Induction process for twins
The effect of induction method in twin pregnancies: a secondary analysis for the twin birth study | BMC Pregnancy and Childbirth
- Research article
- Open Access
- Published:
- Elad Mei-Dan1,
- Elizabeth V. Asztalos1,
- Andrew R. Willan2 &
- …
- Jon F. R. Barrett1
BMC Pregnancy and Childbirth volume 17, Article number: 9 (2017) Cite this article
-
5795 Accesses
-
13 Citations
-
3 Altmetric
-
Metrics details
Abstract
Background
This secondary analysis for the Twin Birth Study, an international, multicenter trial, aimed to compare the cesarean section rates and safety between methods of induction of labor in twin pregnancies.
Methods
Women with twin pregnancies where the first twin was in a cephalic presentation and who presented for labor induction, were non-randomly assigned to receive prostaglandin or amniotomy and/or oxytocin. Main outcome measures were the rates of unplanned cesarean section and neonatal and maternal mortality or serious morbidity.
Results
153 (41.5%) were induced by prostaglandin (prostaglandin group) and 215 (58.5%) were induced by amniotomy and/or oxytocin alone (no prostaglandin group). Induction using prostaglandin was more common in countries with a low perinatal mortality rate <10/1000 (45.7 versus 32.5%, p = 0.02). Cesarean section rates were similar in the two groups: 62/153 (40.5%) in the prostaglandin group and 87/215 (40.5%) in the no prostaglandin group (odds ratio 1, 95% CI 0.65-1.5). Nulliparity, late maternal age, non-cephalic presentation of twin B and high country’s perinatal mortality rate were found to be independently associated with the induction to end with an unplanned cesarean section. There were no significant differences between groups with respect to maternal or neonatal adverse outcomes.
There were no significant differences between groups with respect to maternal or neonatal adverse outcomes.
Conclusions
The need for cervical ripening by prostaglandin had no effect on the incidence of cesarean delivery or an abnormal outcome. There is a significant risk of unplanned cesarean section independent of chosen induction method.
Trial registration
This trial was registered at the International Standard Randomized Controlled Trial Register (identifier ISRCTN74420086; December 9, 2003) and retrospectively registered at the www.clinicaltrials.gov (identifier NCT 00187369; September 12, 2005).
Peer Review reports
Background
Twin birth are increasingly common and now occur in 2 to 3% of all births [1–3]. These pregnancies pose an increased risk for adverse perinatal outcomes compared to singletons at all gestations [1, 2]. In late twin pregnancy perinatal mortality rates rise dramatically from 8.4 per 1000 at 38 weeks of gestation to 12.7 and 15.6 per 1000 at 40 and 41 weeks, respectively [2, 4]. In attempt to limit these late term losses an elective delivery at 37–39 weeks of gestation has been widely recommended [1, 5–8]. This has led to a marked rise in induction of twin pregnancies from 5.8% in 1989 to 13.8% in 1999, with a concomitant decrease in twin stillbirth rates [9]. Oxytocin and prostaglandins (PG) are commonly used induction methods in twin gestations, however despite their increase use, information regarding the outcome of these induced labors is minimal [10–12].
In late twin pregnancy perinatal mortality rates rise dramatically from 8.4 per 1000 at 38 weeks of gestation to 12.7 and 15.6 per 1000 at 40 and 41 weeks, respectively [2, 4]. In attempt to limit these late term losses an elective delivery at 37–39 weeks of gestation has been widely recommended [1, 5–8]. This has led to a marked rise in induction of twin pregnancies from 5.8% in 1989 to 13.8% in 1999, with a concomitant decrease in twin stillbirth rates [9]. Oxytocin and prostaglandins (PG) are commonly used induction methods in twin gestations, however despite their increase use, information regarding the outcome of these induced labors is minimal [10–12].
The Twin Birth Study (TBS) was an international, multicenter, randomized controlled trial that compared planned vaginal delivery (VD) to planned cesarean section (CS) in twin pregnancies between 32 and 38 weeks gestation where the first twin was in a cephalic presentation at the time of randomization [1]. The study reported there was no difference in fetal and neonatal outcomes between the two approaches.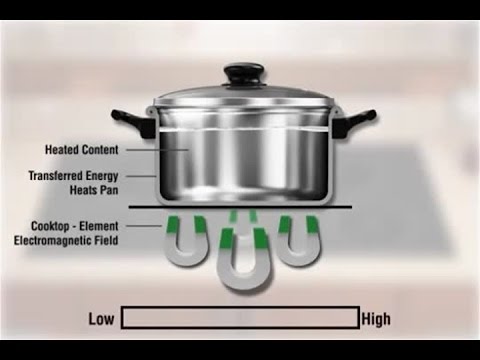 In this nonrandomized secondary analysis of the TBS data on women who had induction of labor, the primary objective was to compare the rate of unplanned CS and safety between various induction methods that were employed both on neonatal and maternal mortality or serious morbidity.
In this nonrandomized secondary analysis of the TBS data on women who had induction of labor, the primary objective was to compare the rate of unplanned CS and safety between various induction methods that were employed both on neonatal and maternal mortality or serious morbidity.
Methods
Initial Study [1]
Women were enrolled in the TBS if they were between 32 and 38 weeks of gestation, the first twin was in the cephalic presentation, and both twins were alive with an estimated weight between 1500 g and 4000 g. Exclusion criteria were mono-amniotic twins, fetal reduction at 13 or more weeks of gestation, the presence of a lethal fetal anomaly, contraindication to labor or VD (e.g., fetal compromise, second twin substantially larger than the first twin, fetal anomaly or condition that might cause mechanical problems at delivery, and previous vertical uterine incision or more than one previous low-segment CS), and previous participation in the TBS. Participants aged under 16 years were not included in this study. Randomization took place between December 13, 2003 and April 4, 2011; women were randomly assigned to planned CS or planned VD. Randomization was centrally controlled at the Center for Mother, Infant, and Child Research at the Sunnybrook Health Sciences Center in Toronto, ON, Canada. Data were abstracted from the medical records at participating centers by trained study staff and were recorded, after delivery, on standardized data-collection forms. Participating centers were prepared to perform a CS within 30 min if necessary; and had anesthetic, obstetrical, and nursing staff available in the hospital at the time of delivery. A qualified obstetrician, experienced at vaginal twin delivery, was required to attend all vaginal deliveries. Elective delivery by means of either CS (for women in the planned CS group) or labor induction (for women in the planned VD group) was planned between 37 weeks 5 days and 38 weeks 6 days of gestation. The methods of induction, the use of oxytocin and the decision of oxytocin regimen were not prescriptive and each center/clinician could choose the preferred methods of induction and dosing.
Randomization took place between December 13, 2003 and April 4, 2011; women were randomly assigned to planned CS or planned VD. Randomization was centrally controlled at the Center for Mother, Infant, and Child Research at the Sunnybrook Health Sciences Center in Toronto, ON, Canada. Data were abstracted from the medical records at participating centers by trained study staff and were recorded, after delivery, on standardized data-collection forms. Participating centers were prepared to perform a CS within 30 min if necessary; and had anesthetic, obstetrical, and nursing staff available in the hospital at the time of delivery. A qualified obstetrician, experienced at vaginal twin delivery, was required to attend all vaginal deliveries. Elective delivery by means of either CS (for women in the planned CS group) or labor induction (for women in the planned VD group) was planned between 37 weeks 5 days and 38 weeks 6 days of gestation. The methods of induction, the use of oxytocin and the decision of oxytocin regimen were not prescriptive and each center/clinician could choose the preferred methods of induction and dosing.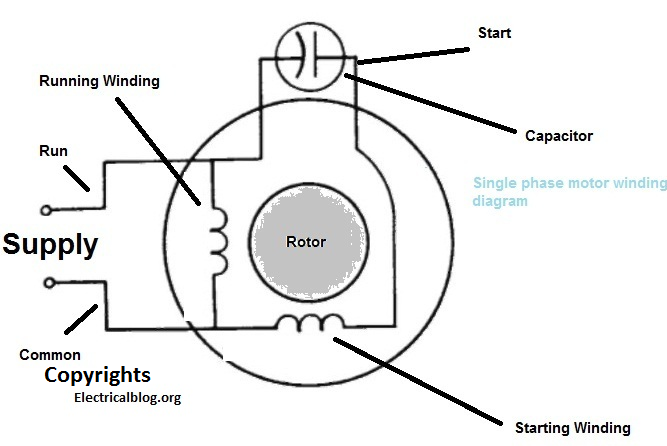 The patients included in the analysis for this paper were those who were randomized to planned VD and had labor induced.
The patients included in the analysis for this paper were those who were randomized to planned VD and had labor induced.
Baseline factors, such as maternal age, parity, chorionicity, gestational age at induction and the country’s perinatal mortality rate (PMR), associated with the method of induction were compared with respect to discrete variables using contingency table chi-squared tests and with respect to continuous variables using two-sample t-tests. The effect of the method of induction on unplanned CS; neonatal mortality or serious neonatal morbidity; and, maternal death or serious maternal morbidity was investigated using logistic regression. The effect of the method of induction on the time intervals of the induction delivery process, viz., the duration between active labor and full dilation, the duration between active labor and delivery and the duration between delivery and discharge were investigated using two-sample t-tests. Odds ratios and their corresponding 95% confidence intervals are provided for binary outcomes, while means and standard deviations are provided for continuous outcomes. For the neonatal outcome the unit of analysis is infant and generalized estimating equations were used to account for the correlation between infants from the same pregnancy. All p-values in all tables are two-sided. The level for declaring statistical significance was set to 0.05. Since the analysis was secondary to a randomized clinical trial, no power calculations were performed. The power of the analysis and corresponding results are reflected in the width of the confidence intervals. This research adhered to the STROBE guidelines for observational studies.
For the neonatal outcome the unit of analysis is infant and generalized estimating equations were used to account for the correlation between infants from the same pregnancy. All p-values in all tables are two-sided. The level for declaring statistical significance was set to 0.05. Since the analysis was secondary to a randomized clinical trial, no power calculations were performed. The power of the analysis and corresponding results are reflected in the width of the confidence intervals. This research adhered to the STROBE guidelines for observational studies.
Results
The planned VD arm was randomly assigned to 1406 women. Of these, 368 women were identified as having undergone induction: 153 (42%) underwent induction with the use of prostaglandin (PG group) and 215 (58%) underwent induction with amniotomy and/or oxytocin (no PG group), (Fig. 1). Table 1 outlines the characteristics of the women in the two comparison groups at the time of randomization and at the time of delivery. The two groups were similar apart from the national PMR. Women were more likely to have PG as the method of induction in countries with a lower PMR as compared to the non-PG approach. In total, 149/368 (40.5%) women underwent a CS after induction of labor. The incidence in the two groups of induction was similar: 62/153 (40.5%) in the PG group and 87/215 (40.5%) in the no PG group. Table 2 outlines the CS rate by method of induction and the variables of interest that were found to be significantly associated with an unplanned CS following induction of labor. The method of induction of labor had no effect on the rate of CS for both twins. Nulliparous women and women over the age of 30 years were more likely to be unsuccessful with planned induction of labor and require an unplanned CS. In addition, a CS was more likely to occur when twin B presentation was non-cephalic and in countries where the national PMR is ≥ 10/1000. Using multiple regression models, parity, maternal age, presentation of twin B and PMR were found to be independently associated with an unplanned CS following induction of twin pregnancies (Table 3).
The two groups were similar apart from the national PMR. Women were more likely to have PG as the method of induction in countries with a lower PMR as compared to the non-PG approach. In total, 149/368 (40.5%) women underwent a CS after induction of labor. The incidence in the two groups of induction was similar: 62/153 (40.5%) in the PG group and 87/215 (40.5%) in the no PG group. Table 2 outlines the CS rate by method of induction and the variables of interest that were found to be significantly associated with an unplanned CS following induction of labor. The method of induction of labor had no effect on the rate of CS for both twins. Nulliparous women and women over the age of 30 years were more likely to be unsuccessful with planned induction of labor and require an unplanned CS. In addition, a CS was more likely to occur when twin B presentation was non-cephalic and in countries where the national PMR is ≥ 10/1000. Using multiple regression models, parity, maternal age, presentation of twin B and PMR were found to be independently associated with an unplanned CS following induction of twin pregnancies (Table 3). Table 4 outline other neonatal and maternal outcomes, as well as time intervals in the induction and delivery process, for the two groups who underwent induction. The two groups were similar in the incidence of the maternal and neonatal composite outcomes as defined by the protocol in the TBS [1]. The breakdowns of the individual maternal and neonatal outcomes as well as maternal and fetal reasons for cesarean section by therapeutic group are shown in tables Additional file 1: Table S1 and Additional file 2: Table S2, respectively.
Table 4 outline other neonatal and maternal outcomes, as well as time intervals in the induction and delivery process, for the two groups who underwent induction. The two groups were similar in the incidence of the maternal and neonatal composite outcomes as defined by the protocol in the TBS [1]. The breakdowns of the individual maternal and neonatal outcomes as well as maternal and fetal reasons for cesarean section by therapeutic group are shown in tables Additional file 1: Table S1 and Additional file 2: Table S2, respectively.
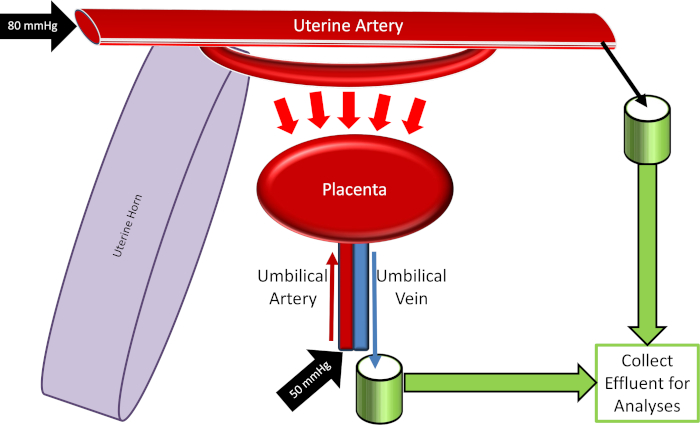
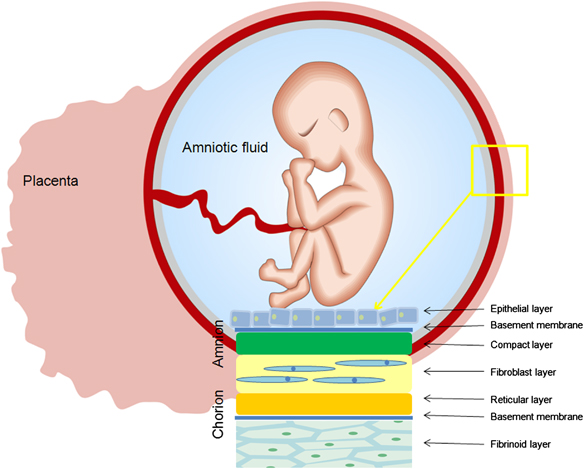
Flow diagram of women randomized to the planned vaginal birth arm of the Twin Birth Study
Full size image
Table 1 Baseline characteristics by method of inductionFull size table
Table 2 Cesarean delivery by method of induction and covariablesFull size table
Table 3 Results of the multivariable logistic regression of cesarean deliveryFull size table
Table 4 Other outcome variables by method of inductionFull size table
Discussion
In this secondary analysis, we were able to demonstrate that the method of induction of labor in twins had no effect on the rate of unplanned CS.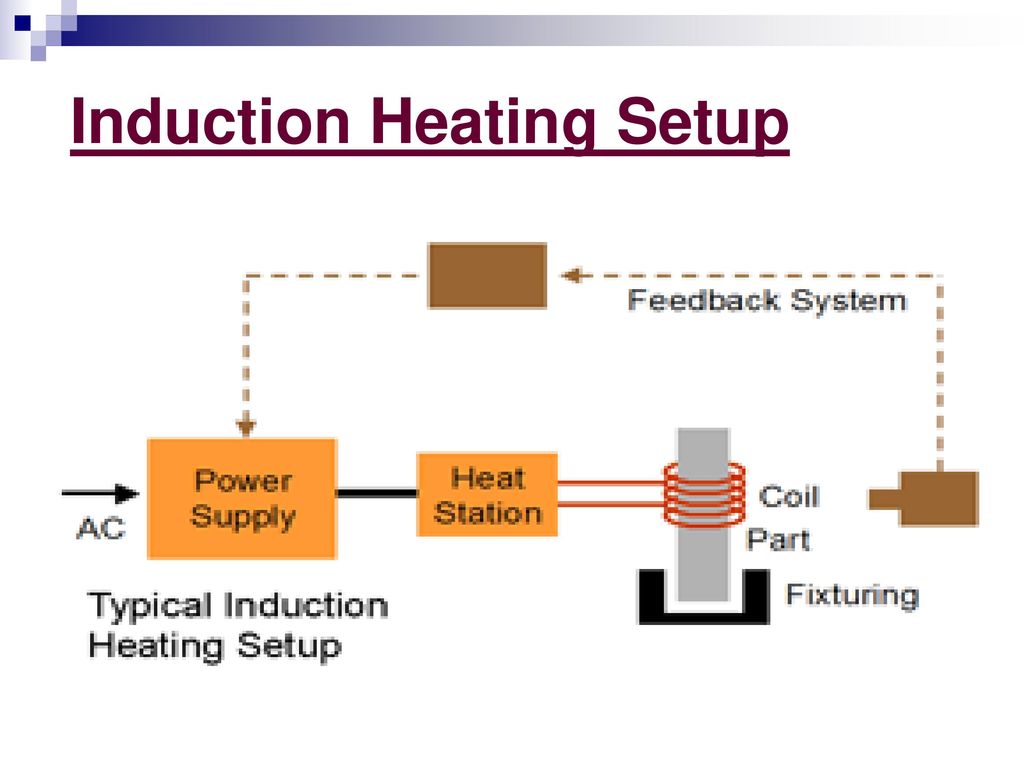 In addition, we showed that neither approach contributed to an adverse outcome for either the woman or her infant. However, using either method of induction the rate of an unplanned CS is higher than what has been reported in singleton pregnancies [13–17]. Furthermore, while induction in whom cervical ripening is not required (no PG group) is associated with a lower rate of CS in the case of singleton pregnancies [18, 19], we did not find the same result in twin pregnancies. We postulate that there may be a different mechanism associated with labor and delivery in twins or that the primary higher risk for CS in twins masks this difference [20, 21]. Since CS rate was similar in both groups, we feel this study indicates that all twins in whom induction of labor is indicated should be informed of a significant risk of unplanned CS, regardless of intervention. Late maternal age and nulliparity remained strongly associated with an unplanned CS following induction of labor, as has been shown in many studies [22–24].
In addition, we showed that neither approach contributed to an adverse outcome for either the woman or her infant. However, using either method of induction the rate of an unplanned CS is higher than what has been reported in singleton pregnancies [13–17]. Furthermore, while induction in whom cervical ripening is not required (no PG group) is associated with a lower rate of CS in the case of singleton pregnancies [18, 19], we did not find the same result in twin pregnancies. We postulate that there may be a different mechanism associated with labor and delivery in twins or that the primary higher risk for CS in twins masks this difference [20, 21]. Since CS rate was similar in both groups, we feel this study indicates that all twins in whom induction of labor is indicated should be informed of a significant risk of unplanned CS, regardless of intervention. Late maternal age and nulliparity remained strongly associated with an unplanned CS following induction of labor, as has been shown in many studies [22–24]. On the other hand, the finding that CS occurs more commonly following induction in countries where the PMR is ≥ 10/1000, was not reported previously. It is possible that in low-income countries and in low-resource centers (as a surrogate for higher PMR) physicians are more comfortable with the decision for a controlled CS than with a potentially long and uncontrolled VD in this setting. In the same manner, countries with higher PMR are usually the ones with less economic resources, so it is not surprising that PG (usually a more expensive drug than oxytocin or nearly costless amniotomy) was used less often in these countries. While induction with PG has been reported to be associated with adverse events such as fetal heart rate abnormalities or even uterine rupture [25], we did not find this association or other fetal or maternal adverse outcomes in our trial. Although not powered to assess rare maternal adverse outcomes, this study suggests that both approach of induction of labor, PG or no PG, are safe in twin pregnancies.
On the other hand, the finding that CS occurs more commonly following induction in countries where the PMR is ≥ 10/1000, was not reported previously. It is possible that in low-income countries and in low-resource centers (as a surrogate for higher PMR) physicians are more comfortable with the decision for a controlled CS than with a potentially long and uncontrolled VD in this setting. In the same manner, countries with higher PMR are usually the ones with less economic resources, so it is not surprising that PG (usually a more expensive drug than oxytocin or nearly costless amniotomy) was used less often in these countries. While induction with PG has been reported to be associated with adverse events such as fetal heart rate abnormalities or even uterine rupture [25], we did not find this association or other fetal or maternal adverse outcomes in our trial. Although not powered to assess rare maternal adverse outcomes, this study suggests that both approach of induction of labor, PG or no PG, are safe in twin pregnancies.
Our study’s strength lies in its size (82 participating centers in 23 countries), and a high rate of follow-up. The main limitation of this study is the fact it is a secondary analysis. The method of induction of labor was not randomized and baseline cervical exam, bishop score, the type of PG used and dosing intervals were not available as one of the variables in the analysis between the two groups of induction. Lastly, this study assessed the pharmacological methods of induction (e.g., PG or oxytocin) and is lacking the use of mechanical induction in twin (e.g., single or double balloon catheter) and its comparison with pharmacological methods. Bush et al [11], in a similar study, compared intra-vaginal misoprostol to oxytocin for the induction of labor in twin gestations. They reported a shorter length of induction to delivery and a trend toward a lower CS rate (16.9 vs. 31.6%, p = 0.06) in the oxytocin-only group. They too concluded that both PG and oxytocin appear to be safe and efficacious for use in induction of labor in twins. Huber et al [26] and Okby et al [21] analyzed twin induction using PG followed by amniotomy/oxytocin as an induction method. They found CS rate with induction of labor in twin pregnancy to be similar to our study (43.7 and 31.2%, respectively). Taylor et al [3] and Suzuki et al [7], in a study in which a variety of methods of induction were used, found CS rate to be lower than our study (19 and 18%, respectively). In their studies however only induced women for the indication of advanced gestational age where included, whereas our study other indications for induction were included which may explain our higher CS rate. In a recent study, de Castro et al [27] found induction of labor with Foley catheter to be an independent risk factor for having CS. In their retrospective study of 883 women with twins who underwent a trial of labor, other methods of induction were not assessed and information regarding neonatal mortality and morbidity was missing. As in our study, others have shown that both PG and oxytocin are safe induction agents in twin pregnancy and are not associated with higher rates of hyperstimulation or adverse neonatal or maternal outcomes compared to induction in singleton [3, 11, 12, 28].
Huber et al [26] and Okby et al [21] analyzed twin induction using PG followed by amniotomy/oxytocin as an induction method. They found CS rate with induction of labor in twin pregnancy to be similar to our study (43.7 and 31.2%, respectively). Taylor et al [3] and Suzuki et al [7], in a study in which a variety of methods of induction were used, found CS rate to be lower than our study (19 and 18%, respectively). In their studies however only induced women for the indication of advanced gestational age where included, whereas our study other indications for induction were included which may explain our higher CS rate. In a recent study, de Castro et al [27] found induction of labor with Foley catheter to be an independent risk factor for having CS. In their retrospective study of 883 women with twins who underwent a trial of labor, other methods of induction were not assessed and information regarding neonatal mortality and morbidity was missing. As in our study, others have shown that both PG and oxytocin are safe induction agents in twin pregnancy and are not associated with higher rates of hyperstimulation or adverse neonatal or maternal outcomes compared to induction in singleton [3, 11, 12, 28].
Conclusion
Both methods of induction, PG or no PG, are associated with the same high rate of unplanned CS, but are safe for use in induction of labor in twins. Further studies are needed to determine the effectiveness and safety of various induction methods in twin pregnancy.
Abbreviations
- CS:
-
Cesarean section
- PG:
-
Prostaglandins
- PMR:
-
Perinatal mortality rate
- RCT:
-
Randomized controlled trial
- TBS:
-
Twin birth study
- VD:
-
Vaginal delivery
References
Barrett JF, Hannah ME, Hutton EK, Willan AR, Allen AC, Armson BA, et al. Twin Birth Study Collaborative Group. A randomized trial of planned caesarean or vaginal delivery for twin pregnancy. N Engl J Med. 2013;369:1295–305.
Article CAS PubMed PubMed Central Google Scholar
Harle T, Brun JL, Leng JJ. Induction of labor in twin pregnancy after 36 weeks does not increase maternal-fetal morbidity. Int J Gynaecol Obstet. 2002;77:15–21.
Article CAS PubMed Google Scholar
Taylor M, Rebarber A, Saltzman DH, Klauser CK, Roman AS, Fox NS. Induction of labor in twin compared with singleton pregnancies. Obstet Gynecol. 2012;120:297–301.
Article PubMed Google Scholar
Kiely JL. What is the population-based risk of preterm birth among twins and other multiples? Clin Obstet Gynecol.
 1998;41:3–11.
1998;41:3–11.Article CAS PubMed Google Scholar
Spong CY, Mercer BM, D’alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118:323–33.
Article PubMed PubMed Central Google Scholar
Hartley RS, Emanuel I, Hitti J. Perinatal mortality and neonatal morbidity rates among twin pairs at different gestational ages: optimal delivery timing at 37 to 38 weeks’ gestation. Am J Obstet Gynecol. 2001;184:451–8.
Article CAS PubMed Google Scholar
Suzuki S, Otsubo Y, Sawa R, Yoneyama Y, Araki T. Clinical trial of induction of labor versus expectant management in twin pregnancy. Gynecol Obstet Invest. 2000;49:24–7.
Article CAS PubMed Google Scholar
Minakami H, Sato I. Reestimating date of delivery in multifetal pregnancies. JAMA. 1996;275:1432–4.
Article CAS PubMed Google Scholar
Ananth CV, Joseph KS, Kinzler WL. The influence of obstetric intervention on trends in twin stillbirths: United Sates 1989–99. J Maternal Fetal Neonatal Med. 2004;15:380–7.
Article CAS Google Scholar
Manor M, Blickstein I, Ben-Arie A, Weissman A, Hagay Z. Case series of labor induction in twin gestations with an Intrauterine Balloon catheter. Gynecol Obstet Invest. 1999;47:244–6.
Article CAS PubMed Google Scholar
Bush MC, Csaba A, Eddleman KA, Saphier CJ. Is misoprostol safe for labor induction in twin gestations? J Matern Fetal Neonatal Med. 2006;19:35–8.
Article CAS PubMed Google Scholar
Fausett MB, Barth Jr WH, Yoder BA, Satin AJ. Oxytocin labor stimulation of twin gestations: Effective and efficient. Obstet Gynecol. 1997;90:202–4.
Article CAS PubMed Google Scholar
Cammu H, Martens G, Ruyssinck G, Amy JJ. Outcome after elective labor induction in nulliparous women: a matched cohort study. Am J Obstet Gynecol. 2002;186:240–4.
Article PubMed Google Scholar
Seyb ST, Berka RJ, Socol ML, Dooley SL. Risk of caesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol. 1999;94:600–7.
CAS PubMed Google Scholar
Vrouenraets FP, Roumen FJ, Dehing CJ, van den Akker ES, Aarts MJ, Scheve EJ. Bishop score and risk of caesarean delivery after induction of labor in nulliparous women.
 Obstet Gynecol. 2005;105:690–7.
Obstet Gynecol. 2005;105:690–7.Article PubMed Google Scholar
Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of a caesarean delivery among nulliparous women at term. Obstet Gynecol. 2010;116:35–42.
Article PubMed Google Scholar
Battista L, Chung JH, Lagrew DC, Wing DA. Complications of labor induction among multiparous women in a community-based hospital system. Am J Obstet Gynecol. 2007;197:241. e1–7.
Article PubMed Google Scholar
Breart G, Goujard J, Maillard F, Chavigny C, Rumeau-Rouquette C, Sureau C. Comparison of 2 obstetrical attitudes vis-a-vis inducing labor at term. Randomized study. J Gynecol Obstet Biol Reprod. 1982;11:107–12.
CAS Google Scholar
Augensen K, Bergsjo P, Eikeland T, Askvik K, Carlsen J. Randomised comparison of early versus late induction of labour in post-term pregnancy. Br Med J (Clin Res Ed). 1987;294:1192–5.
Article CAS Google Scholar
Turton P, Arrowsmith S, Prescott J, Ballard C, Bricker L, Neilson J, et al. A comparison of the contractile properties of myometrium from singleton and twin pregnancies. PLoS One. 2013;8:e63800.
Article CAS PubMed PubMed Central Google Scholar
Okby R, Shoham-Vardi I, Ruslan S, Sheiner E. Is induction of labor risky for twins compare to singleton pregnancies? J Matern Fetal Neonatal Med. 2013;26:1804–6.
Article PubMed Google Scholar
Wang Y, Tanbo T, Abyholm T, Henriksen T. The impact of advanced maternal age and parity on obstetric and perinatal outcomes in singleton gestations.
 Arch Gynecol Obstet. 2011;284:31–7.
Arch Gynecol Obstet. 2011;284:31–7.Article PubMed Google Scholar
Parrish KM, Holt VL, Easterling TR, Connell FA, LoGerfo JP. Effect of changes in maternal age, parity, and birth weight distribution on primary caesarean delivery rates. JAMA. 1994;271:443–7.
Article CAS PubMed Google Scholar
Mehta S, Tran K, Stewart L, Soutter E, Nauta M, Yoong W. Pregnancy outcomes in women greater than 45 years: a cohort control study in a multi-ethnic inner city population. Arch Gynecol Obstet. 2014;289:1125–8.
Article PubMed Google Scholar
Kent A. Induction of labor. Rev Obstet Gynecol. 2012;5:113–4.
Google Scholar
Huber G, Schütz H, Seelbach-Göbel B. Induction of labor in twin pregnancies with oral misoprostol versus vaginal dinoprostone - is it effective and safe? J Matern Fetal Neonatal Med.
 2015;28:1043–6.
2015;28:1043–6.Article CAS PubMed Google Scholar
de Castro H, Haas J, Schiff E, Sivan E, Yinon Y, Barzilay E. Trial of labour in twin pregnancies: a retrospective cohort study. BJOG. 2015. doi:10.1111/1471-0528.13521.
PubMed Google Scholar
Simões T, Condeço P, Dias E, Ventura P, Matos C, Blickstein I. Induction of labor with oral misoprostol in nulliparous mothers of twins. J Perinat Med. 2006;34:111–4.
Article PubMed Google Scholar
Download references
Acknowledgments
We thank the Steering Committee (Twin Birth Study) for reviewed our findings and approved publication: J. Barrett (Chair), E. Asztalos, A. Willan, M. Hannah, E. Hutton, A. Allen, A. Armson, A. Gafni, KS. Joseph, A. Ohlsson, S. Ross.
Funding
TBS was supported by a grant (63164) from the Canadian Institutes of Health Research (CIHR). CIHR had no role in the design, management, data collection, analysis, or interpretation of the data. CIHR had no role in the writing of this manuscript or in the decision to submit for publication.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author upon reasonable request and with permission from the TBS Steering Committee.
Authors’ contributions
All authors have contributed to the study. EM, LA, AW and JB conceived the idea, participated in the analysis, interpreted the results and wrote the paper. AW performed the statistical analysis. All authors have read and approved the final version of the manuscript. LA and AW have access to all data of this study and are the guarantors.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All the women from the initial TBS study provided written informed consent before being enrolled. The research ethics committee at each participating center approved the study protocol of the initial TBS, which is available with the full text of the original article at NEJM.org. All secondary analyses were approved by the Research Ethics Board at the Sunnybrook Health Sciences Center. Clinical trial identification- International Standard Randomized Controlled Trial Register (identifier ISRCTN74420086; December 9, 2003) and retrospectively registered at the www.clinicaltrials.gov (identifier NCT 00187369; September 12, 2005).
Author information
Authors and Affiliations
Women and Babies Program, Sunnybrook Health Sciences Center, Sunnybrook Research Institute, 2075 Bayview Ave, Toronto, ON, M4N 3M5, Canada
Elad Mei-Dan, Elizabeth V. Asztalos & Jon F.
 R. Barrett
R. BarrettChild Health Evaluative Sciences, SickKids Research Institute, University of Toronto, The Hospital for Sick Children, 555 University Avenue, Toronto, M5G 1X8, ON, Canada
Andrew R. Willan
Authors
- Elad Mei-Dan
View author publications
You can also search for this author in PubMed Google Scholar
- Elizabeth V. Asztalos
View author publications
You can also search for this author in PubMed Google Scholar
- Andrew R. Willan
View author publications
You can also search for this author in PubMed Google Scholar
- Jon F. R. Barrett
View author publications
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elad Mei-Dan.
Additional files
Additional file 1: Table S1.
Adverse maternal or neonatal outcomes by method of induction. (RTF 86 kb)
Additional file 2: Table S2.
Maternal and fetal reasons for cesarean section by therapeutic group. (RTF 52 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Giving birth to twins | Pregnancy Birth and Baby
Twins are more likely to be born early, often before 38 weeks, so it's important to understand your birth options. Less than half of all twin pregnancies last beyond 37 weeks.
Less than half of all twin pregnancies last beyond 37 weeks.
Because of the likelihood that your babies will be born early, there is a good chance one or both of them will spend some time in special care.
As twins are often born prematurely, it's a good idea to discuss birth options with your midwife or doctor early in your pregnancy.
You should also discuss where you would like to give birth. You will most likely be advised to give birth in a hospital because there's a higher chance of complications with a twin birth.
It's common for more medical staff to be involved in the birth of twins, such as a midwife, an obstetrician and two paediatricians - one for each baby.
While the process of labour is the same as when single babies are born, twin babies are more closely monitored. To do this, an electronic monitor and a scalp clip might be fitted on the first baby once your waters have broken. You will be given a drip in case it is needed later.
Vaginal birth
About one third of all twins are born vaginally and the process is similar to that of giving birth to a single baby. If you're planning a vaginal delivery, it's usually recommended that you have an epidural for pain relief. This is because, if there are problems, it's easier and quicker to assist the delivery when the mother already has good pain relief.
If you're planning a vaginal delivery, it's usually recommended that you have an epidural for pain relief. This is because, if there are problems, it's easier and quicker to assist the delivery when the mother already has good pain relief.
If the first twin is in a head down position (cephalic), it's usual to consider having a vaginal birth. However, there may be other medical reasons why this would not be possible. If you have had a previous caesarean section, it's usually not recommended you have a vaginal birth with twins.
If you have a vaginal birth, you may need an assisted birth, which is when a suction cup (ventouse) or forceps are used to help deliver the babies.
Once the first baby is born, the midwife or doctor will check the position of the second baby by feeling your abdomen and doing a vaginal examination. If the second baby is in a good position, the waters will be broken and this baby should be born soon after the first as the cervix is already fully dilated.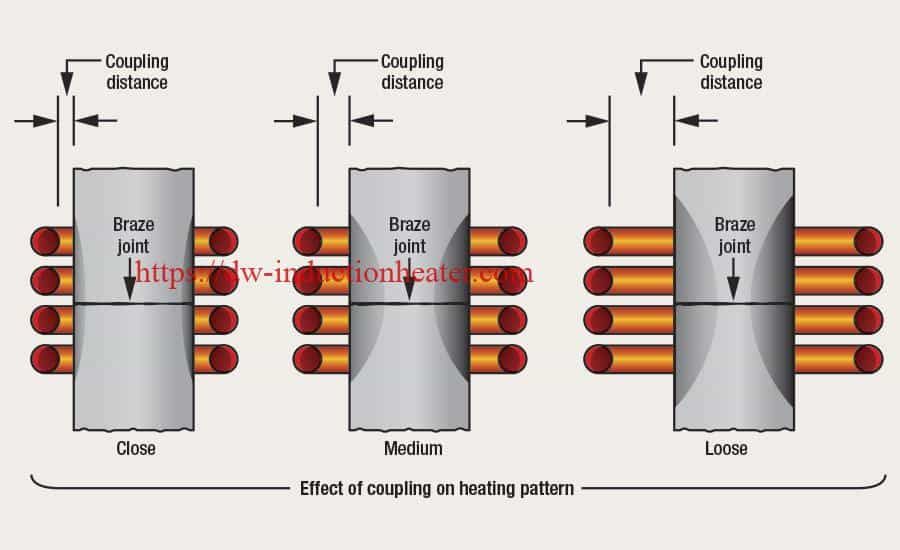 If contractions stop after the first birth, hormones will be added to the drip to restart them.
If contractions stop after the first birth, hormones will be added to the drip to restart them.
Caesarean section
You may choose to have an elective caesarean from the outset of your pregnancy, or your doctor may recommend a caesarean section later in the pregnancy as a result of potential complications. You’re nearly twice as likely to have a caesarean if you’re giving birth to twins than if you’re giving birth to a single baby.
The babies' position may determine whether they need to be delivered by caesarean section or not. If the presenting baby - the one that will be born first - is in a breech position (feet, knees or buttocks first), or if one twin is lying in a transverse position (with its body lying sideways), you will need to have a caesarean section.
Some conditions also mean you will need a caesarean section; for example if you have placenta praevia (a low-lying placenta) or if your twins share a placenta.
If you have previously had a very difficult delivery with a single baby, you may be advised to have a caesarean section with twins. Even if you plan a vaginal birth, you may end up having an emergency caesarean section.
Even if you plan a vaginal birth, you may end up having an emergency caesarean section.
This could be because:
- one or both babies become distressed
- the umbilical cord prolapses (falls into the birth canal ahead of the baby)
- your blood pressure is going up
- the labour is progressing too slowly
- assisted delivery doesn't work
In very rare cases, you may deliver one twin vaginally and then require a caesarean section to deliver the second twin if it becomes distressed.
After the birth
After the birth, your midwife will examine the placenta to determine what type of twins you have. Twins can either be fraternal or identical.
If your babies need special care
Depending on where you plan to give birth, you may need to go to another hospital with appropriate facilities if complications in your pregnancy indicate you're likely to have an early delivery. This may not be near to home, so make sure to check there are enough beds for both your babies in the neonatal unit.
Ask if your chosen hospital has a transitional care unit or a special care nursery. These are places that allow mothers to care for their babies if they need special care but not intensive care. These hospitals are more likely to be able to keep you and your babies in the same place.
You might also want to ask if your hospital has cots that allow co-bedding (where your babies sleep in a single cot), if this is appropriate and if you want your babies to sleep together.
If you have one baby in the hospital and one at home, you will need to think about splitting your time between the two. When you visit your baby in hospital, ask if you can bring their twin and if co-bedding is allowed during visits.
If you want to breastfeed and only one twin can feed effectively, you may need to express milk to feed the twin who is having trouble feeding. You may then need to put the twin who can feed on the breast to encourage milk production in order to get enough milk to feed both babies.
Check if your hospital offers support from a community neonatal nurse, which would allow for you and your babies to leave hospital earlier, for example if your baby is still tube-fed.
When you go to clinics for follow-up appointments, it's a good idea to ask not to be booked into early morning appointments. Getting out of the house with two babies, particularly if one is unwell, can be difficult.
For more information and support, visit Twins Research Australia.
Learn more here about the development and quality assurance of healthdirect content.
Birth of twins: what is the probability? | PHARMACY
Twins or dizygotic twins are born when 2 different eggs are fertilized by 2 different sperm at the same time. Identical twins, or homozygous twins, give birth if 1 egg is fertilized by 1 sperm and then divides, forming 2 embryos. Identical twin births occur around the world with approximately the same frequency of 3-4 cases per 1000 births, the frequency of birth of dizygotic twins varies significantly around the world, from 6 cases per 1000 births in Asia to 40 cases per 1000 births in Africa. nine0003
nine0003
Scientists believe that the birth of twins is based on a genetic component, but the details of this relationship have not previously been sufficiently studied. In a new study, scientists from the Free University of Amsterdam (Vrije Universiteit), the Netherlands, have identified 2 gene variants associated with the birth of dizygotic twins.
The results of the study are relevant for the European population, since the population of Asia and Africa may have additional gene variants, scientists note. nine0003
Until now, researchers have not been able to analyze in detail some of the factors that likely increase a woman's chances of having twins. For example, women who became mothers in adulthood and those who had relatives who gave birth to twins were more likely to have dizygotic twins than other females. Therefore, the researchers decided to analyze the genes responsible for the birth of twins. They started by collecting genetic information from databases in the Netherlands, Australia, and the United States. As a result, they identified 1980 mothers of twins conceived without infertility treatment and compared their genome with that of 12,953 women from the control group who did not give birth to dizygotic twins.
As a result, they identified 1980 mothers of twins conceived without infertility treatment and compared their genome with that of 12,953 women from the control group who did not give birth to dizygotic twins.
After searching for and isolating the genetic variants that distinguish mothers from the two groups, the scientists sent the results to their colleagues in Iceland, who conducted a similar study on 3,597 mothers who gave birth to dizygotic twins and 297,348 women from the control group.
This allowed us to identify 2 gene variants that appeared more often in mothers of twins than in mothers who gave birth to 1 child. One gene variant is associated with increased levels of follicle-stimulating hormone (FSH) in women, and also plays an important role in reproductive function in men. FSH stimulates a woman's ovaries to release an egg. Its elevated level can lead to the simultaneous release of several eggs from the ovaries, which can subsequently lead to the fertilization of 2 eggs at once and the birth of twins. nine0003
nine0003
The second variant of the SMAD3 gene is involved in cell signaling and, according to the researchers, likely plays a role in how a woman's body responds to FSH. If a woman's ovaries are sensitive to FSH, this can lead to the release of several eggs at once and their subsequent fertilization, even if her body produces FSH in moderate amounts.
Interestingly, the presence of the first gene variant in a woman increases the relative probability of having twins by 18%, and the second - by 9%. The combination of these gene variants increases the chances of having twins by 29%.
Scientists note that these 2 gene variants do not show the full picture of the influence of the genome on the birth of twins, perhaps in the future additional genes will be identified that play a role in this process.
Adapted from www.medicaldaily.com
Induction heating, basic principles and technologies.
August 1, 2013
Induction heating is a method of non-contact heating by high-frequency currents (eng. RFH - radio-frequency heating, heating by radio-frequency waves) of electrically conductive materials. nine0003
RFH - radio-frequency heating, heating by radio-frequency waves) of electrically conductive materials. nine0003
Description of the method.
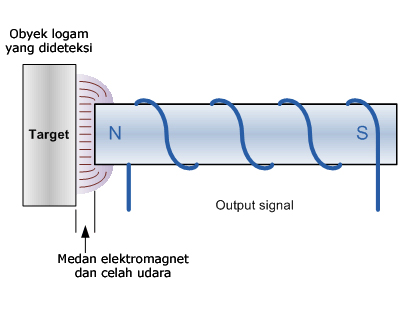
Induction heating is the heating of materials by electric currents that are induced by an alternating magnetic field. Therefore, this is the heating of products made of conductive materials (conductors) by the magnetic field of inductors (sources of an alternating magnetic field). Induction heating is carried out as follows. An electrically conductive (metal, graphite) workpiece is placed in the so-called inductor, which is one or more turns of wire (most often copper). Powerful currents of various frequencies (from tens of Hz to several MHz) are induced in the inductor using a special generator, as a result of which an electromagnetic field arises around the inductor. The electromagnetic field induces eddy currents in the workpiece. Eddy currents heat the workpiece under the action of Joule heat (see the Joule-Lenz law). nine0003
The inductor-blank system is a coreless transformer in which the inductor is the primary winding. The workpiece is a secondary winding short-circuited. The magnetic flux between the windings closes in air.
The workpiece is a secondary winding short-circuited. The magnetic flux between the windings closes in air.
At high frequency, eddy currents are displaced by the magnetic field formed by them into thin surface layers of the workpiece Δ (Surface-effect), as a result of which their density increases sharply, and the workpiece is heated. The underlying layers of the metal are heated due to thermal conductivity. It is not the current that is important, but the high current density. In the skin layer Δ, the current density decreases by a factor of e relative to the current density on the workpiece surface, while 86.4% of heat is released in the skin layer (of the total heat release. The depth of the skin layer depends on the radiation frequency: the higher the frequency, the thinner skin layer It also depends on the relative magnetic permeability μ of the workpiece material.0003
For iron, cobalt, nickel and magnetic alloys at temperatures below the Curie point, μ has a value from several hundreds to tens of thousands. For other materials (melts, non-ferrous metals, liquid low-melting eutectics, graphite, electrolytes, electrically conductive ceramics, etc.), μ is approximately equal to one.
For other materials (melts, non-ferrous metals, liquid low-melting eutectics, graphite, electrolytes, electrically conductive ceramics, etc.), μ is approximately equal to one.
For example, at a frequency of 2 MHz, the skin depth for copper is about 0.25 mm, for iron ≈ 0.001 mm.
The inductor gets very hot during operation, as it absorbs its own radiation. In addition, it absorbs heat radiation from a hot workpiece. They make inductors from copper tubes cooled by water. Water is supplied by suction - this ensures safety in case of a burn or other depressurization of the inductor. nine0003
Application:
Ultra-clean non-contact melting, brazing and metal welding.
Obtaining experimental samples of alloys.
Bending and heat treatment of machine parts.
Jewelry business.
Machining small parts that can be damaged by flame or arc heating.
Surface hardened.
Hardening and heat treatment of parts with complex shapes.
Decontamination of medical instruments.
Benefits.
High speed heating or melting of any electrically conductive material. nine0003
Can be heated under protective gas, in oxidizing (or reducing) media, in non-conductive liquids, in vacuum.
Heating through the walls of a protective chamber made of glass, cement, plastics, wood - these materials absorb electromagnetic radiation very weakly and remain cold during operation of the installation. Only electrically conductive material is heated - metal (including molten), carbon, conductive ceramics, electrolytes, liquid metals, etc.
Due to the emerging MHD forces, the liquid metal is intensively mixed, up to keeping it suspended in air or protective gas - this is how ultrapure alloys are obtained in small quantities (levitation melting, melting in an electromagnetic crucible).
Since the heating is carried out by means of electromagnetic radiation, there is no contamination of the workpiece with the combustion products of the torch in the case of gas flame heating, or the electrode material in the case of arc heating. Placing the samples in an inert gas atmosphere and a high heating rate will eliminate scale formation. nine0003
Placing the samples in an inert gas atmosphere and a high heating rate will eliminate scale formation. nine0003
Ease of use due to the small size of the inductor.
The inductor can be made in a special shape - this will allow uniform heating over the entire surface of parts of complex configuration, without leading to warping or local non-heating.
Easy to carry out local and selective heating.
Since the most intense heating occurs in the thin upper layers of the workpiece, and the underlying layers are heated more gently due to thermal conductivity, the method is ideal for surface hardening of parts (the core remains viscous). nine0003
Easy automation of equipment - heating and cooling cycles, temperature control and holding, feeding and removal of workpieces.
Induction Heating Units:
Units operating up to 300 kHz use IGBT or MOSFET inverters. Such installations are designed for heating large parts. To heat small parts, high frequencies are used (up to 5 MHz, the range of medium and short waves), high-frequency installations are built on electronic tubes. nine0003
nine0003
Also, for heating small parts, high-frequency installations are built on MOSFET transistors for operating frequencies up to 1.7 MHz. Controlling and protecting transistors at higher frequencies presents certain difficulties, so higher frequency settings are still quite expensive.
The inductor for heating small parts is small and has low inductance, which leads to a decrease in the quality factor of the working resonant circuit at low frequencies and a decrease in efficiency, and also poses a danger to the master oscillator (the quality factor of the resonant circuit is proportional to L/C, the resonant circuit with low quality factor too well "pumped" with energy, forms a short circuit along the inductor and disables the master oscillator). To increase the quality factor of the oscillatory circuit, two ways are used:
- increasing the operating frequency, which leads to the complexity and cost of the installation;
- the use of ferromagnetic inserts in the inductor; pasting the inductor with panels of ferromagnetic material.
Since the inductor works most efficiently at high frequencies, induction heating received industrial application after the development and start of production of powerful generator lamps. Prior to World War I, induction heating was of limited use. At that time, high-frequency machine generators (works by V.P. Vologdin) or spark discharge installations were used as generators. nine0003
The oscillator circuit can in principle be any (multivibrator, RC oscillator, independently excited oscillator, various relaxation oscillators) operating on a load in the form of an inductor and having sufficient power. It is also necessary that the oscillation frequency be sufficiently high.
For example, to "cut" a steel wire with a diameter of 4 mm in a few seconds, an oscillatory power of at least 2 kW at a frequency of at least 300 kHz is required.
Choose a circuit according to the following criteria: reliability; fluctuation stability; stability of the power released in the workpiece; ease of manufacture; ease of setup; minimum number of parts to reduce cost; the use of parts that in total give a reduction in weight and dimensions, etc.
For many decades, an inductive three-point generator (Hartley generator, generator with autotransformer feedback, circuit on an inductive loop voltage divider) has been used as a generator of high-frequency oscillations. This is a self-excited parallel power supply circuit for the anode and a frequency-selective circuit made on an oscillatory circuit. It has been successfully used and continues to be used in laboratories, jewelry workshops, industrial enterprises, as well as in amateur practice. For example, during the Second World War, surface hardening of the rollers of the T-34 tank was carried out on such installations. nine0003
Disadvantages of three points:
Low efficiency (less than 40% when using a lamp).
Strong frequency deviation at the moment of heating workpieces made of magnetic materials above the Curie point (≈700С) (μ changes), which changes the depth of the skin layer and unpredictably changes the heat treatment mode. When heat treating critical parts, this may be unacceptable. Also, powerful RF installations must operate in a narrow range of frequencies allowed by Rossvyazokhrankultura, since with poor shielding they are actually radio transmitters and can interfere with television and radio broadcasting, coastal and rescue services. nine0003
Also, powerful RF installations must operate in a narrow range of frequencies allowed by Rossvyazokhrankultura, since with poor shielding they are actually radio transmitters and can interfere with television and radio broadcasting, coastal and rescue services. nine0003
When blanks are changed (for example, from a smaller to a larger one), the inductance of the inductor-blank system changes, which also leads to a change in the frequency and depth of the skin layer.
When changing from single-turn to multi-turn, larger or smaller inductors, the frequency also changes.
Under the leadership of Babat, Lozinsky and other scientists, two- and three-circuit generator circuits were developed that have a higher efficiency (up to 70%), and also better keep the operating frequency. The principle of their action is as follows. Due to the use of coupled circuits and the weakening of the connection between them, a change in the inductance of the working circuit does not entail a strong change in the frequency of the frequency setting circuit.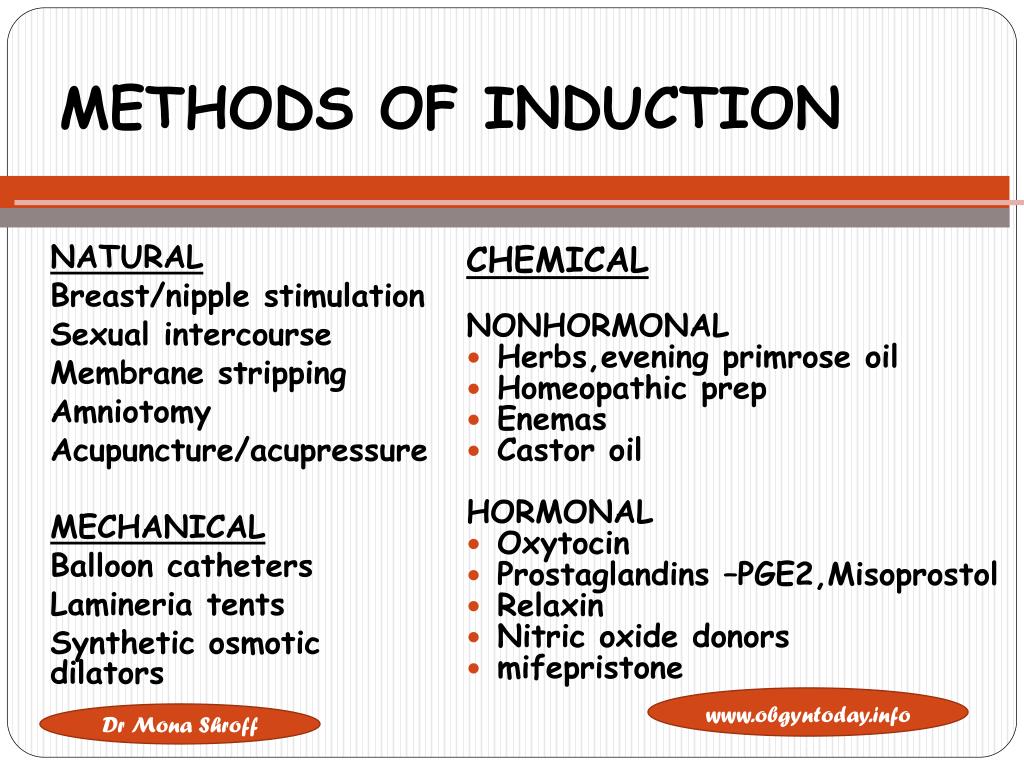 Radio transmitters are constructed according to the same principle. nine0003
Radio transmitters are constructed according to the same principle. nine0003
The disadvantage of multi-circuit systems is the increased complexity and the occurrence of parasitic oscillations in the VHF band, which uselessly dissipate power and disable the elements of the installation. Also, such installations are prone to delaying oscillations - a spontaneous transition of the generator from one of the resonant frequencies to another.
Modern high-frequency generators are inverters based on IGBT assemblies or high-power MOSFET transistors, usually made according to the bridge or half-bridge scheme. Operate at frequencies up to 500 kHz. The gates of the transistors are opened using a microcontroller control system. The control system, depending on the task, allows you to automatically hold
a) constant frequency
b) constant power dissipated in the workpiece
c) maximum efficiency.
For example, when a magnetic material is heated above the Curie point, the thickness of the skin layer increases sharply, the current density drops, and the workpiece begins to heat up worse. The magnetic properties of the material also disappear and the magnetization reversal process stops - the workpiece begins to heat up worse, the load resistance abruptly decreases - this can lead to the "spacing" of the generator and its failure. The control system monitors the transition through the Curie point and automatically increases the frequency with an abrupt decrease in load (or reduces power). nine0003
The magnetic properties of the material also disappear and the magnetization reversal process stops - the workpiece begins to heat up worse, the load resistance abruptly decreases - this can lead to the "spacing" of the generator and its failure. The control system monitors the transition through the Curie point and automatically increases the frequency with an abrupt decrease in load (or reduces power). nine0003
Remarks.
The inductor should be positioned as close to the workpiece as possible. This not only increases the electromagnetic field density near the workpiece (in proportion to the square of the distance), but also increases the power factor Cos(φ).
Increasing the frequency dramatically reduces the power factor (in proportion to the cube of the frequency).
When magnetic materials are heated, additional heat is also released due to magnetization reversal; their heating to the Curie point is much more efficient. nine0003
When calculating the inductor, it is necessary to take into account the inductance of the tires leading to the inductor, which can be much greater than the inductance of the inductor itself (if the inductor is made in the form of a single turn of a small diameter or even part of a turn - an arc).
There are two cases of resonance in oscillatory circuits: voltage resonance and current resonance.
Parallel oscillatory circuit - resonance of currents.
In this case, the voltage on the coil and on the capacitor is the same as that of the generator. At resonance, the resistance of the circuit between the branching points becomes maximum, and the current (I total) through the load resistance Rn will be minimal (the current inside the circuit I-1l and I-2s is greater than the generator current). nine0003
Ideally, the loop impedance is infinite - the circuit draws no current from the source. When the frequency of the generator changes in any direction from the resonant frequency, the impedance of the circuit decreases and the linear current (Itot) increases.
Series oscillatory circuit - voltage resonance.
The main feature of the series resonant circuit is that its impedance is minimal at resonance. (ZL + ZC - minimum). When the frequency is tuned to a value above or below the resonant frequency, the impedance increases.