Is genital itching a sign of pregnancy
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast. The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women. Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
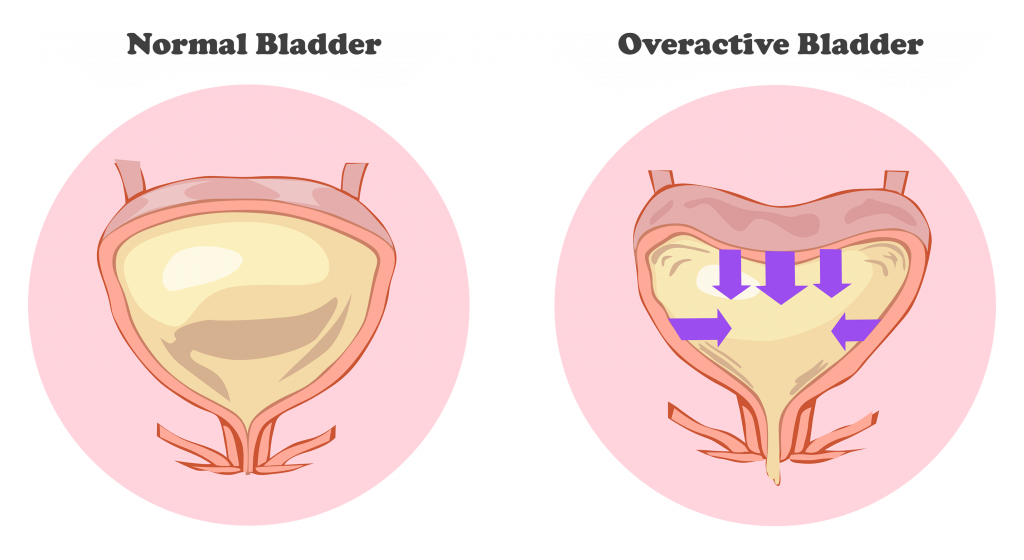
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.
Symptoms include:
- frequent and urgent need to urinate
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.

- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.

- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.
Vaginal Itching During Pregnancy: Causes, Symptoms, and More
Pregnant women often experience vaginal itching at some point during pregnancy. This is a normal and common occurrence.
Many things can cause vaginal itching during pregnancy. Some may be the result of changes your body is going through. Other causes may not be associated with your pregnancy at all.
Read on to review the potential causes of vaginal itching during pregnancy, plus learn hands-on information about treatment and prevention.
These conditions may cause vaginal itching during pregnancy:
Bacterial vaginosis
Bacterial vaginosis can occur if the balance between the good and bad bacteria in the vagina changes. This common vaginal infection typically happens to sexually active women, whether they’re pregnant or not. Symptoms include:
- a thin, opaque or grayish discharge
- itching
- burning
- redness
- a fishlike odor, especially after sexual intercourse
Yeast infection
In addition to bacteria, your vagina normally contains a small amount of yeast. The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
The hormonal changes associated with pregnancy can disrupt the pH balance of the vagina, causing yeast to multiply. For this reason, yeast infections are common during pregnancy.
Symptoms can include:
- itching
- burning
- a thick vaginal discharge that has the texture of cottage cheese
Increase in vaginal discharge
The amount of vaginal discharge and cervical mucus you secrete may increase throughout pregnancy. Hormonal changes causes this as well as the softening of the cervix and vaginal walls.
Discharge is designed to protect your vagina from infection, but it can irritate the skin of the vulva, making it red and itchy.
Vaginal dryness
Hormonal changes may cause vaginal dryness to occur in some people during pregnancy. Anecdotal evidence indicates that those who are breastfeeding when they conceive are more likely to experience this symptom.
Redness, irritation, and pain during sex may also occur.
Low progesterone may also cause vaginal dryness in some pregnant women. Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Since this hormone is necessary for sustaining pregnancy, talk to your doctor if you have this symptom.
Sensitivity to products
During pregnancy, the vagina becomes engorged with blood, and your skin may feel stretched and more sensitive than usual.
Products that you used comfortably before conceiving may now irritate your skin, causing it to itch and redden. Products that can cause this to occur include:
- detergent
- bubble bath
- body wash
- soap
Urinary tract infection (UTI)
The uterus sits on top of the bladder. As it expands during pregnancy, greater pressure is placed on the bladder. This can block the expulsion of urine, causing an infection to occur.
For this reason, pregnant women can be at greater risk for getting a UTI.
Bacteria can also cause UTIs, such as group B strep bacteria (GBS). Around 1 in 4 pregnant women test positive for GBS. GBS in adults doesn’t usually show symptoms. Since the GBS bacteria can be harmful to a newborn, your doctor will test you for it during pregnancy.
Symptoms include:
- frequent and urgent need to urinate
- abdominal pain
- vaginal itching and burning
- blood in urine
- pain during intercourse
Cholestasis of pregnancy
This liver condition may occur late in pregnancy. Why it happens isn’t completely understood. Experts think genetics and pregnancy hormones play a role.
Cholestasis of pregnancy causes extreme itchiness on the palms of the hands and soles of the feet. The itching may start to affect the entire body, including the vaginal area. Rashes and redness don’t occur with this condition.
Sexually transmitted infections (STIs)
STIs, such as genital herpes, HPV, and trichomoniasis, may all have vaginal itching as an early symptom.
You can become pregnant while you have an STI or get one during pregnancy. Since STIs may not show symptoms, it’s important to let your doctor know if you think you may have one contracted one.
If an STI does show symptoms, you may have:
- rash
- burning sensation
- warts
- fever
- vaginal discharge
- flu-like symptoms
STIs can adversely affect you and your baby, but you can get treated while you’re pregnant, eliminating those risks.
Vaginal itching during pregnancy is often nothing to worry about and can often be resolved with at-home treatments.
However, during this time it may make sense to be especially proactive and talk with your doctor about any troubling symptoms you experience.
Treatments for vaginal itching will vary based on the cause. They include:
- Over-the-counter antifungal treatments. If your doctor has confirmed that you have a yeast infection, you can use an OTC antifungal cream or suppository to treat it. Don’t use fluconazole (Diflucan). This prescribed antifungal medication has been linked to an increased risk of miscarriage and shouldn’t be taken during pregnancy.
- Baking soda. Itchy skin can be soothed by soaking in a baking soda bath or using a baking soda compresses on the area.
- Cool water. Cool baths and cold compresses may also help reduce itching.
- Product elimination. If you think the products you’re using are causing your symptoms, try eliminating all of them and use all-natural, gentle products designed for use during pregnancy or for babies.

- Antibiotics. You’ll need prescription medication if you have a UTI, STI, or bacterial vaginosis.
- Corticosteroids. Topical anti-itch creams such as corticosteroids may help reduce itching.
- Other medications. If you have cholestasis, your doctor will monitor you and might recommend you use anti-bile medications.
It may be hard to completely avoid vaginal itching during pregnancy, but certain proactive behaviors may help. Consider these tips:
- Try to keep your vaginal pH in the healthy range by eating yogurt that contains live cultures. You can also take a Lactobacillusacidophilus supplement daily with your doctor’s approval.
- Wear underwear made from cotton or another breathable fabric.
- Avoid wearing clothing that’s too tight.
- Immediately change out of damp clothing, such as bathing suits or exercise gear.
- Avoid using products that contain scents, chemicals, or irritants.

- Practice good hygiene, especially after going to the bathroom. Always wipe from front to back.
- Don’t douche. Douching alters the vagina’s natural pH balance. Follow our guide to clean your vagina and vulva.
- Try to reduce your stress levels with prenatal yoga, meditation, or deep breathing.
Mention any uncomfortable symptom that worries you during pregnancy to your doctor. If you have vaginal itching that doesn’t respond to at-home treatment within a few days, have your doctor check it out.
If vaginal itching is accompanied by other symptoms, such as pain or a thick, smelly discharge, see your doctor to rule out an infection. Also see your doctor if you notice streaky blood in your discharge.
Vaginal itching is a common occurrence during pregnancy and often nothing to worry about. It’s mostly associated with the normal hormonal changes you can expect during this time.
If you’re concerned about this symptom, or other symptoms accompany it, such as pain or odor, your doctor will be able to prescribe treatments that can help.
What happens to the vagina during pregnancy?
These vaginal changes may seem strange, but most of them are completely normal during pregnancy.
Anastasia Nikiforova
The first pregnancy is a time of a million thoughts and worries. But don't worry, women have been giving birth for hundreds of thousands of years, and our bodies "know" what to do. During the 9 months of pregnancy, many important changes take place in the body, and the vagina is no exception. Here are the top 10 completely normal changes associated with pregnancy (which, however, may seem a little strange).
Contents of the article
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
1. Your perineum may turn bluish or purple
The last thing we look forward to is a change in color from your vagina, but this is exactly what can happen in early pregnancy. Blueness of the vagina, labia, or cervix is called Chadwick's symptom and is caused by increased blood flow. You may not even notice the color change unless you specifically check, as the symptom does not cause any discomfort. Be that as it may, the blue or purple hue will disappear shortly after childbirth.
Blueness of the vagina, labia, or cervix is called Chadwick's symptom and is caused by increased blood flow. You may not even notice the color change unless you specifically check, as the symptom does not cause any discomfort. Be that as it may, the blue or purple hue will disappear shortly after childbirth.
Chadwick's symptom is considered to be one of the first signs of pregnancy, as the color change can occur as early as 4 weeks.
2. Your vagina can turn into a magical land of orgasms
During pregnancy, the volume of blood in our body can increase by 50%, and increased blood flow does not bypass the "southern regions". This makes the vagina swollen and hypersensitive in the first and second trimesters of pregnancy. Throw in increased levels of oxytocin, estrogen, and progesterone into the equation, and the result can be better orgasms and increased libido. Do not forget to discuss the changes with your partner - the downside of orgasms can be discomfort and increased sensitivity of the vagina. Perhaps the usual caresses will have to be adapted.
Perhaps the usual caresses will have to be adapted.
3. Varicose veins of the labia and vulva may develop
Varicose veins in the legs are not uncommon during pregnancy due to increased blood flow and the weight of the abdomen. But changes can also appear in your most intimate places! According to the study, from 18 to 22% of women experience varicose veins of the labia and vulva. As a rule, this condition develops in the second and third trimesters. Some women do not notice any signs, others may feel swelling and pain. The good news is that most varicose veins will disappear within a few weeks of giving birth.
To cope with vulvar varicose veins, try the following:
- Special underwear for pregnant women with compression properties
- Cool compresses for the affected area
- Avoid sitting for too long
- Rise the consumption of water
- and thighs when possible
4.
 Your vaginal pH will change
Your vaginal pH will change In other words, you will most likely smell differently. According to research, vaginal odor can become metallic or salty. A change or increase in odor can occur due to hormonal fluctuations. Or maybe it only seems so because of the increased sense of smell during pregnancy. However, if the smell seems very intense or unpleasant, accompanied by burning and itching, you should definitely consult a doctor - this may be a sign of an infection.
5. Your vagina may hurt like it was stabbed
And chances are no one told you this could happen. Don't panic - most likely there is nothing to worry about. Shooting pain may be a normal consequence of pregnancy. The pain is caused by the baby's pressure on certain nerves or natural changes in the cervix. Often it occurs in the third trimester after you get up after sitting or lying down for a long time.
How to relieve pain?
- Stay active
- Limit the movements associated with the twisting of the body or lifting
- Try massage for pregnant women
- Swate
- Bandage
6.
 Vagina will become more vulnerable to infection
Vagina will become more vulnerable to infection , for the driving mushrooms. They grow more during pregnancy due to increased estrogen levels and changes in your vaginal pH levels. Topical antifungal medications are most preferred for fighting candida, but oral medications are associated with certain risks, including miscarriage.
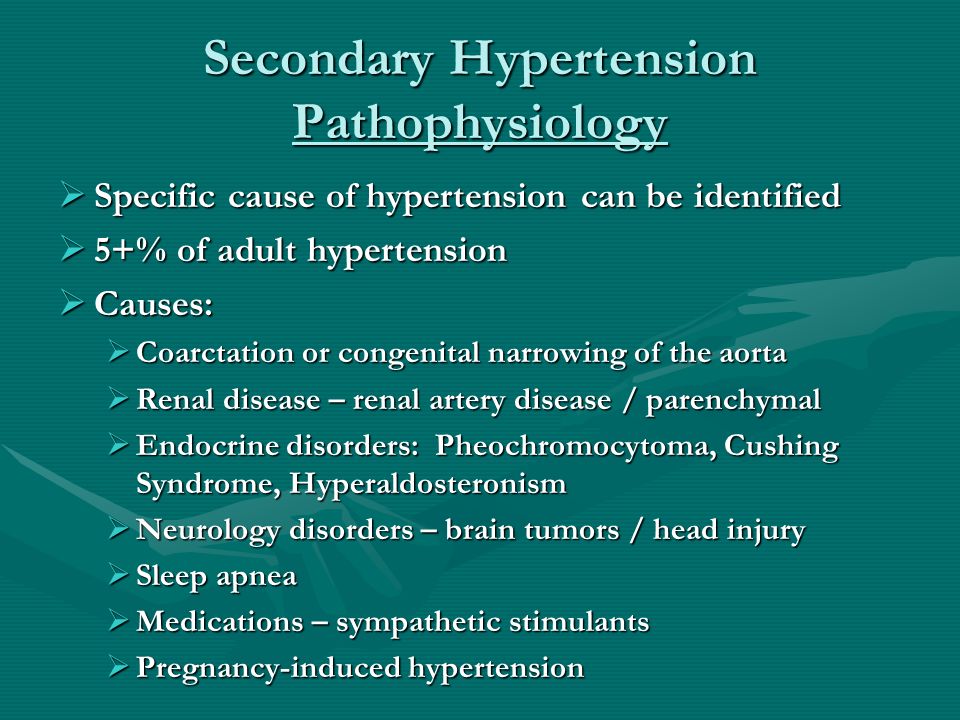
Another problem associated with pregnancy can be urinary tract infections (UTIs). They not only cause discomfort, but also can make you want to go to the toilet even more often (although it would seem that there is nowhere to go more often). Pregnancy does not greatly increase the incidence of UTIs, but it increases the risk of kidney-related complications by as much as 40%. This, in turn, can lead to an increased risk of preeclampsia, preterm labor, and low birth weight.
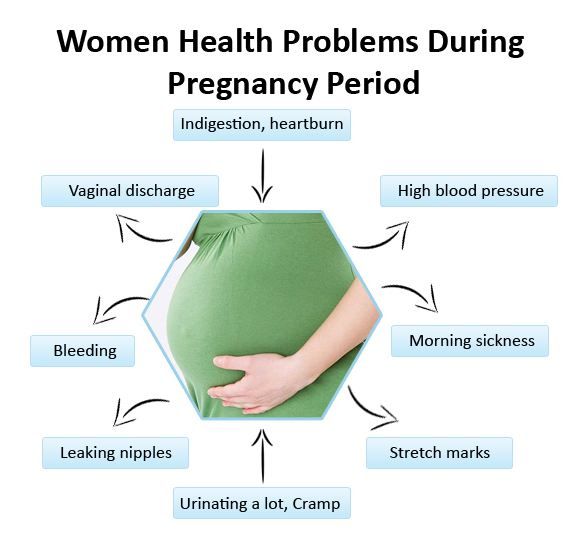
7. Your vagina will produce more discharge
Stock up on panty liners—shortly after conception (often before you even realize you're pregnant), your vagina goes into "Stakhanovite mode" of secretion production. This is needed by the body in order to protect the cervix and help prevent infections.
This is needed by the body in order to protect the cervix and help prevent infections.
Medically this discharge is called leucorrhea or leucorrhea. They should be not too thick, slightly sticky, have a milky tint and a slight smell similar to your usual scent.
If the discharge is yellow or green, thick, or has a bad smell, you may have an infection. Toward the end of pregnancy, the sticky mucous plug of the cervix may come off - this will be a sign of the approach of childbirth.
8. Severe itching in the perineum may occur
Unfortunately, itching in the perineum is a common pregnancy symptom that can occur at any time. Itching can be caused by increased secretions, a change in pH levels, or a yeast infection, which we talked about earlier. All this can irritate the sensitive skin of the vulva.
Talk to your gynecologist if irritation persists or is accompanied by other warning signs such as abnormal discharge, sores, or a burning sensation.
9. Vaginal flora can get a little weird
Our vaginas are full of bacteria - and that's perfectly normal. However, starting from the first trimester of pregnancy, the bacterial environment may change. Why does it matter if the cause is not an infection? Because, according to several studies, women with lower vaginal levels of lactobacilli may be more likely to have preterm labor. Someday, measuring vaginal bacteria levels will help determine if a woman is at risk for preterm labor, but more research is still needed.
10. The vagina may remain stiff. But there is a way to help her!
The perineum, the area between the vagina and anus, may remain stiff and rupture during childbirth. Medical statistics state that from 53 to 79% of women in labor experience ruptures of vaginal tissues. And some experts say that for women with first births, this figure is closer to 90%. In accordance with a 2014 study, women in labor who experienced severe tears during their first birth were 5 times more likely to experience them during subsequent births.
In accordance with a 2014 study, women in labor who experienced severe tears during their first birth were 5 times more likely to experience them during subsequent births.
But there is a potential solution: massage of the vulva and perineum, especially in the last month of pregnancy. This helps reduce the risk of this painful problem.
Did you have any interesting changes in your body during pregnancy?
Source
Changes in a woman's body during pregnancy
From the very first days of pregnancy, the body of a pregnant woman undergoes profound transformations. These transformations are the result of the coordinated work of almost all body systems, as well as the result of the interaction of the mother's body with the child's body.
During pregnancy, many internal organs undergo significant restructuring. These changes are adaptive in nature, and, in most cases, are short-lived and completely disappear after childbirth.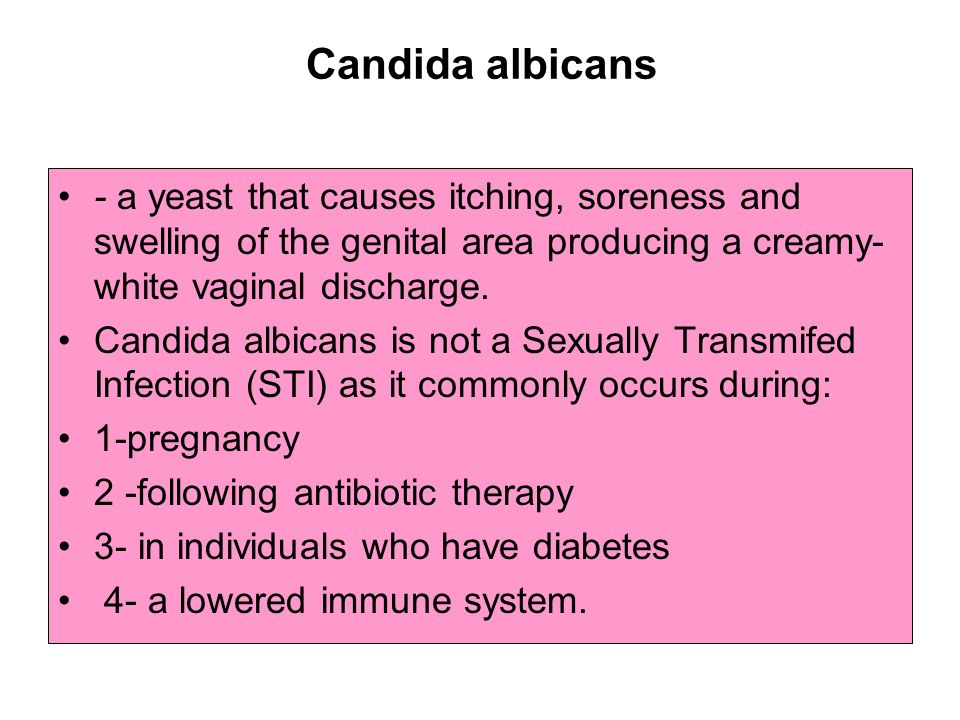 Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy.
Consider the changes in the basic systems of the vital activity of a woman's body during pregnancy.
The respiratory system during pregnancy works hard. The respiratory rate increases. This is due to an increase in the need of the mother and fetus for oxygen, as well as in the limitation of the respiratory movements of the diaphragm due to an increase in the size of the uterus, which occupies a significant space of the abdominal cavity.
Cardio The mother's vascular system has to pump more blood during pregnancy to ensure an adequate supply of nutrients and oxygen to the fetus. In this regard, during pregnancy, the thickness and strength of the heart muscles increase, the pulse and the amount of blood pumped by the heart in one minute increase. In addition, the volume of circulating blood increases. In some cases, blood pressure increases. The tone of the blood vessels during pregnancy decreases, which creates favorable conditions for enhanced
to supply tissues with nutrients and oxygen. During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. and changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
During pregnancy, the network of vessels of the uterus, vagina, and mammary glands decreases sharply. On the external genitalia, in the vagina, lower extremities, there is often an expansion of the veins, sometimes the formation of varicose veins. Heart rate decreases in the second half of pregnancy. It is generally accepted that the rise in blood pressure over 120-130 and a decrease to 100 mm Hg. signal the occurrence of pregnancy complications. But it is important to have data on the initial level of blood pressure. and changes in the blood system. During pregnancy, blood formation increases, the number of red blood cells, hemoglobin, plasma and bcc increases. BCC by the end of pregnancy increases by 30-40%, and erythrocytes by 15-20%. Many healthy pregnant women have a slight leukocytosis. ESR during pregnancy increases to 30-40. Changes occur in the coagulation system that contribute to hemostasis and prevent significant blood loss during childbirth or placental abruption and in the early postpartum period.
Kidneys work hard during pregnancy. They secrete decay products of substances from the body of the mother and fetus (the waste products of the fetus pass through the placenta into the mother's blood).
Changes in the digestive system are represented by increased appetite (in most cases), craving for salty and sour foods. In some cases, there is an aversion to certain foods or dishes that were well tolerated before the onset of pregnancy. Due to the increased tone of the vagus nerve, constipation may occur.
The most significant changes, however, occur in the genitals of the pregnant woman. These changes prepare the woman's reproductive system for childbirth and breastfeeding.
The uterus of a pregnant woman increases significantly in size. Its mass increases from 50 g - at the beginning of pregnancy to 1200 g - at the end of pregnancy. The volume of the uterine cavity by the end of pregnancy increases by more than 500 times! The blood supply to the uterus is greatly increased. In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy.
In the walls of the uterus, the number of muscle fibers increases. The cervix is filled with thick mucus that clogs the cavity of the cervical canal. The fallopian tubes and ovaries also increase in size. In one of the ovaries, there is a "corpus luteum of pregnancy" - a place for the synthesis of hormones that support pregnancy.
The walls of the vagina loosen and become more elastic.
External genitalia (labia minor and major) also increase in size and become more elastic. The tissues of the perineum are loosened. In addition, there is an increase in mobility in the joints of the pelvis and a divergence of the pubic bones. The changes in the genital tract described above are of extremely important physiological significance for childbirth. Loosening the walls, increasing the mobility and elasticity of the genital tract increases their throughput and facilitates the movement of the fetus through them during childbirth.
Skin in the genital area and midline of the abdomen usually becomes darker in color. Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Sometimes "stretch marks" form on the skin of the lateral parts of the abdomen, which turn into whitish stripes after childbirth.
Mammary glands increase in size, become more elastic, tense. When pressing on the nipple, colostrum (first milk) is released. Changes of the bone skeleton and muscular system . An increase in the concentration of the hormones relaxin and progesterone in the blood contributes to the leaching of calcium from the skeletal system. This accomplishes two goals. On the one hand, this helps to reduce the rigidity of the joints between the pelvic bones (especially the pubic joint) and increase the elasticity of the pelvic ring. Increasing the elasticity of the pelvis is of great importance in increasing the diameter of the internal bone ring in the first stage of labor and further reducing the resistance of the birth tract to fetal movement in the second stage of labor. Secondly, calcium, washed out of the mother's skeletal system, is used to build the skeleton of the fetus.
It should be noted that calcium compounds are washed out of all bones of the maternal skeleton (including the bones of the foot and spine). As shown earlier, a woman's weight increases during pregnancy by 10 -12 kg. This additional load against the background of a decrease in bone stiffness can cause foot deformity and the development of flat feet. A shift in the center of gravity of the body of a pregnant woman due to an increase in the weight of the uterus can lead to a change in the curvature of the spine and the appearance of pain in the back and pelvic bones. Therefore, for the prevention of flat feet, pregnant women are advised to wear comfortable shoes with low heels. It is advisable to use insoles that support the arch of the foot. For the prevention of back pain, special physical exercises are recommended that can unload the spine and sacrum, as well as wearing a comfortable bandage. Despite an increase in calcium loss by the bones of the skeleton of a pregnant woman and an increase in their elasticity, structure and bone density (as is the case with osteoporosis in older women).
Changes in the nervous system . In the first months of pregnancy and at the end of it, there is a decrease in the excitability of the cerebral cortex, which reaches its greatest degree by the time of the onset of childbirth. By the same period, the excitability of the receptors of the pregnant uterus increases. At the beginning of pregnancy, there is an increase in the tone of the vagus nerve, in connection with which various phenomena often occur: changes in taste and smell, nausea, increased salivation, etc.
Active endocrine glands there are significant changes that contribute to the correct course of pregnancy and childbirth. Changes in body weight. By the end of pregnancy, a woman's weight increases by about 10-12 kg. This value is distributed as follows: fetus, placenta, membranes and amniotic fluid - approximately 4.0 - 4.5 kg, uterus and mammary glands -1.0 kg, blood - 1.5 kg, intercellular (tissue) fluid - 1 kg , an increase in the mass of adipose tissue of the mother's body - 4 kg.