+7 (495) 360-01-70
Paid services of the hospital
+7 (495) 360-40-93
Contract for the contract for childbirth
8 (916) 595-26-04
Consultation on paid maternity hospital services
+7 (495) 360-40-93+7 (966) 039-07-70+7 (985) 032-50- 89
appointment from 9.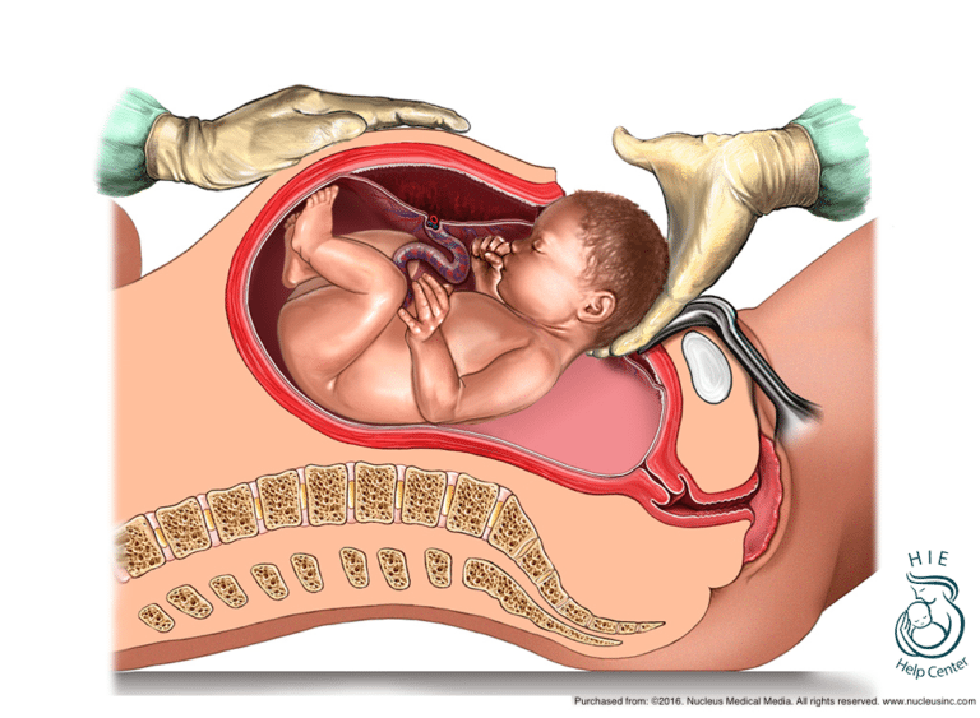 00 to 17.00
00 to 17.00
Maternity hospital departments 29
Endocrine Women's Center
Neonatal and Prematurity Pathology Unit
Neonatology Unit
WHO: Women in labor and doctors increasingly opt for caesarean section |
According to the World Health Organization, modern surgical approaches, effective painkillers and antibiotics make it possible to perform surgery with minimal risk to mother and child. A new WHO study in this area has shown that in countries where at least 10% of women undergo this operation, maternal and child mortality is reduced. However, caesarean section certainly has its downsides.
“My doctor recommended a caesarean section almost immediately. He explained it by my age. Although this was the second birth for me, but I was already 44 years old. And when I came to the hospital at the appointed time, they said: why, actually, a caesarean? according to what evidence? But my doctor insisted, he didn't want to risk anything.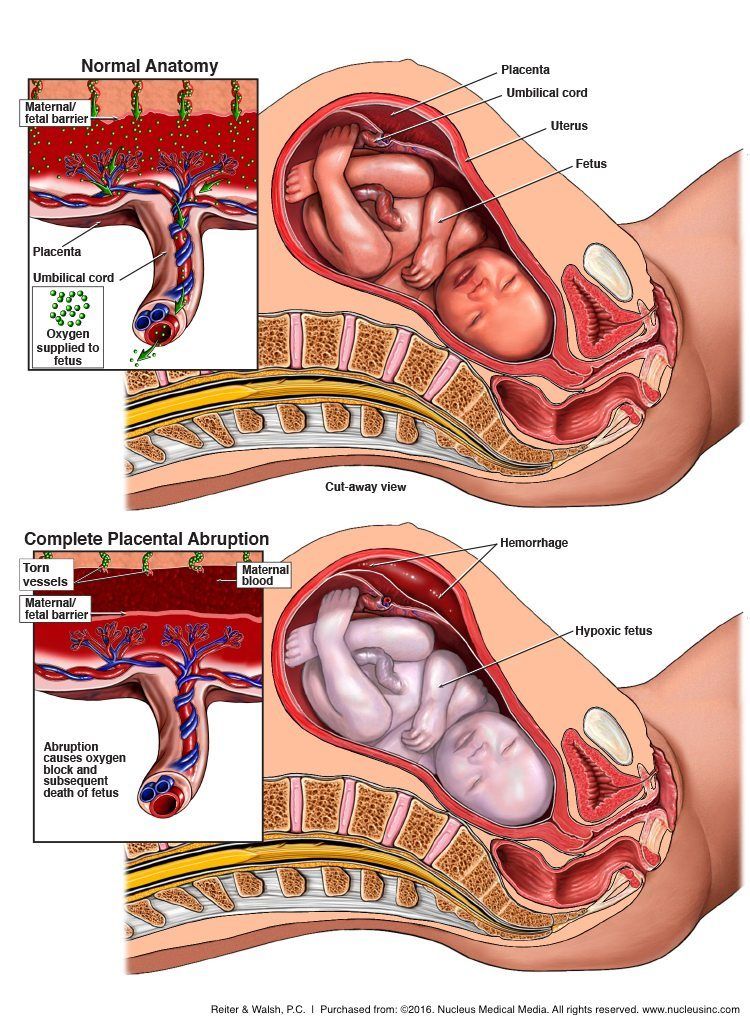 And then, after the birth, he told me that the child had an entanglement of the umbilical cord, and during childbirth this loop could tighten around the child’s neck.
And then, after the birth, he told me that the child had an entanglement of the umbilical cord, and during childbirth this loop could tighten around the child’s neck.
More and more women choose caesarean section as the most painless, quick and safe way to give birth. Caesarean section is especially popular in developed and developing countries. The numbers are impressive. For example, in Brazil, 45% of women choose a caesarean section. In European countries, this figure has increased from 15% to 22% over the past 20 years. WHO spokeswoman Dr. Marlene Temmerman says:
In Brazil, 45% of women opt for a caesarean section. In European countries, this figure has grown from 15% to 22% over the past 20 years
“In many developing and developed countries, there is a real epidemic of caesarean sections. A cesarean is done even when there is no medical need for it. You may be wondering: so what? If women choose caesarean section and it is safe, why not? Yes, in modern conditions it is really safe. But do not forget that this is still an operation, a surgical intervention.
But do not forget that this is still an operation, a surgical intervention.
A caesarean section can cause serious complications for both the baby and the mother. Marlene Temmerman explains:
“Women who have a cesarean are at a higher risk of bleeding. Also, do not forget about the scars that remain from previous births that have passed with the help of surgical intervention. Serious complications may arise. And even in some developed countries, where caesareans are often performed, a higher level of maternal mortality has been reported compared to other developed countries. Of course, this operation is not the main cause of death among women in childbirth, but the connection certainly exists.
However, the preference for caesarean is made, of course, not only by women, but also by doctors. And they are partly understandable. It is better to perform a scheduled operation at a prearranged time than to receive a call from a patient in the middle of the night and then have to deal with this or that unforeseen situation during childbirth:
adjust your schedule.