Losing baby miscarriage
Why we need to talk about losing a baby
Why we need to talk about losing a baby- All topics »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Resources »
- Fact sheets
- Facts in pictures
- Multimedia
- Publications
- Questions & answers
- Tools and toolkits
- Popular »
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Monkeypox
- All countries »
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
- Regions »
- Africa
- Americas
- South-East Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- WHO in countries »
- Statistics
- Cooperation strategies
- Ukraine emergency
- All news »
- News releases
- Statements
- Campaigns
- Commentaries
- Events
- Feature stories
- Speeches
- Spotlights
- Newsletters
- Photo library
- Media distribution list
- Headlines »
- Focus on »
- Afghanistan crisis
- COVID-19 pandemic
- Northern Ethiopia crisis
- Syria crisis
- Ukraine emergency
- Monkeypox outbreak
- Greater Horn of Africa crisis
- Latest »
- Disease Outbreak News
- Travel advice
- Situation reports
- Weekly Epidemiological Record
- WHO in emergencies »
- Surveillance
- Research
- Funding
- Partners
- Operations
- Independent Oversight and Advisory Committee
- Data at WHO »
- Global Health Estimates
- Health SDGs
- Mortality Database
- Data collections
- Dashboards »
- COVID-19 Dashboard
- Triple Billion Dashboard
- Health Inequality Monitor
- Highlights »
- Global Health Observatory
- SCORE
- Insights and visualizations
- Data collection tools
- Reports »
- World Health Statistics 2022
- COVID excess deaths
- DDI IN FOCUS: 2022
- About WHO »
- People
- Teams
- Structure
- Partnerships and collaboration
- Collaborating centres
- Networks, committees and advisory groups
- Transformation
- Our Work »
- General Programme of Work
- WHO Academy
- Activities
- Initiatives
- Funding »
- Investment case
- WHO Foundation
- Accountability »
- Audit
- Budget
- Financial statements
- Programme Budget Portal
- Results Report
- Governance »
- World Health Assembly
- Executive Board
- Election of Director-General
- Governing Bodies website
- Home/
- Newsroom/
- Spotlight/
- Why we need to talk about losing a baby
Why we need to talk about losing a baby
WHO/M. Purdie
© Credits
Losing a baby in pregnancy through miscarriage or stillbirth is still a taboo subject worldwide, linked to stigma and shame. Many women still do not receive appropriate and respectful care when their baby dies during pregnancy or childbirth. Here, we share your stories from around the globe.
Miscarriage is the most common reason for losing a baby during pregnancy. Estimates vary, although March of Dimes, an organization that works on maternal and child health, indicates a miscarriage rate of 10-15% in women who knew they were pregnant. Pregnancy loss is defined differently around the world, but in general a baby who dies before 28 weeks of pregnancy is referred to as a miscarriage, and babies who die at or after 28 weeks are stillbirths. Every year, nearly 2 million babies are stillborn, and many of these deaths are preventable. However, miscarriages and stillbirths are not systematically recorded, even in developed countries, suggesting that the numbers could be even higher.
Around the world, women have varied access to healthcare services, and hospitals and clinics in many countries are very often under-resourced and understaffed. As varied as the experience of losing a baby may be, around the world, stigma, shame and guilt emerge as common themes. As these first-person accounts show, women who lose their babies are made to feel that should stay silent about their grief, either because miscarriage and stillbirth are still so common, or because they are perceived to be unavoidable.
Jessica Zucker, clinical psychologist and writer, USA
"As a clinical psychologist, I specialise in women's reproductive and maternal mental health and have done so for over a decade. It wasn't until I experienced this 16-week miscarriage first-hand that I could truly grasp the anguish and the circuitousness of grief I had heard my patients speak of for so many years. After my miscarriage, I poured over the research which shows that a majority of women report experiencing feelings of shame, self-blame and guilt following pregnancy loss. "
"
Jessica's story
All of this takes an enormous toll on women. Many women who lose a baby in pregnancy can go on to develop mental health issues that last for months or years– even when they have gone on to have healthy babies.
Cultural and societal attitudes to losing a baby can vary tremendously around the globe. In sub-Saharan Africa, a common belief is that a baby might be stillborn because of witchcraft or evil spirits.
Larai, 44, pharmacist, Nigeria
“Coping with my miscarriage was traumatic. The medical staff contributed a lot to my grief despite the fact that I am a doctor too. The other issue is the cultural attitude. In most traditional African cultures, people think you can lose a baby because of a curse or witchcraft. Here, child loss is surrounded by stigma because some people believe there is something wrong with a woman who has had recurrent losses, that she may have been promiscuous, and so the loss is seen as a punishment from God. "
"
Larai’s story
People, especially those with high profiles, are taking to social media to share their experiences, like in the case of Kimberly Van Der Beek and her husband, actor James Van Der Beek, best known for his role in American television series Dawson’s Creek. The couple recently shared a heartfelt post on Instagram where they opened up about the painful process of suffering multiple miscarriages — and then learning how to move past it.
Kimberly Van Der Beek, USA
"I’ve had three miscarriages, all around 10 weeks gestation. I let them all happen naturally. I had a loving husband, a compassionate birthing team and I felt spiritually grounded about them. And even in the best of circumstances, I was devastated every single time. After one of them I sat in the shower crying for almost five hours. What I find disheartening is that not all women, or fathers for that matter, are treated with the same compassion or have support during this gut wrenching time".
Kimberly's story
There are many reasons why a miscarriage may happen, including fetal abnormalities, the age of the mother, and infections, many of which are preventable such as malaria and syphilis, though pinpointing the exact reason is often challenging.
General advice on preventing miscarriage focuses on eating healthily, exercising, avoiding smoking, drugs and alcohol, limiting caffeine, controlling stress, and being of a healthy weight. This places the emphasis on lifestyle factors, which, in the absence of specific answers, can lead to women feeling guilty that they have caused their miscarriage.
Lisa, 40, marketing manager, UK
“I’ve had four miscarriages. Each time it happens, a piece of you dies. The most traumatic was the first one. We were so excited about our new baby. But when we went in for the 12-week scan, I was told I had a missed miscarriage, also called a silent miscarriage, which meant the baby died a long time ago but my body hadn't showed any signs. I was devastated. I also couldn’t believe that they were going to just send me home with my dead baby inside me, and no advice about what to do."
I was devastated. I also couldn’t believe that they were going to just send me home with my dead baby inside me, and no advice about what to do."
Lisa’s story
As with other health issues such as mental health, around which there is tremendous taboo still, many women report that no matter their culture, education or upbringing, their friends and family do not want to talk about their loss. This seems to connect with the silence that shrouds talking about grief in general.
Susan, 34, writer, USA
“I’ve been on the fertility train for nearly 5 years. As my own IVF began, I quickly learned that I had no idea what I was in for; it was so physically and emotionally exhausting. Thankfully, I did get pregnant, and my husband and I were so excited. However, after 7 weeks, the baby stopped growing. I then quit IVF hormones, and after 2 more weeks, the miscarriage began. It lasted 19 days. I didn’t realize miscarriages were a long process of pain and heavy bleeding. That the realities of fertility and miscarriage are so shrouded behind shame and silence. "
"
Susan's story
Stillbirths happen later in pregnancy, and more than 40% occur during labour, many of which are preventable. Around 84% of stillbirths take place in low- and lower middle-income countries. Providing better quality of care during pregnancy and childbirth could prevent over half a million stillbirths worldwide. Even in high-income countries, substandard care is a significant factor in stillbirths.
There are clear ways in which to reduce the number of babies who die in pregnancy – improving access to antenatal care (in some areas in the world, women do not see a health care worker until they are several months pregnant), introducing continuity of care through midwife-led care, and introducing community care where possible.
Integrating the treatment of infections in pregnancy, fetal heart rate monitoring and labour surveillance, as part of an integrated care package could save 832 000 who would otherwise have been stillborn.
How women are treated during pregnancy is linked to their sexual and reproductive rights, over which many women around the world do not have autonomy.
Societal pressures in many parts of the world can mean that women get pregnant when they are not physically or mentally ready. Even in 2019, 200 million women who want to avoid pregnancy have no access to modern contraception. And when they do get pregnant, 30 million women do not give birth in a health facility and 45 million women receive inadequate or no antenatal care, putting both mother and baby at much greater risk of complications and death.
Emilia, 36, retailer, Colombia
"When I had a stillbirth at 32 weeks, my baby already had a name. I rushed to the clinic with very high blood pressure. After a checkup, the doctor told me to take some rest and prescribed a medication to lower my blood pressure. After a week I still had the same symptoms. The doctor rushed me to take an ultrasound and he told me that the baby had no vital signs. If I had been given more information from the very beginning, and received more medical attention at critical moments, my baby could have been saved. "
"
Emilia’s story
How women are treated during pregnancy is linked to their sexual and reproductive rights, over which many women around the world do not have autonomy.
Societal pressures in many parts of the world can mean that women get pregnant when they are not physically or mentally ready. Even in 2019, 200 million women who want to avoid pregnancy have no access to modern contraception. And when they do get pregnant, 30 million women do not give birth in a health facility and 45 million women receive inadequate or no antenatal care, putting both mother and baby at much greater risk of complications and death.
Divya Samson Panabakam, 30, consultant, India
"In 2013 I had my first miscarriage. As soon as I started bleeding I went to the hospital and I was sent to get a sonogram, but the person in charge thought that I wasn’t married and made me wait. I asked her: “Even if I wasn’t married, why would you want to treat someone who is losing a baby this way?”. She just looked at me and replied: 'It’s not an emergency, only a woman over 60 would be treated as an emergency case'."
She just looked at me and replied: 'It’s not an emergency, only a woman over 60 would be treated as an emergency case'."
Read More
Cultural practices such as female genital mutilation (FGM) and child marriage are hugely damaging to girls’ sexual and reproductive health, and the health of their babies. Having babies too young can be dangerous for both the mothers and the babies. Adolescent mothers (aged 10 – 19 years) are far more likely to have eclampsia or uterine infections than women aged 20-24 years, which can increase the risk of stillbirth. Babies born to women younger than 20 years are also more likely to be of low birthweight, preterm, or have severe neonatal conditions, all of which can increase the risk of stillbirth.
FGM increases a woman’s risk of prolonged and obstructed labour, haemorrhage, severe tearing and a need for instrumental delivery. Her baby is much more likely to need resuscitation at delivery and faces a high risk of death during labour or after birth.
Putting women at the centre of their care is vital to a positive pregnancy experience – biomedical and physiological aspects of care need to be joined with social, cultural, emotional and psychological support.
Yet many women, even in developed countries with access to the best healthcare, receive inadequate care after losing a baby. The language used around miscarriage and stillbirth can be traumatic in itself – terminology referring to an “incompetent cervix” or a “blighted ovum” can be distressing.
Andrea, 28, stylist, Colombia
"When I was 12 weeks pregnant, I went for a check-up and had an ultrasound. The doctor told me that something was wrong without specifying what it was. The next day I woke up and noticed that the bed sheet were stained with blood. I did not receive any information on why I had a miscarriage. The nurses were very cold and unfriendly and they behaved as if it was just a medical procedure. Among all the staff at the hospital the only one who had a bit of humanity was the doctor, who later reassured me that I could try again to get pregnant. "
"
Andrea's story
Depending on the policy of the hospital, the babies’ bodies may be treated as clinical waste and incinerated. Sometimes when a woman finds out her baby has died, she is required to carry the dead baby for several weeks before she can give birth. Though there may be clinical reasons for this delay, this is distressing to the woman and her partner. Even in developed countries, women may birth their dead baby in maternity units, surrounded by women with healthy babies.
Not all hospitals or clinics can adopt new policies or provide more services. This is a reality of overburdened health care systems. Yet encouraging more sensitivity in dealing with bereaved couples, and removing the taboo and stigma around talking about baby loss does not need to cost money. This is reflected in some of the stories featured here.
Becky, 38, primary school teacher, Viet Nam/UK
"My husband and I were over the moon when I fell pregnant with twin girls and were devastated to lose one of them – we called her Isla - at 34 weeks. I was terrified that we were going to lose our other baby too, and insisted on staying in hospital. The next day I delivered our girls via caesarean section. Overall the hospital was incredibly supportive and we were given a private room and time to spend with Isla. However a number of doctors showed complete insensitivity with one even asking why I was crying and telling me to cheer up".
I was terrified that we were going to lose our other baby too, and insisted on staying in hospital. The next day I delivered our girls via caesarean section. Overall the hospital was incredibly supportive and we were given a private room and time to spend with Isla. However a number of doctors showed complete insensitivity with one even asking why I was crying and telling me to cheer up".
Becky's story
Healthcare staff can show sensitivity and empathy, acknowledge how the parents feel, provide clear information, and understand that the parents may need specific support both in dealing with their loss and in potentially trying to have another baby. Providing human rights based care, that is socioculturally relevant, respectful and dignified is as much a requirement for competent maternal and newborn care as clinical competence.
Sarah, 40, civil servant, Australia
"Stillbirth is so common in Australia when it happens to you or someone you know. It’s suddenly everywhere. Stillbirth affects around 2000 Australian families each year. Our rate of stillbirth hasn’t changed in 20 years and for Indigenous Australians it’s twice as high. Yet before it happened to me and I became that one in six, I never considered that babies could die in utero. It’s never spoken about. The doctor told me about my increased risk of cord prolapse with polyhydramnios but no one mentioned I was at an increased risk of fetal death".
It’s suddenly everywhere. Stillbirth affects around 2000 Australian families each year. Our rate of stillbirth hasn’t changed in 20 years and for Indigenous Australians it’s twice as high. Yet before it happened to me and I became that one in six, I never considered that babies could die in utero. It’s never spoken about. The doctor told me about my increased risk of cord prolapse with polyhydramnios but no one mentioned I was at an increased risk of fetal death".
Sarah's story
Key messages around support
The Unacceptable Stigma And Shame Women Face After Baby Loss Must End
Op-ed by Dr Princess Nothemba Simelela, Assistant director-general for family, women, children and adolescents, WHO
Find out more
More on WHO's work
More on WHO's work with partners
All illustrations WHO/M. Purdie
Join WHO in action
Miscarriage | Pregnancy Birth and Baby
The loss of a baby through miscarriage can be very distressing.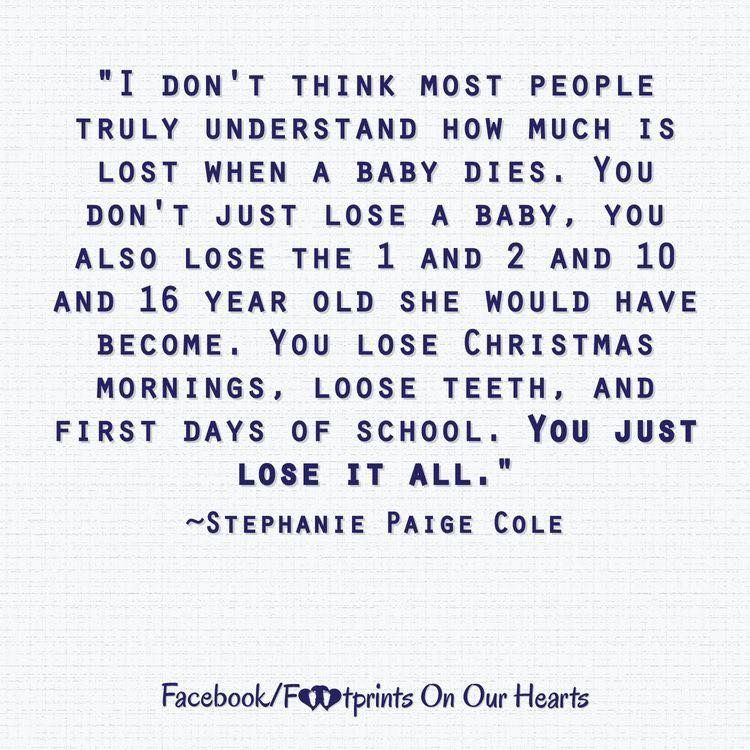 A miscarriage generally occurs for reasons outside your control and nothing can be done to prevent or stop it from happening. Most women who have had a miscarriage will go on to have a healthy pregnancy in the future.
A miscarriage generally occurs for reasons outside your control and nothing can be done to prevent or stop it from happening. Most women who have had a miscarriage will go on to have a healthy pregnancy in the future.
What is a miscarriage?
A miscarriage is the loss of your baby before 20 weeks of pregnancy. The loss of a baby after 20 weeks is called a stillbirth.
Up to 1 in 5 confirmed pregnancies end in miscarriage before 20 weeks, but many other women miscarry without having realised they are pregnant.
Common signs of miscarriage include:
- cramping tummy pain, similar to period pain
- vaginal bleeding
If you think you are having a miscarriage, see your doctor or go to your local emergency department.
Many women experience vaginal spotting in the first trimester that does not result in pregnancy loss.
What are the types of miscarriage?
There are several types of miscarriage — threatened, inevitable, complete, incomplete or missed.
Other types of pregnancy loss include an ectopic pregnancy, molar pregnancy and a blighted ovum.
Threatened miscarriage
When your body is showing signs that you might miscarry, that is called a 'threatened miscarriage'. You may have light vaginal bleeding or lower abdominal pain. It can last days or weeks and the cervix is still closed.
The pain and bleeding may resolve and you can go on to have a healthy pregnancy and baby. Or things may get worse and you go on to have a miscarriage.
There is rarely anything a doctor, midwife or you can do to prevent a miscarriage. In the past bed rest was recommended, but there is no scientific proof that this helps at this stage.
Inevitable miscarriage
Inevitable miscarriages can come after a threatened miscarriage or without warning. There is usually a lot more vaginal bleeding and strong lower stomach cramps. During the miscarriage your cervix opens and the developing fetus will come away in the bleeding.
Complete miscarriage
A complete miscarriage has taken place when all the pregnancy tissue has left your uterus. Vaginal bleeding may continue for several days. Cramping pain much like labour or strong period pain is common — this is the uterus contracting to empty.
If you have miscarried at home or somewhere else with no health workers present, you should have a check-up with a doctor or midwife to make sure the miscarriage is complete.
Incomplete miscarriage
Sometimes, some pregnancy tissue will remain in the uterus. Vaginal bleeding and lower abdominal cramping may continue as the uterus continues trying to empty itself. This is known as an 'incomplete miscarriage'.
Your doctor or midwife will need to assess whether or not a short procedure called a ‘dilatation of the cervix and curettage of the uterus’ (often known as a ‘D&C’) is necessary to remove any remaining pregnancy tissue. This is an important medical procedure done in an operating theatre.
Missed miscarriage
Sometimes, the fetus has died but stayed in the uterus. This is known as a 'missed miscarriage'.
If you have a missed miscarriage, you may have a brownish discharge. Some of the symptoms of pregnancy, such as nausea and tiredness, may have faded. You might have noticed nothing unusual. You may be shocked to have a scan and find the fetus has died.
If this happens, you should discuss treatment and support options with your doctor.
Recurrent miscarriage
A small number of women have repeated miscarriages. If this is your third or more miscarriage in a row, it’s best to discuss this with your doctor who may be able to investigate the causes, and refer you to a specialist.
A miscarriage can occur suddenly or over a number of weeks. The symptoms are usually vaginal bleeding and lower tummy pain. It is important to see your doctor or go to the emergency department if you have signs of a miscarriage.
The most common sign of a miscarriage is vaginal bleeding, which can vary from light red or brown spotting to heavy bleeding. If it is very early in the pregnancy, you may think that you have your period.
If it is very early in the pregnancy, you may think that you have your period.
Other signs may include:
- cramping pain in your lower tummy, which can vary from period-like pain to strong labour-like contractions
- passing fluid from your vagina
- passing of blood clots or pregnancy tissue from your vagina
What really happens during a miscarriage?
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
What should I do if I think I’m having a miscarriage?
If you are concerned that you are having a miscarriage, call your doctor or midwife for advice and support.
Keep in mind that many women experience vaginal spotting in the first trimester of pregnancy that does not result in a miscarriage.
If you are alone, consider calling your partner or a friend for help and support.
If you have very heavy bleeding, strong pain or feel unwell, call triple zero (000) or have someone take you to your nearest emergency department.
How is a miscarriage managed?
Unfortunately, nothing can prevent a miscarriage from happening once it has begun. What happens now depends on your own health and what is happening to you.
Each approach has benefits and risks. You should discuss these with your doctor.
Expectant or natural management
Also called ‘watch and wait’, expectant management may be recommended in early pregnancy. This involves going home and waiting until the pregnancy tissue has passed from your womb by itself. This can happen quickly, or it may take a few weeks.
Medical management
You may be offered medication that speeds up the passing of the pregnancy tissue. You may be asked to stay in hospital until the tissue has passed, or you may be advised to go home.
Surgical management
You may be advised to have a form of minor surgery called a 'dilatation and curettage' (also called a D&C or a curette). This procedure is often recommended if you have heavy bleeding, significant pain or signs of infection. It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
It may also be recommended if expectant or medical management has failed. You may also decide that you prefer this option.
This procedure is done under general anaesthesia in an operating theatre. It takes 5-10 minutes once you are asleep. The doctor opens the cervix and removes the remaining pregnancy tissue.
How is a miscarriage treated?
Once it is confirmed that you are having a miscarriage, your doctor may offer or recommend treatment. There are many options. All have benefits and risks — discuss these with your doctor.
If the miscarriage is complete
If it seems the miscarriage is complete, you should still see your doctor for a check-up. You may be advised to have an ultrasound to make sure your uterus is empty.
If you go to hospital
If you go to your hospital’s emergency department, you will be seen first by a triage nurse, who will assess how urgently you need to be seen by a doctor. Depending on your symptoms, you will either be taken in to see a doctor immediately, or you will be asked to wait.
If you are waiting to be seen and your symptoms become worse or you feel like you need to go to the toilet, let the staff know immediately.
What happens if I miscarry at home?
Some women miscarry at home before they have a chance to see their doctor or get to the hospital.
If this happens, then:
- use pads to manage the bleeding
- if you can, save any pregnancy tissue that you pass, as your doctor may recommend it is tested to see why your miscarriage happened
- take medications such as paracetamol if you have pain
- rest
- call your doctor or midwife
There is a chance you may see your baby in the tissue that you pass, but often the baby is too small to recognise, or may not be found at all. It is normal to want to look at the remains, but you may decide you do not want to. There is no right or wrong thing to do.
Some women miscarry while on the toilet. This can also happen if you are out and about, or in hospital. There is no right or wrong way to handle this.
There is no right or wrong way to handle this.
Why do miscarriages happen?
Many women wonder if their miscarriage was their fault. In most cases, a miscarriage has nothing to do with anything you have or have not done. There is no evidence that exercising, stress, working or having sex causes a miscarriage.
Most parents do not ever find out the exact cause. However, it is known that miscarriages often happen because the baby fails to develop properly, usually due to a chromosomal abnormality that was spontaneous, not inherited.
Occasionally, miscarriage is caused by:
- hormonal abnormalities
- immune system and blood clotting problems
- medical conditions such as thyroid problems or diabetes
- severe infections causing high fevers (not common colds)
- physical problems with your womb or cervix
What are the risk factors for miscarriage?
Women are more likely to have miscarriages if they:
- are older
- smoke
- drink alcohol in the first trimester
- drink too much caffeine in coffee, tea or energy drinks
- have had several previous miscarriages
Can you prevent a miscarriage?
Living healthily — no cigarettes, no alcohol and little to no caffeine — can decrease your risk of miscarriage. It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
It’s a good idea to avoid contact with people who have a serious infectious illness when you’re pregnant.
Who can I talk to for advice and support?
Talk to your doctor or midwife for information and advice on what do and how to look after yourself if you experience a miscarriage.
Your hospital should be able to provide details of available support services, such as bereavement support.
SANDS is an independent organisation that provides support for miscarriage, stillbirth and newborn death. You can call them on 1300 072 637 or visit www.sands.org.au.
You can also call Pregnancy, Birth and Baby on 1800 882 436, 7am to midnight (AET) to speak to a maternal child health nurse for advice and emotional support.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage.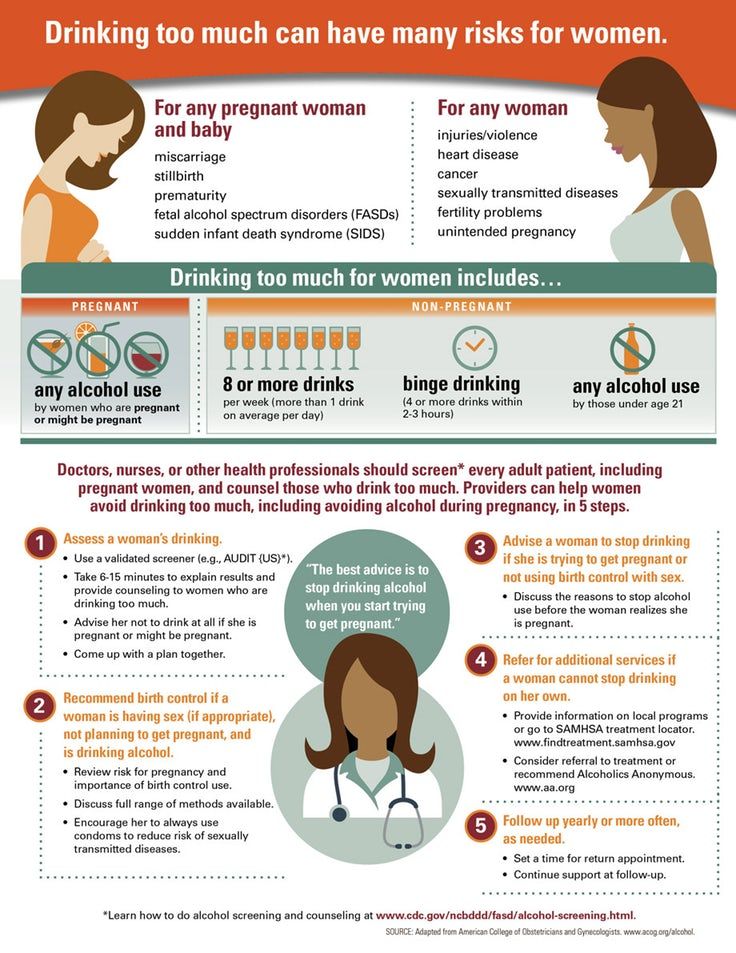 Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
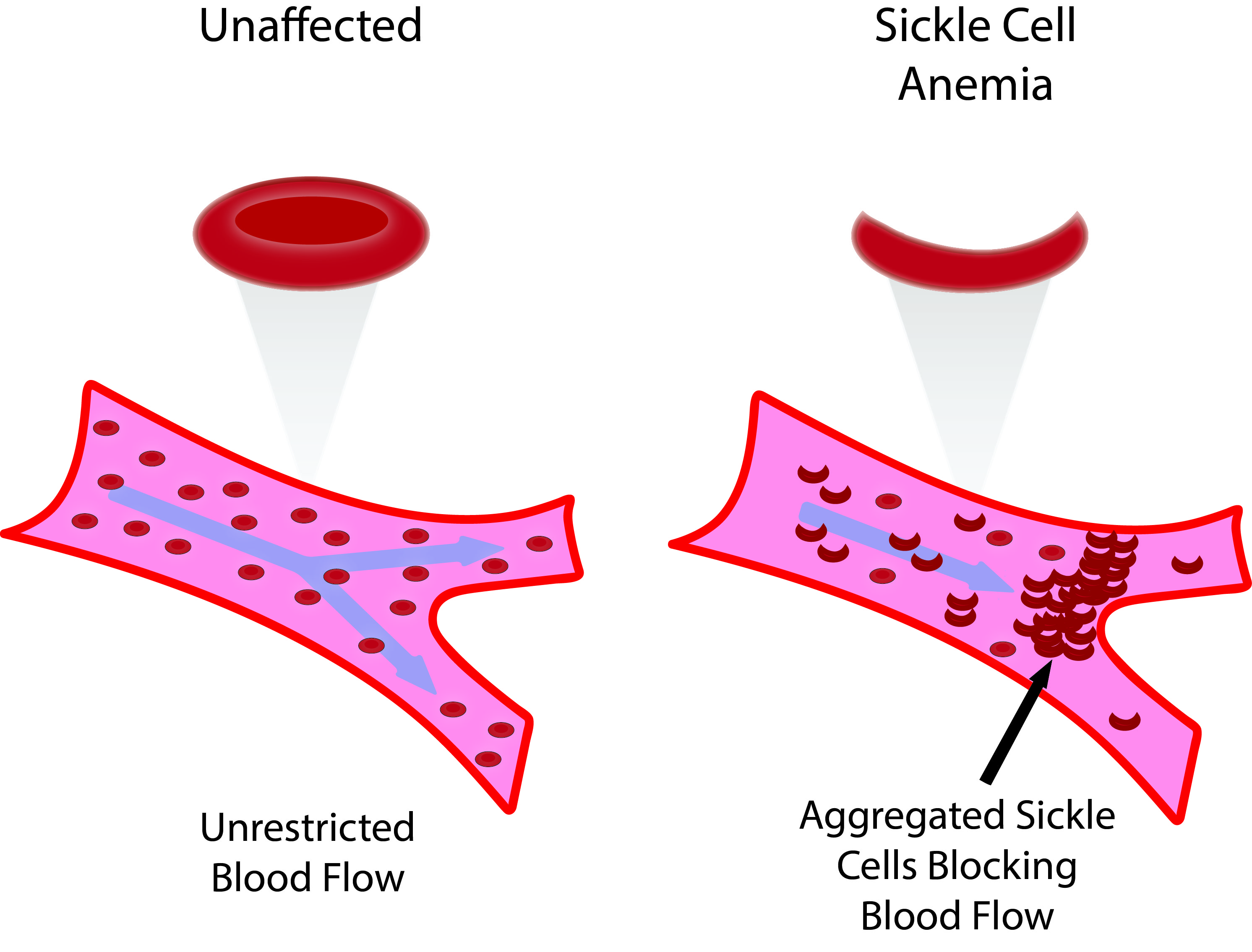
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be started.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
miscarriage, symptoms - Health Clinic 365 G.
 Yekaterinburg
Yekaterinburg Causes of miscarriage
Questions to the doctor about miscarriage
Diagnostics of miscarriage
Treatment and prevention of miscarriage
- this . According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Miscarriage symptoms .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Contact your doctor in the following cases:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can place a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy.