Infant sickness symptoms
Newborn Illness - How to Recognize
Is this your child's symptom?
- How infections and other serious diseases can present in newborns
- Newborns are at higher risk for infections. Infections may present at any time during the first month. Watch your baby carefully for signs of illness. This is especially crucial during the first 7 days of life.
- Newborns that get a blood infection (sepsis) can get very sick quickly.
- The symptoms of serious illness in newborns can be subtle. The question below deals with sick newborns:
- "Age under 1 month old (newborn) and starts to look or act abnormal in any way." Look for this question in the "Call Your Doctor Now" section. It is listed in at least 10 topics.
- Feeding is the one reliable measure of a newborn's well-being. Newborns should be eating machines. If your baby isn't feeding well, call your baby's doctor. Also, call if your baby has an abrupt change in his feeding pattern.
(Exception: never a good feeder, but takes enough milk and nothing has changed).
- If how your baby looks or acts changes and it's not normal, call now. Don't wait to call your baby's doctor for expert advice.
When to Call for Newborn Illness - How to Recognize
Call 911 Now
- Can't wake up
- Not moving or very weak
- New moaning or grunting noises with each breath
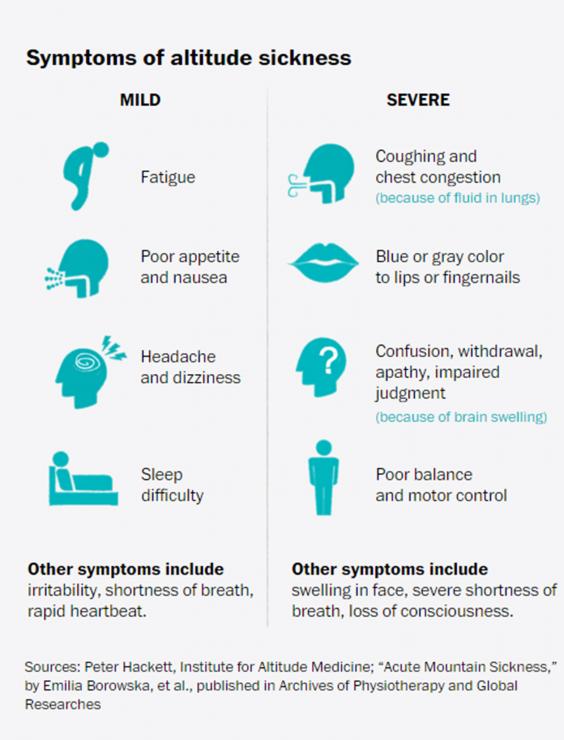
- Bluish (or gray) lips, tongue or face now
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
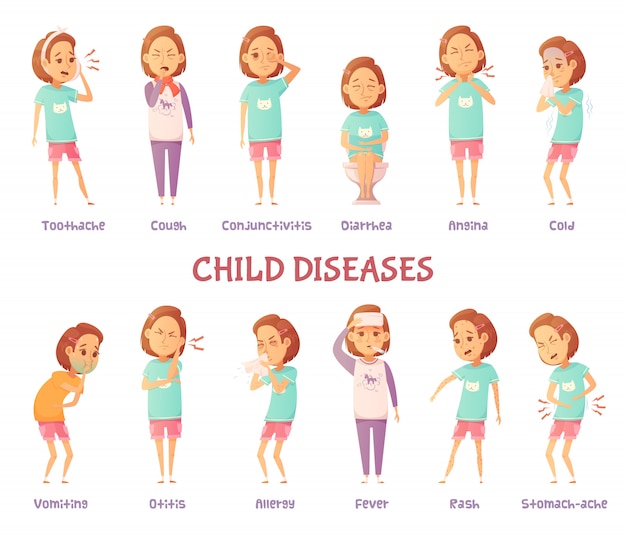
- Any symptoms of illness such as coughing, diarrhea or vomiting
- Changes in feeding. Signs are having to wake up for feeds or can't finish feeds.
- Sweating during feedings
- Sleeping more than normal
- Change in color (such as pale, bluish or gray arms and legs)
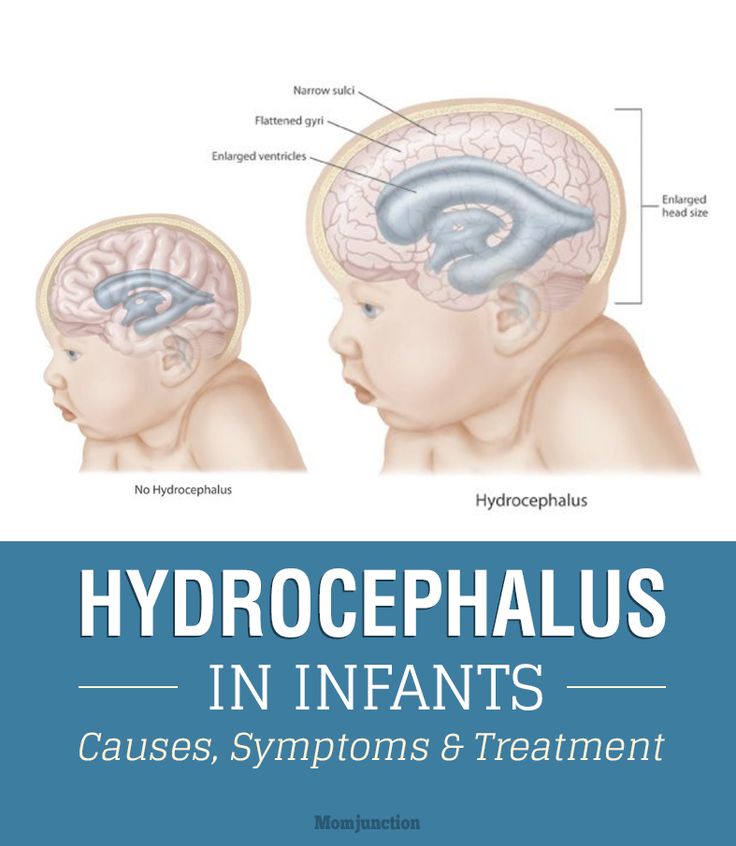
- Soft spot on top of head looks swollen
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.

- Low temperature below 96.8° F (36.0° C) rectally that does not go up with warming
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Urine color is pink, orange or peach
- You think your child needs to be seen, but the problem is not urgent. Child has none of the urgent symptoms listed above.
- You have other questions or concerns
Self Care at Home
- Your baby is feeding, moving and sleeping normally
- There are no signs of illness
- Your newborn is well
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Newborns Without Signs of Illness
- What You Should Know About Newborn Illness:
- Based on this review, your baby doesn't have any signs of illness right now.

- The symptoms of serious illness in newborns can be subtle. Watch your baby carefully for signs of illness. If how your baby looks or acts changes and it's not normal, call now.
- During the early weeks of life, careful watching is always the best approach.
- Based on this review, your baby doesn't have any signs of illness right now.
- Call Your Doctor If:
- Your baby has a fever
- Your baby has any symptoms of illness
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/21/2022
Last Revised: 01/21/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Recognizing Newborn Illnesses - familydoctor.org
Bringing your baby home from the hospital is a very exciting time.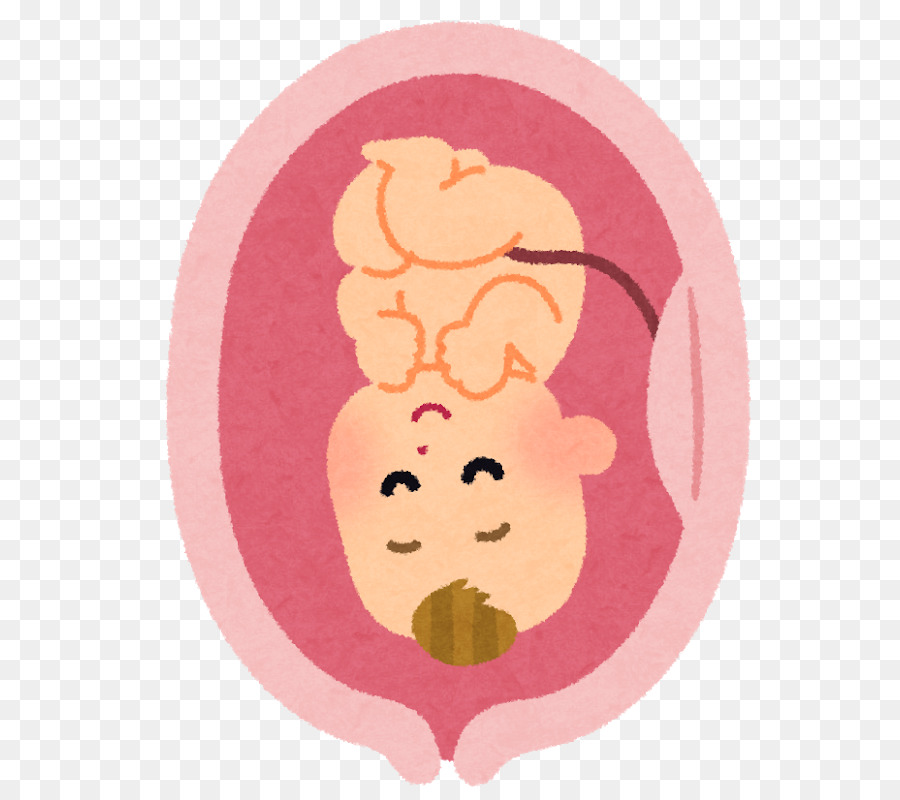 But having a newborn around can be stressful for lots of reasons. One of these is concern about the new baby getting sick. How will you know? It can be hard to tell when a newborn is sick. You may not know what your baby’s normal behavior is yet. This makes it difficult to tell if your baby’s behavior is not normal. Signs of serious illness in newborns can be subtle. They aren’t always easy to spot.
But having a newborn around can be stressful for lots of reasons. One of these is concern about the new baby getting sick. How will you know? It can be hard to tell when a newborn is sick. You may not know what your baby’s normal behavior is yet. This makes it difficult to tell if your baby’s behavior is not normal. Signs of serious illness in newborns can be subtle. They aren’t always easy to spot.
It is important to be aware of what signs could mean that your newborn is sick. Their immune system is not as strong after birth, so it’s harder for them to fight off infections. And once they do get an infection, it can get worse quickly. That’s why you should know what to look for.
Path to improved health
One of the main things to look for in your newborn is if they look or act in any way that seems abnormal to you. If this happens, call your baby’s doctor right away. Some of the ways they could look or act abnormal include:
- Any symptoms of illness. These include crying more often, irritability, coughing, diarrhea, or vomiting.
 If your newborn vomits green (bile), call the doctor right away.
If your newborn vomits green (bile), call the doctor right away. - Changes in feeding. Newborns usually eat frequently. If you have to wake your newborn to eat or they can’t finish their feedings, they could be sick.
- If your newborn has a fever, especially over 100.4 F (38 C), call the doctor.
- Low body temperature. If your baby’s temperature falls below 96.8 F (36 C), call the doctor.
- Changes in how they cry. Their cry could be weak, sound strange, or be frantic without stopping.
- Weak sucking or not being able to suck for very long
- Sweating while they eat
- Sleeping more than normal (needing to be woken up to eat, for example)
- Decreased muscle tone or floppy limbs.
- Moaning or grunting noises when they breathe.
- Decreased urination (fewer wet diapers) and dry mouth (dehydration).
- Any change in color, such as pale, bluish, or gray arms and legs
It can be hard to tell if your newborn is sick.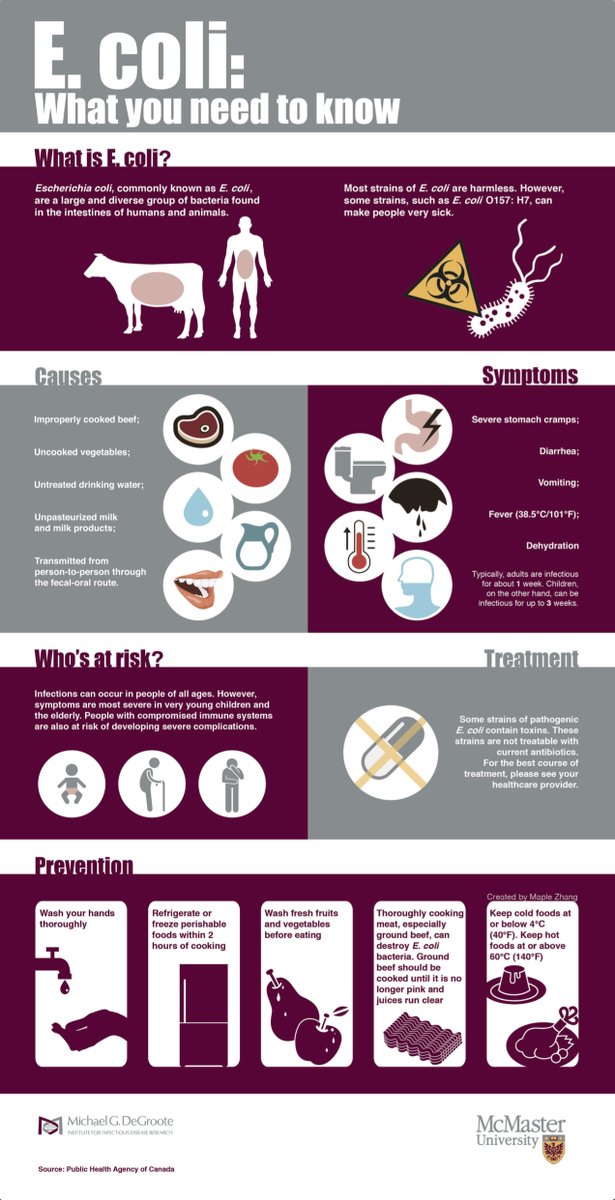 Pay attention and watch them closely for any of these signs of illness. If you have any question at all about your newborn, call their doctor.
Pay attention and watch them closely for any of these signs of illness. If you have any question at all about your newborn, call their doctor.
Things to consider
While illness is not normal for a newborn, there are some conditions that are common in the first few weeks after birth. Watch your newborn for signs of any of these conditions and call their doctor if you see symptoms.
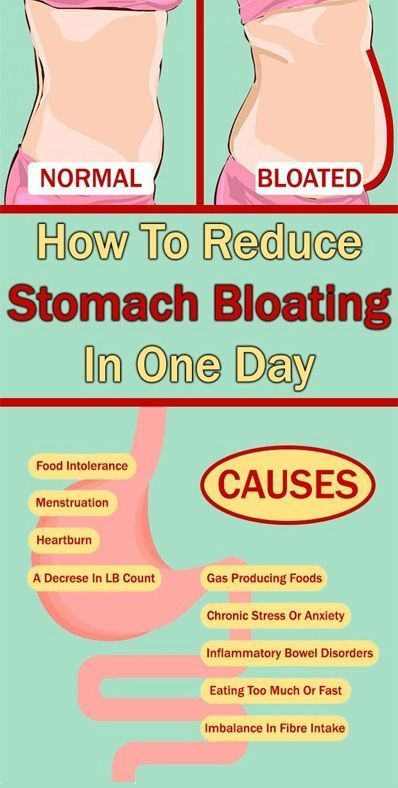
Abdominal distension. Your baby’s abdomen (stomach) should feel soft between feedings. If it feels swollen or hard, there could be a problem. It might be gas or constipation. But if they haven’t had a bowel movement for more than a day or two, or if they are vomiting, a swollen stomach could be a sign of an intestinal problem.
Blue baby. Your newborn may show mildly blue hands and feet if they are cold. They may go a little blue around the face, tongue, or lips if they are crying hard. But if they have persistent blue coloring plus breathing or feeding difficulties, it is an emergency. It could be a sign that the heart or lungs are not working correctly. Call the doctor or go to the emergency room right away.
It could be a sign that the heart or lungs are not working correctly. Call the doctor or go to the emergency room right away.
Coughing during feeding. Your newborn may cough or sputter a bit as they learn and adjust to a feeding routine. But if they cough or gag regularly when they are trying to eat, there could be a problem in the lungs or digestive system.
Excessive crying. Newborns cry, sometimes for no reason. If your baby won’t stop crying, make sure they are fed, burped, warm, and have a clean diaper. Then try to hold them and soothe them. You can’t “spoil” a newborn with too much attention, so don’t hesitate to pick them up when they are crying. Soon you’ll get used to your newborn’s crying patterns. But if their crying sounds different, such as shrieking, or it goes on for an unusually long time, call your doctor.
Jaundice. Many healthy newborns have a yellowish tinge to their skin. This is called jaundice. It happens when a chemical called bilirubin builds up in the baby’s blood. Mild cases of jaundice are harmless. But if the buildup gets to be too much and it isn’t treated, it can cause problems. Jaundice normally appears on the face first, followed by the chest and abdomen, and finally it spreads to the arms and legs. Sometimes the whites of the eyes can become yellowish, as well. If you notice your baby developing jaundice, call the doctor.
Mild cases of jaundice are harmless. But if the buildup gets to be too much and it isn’t treated, it can cause problems. Jaundice normally appears on the face first, followed by the chest and abdomen, and finally it spreads to the arms and legs. Sometimes the whites of the eyes can become yellowish, as well. If you notice your baby developing jaundice, call the doctor.
Respiratory distress. In most cases, if your newborn is having trouble breathing, it’s because their nasal passages are blocked. This is normally easy to remedy by using saline nasal drops and a bulb syringe to suck the mucus out. But there are other signs that could mean your baby is having serious breathing problems. These include
- Fast breathing (more than 60 breaths in one minute). Remember, though, that babies breathe faster than adults.
- This is when the stomach muscles between the ribs get sucked in with each breath, making the ribs stick out.
- Flaring of the nose.
- Grunting while breathing.

- Persistent blue coloring.
Call your newborn’s doctor right away if he or she develops any of these signs of respiratory distress.
Questions to ask your doctor
- What signs should I look for that my newborn may be sick?
- How do I know what’s normal when I just brought him or her home?
- How do I know if my baby is vomiting or just spitting up?
- My baby cries all the time. Could they have colic?
Resources
National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development: What are some of the basics of infant health?
National Institutes of Health, MedlinePlus: Common Infant and Newborn Problems
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone. Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Children's infections - types, descriptions, differences and features
However, this limitation does not give any guarantee that the disease will not occur in adulthood. Modern medicine recommends following mandatory vaccinations, although many parents still refuse to give them to their children. What childhood infections are known, and how do they threaten young patients?
All childhood infectious diseases are transmitted through contact with a sick patient by airborne droplets or household contact. In some cases, the child may not become infected because the antibodies were passed on from the mother. Childhood infections include:
- Scarlet fever.
- Rubella.
- Measles.
- Chicken pox.
- Poliomyelitis.
- Whooping cough.
- Viral mumps (mumps).
Diseases such as acute respiratory infections, intestinal infections, meningitis, mononucleosis are also often recorded in childhood. But they are often found in adults, so it is inappropriate to classify them as childhood infections.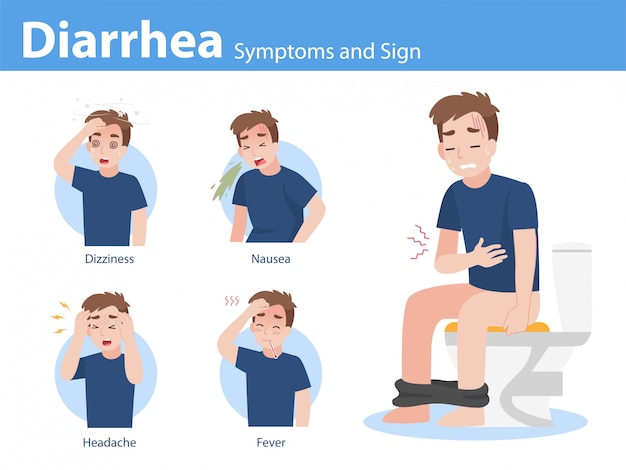
Measles
Measles is a highly contagious infection. The infectious agent spreads with air flow, while it does not quickly die in the external environment. The incubation period averages 20 days. The initial symptoms are very similar to the common cold, and around the 4th day a rash appears that spreads throughout the body. Even on the mucous membranes in the mouth, small-dotted formations are observed.
Measles fever persists until the rash disappears. But it is important to understand that this is a very serious disease for the child’s immune system, therefore, after measles, bronchitis, otitis media and even pneumonia are often observed.
Viral parotitis
Infection is spread by airborne droplets. The incubation period lasts from 7 to 20 days. The first symptoms include the appearance of headaches, which is not surprising, since with this disease the nervous system suffers, and the temperature is kept high up to 39 degrees. The infection also affects the pancreas, and in boys the testicles, so often after the disease in adulthood, male infertility is diagnosed.
The disease is very serious, it can be complicated by meningitis, so it is important not to refuse vaccination and consult a doctor at the first sign of the disease.
Scarlet fever
The infection has a streptococcal nature, is characterized by high contagiousness, and the virtual absence of an incubation period. The child develops a sore throat, vomiting, fever, and a punctate rash is localized mainly on the abdomen, cheeks, armpits, and groin.
Diphtheria
The causative agent of the disease is diphtheria bacillus, and the child is infected by its negative effect on the tonsils. Symptoms appear on average 10 days after infection, the main of which is considered to be a gray coating on the tonsils - it distinguishes the disease from a sore throat. Diphtheria is dangerous for the life of a child, so you should not refuse DTP vaccination, because it was she who turned this disease into a rare infection.
Varicella
Very easily transmitted, incubation period 7 to 21 days. The disease is treated easily, and it is characterized by a blistering rash. Chickenpox is carried by almost everyone.
The disease is treated easily, and it is characterized by a blistering rash. Chickenpox is carried by almost everyone.
Poliomyelitis
This is a viral infection with an incubation period of up to 30 days, although in fact it is much shorter. The symptoms of infection can be called classic for a viral infection, but there is still one difference - pain in the limbs. To prevent infection, you need to be vaccinated.
Rubella
Infection has many similarities with measles - the same rash and fever. But there is one difference - with rubella, the lymph nodes become inflamed, but it is much easier to tolerate, and the rash goes away earlier.
Infectious diseases should only be treated by a physician. Considering that many childhood infections have common features, and the onset of the disease is almost always the same, one cannot do without a specialist. Self-medication of children can lead to undesirable or negative consequences, as well as the choice of a poor-quality doctor. That is why you should use the services of only qualified professionals with experience.
That is why you should use the services of only qualified professionals with experience.
Ask a question to a specialist
Your e-mail *
Question
* — mandatory fields
Top
Make an appointment
Phone *
Your e-mail *
City *
Select the city Borisov Zhodino
Specialist *
Comment
* - 9003 required fields
Write a review:
Your name*
E-mail*
Phone*
Request a call back
Do you want us to call you back within 15 minutes?
Telephone *
Call from which branch? *
-- Select city --Borisov Zhodino
* — mandatory fields
Make an appointment
Phone *
Your e-mail
City *
-- Select city --Borisov Zhodino
Specialist *
CARDIOLOGY
0003
Make an appointment
Phone *
Your e-mail
City *
-- Select the city --Borisov Zhodino
Specialist *
Ultrasound diagnostics
Comments
mandatory fields - * mandatory fieldsMake an appointment
Phone *
City *
-- Select city --Borisov Zhodino
Specialist *
Gynecologist
Comment
* — mandatory fields
Sign up for reception
Phone *
Your e-mail
City *
-Select the city-Borisjodino
Specialist *
Dermatology
Comment
*-Fields Mandatory
Make an appointment
Phone *
City *
-- Select city -- Borisov Zhodino
Specialist *
Mammologist
Comment
* — mandatory fields
Make an appointment
Phone *
City *
-- Select city -- Zhodino
Specialist *
Neurologist
Comment
Make an appointment
Phone *
City *
-- Select city -- Borisov Zhodino
Specialist *
ONCODERMATOLOGY
Comment
* — mandatory fields
Sign up for reception
Phone *
Your e-mail
City *
-Select a city-Borizjodino
Specialist *
otorinolaryngologist (ENT)
Comment
*-Fields Mandatory for filling out
Make an appointment
Phone *
Your e-mail
City *
-- Select a city --Borisov Zhodino
Specialist *
PROCTOLOGY
Comment
* — mandatory fields
Make an appointment
Phone *
Your e-mail
City *
-- Select city --Borisov Zhodino
Specialist *
Therapist
Comment
required fields - * fields are requiredMake an appointment
Phone *
Your e-mail
City *
-- Select city --Borisov Zhodino
Specialist *
Urologist
Comment
* - required fields
Sign up for reception
Phone *
Your e-mail
City *
-Select the city-Borisjodino
Specialist *
Functional diagnostics
Comment
*-Pauls Mandatory to fill out
Make an appointment
Phone *
Your e-mail
City *
-- Select city --Borisov Zhodino
Specialist *
Endocrinologist
Comment
required fields - * mandatory fields -Make an appointment
Phone *
Your e-mail
City *
-- Select city -- Borisov Zhodino
Program *
“I'm healthy! VIP»
Comment
* — mandatory fields
Make an appointment
Phone *
Your e-mail
City *
-- Choose a city - Borisov Zhodino
Program *
"I want to become a mother!"
Comment
* — mandatory fields
Make an appointment
Phone *
City *
-- Select city --Borisov Zhodino
Program *
"Women's Health"
Comment
* - mandatory fields
Sign up for the reception
Phone *
Your e-mail
City *
-Select the city-Borizjodino
Program *
“Male Health”
Comment
*-Fields Mandatory
Make an appointment
Phone *
City *
-- Select city -- Borisov Zhodino
Program *
"From A to Z"
Commentary
* - mandatory fields
Scarlet fever: symptoms, diagnosis and treatment
Attention!
This information is for parents.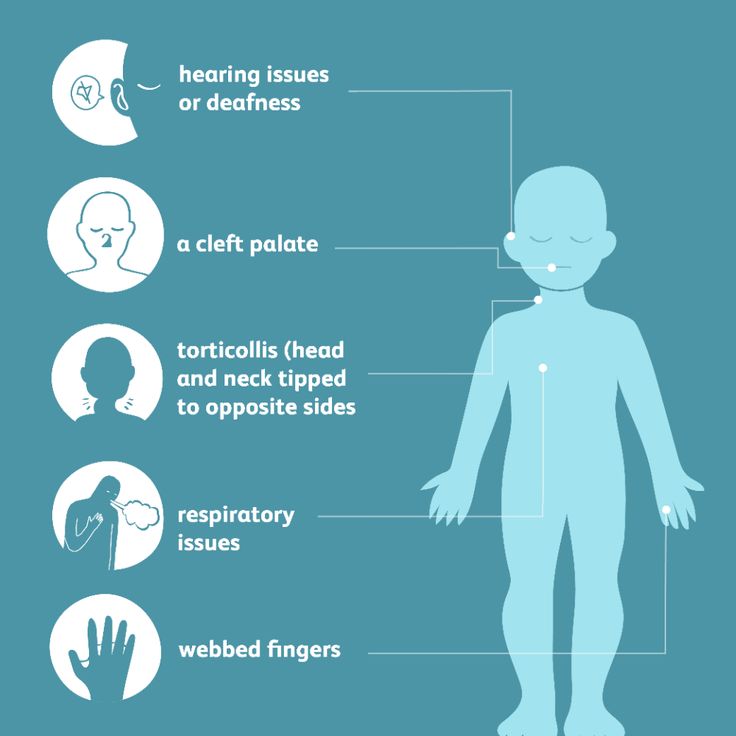 It will allow you to identify the symptoms of scarlet fever in time and take the child to the doctor in a timely manner.
It will allow you to identify the symptoms of scarlet fever in time and take the child to the doctor in a timely manner.
Contents
- What is scarlet fever
- Causes of scarlet fever
- Modes of infection
- Symptoms
- Diagnostics
- Treatment
- Diet for scarlet fever
- Complications
- Prophylaxis
- Which doctor to contact
Scarlet fever is now considered a separate infectious disease. But, until the 16th century, it was not distinguished from other rash diseases. In 1556, the Italian physician Ingrassias was the first to separate the signs of scarlet fever from those of measles. He called the new disease scarlet fever (from the word scarlatto - crimson from the Italian language).
A century later, the English doctor Thomas Sydenham fully described the clinical picture of the disease. In the pre-bacteriological era, ideas about scarlet fever were based on miasmatic theory. It was considered the result of exposure to the body of sewage. In the 40s of the 20th century, in the works of the spouses Dick and V.I. Ioffe proved the streptococcal etiology of the disease.
It was considered the result of exposure to the body of sewage. In the 40s of the 20th century, in the works of the spouses Dick and V.I. Ioffe proved the streptococcal etiology of the disease.
Description
Scarlet fever is an acute infectious pathology. Causes the disease beta-hemolytic streptococcus type A. It is transmitted from the patient by airborne droplets and contact. It is characterized by an increase in body temperature, the appearance of rashes on the skin, sore throat. The oropharynx is predominantly affected by the causative agent of the disease, a characteristic exanthema appears, inflammation is accompanied by severe intoxication.
Scarlet fever is manifested by a characteristic symptom complex, including general intoxication, fever, scarlet fever. Patients have a crimson tongue, an increase in regional lymph nodes. On the skin, a small punctate rash with fine scaly peeling is visible. The patient has a characteristic exanthema.
The disease mainly affects children under ten years of age. In schoolchildren and adults who have crossed this age line, susceptibility to infection with streptococcus decreases. This is associated with the maturation of the immune system. It quickly gives a specific reaction in response to the introduction of the pathogen, but this does not completely exclude the possibility of the disease.
In schoolchildren and adults who have crossed this age line, susceptibility to infection with streptococcus decreases. This is associated with the maturation of the immune system. It quickly gives a specific reaction in response to the introduction of the pathogen, but this does not completely exclude the possibility of the disease.
Scarlet fever is more common among children between the ages of three and ten. This is associated with the imperfection of the immune system and being in children's institutions, in which infection often occurs.
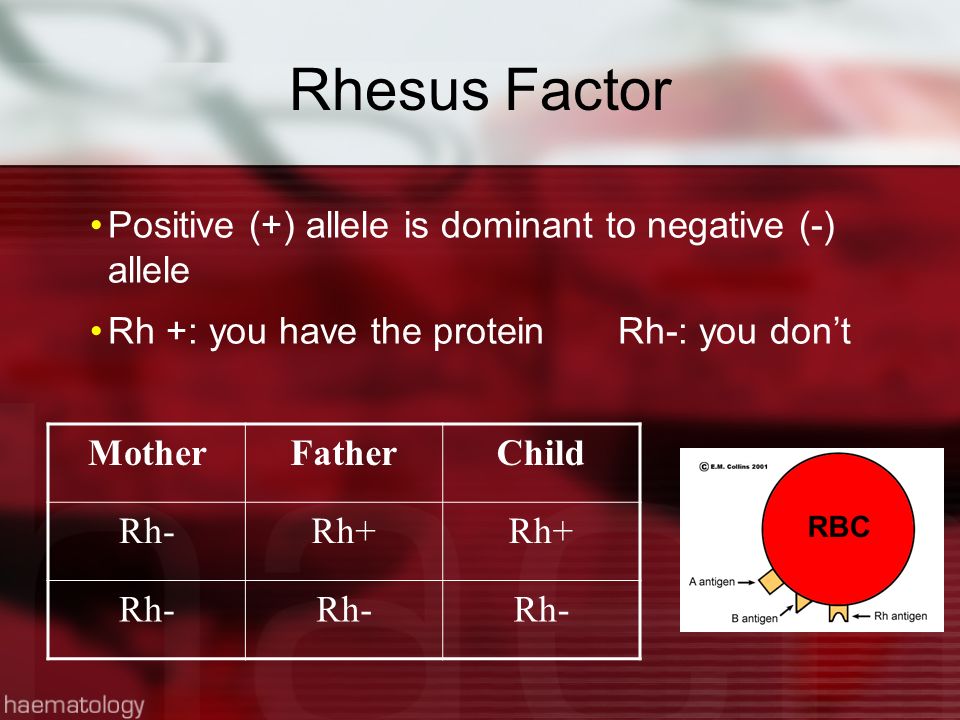
In newborns and toddlers in the first year of life, scarlet fever is diagnosed very rarely. This is associated with the presence in the bloodstream of maternal immune cells that got there through the placenta.
Causes of scarlet fever
Causes scarlet fever in adults and children - beta-hemolytic streptococcus type A. It belongs to the genus of facultative aerobic, gram-positive bacteria Streptococcus, which have an ovoid shape.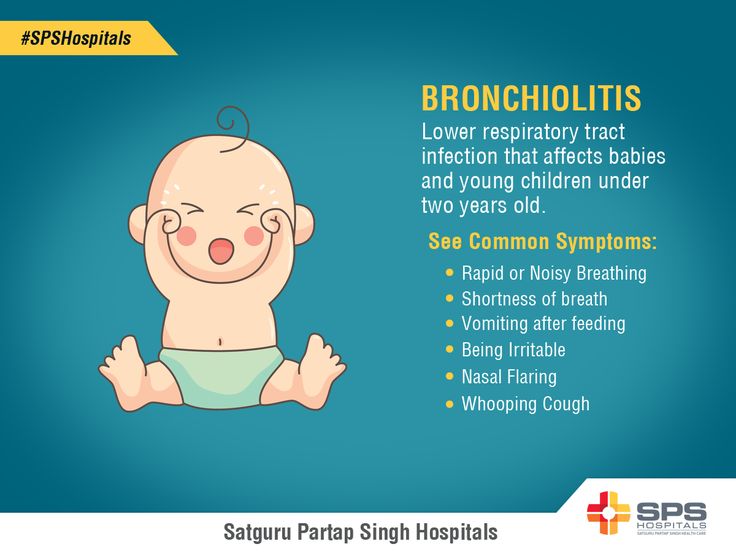
Its source is a carrier of a pathogenic bacterium or a patient with this disease. Especially such people are contagious at the beginning of the disease. The risk of transmitting the pathogen to other people completely disappears after three weeks from the onset of symptoms.
According to experts, up to 20% of the population are considered asymptomatic carriers of the scarlet fever pathogen. In rare cases, a person is a source of infection for several years.
The natural susceptibility of the human body to the bacterium Streptococcus pyogenes remains at a high level throughout life in most people. The immunity that is formed in people who have had scarlet fever is type-specific.
The bacterium secretes erythrogenic toxin, the person has no antitoxic immunity. This means that the risk of infection with other types of streptococcus is high. The maximum incidence of scarlet fever in children and adults occurs in autumn and winter.
How does infection occur?
Infected with streptococcus by airborne droplets and household way.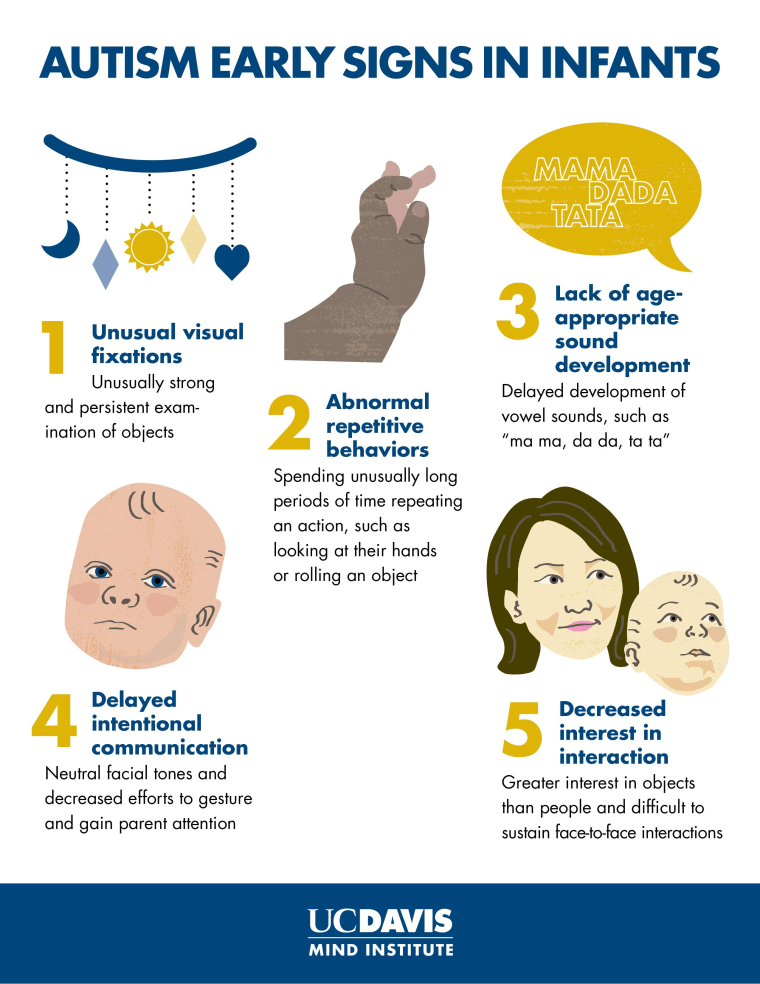 Experts consider the spread of the pathogen through the air along with drops of saliva of an infected person to be the main way of infection. Healthy people inhale an aerosol containing microorganisms. Infected saliva by an infected person is scattered over a distance of up to one and a half meters.
Experts consider the spread of the pathogen through the air along with drops of saliva of an infected person to be the main way of infection. Healthy people inhale an aerosol containing microorganisms. Infected saliva by an infected person is scattered over a distance of up to one and a half meters.
The patient releases a large amount of the pathogen when coughing, sneezing, talking into the environment. If these bacteria get on food, an alimentary mode of transmission is possible. More often, people who are close to the source of infection become infected with scarlet fever.
The entrance gate for the penetration of the pathogen into the body is the mucous membrane of the nasopharynx, pharynx, less often the genitals. Sometimes the pathogen enters the body through damaged skin. In the zone of introduction of bacteria, a local infectious focus appears with typical necrotic manifestations.
Microorganisms multiply in it and release toxins into the blood, which contribute to the development of intoxication. The presence of this toxic substance in the bloodstream causes capillary dilation. On the skin, this is manifested by the formation of a specific rash.
The presence of this toxic substance in the bloodstream causes capillary dilation. On the skin, this is manifested by the formation of a specific rash.
Gradually, the body develops antitoxic immunity, which helps to subside intoxication. Therefore, the rash disappears over time. Sometimes the pathogens themselves enter the bloodstream. This leads to damage to other organs and tissues, these include:
- lymph nodes;
- meninges;
- temporal bone tissue;
- hearing aid and others.
Purulent-necrotic inflammation develops in them.
Symptoms of scarlet fever in children and adults
The incubation period for scarlet fever lasts from one to twelve days. The disease begins acutely. First, the patient has a fever. Then signs of intoxication appear:
- muscle pain;
- increased heart rate;
- weakness;
- headache.
Fever accompanies drowsiness and apathy. Perhaps the onset of euphoria, increased mobility. Intoxication in most patients often causes vomiting. Other symptoms of scarlet fever include:
Intoxication in most patients often causes vomiting. Other symptoms of scarlet fever include:
- Sore throat. Reveal redness and tonsils, arches of the tongue, soft palate and posterior pharyngeal wall. Sometimes follicular-lacunar tonsillitis is formed. The mucosa is covered with a purulent, fibrous, necrotic coating.
- Regional lymphadenitis. Lymph nodes become dense and painful.
- Raspberry tongue. By the fifth day of illness, the tongue becomes bright crimson. Removes plaque from the surface. Reveal hypertrophy of the papillae. Lips are also painted in crimson color. This symptom occurs in adults with a severe form of the disease.
- Spotted rash. It is formed for the first time days of illness. Dots of dark shades appear on the skin of the face, as well as the upper part of the body. Then later they appear on the flexor surfaces of the upper limbs, sides and inner surface of the legs. Dark red stripes form in the folds of the skin. Sometimes the elements of the rash merge into erythema.
- Minor hemorrhages. They arise due to fragile vessels that are easily damaged by squeezing and rubbing the affected skin.
There are no rashes in the nasolabial triangle in scarlet fever (Filatov's symptom). In this area, the skin usually turns pale.
By the fifth day, the symptoms of the disease subside. The rash first turns pale, and by the ninth day it disappears completely. After these rashes, fine scaly peeling remains on the skin, and coarse scaly peeling is detected on the feet and palms. In adults, scarlet fever is asymptomatic. The patient notices a pale, rapidly passing rash and a slight catarrhal inflammation of the throat.
Diagnosis of scarlet fever
Scarlet fever is characterized by a high degree of symptom specificity. This allows you to set the correct diagnosis already during the interview and examination of the patient. To confirm it, the following methods are used:
- general clinical blood test - reveals signs of this infection: neutrophilic leukocytosis, elevated ESR, leukocyte formula shifts to the left;
- ECG and ultrasound of the heart are performed for suspected cardiovascular complications;
- express diagnosis of RCA - it is done as a specific test;
- otoscopy is performed, if there is a suspicion of otitis, it is performed by an otolaryngologist during examination.
If a lesion of the urinary system is suspected, its condition is assessed using an ultrasound of the kidneys.
Treatment of scarlet fever
With this pathology, it is strictly forbidden to self-medicate, you must consult a doctor.
The basis of the treatment of scarlet fever is the correct and timely administration of antibacterial drugs. Preference is given to synthetic analogues of penicillin or macrolide antibiotics. In severe cases, cephalosporins are prescribed. To alleviate the patient's condition, detoxification therapy is carried out.
In a severe and moderate condition of the patient, intravenous administration of drugs is indicated. In the absence of indications for hospitalization at home, an adequate drinking regimen is organized for the child. The volume of fluid is determined by the attending physician, taking into account the age of the baby. Streptococcus produces a lot of toxins, so the patient is prescribed antiallergic drugs.
Non-steroidal anti-inflammatory drugs are given at high temperature. For small hemorrhages, agents that strengthen the vascular wall are recommended. To alleviate the manifestations of angina, antiseptic solutions are locally prescribed. For the same purpose, tube quartz is recommended.
Diet for scarlet fever
During the treatment of scarlet fever, the patient is prescribed a diet aimed at activating the defenses. Products should be easy to digest. Patients are recommended dietary table number 13. Food should be fractional up to five times a day. The following foods are not recommended for scarlet fever:
- muffin;
- fresh bread;
- fatty broths;
- fatty meats;
- canned food;
- sausages;
- salted fish;
- raw vegetables high in coarse fiber;
- smoked products;
- legumes;
- whole milk and cream;
- fatty sour cream;
- hard cheeses;
- barley groats, millet, barley;
- chocolate;
- confectionery.

In the absence of kidney disease, you can drink up to 2.5 liters per day.
Complications of scarlet fever
Most cases of the disease have a favorable outcome. In severe course of the disease, the following complications develop:
- otitis media;
- lymphadenitis;
- inflammation of the skin;
- severe allergization;
- carditis;
- arthritis;
- jade.
Late complications of the disease are possible. These include:
- synovitis;
- heart valve disease;
- glomerulonephritis;
- rheumatism;
- Sydenham's chorea.
These complications occur several weeks after recovery.
Prevention of scarlet fever
There are no vaccinations against this disease. Non-specific prevention measures consist in isolating infected people. Carry out quarantine measures in children's institutions. Patients with scarlet fever are discharged only ten days after the day of hospitalization.