Infant runny eye
Baby Watering Eyes Causes and Treatments
If you discover that your child has watery eyes, it could be due to several reasons. This symptom, called epiphora, can be caused by blocked tear ducts, infections, and allergies.
The different causes of watery eyes in babies and toddlers require different treatments. Some require minimal action on the part of the parents, while other treatments include prescription medications or even surgery.
You should always see your child’s pediatrician if you’re concerned about your child’s watery eyes.
Watery eyes can be a symptom of numerous medical conditions. A likely cause of watery eyes in infants can be blocked tear ducts. These often resolve on their own.
Other causes of watery eyes in infants and toddlers include infections like conjunctivitis (pink eye) or even the common cold. Your child may even experience watery eyes from irritants or hay fever.
Blocked tear duct
Your baby may have a blocked tear duct causing watery eyes. This condition is quite common in infants, with one-third of them having the condition.
Blocked tear ducts occur when tears cannot move from the corners of the eyelids into the ducts lining your nose. This causes tears to back up in the eye. Many infants experience this because the end of the tear duct’s membrane does not open, or because the opening is too narrow at birth. The condition resolves itself in 90 percent of infants by their first birthday.
Other causes of blocked tear ducts are less common but include:
- nasal polyps
- cyst or tumor
- trauma to the eye
You may see symptoms of a blocked tear duct right after birth or within the first few months of your child’s life.
Other symptoms of a blocked tear duct include:
- pus in the eye
- crusting eyelids and eyelashes
Your child may experience an infection related to a blocked tear duct. Symptoms of the infection, called dacryocystitis, include:
- redness in the inner corner of the eye
- bump at the side of the nose that is tender or swollen
It’s important to visit a pediatrician if you suspect this condition in your infant.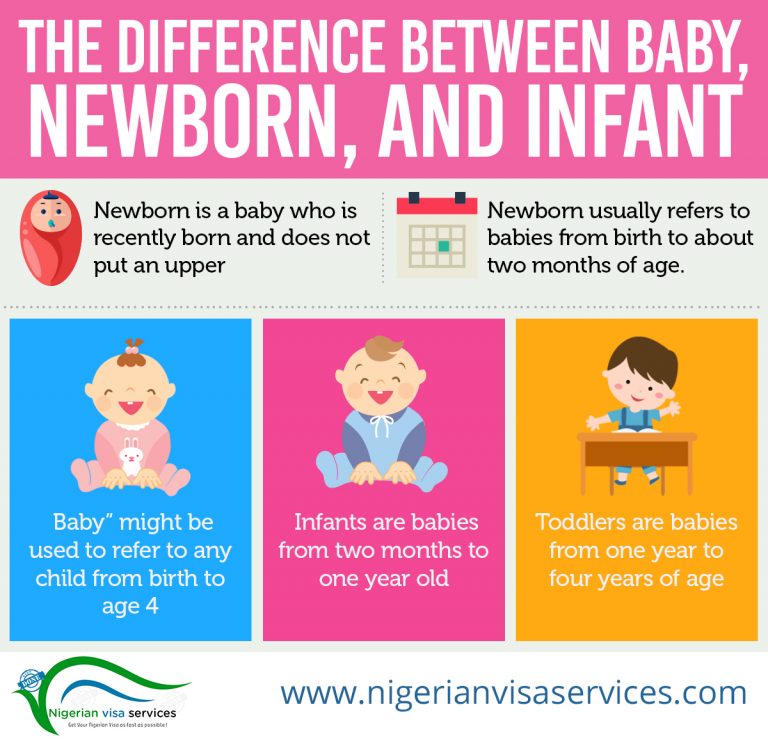 The symptoms associated with a blocked tear duct may rarely actually be symptoms of childhood glaucoma.
The symptoms associated with a blocked tear duct may rarely actually be symptoms of childhood glaucoma.
Common cold
Your child’s watery eyes can also be a symptom of a common cold.
Children are more susceptible to colds than adults because they’ve not built up immunity and often touch their eyes, nose, and mouth, causing more germs to spread. Your child may develop watery eyes along with other cold symptoms like a stuffed or runny nose and sneezing.
Infections
Your infant’s watery eyes may also be caused by an infection.
Conjunctivitis, also known as pink eye, may be causing the watery eyes. This can occur in children at any time. Pink eye occurs when a virus or, less commonly, bacteria get into the eye. Conjunctivitis can also be caused by irritation.
Symptoms of pink eye include:
- red eyes
- swollen eyes
- discharge of pus from the eye
Newborns are particularly at risk if they develop pink eye and it goes untreated for too long. A mother can pass on an infection to her newborn during childbirth, such as chlamydia or gonorrhea, even if she doesn’t have symptoms.
A mother can pass on an infection to her newborn during childbirth, such as chlamydia or gonorrhea, even if she doesn’t have symptoms.
If your newborn shows signs of pink eye, see a doctor immediately. The doctor will look for swelling, redness, and dilated blood vessels.
Allergies
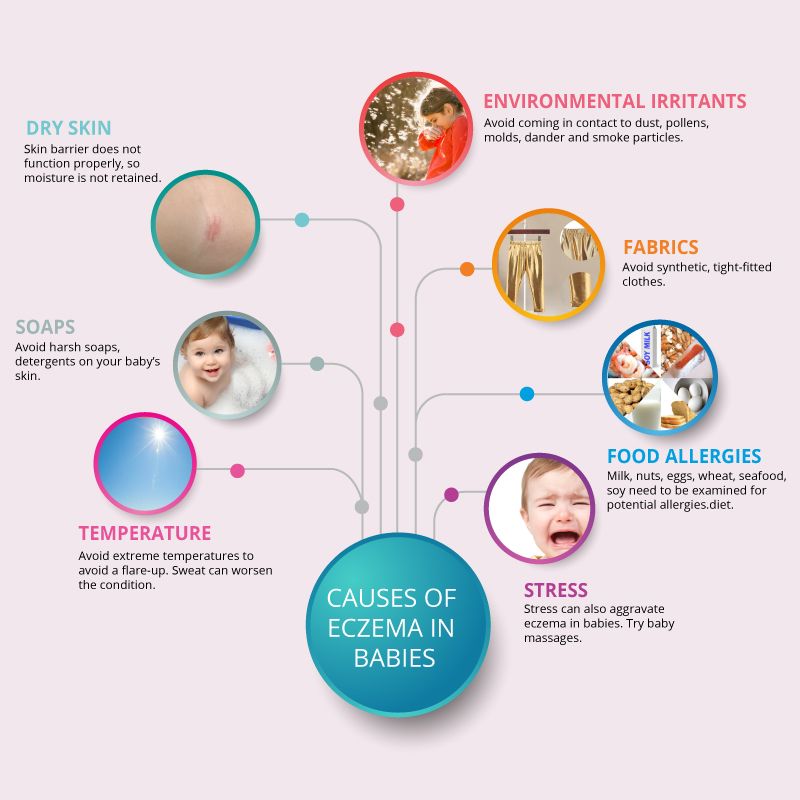
Watery, red eyes may be a symptom of allergic conjunctivitis. Irritants like pollen, dust, and smoke can cause an allergic reaction in the eye.
Hay fever, known as allergic rhinitis, may also cause watery eyes. Other symptoms for this condition include:
- runny and/or itchy nose
- sneezing
- nasal congestion and postnasal drip
- congestion
- ear canal pressure or pain
Toddlers may experience watery eyes for many of the same reasons as infants. An unresolved blocked tear duct from infancy or an infection or allergies may be causing the symptom.
Toddlers are also more likely than older children and adults to develop frequent colds, which may cause watery eyes.
The treatment for watery eyes in infants and toddlers will vary. Often, you don’t need to do much to treat the watery eyes and the symptom will clear up on its own.
In other cases, you may need a prescription to clear up an infection. Or your child may need to have surgery to resolve a long-lasting blocked tear duct.
Home remedies
You may consider home remedies if a doctor recommends them or if your child’s watery eyes look white in color and not irritated.
Blocked tear ducts can resolve on their own, but your doctor may recommend massaging the tear duct to help it open. You can massage the outside of your child’s nose (from the eye to the corner of the nose) with a clean index finger. Apply firm pressure during the massage.
You may also find that gently pressing a warm cloth to the eye also helps clean the eye and provides comfort to your child.
For older children, watery eyes caused by colds or hay fever may be minimized with over-the-counter cold and allergy medications recommended by a doctor.
Medical treatment
Your child’s watery eyes may require medical treatment if they’re infected or if the tearing persists.
Blocked tear ducts can get infected at times and may require an antibiotic to treat. These can be administered topically with an ointment or eye drop, orally, or even in some cases intravenously at the hospital.
Conjunctivitis caused by bacteria may also require antibiotics to clear the condition out of your child’s eye. A pediatrician may recommend rinsing the eye with saline to clear out buildup in the eye.
If your child’s blocked tear duct does not resolve itself, your child may need a greater level of medical care. A doctor may recommend nasolacrimal duct probing. This involves the doctor inserting a small probe through your child’s tear duct into their nose to widen the passage. A doctor may be able to do this with a local anesthetic for your child, or it may require general anesthesia.
If the probing procedure does not help the blocked tear duct, your child may need another procedure. There are varying types of procedures. Many have low complication rates and do not require overnight hospitalization.
There are varying types of procedures. Many have low complication rates and do not require overnight hospitalization.
See a pediatrician right away if your newborn develops watery eyes, as they may be a sign of a more serious condition, like pink eye. Newborn pink eye caused by a bacterial infection needs to be treated within 24 hours of symptoms.
You should also see a doctor if the following symptoms accompany your child’s watery eyes:
- inflammation
- redness
- discharge that is yellow or green in color
- pain
- changes in eye or eyelid structure
- sensitivity to light
- itching (your child may rub their eyes often)
Several conditions can cause watery eyes in infants and children. Some like blocked tear ducts or a viral infection may resolve on their own with time. Other causes may require more immediate medical treatment.
You should talk to your child’s doctor to diagnose the condition and begin appropriate treatment if your child’s watery eyes are accompanied by other symptoms, or if you’re concerned.
Sticky eye | Pregnancy Birth and Baby
Sticky eye | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is sticky eye?
If your baby's eye is very watery and there is some discharge, it's probably a blocked tear duct. This is also known as 'sticky eye'. This condition usually gets better by itself, but it's still wise to check with your doctor. There are things you can do to help it get better and avoid infection.
What causes sticky eye?
Glands inside the upper eyelids produce tears. The tears flow over the surface of the eye. They drain away through small openings in the inside corner of the upper and lower eyelids. The tears then flow through the tear duct to the nose.
About 1 in 20 babies is born with tear ducts that are too narrow or blocked completely. Sometimes the tear duct (tube) is blocked by a plug of mucus or cells that developed before the baby was born. This means their tears can't drain away and their eyes are wet all the time.
Sometimes the tear duct (tube) is blocked by a plug of mucus or cells that developed before the baby was born. This means their tears can't drain away and their eyes are wet all the time.
Is it sticky eye?
If your baby has sticky eye, their eye or eyes will water a lot. They may have tears running down their cheeks. Sometimes there may be swelling and a sticky yellow or green discharge. Sticky eye is not an infection and should not cause your child pain.
Other symptoms may mean the eye is infected, such as red, swollen, or sore eyes. Your baby may also have a fever or be fussier than usual.
Eye infections include conjunctivitis and dacryocystitis. You should always see your doctor if you think your baby has an eye infection.
You should also see your doctor if:
- your baby seems sensitive to light
- they have large amounts of eye discharge
- they are constantly squeezing their eyes shut
- the side of their nose seems swollen, red, and painful
- the tear duct is still blocked by the time they reach 1 year of age
How is sticky eye treated?
Sticky eye normally clears up by the time your baby is 12 months. If there is any sign of infection, your doctor might give your baby some antibiotic eye drops or ointment.
If there is any sign of infection, your doctor might give your baby some antibiotic eye drops or ointment.
Some babies will need surgery if the blocked tear duct doesn't improve. This is done with a general anaesthetic, so the doctor can open the tear duct with a probe.
How do I manage my baby’s sticky eye?
There are ways for you to help manage and treat your baby’s sticky eye.
To help the blocked tear duct, your doctor may teach you a special massage.
If your baby has sticky eye, it is important to keep their eyes clean. This will help prevent infection.
Wash the affected eye or eyes as needed, following the directions below:
- Wash your hands thoroughly with soap and water.
- Pat the eye dry with a clean (or disposable) towel.
- Gently wipe each eye with a disposable cotton swab soaked in water or a weak saline solution, making sure to wipe from the inside corner of the eye to the outside corner.
- Do not touch the eye itself or clean inside the eyelid because you may damage the eye.

- Use a new cotton swab for each eye.
- Wash your hands again.
You can make saline solution by dissolving:
- 1 teaspoon of salt
- 1 cup (250ml) of boiling water
Make sure that the solution has cooled to room temperature before using.
There is also evidence to support using breastmilk to clean your baby's eye. This will not cause any harm to your baby.
If you see signs of an infection, you should see your doctor.
Sources:
Children's Health Queensland Hospital and Health Service (Blocked tear duct (nasolacrimal duct obstruction)), Royal Australian College of General Practitioners (RACGP) (Acute red eye in children), The Royal Hospital for Women (Sticky eye care for a neonate), Perth Children’s Hospital (Blocked tear duct (Nasolacrimal duct obstruction)), International Ophthalmology (The natural process of congenital nasolacrimal duct obstruction and effect of lacrimal sac massage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Conjunctivitis
- Cleaning your baby's ears, eyes and nose
Need more information?
Conjunctivitis | SA Health
Conjunctivitis is an inflammation of the lining of the eye and eyelid caused by bacteria, viruses, chemicals or allergies.
Read more on SA Health website
Conjunctivitis
Conjunctivitis is an inflammation of the surface of the eye. It is very common in young children and it can be highly contagious. Learn more here.
Read more on Pregnancy, Birth & Baby website
Pollen - a trigger for hay fever - National Asthma Council Australia
Plant pollen is well known as a trigger for seasonal allergic rhinitis (hay fever) and seasonal allergic conjunctivitis.
Read more on National Asthma Council Australia website
Conjunctivitis in babies, children & teens | Raising Children Network
Conjunctivitis is a type of eye infection. It’s very common and can be very contagious. Your child needs to see a GP for the right conjunctivitis treatment.
Read more on raisingchildren.net.au website
Other Allergic Conditions - Allergy & Anaphylaxis Australia
Other Allergic Conditions included: Urticaria (Hives), Eczema (Atopic Dermatitis), Allergic Conjunctivitis, Allergic Rhinitis (hayfever), Sinusitis
Read more on Allergy and Anaphylaxis Australia website
Conjunctivitis - MyDr.com.
 au
au Conjunctivitis is an inflammation of the eye's conjunctiva and may be contagious. Treatment depends on the cause.
Read more on myDr website
Conjunctivitis: self-care - MyDr.com.au
A major cause of eye problems is allergic, bacterial or viral conjunctivitis (inflammation of the 'wet' surfaces of the eye). Find out what products are available for conjunctivitis.
Read more on myDr website
Allergic conjunctivitis - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Allergic conjunctivitis usually causes mild to moderate symptoms, including redness, which respond to non medicated treatment. However, sometimes symptoms can be extremely severe and debilitating with swelling of the eyelids and conjunctivae and a sensation of grittiness and burning.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Conjunctivitis - Better Health Channel
Conjunctivitis is an eye infection caused by a bacteria or virus. Symptoms include eye redness, a discharge and swollen lids. Conjunctivitis is treated with antibacterial eye drops or ointment. Children must not attend school or child care if they have conjunctivitis.
Read more on Better Health Channel website
Blocked tear duct: babies & toddlers | Raising Children Network
Many babies get a blocked tear duct. Symptoms include watering eyes and discharge. Blocked tear ducts mostly fix themselves, but it’s good to see a GP.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Physiological runny nose in a newborn — Medical Center "Healer"
When it comes to a runny nose in a baby, one must understand that this is primarily a physiological process. A newborn baby, as soon as it is born, begins to breathe on its own. In the womb, babies breathe in a completely different way, they have a nose, lungs did not develop, but they received oxygen in a completely different way, through the umbilical cord. And now, having been born into the world, the baby begins to get used to the environment on its own.
Features
Normally, a baby's runny nose lasts 10-12 weeks. During this period of adaptation, the child naturally develops more mucus in the nose. There is nothing pathological in this. Such transparent mucus in the nose absolutely does not prevent the baby from living an independent life, does not prevent him from eating on his own.
There is nothing pathological in this. Such transparent mucus in the nose absolutely does not prevent the baby from living an independent life, does not prevent him from eating on his own.
We are very fond of young mothers because of their inexperience to resort to various aspiratory devices for pumping mucus out of their child's nose. They think they help him in some way. The child already has narrow, swollen nasal passages, and we still climb there with an aspirator and try to get the mucus out of there. Thus, we only injure the mucous surface.
If your baby has a runny nose because he is too cold, you can simply warm him up. And this runny nose will soon pass. Physiological rhinitis does not go away so quickly. And so the child must be helped. Usually we like to have the child lie down all the time. We walk with him in a stroller, he lies at home. And how is this mucus in this case supposed to move up and down? Turn the baby over more often, do not forget about airing the room, about walking in the fresh air.
Do not confuse with pathology
Do not confuse physiological rhinitis with allergic or inflammatory rhinitis. Experienced pediatric ENT doctors in Makhachkala know that a newborn does not usually suffer from allergic rhinitis. Only if an allergen somehow got into the body, or it happens that the mixture did not fit. But in this case, as soon as we remove the allergic process, the runny nose stops.
In the inflammatory nature of the discharge from the nose is not transparent, but yellowish, greenish with an admixture of blood. Of course, then you already need to run to a medical clinic to a specialist. Because the process can become chronic. Do not get used to vasoconstrictor drops. After all, they do not cure a runny nose, but only relieve a symptom, and besides, it is very easy to get used to them. Thus, you will not even notice how your child's normal physiological runny nose has become chronic.
Preventive measures
The heating season is ahead of us. We will definitely face the fact that the heaters will turn on in the rooms, and this will lead to overdrying of the air in the living quarters. Specialists in ENT diseases in children are advised to hang in the room where the baby sleeps, next to the crib, hang a hygrometer to determine humidity and a thermometer that will show the temperature in the room. The temperature for newborns in the room should be within 18-20 degrees, and humidity 60-70%.
We will definitely face the fact that the heaters will turn on in the rooms, and this will lead to overdrying of the air in the living quarters. Specialists in ENT diseases in children are advised to hang in the room where the baby sleeps, next to the crib, hang a hygrometer to determine humidity and a thermometer that will show the temperature in the room. The temperature for newborns in the room should be within 18-20 degrees, and humidity 60-70%.
"If parents see that the child has accumulated mucus in the nasal passages, it is recommended to put 1 drop into each nostril of a solution with sea salt. It can be Aqualor or Aquamaris. It is also very useful to put small children on their tummy. put on his tummy. Let him buck and move. Yes, it is uncomfortable for him, it is not comfortable. It is also desirable to put your hand, let him push off. Thus, he physiologically begins to breathe actively, and with this air, the accumulated mucus will independently and easily come out of nasal passages".
Other items
Khanverdiev Rustam Abdulmazhidovich
pediatric surgeon, circumcision, surgeon
Infantile hemangioma: diagnosis and treatment
Infantile hemangioma is a congenital malformation of the capillaries in a child, which is classified as benign…
Dropsy of the testicles in children: what is it, how is it manifested and how is it treated?
Dropsy of the testicular membranes (hydrocele) is a benign process in which serous fluid accumulates in the scrotum cavity…
November 25, 2022
How to recognize eye diseases in a child?
You have a joyful event in your family – a child was born! But you must remember that there are certain rules for inspecting this new…
November 17, 2022
Rules for preparing for analyzes
For the most accurate diagnosis of diseases, the most modern laboratory equipment is not enough.
November 1, 2022
Runny nose in a baby causes and treatment
Snot in a baby appears very often, but not all parents understand how dangerous or harmless it is and what to do if their baby has a runny nose.
A runny nose in infants is not always due to the addition and development of the disease, it can also have completely physiological causes associated with the age and development of the child's body during this tender period.
As with any other pathological condition, there may be causes of a runny nose in infants.
- physiological;
- pathological.
Physiological causes
The mucous membrane of the nasal cavities immediately after birth, although it is formed correctly, but cannot fully perform its functions, participate in the regulatory mechanisms of the body. In some children, this leads to excessive dryness of the nasal cavity with insufficient secretion production, while in others to its abundant secretion - a newborn runny nose.
Mucosal function returns to normal only after reaching 10 months of age. It's not worth worrying. This is not dangerous and should go away on its own over time, but the ENT doctors of Dr. Korenchenko's clinic advise you to go to the pediatrician. so as not to miss the beginning of the development of the pathological process behind imaginary well-being.
It's not worth worrying. This is not dangerous and should go away on its own over time, but the ENT doctors of Dr. Korenchenko's clinic advise you to go to the pediatrician. so as not to miss the beginning of the development of the pathological process behind imaginary well-being.
Pathological causes
The most common cause is colds, which are especially common in newborns. Own immunity has not yet been formed, and maternal immunity is not always effective enough and, moreover, is weakening every day. Any infection that for an adult or older child will go completely unnoticed in a newborn can cause acute respiratory infections and a runny nose.
The first symptoms of an acute infectious disease are fever and a runny nose. Later, cough, shortness of breath, shortness of breath join. Sleep and appetite disorders. The child becomes restless, cries, refuses to eat. Abundant snot in infants causes irritation of the skin around the nose, on the upper lip, in the nasolabial folds. At the first appearance of such symptoms, we strongly advise you to contact your pediatrician immediately.
At the first appearance of such symptoms, we strongly advise you to contact your pediatrician immediately.
Another common cause of a runny nose in a newborn is an allergic reaction to an external irritant. With age and with the formation of one's own full-fledged immune defense, this disease can go away on its own, but in infancy, intolerance to any substances is more common than in adults. Irritants can be ordinary household dust, pet or bird hair, extraneous odors, creams and preparations that treat the baby's skin, even the smell of the mother and breast milk can provoke snot in the baby.
Relatively infrequently, the cause of snot in infants is vasomotor rhinitis, a disease associated with impaired blood supply to the nasal mucosa. The correct diagnosis can only be established by a doctor.
Treatment
To free the nasal passages, use special micro-suckers or a small enema, but only for suctioning the secretions, not for washing. The pear cannula or enema should be inserted with caution and very shallowly, only 0.5-0.8 cm deep into the nasal passage.
The pear cannula or enema should be inserted with caution and very shallowly, only 0.5-0.8 cm deep into the nasal passage.
Any folk or sorcerer's remedies, potions or manipulations can be performed only after agreement with the doctor. Uncontrolled self-medication can harm the baby. Too tender age for a child to take such risks!
Medicines should only be used as prescribed by a doctor, strictly following his instructions and recommendations. Only a doctor can accurately determine the condition of the child and correctly prescribe the treatment of a runny nose in infants with medications.
Most commonly prescribed drugs
- Aqua Maris;
- Aqualor Baby;
- Nazol Baby;
- Otrivin Baby;
- Doctor Mom;
- Saline;
- Nazivin for children.

Please note that all listed preparations have the prefix "baby" or "children's". It is impossible to use adult medicines to treat a runny nose in infants.
Physiological runny nose in infants does not need treatment, but only a doctor can determine the absence of pathology.
DO NOT!
- use an enema to wash the sinuses with fluid injection. A pear and an enema can only be used to suck snot from a baby, and then with caution;
- independently prescribe antibacterial and antiviral drugs;
- use vasoconstrictor nasal drops and sprays without medical advice.
Remember! At this age, the baby's health is very fragile. Having taken up the treatment of a runny nose in a baby on your own or according to the recipes of familiar grandmothers, instead of improving your health, you can do much harm to him.