Induced during pregnancy
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).
- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
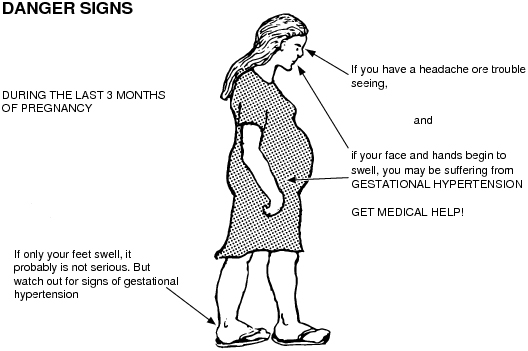
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).

- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
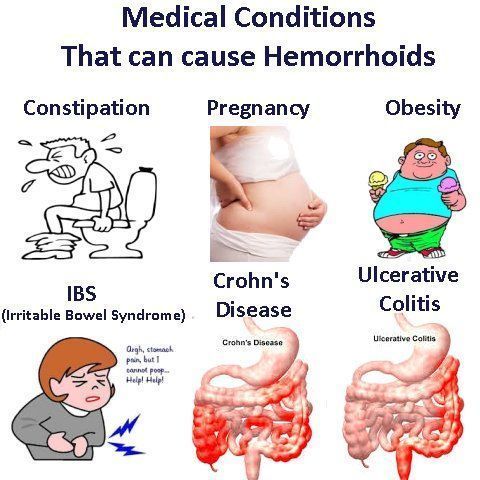
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.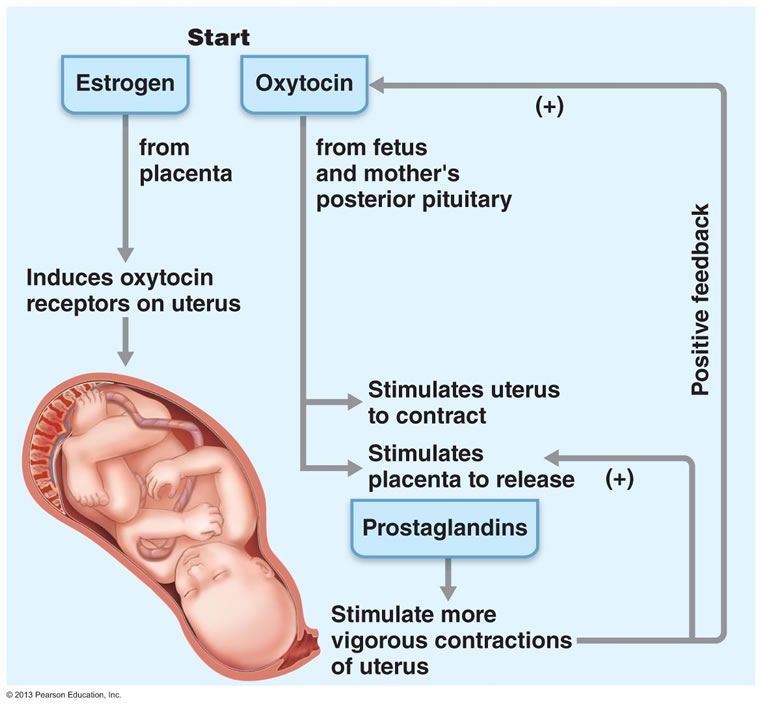 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.

- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery. Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
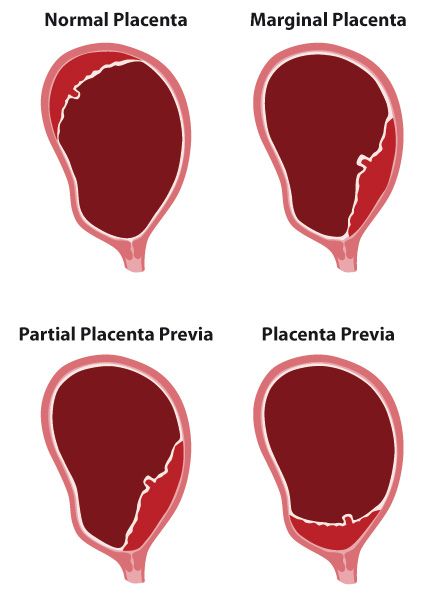
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.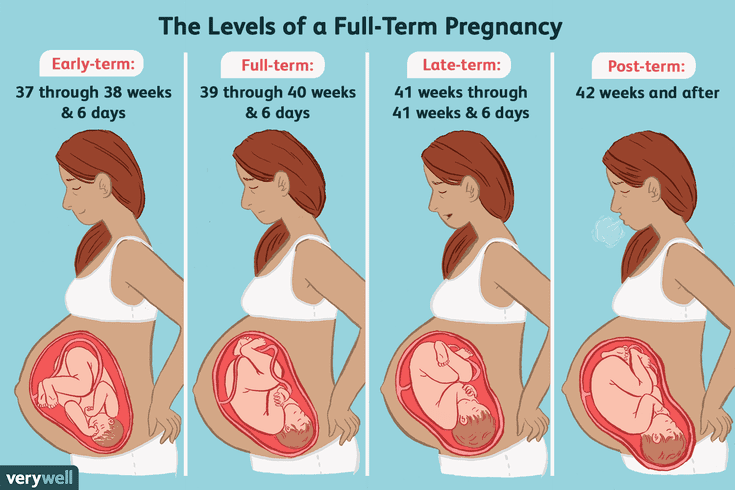
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
Induced labour | Pregnancy Birth and Baby
What is an induced labour?
Labour normally starts naturally any time between 37 and 42 weeks of pregnancy. The cervix softens and starts to open, you will get contractions, and your waters break.
In an induced labour, or induction, these labour processes are started artificially. It might involve mechanically opening your cervix, breaking your waters, or using medicine to start off your contractions — or a combination of these methods.
In Australia, about 1 in 3 women has an induced labour.
What are the differences between an induced and a natural labour?
An induced labour can be more painful than a natural labour. In natural labour, the contractions build up slowly, but in induced labour they can start more quickly and be stronger. Because the labour can be more painful, you are more likely to want some type of pain relief.
If your labour is induced, you are also more likely to need other interventions, such as the use of forceps or ventouse (vacuum) to assist with the birth of your baby. You will not be able to move around as much because the baby will be monitored more closely than during a natural labour.
You will only be offered induced labour if there is a risk to you or your baby's health. Your doctor might recommend induced labour if:
- you are overdue (more than 41 weeks pregnant)
- there is a concern the placenta is not working as it should
- you have a health condition, such as diabetes, kidney problems, high blood pressure or pre-eclampsia
- the baby is making fewer movements, showing changes in its heart rate, or not growing well
- your waters have broken, but the contractions have not started naturally
- you are giving birth to more than one baby (twins or multiple birth)
Not everyone can have an induced labour.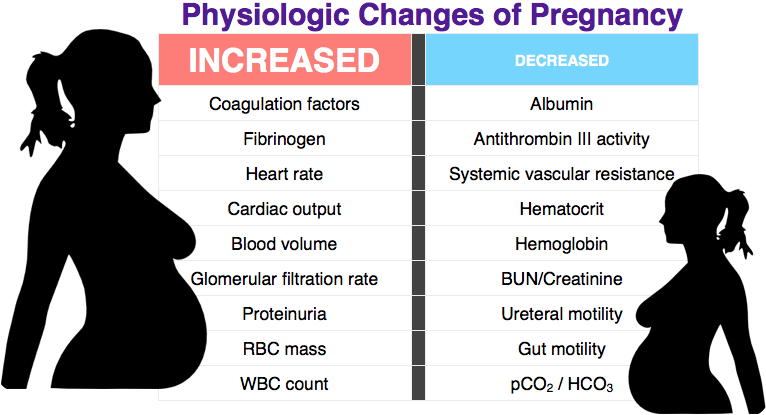 It is not usually an option if you have had a caesarean section or major abdominal surgery before, if you have placenta praevia, or if your baby is breech or lying sideways.
It is not usually an option if you have had a caesarean section or major abdominal surgery before, if you have placenta praevia, or if your baby is breech or lying sideways.
Can I decide whether to have an induced labour?
If you are overdue, you might decide to wait and see if labour will start naturally. However, if there is a chance you or your baby are at risk of complications, you might need to consider induced labour before your due date.
When making your decision, discuss the risks and benefits with your doctor. Do not be afraid to ask lots of questions, such as:
- Why do I need an induction?
- How will it affect me and my baby?
- What will happen if I do not have the induction?
- What procedures are involved and how will you care for me and my baby?
You might need to consider several other health concerns. For example, there is a higher risk of stillbirth or other problems if your baby is not born before 42 weeks, and an increased risk of infection if your waters break more than 24 hours before labour starts.
What can I expect with an induced labour?
During the late stages of your pregnancy, your healthcare team will carry out regular checks on your health and your baby's heath. These checks help them decide whether it is better to induce labour or to keep the baby inside. Always tell your doctor or midwife if you notice your baby is moving less than normal.
If they decide it is medically necessary to induce labour, first your doctor or midwife will do an internal examination by feeling inside your vagina. They will feel your cervix to see if it is ready for labour. This examination will also help them decide on the best method for you.
It can take from a few hours to as long as 2 to 3 days to induce labour. It depends how your body responds to the treatment. It is likely to take longer if this is your first pregnancy or you are less than 37 weeks pregnant.
What options are there to induce labour?
There are different ways to induce labour. Your doctor or midwife will recommend the best method for you when they examine your cervix. You may need a combination of different strategies. You will need to provide written consent for the procedure.
You may need a combination of different strategies. You will need to provide written consent for the procedure.
Sweeping the membranes
During a vaginal examination, the midwife or doctor makes circular movements around your cervix with their finger. This action should release a hormone called prostaglandins. You do not need to be admitted to hospital for this procedure and it is often done in the doctor's room. This can be enough to get labour started, meaning you will not need any other methods.
Risks: This is a simple and easy procedure; however, it does not always work. It can be a bit uncomfortable, but it does not hurt.
Oxytocin
A synthetic version of the hormone oxytocin is given to you via a drip in your arm to start your contractions. When the contractions start, the amount of oxytocin is adjusted so you keep on having regular contractions until the baby is born. This whole process can take several hours.
Risks: Oxytocin can make contractions stronger, more frequent and more painful than in natural labour, so you are more likely to need pain relief. You will not be able to move around much because of the drip in your arm and you will also have a fetal monitor around your abdomen to monitor your baby.
You will not be able to move around much because of the drip in your arm and you will also have a fetal monitor around your abdomen to monitor your baby.
Sometimes the contractions can come too quickly, which can affect the baby's heart rate. This can be controlled by slowing down the drip or giving you another medicine.
Artificial rupture of membranes ('breaking your waters')
Artificial rupture of membranes (ARM) is used when your waters do not break naturally. Your doctor or midwife inserts a small hook-like instrument through your vagina to make a hole in the membrane sac that is holding the amniotic fluid. This will increase the pressure of your baby's head on your cervix, which may be enough to get labour started. Many women will also need oxytocin to start their contractions.
Risks: ARM can be a bit uncomfortable but not painful. There is a small increased risk of a prolapsed umbilical cord, bleeding or infection.
Prostaglandins
A synthetic version of the hormone prostaglandins is inserted into your vagina to soften your cervix and prepare your body for labour. It can be in the form of a gel, which may be given in several doses (usually every 6 to 8 hours), or a pessary and tape (similar to a tampon), which slowly releases the hormone over 12 to 24 hours. You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
It can be in the form of a gel, which may be given in several doses (usually every 6 to 8 hours), or a pessary and tape (similar to a tampon), which slowly releases the hormone over 12 to 24 hours. You will need to lie down and stay in hospital after the prostaglandins is inserted. You may also then need ARM if your waters have not broken, or oxytocin to bring on the contractions.
Prostaglandins gel is often the preferred method of inducing labour since it is the closest to natural labour. Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
Risks: Some women find their vagina is sore after the prostaglandin gel, or they might experience nausea, vomiting or diarrhoea. These side effects are rare and there is no evidence that induction using prostaglandin is any more painful than a natural labour.
Very rarely, the contractions can come too strongly, which can affect the baby's heart rate. This can be controlled by giving you another medicine or removing the pessary.
You need to let your doctor or midwife know immediately if you start bleeding, or if your baby is moving less, because this could be a sign that something is wrong.
Cervical ripening balloon catheter
A cervical ripening balloon catheter is a small tube attached to a balloon that is inserted into your cervix. The balloon is inflated with saline, which usually puts enough pressure on your cervix for it to open. It stays in place for up to 15 hours, and then you will be examined again.
Tell your midwife or doctor straight away if you start to experience painful, regular contractions 5 minutes apart for your first baby, or 10 minutes apart for subsequent babies, or if your waters break, because these are both signs that your labour is beginning.
You may also need ARM or oxytocin if you are using a cervical ripening balloon catheter.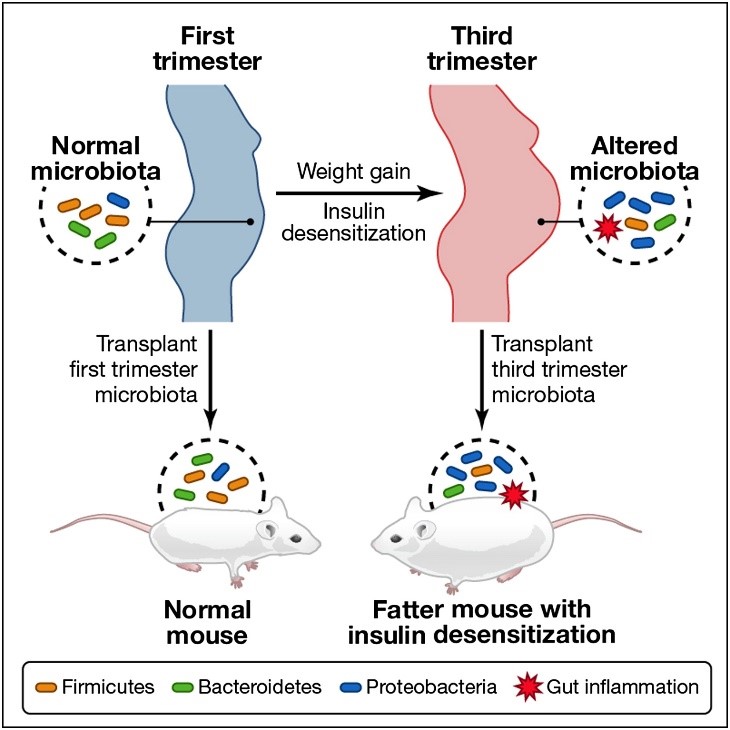
Risks: Inserting the catheter can be a bit uncomfortable but not painful.
You also need to let your doctor or midwife know immediately if you start bleeding, or your baby is moving less, because this could be a sign that something is wrong.
Can I have pain relief during induced labour?
Induced labour is usually more painful than natural labour. Depending on the type of induction you are having, this could range from discomfort with the procedure or more intense and longer lasting contractions as a result of the medication you have been given. Women who have induced labour are more likely to ask for an epidural for relief.
Because inductions are almost always done in hospital, the full range of pain relief should be available to you. There is usually no restriction on the type of pain relief you can have if your labour is induced.
Are there any risks with inducing labour?
There are some increased risks if you have an induced labour. These include that:
These include that:
- it will not work — in about 1 of 4 cases, women go on to have a caesarean
- your baby will not get enough oxygen and their heart rate is affected
- you or your baby get an infection
- your uterus tears
- you bleed a lot after the birth
What happens if the induction does not work?
Not all induction methods will work for everyone. Your doctor may try another method, or you might need to have a caesarean. Your doctor will discuss all of these options with you.
Learn more here about the development and quality assurance of healthdirect content.
Obstetrics and Gynecology Modern pathogenetic mechanisms for the development of a severe form of ovarian hyperstimulation syndrome, clinical and laboratory characteristics of pregnant women during the manifestation of the syndrome, as well as features of the course and management induced pregnancy, which occurred against the background of a severe form of the syndrome.
The widespread introduction of assisted reproductive technologies into clinical practice has led to an increase in the proportion of induced pregnancies that have a complicated course. According to the World Congress "Fertility and Infertility", every fifth induced pregnancy is terminated before 20 weeks, every third pregnancy ends in premature birth in the period from 24 to 36 weeks. At the same time, the main range of complications is associated with ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies [2, 3]. nine0003
Ovarian hyperstimulation syndrome is an iatrogenic complication of assisted reproductive technology cycles. Currently, it is defined as a systemic disease that develops as a result of activation of the production of vasoactive mediators by the ovaries against the background of stimulation of their function. The complication develops in the luteal phase of the cycle or early in pregnancy.
Substantiation of management tactics for pregnant women with OHSS is impossible without understanding the pathogenetic mechanisms of the development of the pathological process. However, these questions have not been fully resolved. In the recent literature, the role of a specific mutation of the follicle-stimulating hormone receptor genes is discussed, as a result of which sensitivity to chorionic gonadotropin (CG) increases, which leads to excessive stimulation of granulosa cell receptors and, as a result, intensive growth and development of follicles [6]. nine0003
However, these questions have not been fully resolved. In the recent literature, the role of a specific mutation of the follicle-stimulating hormone receptor genes is discussed, as a result of which sensitivity to chorionic gonadotropin (CG) increases, which leads to excessive stimulation of granulosa cell receptors and, as a result, intensive growth and development of follicles [6]. nine0003
In recent years, parallels have been drawn in the literature between OHSS and systemic inflammatory response syndrome (SIRS), since the development of this iatrogenic condition is accompanied by a pronounced reaction of the immune system. In the blood plasma and peritoneal fluid of patients with OHSS, high levels of pro-inflammatory vasoactive markers are determined [8], against which the parameters of hemostasis deteriorate sharply, predetermining the development of disseminated intravascular coagulation (DIC) and a high risk of thromboembolic complications. It is known that the successful course and outcome of pregnancy largely depend on the processes of
implantation and placentation. According to modern concepts, the stages of egg maturation, implantation, and embryo development are cytokine-dependent processes and are controlled by the immune system. Embryo implantation and the course of physiological pregnancy are associated with a shift in the cytokine balance towards the dominance of factors with immunosuppressive
According to modern concepts, the stages of egg maturation, implantation, and embryo development are cytokine-dependent processes and are controlled by the immune system. Embryo implantation and the course of physiological pregnancy are associated with a shift in the cytokine balance towards the dominance of factors with immunosuppressive
activity. One of the causes of cytokine imbalance is a change in the ratio of T-helper (Th) cells. With a normally developing pregnancy, starting from the early
terms, regulatory Th3 cytokines predominate in the blood, which block the reactions of cellular immunity, promote the development and invasion of the trophoblast, and also stimulate steroidogenesis [2, 4].
In case of OHSS, unfavorable conditions for implantation and further development of the embryo, consisting in a high level of biologically active substances, generalized damage to the endothelium, and electrolyte imbalance disrupt normal intercellular interactions, cause defective implantation, and can lead to spontaneous termination of pregnancy in the early stages. Systemic coagulopathy that accompanies OHSS and SIRS can also disrupt the implantation process and manifest in the future the development of placental insufficiency, since the depth of trophoblast invasion into the spiral arteries decreases due to impaired fusion of syncytium. In addition, an increase in the level of pro-inflammatory cytokines leads to an increase in the synthesis of prostaglandins by the amniotic membranes and the development of a number of
Systemic coagulopathy that accompanies OHSS and SIRS can also disrupt the implantation process and manifest in the future the development of placental insufficiency, since the depth of trophoblast invasion into the spiral arteries decreases due to impaired fusion of syncytium. In addition, an increase in the level of pro-inflammatory cytokines leads to an increase in the synthesis of prostaglandins by the amniotic membranes and the development of a number of
complications: chorioamnionitis, placental abruption, premature rupture of amniotic fluid, chronic DIC.
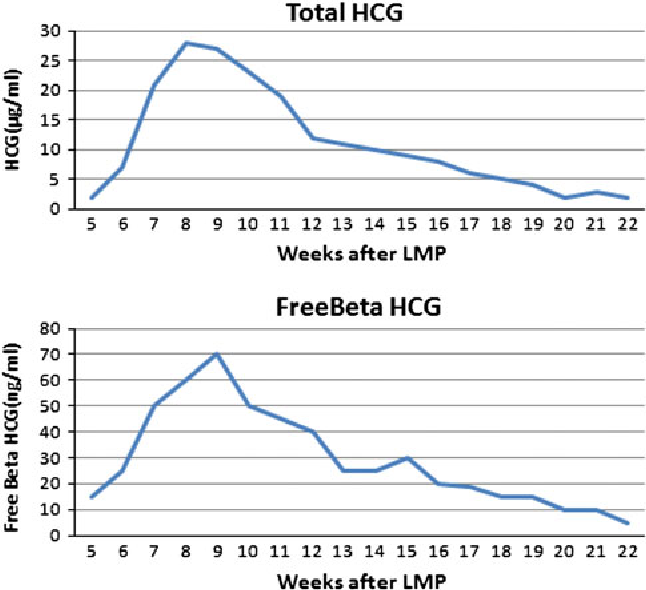
The features of the clinical picture of OHSS, manifesting most often on days 12–14 after the administration of an ovulatory dose of CG, are pronounced hemoconcentration and hypovolemia at hematocrit levels ≥45%; leukocytes ≥16 109/l; platelets ≥445´109/l; ESR ≥15.1 mm/h. Leukocytosis in OHSS is caused by both blood clotting and the body's response to the release of pro-inflammatory cytokines into the systemic circulation. nine0003
nine0003
Functional disorders of the liver accompany the course of OHSS in more than 50% of cases and are manifested by an increase in transaminase levels by 3.5 times, which exceeds similar indicators not only in spontaneous pregnancy, but also in induced pregnancy without signs of OHSS. Such changes are associated with the formation of microthrombi due to ischemia and damage to the vascular endothelium mediated by interleukin-6. The transition of plasma proteins from the vascular bed to the "third space" against the background of a decrease in the protein-synthesizing function of the liver manifests itself in the form of hypoproteinemia (<50 g/l) and hypoalbuminemia (<27 g/l). nine0003
An increase in the thrombogenic potential of the blood is primarily due to the activation of the procoagulant link of hemostasis. The marker of these disorders is the level of fibrinogen, which is 2 times higher than the similar value in spontaneous pregnancy, which is considered as a risk factor for the development of vascular disorders and an indicator of the acute phase of inflammation.
The activation of the vascular-platelet link of hemostasis is indicated by an increase in the number of platelets, as well as the concentration of von Willebrand factor, a marker of endothelial cell activation, which is almost 3 times higher than the values characteristic of spontaneous pregnancy and 2.5 times higher than the values for induced pregnancy without the presence of the syndrome . These disorders are realized through the development of the current DIC, the laboratory reflection of which is an increase in the concentration of D-dimer (a marker of thrombinemia) by more than 10 times compared with the normative values during spontaneous pregnancy and the depletion of the anticoagulant link of hemostasis (decrease in the activity of the natural anticoagulant antithrombin III). nine0003
It should be noted that the indicators of activated partial thromboplastin time, prothrombin index and international normalized ratio are within the normal range.
All described changes reach their peak in the first days of implantation and development of pregnancy. By 14 weeks of pregnancy, against the background of heparin therapy, the anticoagulant and procoagulant links of hemostasis are completely restored. The only exceptions are the levels of D-dimer and von Willebrand factor, which, despite their slight decrease in dynamics, still remain high, which indicates persistent systemic changes in the endothelium. nine0003
By 14 weeks of pregnancy, against the background of heparin therapy, the anticoagulant and procoagulant links of hemostasis are completely restored. The only exceptions are the levels of D-dimer and von Willebrand factor, which, despite their slight decrease in dynamics, still remain high, which indicates persistent systemic changes in the endothelium. nine0003
Since D-dimer is a marker of pathological activation of hemostasis and intravascular microthrombosis, it can be assumed that pronounced changes in this parameter in combination with hyperfibrinogenemia, a decrease in antithrombin III, and a simultaneous increase in the concentration of von Willebrand factor create unfavorable conditions during implantation and embryogenesis, leading to microthrombosis of spiral arteries. After all, it is known that pathological activation of hemostasis is not typical for the first trimester of physiological pregnancy. nine0003
Another biological marker, a classic acute phase protein synthesized by the liver in response to inflammation and tissue damage, is C-reactive protein. The active participation of this protein, together with cytokines, in a nonspecific systemic inflammatory response has been proven [1]. In patients with OHSS during the period of manifestation of the syndrome, the concentration of this protein is tens of times higher than the normative data in spontaneous pregnancy and 4 times in pregnant women without the syndrome. The pathogenesis of microthrombosis in the chorionic villi in pregnant women with OHSS is partially associated with the level of C-reactive protein. nine0003
The active participation of this protein, together with cytokines, in a nonspecific systemic inflammatory response has been proven [1]. In patients with OHSS during the period of manifestation of the syndrome, the concentration of this protein is tens of times higher than the normative data in spontaneous pregnancy and 4 times in pregnant women without the syndrome. The pathogenesis of microthrombosis in the chorionic villi in pregnant women with OHSS is partially associated with the level of C-reactive protein. nine0003
Systemic changes in the body in OHSS, along with multiple organ disorders, lead to a weakening of the barrier functions of the epithelium of the mucous membranes and the translocation of microorganisms from traditional biotopes to sterile tissues. There is an activation of opportunistic microorganisms with the development of infections of the urogenital tract and dysbiotic processes in the vagina in every
fourth pregnant woman, including true bacteriuria in titers of 5–6 lg CFU / ml in 10. 6%. It is important to note that these women were carefully examined for the presence of infection before treatment in assisted reproductive technology programs, and before the development of OHSS, their vaginal microcenosis corresponded to the age norm. nine0003
6%. It is important to note that these women were carefully examined for the presence of infection before treatment in assisted reproductive technology programs, and before the development of OHSS, their vaginal microcenosis corresponded to the age norm. nine0003
The described pathological changes convincingly demonstrate that during the manifestation of OHSS the embryo is in "extreme" conditions of existence: hypovolemia, deficiency of proteins as the main building material, development of SIRS and activation of coagulation with subsequent incomplete restructuring of the spiral arteries eventually lead to ischemia, the development of circulatory hypoxia in tissues, acidosis, disruption of the energy and plastic supply of cells in the most vulnerable periods of embryonic development. Polymorphism of thrombophilia genes and activation of opportunistic flora against the background of immune imbalance, even with successful implantation, create additional conditions for a complicated course of pregnancy. nine0003
nine0003
Pregnancies that occur against the background of OHSS end in timely delivery in 47.1% of cases, premature delivery in 22.9%. In the first trimester, 45.5% of pregnant women have a low attachment of the chorion, in every 3-4 cases - chorion hypoplasia with signs of inflammation (deciduitis), which is 4.5 times higher than in pregnant women without signs of OHSS. Chorionic detachment up to 12 weeks is diagnosed in every fourth patient with OHSS. It is known that during an induced multiple pregnancy in the first trimester, a spontaneous stop in the development of one or more embryos may occur (self-reduction, "vanishing twin"). This phenomenon is 2.5 times more common in women with OHSS. The frequency of early fetal losses in this category of pregnant women is three times higher than in spontaneous pregnancy. nine0003
The second trimester of pregnancy, which occurred against the background of OHSS, proceeds with the phenomena of threatened abortion in 38%, anemia - in 29%, isthmic-cervical insufficiency - in 25%, placental abruption - in 11%.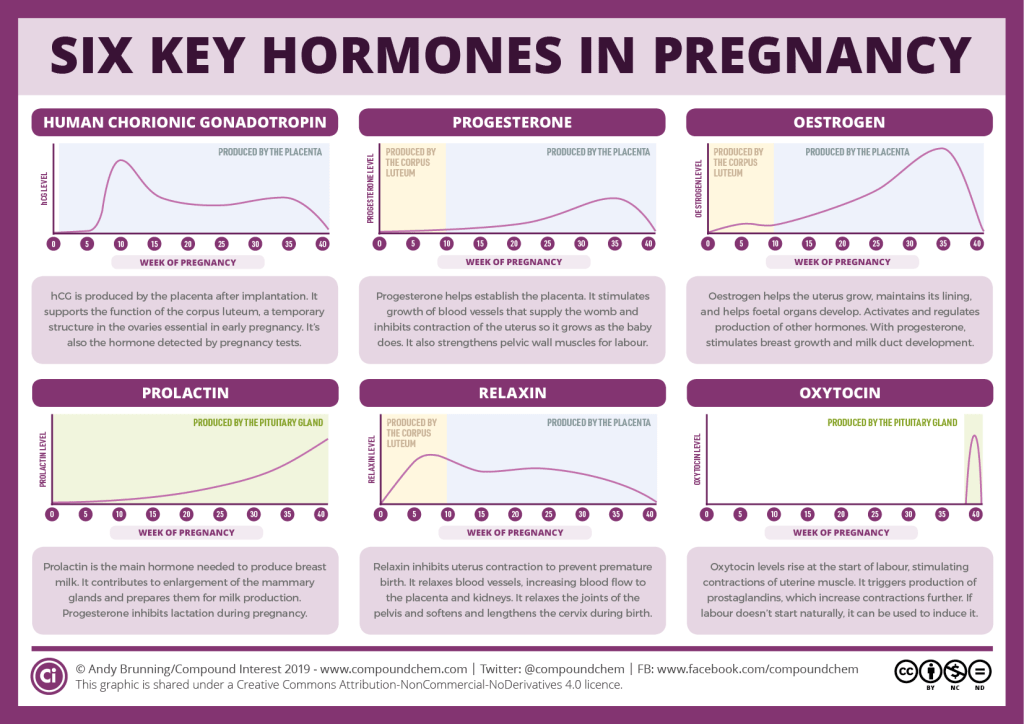 In the genesis of isthmic-cervical insufficiency, the main role is played by multiple pregnancies, the frequency of which in this category of patients is 35%.
In the genesis of isthmic-cervical insufficiency, the main role is played by multiple pregnancies, the frequency of which in this category of patients is 35%.
The course of the third trimester of pregnancy in every third woman is characterized by the development of fetoplacental insufficiency, the formation of which is preceded by chronic DIC, caused by an increased level of pro-inflammatory cytokines and proteins of the acute phase of inflammation. Almost 50% of cases of fetoplacental insufficiency are complicated by fetal growth retardation or chronic fetal hypoxia, which is associated with earlier and more pronounced disorders of the blood coagulation potential. Preeclampsia develops in 12% of women, inpatient treatment in the later stages due to premature detachment of a normally located or placenta previa requires 14% of pregnant women. nine0003
It is known what an important role in the period of early embryogenesis is played by an adequate supply of the body of a pregnant woman with thyroid hormones. The study of thyroid function during the manifestation of the syndrome showed that 30% of pregnant women with OHSS without initial thyroid pathology are diagnosed with subclinical hypothyroidism. The level of thyroid-stimulating hormone (TSH) in this subgroup of women exceeds the upper limit of the norm (4.0 IU / l), while the concentration of free thyroxine (fT4) is closer to the lower limit of the norm. However, by 7 weeks, these changes persist only in 12% of pregnant women, while the fT4 level may decrease even more. nine0003
The study of thyroid function during the manifestation of the syndrome showed that 30% of pregnant women with OHSS without initial thyroid pathology are diagnosed with subclinical hypothyroidism. The level of thyroid-stimulating hormone (TSH) in this subgroup of women exceeds the upper limit of the norm (4.0 IU / l), while the concentration of free thyroxine (fT4) is closer to the lower limit of the norm. However, by 7 weeks, these changes persist only in 12% of pregnant women, while the fT4 level may decrease even more. nine0003
The increase in TSH levels during the manifestation of the syndrome and for two weeks after the embryo transfer is a consequence of a sharp increase in estrogen production. Indeed, the ultra-high concentration of estradiol in pregnant women with OHSS, 30 times higher than in spontaneous pregnancy, can stimulate the production of TSH through the classical feedback mechanism. The resulting relative hypothyroxinemia without timely compensation can have an adverse effect on the development of the fetus. It is important to take into account such changes in the first trimester of gestation, that is, during the period when the fetal thyroid system is in absolute dependence on the mother's thyroid hormones, the need for which increases by 30–50%. nine0003
It is important to take into account such changes in the first trimester of gestation, that is, during the period when the fetal thyroid system is in absolute dependence on the mother's thyroid hormones, the need for which increases by 30–50%. nine0003
Management of early pregnancy due to OHSS should be carried out in a hospital with monitoring during the manifestation of the syndrome of the following indicators:
· clinical blood test - daily until hemoconcentration is eliminated;
biochemical blood test to assess the degree of hypoproteinemia and liver function - at least 2 times a week;
· indicators of the hemostasis system with the determination of the most variable parameters (D-dimer - a marker of intravascular coagulation, antithrombin III - the main natural anticoagulant) - 2 times a week; nine0011 general urinalysis - 1 time per week.
It is important to assess the severity of the systemic inflammatory response, which in pregnant women with OHSS is reflected in the indicators of leukocytosis, leukocyte count, ESR, C-reactive protein, fibrinogen, D-dimer.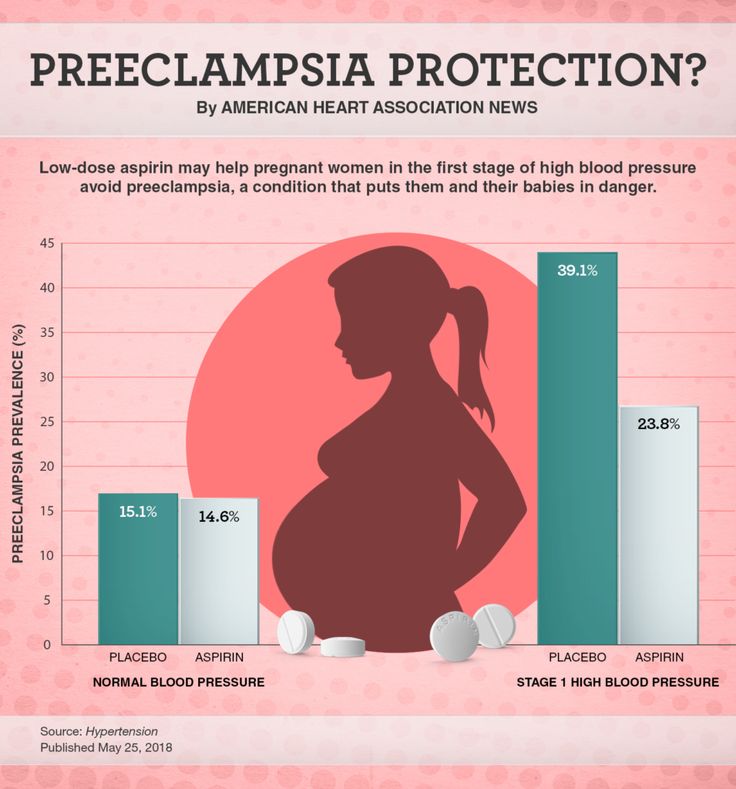
All patients should undergo infectious screening (microbiological examination of the discharge of the cervical canal and vagina with an assessment of vaginal microcenosis, microbiological examination of urine) to detect activation of a bacterial-viral infection. nine0003
Taking into account the contribution of immune imbalance to the development of SIRS in OHSS, which is reflected by a high level of pro-inflammatory cytokines, it is advisable to be cautious about prescribing antibiotic therapy, despite leukocytosis, an increase in ESR and an increase in the concentration of fibrinogen, C-reactive protein. The rationale for the use of antibacterial drugs in pregnant women with OHSS can be considered the detection of microorganisms in any of the biological fluids (urine, cervical mucus, vaginal discharge) in titers of 5 lg CFU / ml or more. nine0003
In case of regression of clinical and laboratory symptoms of OHSS, monitoring of laboratory parameters in the first trimester of pregnancy is carried out at least once every 14 days. Particular attention in the clinical blood test should be given to assessing the number of leukocytes, leukocyte formula, ESR; in biochemical analysis - markers of liver and kidney function; in the hemostasiogram - the concentration of fibrinogen, antithrombin III, D-dimer. In the II and III trimesters of pregnancy, the control of clinical and laboratory indicators is carried out at least once a month. nine0003
Particular attention in the clinical blood test should be given to assessing the number of leukocytes, leukocyte formula, ESR; in biochemical analysis - markers of liver and kidney function; in the hemostasiogram - the concentration of fibrinogen, antithrombin III, D-dimer. In the II and III trimesters of pregnancy, the control of clinical and laboratory indicators is carried out at least once a month. nine0003
Evaluation of the functional state of the thyroid gland by determining the levels of TSH and fT4 in blood plasma is necessary for all women with OHSS during the manifestation of the syndrome and at 12 weeks of gestation. Subclinical hypothyroidism and hypothyroxinemia in early pregnancy is transient, but its persistence by the end of the first trimester dictates the need to prescribe L-thyroxine at a dose of 2.3 μg/kg, followed by monthly laboratory monitoring.
Control over the state of the fetoplacental complex includes dynamic ultrasound from early pregnancy, Doppler - from 24 weeks, fetal cardiotocography - from 33-34 weeks of pregnancy. nine0003
nine0003
The complex of preventive and therapeutic measures should include, first of all, the correction of plasma and vascular-platelet hemostasis with the help of low molecular weight heparins (LMWH). The issue of prescribing preventive anticoagulant therapy to patients with OHSS remains debatable. Some researchers believe that there are no randomized trials proving the effectiveness of using LMWH in patients with OHSS to prevent thromboembolic complications [5]; moreover, cases of thrombosis on the background of heparin therapy have been described. However, in this category of women, along with the state of hypercoagulability, there are
and other equally important factors that increase the risk of thromboembolism. These are prolonged immobilization, compression of the pelvic vessels by enlarged ovaries and ascites, polymorphism of thrombophilia genes, hyperestrogenism, and most importantly, pregnancy, the success of prolonging which under such conditions depends on earlier correction of coagulation disorders and timely prevention of placental insufficiency. In addition, the simultaneous decrease in markers of the acute phase of inflammation against the background of heparin therapy indicates the benefits of prescribing LMWH. nine0011 Since the processes of inflammation and coagulation are links in the same chain, this type of therapy in pregnant women with OHSS can be considered pathogenetically justified.
In addition, the simultaneous decrease in markers of the acute phase of inflammation against the background of heparin therapy indicates the benefits of prescribing LMWH. nine0011 Since the processes of inflammation and coagulation are links in the same chain, this type of therapy in pregnant women with OHSS can be considered pathogenetically justified.
Elimination of hypoproteinemia, liver dysfunction and iron deficiency anemia is implemented through a balanced protein diet, enteral protein nutrition as a food supplement to the basic diet, iron preparations. Liver dysfunction spontaneously regresses within a month after the relief of symptoms of OHSS and in the vast majority of cases does not require additional prescription of drugs. nine0003
The question of the effectiveness of immunoglobulin therapy for the prevention of secondary infection in conditions of protein loss in this category of patients remains unresolved. Arguments in favor of this approach are based on the properties of immunoglobulins: a decrease in the level of pro-inflammatory cytokines, an increase in the activity of T-suppressors, and the prevention of damage to cell membranes [7]. However, there are no evidence-based studies on the use of immunoglobulins in this group of patients. Thus, pregnancies that occurred against the background of OHSS represent a group of high
However, there are no evidence-based studies on the use of immunoglobulins in this group of patients. Thus, pregnancies that occurred against the background of OHSS represent a group of high
risk for the development of various complications and require careful monitoring and preventive measures
starting from the early stages of development, even against the background of clinical well-being
, which allows every second woman to successfully complete pregnancy.
An algorithm for the management of induced pregnancy in OHSS is presented in the appendix.
Application. Management algorithm for induced pregnancy complicated by severe OHSS .
1. Makatsaria A.D., Bitsadze V.O., Akinshina S.V. Syndrome of systemic inflammatory response in the
wool. − M.: MIA, 2006.
2. Sidelnikova V.M. Habitual pregnancy loss. – M.: Triada-X, 2002.
3. Allen V.M., Wilson R.D., Cheung A. Pregnancy outcomes after assisted reproductive technology // J. Obstet.
Obstet.
Gynaecol. Can. - 2006. - Vol. 28, 3. - P. 220-250.
4. Christiansen O.B., Nielsen H.S., Kolte A.M. Inflammation and miscarriage // Semin. Fetal Neonatal Med. - 2006. - Vol. 11, 5. – P. 302–308.
5. Delvigne A., Rozenberg S. Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS) // Hum. reproduction. update. - 2003. - Vol. nine, 1. – P. 77–96.
6. Montanelli L., Delbaere A, Di Carlo C. et al. A mutation in the follicle-stimulating hormone receptor as a cause of familial spontaneous ovarian hyperstimulation syndrome // J. Clin. Endocrinol. Metab. - 2004. - Vol. 89, 4. - P. 1255-1258.
7. Ovarian hyperstimulation syndrome // Eds J. Gerris et al. – London: Informa Healthcare, 2006.
8. Ovarian hyperstimulation syndrome // Practice Committee of the American Society for Reproductive Medicine // Fertil. and Steril. - 2008. - Vol. nine0, 3. – P. 188–193.
Saroyan Tatevik Tigranovna, Ph.D. honey. Sciences, ml. scientific collaborator 1st Gynecological Department of the FGU NTsAGiP named after academician V.I. Kulakova Ministry of Health and Social Development of Russia
honey. Sciences, ml. scientific collaborator 1st Gynecological Department of the FGU NTsAGiP named after academician V.I. Kulakova Ministry of Health and Social Development of Russia
Address: 117997, Moscow, st. Academician Oparina, 4.
Phone: 8 (495) 438-26-22
E-mail: [email protected]
Management of pregnancy resulting from the use of ART. Pregnancy after IVF
The widespread introduction of Assisted Reproductive Technologies (ART) in medicine and the increasing awareness of infertile couples who want to have children have led to a significant increase in the number of pregnant women who become pregnant as a result of the use of ART. nine0003
But what is special about an induced pregnancy? Isn't it all over already? After all, the problem is solved. And I'm finally pregnant! Isn't it time for me to relax and not go anywhere else, not take endless tests ???
Unfortunately, you can't relax. After all, it is known that induced pregnancy is at high risk for the development of a wide variety of obstetric complications. In this regard, there is an urgent need for careful monitoring and examination of pregnant women in order to reduce the incidence of complications, develop tactics for managing pregnancy and childbirth, maintaining the health of the woman and getting a healthy baby. nine0003
In this regard, there is an urgent need for careful monitoring and examination of pregnant women in order to reduce the incidence of complications, develop tactics for managing pregnancy and childbirth, maintaining the health of the woman and getting a healthy baby. nine0003
Statistics show that the pregnancy rate in the IVF program for embryo transfer is 36%, while the birth rate for embryo transfer is only 25%, i.e. 1/3 of women who become pregnant as a result of IVF, unfortunately, will lose this pregnancy.
The majority of women who resort to IVF technology have severe disorders in the reproductive system. The body of such a patient is often not able to endure pregnancy. Age, the presence of gynecological and somatic diseases, surgical interventions, severe hormonal disorders, etc. complicate the course of pregnancy. The imbalance of sex steroids, violates the hormonal supply of early pregnancy, has an adverse effect on microcirculation and the development of uteroplacental circulation. nine0003
nine0003
The peculiarities of the course of pregnancy resulting from IVF include:
- tendency to miscarriage;
- multiple pregnancy;
- high infectious index.
An analysis of the course of induced pregnancy showed that the highest frequency of termination of pregnancy after IVF occurs in the first trimester, in the second and third trimesters, a decrease in the frequency of the threat of termination by 1.5 times is characteristic.
nine0113Pregnancy after ART is characterized by the formation of primary placental insufficiency, which requires early prescription of drugs aimed at its prevention and treatment.
In general, during pregnancy after IVF, the frequency of obstetric complications (the threat of spontaneous abortion, isthmic-cervical insufficiency, preeclampsia, infection of the fetus, bleeding disorders, the formation of placental insufficiency, improper attachment of the placenta) is 2-3 times higher than during pregnancy, occurring naturally.