Milk sensitivity symptoms
Milk allergy - Symptoms and causes
Overview
Milk allergy is an atypical immune system response to milk and products containing milk. It's one of the most common food allergies in children. Cow's milk is the usual cause of milk allergy, but milk from sheep, goats, buffalo and other mammals also can cause a reaction.
An allergic reaction usually occurs soon after you or your child consumes milk. Signs and symptoms of milk allergy range from mild to severe and can include wheezing, vomiting, hives and digestive problems. Milk allergy can also cause anaphylaxis — a severe, life-threatening reaction.
Avoiding milk and milk products is the primary treatment for milk allergy. Fortunately, most children outgrow milk allergy. Those who don't outgrow it may need to continue to avoid milk products.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Product for Nursing from Mayo Clinic Store
Symptoms
Milk allergy symptoms, which differ from person to person, occur a few minutes to a few hours after you or your child drinks milk or eats milk products.
Immediate signs and symptoms of milk allergy might include:
- Hives
- Wheezing
- Itching or tingling feeling around the lips or mouth
- Swelling of the lips, tongue or throat
- Coughing or shortness of breath
- Vomiting
Signs and symptoms that may take more time to develop include:
- Loose stools or diarrhea, which may contain blood
- Abdominal cramps
- Runny nose
- Watery eyes
- Colic, in babies
Milk allergy or milk intolerance?
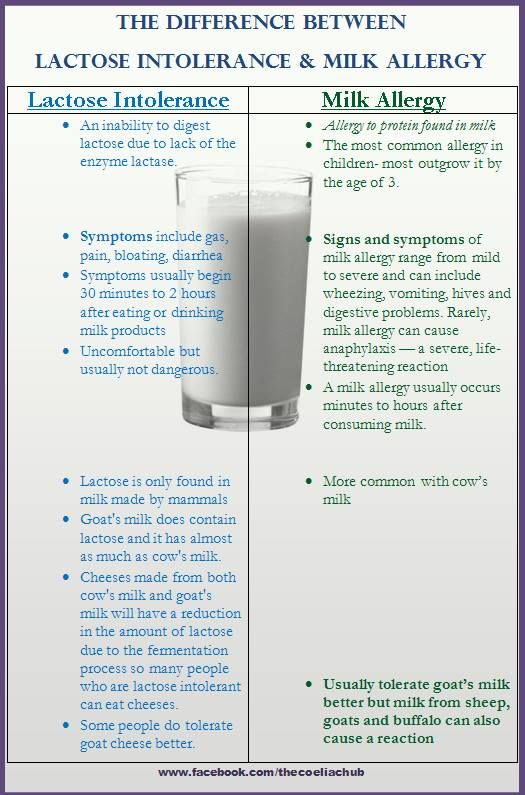
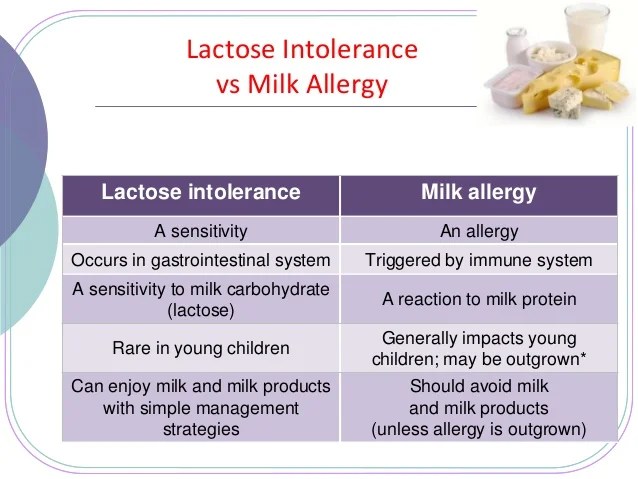
A true milk allergy differs from milk protein intolerance and lactose intolerance. Unlike milk allergy, intolerance doesn't involve the immune system. Milk intolerance requires different treatment from true milk allergy.
Common signs and symptoms of milk protein intolerance or lactose intolerance include digestive problems, such as bloating, gas or diarrhea, after consuming milk or products containing milk.
Anaphylaxis
Milk allergy can cause anaphylaxis, a life-threatening reaction that narrows the airways and can block breathing. Milk is the third most common food — after peanuts and tree nuts — to cause anaphylaxis.
If you or your child has a reaction to milk, tell your health care provider, no matter how mild the reaction. Tests can help confirm milk allergy, so you can avoid future and potentially worse reactions.
Anaphylaxis is a medical emergency and requires treatment with an epinephrine (adrenaline) shot (EpiPen, Adrenaclick, others) and a trip to the emergency room. Signs and symptoms start soon after milk consumption and can include:
- Constriction of airways, including a swollen throat that makes it difficult to breathe
- Facial flushing
- Itching
- Shock, with a marked drop in blood pressure
When to see a doctor
See your provider or an allergist if you or your child experiences milk allergy symptoms shortly after consuming milk. If possible, see your provider during the allergic reaction to help make a diagnosis. Seek emergency treatment if you or your child develops signs or symptoms of anaphylaxis.
If possible, see your provider during the allergic reaction to help make a diagnosis. Seek emergency treatment if you or your child develops signs or symptoms of anaphylaxis.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
All true food allergies are caused by an immune system malfunction. If you have milk allergy, your immune system identifies certain milk proteins as harmful, triggering the production of immunoglobulin E (IgE) antibodies to neutralize the protein (allergen). The next time you come in contact with these proteins, IgE antibodies recognize them and signal your immune system to release histamine and other chemicals, causing a range of allergic signs and symptoms.
There are two main proteins in cow's milk that can cause an allergic reaction:
- Casein, found in the solid part (curd) of milk that curdles
- Whey, found in the liquid part of milk that remains after milk curdles
You or your child may be allergic to only one milk protein or to both. These proteins may be hard to avoid because they're also in some processed foods. And most people who react to cow's milk will react to sheep, goat and buffalo milk.
These proteins may be hard to avoid because they're also in some processed foods. And most people who react to cow's milk will react to sheep, goat and buffalo milk.
Food protein-induced enterocolitis syndrome (FPIES)
A food allergen can also cause what's sometimes called a delayed food allergy. Although any food can be a trigger, milk is one of the most common. The reaction, commonly vomiting and diarrhea, usually occurs within hours after eating the trigger rather than within minutes.
Unlike some food allergies, FPIES usually resolves over time. As with milk allergy, preventing an FPIES reaction involves avoiding milk and milk products.
Risk factors
Certain factors may increase the risk of developing milk allergy:
- Other allergies. Many children who are allergic to milk also have other allergies.
 Milk allergy may develop before other allergies.
Milk allergy may develop before other allergies. - Atopic dermatitis. Children who have atopic dermatitis — a common, chronic inflammation of the skin — are much more likely to develop a food allergy.
- Family history. A person's risk of a food allergy increases if one or both parents have a food allergy or another type of allergy or allergic disease — such as hay fever, asthma, hives or eczema.
- Age. Milk allergy is more common in children. As they age, their digestive systems mature, and their bodies are less likely to react to milk.
Complications
Children who are allergic to milk are more likely to develop certain other health problems, including:
- Nutritional deficiencies. Because of dietary restrictions and feeding challenges, children with milk allergy may have slowed growth as well as vitamin and mineral deficiencies.
- Reduced quality of life.
 Many common, and sometimes unexpected, foods contain milk, including some salad dressings or even hot dogs. If you or your child is severely allergic, avoiding milk exposure may increase stress or anxiety levels when it comes to making food choices.
Many common, and sometimes unexpected, foods contain milk, including some salad dressings or even hot dogs. If you or your child is severely allergic, avoiding milk exposure may increase stress or anxiety levels when it comes to making food choices.
Prevention
There's no sure way to prevent a food allergy, but you can prevent reactions by avoiding the food that causes them. If you know you or your child is allergic to milk, avoid milk and milk products.
Read food labels carefully. Look for casein, a milk derivative, which can be found in some unexpected places, such as in some canned tuna, sausage or nondairy products. Question ingredients when ordering in restaurants.
Sources of milk
Obvious sources of allergy-causing milk proteins are found in dairy products, including:
- Whole milk, low-fat milk, skim milk, buttermilk
- Butter
- Yogurt
- Ice cream, gelato
- Cheese and anything that contains cheese
- Half-and-half
Milk can be harder to identify when it's used as an ingredient in processed foods, including baked goods and processed meats. Hidden sources of milk include:
Hidden sources of milk include:
- Whey
- Casein
- Ingredients spelled with the prefix "lact" — such as lactose and lactate
- Candies, such as chocolate, nougat and caramel
- Protein powders
- Artificial butter flavor
- Artificial cheese flavor
- Hydrolysates
Even if a food is labeled "milk-free" or "nondairy," it may contain allergy-causing milk proteins — so you have to read the label carefully. When in doubt, contact the manufacturer to be sure a product doesn't contain milk ingredients.
When eating out, ask how foods have been prepared. Does your steak have melted butter on it? Was your seafood dipped in milk before cooking?
If you're at risk of a serious allergic reaction, talk with your health care provider about carrying and using emergency epinephrine (adrenaline). If you have already had a severe reaction, wear a medical alert bracelet or necklace that lets others know you have a food allergy.
Milk alternatives for infants
In children who are allergic to milk, breastfeeding and the use of hypoallergenic formula can prevent allergic reactions.
- Breastfeeding is the best source of nutrition for your infant. Breastfeeding for as long as possible is recommended, especially if your infant is at high risk of developing milk allergy.
-
Hypoallergenic formulas are produced by using enzymes to break down (hydrolyze) milk proteins, such as casein or whey. Further processing can include heat and filtering. Depending on their level of processing, products are classified as either partially or extensively hydrolyzed. Or they may also be called elemental formulas.
Some hypoallergenic formulas aren't milk based, but instead contain amino acids. Besides extensively hydrolyzed products, amino-acid-based formulas are the least likely to cause an allergic reaction.
- Soy-based formulas are based on soy protein instead of milk.
 Soy formulas are fortified to be nutritionally complete — but, unfortunately, some children with a milk allergy also develop an allergy to soy.
Soy formulas are fortified to be nutritionally complete — but, unfortunately, some children with a milk allergy also develop an allergy to soy.
If you're breastfeeding and your child is allergic to milk, cow's milk proteins passed through your breast milk may cause an allergic reaction. You may need to exclude from your diet all products that contain milk. Talk to your health care provider if you know — or suspect — that your child has milk allergy and develops allergy signs and symptoms after breastfeeding.
If you or your child is on a milk-free diet, your health care provider or dietitian can help you plan nutritionally balanced meals. You or your child may need to take supplements to replace calcium and nutrients found in milk, such as vitamin D and riboflavin.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Lactose intolerance - Symptoms and causes
Overview
Small intestine
Small intestine
The small intestine is a hollow tube that runs from the stomach to the large intestine (colon).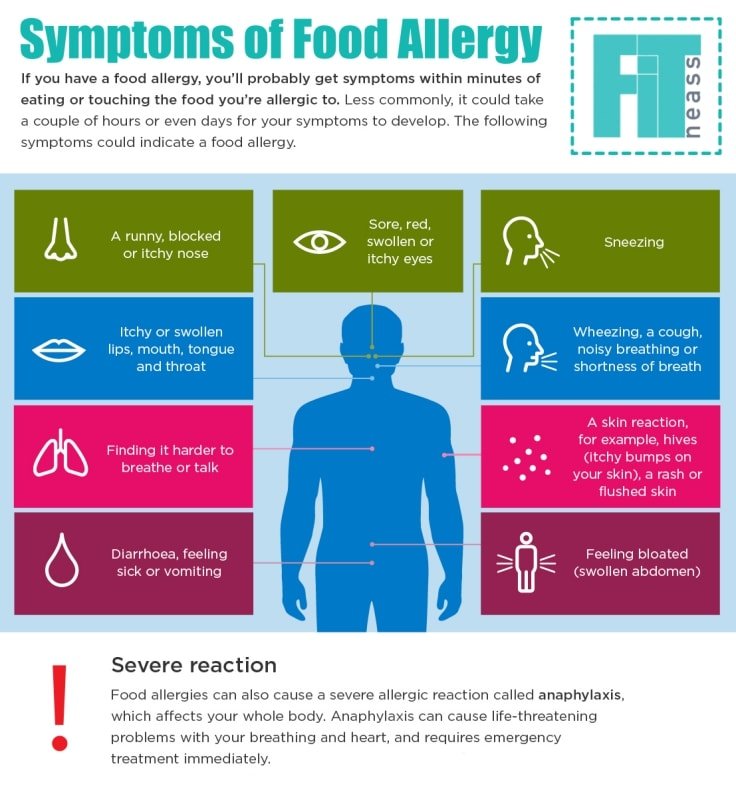
People with lactose intolerance are unable to fully digest the sugar (lactose) in milk. As a result, they have diarrhea, gas and bloating after eating or drinking dairy products. The condition, which is also called lactose malabsorption, is usually harmless, but its symptoms can be uncomfortable.
Too little of an enzyme produced in your small intestine (lactase) is usually responsible for lactose intolerance. You can have low levels of lactase and still be able to digest milk products. But if your levels are too low you become lactose intolerant, leading to symptoms after you eat or drink dairy.
Most people with lactose intolerance can manage the condition without having to give up all dairy foods.
Products & Services
- Book: Mayo Clinic Book of Home Remedies
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
The signs and symptoms of lactose intolerance usually begin from 30 minutes to two hours after eating or drinking foods that contain lactose.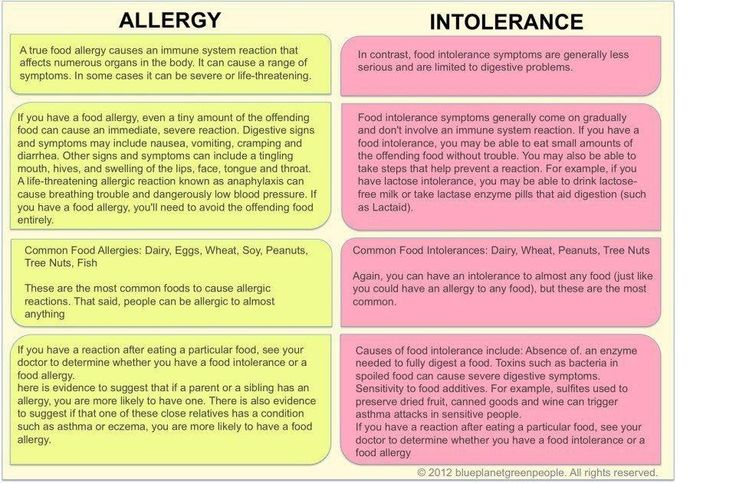 Common signs and symptoms include:
Common signs and symptoms include:
- Diarrhea
- Nausea, and sometimes, vomiting
- Stomach cramps
- Bloating
- Gas
When to see a doctor
Make an appointment with your doctor if you frequently have symptoms of lactose intolerance after eating dairy foods, particularly if you're worried about getting enough calcium.
Request an Appointment at Mayo Clinic
Get the latest health information from Mayo Clinic delivered to your inbox.
Subscribe for free and receive your in-depth guide to digestive health, plus the latest on health innovations and news. You can unsubscribe at any time.
Email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
Lactose intolerance occurs when your small intestine doesn't produce enough of an enzyme (lactase) to digest milk sugar (lactose).
Normally, lactase turns milk sugar into two simple sugars — glucose and galactose — which are absorbed into the bloodstream through the intestinal lining.
If you're lactase deficient, lactose in your food moves into the colon instead of being processed and absorbed. In the colon, normal bacteria interact with undigested lactose, causing the signs and symptoms of lactose intolerance.
In the colon, normal bacteria interact with undigested lactose, causing the signs and symptoms of lactose intolerance.
There are three types of lactose intolerance. Different factors cause the lactase deficiency underlying each type.
Primary lactose intolerance
People who develop primary lactose intolerance — the most common type — start life producing enough lactase. Infants, who get all their nutrition from milk, need lactase.
As children replace milk with other foods, the amount of lactase they produce normally drops, but usually remains high enough to digest the amount of dairy in a typical adult diet. In primary lactose intolerance, lactase production falls off sharply by adulthood, making milk products difficult to digest.
Secondary lactose intolerance
This form of lactose intolerance occurs when your small intestine decreases lactase production after an illness, injury or surgery involving your small intestine. Diseases associated with secondary lactose intolerance include intestinal infection, celiac disease, bacterial overgrowth and Crohn's disease.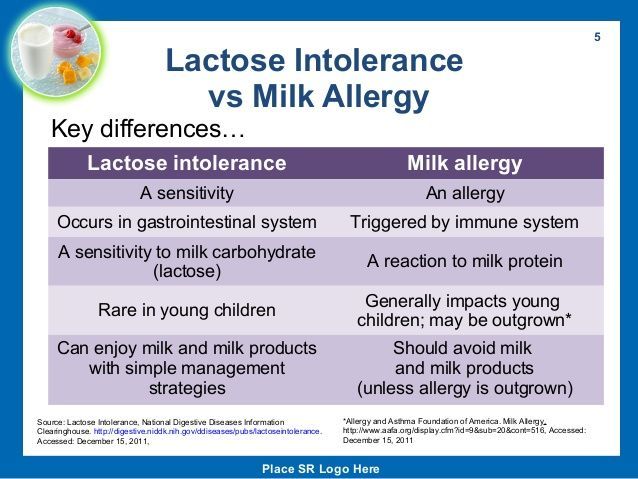
Treatment of the underlying disorder might restore lactase levels and improve signs and symptoms, though it can take time.
Congenital or developmental lactose intolerance
It's possible, but rare, for babies to be born with lactose intolerance caused by a lack of lactase. This disorder is passed from generation to generation in a pattern of inheritance called autosomal recessive, meaning that both the mother and the father must pass on the same gene variant for a child to be affected. Premature infants can also have lactose intolerance because of an insufficient lactase level.
Risk factors
Factors that can make you or your child more prone to lactose intolerance include:
- Increasing age. Lactose intolerance usually appears in adulthood. The condition is uncommon in babies and young children.
- Ethnicity. Lactose intolerance is most common in people of African, Asian, Hispanic and American Indian descent.

- Premature birth. Infants born prematurely might have reduced levels of lactase because the small intestine doesn't develop lactase-producing cells until late in the third trimester.
- Diseases affecting the small intestine. Small intestine problems that can cause lactose intolerance include bacterial overgrowth, celiac disease and Crohn's disease.
- Certain cancer treatments. If you've had radiation therapy for cancer in your stomach or you have intestinal complications from chemotherapy, your risk of developing lactose intolerance increases.
By Mayo Clinic Staff
Related
Products & Services
Gluten and lactose sensitivity
Gluten and lactose intolerance are the most common digestive disorders in which the human body cannot break down foods containing grains and milk. This can be expressed by many symptoms - from mild abdominal pain and flatulence to diarrhea, abdominal cramps and bloody stools. As a rule, intolerance does not appear unexpectedly, but due to frequent and long-term use of products.
As a rule, intolerance does not appear unexpectedly, but due to frequent and long-term use of products.
Sensitivity to gluten and lactose occurs not only in intolerance, but also in a number of diseases that have similar symptoms and require a thorough diagnostic approach - analysis of anamnesis, clinical and laboratory data.
Therefore, we have developed test packages in which one-stage diagnostics of all major conditions associated with gluten and lactose sensitivity is carried out:

Only blood (capillary or venous) is needed to diagnose gluten sensitivity
To diagnose lactose sensitivity, blood (capillary or venous), feces (1 teaspoon in a sterile container) and saliva (buccal scraping) are needed.
Get price
| Gluten and lactose sensitivity |
| Gluten package0037 |
| milk allergy: IgE f02 cow's milk |
| milk allergy: IgE f300 goat's milk |
Milk allergy (lactose): milk allergy in children and adults
Milk allergy (or lactose allergy) is a response of the human immune system to milk protein. An interesting fact is that for one person only sheep's milk can be an allergen, and he can safely drink goat's and cow's milk, and for another person, absolutely all dairy products can serve as allergens.
This is due to the fact that the milk of artiodactyl animals does not contain the same types of proteins.
And so some people are allergic to one type of protein in milk, while others are allergic to several types of proteins. In the event that casein (a protein whose percentage in milk is 80% of all proteins) acts as an allergen for a person, then a person cannot eat any types of dairy products. That is, when a person is allergic to cow's milk (or, to be more precise, to cow's milk protein), he can still drink goat's milk without any difficulty.
Types of proteins in milk
In general, it can be said that milk contains different types of proteins, which determine the nature of human allergic disease.
Casein is found in all types of milk, as mentioned above. And this means that it is not possible to replace the use of one milk with another in the presence of an allergy to milk.
Whey proteins. Such proteins are temperature sensitive.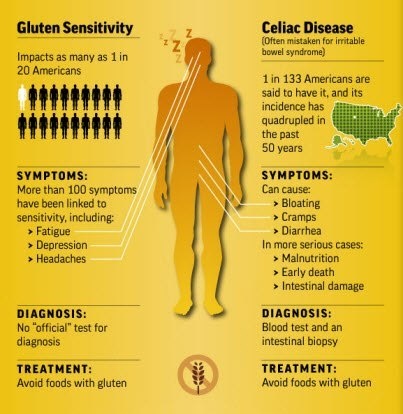 Accordingly, when milk is boiled, the process of destruction of such proteins occurs. That is why, if it is impossible to eat raw milk, you can safely use boiled milk.
Accordingly, when milk is boiled, the process of destruction of such proteins occurs. That is why, if it is impossible to eat raw milk, you can safely use boiled milk.
Causes of allergy to lactose
Causes of allergy to lactose (milk sugar) may be as follows:
Genetic heredity to ensure that a hypersensitive reaction is formed in the human body to the intake of substances that serve as irritants.
Malfunctions of the immune system when specific immunoglobulin E is produced in large quantities.
If the enzyme that is responsible for processing the protein contained in milk is not present in the patient's body or is present, but in too small a quantity, then the human body will react to proteins as if they were foreign substances and react accordingly.
Symptoms of an allergy to milk (lactose)
Symptoms of an allergy in adults are as follows: , flatulence, spasms.
Severe symptoms
Symptoms may become more severe. For example, in adults, there may be sudden changes in pressure, choking, or there is a strong degree of swelling of the throat and mouth.
It is worth noting the fact that it does not matter what kind of milk a person is allergic to, since the symptoms will be the same for an allergy to cow's protein, and an allergy to goat's, and sheep's.
If you experience any of the above symptoms, you should immediately consult a doctor for qualified assistance and treatment. It is almost impossible to remove milk from among the irritants that cause an allergic reaction, even if drugs are used for this. The only thing that can be done to prevent lactose allergy is to remove milk, and also dairy products, if necessary, from the list of foods consumed. At the same time, it is worth mentioning that milk, one way or another, is an integral part of a huge number of products, such as chocolate, white bread, ice cream, sour cream, breakfast cereals, pastry, cream, condensed milk, and instant soups, as well as dry soups. mixtures. So in the event that the patient has a pronounced allergic reaction to milk, you should stop eating not only yogurt, kefir, cheese, milk and cottage cheese, but also the aforementioned products that contain milk. In addition, milk components can be found in cosmetics, and therefore they should be checked for the presence of an allergen. Since sometimes it can be quite difficult to determine whether a product contains milk or not, people who are prone to this type of allergy are strongly advised to always carry medications with them, which can quickly remove the symptoms of milk allergy that have appeared.
mixtures. So in the event that the patient has a pronounced allergic reaction to milk, you should stop eating not only yogurt, kefir, cheese, milk and cottage cheese, but also the aforementioned products that contain milk. In addition, milk components can be found in cosmetics, and therefore they should be checked for the presence of an allergen. Since sometimes it can be quite difficult to determine whether a product contains milk or not, people who are prone to this type of allergy are strongly advised to always carry medications with them, which can quickly remove the symptoms of milk allergy that have appeared.
Milk allergy in a child
When a child has a milk allergy, the disease process is accompanied by the same symptoms as in adults. If a child has an allergy to milk protein, which is found in dairy products such as milk (breast), cottage cheese, cheese, yogurt, kefir, etc., then he may be more capricious, and also lag behind in growth and development ( this is due to the fact that he does not receive the necessary amount of nutrients for this). In addition, he may have loose stools or burp after feeding. It is much easier to understand that milk has become the cause of an allergic disease when the sick person is a child. Because, unlike an adult, whose diet should still be checked for possible irritants, a child's milk allergy can manifest itself immediately during breastfeeding. At the same time, it should be added that over time, in young children, an allergy to milk disappears, remaining in adulthood in only 1% of those who were ill.
In addition, he may have loose stools or burp after feeding. It is much easier to understand that milk has become the cause of an allergic disease when the sick person is a child. Because, unlike an adult, whose diet should still be checked for possible irritants, a child's milk allergy can manifest itself immediately during breastfeeding. At the same time, it should be added that over time, in young children, an allergy to milk disappears, remaining in adulthood in only 1% of those who were ill.
If a child develops the above symptoms, they should be taken to a specialist immediately. In order to find out if there is an allergy specifically to milk, and, as a possible consequence, to dairy products, the following procedures can be carried out: to check the blood for the content of immunoglobulins in it, skin allergic tests are performed; to check the blood for the content of antibodies in it, take its analysis.
The presence of such an allergic disease creates a large number of inconveniences for the patient, especially if it is a small child.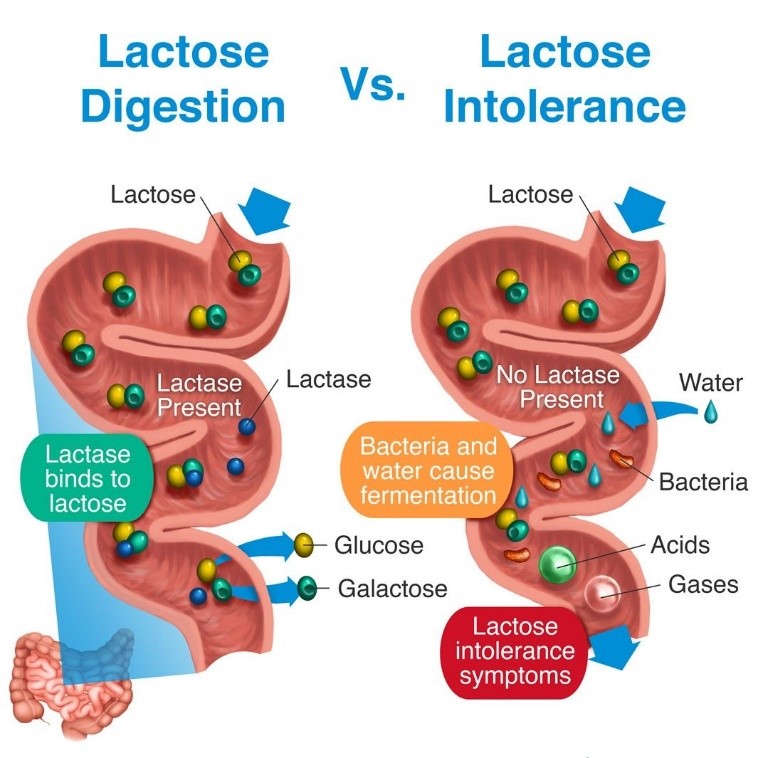 They are advised to give milk substitutes for food, which are designed specifically for allergy sufferers. The composition of such milk includes milk of plant origin and goat's milk, which is completely harmless to your baby, because intolerance to goat's milk is extremely rare. Its important advantage is the fact that it is close to the female in its composition. For adults, it is recommended to eat such types of milk as oat, rice, soy and almond. At the same time, for approximately a quarter of people who are allergic to milk protein, soy is also an allergen, so they cannot change milk to soy in their diet. There is no such protein in rice milk, but at the same time, its disadvantage is the low level of nutritional and beneficial properties compared to their level in other types of milk.
They are advised to give milk substitutes for food, which are designed specifically for allergy sufferers. The composition of such milk includes milk of plant origin and goat's milk, which is completely harmless to your baby, because intolerance to goat's milk is extremely rare. Its important advantage is the fact that it is close to the female in its composition. For adults, it is recommended to eat such types of milk as oat, rice, soy and almond. At the same time, for approximately a quarter of people who are allergic to milk protein, soy is also an allergen, so they cannot change milk to soy in their diet. There is no such protein in rice milk, but at the same time, its disadvantage is the low level of nutritional and beneficial properties compared to their level in other types of milk.
It is also recommended to change the butter for a product such as margarine. It is worth paying attention to the fact that dairy products contain a large amount of vitamin B. In this regard, if a person excludes dairy products from the list of foods he eats, he must necessarily compensate for this.