Miscarriage after 1 month
Miscarriage - Causes - NHS
There are many reasons why a miscarriage may happen, although the cause is often not identified.
If a miscarriage happens during the first trimester of pregnancy (the first 3 months), it's usually caused by problems with the unborn baby (foetus). About 3 in every 4 miscarriages happen during this period.
If a miscarriage happens after the first trimester of pregnancy, it may be the result of things like an underlying health condition in the mother.
These late miscarriages may also be caused by an infection around the baby, which leads to the bag of waters breaking before any pain or bleeding. Sometimes they can be caused by the neck of the womb opening too soon.
First trimester miscarriages
First trimester miscarriages are often caused by problems with the chromosomes of the foetus.
Chromosome problems
Chromosomes are blocks of DNA. They contain a detailed set of instructions that control a wide range of factors, from how the cells of the body develop to what colour eyes a baby will have.
Sometimes something can go wrong at the point of conception and the foetus receives too many or not enough chromosomes. The reasons for this are often unclear, but it means the foetus will not be able to develop normally, resulting in a miscarriage.
This is very unlikely to recur. It does not necessarily mean there's any problem with you or your partner.
Placenta problems
The placenta is the organ linking your blood supply to your baby's. If there's a problem with the development of the placenta, it can also lead to a miscarriage.
Things that increase your risk
An early miscarriage may happen by chance. But there are several things known to increase your risk of problems happening.
But there are several things known to increase your risk of problems happening.
Your age can also have an influence:
- in women under 30, 1 in 10 pregnancies will end in miscarriage
- in women aged 35 to 39, up to 2 in 10 pregnancies will end in miscarriage
- in women over 45, more than 5 in 10 pregnancies will end in miscarriage
A pregnancy may also be more likely to end in miscarriage if you:
- are obese
- smoke
- use drugs
- drink lots of caffeine
- drink alcohol
Second trimester miscarriages
Long-term health conditions
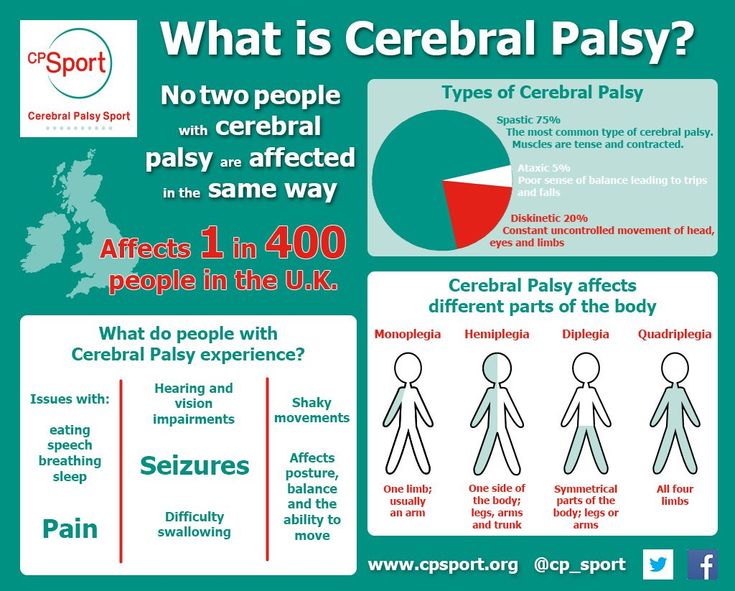
Several long-term (chronic) health conditions can increase your risk of having a miscarriage in the second trimester, especially if they're not treated or well controlled.
These include:
- diabetes (if it's poorly controlled)
- severe high blood pressure
- lupus
- kidney disease
- an overactive thyroid gland (hyperthyroidism)
- an underactive thyroid gland (hypothyroidism)
- antiphospholipid syndrome (APS)
Infections
The following infections may also increase your risk:
- rubella (german measles)
- cytomegalovirus (CMV)
- bacterial vaginosis
- HIV
- chlamydia
- gonorrhoea
- syphilis
- malaria
Food poisoning
Food poisoning, caused by eating contaminated food, can also increase the risk of miscarriage. For example:
For example:
- listeriosis – most commonly found in unpasteurised dairy products, such as blue cheese
- toxoplasmosis – which can be caught by eating raw or undercooked infected meat
- salmonella – most often caused by eating raw or partly cooked eggs
Read more about foods to avoid in pregnancy.
Medicines
Medicines that increase your risk include:
- misoprostol – used for stomach ulcers
- retinoids – used for eczema and acne
- methotrexate – used for conditions such as rheumatoid arthritis
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen; these are used for pain and inflammation
To be sure a medicine is safe in pregnancy, always check with your doctor, midwife or pharmacist before taking it.
Read more about medicines during pregnancy.
Womb structure
Problems and abnormalities with your womb can also lead to second trimester miscarriages. Possible problems include:
- non-cancerous growths in the womb called fibroids
- an abnormally shaped womb
Weakened cervix
In some cases, the muscles of the cervix (neck of the womb) are weaker than usual. This is known as a weakened cervix or cervical incompetence.
A weakened cervix may be caused by a previous injury to this area, usually after a surgical procedure. The muscle weakness can cause the cervix to open too early during pregnancy, leading to a miscarriage.
Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a condition where the ovaries are larger than normal. It's caused by hormonal changes in the ovaries.
It's caused by hormonal changes in the ovaries.
PCOS is known to be a leading cause of infertility as it can prevent the release of an egg (ovulation). There's some evidence to suggest it may also be linked to an increased risk of miscarriage.
Misconceptions about miscarriage
An increased risk of miscarriage is not linked to:
- your emotional state during pregnancy, such as being stressed or depressed
- having a shock or fright during pregnancy
- exercise during pregnancy – but discuss with your GP or midwife what type and amount of exercise is suitable for you during pregnancy
- lifting or straining during pregnancy
- working during pregnancy – or work that involves sitting or standing for long periods
- having sex during pregnancy
- travelling by air
- eating spicy food
Recurrent miscarriages
If you have had a miscarriage, it's natural to worry that you'll have another if you get pregnant again. But most miscarriages are a one-off event.
But most miscarriages are a one-off event.
About 1 in 100 women experience recurrent miscarriages (3 or more in a row) and many of these women go on to have a successful pregnancy.
Page last reviewed: 09 March 2022
Next review due: 09 March 2025
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman.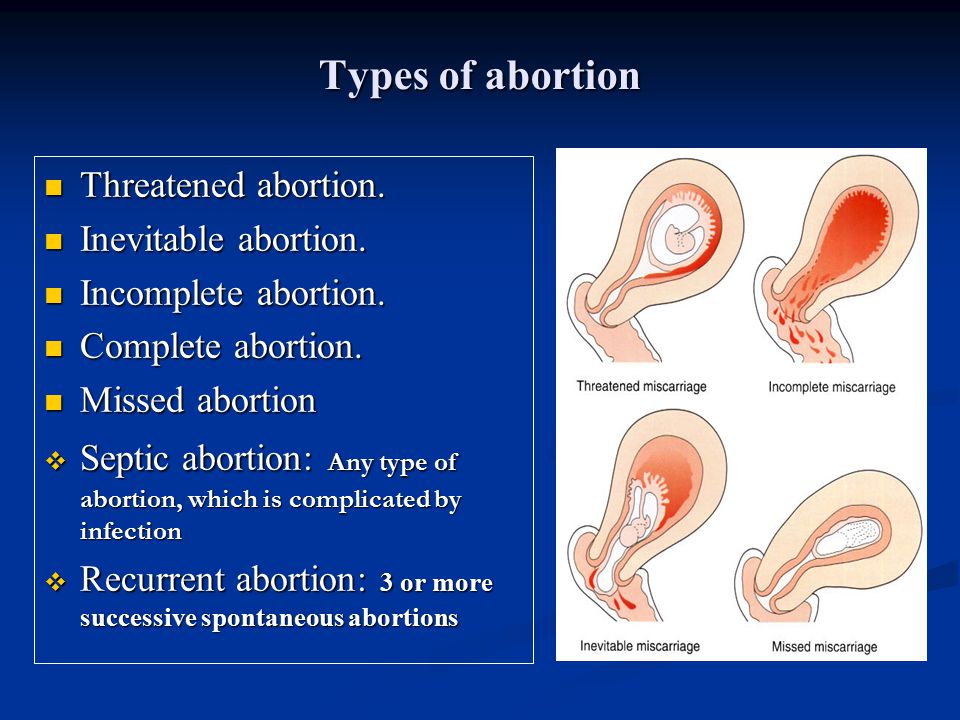 It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
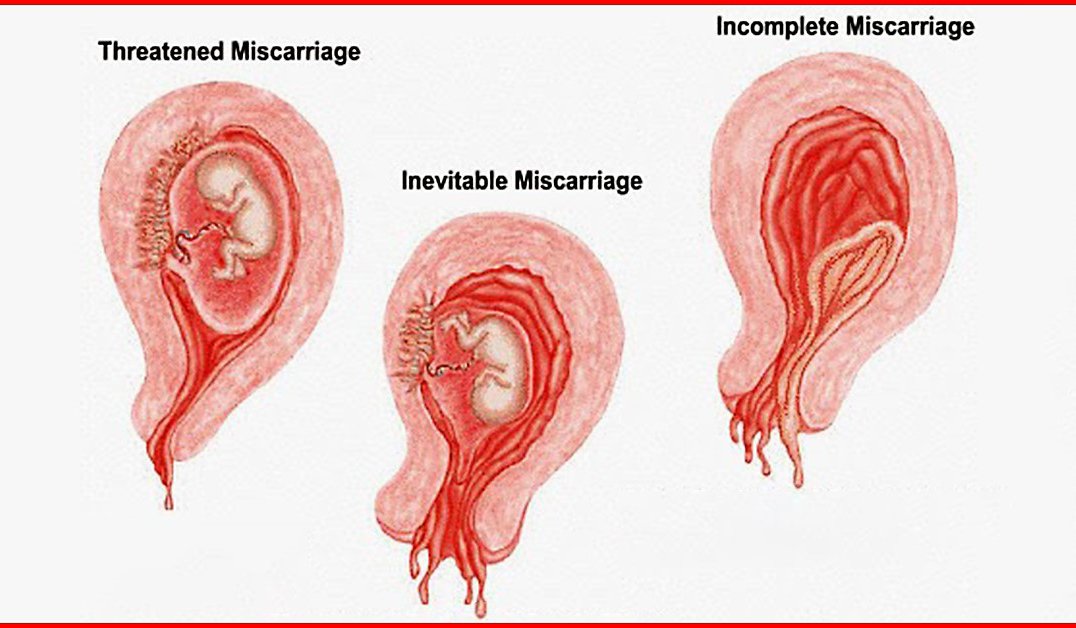
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen.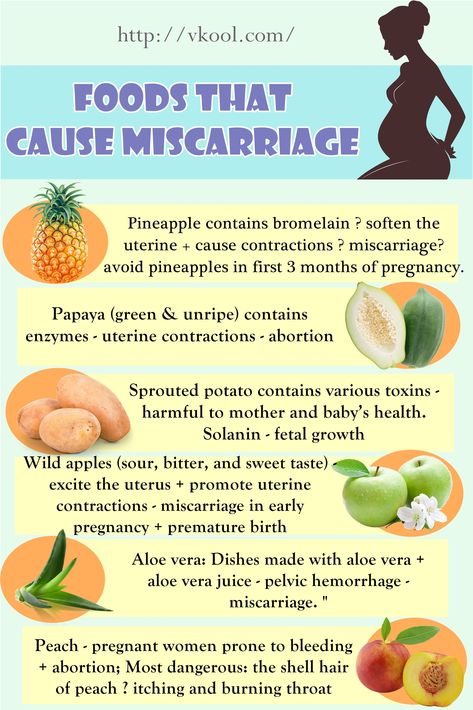 Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily. The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it. Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean.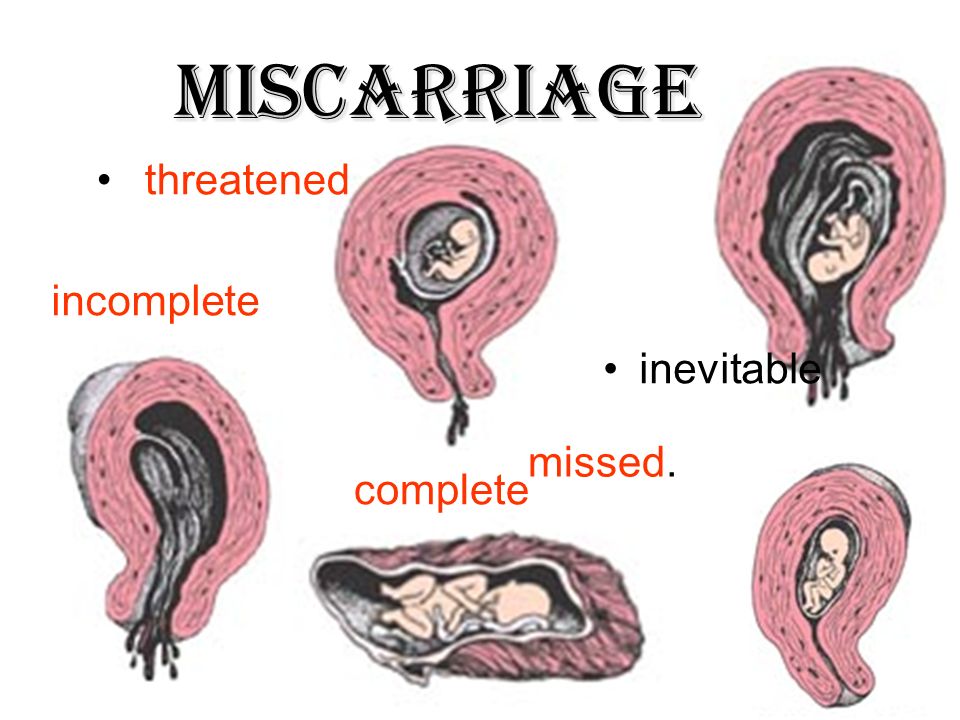 If you look closely, you might be able to see where the eyes, arms and legs were forming.
If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.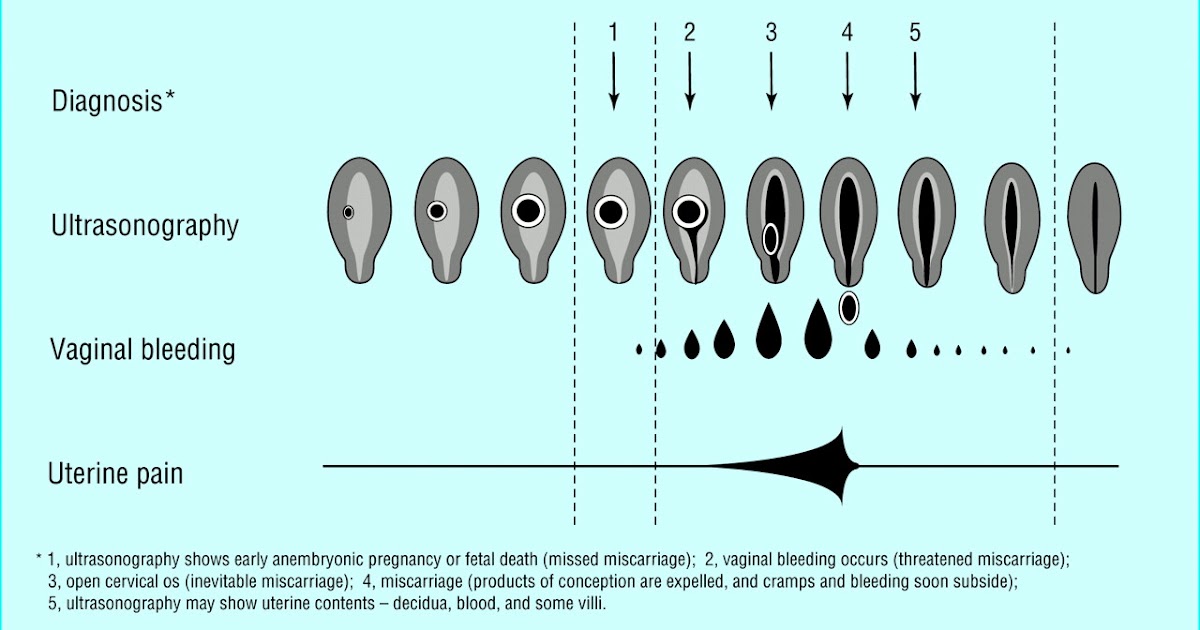
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient.com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- What happens after miscarriage
- Miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.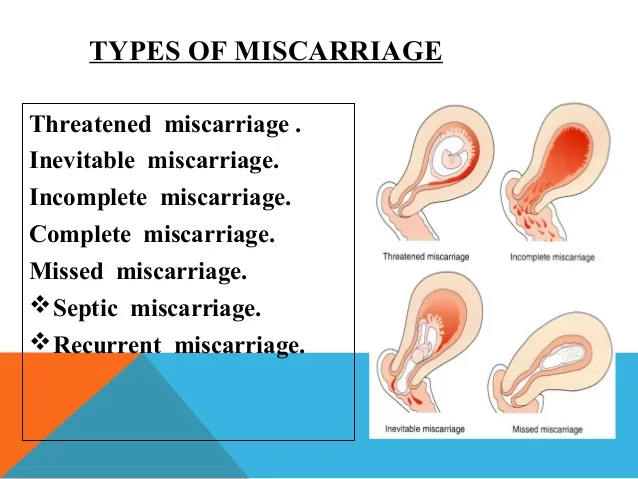
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Early miscarriage - symptoms and how to prevent it
The term "early miscarriage" refers to a spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body. nine0003
However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body. nine0003
In addition, a curious pattern was revealed: more often than a natural one, a pregnancy induced artificially ends in a miscarriage. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.
Why can an early miscarriage occur?
Here are the most common causes, each of which significantly increases the risk of miscarriage: nine0003
- the expectant mother has certain infectious diseases, as well as STDs;
- intoxication of a woman's body for various reasons, including as a result of her living in an ecologically unfavorable region;
- all kinds of metabolic disorders in the body;
- hormonal disruptions, including those caused by a malfunction of the thyroid gland;
- various neoplasms in the uterus and others, as well as the cervix, pathologies; nine0012
- maintenance by the future mother of a life far from a healthy lifestyle.
 May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition;
May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition; - obesity;
- immune status disorders;
- cardiac diseases;
- diabetes mellitus;
- too early for pregnancy or, conversely, the patient's overly mature age at times increases the risk of miscarriage; nine0012
- all kinds of pathologies of chromosomes and genes;
- prolonged exposure to stress or severe psycho-emotional trauma in a woman.
The timing of a miscarriage may depend, among other things, on the patient's genetic predisposition to miscarriage. Finally, often its specific cause remains unexplained to the end.
Symptoms of miscarriage
A pregnant woman should urgently seek medical help if she has the following warning signs: nine0003
- bleeding from the vagina;
- spotting discharge from the genital tract. They can have both light pink and intense red or brownish tint;
- convulsions;
- severe pain in the lumbar region;
- abdominal pain, etc.
All of the above signs can be symptoms of a miscarriage. Timely provision of qualified medical care is the key to maintaining pregnancy. nine0003
Life after miscarriage
If a woman could not bear the pregnancy - an early miscarriage crossed out all her plans - then she needs to calm down and take all measures to prevent such complications in the future. Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment. nine0003
Gynecologists of the corresponding department of our private clinic in Ryazan will help you find out what could have caused the miscarriage, as well as make recommendations on how to prepare for pregnancy. They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped! nine0003
They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped! nine0003
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection? nine0012
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child. nine0003
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child. nine0003
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, injury, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same. nine0003
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same. nine0003
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss. nine0003
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss. nine0003
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it. nine0003
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful. nine0003
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage. nine0003
nine0003
Hormone imbalance in a woman's body is likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time. nine0003
An excess of male sex hormones that suppress the production of estrogens and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png)
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor. nine0003
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 o C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections. nine0003
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections. nine0003
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect. nine0003
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect. nine0003
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth. nine0003
In isthmic-cervical insufficiency, there is only one method of treatment - a mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor. nine0003
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor. nine0003
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children. nine0003
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriage due to impaired hemostasis
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis). nine0003
Disorders of the blood coagulation system leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (a tendency to bleed). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can manifest themselves even in childhood in the form of increased bleeding during cuts, extractions of teeth, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop. nine0003
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of a blood clotting disorder.