Itchy irritated vulva during pregnancy
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
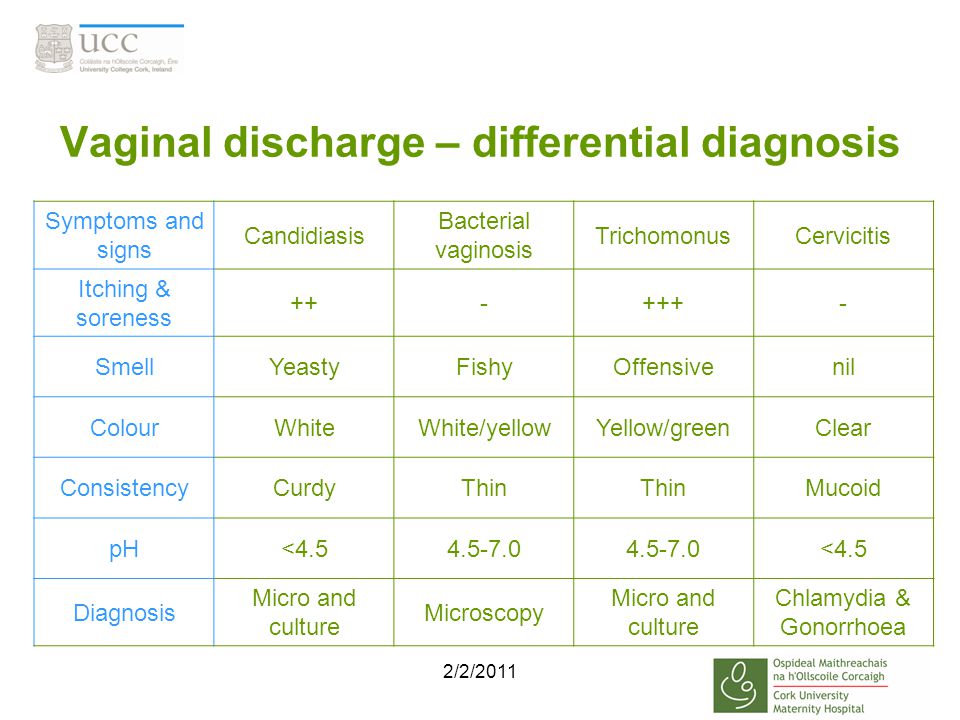
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast. The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women.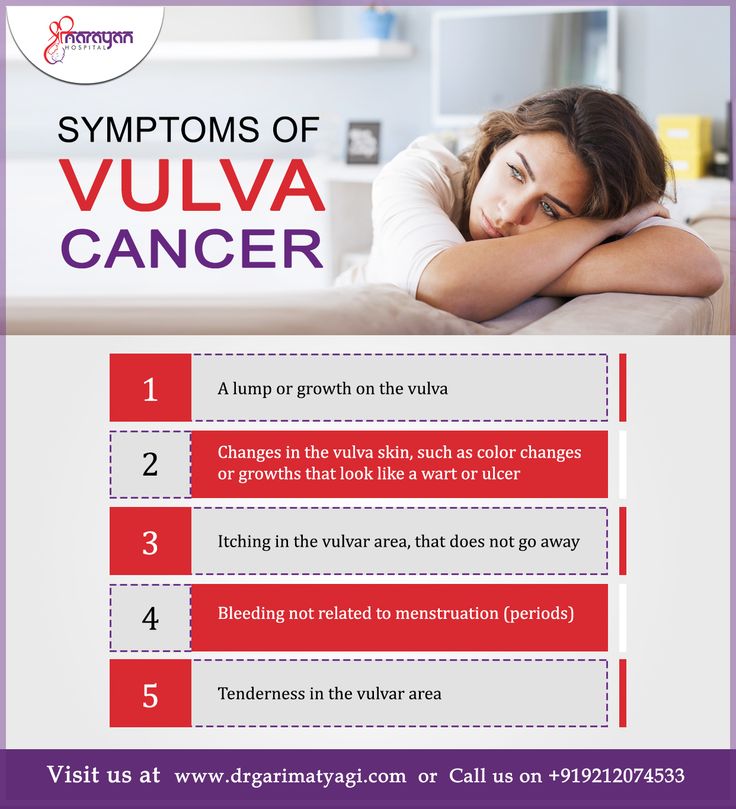 Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.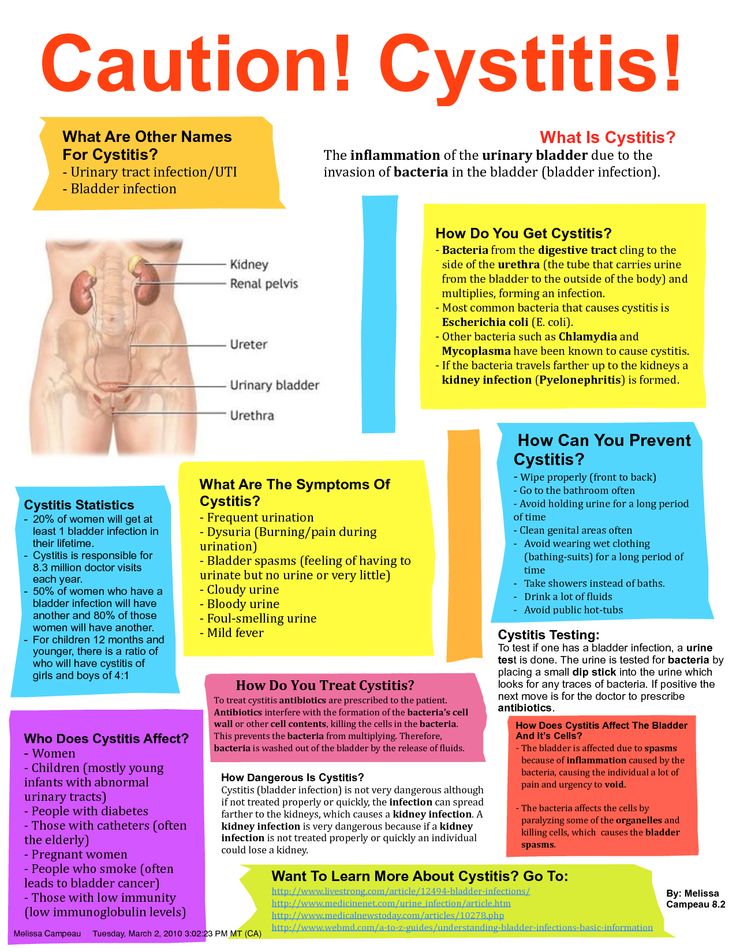
Symptoms include:
- frequent and urgent need to urinate
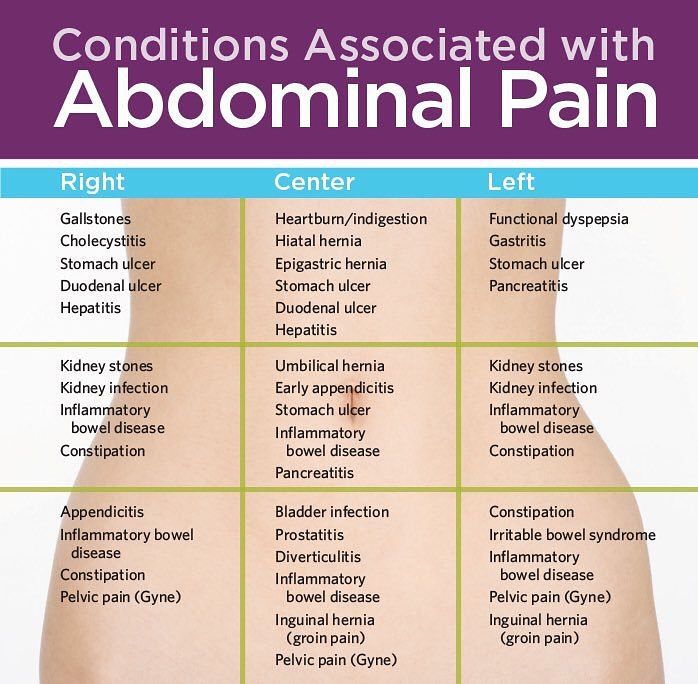
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.

- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
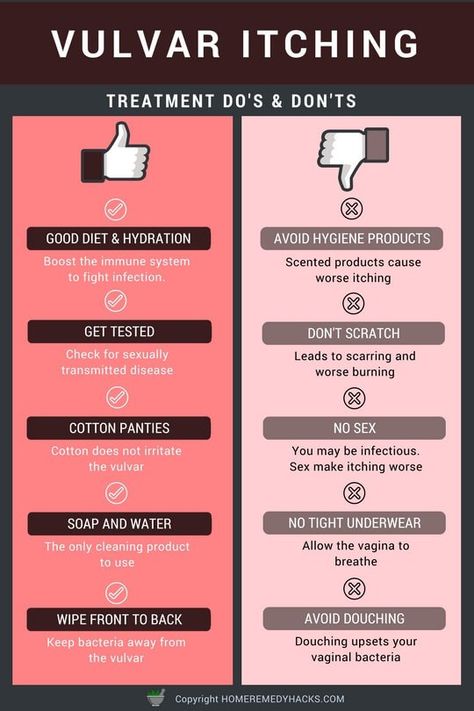
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.

- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast. The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women. Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.
Symptoms include:
- frequent and urgent need to urinate
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.
- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.

- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.
why does it occur and how to solve the problem?
Pregnancy is one of the important and responsible stages in a woman's life. In most cases, this is 9 months of anxious waiting to meet your baby. However, during pregnancy, a woman's body undergoes major hormonal changes and pleasant emotions can go hand in hand with painful and uncomfortable sensations in different areas of the body. Including unpleasant symptoms may appear in the intimate area. nine0003
Discomfort in the vagina often manifests itself in the form of itching, burning, irritation and swelling. The main thing, when these symptoms appear, is to understand that it is necessary to establish their cause and eliminate it as soon as possible, because there are risks of harming the health of the fetus.
Various sexual infections can affect the appearance of discomfort in the perineum. Unfortunately, during pregnancy, a woman is prone to various infectious diseases. As mentioned above, bearing a baby causes a restructuring of the hormonal background in a woman's body: the level of the hormone progesterone rises and the activity of the immune system naturally decreases, which creates favorable conditions for the exacerbation of chronic infections and the emergence of new ones.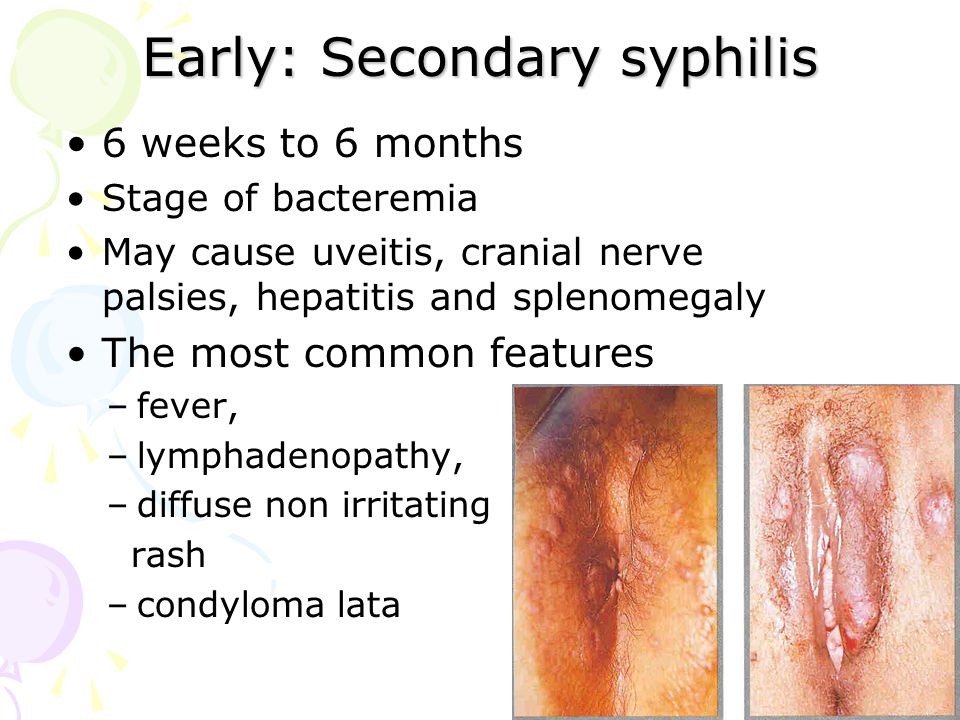 nine0003
nine0003
How dangerous is the development of infectious diseases of the vagina and vulva during the bearing of a baby? Normally, during pregnancy, the amniotic bladder and water, as well as the mucous plug of the cervix, protect the fetus from various infections and bacteria, so your unborn baby is safe.
The presence in the body of a woman in an interesting position of an infectious disease and the lack of necessary therapy can adversely affect the course of pregnancy. For example, an untreated infection can lead to damage to the membranes, the fluid in which the unborn child is located, and the fetus itself. nine0003
There is also a high probability of physical contact of the child with the infection during passage through the birth canal. Therefore, in case of any discomfort in the intimate area during pregnancy, you should consult a specialist.
You can suspect the appearance of an infection of the vagina and vulva by a series of symptoms: cramps, itching, burning. Often, sexual infections provoke colpitis - inflammation of the mucous membrane of the vagina and the vaginal part of the cervix. By itself, colpitis often causes discomfort in the groin of pregnant women. It can be provoked not only by sexual infections, but also by endocrine or chronic diseases, stress, lack of hygiene. nine0003
Often, sexual infections provoke colpitis - inflammation of the mucous membrane of the vagina and the vaginal part of the cervix. By itself, colpitis often causes discomfort in the groin of pregnant women. It can be provoked not only by sexual infections, but also by endocrine or chronic diseases, stress, lack of hygiene. nine0003
Bacterial vaginosis can also cause discomfort. This pathology, caused by a decrease in the number of lactobacilli in the vagina, as a result, their place is taken by other microorganisms that are always present in the vagina, but in excess lead to the development of dysbiosis. Bacterial vaginosis can occur without symptoms, but sometimes it occurs with clinical manifestations. It is usually accompanied by discomfort, as well as vaginal discharge that is white, gray, or yellow-green in color with an unpleasant "fishy" odor. nine0003
Bacterial vaginosis also adversely affects the course of pregnancy, can provoke inflammation of the pelvic organs, premature birth, chorioamnionitis - inflammation of the amniotic membranes and infection of the amniotic fluid.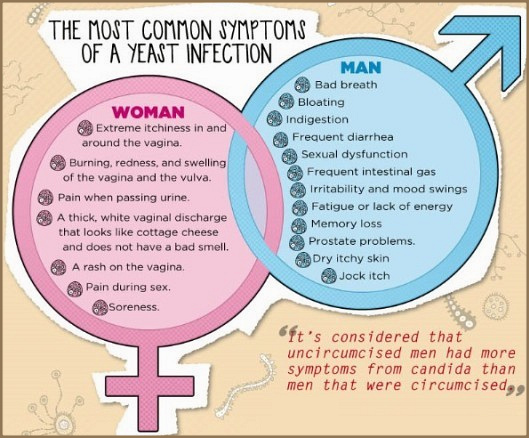
Itching in the intimate area during pregnancy can appear with vulvovaginal candidiasis - infection of the mucous membranes of the vulva and vagina with yeast-like fungi of the genus Candida. It should be noted that the first episode of the incidence of vulvovaginal candidiasis is observed during pregnancy. This is due to changes in hormonal levels, reduced immunity. This disease, in addition to discomfort in the groin area, itching and burning, is characterized by: moderate hyperemia, white and thick discharge like cottage cheese, sour smell from the vagina, pain during sexual intercourse and urination. nine0003
However, itching and burning are not always symptoms of serious pathologies. Occasionally, discomfort can occur with the use of poorly fitting underwear or aggressive pH soaps.
Feeling discomfort in the groin, you should consult with a specialist. The specialist can conduct an examination, collect an anamnesis and prescribe, if necessary, laboratory and / or other diagnostic tests. All this will help to establish a diagnosis and choose an individual treatment regimen. nine0003
All this will help to establish a diagnosis and choose an individual treatment regimen. nine0003
In order to prevent the appearance of discomfort in the intimate area and not spoil the pleasant waiting time for the addition, it is necessary to follow preventive recommendations.
- It is necessary to carry out external hygiene of the intimate area. Normally 2 times a day - no more and no less. Frequent washing can lead to “overdrying” of the skin and mucous membranes of the intimate area, and a lack of hygiene can lead to the development of various inflammations. You should not self-douche or vaginal lavage unless recommended by a specialist in your particular case. nine0031
- Choose a quality cleanser. Ideally, this should be a hypoallergenic product that is dermatologically tested, contains lactic acid and components that care for the skin of the genital organs. Epigen Intim Gel is ideal for daily hygiene of the inguinal zone during pregnancy and after childbirth.
 Epigen Intim gel contains activated glycyrrhizic and lactic acids in its composition. Its pH is slightly acidic, which corresponds to the normal acid-base balance of the skin of the intimate area. The tool helps to eliminate discomfort (irritation) due to wearing panty liners or not very comfortable underwear. It has a very pleasant aroma and helps to neutralize unpleasant odors in the intimate area with constant use. nine0031
Epigen Intim gel contains activated glycyrrhizic and lactic acids in its composition. Its pH is slightly acidic, which corresponds to the normal acid-base balance of the skin of the intimate area. The tool helps to eliminate discomfort (irritation) due to wearing panty liners or not very comfortable underwear. It has a very pleasant aroma and helps to neutralize unpleasant odors in the intimate area with constant use. nine0031 - Abandon synthetic underwear in favor of natural fabrics. Cotton panties do not create a "greenhouse effect", especially in the heat.
Treatment of discomfort in the intimate area will be different. The diagnosed disease will influence the choice of therapy. Spray Epigen Intim can be included in the complex treatment of diseases accompanied by discomfort - nonspecific colpitis (vaginitis), bacterial vaginosis, thrush, herpes. nine0003
Spray Epigen Intim
More
Buy
Epigen Intim Spray
The drug has antipruritic and anti-inflammatory action.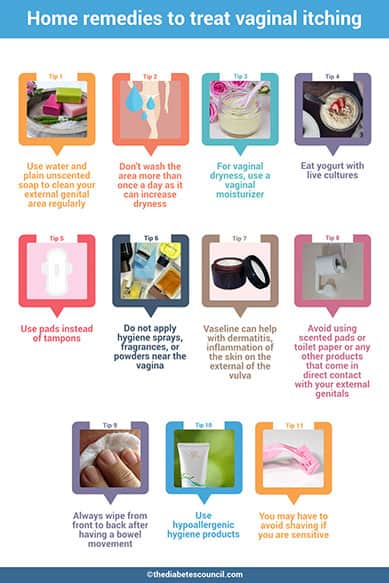 Thanks to the active ingredient - activated glycyrrhizic acid, Epigen Intim spray helps to eliminate itching and irritation. It also helps to eliminate inflammation, swelling and redness of tissues. The drug is also able to increase the local immunity of the vagina, by stimulating the production of its own interferons. Spray Epigen Intim promotes healing and restoration of the integrity of the damaged mucosa, due to which the protective function of the mucosa will be restored and the number of lactobacilli will increase. nine0003
Thanks to the active ingredient - activated glycyrrhizic acid, Epigen Intim spray helps to eliminate itching and irritation. It also helps to eliminate inflammation, swelling and redness of tissues. The drug is also able to increase the local immunity of the vagina, by stimulating the production of its own interferons. Spray Epigen Intim promotes healing and restoration of the integrity of the damaged mucosa, due to which the protective function of the mucosa will be restored and the number of lactobacilli will increase. nine0003
The drug is successfully used to treat viral infections (caused by the human papillomavirus, genital herpes), diseases associated with a decrease in local immunity (nonspecific vaginitis, thrush, bacterial vaginosis), etc. It can be used to treat exacerbations in conjunction with antiviral, antifungal and antimicrobial drugs, and for the prevention of these vaginal infections.
more nine0003
By the way, while carrying a baby, the use of many drugs sold in pharmacies is limited or prohibited.

But Epigen Intim spray is approved for use in pregnant and lactating women and is dispensed without a doctor's prescription. The drug is applied both externally and intravaginally, depending on the disease.
In the presence of itching, burning, irritation and swelling in the groin area, a woman feels as uncomfortable as possible. Intimate discomfort can bring especially many experiences to women during pregnancy. To minimize the risks of discomfort, try to follow the simple rules indicated in the article. When discomfort appears in the perineum, the most correct thing is to visit a specialist and not self-medicate, since now you are responsible not only for yourself, but also for the unborn baby. nine0003
Itching during pregnancy. What is Pregnancy Itching?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
Itching during pregnancy is a pathological condition that is a symptom of various diseases that have arisen or worsened during gestation. It is manifested by a sensation of painful tickling irritation of the skin and mucous membranes, which causes a scratching reflex. There may be a rash, other skin symptoms, signs of damage to various organs and systems. It is diagnosed with the help of biochemical, immunological, hormonal, allergological, microbiological studies, PCR, RIF, ELISA, ultrasound. For pathogenetic and symptomatic treatment of itching, antihistamines, corticosteroids, emollients, and sedative herbal remedies are used. nine0003
ICD-10
L29.8 Pruritus other
- Causes
- Pathogenesis
- Symptoms of itching during pregnancy
- Complications
- Diagnostics
- Treatment of itching during pregnancy
- Prognosis and prevention
- Prices for treatment
General
According to observations of obstetricians-gynecologists, temporary or permanent itching sensations of varying intensity occur in more than half of pregnant women. 45-50% of patients complain of genital (intimate), 18-22% - skin, 8-10% - anal itching. In some women during pregnancy, the simultaneous appearance of different types of itching is noted. Usually, the disorder develops as a result of an exacerbation of pre-existing diseases. In some cases, the cause of diseases, the symptom of which is itching, is the changes that occur during pregnancy. The relevance of timely diagnosis of the pathology that caused itching of the skin or mucous membranes is due to the risk of developing serious obstetric complications in some pathologies. nine0003
45-50% of patients complain of genital (intimate), 18-22% - skin, 8-10% - anal itching. In some women during pregnancy, the simultaneous appearance of different types of itching is noted. Usually, the disorder develops as a result of an exacerbation of pre-existing diseases. In some cases, the cause of diseases, the symptom of which is itching, is the changes that occur during pregnancy. The relevance of timely diagnosis of the pathology that caused itching of the skin or mucous membranes is due to the risk of developing serious obstetric complications in some pathologies. nine0003
Itching during pregnancy
Causes
Specialists in the fields of obstetrics name many factors that can provoke the occurrence of itchy sensations in pregnant women. Itching can manifest diseases that have become aggravated or that have arisen in the gestational period, systemic responses of the body to the action of exogenous agents and endogenous metabolites. The most common causes of the disorder are:
The most common causes of the disorder are:
- Skin and fungal diseases. Itching is observed in atopic and contact dermatitis, dermatophytosis, chronic lichen simplex, psoriasis, seborrhea, eczema. Itchy sensations are characteristic of a parasitic skin lesion - head and pubic lice, scabies. In the cold season, itching accompanies the development of xerosis. In many patients, these disorders are detected even before pregnancy, although infection with skin parasites or the manifestation of pathology is possible during the gestation period. nine0031
- System processes. Itching is accompanied by endogenous intoxication with natural and pathological metabolites in some forms of oncopathology (Hodgkin's lymphoma, polycythemia vera), liver diseases with cholestasis (viral hepatitis, gallstone disease, hepatosis), endocrinopathies (diabetes mellitus, hyperthyroidism, hypothyroidism), iron deficiency anemia, terminal renal failure with glomerulonephritis, pyelonephritis, hydronephrosis, nephrolithiasis.

- Genital infections. Often they are manifested not by skin, but by intimate itching that occurs due to irritation with toxins, and pathological secretions (whites). The symptom is more pronounced with candidiasis, genital herpes, gardnerellosis, chlamydia, gonorrhea. Reduced immunity and hormonal changes characteristic of pregnancy often lead to the development of bacterial vaginosis, one of the signs of which is itching in the genital area. nine0031
- Urological and proctological diseases. Itching in the perineum is caused not only by intense vaginal leucorrhea, but also by irritation with urine during frequent urination in pregnant women with urethritis, cystitis, pyelonephritis, pathological changes characteristic of hemorrhoids, anal fissures, local perianal dermatitis. One of the causes of anal itching is enterobiasis - helminthic invasion, in which part of the life cycle of the parasite is associated with skin lesions near the anus.
- Exogenous influences. The influence of a pathological agent can be external (through the skin and mucous membranes) and internal (after absorption in the gastrointestinal tract).
 In both cases, the development of an allergic or toxic systemic reaction with itching of varying intensity is possible. Provoking factors are most often drugs (aspirin, antibiotics, anesthetics), food, plant pollen, animal hair, dust, insect bites. nine0031
In both cases, the development of an allergic or toxic systemic reaction with itching of varying intensity is possible. Provoking factors are most often drugs (aspirin, antibiotics, anesthetics), food, plant pollen, animal hair, dust, insect bites. nine0031 - Neurological and psychiatric disorders. Tingling, paresthesia, intermittent intense itching caused by changes in the peripheral nervous system may be early signs of multiple sclerosis, preceding the main neurological symptoms. Neurogenic itching can be a consequence of stress, a sign of postherpetic neuralgia, brain tumors. In rare cases, itching manifests itself as part of a tactile hallucinosis.
- Dermatoses of pregnancy. In 1.5-3.0% of patients, usually with a hereditary predisposition, physiological changes during pregnancy (skin stretching with damage to the connective tissue, hyperestrogenism, immune restructuring) provoke an allergic reaction or intrahepatic bile stasis. As a result, one of the specific gestational pruritic dermatoses develops - atopic dermatitis, pemphigoid, cholestasis of pregnancy.
 nine0031
nine0031
Probable prerequisites for more frequent occurrence of itching in various diseases in pregnant women are an increase in dryness of the skin as a result of the influence of progesterone, a physiological decrease in immunity aimed at maintaining gestation, stretching and rupture of the connective tissue fibers of the skin with the formation of autoantigens, and a violation of the natural microflora of the vagina. Pregnancy also serves as a trigger for the development of a number of diseases accompanied by itching - gestational diabetes, postpartum autoimmune thyroiditis, etc. Additional risk factors are obesity, wearing synthetic clothing and underwear, the use of scented pads and irritating alkaline products for skin and genital care, non-compliance with the rules personal hygiene, the use of spicy food with seasonings, spices. nine0003
Pathogenesis
The mechanism of itching during pregnancy depends on the causes that caused it, however, the key link in the pathogenesis in all cases is the irritation of certain sections of the afferent pathways that transmit nerve impulses. Most often, itching occurs due to stimulation of peripheral nocireceptors. The receptor apparatus is usually affected by mediators formed during a local inflammatory, allergic, autoimmune reaction, microbial toxins, metabolites (bile acids, nitrogenous compounds, high concentrations of glucose), drugs. nine0003
Most often, itching occurs due to stimulation of peripheral nocireceptors. The receptor apparatus is usually affected by mediators formed during a local inflammatory, allergic, autoimmune reaction, microbial toxins, metabolites (bile acids, nitrogenous compounds, high concentrations of glucose), drugs. nine0003
Perhaps the development of itchy sensations due to damage, in which the inflammatory reaction is secondary, constant local influences (insect bites, movement of helminths, irritation with urine, leucorrhoea). Sometimes pathological afferentation, characteristic of itching, is noted against the background of microcirculatory disorders (for example, in diabetes mellitus), damage to sensory nerve fibers (with multiple sclerosis). With volume neoplasms of the brain, strokes, neurotic and mental disorders, the focus of pathological impulses, subjectively perceived as itching, is localized in the central parts of the nervous system. nine0003
Symptoms of itching during pregnancy
The main symptom of the disorder is local or generalized itching sensations of varying intensity, from slight tingling and burning to an unbearable desire to scratch or rub the skin, mucous membranes. Depending on the causes of itching, it can be constant or periodic, serve as the only sign of the disease or be accompanied by other skin manifestations - redness, scratching, macular, papular, vesicular, pustular rash, peeling. In general, the clinical picture is characterized by significant polymorphism, determined by the leading pathology, the symptom of which was skin or intimate itching. nine0003
Depending on the causes of itching, it can be constant or periodic, serve as the only sign of the disease or be accompanied by other skin manifestations - redness, scratching, macular, papular, vesicular, pustular rash, peeling. In general, the clinical picture is characterized by significant polymorphism, determined by the leading pathology, the symptom of which was skin or intimate itching. nine0003
Complications
Diseases with intense itching can be complicated by secondary infection of excoriated sites. The likelihood of developing obstetric complications depends on the influence of the underlying disease on pregnancy. Most skin diseases, transient allergic reactions, dermatosis of pregnant women cause discomfort and worsen the quality of life, but do not pose a serious threat to the woman and the fetus. In severe cholestasis of pregnant women, many systemic processes, the likelihood of gestosis, spontaneous miscarriage, premature birth, fetoplacental insufficiency, fetal growth retardation, anomalies in labor, coagulopathic bleeding, DIC increases. Possible complications of infectious diseases that occur with itching are chorioamnionitis, intrauterine infection of the fetus, postpartum endometritis, obstetric peritonitis. nine0003
Possible complications of infectious diseases that occur with itching are chorioamnionitis, intrauterine infection of the fetus, postpartum endometritis, obstetric peritonitis. nine0003
Diagnostics
The main task of a diagnostic search for complaints of a patient about itching of the skin, genitals, and perianal area is to identify the cause that caused the disorder. To make a diagnosis, a wide range of laboratory and instrumental diagnostic methods are used to determine the state of various organs and systems, to detect biochemical markers of the disease. In addition to a gynecological examination, general blood and urine tests during pregnancy, the following are recommended: nine0003
- Biochemical blood test. Indicative for some diseases are data on the level of glucose, bile acids, total bilirubin, cholesterol, triglycerides, serum iron, urea, uric acid, creatinine, enzymes (AlT, AST, alkaline phosphatase), the composition of blood protein fractions.

- Hormonal studies. To exclude endocrinopathies, manifested by itching of the skin, mucous membranes, an insulin resistance index, an assessment of the blood levels of insulin, TSH, thyroxine, triiodothyronine, and thyroxin-binding globulin are used. In some cases, determine the level of sex hormones. nine0031
- Study of immune and allergic status. Confirmation of the atopic nature of the disease is an increased concentration in the blood of IgE, histamine. In some disorders, specific markers of autoimmune processes (antibodies to collagen, AT-TPO, AT rTTG) are detected.
- Diagnosis of infections. Highly sensitive methods for detecting infectious diseases are polymerase chain reaction, RIF, ELISA. With their help, you can detect signs of genital herpes, candidiasis, chlamydia, mycoplasmosis, ureaplasmosis, and other urogynecological diseases. nine0031
- Culture of the detachable urogenital tract. Microbiological examination allows not only to determine the causative agent of an infectious disease, but also to assess its sensitivity to antibacterial drugs.
 The method is especially indicated for patients with itching of the vulva, vagina, urethra.
The method is especially indicated for patients with itching of the vulva, vagina, urethra.
In the presence of elements of the rash, a scraping or separated skin is analyzed. To assess the morphological state of various organs, ultrasound diagnostics that is safe for the fetus is used - ultrasound of the kidneys, liver, gallbladder, small pelvis. As additional methods, chemical and toxicological analyzes, histological examination of biopsy specimens, scraping for enterobiasis, and fecal analysis for helminth eggs can be recommended. Differential diagnosis is usually carried out between diseases in which itching occurs during pregnancy. In addition to an obstetrician-gynecologist and a dermatologist, according to indications, the patient is consulted by a venereologist, an infectious disease specialist, an endocrinologist, a gastroenterologist, a hepatologist and a urologist. nine0003
Treatment of itching during pregnancy
When developing tactics for managing a patient with complaints of itchy sensations, the influence of the underlying disease on gestation is taken into account. In most cases, it is possible to prolong pregnancy until the term of physiological birth. The treatment regimen is determined by the protocol for the relevant disorder, may include antibiotics, hormones, antifungal, hormonal, anticonvulsant drugs, drugs from other pharmacotherapeutic groups, taking into account their possible impact on fetal development. To reduce or eliminate itching, nonspecific pathogenetic and symptomatic therapy is effective: nine0003
In most cases, it is possible to prolong pregnancy until the term of physiological birth. The treatment regimen is determined by the protocol for the relevant disorder, may include antibiotics, hormones, antifungal, hormonal, anticonvulsant drugs, drugs from other pharmacotherapeutic groups, taking into account their possible impact on fetal development. To reduce or eliminate itching, nonspecific pathogenetic and symptomatic therapy is effective: nine0003
- Antihistamines. Due to the blockade of histamine receptors, the transmission of excitation along sensitive C-fibers decreases, the release of mediators by mast cells decreases. Suppression of an allergic reaction can significantly reduce the intensity of itching or completely stop it.
- Glucocorticoids. Local application of corticosteroid ointments, creams, emulsions has a pronounced antipruritic effect. Local treatment is more effective with limited dermatitis and dermatosis. Given the possible effects on the fetus, systemic corticosteroids during gestation are used to a limited extent.
 nine0031
nine0031 - Emollients. Since the skin becomes drier during pregnancy, which increases itching, its moisturizing and softening have a positive therapeutic effect. Means of this group also allow you to accelerate the restoration of damaged epidermis and lipid intercellular structures of the skin.
- Herbal sedatives. Due to the mutual influence of itching and emotional disorders (bad mood, irritability), the appointment of sedative preparations makes it possible to reduce the intensity of perception of uncomfortable sensations at the level of the central nervous system. Sedative therapy also contributes to the normalization of disturbed sleep. nine0031
The patient is advised to exclude from the diet foods that increase irritation or can cause allergies, normalize the drinking regimen, get enough rest, and avoid stress. Usually, natural delivery is recommended for pregnant women with itching. Caesarean section is performed only if there are obstetric indications.
Prognosis and prevention
In the absence of systemic disease, pregnancy outcomes in women with pruritus are usually favorable. The prognosis worsens when serious somatic diseases, endocrinopathies are detected. As a preventive measure, for patients suffering from skin and other pathologies, when planning pregnancy, it is necessary to take into account the recommendations of a dermatologist and specialized specialists. Pregnant women without concomitant pathology are advised to carefully observe the rules of personal hygiene, refuse synthetic underwear, moisturize the skin with natural means, avoid situations in which sweating increases sharply - staying in stuffy rooms, overheating in the sun. For washing linen and clothes, it is better to use phosphate-free neutral washing powders. nine0003
You can share your medical history, what helped you with the treatment of itching during pregnancy.
Sources
- Dermatoses in pregnant women: Abstract of the dissertation / Alenkina A.