Is it normal to have a runny nose during pregnancy
Baby (and tissues!) on board: Tips for managing pregnancy rhinitis | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
October 6, 2020
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
When you think of side effects or symptoms brought on by pregnancy, nasal congestion and runny nose are not typically among the first to come to mind.
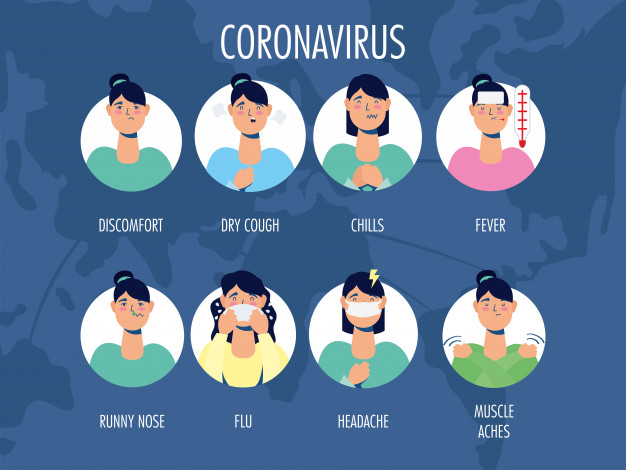
But maybe they should. Having a stuffy nose, difficulty breathing or sleeping, and snoring when pregnant can be alarming, especially amid the COVID-19 pandemic and the start of flu season.
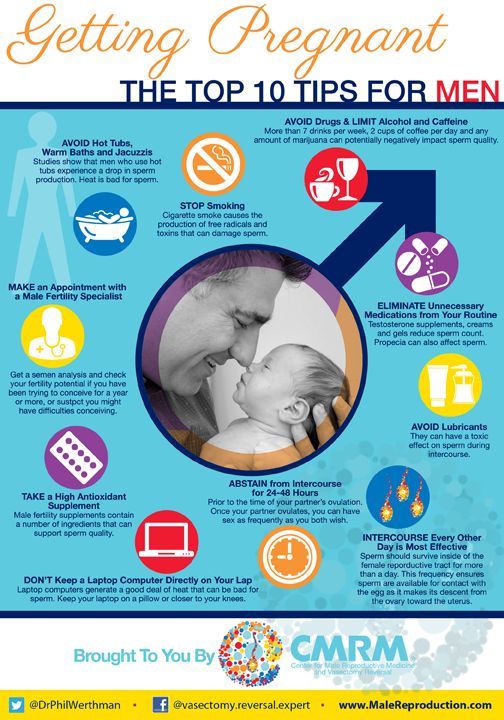
Pregnancy rhinitis, also called gestational rhinitis, is a common ailment in the second and third trimesters, affecting approximately 20% of women. Characterized by inflammation and swelling of the mucous membranes in the nose, pregnancy rhinitis symptoms include congestion (nasal obstruction), sneezing, postnasal drip, and runny nose. These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
All these issues can dramatically affect your mood and quality of life. The good news is that, for most patients, pregnancy rhinitis is temporary and there are safe, effective treatments available.
I've invited my colleague, Ashleigh Halderman, M.D., an ear, nose, and throat specialist at UT Southwestern to explain in more detail the causes of pregnancy rhinitis and how patients can manage their symptoms.
What causes pregnancy rhinitis?
Dr. Ashleigh HaldermanThe root cause of rhinitis can be allergic (affected by environmental irritants) or non-allergic (caused by infection). However, we are still learning how rhinitis is related to pregnancy.
We know that smoking, as well as having chronic rhinitis before pregnancy, predisposes patients to developing pregnancy rhinitis. Research suggests a few more potential causes:
Research suggests a few more potential causes:
- Having extra fluid in the body: During pregnancy, the body makes more blood and fluids, which can cause swelling, even in unexpected places such as the nasal passages. Blood vessels in the nose can swell with this additional volume, causing stuffiness.
- Higher levels of estrogen: Estrogen in older formulations of birth control pills has been associated with a side effect of nasal obstruction. However, in studies of the menstrual cycle, we don't see congestion with fluctuating estrogen levels. So, the connection remains unclear for now.
- Creation of human growth hormone: The placenta creates a variant of the human growth hormone (HGH), which has been associated with nasal symptoms in other conditions. For example, tumors that grow on the pituitary glands secrete growth hormones, which can cause severe nasal congestion.
Gestational rhinitis is under-researched. Data to date suggest no known association of rhinitis with pre-existing asthma, maternal age, duration of pregnancy, or the number of times a patient has been pregnant. However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
Related reading: How to manage allergies and asthma during pregnancy
How long do symptoms last?
The annoying, uncomfortable symptoms of pregnancy rhinitis typically last six weeks or longer. For most patients, symptoms typically resolve two weeks after delivery.
Approximately a third of patients who had chronic rhinitis before pregnancy will have the same level of symptoms during, and a third will experience worsening of rhinitis symptoms. However, the remaining third will have less severe or no symptoms during pregnancy. I've had many women tell me they've felt the best, sinus-wise, when they were pregnant. However, there's no specific reason why this occurs.
Related reading: 5 weird pregnancy symptoms you might not know about
What treatments are available?
The first step toward relief is a visit with your doctor to rule out infection, such as COVID-19, influenza, or sinusitis.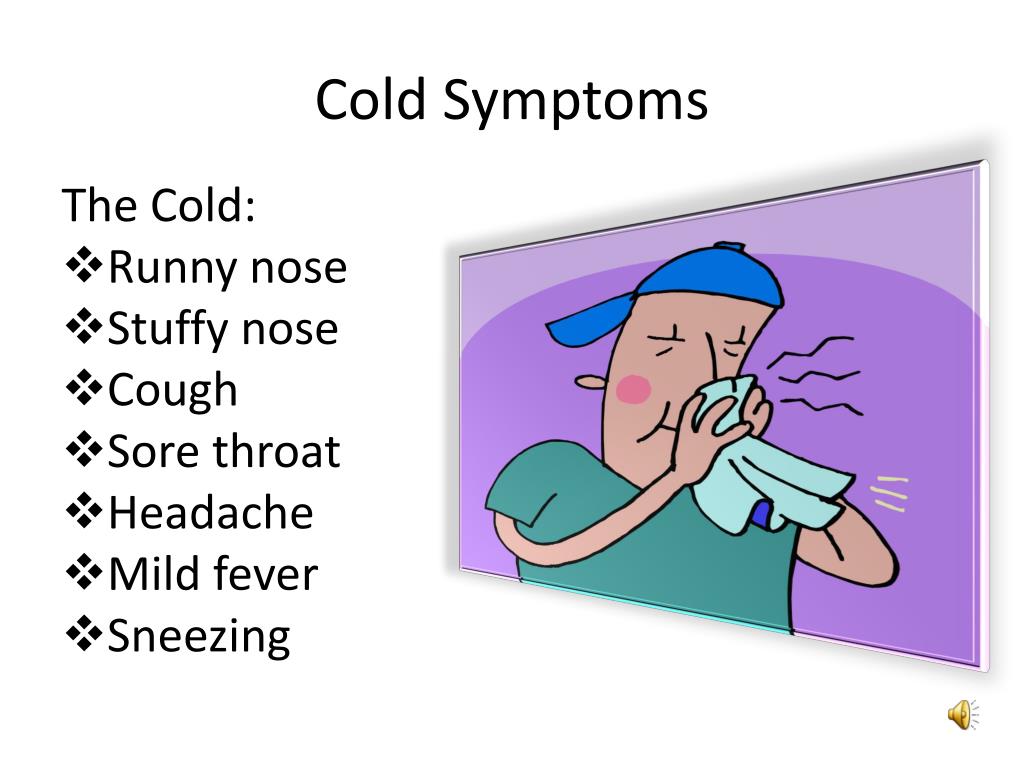 We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
From there, your doctor and Ob/Gyn may suggest:
- Getting regular exercise: Working out has been shown to significantly help relieve nasal congestion and regulate the sleep cycle. All the more reason to bust a move during pregnancy!
- Elevating your mattress: Try positioning the mattress so your whole body is situated at a 45-degree angle. While not widely studied, patients have reported that this helps clear the nasal passages enough to sleep.
- Using a humidifier: Adding a little moisture to the air can help alleviate nasal irritation. Many patients use them at night to wake up feeling less stuffy.
- Trying a sinus wash: Nasal saline sprays or sinus irrigation systems such as a neti pot can help clear the sinuses. Make sure to use distilled or boiled (and cooled) water – using water straight from the tap is not recommended.
Topical decongestants such as Afrin can be incredibly and immediately effective, but there is a risk of dependency. If you use this type of treatment more than once or twice a week, your nose can become "addicted" to it, which can lead to rhinitis medicamentosa – the spray will stop working as well, and your symptoms may get worse. Also, unlike gestational rhinitis, rhinitis medicamentosa won’t resolve after you deliver. It will only resolve when you stop using topical decongestants.
In general, pregnant patients can take decongestants that include pseudoephedrine as directed. However, we always recommend talking with your Ob/Gyn first, especially if you have high blood pressure.
Your Ob/Gyn might also recommend a steroid nasal spray, such as Flonase or Rhinocort, for severe symptoms. If you were using a spray to manage chronic rhinitis prior to pregnancy, your Ob/Gyn might advise you to keep using it during pregnancy. It is generally considered safe to use these products while breastfeeding, under your Ob/Gyn's guidance.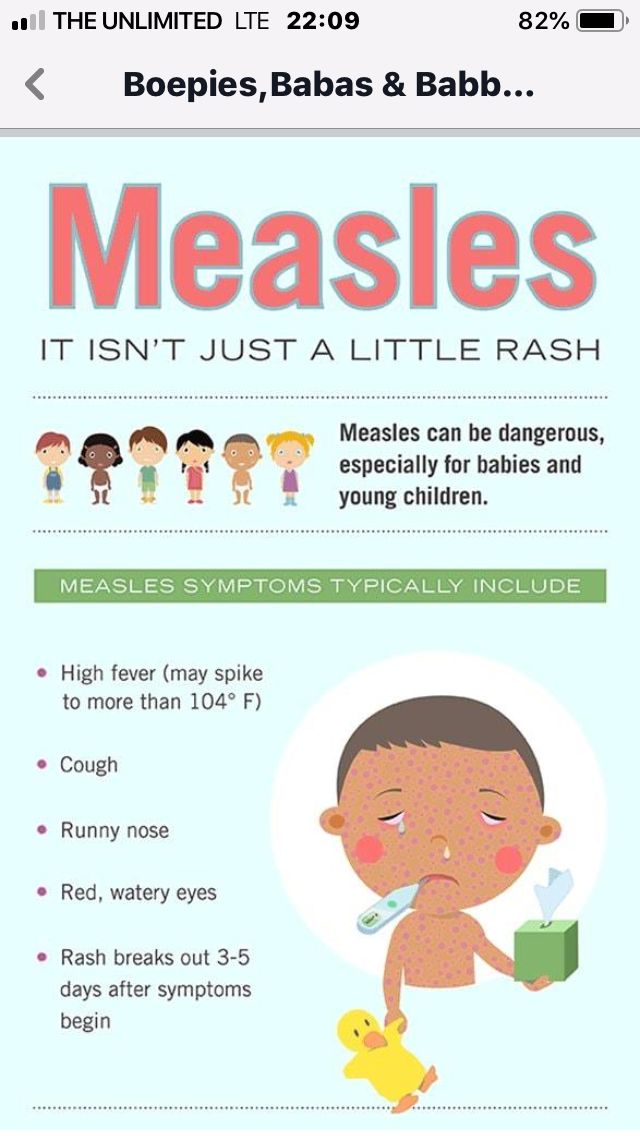
Your body will change in interesting ways during pregnancy. If you have new or unusual symptoms, call your doctor. We'll help you sort out what's normal from what could be a sinus infection or respiratory illness.
To talk with a doctor about nasal symptoms during pregnancy, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.
 D.
D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
More Articles
Pregnancy rhinitis | Pregnancy Birth and Baby
Pregnancy rhinitis | Pregnancy Birth and Baby beginning of content5-minute read
Listen
If you have unexplained breathing problems, see your doctor as soon as possible. If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
What is pregnancy rhinitis?
Pregnancy rhinitis usually involves a stuffy nose, itchy eyes, and post-nasal drip. These symptoms seem to come out of nowhere during pregnancy. While it's not a life-threatening medical condition, pregnancy rhinitis can be bothersome. There are things you can do to find some relief.
What are the symptoms pregnancy rhinitis?
Symptoms of pregnancy rhinitis are like those of allergic rhinitis (hay fever). These include:
- a runny or congested nose
- sneezing
- itchy eyes
- watery eyes
While it might feel like you are getting a cold, pregnancy rhinitis is not associated with bacterial or viral infection. This means it is not contagious.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
What causes pregnancy rhinitis?
Rhinitis is an inflammation of the lining of your nose.
People who are affected by allergies may also experience similar symptoms during pregnancy. In these circumstances, symptoms are triggered by one or more allergens. These allergens may be seasonal, such as:
- pollens
- fungi
- moulds
Or they can be perennial (year-round) such as:
- dust mites
- pets
- cockroaches
Rhinitis in pregnancy may also have a non-allergic origin. It's not known exactly why rhinitis occurs more frequently in pregnancy. Some research suggests that factors such as hormones increase the likelihood of rhinitis during pregnancy.
Smoking is also associated with pregnancy rhinitis. It's never too late for future parents to quit smoking.
How is pregnancy rhinitis diagnosed?
Pregnancy rhinitis should be distinguished from other conditions such as infections.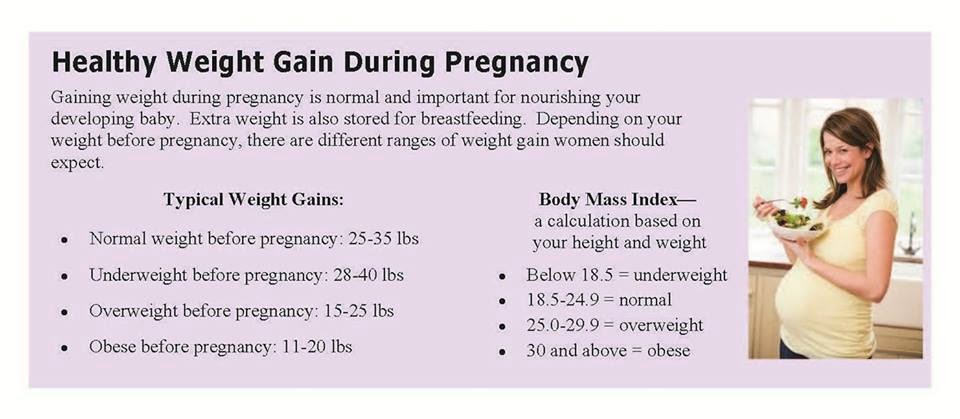 Your doctor can do this during a routine visit.
Your doctor can do this during a routine visit.
You may have a breathing problem if:
- you feel you can't get enough air through both your nose and mouth
- you are breathless
- you feel like you're being suffocated
- your chest feels very tight
- you are needing more of your usual asthma or lung medications
If you have unexplained breathing problems, see your doctor as soon as possible. If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How long will my symptoms last?
While pregnancy rhinitis can occur at any time during your pregnancy, it is most common during the first trimester.
Symptoms may last for at least 6 weeks. The good news is they usually disappear within 2 weeks of your baby's birth.
How is pregnancy rhinitis treated?
Your pregnancy rhinitis may be triggered by a known allergen. If this is the case, you can try and avoid or limit your exposure to the allergen.
Nasal irrigation is a drug-free technique to clear out air-borne allergens and mucus from blocked nostrils.
Using salt water (saline) nasal sprays can provide relief and is a good solution during pregnancy.
Persistent symptoms are managed individually. If you have itchy-watery eyes, there are certain eye drops that are approved for use during pregnancy. Similarly, specific medicated nasal sprays and antihistamines can be used.
However, always check with your doctor or pharmacist before taking any medicine while pregnant.
Is there an impact on my unborn baby?
There are insufficient studies to fully understand the impact of pregnancy rhinitis on the growth and development of unborn babies.
However, any condition that reduces your quality of life has the potential to affect your baby.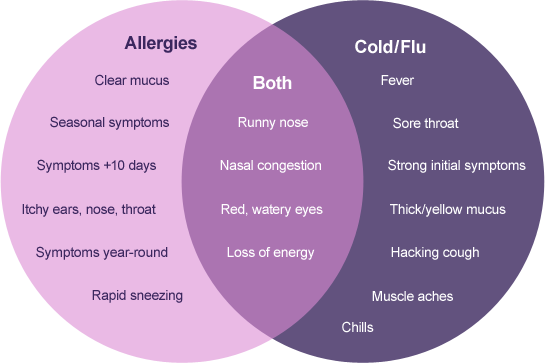 This includes the quality of your sleep during pregnancy.
This includes the quality of your sleep during pregnancy.
If you are concerned about your sleep or breathing during pregnancy, speak to your doctor. They can help you find the best way to clear your breathing passages and improve your sleep.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Auris Nasus Larynx (Medical Management of rhinitis in pregnancy), American Journal of Rhinology & Allergy (Redefining Pregnancy-induced Rhinitis), International Journal of Chemistry, Mathematics and Physics (Chronic Rhinosinusitis and Its Impact on Pregnancy), South Eastern Sydney Local health District/The Royal Hospital for Women (Hay Fever in Pregnancy and Breastfeeding), The Royal Women’s Hospital (Medicines in Pregnancy), Australasian Society of Clinical Immunology and Allergy (ASCIA) (Allergic Rhinitis Clinical Update)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Medicines during pregnancy
- Cold and flu during pregnancy and breastfeeding
- Allergies: controlling your environment
- Airborne allergies
- Allergies and hay fever during pregnancy
Need more information?
Allergic rhinitis - symptoms, causes and treatment - MyDr.com.au
Rhinitis means inflammation of the lining of the nose. Allergic rhinitis means that this inflammation is caused by an allergy.
Read more on myDr website
Allergic rhinitis (hay fever)? - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Allergic rhinitis (commonly known as hay fever) affects around 18% of people in Australia and New Zealand. It can affect children and adults.
It can affect children and adults.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergic Rhinitis (hayfever) - Allergy & Anaphylaxis Australia
Allergic rhinitis (hay fever) is one of the most common allergic conditions affecting 1 in 5 people in Australia. It is caused by the body’s immune system reacting to common allergens in the environment such as pollen, house dust mite, moulds and animal danders (skin cells and fur).
Read more on Allergy and Anaphylaxis Australia website
Hay Fever (Allergic Rhinitis) - Australasian Society of Clinical Immunology and Allergy (ASCIA)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) is the peak professional body of clinical immunology and allergy in Australia and New Zealand. ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Immunotherapy for Allergic Rhinitis (Hay Fever) - Allergy & Anaphylaxis Australia
Allergen Immunotherapy (AIT) has been used for over 100 years and is a proven treatment providing long-term relief for hay fever. The aim of AIT is to help people react less to their trigger allergen/s that cause symptoms (such as grass pollen/house dust mite). This means having no/less symptoms and a better quality of life.
Read more on Allergy and Anaphylaxis Australia website
Pollen - a trigger for hay fever - National Asthma Council Australia
Plant pollen is well known as a trigger for seasonal allergic rhinitis (hay fever) and seasonal allergic conjunctivitis.
Read more on National Asthma Council Australia website
Hay Fever & Asthma | Hay Fever-related Asthma Causes & Symptoms - Asthma Australia
Hay fever is a common allergy, also known as allergic rhinitis, that can also trigger asthma flare-ups. Learn more about hay fever-related asthma & symptoms here.
Read more on Asthma Australia website
Other Allergic Conditions - Allergy & Anaphylaxis Australia
Other Allergic Conditions included: Urticaria (Hives), Eczema (Atopic Dermatitis), Allergic Conjunctivitis, Allergic Rhinitis (hayfever), Sinusitis
Read more on Allergy and Anaphylaxis Australia website
Thunderstorm asthma - Australasian Society of Clinical Immunology and Allergy (ASCIA)
It seems reasonable to think that rain would relieve allergic rhinitis (hay fever) and asthma triggered by pollen, by washing pollen out of the air. However, rain from some thunderstorms can make some people's symptoms worse. Epidemics of thunderstorm asthma in Australia have occurred in Melbourne and Wagga Wagga.
However, rain from some thunderstorms can make some people's symptoms worse. Epidemics of thunderstorm asthma in Australia have occurred in Melbourne and Wagga Wagga.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergy Treatments - Australasian Society of Clinical Immunology and Allergy (ASCIA)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) is the peak professional body of clinical immunology and allergy in Australia and New Zealand. ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.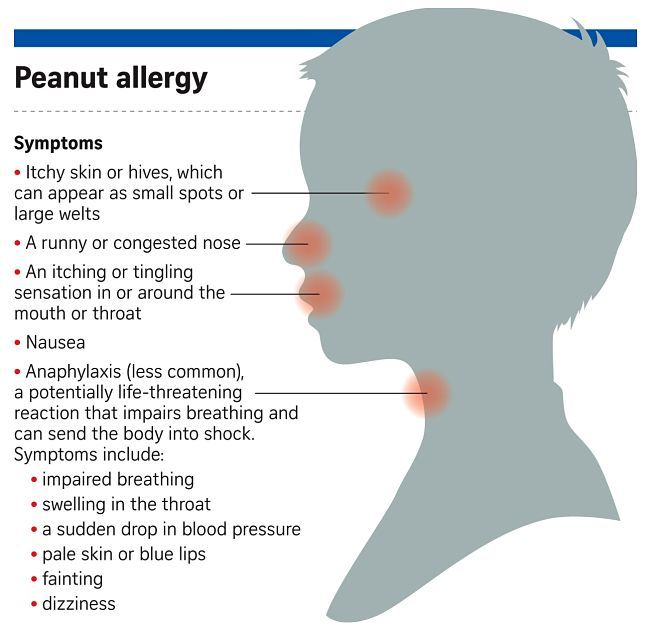
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnancy rhinitis - why does it occur and how to treat it?
Rhinitis of pregnant women is not dangerous, but worsens the quality of life of a woman during pregnancy.Article rating
3.28 (Votes: 36)
Contents
- How long does pregnancy rhinitis occur and how long does it last?
- Symptoms of pregnancy rhinitis
- Causes of pregnancy rhinitis
- How to distinguish the symptoms of rhinitis during pregnancy from other pathologies?
- Treatment of rhinitis of pregnant women
- General recommendations for pregnant women who have symptoms of rhinitis
- Drugs for the treatment of rhinitis
Rhinitis of pregnancy (nasal obstruction) is a common pathology that occurs in about 30% of expectant mothers. Manifested by a typical triad of symptoms: nasal congestion, difficulty breathing, the presence of mucous secretions. By itself, it is not dangerous, but worsens the quality of life of a woman during pregnancy. The difficulty of stopping the pathology and relieving symptoms lies in the fact that during pregnancy there are restrictions on the use of a number of physiotherapeutic methods and drugs.
Manifested by a typical triad of symptoms: nasal congestion, difficulty breathing, the presence of mucous secretions. By itself, it is not dangerous, but worsens the quality of life of a woman during pregnancy. The difficulty of stopping the pathology and relieving symptoms lies in the fact that during pregnancy there are restrictions on the use of a number of physiotherapeutic methods and drugs.
When does pregnancy rhinitis occur and how long does it last?
Most often, pathology occurs:
- up to and including the 20th week of pregnancy - in this case, rhinitis usually resolves on its own (after about a month or two) and does not manifest itself in the later stages;
- after the 20th week of pregnancy - this condition can continue until childbirth and after them (after 2-3 weeks).
If the symptoms last longer than two months and are not relieved by any independent action (vasoconstrictor sprays are prohibited!), then the cause may be hiding in a chronic disease.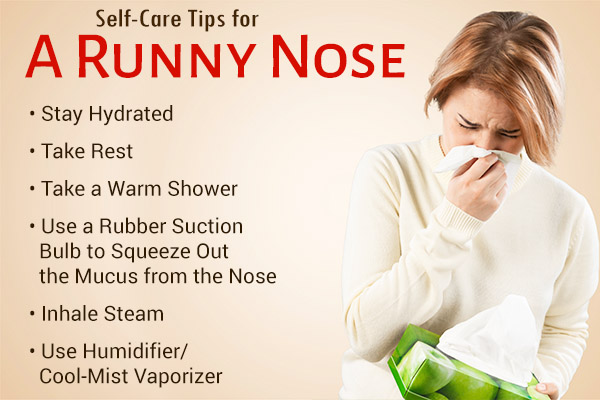
Symptoms of pregnancy rhinitis
- Difficult nasal breathing, nasal congestion;
- Nasal discomfort, sneezing;
- Presence of clear mucous discharge;
- Feeling of constriction in the region of the nose and sinuses;
- Mild headaches.
Difficulty in nasal breathing in the mother leads to sleep disturbance and hypoxia, which is also felt by the fetus.
Causes of pregnancy rhinitis
The pathogenesis of the disease is still a controversial issue. Most doctors are inclined to believe that it is of a hormonal nature and is associated with an increased level of estrogen and acetylcholine in the blood serum (as a result), which leads to hyperemia of the nasal mucosa and swelling. The concentration of estradiol, estrone, estriol in the bloodstream of pregnant women increases, in some future mothers, for this reason, the shape of the nose may change, it may increase in size.
There is evidence that pregnant women with symptoms of vasomotor rhinitis have elevated serum placental hormone levels. Another reason that can cause long-term nasal obstruction is the tone of smooth muscle cells under the influence of the inhibitory action of the steroid hormone progesterone. It causes fluid retention in the body and has such a side effect on the nasal mucosa.
Another reason that can cause long-term nasal obstruction is the tone of smooth muscle cells under the influence of the inhibitory action of the steroid hormone progesterone. It causes fluid retention in the body and has such a side effect on the nasal mucosa.
Histochemical studies have shown that nasal congestion may occur due to plethora due to hyperactivity of the parasympathetic nervous system in pregnant women.
How to distinguish the symptoms of pregnancy rhinitis from other pathologies?
Symptoms of rhinitis during pregnancy are really similar to manifestations of other diseases, for example, viral infections, sinusitis. It is difficult for a future mother to distinguish a pathology by external signs, therefore a doctor's consultation is necessary. Our clinic employs specialists with extensive experience who will quickly diagnose and prescribe treatment.
If the symptoms are accompanied by a sore throat, fever, then this indicates the presence of a bacterial and/or viral infection or other inflammatory process.
With sinusitis, mucous discharge may have a yellowish or greenish tinge. When pressing in the area of the maxillary and frontal sinuses, there are painful sensations, when the head is tilted, the pain may intensify. Also, sinusitis often causes an increase in temperature, while with nasal obstruction, such symptoms are not observed.
Sometimes rhinitis of pregnancy is confused with allergic rhinitis, which may worsen, there may be sensitization to allergens to which patients have not previously reported sensitivity.
Treatment of pregnancy rhinitis
In our clinic, a thorough diagnosis is carried out in order to exclude diseases similar to rhinitis in terms of symptoms. After the examination, individual treatment is prescribed depending on the severity, severity and indications.
Treatment is complicated by the fact that many drugs can cause contraction of the myometrium and fetal circulation or vasoconstriction with impaired placental function. Therefore, a doctor should prescribe drug therapy, you can not use drugs on your own - they can cause a violation of the development of the fetus.
Therefore, a doctor should prescribe drug therapy, you can not use drugs on your own - they can cause a violation of the development of the fetus.
General advice for pregnant women with symptoms of rhinitis
- Washing the nose with mild saline solution (2 teaspoons of sea salt per glass of water). Salt solution improves the discharge of nasal mucus and reduces the feeling of congestion.
- Nasal douches (nose washers) are very helpful. You can use regular saline for them.
- Ventilate the room before going to bed, use humidifiers. Dry air can exacerbate unpleasant symptoms.
- Use a high pillow (or multiple pillows) to sleep with your head well above your torso.
- Walking in the fresh air before going to bed is useful.
- Do morning exercises and breathing exercises several times a day to reduce the symptoms of hypoxia.
- Do not wear perfume and stay away from smokers.
Do not use vasoconstrictor nasal drops during pregnancy as they may cause vasomotor rhinitis.
Preparations for the treatment of rhinitis
Preparations for use during pregnancy are selected with great care and individually. Pregnant women are not given oral systemic corticosteroids, although their effect on the fetus is not fully understood. In some cases, the doctor prescribes corticosteroids in the form of aerosols. Oral antihistamines are also not prescribed due to the increased risk of embryopathies. The choice of physiotherapy is also limited, because most methods negatively affect the development of the fetus.
If you suffer from rhinitis, headaches or other unpleasant symptoms, we advise you to see a doctor immediately. Timely treatment is the key to the quality of life of the mother, which is very important for bearing the fetus. And also allows you not to miss other more serious diseases that can adversely affect the health of the mother and child.
Important! Do not use drugs that were prescribed to you by a doctor before pregnancy, or drugs prescribed to someone else.
Rhinitis during pregnancy usually does not pose a threat to either the fetus or the mother, but improper treatment can lead to unpredictable consequences.
Seeing a doctor early can help keep you healthy.
Don't delay treatment, call now. We work around the clock in Moscow.
tel.: 8 (499) 501-15-53 (24 hours)
treatment of diseases of the ear, throat, nose in children and adults
This normalizes the pressure in the chest cavity and cranial cavity, which contributes to the best blood circulation in the vital organs. Back in the 19th century, it was found that nasal congestion leads to problems with heart rhythm, and also negatively affects the functioning of the gastrointestinal tract. Therefore, nasal congestion should not be neglected! Moreover, you should pay close attention to the runny nose for pregnant women.
Not everyone knows, but the nose is closely related to the work of the female reproductive system. The so-called genital points of Fliess are located in the region of the anterior end of the middle turbinate and in the mucous membrane of the tubercle of the nasal septum. During normal nasal breathing, reflexes from these points contribute to the optimal physiological function of the female genital organs. In diseases of the nose and paranasal sinuses with difficulty in nasal breathing, normal reflexes disappear from these points, pathological reflexes appear and various diseases or dysfunctions of the female genitalia occur, which may be associated, including premature birth, weak labor activity, pathology fetus. In addition, in the course of a series of experiments, it was found that irritation of the nasal mucosa is accompanied by a stronger contraction of the uterus than its contraction due to irritation of other parts of the body. In this regard, it is very important to pay special attention to the prevention of diseases of the nose and paranasal sinuses in pregnant women.
The so-called genital points of Fliess are located in the region of the anterior end of the middle turbinate and in the mucous membrane of the tubercle of the nasal septum. During normal nasal breathing, reflexes from these points contribute to the optimal physiological function of the female genital organs. In diseases of the nose and paranasal sinuses with difficulty in nasal breathing, normal reflexes disappear from these points, pathological reflexes appear and various diseases or dysfunctions of the female genitalia occur, which may be associated, including premature birth, weak labor activity, pathology fetus. In addition, in the course of a series of experiments, it was found that irritation of the nasal mucosa is accompanied by a stronger contraction of the uterus than its contraction due to irritation of other parts of the body. In this regard, it is very important to pay special attention to the prevention of diseases of the nose and paranasal sinuses in pregnant women.
In general, the concept of "runny nose" is a household and simple generalized name for more than two dozen different diseases known to specialists. The Internet and the pages of various near-medical magazines are full of all kinds of "good" advice on its treatment. These are decoctions of herbs, and plant juices, and even secretions from human and animal organisms. With the results of such alternative treatment, then ENT doctors have to fight. Burns of the nasal mucosa, allergic reactions, severe sinusitis - this is an incomplete list of possible consequences. Therefore, when a runny nose appears, it is not recommended to delay visiting a specialist, and even more so to apply untested and medically unreasonable methods of treatment to yourself.
The Internet and the pages of various near-medical magazines are full of all kinds of "good" advice on its treatment. These are decoctions of herbs, and plant juices, and even secretions from human and animal organisms. With the results of such alternative treatment, then ENT doctors have to fight. Burns of the nasal mucosa, allergic reactions, severe sinusitis - this is an incomplete list of possible consequences. Therefore, when a runny nose appears, it is not recommended to delay visiting a specialist, and even more so to apply untested and medically unreasonable methods of treatment to yourself.
Returning to the topic of the question, I would like to note that during pregnancy, the most common diseases of the nose and paranasal sinuses in patients are: acute rhinitis (acute rhinitis), sinusitis (or sinusitis), allergic rhinitis and hypertrophic rhinitis (varieties of chronic rhinitis).
Consider the main diseases. Acute rhinitis is an acute infectious disease that occurs with inflammation of the nasal mucosa, most often caused by viruses (rhinovirus, adenovirus, parainfluenza virus, etc. ). From the very beginning, it is preferable to use synthetic preparations of interferon, the main antiviral protection factor, for example, the drug "Grippferon" for treatment. Unfortunately, this group of drugs is officially contraindicated for pregnant women. But it is possible to use frequent irrigation of the nasal cavity with saline solutions in order to reduce the concentration of irritants on the mucous membrane. It is very important not to ignore the indication: in case of a cold, keep your feet warm and avoid drafts. Cold irritation of the receptors of the skin of the feet reflexively increases the permeability of the vessels of the upper respiratory tract, facilitating the penetration of the infection into the body. Do not rush at the slightest sign of a cold and acute rhinitis to pour vasoconstrictor drops into the nose in abundance: naphthyzinum, glazolin, sanorin and other analogues. Edema of the nasal mucosa is a positive, evolutionarily acquired, protective phenomenon that prevents the virus from entering the body further through the barrier - the nasal mucosa.
). From the very beginning, it is preferable to use synthetic preparations of interferon, the main antiviral protection factor, for example, the drug "Grippferon" for treatment. Unfortunately, this group of drugs is officially contraindicated for pregnant women. But it is possible to use frequent irrigation of the nasal cavity with saline solutions in order to reduce the concentration of irritants on the mucous membrane. It is very important not to ignore the indication: in case of a cold, keep your feet warm and avoid drafts. Cold irritation of the receptors of the skin of the feet reflexively increases the permeability of the vessels of the upper respiratory tract, facilitating the penetration of the infection into the body. Do not rush at the slightest sign of a cold and acute rhinitis to pour vasoconstrictor drops into the nose in abundance: naphthyzinum, glazolin, sanorin and other analogues. Edema of the nasal mucosa is a positive, evolutionarily acquired, protective phenomenon that prevents the virus from entering the body further through the barrier - the nasal mucosa. The use of vasoconstrictor drops is justified only in cases where the course of acute rhinitis is complicated by the development of otitis media or sinusitis. Indeed, in large doses, they can adversely affect blood circulation, and their abuse can provoke drug dependence and the development of hypertrophic rhinitis. It is better for pregnant women with severe rhinitis to use vasoconstrictor drops "for babies" with a minimum concentration of the active drug.
The use of vasoconstrictor drops is justified only in cases where the course of acute rhinitis is complicated by the development of otitis media or sinusitis. Indeed, in large doses, they can adversely affect blood circulation, and their abuse can provoke drug dependence and the development of hypertrophic rhinitis. It is better for pregnant women with severe rhinitis to use vasoconstrictor drops "for babies" with a minimum concentration of the active drug.
The next disease we propose to consider is hypertrophic rhinitis. It is caused by an increase in the size of the turbinates - special outgrowths on the side wall of the nasal cavity that regulate the speed of air flow. Their excessive increase sharply complicates breathing through the nose. In addition to the abuse of vasoconstrictor drops, the development of this disease in pregnant women is promoted by increased venous pressure (due to an increase in the uterus, a decrease in the amplitude of movement of the diaphragm and difficulty in outflow of venous blood), as well as a physiological lack of hormones of the adrenal cortex responsible for vascular tone.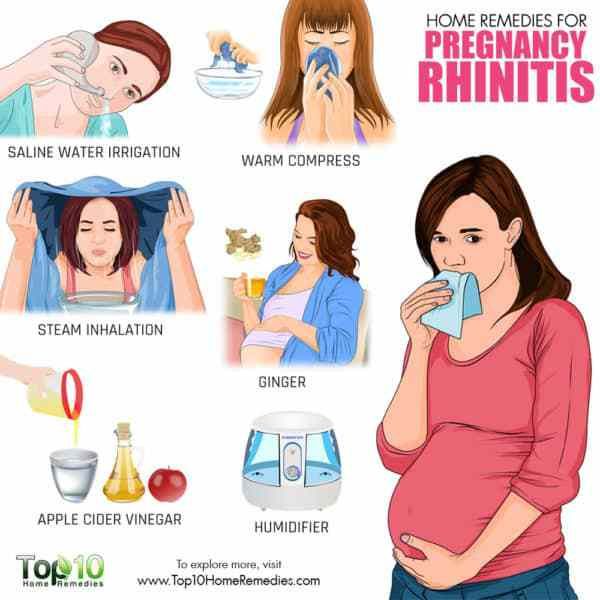 At the initial stage, in the treatment of the disease, breathing exercises can be used (slow inhalation and exhalation through the nose with a frequency of five respiratory movements per minute), oxygen breathing through the nose, massage of reflex points (paranasal points and he-gu points on the left hand between the index and thumbs). Massage of biologically active points is performed counterclockwise for at least two minutes. In an advanced stage, the treatment of the disease is surgical (radio wave, laser, ultrasonic or mechanical action on the turbinates aimed at reducing their size). In the presence of hypertrophic rhinitis and dependence on vasoconstrictor drops, it is best to get rid of these diseases in advance, before the planned desired pregnancy, or if the disease developed during pregnancy, then in a planned manner after its resolution.
At the initial stage, in the treatment of the disease, breathing exercises can be used (slow inhalation and exhalation through the nose with a frequency of five respiratory movements per minute), oxygen breathing through the nose, massage of reflex points (paranasal points and he-gu points on the left hand between the index and thumbs). Massage of biologically active points is performed counterclockwise for at least two minutes. In an advanced stage, the treatment of the disease is surgical (radio wave, laser, ultrasonic or mechanical action on the turbinates aimed at reducing their size). In the presence of hypertrophic rhinitis and dependence on vasoconstrictor drops, it is best to get rid of these diseases in advance, before the planned desired pregnancy, or if the disease developed during pregnancy, then in a planned manner after its resolution.
In the event that a cold and a runny nose do not go away for a certain amount of time, and facial pains aggravate when the head is tilted, the amount of discharge from the nose increases, which becomes thick, greenish (purulent) appearance, you should immediately contact to an ENT specialist. After all, these symptoms indicate the development of sinusitis (sinusitis). Inflammation develops in the paranasal sinuses. The proximity of the paranasal sinuses to the orbit and the cranial cavity explains the anxiety of the doctor and the patient, because. complications can lead to more serious illnesses.
After all, these symptoms indicate the development of sinusitis (sinusitis). Inflammation develops in the paranasal sinuses. The proximity of the paranasal sinuses to the orbit and the cranial cavity explains the anxiety of the doctor and the patient, because. complications can lead to more serious illnesses.
If sinus radiography is used, the diagnosis of sinusitis is not a difficult problem. During pregnancy, X-rays should not be used. In this case, the way to clarify the diagnosis and its effective treatment are endoscopic examination of the nasal cavity and ultrasound examination of the sinuses. Conservative measures are being taken to improve nasal breathing, reduce the viscosity of the mucopurulent secretion and normalize the drainage of the paranasal sinuses. An excellent way of conservative treatment of sinusitis (rhinosinusitis) is treatment by the method of moving drugs (the common name for the procedure is "cuckoo"). Negative pressure in the nasal cavity during the pronunciation of the word "cuckoo" contributes to the evacuation of the contents of the sinuses. Of the local remedies for sinusitis in pregnant women, "soft" vasoconstrictor drops can be used to facilitate outflow, saline irrigation and a local antibiotic in the form of an aerosol - bioparox, as well as drugs that "thinn" the contents of the sinuses (sinupret).
Of the local remedies for sinusitis in pregnant women, "soft" vasoconstrictor drops can be used to facilitate outflow, saline irrigation and a local antibiotic in the form of an aerosol - bioparox, as well as drugs that "thinn" the contents of the sinuses (sinupret).
If such therapy is ineffective, in the treatment of sinusitis that develops during pregnancy, punctures of the maxillary sinuses are used, as well as antibiotic therapy (in agreement with the gynecologist). The puncture must be performed in a timely manner, delaying the implementation of this procedure is not in the interests of the mother and the unborn child. It should be borne in mind that in the first half of pregnancy, the fetus undergoes the processes of formation of vital organs and systems. Therefore, during this period, it is more favorable to use anti-inflammatory drugs locally, and not to overload the mother's body with medicines. A sinus puncture allows you to accurately diagnose, control the dynamics of the inflammatory process, reliably evacuate pus from the sinus, and inject medications locally into the inflammation site. Drugs must be safe for the mother and fetus.
Drugs must be safe for the mother and fetus.
The sinus puncture procedure in the people has some speculation, because of which patients do not give timely consent to the necessary type of treatment. It is believed that if you make a puncture once, then you will have to do it all your life. We declare responsibly: this is a myth! In fact, the trend is completely opposite: if a puncture is not performed in a timely manner, if there are indications, then the risk of chronic sinusitis increases. And in this regard, if you start sinusitis, it is wrong to treat it, indeed, with subsequent hypothermia, another exacerbation may develop, with the need to pierce the sinus every time. The presence of pus in the sinus, near the brain, eye socket and brain vessels is unacceptable! It should not be forgotten that the progressive course of the inflammatory process in the sinuses and the development of complications may lead to the need for surgical treatment - a complex operation may be required, in comparison with which a sinus puncture is a very simple and easily tolerated procedure.
One of the most common diseases in Kazakhstan is allergic rhinitis, also known as pollinosis (from the Greek word pollinos - pollen). Thus, already in the name of the disease, its cause is determined - the pollen of various plants. There is also a direct causal relationship between air pollution and disease. In addition, a number of factors, including racial and social characteristics, month of birth, age at which first exposure to pollen allergen occurred, family size and serial number of the child in it, maternal smoking and feeding patterns, can affect the incidence of allergic rhinitis. Allergic rhinitis can provoke the development of other diseases of the respiratory tract and ear. It was found that in 24% of children, allergic rhinitis is a predisposing factor in the development of acute and chronic otitis media, in 28% of cases - chronic rhinosinusitis. Symptoms of allergic rhinitis are present in 88% of patients with bronchial asthma. Thus, allergic rhinitis should not be considered as a mild, harmless disease; not only does it significantly affect the quality of life of patients, but it is also a harbinger and predisposing factor in the development of more severe, often disabling diseases.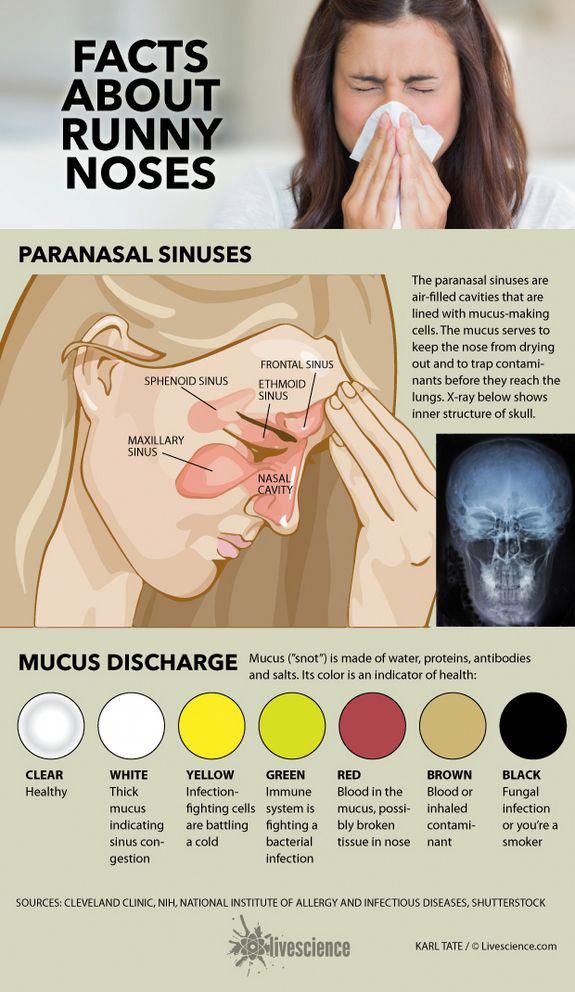
Pregnant women, unfortunately, this is the group among patients with allergic rhinitis, which is very difficult to help with the disease. The doctor has a large number of effective allergy remedies in his arsenal, but pharmacological companies do not want to “get involved” with pregnant women, and in almost all drug annotations, manufacturers indicate that the study of the drug’s effect on pregnancy has not been carried out, it is necessary to weigh the risks and benefits of using the drug . Even for drugs with minimal bioavailability, such as Nasonex, there is no official approval for use in pregnant women. The main reason here is legal. Pharmaceutical firms are catastrophically afraid of lawsuits. Litigation costs may exceed sales profits in this relatively small market segment.
The method of treating allergic rhinitis in pregnant women suggests itself - to avoid contact with the allergen. Pollinosis is a seasonal disease, it is associated with a certain flowering time of a particular plant.