Saline wipes for babies eyes
Sterile Saline Wipe for Eye Care, Case of 576
- Hospital Equipment
- Eye Care
Sterile Saline Wipe for Eye Care, Case of 576
Financing Options:
Product Specifications / Dimensions
| Dimensions | 4" x 6" |
| Scent | Unscented |
| Sterility | Sterile |
| Container Type | Individual Packet |
More Information
Each Sterile Saline Wipe for Eye Care comes with a lint-free applicator soaked with an isotonic solution of sodium chloride.
FAQ For Sterile Saline Wipe for Eye Care, Case of 576
?
Have a question about this product?
Click here to ask us!
Similar Products in the Eye Care Category:
Universal Eye Patch by Acu-Life
$17. 00
Amsler Grid Magnetic Pads - Qty. 3
$30.67
Autodrop Eye Drop Guide
$46.85
Emergency Eye Wash Bottle
$56.10
Leukoplast Fabric Eye Occlusor Bandage
$154.73
Autosqueeze Eye Drop Bottle Squeezer
$48.45
Nexcare Opticlude Orthoptic Eye Patch, Pack of 720
$359.18
Opticlude Orthoptic Eye Patches
$17.34
Pocket-Size Eyewash Bottle
$53.11
Proudly Serving Customers Like You And:
HELP & MORE INFO
Multi-year Inc. 5000 Awarded Business x 4
Shop Securely & With Confidence
Convenient Ways to Pay
Standard Ground Shipping
Most items are processed within 24 hours and are shipped from the warehouse within 48 hours
via 3-7 business day ground delivery service (unless lead-time is otherwise noted on the product page). Free ground shipping only applies to the 48 contiguous United States. Hawaii, Alaska, Puerto Rico and all
international orders are subject to additional fees.
Orders placed over the weekend will be processed first thing Monday morning.
We will attempt to notify you by email and provide a tracking # when your product(s) ship.
Free ground shipping only applies to the 48 contiguous United States. Hawaii, Alaska, Puerto Rico and all
international orders are subject to additional fees.
Orders placed over the weekend will be processed first thing Monday morning.
We will attempt to notify you by email and provide a tracking # when your product(s) ship.
Freight Shipping (Truck Freight)
Heavy items (anything over 150 lbs), bulk-freight, and pallet truck items and custom fabrication
made-to-order items may have longer shipping lead times.
Customer will be notified as soon as Truck-Freight items become available for overland freight shipment
across the 48 contiguous United States.
If you do not have a loading-dock, be sure to choose lift-gate as your delivery option when
purchasing an overland-freight truck item.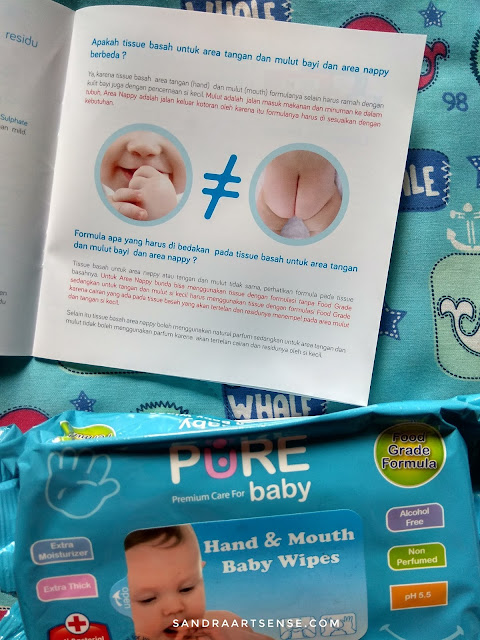 Free Freight Shipping, when applicable, only applies to the 48 contiguous United States.
Hawaii, Alaska, Puerto Rico and all international orders are subject to additional fees.
Free Freight Shipping, when applicable, only applies to the 48 contiguous United States.
Hawaii, Alaska, Puerto Rico and all international orders are subject to additional fees.
Caring for your baby’s ‘sticky’ and ‘watery’ eyes
Skip to content Caring for your baby’s ‘sticky’ and ‘watery’ eyesYour baby’s eyes are kept moist and healthy by tears that wash over the surface of their eyes constantly. Tears are produced in the lacrimal glands and there is one lacrimal gland above each eye. Your baby’s tears are then carried away from the eye by a tear duct, which is a very fine tube. When babies are born, their tear ducts are sometimes not fully developed and patent (clear). Studies have shown that approximately one in five babies are born with tear ducts that are not fully developed and either one or both eyes may be affected in this way. In the majority of cases however, the tear ducts will develop slowly over a few weeks, without any need for intervention or there being any problems. For some babies however, this process can take several months to complete.
For some babies however, this process can take several months to complete.
It is also possible for a baby’s tear ducts to become blocked by amniotic fluid or debris deposited around the time of their birth eg vernix and skin cells. See also our article, ‘Your newborn baby’s skin’. Many parents do not realise that their newborn baby is unable to shed tears in the initial weeks following their birth – this is perfectly normal. Because babies do not produce tears, it is very difficult for any debris that has collected to be washed away. You may therefore, need to wipe away any eye discharge that has accumulated and this will be explained later in this article.
Newborn babies frequently develop watery or sticky eyes after their birth. You may notice a collection of clear, white or yellow-coloured discharge at the inner corner of your baby’s eyes (closest to their nose). This discharge is often particularly noticeable during the first 48 hours after your baby’s birth. Where this discharge collects over a period of time, especially overnight, it can dry out forming a crust on your baby’s eyelid(s) and/or eyelashes. This can sometimes cause your baby’s eyelids and eyelashes to become partially glued together, which can be particularly noticeable first thing in the morning. However, the surface of your baby’s eyes – the ‘sclera’ should still continue to look white and healthy despite the presence of any discharge. Your midwife and health visitor will describe this condition as ‘sticky eyes’. In most cases sticky eyes are perfectly harmless and there is no infection present. Occasionally, you may notice that your baby’s eyes do begin to look slightly pink, which is a sign of mild inflammation; however, this usually resolves without requiring any treatment.
Where this discharge collects over a period of time, especially overnight, it can dry out forming a crust on your baby’s eyelid(s) and/or eyelashes. This can sometimes cause your baby’s eyelids and eyelashes to become partially glued together, which can be particularly noticeable first thing in the morning. However, the surface of your baby’s eyes – the ‘sclera’ should still continue to look white and healthy despite the presence of any discharge. Your midwife and health visitor will describe this condition as ‘sticky eyes’. In most cases sticky eyes are perfectly harmless and there is no infection present. Occasionally, you may notice that your baby’s eyes do begin to look slightly pink, which is a sign of mild inflammation; however, this usually resolves without requiring any treatment.
Watery eyes usually resolve on their own, but your baby’s eyes can become watery again if they develop a head cold and their tear ducts become blocked again. Very rarely, watery eyes can indicate there might be other eye problems, so should you have any concerns, it is important that you contact your GP for their advice. If your baby’s tear duct is still blocked by the time they are 12 months’ of age, your GP may advise that your baby is referred to an eye specialist for a minor operation that opens up their tear duct.
If your baby’s tear duct is still blocked by the time they are 12 months’ of age, your GP may advise that your baby is referred to an eye specialist for a minor operation that opens up their tear duct.
If your baby develops sticky eyes, these should be cleaned regularly to prevent a build up of discharge. Where discharge builds up, it is possible for infection to then develop either in the tear duct or the conjunctiva (conjunctivitis). Ideally, you should aim to clean your baby’s eyes every four hours, although you may need to do this more often if their eyes are particularly sticky. If you are still in hospital, the ward staff will show you how to clean your baby’s eyes using sterile salt water – Normal Saline (Sodium Chloride) and cotton wool balls. If you are back at home your community midwife or health visitor can help you with this. You can use ‘cooled’ boiled tap water for cleaning your baby’s eyes; however, using boiled water can cause their eyes to become irritated, so it may be worth asking your midwife, health visitor or GP for some ampoules (plastic pods) of sterile saline.
a). Hand hygiene is very important to prevent infection being introduced into your baby’s eyes. Always wash your hands thoroughly with soap and water before and after bathing each eye
b). Dampen a clean cotton wool ball with sterile saline/cooled boiled water and in one gentle movement, clean along the lash line from the inner corner of your baby’s eye across to the outer corner. Discard the used cotton wool after use
c). This action may need to be repeated more than once in order to remove all the discharge present. Ensure you use a clean cotton wool ball each time
d). Dry your baby’s eye using a clean cotton wool ball – in one gentle action move in the same direction from the inner corner of the baby’s eye outwards
e). Clean your baby’s other eye in the same way. It is very important that you never use the same cotton wool ball for both eyes, because this can spread any infection that might be present
f). Where the eye discharge has dried and become crusted, your baby’s eyelids or lashes may be partially stuck together. Where this is the case, it is important that you don’t try to force their eyelids/lashes apart with your fingertips. Instead, you should always bathe their eyes open using the above technique.
Where this is the case, it is important that you don’t try to force their eyelids/lashes apart with your fingertips. Instead, you should always bathe their eyes open using the above technique.
Where your baby’s tear duct(s) is blocked, massaging it every few hours can help remove the blockage and open up the tear duct. You can do this by gently applying light pressure to the skin over the tear duct between the inner corner of your baby’s eye(s) and their nose. Massage down the side of the nose, moving from the top to the bottom.
Conjunctivitis
While your baby’s tear duct(s) is developing, they can be more prone to picking up infection and developing conjunctivitis. This is where the eyes become inflamed (pink and sore) and the delicate skin around them can become swollen. Conjunctivitis tends to cause a more profuse ‘yellow’ coloured discharge and you may notice that your baby keeps rubbing their eyes because they feel itchy. Where this happens, the infection can be easily introduced from one eye into the other.
While conjunctivitis is a very mild infection, it is nevertheless, extremely contagious and very easy to pick up. It tends to be seen more often in toddlers and school age children. If you think your baby may have developed conjunctivitis, they will need to be seen by your GP. They may advise that your baby is started on antibiotic eye drops or ointment. In order to make sure that your baby has the right antibiotics to fight off the infection, an eye swab will be taken. This enables a sample of the discharge to be examined in a laboratory.
Hand hygiene is very important when bathing your baby’s eyes and instilling eye drops/ointment, because conjunctivitis is so highly contagious. It is therefore best to use a separate hand towel to prevent the infection being picked up by other family members.
If your baby appears to be in pain or is reluctant to open their eyes, or the discharge is a greenish colour and won’t clear up – always contact your GP for their immediate advice.
Elston J (1985). Sticky eyes in infancy. Maternal and Child Health 10(8):248, 250-251.
Fok TF, Wong W, Cheng AFB (1995). Use of eyepatches in phototherapy: effects on conjunctival bacterial pathogens and conjunctivitis. Pediatric Infectious Disease Journal 14(12):1091-1094.
Harris MJ (1996). Infections in the first months of life. Journal of Paediatrics, Obstetrics and Gynaecology 22(2):13-15.
Matejcek A, Goldman RD (2013). Treatment and prevention of ophthalmia neonatorum. Canadian Family Physician 59(11).
Moten J, McGuiness B (2000). Is your midwifery practice evidence based? Here’s milk in your eye: an exploration of the use of colostrum for the treatment of ophthalmia neonatorum. Open Line 8(2):6-7.
Newell SJ, Miller P, Morgan I et al (1997). Management of the newborn baby: midwifery and paediatric perspectives. In: Henderson C, Jones K eds. Essential midwifery. London: Mosby. 229-264.
In: Henderson C, Jones K eds. Essential midwifery. London: Mosby. 229-264.
Verd S (2007). Switch from antibiotic eye drops to instillation of mother’s milk drops as a treatment of infant epiphora. Journal of Tropical Pediatrics 53(1):68-69.
Zuppa AA, D’Andrea V, Catenazzi P et al (2011). Ophthalmia neonatorum: what kind of prophylaxis? Journal of Maternal-Fetal and Neonatal Medicine 24(6):769-773.
Useful websites
http://www.nhs.uk/Conditions/Watering-eye/Pages/Treatment.aspx [Accessed 23 January 2014]
http://www.patient.co.uk/health/tear-duct-blockage-in-babies [Accessed 23 January 2014]
Parents Powwow2017-05-26T16:29:16+01:00Recent Information
- Abdominal Palpation
- Lansinoh HPA Lanolin Nipple Cream
- Difficulties getting pregnant
- Doing a pregnancy test
- How can I increase my chances of getting pregnant?
Acute intestinal infections in babies
The baby fell ill suddenly: body temperature rose, vomiting appeared. The chair became frequent, liquid, plentiful, watery. It contained inclusions of undigested food, sometimes an admixture of mucus, greenery, less often - streaks or an admixture of blood. All bases to assume, what is it an intestinal infection.
The chair became frequent, liquid, plentiful, watery. It contained inclusions of undigested food, sometimes an admixture of mucus, greenery, less often - streaks or an admixture of blood. All bases to assume, what is it an intestinal infection.
Due to repeated vomiting and frequent liquid stools in young children, severe, life-threatening dehydration can occur as early as 6-8 hours. A high temperature, sometimes rising to 40-41 0 , capable of "leading" convulsions.
Call a doctor immediately and start acting energetically without missing a beat: in such a situation, you yourself must become an "ambulance"! Now it doesn’t matter what has overtaken the baby: dysentery, salmonellosis, rotavirus or other intestinal infection (more than 40 pathogens are known) - all of them at first manifest themselves very similarly, and first aid, both with high body temperature and with dehydration of the body as a result of vomiting and frequent loose stools are the same.
To prevent dehydration of the baby's body, from the first hours, start giving the child boiled water - "drink" him. But since not only water is lost with loose stools and vomit, but also salts of sodium, potassium, chlorine and other electrolytes, which are essential for the normal functioning of the heart, kidneys, brain and other organs, water alone is not enough, saline solutions are required.
But since not only water is lost with loose stools and vomit, but also salts of sodium, potassium, chlorine and other electrolytes, which are essential for the normal functioning of the heart, kidneys, brain and other organs, water alone is not enough, saline solutions are required.
For more than 30 years all over the world for oral rehydration (compensation of pathological losses of water and electrolytes through the mouth - "drinking" in case of intestinal infections) glucose-salt solutions specially developed by WHO have been used. In our country, Regidron, which is produced in powders and freely sold in pharmacies, has been widely used both in hospitals and in the treatment of intestinal infections at home. Before use, the contents of the sachet are diluted in a liter of warm boiled water and given to the child to drink. The drug effectively compensates for the existing losses of water and electrolytes, prevents further dehydration of the child's body and aggravation of his condition, but does not have a pronounced therapeutic effect.
In recent years, in accordance with the recommendations of the European Society for Pediatric Gastroenterology and Nutrition (ESPGAN), for better absorption of water and electrolytes in the intestine, the electrolyte composition of solutions has been slightly changed, namely, their osmolarity and sodium-glucose ratio have been reduced. In many pharmacies, the Gastrolit glucose-saline solution, which meets the new standard, has already appeared on sale. Unlike rehydron, gastrolith also contains chamomile extract, which additionally has an anti-inflammatory, antiseptic and antispasmodic effect on the intestines, that is, "Gastrolit" also has a therapeutic effect.
Which glucose-saline solution is best for drinking ?
There are no significant differences in their effectiveness, but when a child is "drinked" with a solution of "Gastrolit", abdominal pain, vomiting, flatulence phenomena (bloating, rumbling, etc.) disappear 1-2 days faster, the frequency and watery nature of the stool decrease . Before use, the content of 1 sachet of gastrolith is diluted in 200 ml necessarily hot boiled water to obtain chamomile infusion and cooled to room temperature.
Before use, the content of 1 sachet of gastrolith is diluted in 200 ml necessarily hot boiled water to obtain chamomile infusion and cooled to room temperature.
If these solutions are not available at home, prepare a decoction - for 1 liter of water, either 100 g of raisins or 500 g of carrots (cut into pieces and boil). Add a teaspoon of table salt (without top), ½ teaspoon of baking soda, 4 teaspoons of granulated sugar to it, bring to a boil and cool - the “homemade rehydron” is ready. It is even easier to prepare a sugar-salt solution - for 1 liter of boiled water you need a teaspoon of salt, ½ teaspoon of baking soda and 8 teaspoons of granulated sugar.
When "drinking" an infant with these solutions, drink from a spoon every 5-7-10 minutes. But little by little! For example, 1-3 teaspoons or 2-3 "sips" through the nipple. It is impossible to give a lot of liquid at once, even if he drinks greedily - this can provoke a new attack of vomiting. For a child 2-3 years old and older, a single dose of solutions can be increased to 2-3 tablespoons, and intervals - up to 10-15 minutes.
What is the total volume of fluid needed to compensate for the pathological loss of water and electrolytes with stool and vomiting ?
WHO experts recommend that in the presence of vomiting and "watery" stools, a young child loses about 10 ml per 1 kg of body weight for each bowel movement. For example, a child weighing 10 kg with each loose stool will lose 100 ml of fluid, which must be “drinked” between bowel movements and feeding the child. To avoid dehydration, the child should receive a total of approximately as much fluid per day, including nutrition, as a healthy baby of the same age needs, plus the amount lost with vomiting and loose stools. If he eats less than he should (and during illness this is almost inevitable), then the missing amount of food must be compensated by liquid.
When gastrolith is used, the solution must not be sweetened and can only be “drained” with gastrolith alone. Age dosages of the required volume of the prepared gastrolith solution for children are detailed in the attached instructions. While the solution of rehydron should be only half the required daily amount of liquid. In this case, the intake of rehydron should be alternated with the intake of the same volume, either weakly brewed unsweetened tea, or boiled water or 5% glucose solution, which can be bought at a pharmacy.
While the solution of rehydron should be only half the required daily amount of liquid. In this case, the intake of rehydron should be alternated with the intake of the same volume, either weakly brewed unsweetened tea, or boiled water or 5% glucose solution, which can be bought at a pharmacy.
It is widely believed that a solution of potassium permanganate (potassium permanganate) helps stop vomiting and diarrhea. I often give it to drink, make enemas with it. Vomiting and diarrhea in most cases really stop, but only for a few hours. Moreover, the chair is absent from the fact that under the influence of potassium permanganate, a fecal plug is often formed, which prevents the exit of intestinal contents. And it's far from safe! With loose stools, the body is freed from a huge amount of pathogenic microbes and viruses, pathogens of intestinal infections, their toxins, gases and other toxic substances formed in the intestines as a result of inflammatory or fermentation processes. With a fecal plug, all of them, lingering in the intestines, begin to be absorbed into the blood, and after a few hours of “relative” well-being, the child’s condition deteriorates sharply - bloating, shortness of breath and indomitable vomiting appear. In such cases, immediate hospitalization is required.
With a fecal plug, all of them, lingering in the intestines, begin to be absorbed into the blood, and after a few hours of “relative” well-being, the child’s condition deteriorates sharply - bloating, shortness of breath and indomitable vomiting appear. In such cases, immediate hospitalization is required.
There are even worse situations with potassium permanganate. A sick baby is given a concentrated solution, believing that it will work more efficiently or a solution containing undissolved crystals. And the ending is tragic: burns of the mucosa of the gastrointestinal tract, intestinal bleeding, intestinal perforation with the development of peritonitis, requiring urgent surgical intervention, and even the death of a child.
Please do not give potassium permanganate by mouth to children under any circumstances !
Vomiting and diarrhea in intestinal infections are initially protective in nature - the body tries to "throw out" microbes and toxic products with vomit and frequent loose stools. It is more expedient to help the body in this - to wash the stomach and even make a cleansing enema. At home, let the child drink as much boiled water as possible and the vomiting that has begun will “wash out” microbes and toxins from the stomach. If it is not there, call it yourself by pressing on the root of the tongue with the handle of a clean spoon, in extreme cases, with a finger wrapped in a sterile gauze or bandage. This should be repeated 2-3 times, and then let the child drink an enterosorbent (smecta, filtrum, enterosgel, etc.), strictly observing the age dosages indicated in the instructions. Enterosorbents "bind" microbes, viruses and their poisons in the gastrointestinal tract, then remove them with feces, which greatly facilitates the course of the disease, quickly reduces the frequency and improves the consistency of the stool. It is not rational to use activated carbon for this purpose - its effectiveness in normal dosages is very low.
It is more expedient to help the body in this - to wash the stomach and even make a cleansing enema. At home, let the child drink as much boiled water as possible and the vomiting that has begun will “wash out” microbes and toxins from the stomach. If it is not there, call it yourself by pressing on the root of the tongue with the handle of a clean spoon, in extreme cases, with a finger wrapped in a sterile gauze or bandage. This should be repeated 2-3 times, and then let the child drink an enterosorbent (smecta, filtrum, enterosgel, etc.), strictly observing the age dosages indicated in the instructions. Enterosorbents "bind" microbes, viruses and their poisons in the gastrointestinal tract, then remove them with feces, which greatly facilitates the course of the disease, quickly reduces the frequency and improves the consistency of the stool. It is not rational to use activated carbon for this purpose - its effectiveness in normal dosages is very low.
After gastric lavage and enterosorbent intake, vomiting in intestinal infections usually stops. If this does not happen, then vomiting and diarrhea, especially in infants, may be one of the manifestations of diseases such as appendicitis, influenza, otitis media, pneumonia, meningitis, etc. In these cases, it is necessary to call a doctor at home or an ambulance » for the hospitalization of the child in the appropriate hospital. It is better to stop therapeutic measures before the doctor arrives, with the exception of antipyretics, and the volume of liquid for “drinking” should not exceed pathological losses with loose stools.
If this does not happen, then vomiting and diarrhea, especially in infants, may be one of the manifestations of diseases such as appendicitis, influenza, otitis media, pneumonia, meningitis, etc. In these cases, it is necessary to call a doctor at home or an ambulance » for the hospitalization of the child in the appropriate hospital. It is better to stop therapeutic measures before the doctor arrives, with the exception of antipyretics, and the volume of liquid for “drinking” should not exceed pathological losses with loose stools.
To feed or not to feed ?
The general rule is this: it is necessary to give food, reducing the daily amount of food, but not more than half. However, it all depends on the frequency of vomiting and the condition of the child, and this is what you need to focus on. Ideal: feed "according to appetite", but more often and in small portions, so as not to overfill the stomach and not provoke vomiting. If the baby is breastfed, continue breastfeeding. But with frequent vomiting (or regurgitation), it is better to switch to “metered” feeding with expressed breast milk in small portions at regular intervals (after 2-2.5-3 hours with a night break). A baby who is bottle-fed, as well as a 2-3-year-old child and older, on the first day of the disease can be fed with normal food (kefir, cottage cheese, adapted infant formula, cereals with half milk, etc.), but preference should be given to medical - prophylactic food products enriched with bifido- or lactobacilli (children's kefir "Bifidok", mixture "Agusha", acidophilic mixture "Baby", "Kroshechka", etc.).
But with frequent vomiting (or regurgitation), it is better to switch to “metered” feeding with expressed breast milk in small portions at regular intervals (after 2-2.5-3 hours with a night break). A baby who is bottle-fed, as well as a 2-3-year-old child and older, on the first day of the disease can be fed with normal food (kefir, cottage cheese, adapted infant formula, cereals with half milk, etc.), but preference should be given to medical - prophylactic food products enriched with bifido- or lactobacilli (children's kefir "Bifidok", mixture "Agusha", acidophilic mixture "Baby", "Kroshechka", etc.).
In case of a pronounced fermentation process (increased gas formation, bloating and rumbling in the abdomen, foamy stools, etc.), it is better to replace the child’s usual food for several days with commercially available and age-adapted low-lactose or lactose-free baby foods. It is also recommended to introduce cereals on water or vegetable broths into the diet, an earlier appointment of meat gosha is shown.
Older children in the acute period of intestinal infection should be completely excluded from the diet of foods that cause fermentation in the intestines and increased gas formation, containing coarse fiber: whole milk and cereals with whole milk, fermented baked milk, cream, black bread, meat, chicken and fish broths, dishes from beans, peas, beets, cabbage, grapes, citrus fruits, as well as all fatty, fried, canned food (except canned food for baby food), limit sweets. Carbonated drinks (fanta, etc.) are also prohibited.
Emergency treatment for high body temperature.
The temperature is not higher than 38 0 (if the child tolerates it well and provided that such rises were not accompanied by convulsions before), you can not “knock down”. But if the mercury column rises above 38-38.5 0 or the so-called "convulsive readiness" appears - trembling of the fingertips and chin, proceed to intense antipyretic measures.
Attention! If the hands and feet are hot , like the rest of the body - start with physical methods of cooling. Undress the baby and fan it vigorously (option: put a fan nearby). Put a napkin moistened with cold water and wrung out on your forehead, and plastic bags with ice or bottles of cold water wrapped in a thin cloth in the armpits and inguinal cavities. Let's drink cool water or a glucose-salt solution (rehydron or gastrolith) as often as possible.
Undress the baby and fan it vigorously (option: put a fan nearby). Put a napkin moistened with cold water and wrung out on your forehead, and plastic bags with ice or bottles of cold water wrapped in a thin cloth in the armpits and inguinal cavities. Let's drink cool water or a glucose-salt solution (rehydron or gastrolith) as often as possible.
If the temperature has risen to 40 0 and above, wiping the body with 3% vinegar or a special mixture is required: water, table vinegar (not essence) and alcohol in equal amounts. Pour the prepared mixture into the palm of your hand and rub the baby’s chest, stomach, back, arms and legs quite intensively, but very carefully - everything except the face. It is very useful to wear stockings or socks moistened with this liquid.
The temperature should drop after 10-15 minutes. If there is no effect, give the child antipyretics: children's panadol, efferalgan, etc. As soon as the temperature drops to at least 38 0 , stop physical cooling. If after some time it rises again, then repeat the cooling measures until the doctor or ambulance arrives.
If after some time it rises again, then repeat the cooling measures until the doctor or ambulance arrives.
Attention! If the hands and feet are cold - doctors call this condition “white hyperthermia”: it indicates a violation of heat transfer due to spasm (contraction) of skin vessels and then physical methods of cooling are contraindicated! They can increase the spasm, the heat transfer will decrease, the temperature will rise even more and the child's condition will worsen before our eyes. You can only gently rub the body with a water-vinegar-alcohol mixture, if possible, to a slight reddening - this procedure expands the blood vessels of the skin and heat transfer increases.
The main thing to reduce the temperature in such cases is antipyretics for children, as well as vasodilators - papaverine, dibazol, etc.
If convulsive readiness or convulsions appear, in addition to antipyretics, give the child any of the antihistamines: pipolfen (it also has an antiemetic effect), suprastin, etc. But this is not enough. If there are convulsions, you can’t hesitate and wait for the local pediatrician - call an ambulance!
But this is not enough. If there are convulsions, you can’t hesitate and wait for the local pediatrician - call an ambulance!
Open a window for fresh air - oxygen is vital for a child;
Don't leave your baby alone, he might fall out of bed. If he is lying on his back, turn his head to one side so that he does not choke on vomit. Even better, the position on his side - this will facilitate their discharge;
Wipe your mouth with a damp gauze pad around your finger to remove vomit and mucus;
· Be careful not to sink the tongue - this threatens to suffocate;
Try not to pick it up so as not to cause pain, but hold it upright when you pick it up.
As the temperature decreases, convulsions usually disappear.
And finally, one more recommendation-caution: all medicines should be only in the age dose. Grind the tablets, dilute in boiled water and give from a spoon. No other drugs (especially antibiotics) - without a doctor's prescription! Do not rush to give enzyme preparations, especially proteolytic (abomin, etc. ) and pancreatin with bovine bile components (festal, etc.) - they can only increase diarrhea, especially with intestinal infections of viral etiology, which in young children are up to 70 -80% of the total. The appointment of antibiotics or other antibacterial drugs (furazolidone, etc.) in these cases only aggravates the course of the disease and contributes to the development of dysbacteriosis.
) and pancreatin with bovine bile components (festal, etc.) - they can only increase diarrhea, especially with intestinal infections of viral etiology, which in young children are up to 70 -80% of the total. The appointment of antibiotics or other antibacterial drugs (furazolidone, etc.) in these cases only aggravates the course of the disease and contributes to the development of dysbacteriosis.
Acute intestinal infections, except for severe forms, can be treated at home. The main directions of treatment tactics and during the hospitalization of the child are the same: a rational diet, "drinking", enzyme preparations (pancreatin, mezim forte, etc.), symptomatic therapy (antiemetic, antipyretic, analgesic drugs, etc.). In severe dehydration, a drip is prescribed.
In recent years, highly effective methods have been developed for the treatment of intestinal infections without antibiotics, including severe forms, using probiotics, enterosorbents, and specific immunoglobulin preparations.
Remember, the earlier treatment is started, the more effective it is. If your baby has diarrhea and/or vomiting, call the doctor at home. Only he, having understood the various causes of the disease, can prescribe the necessary treatment.
61835
We answer your questions in a special section! Most often these are questions of an individual nature in relation to vaccination, immunity and the like.
Questions are answered:
- Immunization specialists
Ask a question
How to choose a lens solution?
Long-life contact lenses - two weeks, a month, three months or more - require daily mechanical cleaning and disinfection with a special solution. This is important not only for the quality of vision, but also for the health of the patient's eyes.
The solution is needed for cleaning and storing lenses, as well as for rinsing the container and tweezers. We tell you how lens care products differ and how to choose a solution that is suitable for your type of lenses.
We tell you how lens care products differ and how to choose a solution that is suitable for your type of lenses.
Bonus at the end of the article - TOP-5 best solutions.
Types and purpose of lens solutions
Contact care products are divided into four types, depending on the functions they perform.
Water-salt
This type of solution is practically not used today, but in the past it was almost the only option for cleaning lenses. Therefore, some patients from those who have been using contact correction for a long time still use it.
Water-salt solution moisturizes and softens lenses, but it does not provide a disinfectant function, so ophthalmologists recommend that this product be discarded.
Multipurpose
Multipurpose (or universal) solution is the best option for everyday use. The tool performs all the functions that are needed for high-quality and safe use of contact lenses:
- Disinfection - the destruction of bacteria, fungi and other microorganisms dangerous to the eyes;
- Moisturizing;
- Cleaning from dirt and dust;
- Removal of protein and lipid deposits that are part of the lacrimal fluid.
The products are considered universal and in most cases suitable for any type of lens, but it is better to consult a specialist before buying - it is important that the liquid is combined with the material from which the lenses are made.
Thanks to a special formula, some products save the patient from the need to mechanically clean the lenses - disinfection and removal of contaminants occur even without it. That is, the patient can simply remove the means of contact correction and immediately place them in a container with a fresh solution. However, this should be discussed with an ophthalmologist as not all solutions are suitable for this cleaning.
Another advantage of multifunctional products is that they do not cause burning, pain or other unpleasant sensations when they get into the eyes.
Enzymatic (enzymatic)
Enzymatic products are designed to remove organic deposits that multifunctional solutions cannot cope with. As a rule, this is true for lenses with a long replacement period. So, for example, they are often recommended for cleaning orthokeratology lenses, the replacement period of which is one year.
So, for example, they are often recommended for cleaning orthokeratology lenses, the replacement period of which is one year.
Enzyme products are in the form of tablets to be added to the multifunctional solution. Suitable for soft and hard lenses.
Peroxide
Solutions based on hydrogen peroxide provide high-quality and deep cleaning of lenses from possible bacteria, fungi and deposits. However, these products do not moisten the lenses and are not suitable for lens storage.
If hydrogen peroxide gets into the eyes, it will cause burning and pain. In some cases, peroxide can even cause corneal burns or mucosal inflammation. Therefore, after using a peroxide solution, the lens must be washed or the exposure time must be maintained, after which the solution will be neutralized and become safe.
In addition, the product is not suitable for everyday use. Contraindicated for hydrogel contact lenses.
Fluid selection
It is not recommended to select the fluid yourself. Seek help from a specialist, he will assess the condition of the eyes and select a product that suits your type of contact lenses.
Seek help from a specialist, he will assess the condition of the eyes and select a product that suits your type of contact lenses.
Sign up for a selection of contact lenses
Top 5 solutions for lenses
Introducing a selection of the best contact lens care products.
Opti Free
Another multifunctional solution that fits all types of soft contact lenses, Opti Free. Provides deep disinfection, reduces the amount of lipid deposits and maintains continuous hydration of the lenses for 16 hours.
Manufactured by Alcon.
Biotrue
Biotrue is a multifunctional solution designed for hydrogel and silicone hydrogel contact correction products. The acidity pH is close to natural tears, making the liquid suitable even for patients with high eye sensitivity or a tendency to allergies.
Manufacturer - Bausch & Lomb.
Aculife
Aculife Multipurpose Soft Lens Solution contains hyaluronic acid, which keeps lenses moist for a long time.