Cerebral palsy diagnosis in utero
Cerebral palsy | Pregnancy Birth and Baby
beginning of content7-minute read
Listen
What is cerebral palsy?
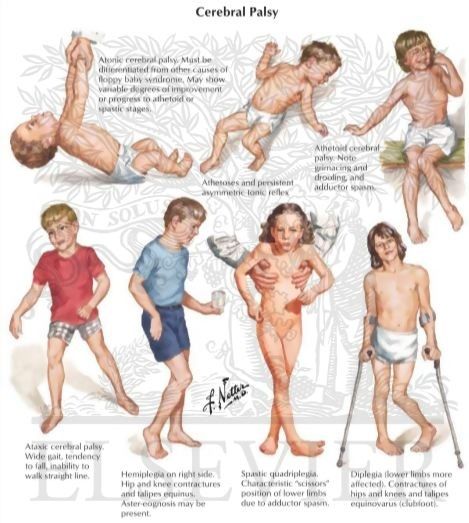
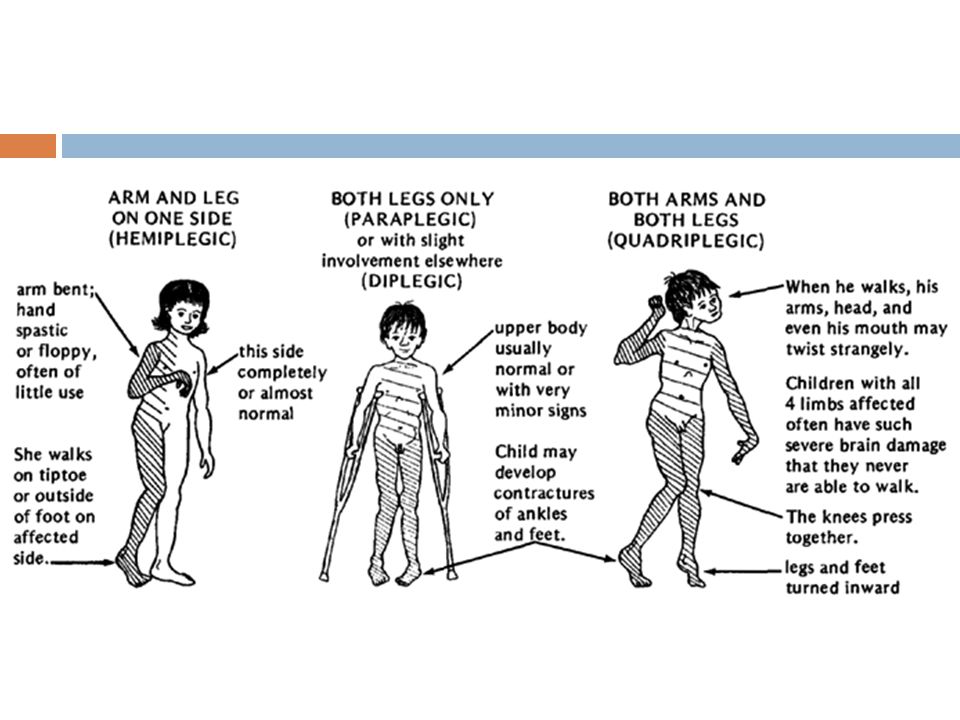
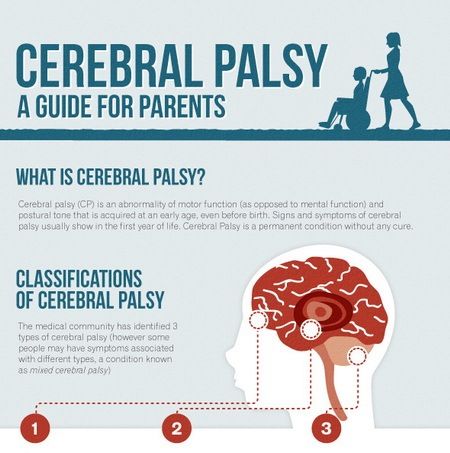
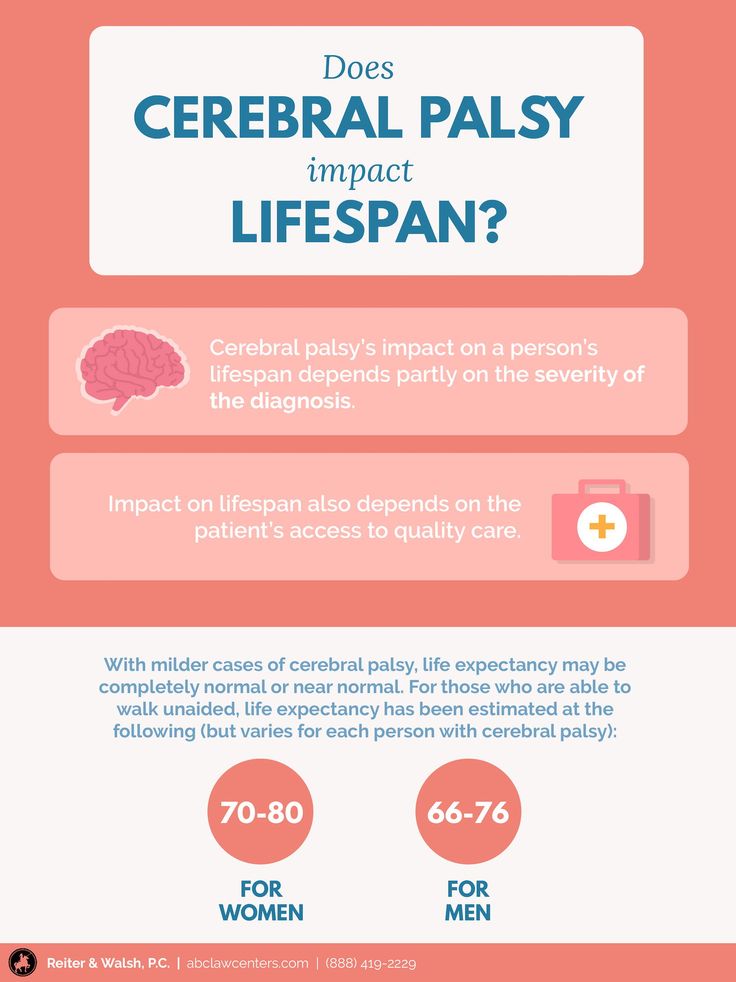
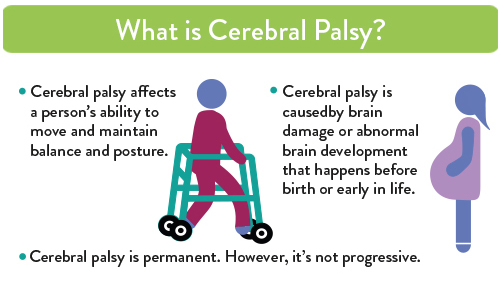
Cerebral palsy is the term for a group of disorders. They can affect muscle tone, posture and/or movement. They can start before, at or after birth.
Cerebral palsy is a life-long disorder that affects people in many ways. The type and severity of cerebral palsy can vary. It can impact a person’s function in different ways.
Cerebral palsy can affect your child’s:
- body movement
- ability to control their muscles
- coordination
- reflexes
- posture
- balance
In Australia, 1 in 500 babies are born with cerebral palsy.
Some children with cerebral palsy might also have:
- epilepsy
- hearing difficulties
- learning difficulties
- visual difficulties
- intellectual impairments
Other children might have no other problems.
There is no cure for cerebral palsy. But there are treatments and therapies that can improve your child’s quality of life.
What causes cerebral palsy?
Cerebral palsy is probably not one condition with one cause. It is a term that covers many different conditions with many different causes.
For many years, people believed that a lack of oxygen during birth caused cerebral palsy. This seems less likely now.
Researchers believe that a chain of events may combine to damage a baby’s developing brain, rather than one single cause.
Risk factors for cerebral palsy include:
- being born early (premature or preterm)
- low birthweight
- rubella and other viral infections during pregnancy
- bacterial infections during pregnancy
- the baby not getting enough oxygen or nutrients in the womb
- the baby having a blood type that is incompatible with the mother
- injury to the brain
- your baby having a stroke
- severe jaundice shortly after birth
Most cases of cerebral palsy in Australia, are caused by a brain injury. This can happen either during pregnancy or before 1 month of age.
This can happen either during pregnancy or before 1 month of age.
Stroke is the most common cause of cerebral palsy in babies older than 1 month of age. The stroke might happen suddenly or be a complication of a heart condition or surgery.
It isn’t always possible to work out why your child has cerebral palsy.
How do I know if my child has cerebral palsy?
There is no single test to diagnose cerebral palsy. It can’t be detected during pregnancy. Good medical care during pregnancy and birth can help to reduce the risk that your baby has cerebral palsy.
Cerebral palsy might take some time to show itself. The condition is often noticed when your baby or toddler doesn’t meet their expected development milestones. Babies with cerebral palsy might have:
- muscle stiffness and spasms
- low muscle tone so that they feel ‘floppy’ when picked up
Other signs to look out for include your baby:
- being unable to hold up their own head at the right stage
- being unable to sit up or roll over by 6 months
- having feeding or swallowing difficulties
- preferring to use one side of their body
Toddlers with cerebral palsy may not be walking by 12 to 18 months or speaking simple sentences by 2 years of age.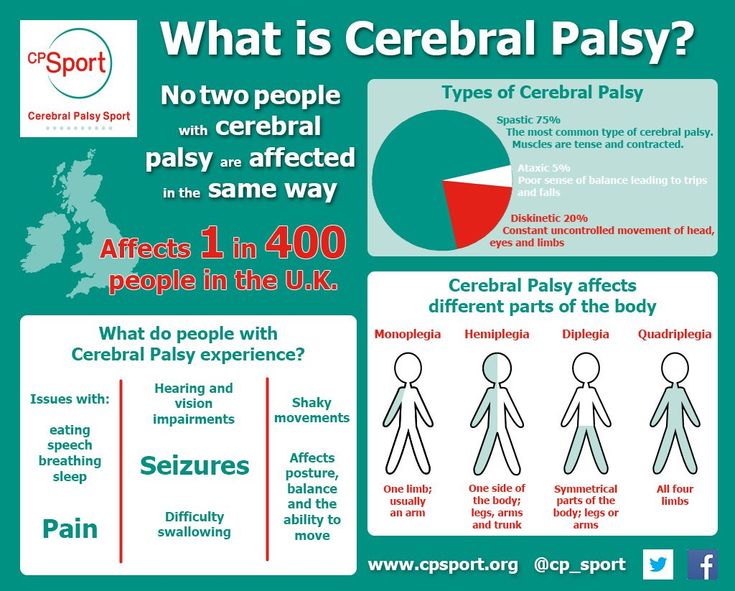
How is cerebral palsy diagnosed?
Australia offers regular health checks for babies and young children. The child health nurses and doctors who run these checks are good at spotting delays in development. But there are many normal variations between children. Talk to your doctor if you are concerned about your child.
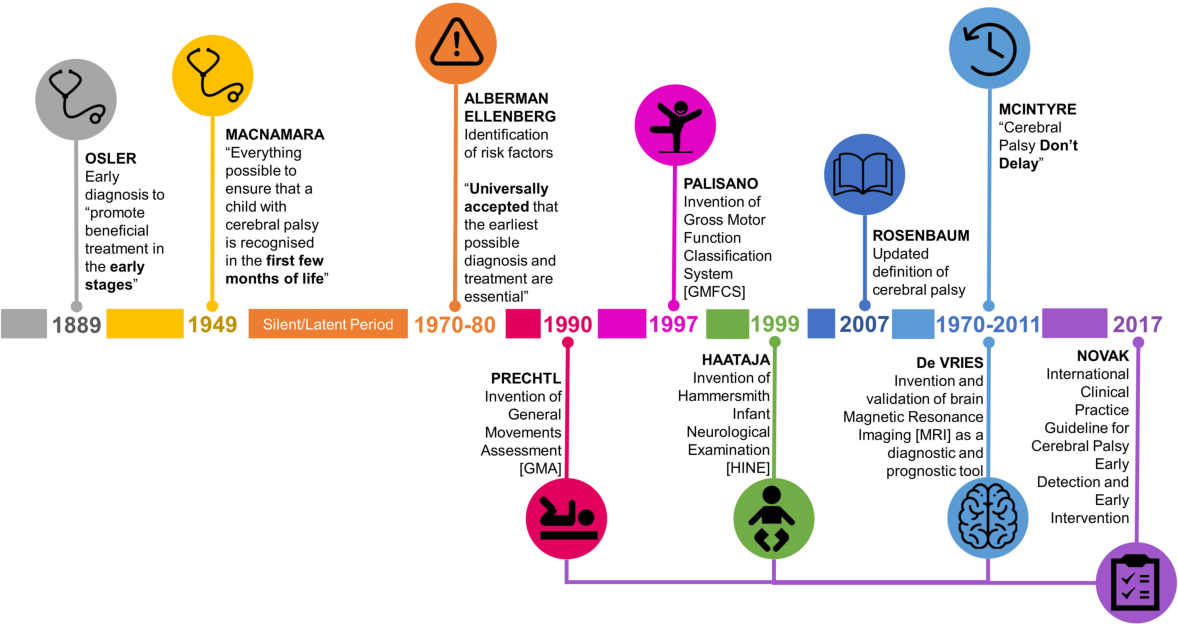
A General Movements Assessment is an examination that can be done from birth until 5 months of age. It is a good predictor of cerebral palsy. In Australia, a growing number of doctors and allied health professionals have been trained to conduct a General Movements Assessment.
Your doctor may also recommend a brain scan such as an MRI scan or a CT scan.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is cerebral palsy treated?
Possible treatment options include:
- management of hearing and vision impairment
- medicines
- occupational therapy
- physiotherapy
- speech therapy, which can help with eating and drinking as well as speech problems
- surgery
Your child might need specialist equipment, for example, a walking frame, a wheelchair, special seating, or special footwear.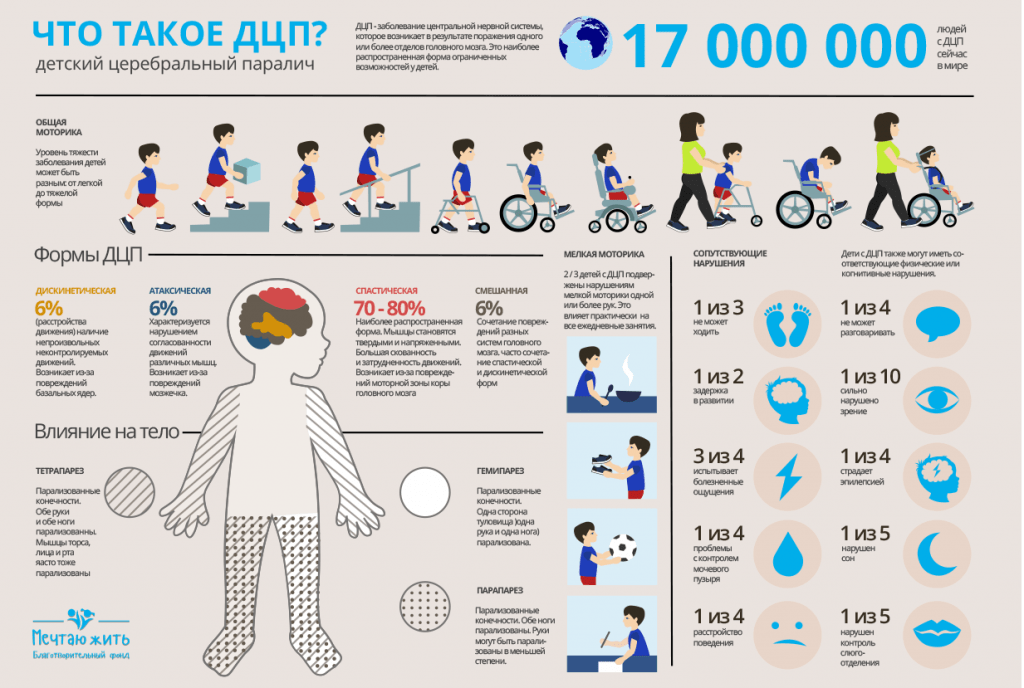
The Cerebral Palsy Alliance has a detailed list of possible treatments.
Can cerebral palsy be prevented?
Cerebral palsy can’t be prevented or cured.
However, some public health measures help to prevent cerebral palsy. These include:
- car seatbelts
- pool fencing
- rubella vaccinations
There are also a number of interventions for high-risk infants. These can reduce the risk or severity of cerebral palsy. Three examples are:
- A course of steroids given to mothers who are at risk of a preterm birth. Steroids can reduce the risk of preterm babies having cerebral palsy.
- Magnesium sulphate given to mothers who are at high risk of very preterm birth can prevent cerebral palsy.
Cooling newborn babies who have suffered a brain injury due to a lack of oxygen at birth. This can reduce the impact of the brain injury.
Caring for a child with cerebral palsy
It can be very upsetting to discover that there is something wrong with your baby’s health.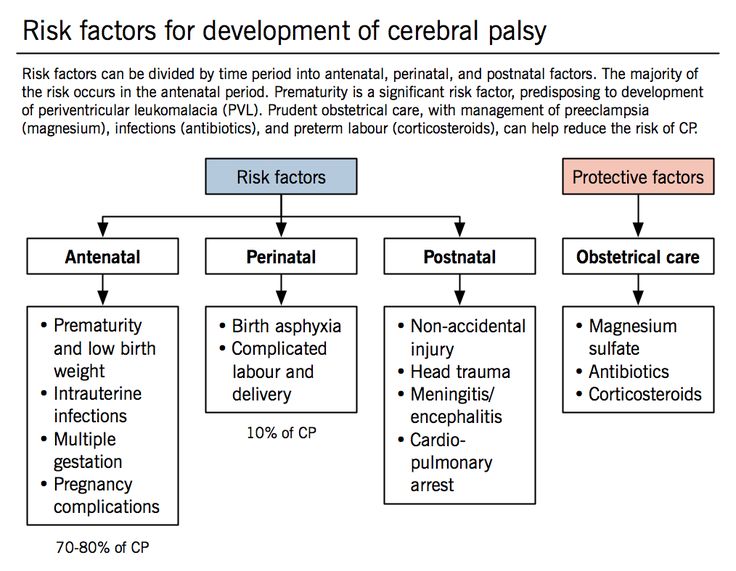
There are many different treatments and interventions to help people with cerebral palsy. Some people need a little help, and some need a lot of help. There is a range of support for you and your family.
A team of doctors and therapists can help you and your child.
Parenting a child with a disability can present challenges and you will need support.
You can apply for various types of financial support. You might also be able to get practical help through the National Disability Insurance Scheme.
Visit Carer Gateway for more information about free services and support for carers.
You can also find information about cerebral palsy from:
- Cerebral Palsy Australia
- Cerebral Palsy Alliance
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
UpToDate (Cerebral palsy: Epidemiology, etiology, and prevention), Cerebral Palsy Alliance (About cerebral palsy), Cerebral Palsy Alliance (Signs and symptoms of cerebral palsy), Cochrane library (Antenatal and intrapartum interventions for preventing cerebral palsy: an overview of Cochrane systematic reviews), Cochrane library (Neonatal interventions for preventing cerebral palsy: an overview of Cochrane Systematic Reviews)Learn more here about the development and quality assurance of healthdirect content.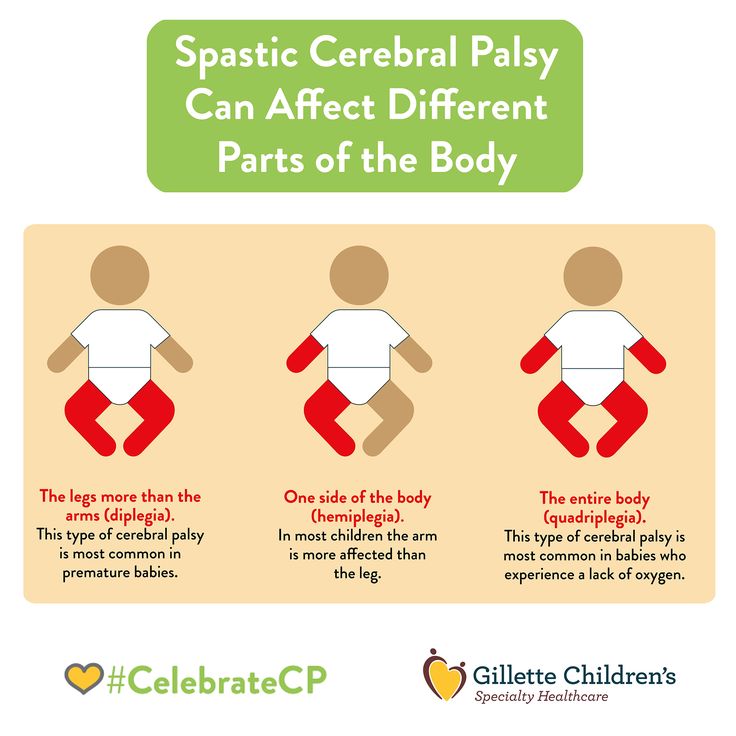
Last reviewed: August 2022
Back To Top
Related pages
- Disability and chronic illness
- What is a congenital disorder?
Need more information?
What is cerebral palsy? | Cerebral Palsy Alliance
Cerebral Palsy Alliance is a non-profit that provides services to thousands of people with a disability and their families. Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Read more on Cerebral Palsy Alliance website
Cerebral palsy | Novita
About cerebral palsy Whilst cerebral palsy is not a progressive condition, changes may occur over time
Read more on Novita Services website
Cerebral palsy in children: a guide
What is cerebral palsy? Get key information about cerebral palsy symptoms, assessment and diagnosis, plus a guide to early intervention funding and support.
Read more on raisingchildren.net.au website
Cerebral palsy | Cerebral Palsy Alliance
Cerebral palsy (CP) is a physical disability that affects movement and posture. It is a permanent life-long condition, but generally does not worsen over time.
Read more on Cerebral Palsy Alliance website
Interventions and Therapies | Cerebral Palsy Alliance
Cerebral Palsy Alliance is a non-profit that provides services to thousands of people with a disability and their families. Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Read more on Cerebral Palsy Alliance website
CPA Telepractice | Cerebral Palsy Alliance
Cerebral Palsy Alliance is a non-profit that provides services to thousands of people with a disability and their families.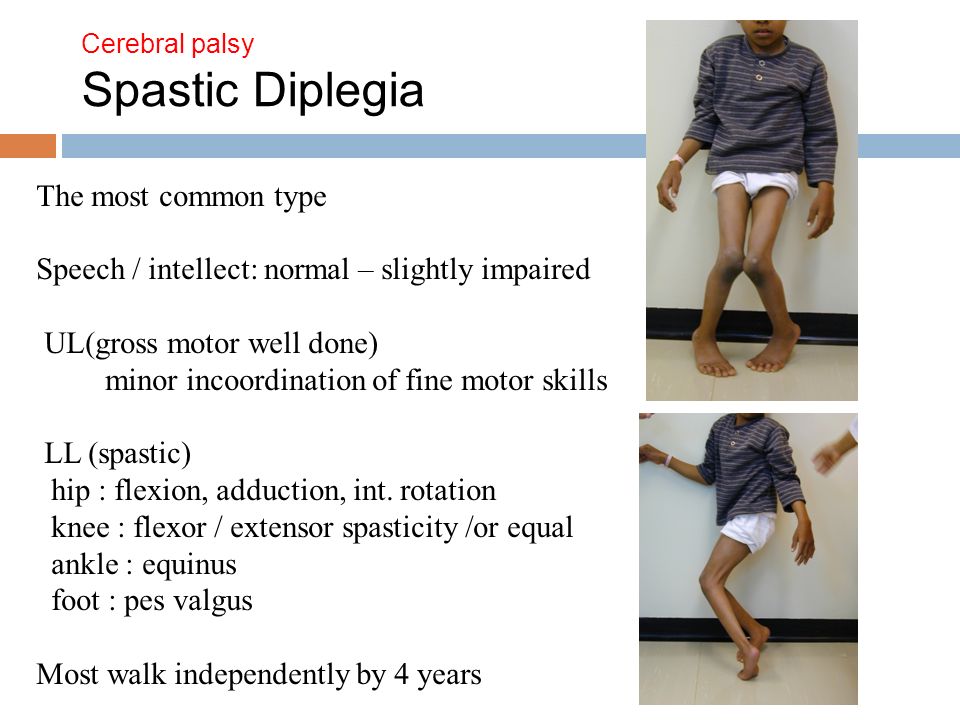 Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Read more on Cerebral Palsy Alliance website
Early Childhood Intervention | Cerebral Palsy Alliance
Cerebral Palsy Alliance is a non-profit that provides services to thousands of people with a disability and their families. Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Read more on Cerebral Palsy Alliance website
All Services and programs | Cerebral Palsy Alliance
Cerebral Palsy Alliance is a non-profit that provides services to thousands of people with a disability and their families. Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Read more on Cerebral Palsy Alliance website
Cerebral Palsy (CP) | Sydney Children's Hospitals Network
What is Cerebral Palsy (CP)? Cerebral palsy, commonly called CP, is the name used to describe a group of conditions that cause problems with movement
Read more on Sydney Children's Hospitals Network website
Resources in other languages | Cerebral Palsy Alliance
Cerebral Palsy Alliance is a non-profit that provides services to thousands of people with a disability and their families.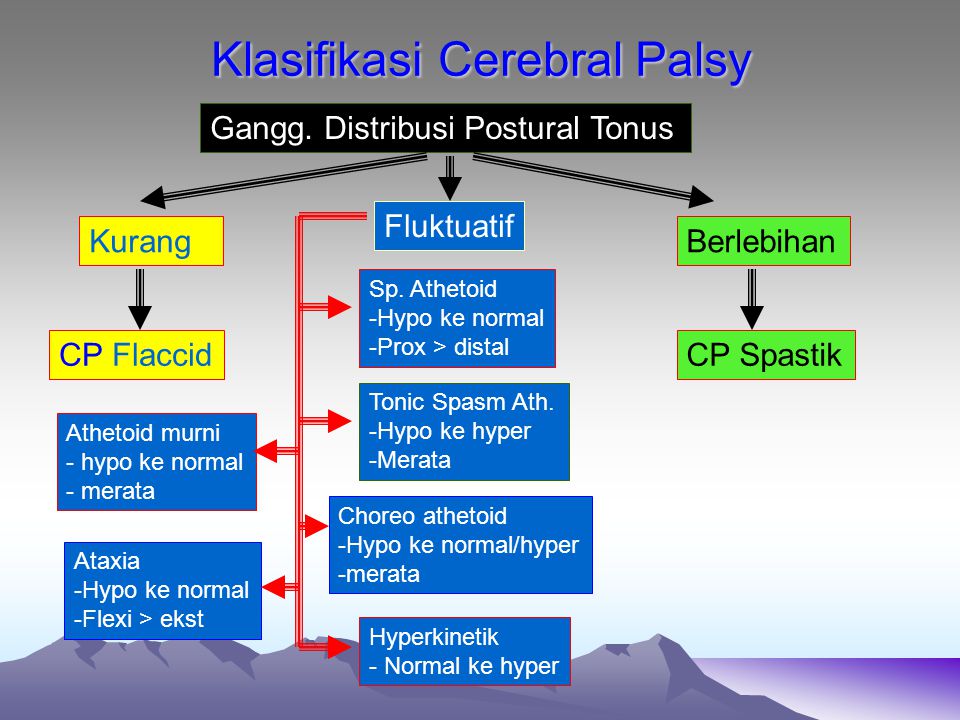 Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Cerebral palsy (CP) is a physical disability that affects the way that a person moves.
Read more on Cerebral Palsy Alliance website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKThis information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.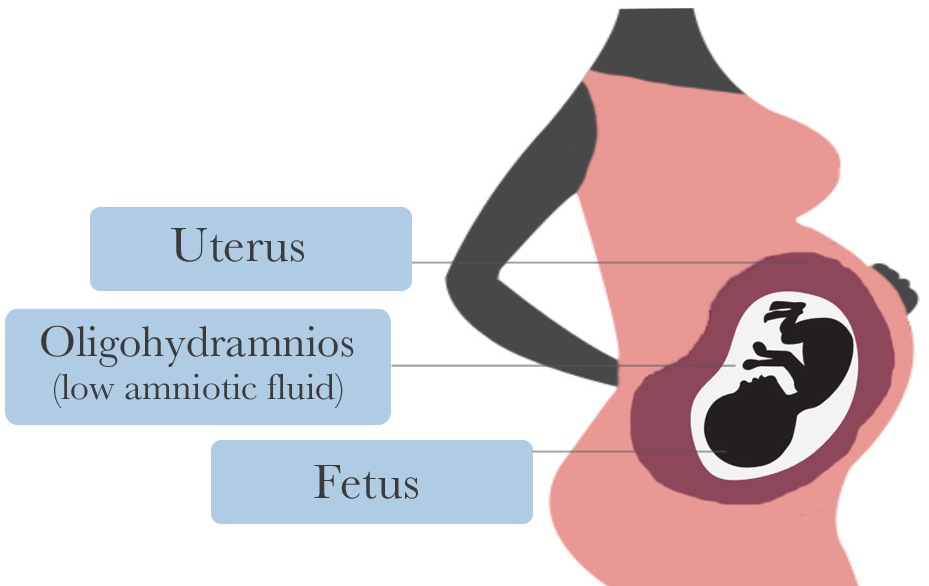
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Causes and Risk Factors of Cerebral Palsy
Cerebral palsy (CP) is caused by abnormal development of the brain or damage to the developing brain that affects a child’s ability to control his or her muscles. There are several possible causes of the abnormal development or damage. People used to think that CP was mainly caused by lack of oxygen during the birth process. Now, scientists think that this causes only a small number of CP cases.
Now, scientists think that this causes only a small number of CP cases.
The abnormal development of the brain or damage that leads to CP can happen before birth, during birth, within a month after birth, or during the first years of a child’s life, while the brain is still developing.
Congenital CP
CP related to abnormal development of the brain or damage that happened before or during birth is called congenital CP. The majority of CP (85%–90%) is congenital. In many cases, the specific cause is not known.
Risk Factors for Congenital CP
Some things increase the chance that a child will have CP. These are called risk factors. It is important to remember that having a risk factor does not mean that a child will have CP. Some of the risk factors for congenital CP are:
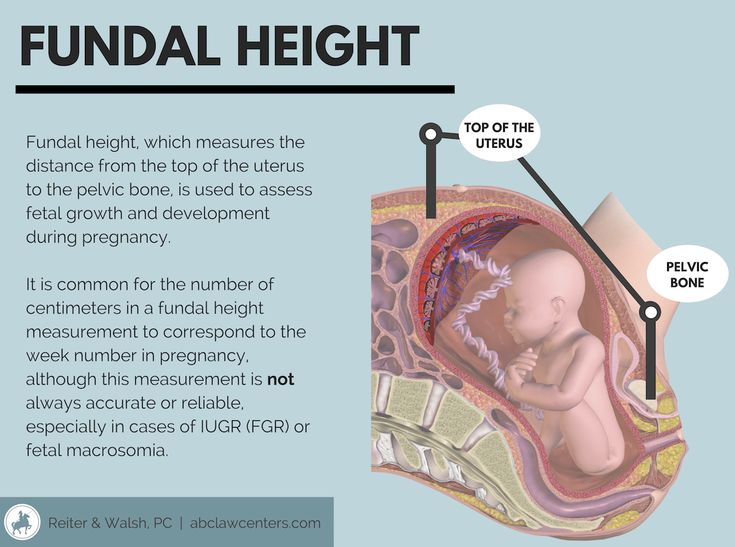
- Low birthweight―Children who weigh less than 5 1/2 pounds (2,500 grams) at birth, and especially those who weigh less than 3 pounds, 5 ounces (1,500 grams) have a greater chance of having CP.
 Read articleexternal icon
Read articleexternal icon - Premature birth―Children who were born before the 37th week of pregnancy, especially if they were born before the 32nd week of pregnancy, have a greater chance of having CP. Intensive care for premature infants has improved a lot over the past several decades. Babies born very early are more likely to live now, but many have medical problems that can put them at risk for CP. Read articleexternal icon
- Multiple births―Twins, triplets, and other multiple births have a higher risk for CP, especially if a baby’s twin or triplet dies before birth or shortly after birth. Some, but not all of this increased risk is due to the fact that children born from multiple pregnancies often are born early or with low birthweight, or both. Read summaryexternal icon
- Assisted reproductive technology (ART) infertility treatments―Children born from pregnancies resulting from the use of some infertility treatments have a greater chance of having CP. Most of the increased risk is explained by preterm delivery or multiple births, or both; both preterm delivery and multiple births are increased among children conceived with ART infertility treatments.
 Read articleexternal icon, Read summaryexternal icon
Read articleexternal icon, Read summaryexternal icon - Infections during pregnancy―Infections can lead to increases in certain proteins called cytokines that circulate in the brain and blood of the baby during pregnancy. Cytokines cause inflammation, which can lead to brain damage in the baby. Fever in the mother during pregnancy or delivery also can cause this problem. Some types of infection that have been linked with CP include viruses such as chickenpox, rubella (german measles), and cytomegalovirus (CMV), and bacterial infections such as infections of the placenta or fetal membranes, or maternal pelvic infections. Read summaryexternal icon, Read articleexternal icon
- Jaundice and kernicterus― Jaundice is the yellow color seen in the skin of many newborns. Jaundice happens when a chemical called bilirubin builds up in the baby’s blood. When too much bilirubin builds up in a new baby’s body, the skin and whites of the eyes might look yellow. This yellow coloring is called jaundice.
 When severe jaundice goes untreated for too long, it can cause a condition called kernicterus. This can cause CP and other conditions. Sometimes, kernicterus results from ABO or Rh blood type difference between the mother and baby. This causes the red blood cells in the baby to break down too fast, resulting in severe jaundice.
When severe jaundice goes untreated for too long, it can cause a condition called kernicterus. This can cause CP and other conditions. Sometimes, kernicterus results from ABO or Rh blood type difference between the mother and baby. This causes the red blood cells in the baby to break down too fast, resulting in severe jaundice. - Medical conditions of the mother―Mothers with thyroid problems, intellectual disability, or seizures have a slightly higher risk of having a child with CP. Read summaryexternal icon
- Birth complications―Detachment of the placenta, uterine rupture, or problems with the umbilical cord during birth can disrupt oxygen supply to the baby and result in CP. Read summaryexternal icon
Preventing CP
In many cases, the cause or causes of congenital CP aren’t fully known, which means that currently little can be done to prevent it. CP related to genetics is not preventable. However, there are actions people can take before and during pregnancy, as well as after birth that might help reduce the risk of developmental problems, including CP.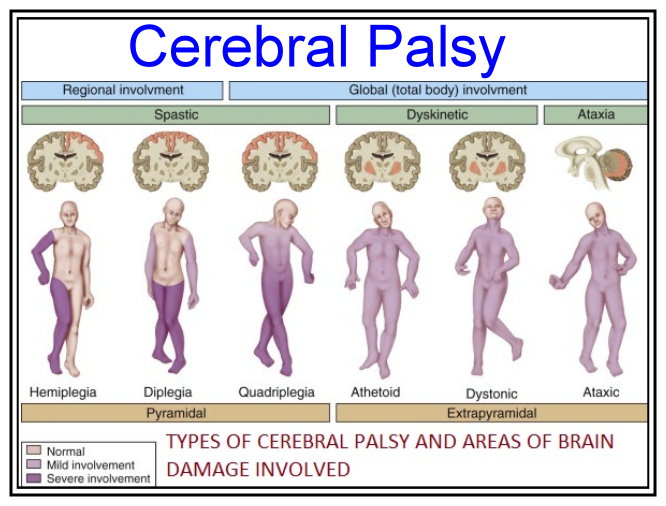
Taking steps to help ensure a healthy pregnancy can help prevent developmental problems, including CP. Acquired CP often is related to an infection or injury, and some of these cases can be prevented.
Before Pregnancy
- Be as healthy as possible before pregnancy. Make sure that any infections in the mother are treated and health conditions are in control, ideally before pregnancy occurs.
- Get vaccinated for certain diseases (such as chickenpox and rubella) that could harm a developing baby. It is important to have many of these vaccinations before becoming pregnant.
- If assistive reproductive technology (ART) infertility treatments are used to get pregnant, consider ways to reduce the chance of a multiple pregnancy (twins, triplets, or more), such as transferring only one embryo at a time.
During Pregnancy
- Learn how to have a healthy pregnancy.
- Get early and regular prenatal care, both for your health and for that of your developing baby.
- Wash your hands often with soap and water to help reduce the risk of infections that might harm your developing baby.
- Contact your health care provider if you get sick, have a fever, or have other signs of infection during pregnancy.
- A flu shot is your best protection against serious illness from the flu. A flu shot can protect pregnant women and their unborn babies, both before and after birth. Flu shots have not been shown to cause harm to pregnant women or their babies.
- If there is a difference in the blood type or Rh incompatibility between mother and baby it can cause Jaundice and kernicterus. Women should know their blood type and talk to their doctor about ways to prevent problems. Doctors can treat the mother with Rh immune globulin (“Rhogam”) when she is 28 weeks pregnant and again shortly after giving birth to prevent kernicterus from occurring.
- Talk to your doctor about ways to prevent problems if you are at risk for preterm delivery.
 Research has shown that taking magnesium sulfate before anticipated early preterm birth reduces the risk of CP among surviving infants. (1,2,3,4)
Research has shown that taking magnesium sulfate before anticipated early preterm birth reduces the risk of CP among surviving infants. (1,2,3,4)
After the Baby is Born
- Learn how to help keep your baby healthy and safe after birth.
- Any baby can get jaundice. Severe jaundice that is not treated can cause brain damage, called kernicterus. Kernicterus is a cause of CP that potentially can be prevented. Your baby should be checked for jaundice in the hospital and again within 48 hours after leaving the hospital. Ask your doctor or nurse about a jaundice bilirubin test. In addition, steps can be taken to prevent kernicterus that is caused by Rh blood type incompatibility between the mother and baby.
- Make sure your child is vaccinated against infections that can cause meningitis and encephalitis, including Haemophilus influenzae type B (HiB vaccine) and Streptococcus pneumoniae (pneumococcal vaccine).
- Take steps to prevent injuries:
- Buckle your child in the car using an infant or child car seat, booster seat, or seat belt (according to the child’s height, weight, and age).
- Make living areas safer for children by using window guards to keep young children from falling out of open windows and using safety gates at the top and bottom of stairs.
- Make sure the surface on your child’s playground is made of a shock-absorbing material, such as hardwood mulch or sand.
- Carefully watch young children at all times around bathtubs, swimming or wading pools, and natural bodies of water. Adults watching kids near water should avoid distracting activities like using a computer or handheld device, reading, or talking on the phone.
- Make sure your child wears a helmet for activities like riding a bike.
- Never hit, throw, shake, or hurt a child.
- Buckle your child in the car using an infant or child car seat, booster seat, or seat belt (according to the child’s height, weight, and age).
For More Information
- American Academy of Pediatrics Healthy Children / Cerebral Palsyexternal icon
- National Institute of Neurological Disorders and Stroke (NINDS) Cerebral Palsy Informationexternal icon
References
- Doyle LW, Crowther CA, Middleton P, Marret S.
 Antenatal magnesium sulfate and neurologic outcome in preterm infants: a systematic review. Obstet Gynecol. 2009 Jun;113(6):1327-33.
Antenatal magnesium sulfate and neurologic outcome in preterm infants: a systematic review. Obstet Gynecol. 2009 Jun;113(6):1327-33. - Magnesium sulfate before anticipated preterm birth for neuroprotection. Committee Opinion No. 455. American College of Obstetricians and Gynecologists. Obstet Gynecol 2010;115:669–71.
- Crowther CA, Middleton PF, Voysey M, et al (2017). Assessing the neuroprotective benefits for babies of antenatal magnesium sulphate: An individual participant meta-analysis. PLoS Med, 14(10):e1002398.
- Magnesium sulfate use in obstetrics. Committee Opinion No. 652. American College of Obstetricians and Gynecologists. Obstet Gynecol 2016;127(1):e52-3.
Infantile cerebral palsy in the "fetters" of intrauterine infection.
In the last ten years, there has been an increase in the frequency of congenital infections, predominantly of viral etiology. High infant mortality, as well as childhood disability as a result of infectious pathology, are a serious demographic problem. Infection of the fetus and the infectious process can begin in the prenatal period, during childbirth, or postnatally. These are the so-called perinatal or intrauterine infections (IUI). The most common IUIs are referred to as the TORCH syndrome. nine0004
Infection of the fetus and the infectious process can begin in the prenatal period, during childbirth, or postnatally. These are the so-called perinatal or intrauterine infections (IUI). The most common IUIs are referred to as the TORCH syndrome. nine0004
The abbreviation TORCH is used to refer to a range of diseases, including toxoplasmosis (Toxoplasmosis), syphilis (Other), rubella (Rubella), cytomegalovirus infection (Cytomegalovirus) and herpes infection (Herpes simplex virus).
In many countries this abbreviation has been changed to STARCH to include human immunodeficiency virus (AIDS) infection. The danger of TORCH syndrome and other viral infections lies in the fact that they cause 80% of congenital malformations in children. Among them, the leading place is occupied by damage to the central nervous system, congenital heart and kidney defects. It has been established that infection of the fetus in the first trimester of pregnancy leads to the development of micro-, hydrocephalus, heart defects, gastrointestinal tract, genitourinary system, skeleton, cataracts, and deafness. nine0004
nine0004
Infection in the II and III trimesters causes hepatosplenomegaly, anemia, jaundice, malnutrition, pneumonia, meningocephalitis, and sepsis in the fetus.
In the Medical Center C0RTEX in 2008-2013 and the first half of 2014, 1009 children were examined and treated with cerebral palsy, mental retardation, with delays in the psychoverbal and motor areas of unspecified genesis. The age of the children ranged from 9 months to 20 years. All children underwent: CEEG, EP, MRI, (PET performed according to indications) of the brain, ultrasound of internal organs, clinical blood and urine tests according to generally accepted methods, testing for TORCH-complex infection by polymerase chain reaction and enzyme immunoassay with the determination of immunoglobulins G and M. nine0004
All children had pre- and perinatal anamnesis: the threat of abortion was noted in 69% of mothers, and in half of them in the 1st and 2nd semesters, severe toxicosis -41%, immunoconflict -23%, chronic intrauterine hypoxia fetus - 73%, 31% of mothers had an exacerbation of genital herpes, 15% of mothers were treated for infertility, more than 30% of mothers had acute respiratory viral infections and 5% of toxoplasmosis during pregnancy.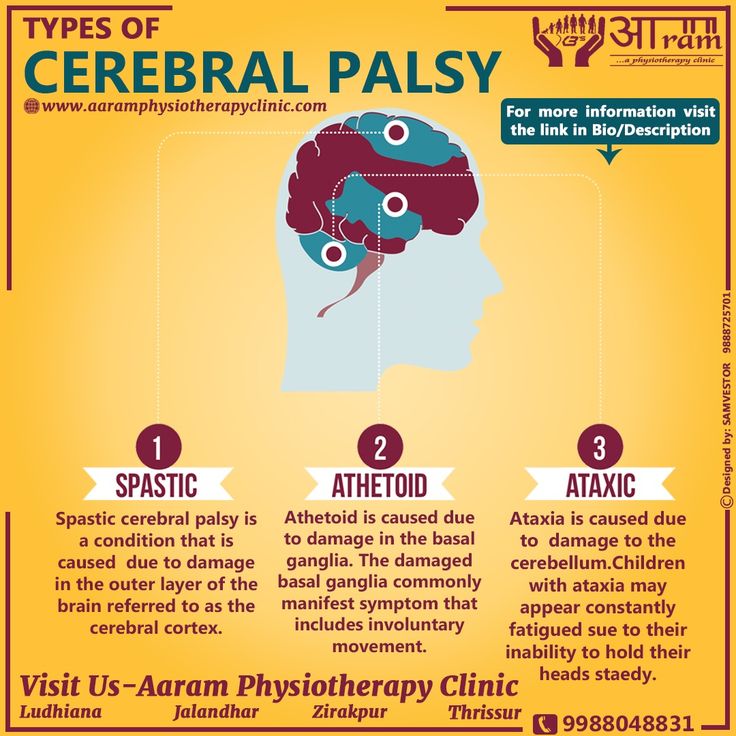 Signs of placental insufficiency were observed in 65% of mothers, and exacerbation of chronic ureoplasmosis, chlamydia, mycoplasmosis was observed in 40% of mothers. nine0004
Signs of placental insufficiency were observed in 65% of mothers, and exacerbation of chronic ureoplasmosis, chlamydia, mycoplasmosis was observed in 40% of mothers. nine0004
Most often, in the examined patients (more than 45%), chronically persistent cytomegalovirus and herpetic infection with symptoms of sluggish leukoencephalitis were verified, in -21% - neuroinfection caused by listeriosis, ureaplasmosis, chlamydia. In 18% of cases, children suffered intrauterine toxoplasmosis, candidiasis, mycoplasmosis, complicated by urosepsis, pneumonia with pulmonary edema, gastric and intestinal bleeding, as well as meningitis and meningoencephalitis. Post-vaccination lesions of the brain were detected in 6% of patients. 5% were diagnosed with acute meningoencephalitis and 3% with acute radiculoanglioneuritis caused by the association of herpetic viruses (HSV, Varicella-Zoster, Epstein-Barr). nine0004
A third of children were diagnosed with intrauterine pneumonia, malnutrition, 40% with neonatal jaundice, hepato-splenomegaly, thymomegaly and subclinical thyroid dysfunction, heart and connective tissue defects were found in 10% of patients, 6% had malformations of the genitourinary system, 30 % pathology of the organs of vision (glaucoma, microphthalmia, coloboma, atrophy of the optic nerves), etc.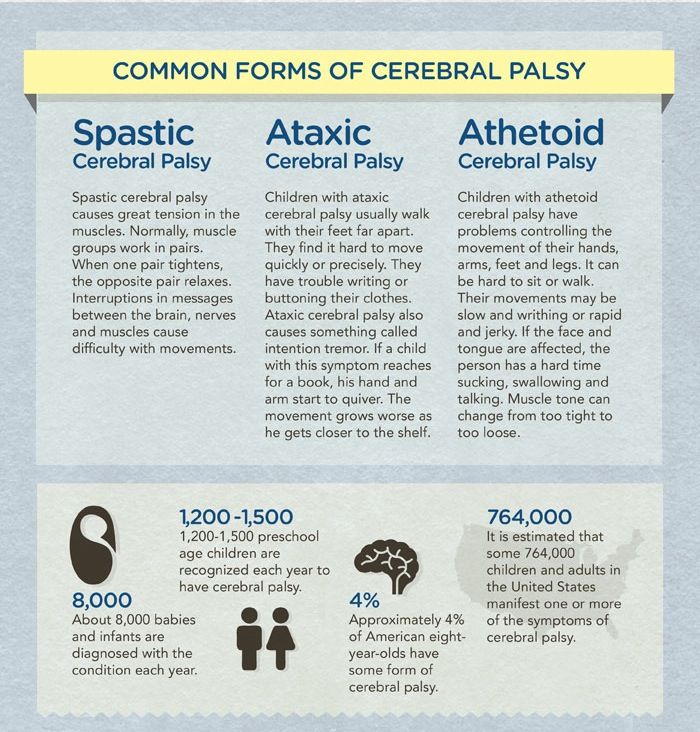 .
.
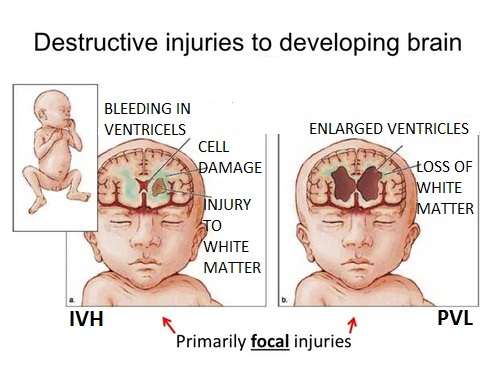
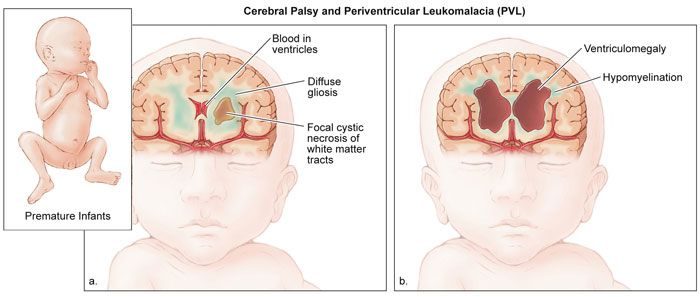
According to neuroimaging data, 56% of the examined patients were found to have subcortical cysts and cysts in the parechima of the brain, 42% — subatrophy of the cerebral cortex, ventriculomegaly — 46%, foci of gliosis and periventricular leukomaalacia — 52%, thinning of the corpus callosum — 27%, congenital anomalies of the brain -11%, intraventricular hemorrhage 65% and occlusion of the CSF tract - 2%. nine0004
In the majority of children with IUI, the formation of a gross neurological defect was observed - up to 77% of the total number of patients, in the form of: tetraparesis, paraparesis, hemiparesis, spastic diplegia, hemiplegia, statomotor and sensitive ataxia. Intellectual and behavioral disorders were observed in 45%, episyndrome - in 55%. With a "lighter" outcome of IUI, in 33% of cases, MMD syndrome (minimal brain dysfunctions) was detected in the form of hyperactivity with attention deficit. These violations were distinguished by the persistence of manifestations and resistance to drug treatment, as well as in 15% turning into "wrong behavior". So IUI have the highest percentage in the etiology of cerebral palsy, mental retardation and epilepsy in children . Therefore, it is very important to carry out diagnostics to identify IUI in pregnant women and newborns.
So IUI have the highest percentage in the etiology of cerebral palsy, mental retardation and epilepsy in children . Therefore, it is very important to carry out diagnostics to identify IUI in pregnant women and newborns.
But what is really happening?
At birth, in maternity hospitals, 70% of children take blood for TORCH syndrome. Then the children are discharged home without results, but with a diagnosis: either IUI or a consequence of IUI if the child is severe. The results of studies on TORCH syndrome are made within 5 to 14 days, plus the time for delivery to the children's clinic at the place of birth of the child. In addition, being the “gold standard”, the virological method is not available to most medical institutions, since cultivation using cell cultures is a labor-intensive, expensive process that requires highly qualified personnel. The reliability and sensitivity of the method depends on: the time elapsed from the moment of material sampling to sowing; quality of material sampling and transportation conditions; the quality of the media and reagents used. nine0004
nine0004
Unfortunately, not all medical institutions comply with these rules and requirements, which affects the accuracy of the results.
So, the results are delivered and attached to the card, but only 10% are evaluated by pediatricians or pediatric neurologists! The situation regarding “childhood” in the country is as follows: if there are no acute clinical manifestations of IUI, then they simply forget about it. And in the case of an IUI diagnosis made in the maternity hospital, most often it is not taken into account, with the further appearance of epileptic seizures and other neurological symptoms in the child, another diagnosis is already made (cerebral palsy, epilepsy, mental retardation, etc.) nine0004
Another variant of . If the child initially had a serious condition at birth, and then he develops poorly and malformations of other organs are detected, then a diagnosis is made; a consequence of the transferred IUI, and the children are offered to be taken to a special boarding school, as unpromising.
As with the first and second options, the "standard" treatment of children with vascular, antiepileptic, nootropic, etc. drugs is ineffective! nine0013
This is because viruses have evolved with their hosts and acquired genes that allow them to adapt to the changing human immune system. They have learned to modulate (change) their activity or hide from the main components of the human immune system, which must fight viruses. All this allows the viruses to "illegally" persist (stay) in the body and live, either in the ganglia (glands) of the cranial nerves in the case of herpes, or in the salivary glands in the case of cytomegavirus, etc. Hidden viruses at a convenient opportunity (hypothermia and hyperinsolation of the body, stress, acute respiratory infections, etc.) begin to activate, multiply and penetrate into the brain hematogenously (through the blood), or retroasconally. This leads to the development of chronic sluggish neuroinfection with the development of the so-called "vicious circle". Which is characterized by slow diffuse damage to the entire substance of the brain, inhibition of the blood-brain barrier, destruction of the myelin sheaths of axons, and a decrease in general immunity. As well as inhibition of the cells of the choroidal plexus of the ventricles of the brain, which leads to a violation of the reverse absorption (absorption) of excess cerebrospinal fluid and a violation of microcirculation processes with the development of hemolytic distension. These changes preserve the already existing hydrocephalus, or lead to it. Enlarged intracerebral ventricles constantly compress the pathways, thereby maintaining paresis or paralysis at the same level. nine0004
Which is characterized by slow diffuse damage to the entire substance of the brain, inhibition of the blood-brain barrier, destruction of the myelin sheaths of axons, and a decrease in general immunity. As well as inhibition of the cells of the choroidal plexus of the ventricles of the brain, which leads to a violation of the reverse absorption (absorption) of excess cerebrospinal fluid and a violation of microcirculation processes with the development of hemolytic distension. These changes preserve the already existing hydrocephalus, or lead to it. Enlarged intracerebral ventricles constantly compress the pathways, thereby maintaining paresis or paralysis at the same level. nine0004
THE MAIN DANGER of the “vicious circle” in case of neuroinfection is that over time, the immature immune system of the child begins to perceive his brain as a FOREIGN organ?! And ... begins to produce antibodies against it, destroying not only the pathways (nerves), but also the medulla itself.
Thus, chronic IUI not only maintains the severity of existing neurological and mental defects in the child, but also further aggravates their degree, or, in their absence, causes their development.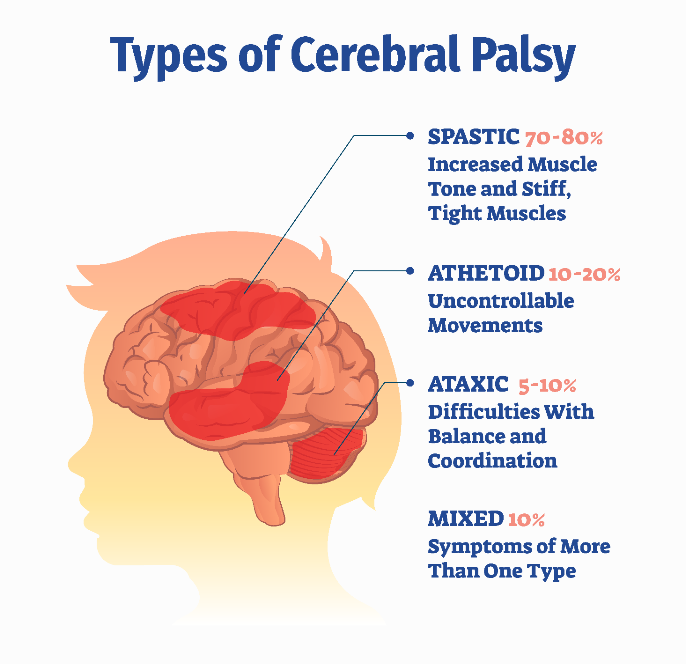 nine0004
nine0004
If your child has even a slight delay in development, or there is no effect from the treatment carried out with an already diagnosed diagnosis: cerebral palsy, delayed psycho-speech or motor development, mental retardation, epilepsy, autism, etc. – , it is urgent to take all measures to examine the child in our center in order to clarify the diagnosis and the cause of its occurrence, as well as to conduct timely pathogenetic treatment. nine0004
The CORTEX Medical Center is currently conducting effective treatment of such patients within the framework of a new medical technology for the treatment of infantile cerebral palsy, developed under the guidance of Academician F.I. Vasilenko.
For the first time, a conceptually new medical technology for the pathogenetic treatment of cerebral palsy and delays in the mental, speech and motor development of children has been developed, which can be considered the basis for effective complex treatment of this disease.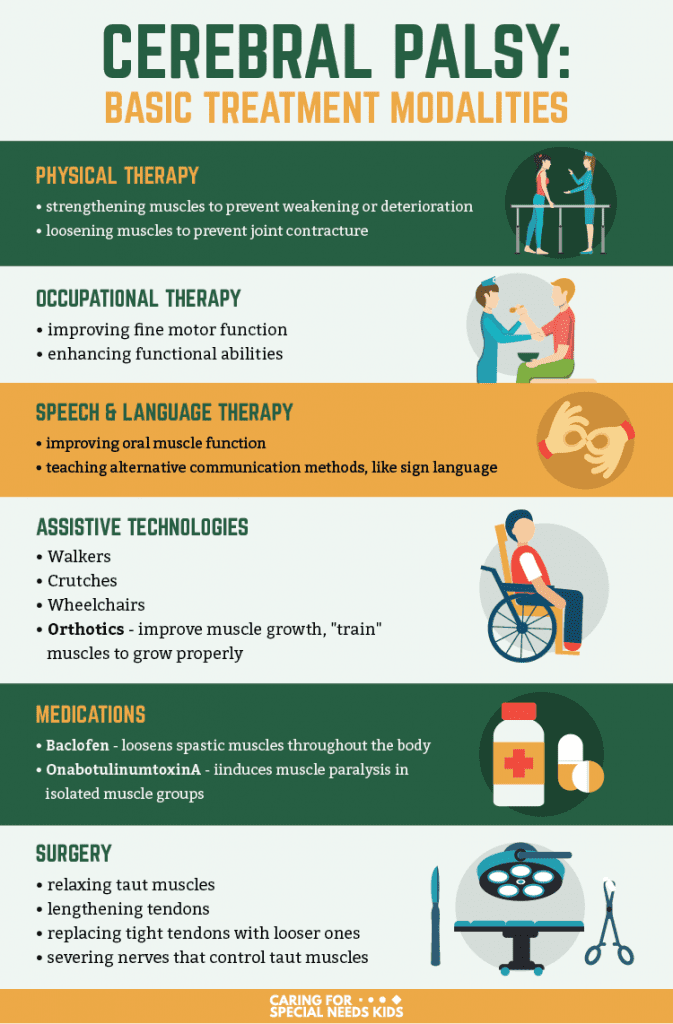 nine0004
nine0004
As part of complex treatment, diagnostics, basic pathogenetic treatment and rehabilitation procedures are carried out.
In addition to the instrumental examination of the brain and spinal cord, together with the Helix laboratory service, a high-precision virological blood test for TORCH syndrome (in accordance with the rules of GCP and GLP) is carried out with an assessment of cellular, humoral immunity to exclude an autoimmune demyelinating process with a % determination of the destruction of the white matter of the brain. and predicting the clinical outcome of perinatal hypoxia, which allows us to clarify the nature of the disease. This neuroimmunological study (technology and a set of special tests) was developed jointly with the state medical University. I.I. Mechnikov . It is very important to conduct a qualitative blood test using this technique. Lab Service Helix selected.
Helix is one of the largest institutions in Russia working in the field of laboratory diagnostics.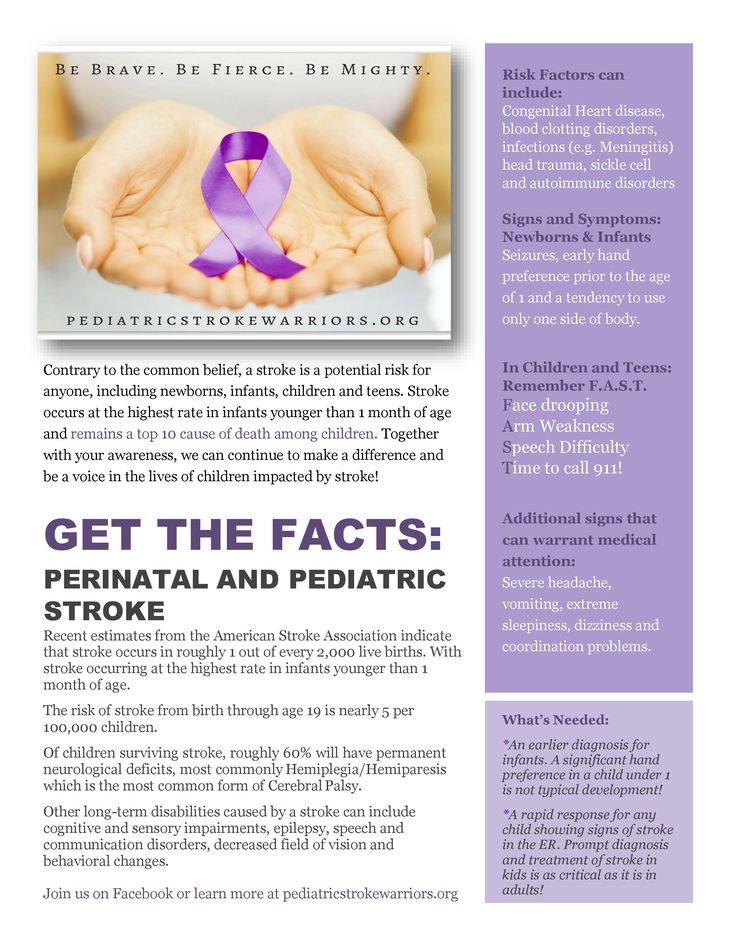 The Swiss auditing company SGS confirmed the competence of HELIX specialists with a certificate of compliance with ISO 9001:2008 “Quality management systems. Requirements”, then a certificate of conformity with GOST P ISO 15189 was obtained-2009 (ISO 15189:2007) Medical laboratories. Particular requirements for quality and competence. This laboratory service has become the first Russian institution working in the field of laboratory diagnostics, which has passed an international audit of this level.
The Swiss auditing company SGS confirmed the competence of HELIX specialists with a certificate of compliance with ISO 9001:2008 “Quality management systems. Requirements”, then a certificate of conformity with GOST P ISO 15189 was obtained-2009 (ISO 15189:2007) Medical laboratories. Particular requirements for quality and competence. This laboratory service has become the first Russian institution working in the field of laboratory diagnostics, which has passed an international audit of this level.
Therefore, the specialists of the CORTEX Medical Center, based on a high-precision blood test, prescribe an effective treatment for the detected intrauterine infection, which helps to increase the effectiveness of the treatment of cerebral palsy, mental retardation, mental retardation, autism and other diseases. nine0004
Early diagnosis of cerebral palsy
Relevance . It has already become obvious that the earlier infantile cerebral palsy (ICP) is recognized in an infant, the earlier efforts can be made to minimize its consequences. Thanks to a deeper analysis of changes in motor skills, improvements in neurological testing and neuroimaging methods, the possibilities of diagnosing cerebral palsy have undergone significant changes: it is possible to diagnose cerebral palsy or assume it already in the first half of a child's life. nine0081
Thanks to a deeper analysis of changes in motor skills, improvements in neurological testing and neuroimaging methods, the possibilities of diagnosing cerebral palsy have undergone significant changes: it is possible to diagnose cerebral palsy or assume it already in the first half of a child's life. nine0081
read also post: Cerebral palsy (at laesus-de-liro.livejournal.com) [read]
Early diagnosis of cerebral palsy . Today, it is recognized by an international team of doctors that accurate early diagnosis or detection of a high risk of cerebral palsy up to 5 months after the birth of a child seems to be the most reasonable when using (or combining) three research approaches, including [ 1 ] the analysis of gross motor skills according to Prechtl, [ 2 ] Hammersmith neurological analysis and [ 3 ] magnetic resonance imaging (MRI) of the brain. The choice of these methods is justified by the highest level of evidence and reliability in the diagnosis of cerebral palsy.
Prechtl method . The observation of the child is carried out for 30-60 minutes (including with the help of video recording), then a table of various types of movements is filled in with an assessment in points. Indicative is the normal type of motor activity at 3-5 months, which is called “fidgety” and consists of multiple quick movements of the neck, head, shoulder, torso, thigh, fingers, feet, special attention is paid to the “hand-face” contact , "arm - arm", "leg - leg". Convulsive-synchronous movements of the arms and legs at 2-4 months reflect the early manifestations of tetraparesis. A significant impoverishment of spontaneous movements of the arms and legs on one side in 2-3 months of life may subsequently manifest itself as spastic hemiparesis. Markers of spastic and dyskinetic forms of cerebral palsy at 3-5 months is the absence of lifting the legs in the supine position, the absence of fussy movements (fidgety). nine0004
read also post: We detect a violation of the child's psychomotor development (laesus-de-liro.
 livejournal.com) [read]
livejournal.com) [read] Neurological examination . Despite the high predictability of the original version of Prechtl's method, it is obvious that it does not replace the analysis of the general neurological status of the child and does not take into account the state of his primitive vocalization. Among the existing set of neurological examination schemes for the early diagnosis of cerebral palsy, the alliance of physicians recommended the Hammersmith neurological examination scheme for infants, which includes 26 items for assessing (on a 4-point scale from 0 to 3) cranial nerve function, posture, quality and quantity of movements, muscle tone, reflexes and reactions. The maximum score for normal development is 78 points. At 3 months of age, with a total score < 57, the prediction of cerebral palsy is 96%. In addition to the Prechtl method, the motor system is evaluated using the Test of Infant Motor Performance (TIMP). Without disputing the value of the Hammersmith scheme, I would like to note the possibility of using other neurological examination schemes in the diagnosis of cerebral palsy.
 General information on the differential diagnosis of cerebral palsy from other diseases can be found in a special guide.
General information on the differential diagnosis of cerebral palsy from other diseases can be found in a special guide. Neuroimaging of the brain . According to meta-analyses of MRI data, structural brain disorders in cerebral palsy vary markedly and the frequency of their detection is 80 - 90%. Less often, violations are detected in the atactic form of cerebral palsy. Pathology manifests itself more often in lesions of the white matter (cystic periventricular leukomalacia, periventricular hemorrhagic infarction), less often in lesions of the cortex, basal ganglia and thalamus, multicystic encephalomalacia, and also in dysgenesis (lisencephaly, pachygyria, cortical dysplasia, polymicrogyria or schizencephaly). However, the absence of pathological disorders in MRI does not exclude the risk of cerebral palsy], which emphasizes the need for examination by various methods, provided that the information obtained is integrated
Apgar score . Each of the considered methods of the cerebral palsy diagnostic triad requires the participation of highly qualified specialists, and neuroimaging is implemented by expensive equipment.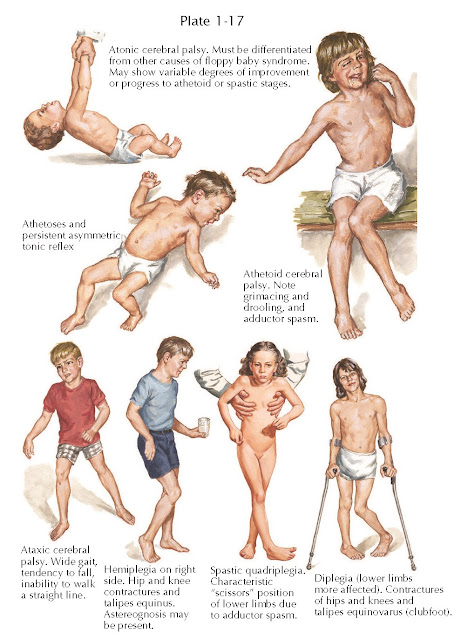 In this regard, I would like to draw attention to the very first scale for assessing the condition of a child used at birth - the Apgar scale, captivating in its simplicity and coverage of all those most important functions of a newborn that are clearly manifested and allow almost instantly assessing its viability. Three of its points are directly related to the early diagnosis of cerebral palsy: the state of breathing and muscle tone and reflex excitability. nine0004
In this regard, I would like to draw attention to the very first scale for assessing the condition of a child used at birth - the Apgar scale, captivating in its simplicity and coverage of all those most important functions of a newborn that are clearly manifested and allow almost instantly assessing its viability. Three of its points are directly related to the early diagnosis of cerebral palsy: the state of breathing and muscle tone and reflex excitability. nine0004
[ APGAR SCALE ]
If the state of muscle tone is determined by the participation of many body systems, including, of course, the nervous system, then the cry of a newborn is largely a reflection of his primitive (primary) vocal motor system. In humans, it produces genetically determined non-verbal vocalizations, such as laughter, moaning or crying, and consists of two structurally and functionally different systems: [ 1 ] the pattern-generating system of the brainstem and [ 2 ] initiating vocalization in affective states of the limbic network.
 The pattern-generating system of the brainstem is conservative in all vertebrates and represents a connected network of formations of the periaqueductal gray matter, the parabrachial nucleus, the reticular formation of the inferolateral part of the pons, controlling the entire pool of phonatory motor neurons (the nuclei of V, VII and XII pairs of cranial nerves, the double nucleus), as well as the muscles of the respiratory apparatus, larynx, oral cavity and tongue during vocalization. The brainstem pattern-generating system itself is controlled by the limbic vocalization-initializing system (the anterior cingulate gyrus, the hypothalamus and other limbic diencephalic structures, and the amygdala) through a complex network of connections. The quiet, weak and almost silent cry of the newborn and the weak voice subsequently are primarily an indicator of the weak air flow created by the respiratory system and breaking through the vocal cords, and, accordingly, the weakness of the primitive vocal motor system.
The pattern-generating system of the brainstem is conservative in all vertebrates and represents a connected network of formations of the periaqueductal gray matter, the parabrachial nucleus, the reticular formation of the inferolateral part of the pons, controlling the entire pool of phonatory motor neurons (the nuclei of V, VII and XII pairs of cranial nerves, the double nucleus), as well as the muscles of the respiratory apparatus, larynx, oral cavity and tongue during vocalization. The brainstem pattern-generating system itself is controlled by the limbic vocalization-initializing system (the anterior cingulate gyrus, the hypothalamus and other limbic diencephalic structures, and the amygdala) through a complex network of connections. The quiet, weak and almost silent cry of the newborn and the weak voice subsequently are primarily an indicator of the weak air flow created by the respiratory system and breaking through the vocal cords, and, accordingly, the weakness of the primitive vocal motor system.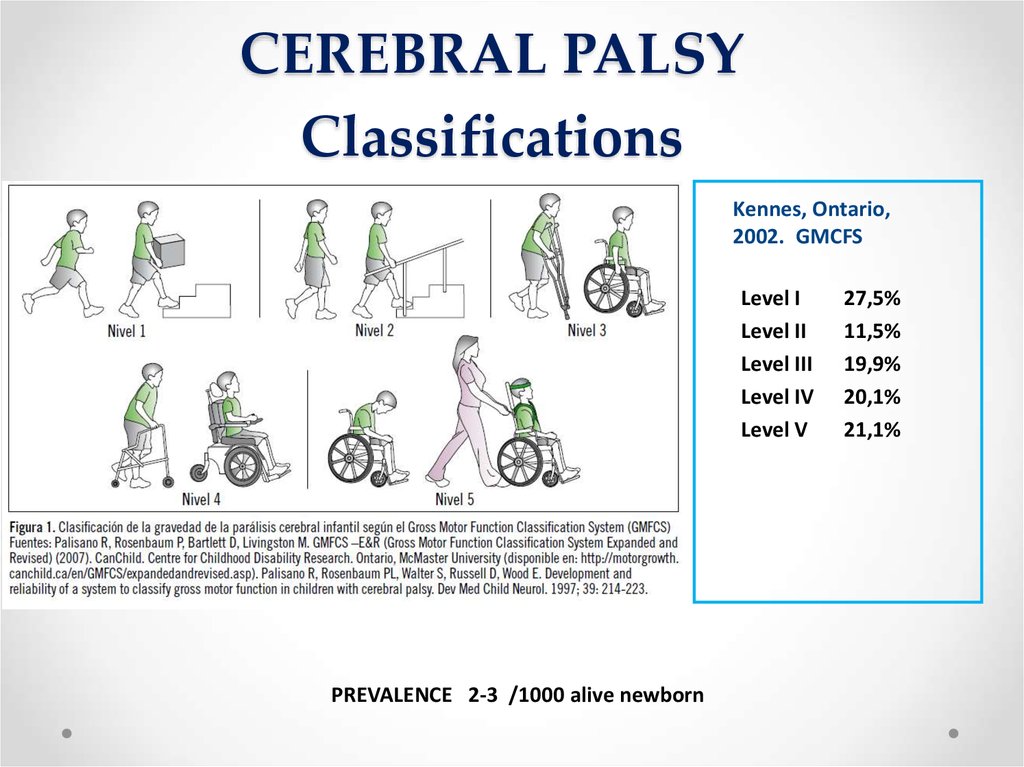 When the latter is disturbed, the normal development of its superstructure is impossible - an arbitrary articulatory motor system, the initial manifestation of the formation of which is cooing, and then babbling. According to speech therapists, the frequency of speech disorders in cerebral palsy is 80%. Children with cerebral palsy are characterized by long-term preservation of postural reflexes (especially labyrinth, symmetrical and asymmetric tonic reflexes), which prevent the development of voluntary movements in the child and, in particular, the articulation apparatus as a whole. Would the low Apgar scores for "respiratory system", "muscle tone" and "reflex excitability" be surprising with a soft cry of a newborn? Low scores on these three items seem to be the first harbinger of a high risk of cerebral palsy. nine0002 " Fingerprint Model " - a computerized diagnostic system designed to automatically detect neurofunctional biomarkers related to specific disorders of infancy and early childhood (for example, the use of a sensory mattress to register reference points of the back).
When the latter is disturbed, the normal development of its superstructure is impossible - an arbitrary articulatory motor system, the initial manifestation of the formation of which is cooing, and then babbling. According to speech therapists, the frequency of speech disorders in cerebral palsy is 80%. Children with cerebral palsy are characterized by long-term preservation of postural reflexes (especially labyrinth, symmetrical and asymmetric tonic reflexes), which prevent the development of voluntary movements in the child and, in particular, the articulation apparatus as a whole. Would the low Apgar scores for "respiratory system", "muscle tone" and "reflex excitability" be surprising with a soft cry of a newborn? Low scores on these three items seem to be the first harbinger of a high risk of cerebral palsy. nine0002 " Fingerprint Model " - a computerized diagnostic system designed to automatically detect neurofunctional biomarkers related to specific disorders of infancy and early childhood (for example, the use of a sensory mattress to register reference points of the back). The novelty of the purpose of the system lies in its focus on early diagnosis of developmental disorders with late manifestation or clinical onset. Registration and quantitative analysis of spontaneous movements of the infant's limbs by means of computerized technologies provide [ 1 ] continuity and [ 2 ] objectivity of observation and [ 3 ] make it possible to detect physiological and pathological asymmetries in the motor skills of the child's limbs.
The novelty of the purpose of the system lies in its focus on early diagnosis of developmental disorders with late manifestation or clinical onset. Registration and quantitative analysis of spontaneous movements of the infant's limbs by means of computerized technologies provide [ 1 ] continuity and [ 2 ] objectivity of observation and [ 3 ] make it possible to detect physiological and pathological asymmetries in the motor skills of the child's limbs. Please note ! In the absence of the possibility of examining a child using neuroimaging methods, the combination of data on the Apgar scale, neurological analysis, dynamics of posture development, general motor skills and vocalization allows moving the diagnosis of cerebral palsy to an earlier date - to the 2nd - 3rd month of life. The introduction of rigorous quantitative assessments into classical examination methods takes their diagnostic and prognostic value to a new level, which is confirmed by the development of a promising system for early diagnosis “The Imprint Model”.