Infection in breast milk
Breast Infection (Mastitis): Symptoms, Causes, Treatments
Written by WebMD Editorial Contributors
In this Article
- How the Breast Is Built
- Breast Infection Causes
- Breast Infection Symptoms
- When to Seek Medical Care
- Breast Infection Exams and Tests
- Breast Infection Treatment
- Breast Infection Home Remedies
- Medications for Mastitis
- Surgery for an Abscess
- Next Steps
- Follow-Up Care After a Breast Infection
- Mastitis Prevention
- Outlook for Breast Infections
How the Breast Is Built
The breast is composed of several glands and ducts that lead to the nipple and the surrounding colored area called the areola. The milk-carrying ducts extend from the nipple into the underlying breast tissue like the spokes of a wheel. Under the areola are lactiferous ducts. These fill with milk during lactation after a woman has a baby. When a girl reaches puberty, changing hormones cause the ducts to grow and cause fat deposits in the breast tissue to increase. The glands that produce milk (mammary glands) that are connected to the surface of the breast by the lactiferous ducts may extend to the armpit area.
Breast Infection Causes
Mastitis is an infection of the tissue of the breast that occurs most frequently during the time of breastfeeding. It can occur when bacteria, often from the baby's mouth, enter a milk duct through a crack in the nipple.
Breast infections most commonly occur one to three months after the delivery of a baby, but they can occur in women who have not recently delivered and in women after menopause. Other causes of infection include chronic mastitis and a rare form of cancer called inflammatory carcinoma.
In healthy women, mastitis is rare. However, women with diabetes, chronic illness, AIDS, or an impaired immune system may be more susceptible.
About 1%-3% of breastfeeding mothers develop mastitis. Engorgement and incomplete breast emptying can contribute to the problem and make the symptoms worse.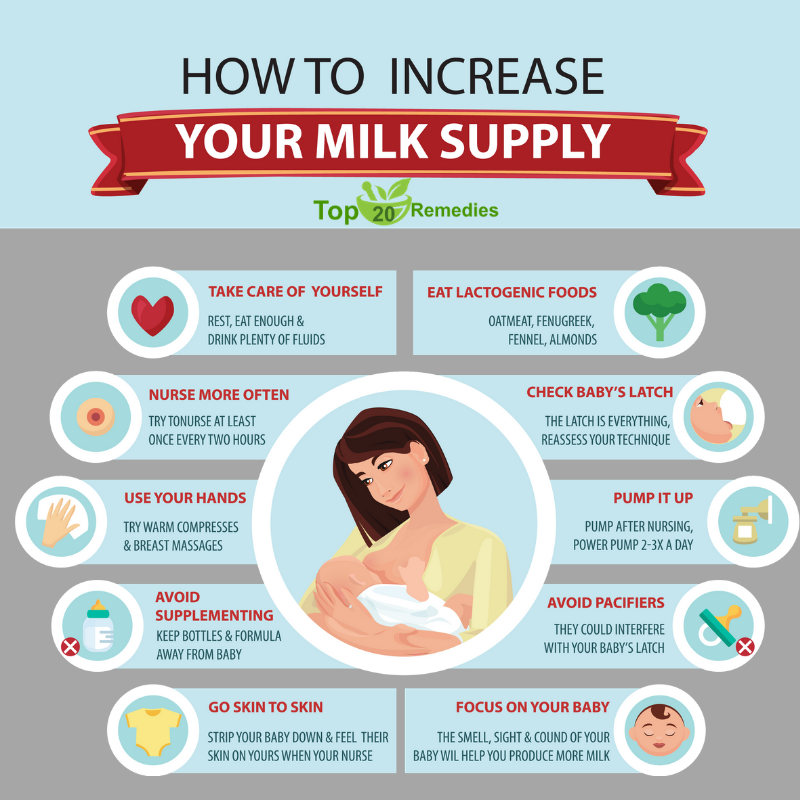
Chronic mastitis occurs in women who are not breastfeeding. In postmenopausal women, breast infections may be associated with chronic inflammation of the ducts below the nipple. Hormonal changes in the body can cause the milk ducts to become clogged with dead skin cells and debris. These clogged ducts make the breast more open to bacterial infection. Infection tends to come back after treatment with antibiotics.
Breast Infection Symptoms
Breast infections may cause pain, redness, and warmth of the breast along with the following symptoms:
- Tenderness and swelling
- Body aches
- Fatigue
- Breast engorgement
- Fever and chills
- Abscess: A breast abscess can be a complication of mastitis. Noncancerous masses such as abscesses are more often tender and frequently feel mobile beneath the skin. The edge of the mass is usually regular and well defined. Indications that this more serious infection has occurred include the following:
- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.
 )
) - Pus draining from the nipple
- Persistent fever and no improvement of symptoms within 48-72 hours of treatment
- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.
When to Seek Medical Care
Call your health care provider as soon as you feel any suspicious lump, whether you are breastfeeding or not. Call for an appointment if:
- You have any abnormal discharge from your nipples.
- Breast pain is making it difficult for you to function each day.
- You have prolonged, unexplained breast pain.
- You have any other associated symptoms such as redness, swelling, pain that interferes with breastfeeding, a mass or tender lump in the breast that does not disappear after breastfeeding.
- If you are breastfeeding, call your doctor if you develop any symptoms of breast infection so that treatment may be started promptly.
You may need to be evaluated in a hospital's emergency department if the breast pain is associated with other signs of an infection (such as a fever, swelling, or redness to the breast) and if your health care provider cannot see you promptly. The below symptoms require emergency treatment:
The below symptoms require emergency treatment:
- A persistent high fever greater than 101.5°F
- Nausea or vomiting that is preventing you from taking the antibiotics as prescribed
- Pus draining from the breast
- Red streaks extending toward your arm or chest
- Dizziness, fainting, or confusion
Breast Infection Exams and Tests
The diagnosis of mastitis and a breast abscess can usually be made based on a physical exam.
- If it is unclear whether a mass is due to a fluid-filled abscess or to a solid mass such as a tumor, a test such as an ultrasound may be done. An ultrasound may also be helpful in distinguishing between simple mastitis and abscess or in diagnosing an abscess deep in the breast. This noninvasive test allows your doctor to directly visualize the abscess by placing an ultrasound probe over your breast. If an abscess is confirmed, aspiration or surgical drainage, and IV antibiotics, are often required.
- Cultures may be taken, either of breast milk or of material taken out of an abscess through a syringe, to determine the type of organism causing the infection.
 This information can help your doctor decide what kind of antibiotic to use.
This information can help your doctor decide what kind of antibiotic to use. - Nonbreastfeeding women with mastitis, or those who do not respond to treatment, may have a mammogram or breast biopsy. This is a precautionary measure because a rare type of breast cancer can produce symptoms of mastitis.
Breast Infection Treatment
Breast infections require treatment by a health care provider.
Breast Infection Home Remedies
After you see a doctor, try the following to help your breast infection heal.
- Pain medication: Take acetaminophen (Tylenol) or ibuprofen (such as Advil) for pain. These drugs are safe while breastfeeding and will not harm your baby. Your doctor may prescribe a prescription strength pain reliever if your pain is severe and not relieved with over-the-counter medication.
- In mild cases of mastitis, antibiotics may not be prescribed at all. If you are prescribed antibiotics, finishing the prescription even if you feel better in a few days is very important.

- Frequent feedings: Do not stop breastfeeding from the affected breast, even though it will be painful and you may be taking antibiotics. Frequent emptying of the breast prevents engorgement and clogged ducts that can only make mastitis worse.
- If needed, use a breast pump to relieve pressure and completely empty the breast.
- You can also breastfeed from the unaffected side and supplement with infant formula as needed.
- The infection will not harm the baby because the germs that caused the infection probably came from the baby’s mouth in the first place.
- Breastfeeding should be avoided in the infected breast when an abscess is present.
- Pain relief: A warm compress applied before and after feedings can often provide some relief. A warm bath may work as well.
- If heat is ineffective, ice packs applied after feedings may provide some comfort and relief.
- Avoid using ice packs just before breastfeeding because it can slow down milk flow.

- Drink plenty of water -- at least 10 glasses a day. Eat well-balanced meals and add 500 extra calories a day while breastfeeding. Dehydration and poor nutrition can decrease milk supply and make you feel worse.
Medications for Mastitis
For simple mastitis without an abscess, oral antibiotics are prescribed. Cephalexin (Keflex) and dicloxacillin (Dycill) are two of the most common antibiotics chosen, but a number of others are available. The antibiotic prescribed will depend on your specific situation, your doctor’s preference, and any drug allergies you may have. This medicine is safe to use while breastfeeding and will not harm the baby.
Chronic mastitis in nonbreastfeeding women can be complicated. Recurrent episodes of mastitis are common. Occasionally, this type of infection responds poorly to antibiotics. Therefore, close follow-up with your doctor is mandatory.
If the infection worsens in spite of oral antibiotics or if you have a deep abscess requiring surgical treatment, you may be admitted to the hospital for IV antibiotics.
Surgery for an Abscess
If an abscess is present, it must be drained. After injection of a local anesthetic, the doctor may drain an abscess near the surface of the skin either by aspiration with a needle and syringe or by using a small incision. This can be done in the doctor’s office or emergency department.
If the abscess is deep in the breast, however, it may require surgical drainage in the operating room. This procedure is usually done under general anesthesia to minimize pain and completely drain the abscess. Antibiotics and heat on the area are also used to treat abscesses.
Next Steps
Mastitis does not cause cancer, but cancer can mimic mastitis in appearance. If a breast infection is slow to go away, your health care provider may recommend a mammogram or other tests to rule out cancer.
Follow-Up Care After a Breast Infection
If you have a breast infection, you may be seen for a recheck in 24-48 hours.
- Take all antibiotics as prescribed.

- Take your temperature three times a day for the first 48 hours after treatment begins. Watch for fever.
- Call your doctor if you develop a high fever, vomiting, or increasing redness, swelling, or pain in the breast.
- Follow up with your doctor in one to two weeks to make sure that the infection has gone away. If the infection spreads or an abscess develops, you may require IV antibiotics or surgical treatment.
Mastitis Prevention
Sometimes mastitis is unavoidable. Some women are more susceptible than others, especially those who are breastfeeding for the first time. In general, good habits to prevent mastitis include the following:
- Breastfeed equally from both breasts.
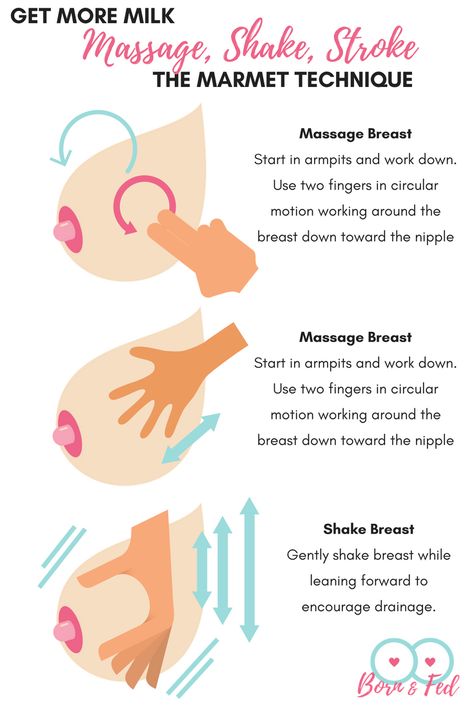
- Empty breasts completely to prevent engorgement and blocked ducts.
- Use good breastfeeding techniques to prevent sore, cracked nipples.
- Allow sore or cracked nipples to air dry.
- Prevent moisture from accumulating in breast pads or bras.
- Avoid dehydration by drinking plenty of fluids.

- Practice careful hygiene: Handwashing, cleaning the nipples, keeping your baby clean.
Outlook for Breast Infections
When treated promptly, the majority of breast infections go away quickly and without serious complications. Most women can and should continue to breastfeed despite an episode of uncomplicated mastitis. With proper treatment, symptoms should begin to resolve within one to two days.
A breast abscess may require surgical drainage, IV antibiotics, and a short hospital stay. A small incision is made and usually heals quite well. Prognosis for complete recovery is also good.
Postmenopausal women with breast abscesses have a high rate of return after simple drainage and frequently need to follow up with a surgeon for more definitive treatment. Chronic infection can result if an abscess is not completely drained, and this can result in a poor cosmetic outcome.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
Causes, Symptoms, and How to Treat
What is a breast infection?
A breast infection, also known as mastitis, is an infection that occurs within the tissue of the breast. Breast infections are most common among women who are breastfeeding, when bacteria from a baby’s mouth enters and infects the breast. This is also known as lactation mastitis. Mastitis also occurs in women who aren’t breastfeeding, but this is not as common.
Breast infections are most common among women who are breastfeeding, when bacteria from a baby’s mouth enters and infects the breast. This is also known as lactation mastitis. Mastitis also occurs in women who aren’t breastfeeding, but this is not as common.
Infection typically affects the fatty tissue in the breast, causing swelling, lumps, and pain. Although most infections are due to breastfeeding or clogged milk ducts, a small percentage of breast infections are associated with rare kinds of breast cancer.
The cause of most breast infections is Staphylococcus aureus bacteria, which causes what is commonly known as a staph infection. Streptococcus agalactiae is the second most common cause.
For breastfeeding mothers, a plugged milk duct can cause milk to back up and an infection to begin. Cracked nipples also increase the risk of breast infection. Bacteria from the baby’s mouth can enter and cause an infection. The bacteria that typically cause infection are also normally found on the skin, even when no infection is taking place. If the bacteria get into the breast tissue, they can multiply quickly and cause painful symptoms.
If the bacteria get into the breast tissue, they can multiply quickly and cause painful symptoms.
You can continue to breastfeed even when you have a mastitis infection because the bacteria are not harmful to your baby. This condition usually occurs in the first few weeks of breastfeeding, but it can occur later.
Non-lactational mastitis occurs in women with weakened immune systems, including women who have had lumpectomies with radiation therapy and women with diabetes. Some infection-like symptoms are a sign of inflammatory breast cancer, but this is very rare. Learn more about mastitis.
Subareolar abscesses occur when the glands under the nipple become blocked and an infection develops under the skin. This can form a hard, pus-filled lump that may need to be drained. This type of abscess normally only occurs in non-lactating women, and there are no known risk factors for it.
Symptoms of a breast infection can start suddenly and may include:
- abnormal swelling, leading to one breast becoming larger than the other
- breast tenderness
- pain or burning while breastfeeding
- a painful lump in the breast
- itching
- warm breast
- chills
- nipple discharge that contains pus
- skin redness in a wedge-shaped pattern
- enlarged lymph nodes in the armpits or neck region
- fever over 101°F, or 38.
 3°C
3°C - feeling ill or rundown
You may experience flu-like symptoms prior to noticing any changes in your breasts. Contact your doctor if you have any combination of these symptoms.
Inflammatory breast cancer
Symptoms of a breast infection may also be associated with inflammatory breast cancer, which is a rare but serious disease. This type of cancer begins when abnormal cells in the breast ducts divide and multiply quickly. These abnormal cells then clog the lymphatic vessels (part of the lymphatic system, which helps remove waste and toxins from the body) in the skin of the breast, causing red, swollen skin that is warm and painful to the touch. Breast changes may occur over the course of several weeks.
Symptoms of inflammatory breast cancer may include:
- thickness or visible enlargement of one breast
- unusual warmth in the affected breast
- discoloration of the breast, making it appear bruised, purple, or red
- tenderness and pain
- dimpling of the skin, similar to orange peel
- enlarged lymph nodes under the arm or near the collarbone
Unlike other forms of breast cancer, women with inflammatory breast cancer do not develop lumps in the breast.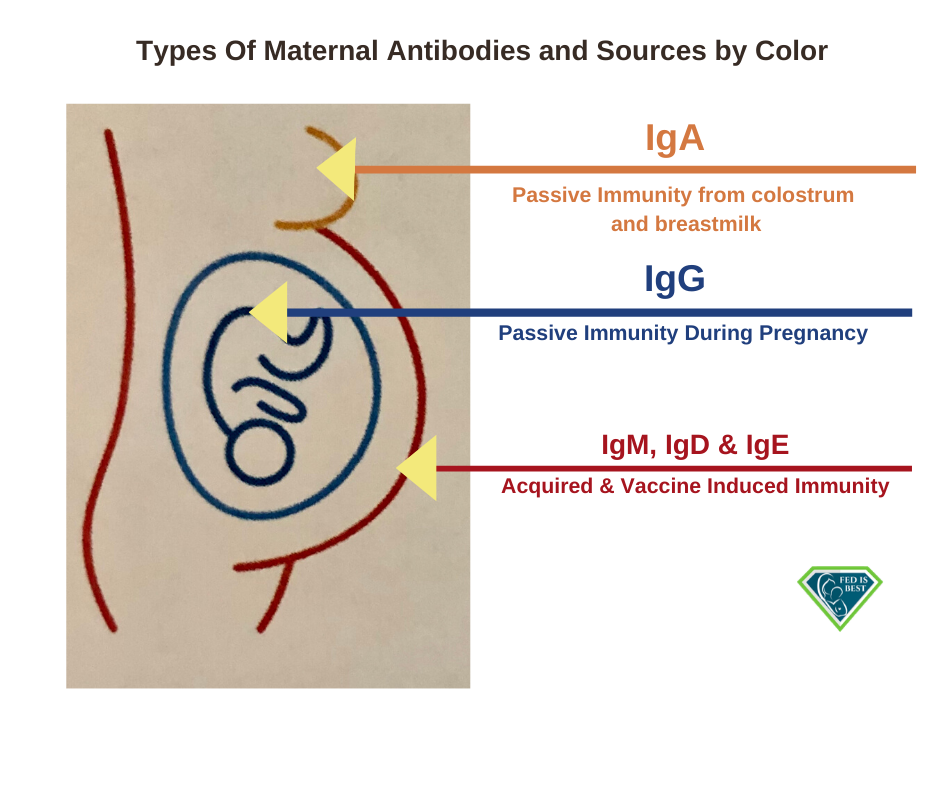 This condition is often confused with a breast infection. Contact your doctor if you experience any of these symptoms.
This condition is often confused with a breast infection. Contact your doctor if you experience any of these symptoms.
In a breastfeeding woman, a doctor can typically diagnose mastitis based on a physical examination and a review of your symptoms. Your doctor will also want to rule out whether the infection has formed an abscess that needs to be drained, which can be done during the physical exam.
If the infection keeps coming back, breast milk may be sent to a laboratory to determine what bacteria might be present.
Other tests may be necessary to determine the cause if you have a breast infection and you’re not breastfeeding. Testing may include a mammogram or even a biopsy of breast tissue to rule out breast cancer. A mammogram is an imaging test that uses low-energy X-rays to examine the breast. A breast biopsy involves the removal of a small tissue sample from the breast for lab testing to determine if any cancerous cell changes are present.
If you don’t already have a primary care doctor, you can browse doctors in your area through the Healthline FindCare tool.
A 10- to 14-day course of antibiotics is generally the most effective form of treatment for this type of infection, and most women feel relief within 48 to 72 hours. It’s important to take all medication as prescribed to make sure the infection doesn’t happen again. You can continue to breastfeed while on most antibiotics, but if nursing is uncomfortable, you can use a breast pump to relieve engorgement and prevent a loss of milk supply.
If you have an abscess due to a severe infection of the breast, it may need to be lanced (clinically incised) and drained. This will help the breast heal faster. You can continue to breastfeed, but seek guidance from a lactation consultant or health care provider on how to care for an abscess.
If your doctor determines that inflammatory breast cancer is causing your symptoms, they will begin treatment based on the stage (severity) of your cancer. Treatment typically involves chemotherapy (using chemicals intravenously to kill cancer cells), radiation therapy (using high-powered X-rays to kill cancer cells), or surgery to remove the breast and surrounding lymph nodes. Lumps and bumps during breastfeeding are very rarely cancer. They’re usually due to a plugged or swollen milk duct.
Lumps and bumps during breastfeeding are very rarely cancer. They’re usually due to a plugged or swollen milk duct.
While receiving treatment for infection, you can also take steps to relieve uncomfortable symptoms at home:
- Warm compresses may ease pain and help lactation. Try applying a warm, wet washcloth to the infected area for 15 minutes, four times a day.
- Empty the breast well.
- Anti-inflammatory medications, such as ibuprofen (Advil, Midol), may help relieve pain.
- Use varied positions to breastfeed.
- If possible, avoid prolonged engorgement before breastfeeding. Feed or pump when it’s time.
Meeting with a lactation consultant to alter your breastfeeding technique or position may help prevent the infection from returning.
If you’re breastfeeding, use these tips to reduce your chances of developing a breast infection:
- Don’t allow yourself to become engorged because you’re late for feedings. Feed or pump.

- Empty at least one breast very well every feeding, and alternate breasts. If you can’t remember which breast was last, use a nursing reminder clip for your bra.
- Avoid sudden changes in feeding schedules.
- Avoid using soap and intense cleaning of the nipple. The areola has self-cleaning and lubricating ability.
- Add a little lecithin or saturated fat to your diet every day to help reduce the risk of developing reoccurring plugged ducts. You can do this with milk, meat (especially liver) and peanuts. Dietary supplements, like lecithin, are not monitored or approved by the FDA. Read labels carefully and compare brands.
- Massage the breasts, especially if you feel a thickening or lump.
- Try different feeding positions. The baby is most efficient at draining ducts in the direction where the chin is pointing.
- Apply warm wet towels to the breast before feeding to increase milk flow.
- Avoid tight-fitting bras that can dig in and impede natural milk flow.

- If you feel a plugged duct, try breastfeeding, massaging the breast, applying heat, and changing the baby’s position.
See a doctor if you’re breastfeeding and have a recent history of plugged ducts, and you experience flu-like symptoms, fever, and breast pain with redness and heat. Antibiotics are very effective in treating an infection. You’ll probably feel better within two days after starting the antibiotics, but it’s important to finish the entire course of antibiotics. The antibiotics chosen are safe for continuing breastfeeding.
With diligent self-care and adherence to your doctor’s directions, you can reduce your risk of a recurrence.
Culture of breast milk for microflora (Breast milk Culture, Routine. Aerobic Bacteria Identification)
Description
Test material Breast milk
Determination of infection in mother's milk.
Research is especially needed in women suffering from postpartum (lactational) mastitis. This is the most common complication after childbirth.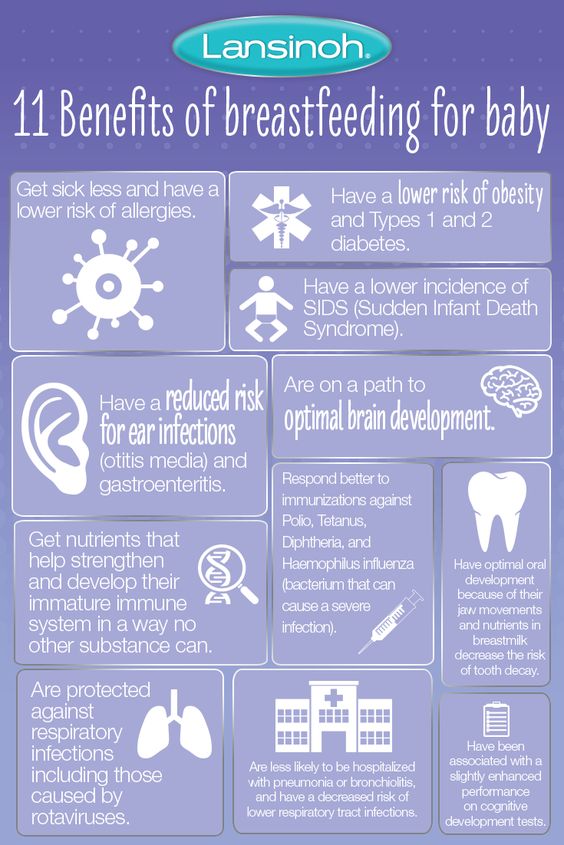 It is extremely dangerous that its initial forms, serous and infiltrative, can quickly turn into a purulent form, up to gangrenous.
It is extremely dangerous that its initial forms, serous and infiltrative, can quickly turn into a purulent form, up to gangrenous.
The main pathogen is Staphylococcus aureus, which is characterized by high virulence and resistance to many antibacterial drugs. Epidermal staphylococcus aureus, streptococcus, enterobacteria, Pseudomonas aeruginosa, etc. are no less dangerous. All of them are characterized by high virulence and polyresistance to antibiotics. Therefore, the exact determination of the pathogen and its sensitivity to antibiotics is extremely important.
This is due to the fact that, regardless of the pathogen, the clinical picture is almost identical: usually at 2-4 weeks of the postpartum period, the temperature quickly rises to 38-39degrees, chills occur. Often mastitis in 2 - 4 days turns into a purulent form.
If breastfeeding is continued, infected mother's milk and especially necessary antibiotic therapy can have an adverse effect on the newborn (dysbacteriosis).
Please note the need to purchase a sterile container for collecting urine and other biological fluids, which must be purchased in advance at any INVITRO medical office on bail. The return of collateral is carried out upon delivery of the analysis and subject to the availability of a check for making a deposit.
Literature
- Guidelines for the bacteriological control of breast milk. Main Department of Medical and Preventive Care for Children and Mothers. Ministry of Health of the USSR, 1984
- Medical Microbiology, Virology and Immunology: Textbook / Ed. A.A. Vorobyov. - M.: Medinformagency, 2004. - 691 p.
Preparation
The examination is carried out before the administration of antibiotics for mastitis and a few days after the end of treatment. Milk from the right and left mammary glands is examined separately.
Before pumping hands and mammary glands are treated with soap, nipples and peripapillary area with 70% alcohol (each gland is treated with a separate swab). The initial portion (5 - 10 ml) is not used for analysis, it is decanted into a separate bowl and poured out.
The initial portion (5 - 10 ml) is not used for analysis, it is decanted into a separate bowl and poured out.
Literature
- Guidelines for the bacteriological control of breast milk. Main Department of Medical and Preventive Care for Children and Mothers. Ministry of health of the USSR, 1984
- Medical Microbiology, Virology and Immunology: Textbook / Ed. A.A. Vorobyov. - M.: Medinformagency, 2004. - 691 p.
Indications
- Mastitis in lactating women.
- Monitoring the effectiveness of antibiotic therapy.
- Dysbacteriosis in children who are breastfed and mixed.
Literature
- Guidelines for the bacteriological control of breast milk. Main Department of Medical and Preventive Care for Children and Mothers. Ministry of Health of the USSR, 1984
- Medical Microbiology, Virology and Immunology: Textbook / Ed.
 A.A. Vorobyov. - M.: Medinformagency, 2004. - 691 p.
A.A. Vorobyov. - M.: Medinformagency, 2004. - 691 p.
Interpretation of results
Interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: anamnesis, results of other surveys, etc.
Specifies the presence or absence of growth, the total contamination, the type of grown microorganisms in the crop.
Interpretation: normal - no growth. When contaminated with associated flora, 1 or more types of bacteria are isolated in low titer (most often it is S. epidermidis). Staphylococcus aureus, bacteria of the Escherichia coli group, Pseudomonas aeruginosa are considered etiologically significant.
The total contamination is indicated as follows:
- massive growth: if the growth of bacteria in breast milk is more than 250 cfu/ml;
- non-massive growth: if the growth of bacteria in breast milk is less than 250 cfu/ml.
The question of stopping breastfeeding is decided by the attending physician, based on the results of the tests and the existing signs of the disease.
Literature
- Guidelines for the bacteriological control of breast milk. Main Department of Medical and Preventive Care for Children and Mothers. Ministry of health of the USSR, 1984
- Medical Microbiology, Virology and Immunology: Textbook / Ed. A.A. Vorobyov. - M.: Medinformagency, 2004. - 691 p.
Feeding in sickness | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less susceptible to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the possibility of using breast milk to treat many diseases, from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed?
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. 7
“Breastfeeding gives the baby everything she needs when she is sick. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. 8 When your baby is sick, the level of immune-boosting cells (leukocytes) in your milk also rises sharply. 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip."
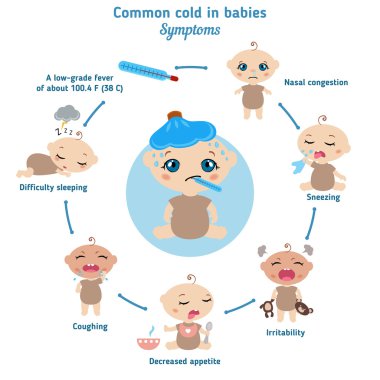
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time. If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed?
Occasionally, if a child feels unwell, they may not have an appetite or the strength to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable.
You can express milk with one of our convenient breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue to breastfeed if I become ill myself?
You may not want to do this if you feel unwell, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson.
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex ** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery.
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers.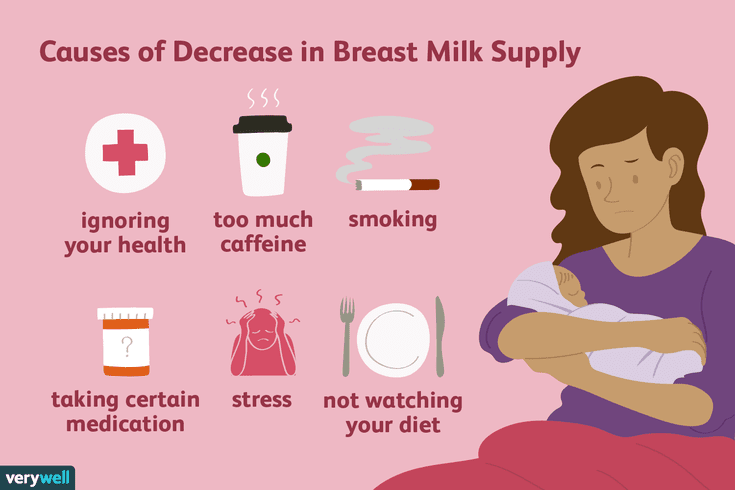 Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose.
Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose.
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, certain medications are allowed. 9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues.
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor.
There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor.
“I was on high doses of epilepsy medication but was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to keep my son safe and minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged.
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.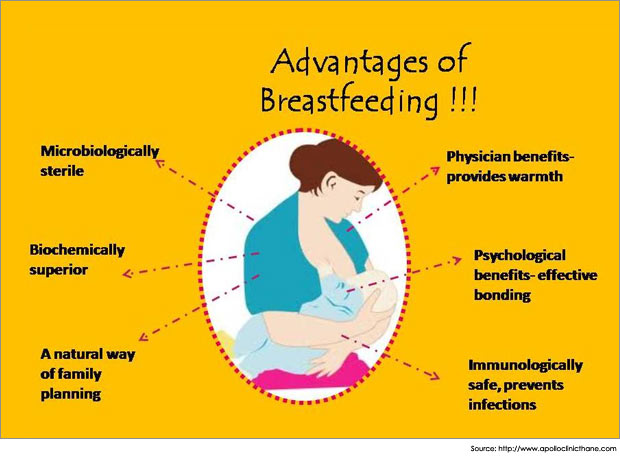
“If the baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account.
Surgery under local or general anesthesia does not necessarily mean that breastfeeding will have to be stopped, or milk will need to be pumped and discarded. By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, in all circumstances, it is best to consult your doctor or attending physician beforehand.
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk. 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if possible. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page.
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects. Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet]. "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F., Hartmann P.I., "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). 2017;12(9):500-506.
Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188.
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps".