Incomplete miscarriage how long
Treating miscarriage | The Royal Women's Hospital
If a miscarriage has begun, there is nothing that can be done to stop it. Any treatment you have will be aimed at avoiding heavy bleeding and infection.
A discussion with the doctor or nurse will help you to work out which treatment options are best and safest for you.
On this page:
- No treatment (expectant management)
- Treatment with medicine
- Surgical treatment (curette)
- Waiting for treatment
- After a miscarriage
No treatment (expectant management)
You can choose to wait and see what will happen. This is called 'expectant management'. If nothing is done, sooner or later the pregnancy tissue will pass naturally. If it is an incomplete miscarriage (where some but not all pregnancy tissue has passed) it will often happen within days, but for a missed miscarriage (where the fetus or embryo has stopped growing but no tissue has passed) it might take as long as three to four weeks.
While you are waiting you may have some spotting or bleeding, much like a period. When the pregnancy tissue passes, you are likely to have heavier bleeding with crampy, period-like pains. You can use sanitary pads and take pain relieving tablets, such as paracetamol.
If your miscarriage is incomplete, with just a small amount of pregnancy tissue remaining, it’s probably best to take a wait and see approach. But if there is heavy bleeding or signs of infection you will need treatment.
If the tissue does not pass naturally or you have signs of infection, the doctor will recommend a dilatation and curettage (D&C). You and the doctor can discuss and decide the preferred option for you.
Things to know
- There are many reasons why some women prefer to wait and see. It may feel more natural, it may help with the grieving process or it may give you more of a sense of control.
- Some women become worried or frightened when the bleeding gets heavier, especially if blood clots, tissue or even a recognisable embryo is passed.
- Usually, the wait and see approach takes longer than any other approaches such as surgery or medication. Sometimes bleeding can last for up to four weeks.
- Although excessive bleeding and blood transfusion are very rare, they are slightly more common with expectant management than with surgery.
- A few women still need to have surgery – sometimes urgently – if they develop infection, bleed heavily or if the tissue does not pass naturally.
- The waiting time can be emotionally draining for some women.
Treatment with medicine
Medicine is available that can speed up the process of passing the pregnancy tissue. For an incomplete miscarriage, the medicine will usually encourage the pregnancy tissue to pass within a few hours. At most it will happen within a day or two. For a missed miscarriage, it may happen quickly, but it can take up to two weeks and, occasionally, longer.
- Medication is not suitable if there is very heavy bleeding or signs of infection.
 It is usually not recommended for pregnancies that are older than about nine weeks.
It is usually not recommended for pregnancies that are older than about nine weeks. - If the tissue does not pass naturally, eventually your doctor will recommend a dilatation and curettage (D&C).
Things to know
- The pregnancy tissue will pass between four to six hours after taking the medicine, during which time you may be in hospital. After a few hours, if the pregnancy hasn’t passed, you may be sent home to wait. This will depend on where you are and which hospital you are in.
- The medicine has side effects which usually pass in a few hours but can be unpleasant, such as nausea, vomiting, diarrhoea, fever and chills. The tablets can be swallowed or dissolved under the tongue, or inserted in the vagina.
- After receiving the medication there may be some spotting or bleeding like a period. When the pregnancy tissue passes, you are likely to notice heavier bleeding and clots with strong cramping, period-like pains. You can use sanitary pads and take pain relieving tablets such as paracetamol.
- Some women may need stronger pain killers or a pain relieving injection.
- A few women still need to have surgery, sometimes urgently, if they develop infection, bleed heavily or if the tissue does not pass.
Surgical treatment (curette)
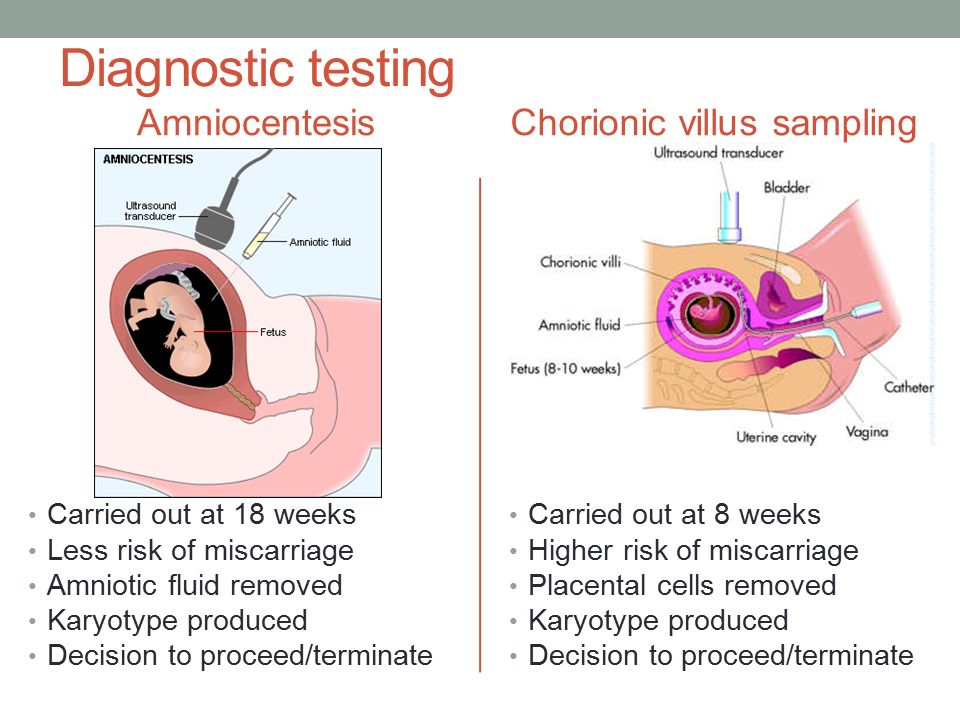
A D&C (or ‘curette’) is a minor operation. The full name is dilatation and curettage. It is done in an operating theatre, usually under general anaesthetic. There is no cutting involved because the surgery happens through the vagina. The cervix (neck of the uterus) is gently opened and the remaining pregnancy tissue is removed so that the uterus is empty. Usually the doctor is not able to see a recognisable embryo.
The actual procedure usually only takes five to ten minutes, but you will usually need to be in the hospital for around four to five hours. Most of this time will be spent waiting and recovering.
You may have to wait a day or two to have a curette and sometimes, while you are waiting, the pregnancy tissue will pass on its own. If this happens and all of the tissue is passed you may not need to have a curette.
If this happens and all of the tissue is passed you may not need to have a curette.
A curette is done in the following circumstances:
- You have heavy or persistent bleeding and/or pain.
- The medical staff advise that this is a better option for you; this may be because of the amount of tissue present, especially with a missed miscarriage.
- This is an option you prefer.
Things to know
The risks of a D&C are very low, but include:
- some pregnancy tissue remains in uterus. This can cause prolonged or heavy bleeding and the operation may need to be repeated
- infection needing antibiotics
- damage to the cervix or uterus. This is very rare (around 1 in 1000) and, when it does happen, it is usually a small hole or tear which will heal itself
- excessive bleeding (very rare)
- anaesthetic risks. These are very low for healthy women, but no anaesthetic or operation is without risk.
Waiting for treatment
If you have heavy bleeding with clots and crampy pain, it is likely that you are passing the pregnancy tissue. The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed. Sometimes the bleeding will continue to be heavy and you may need further treatment.
The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed. Sometimes the bleeding will continue to be heavy and you may need further treatment.
You should go to your nearest emergency department if you have:
- increased bleeding, for instance soaking two pads per hour and/or passing golf ball sized clots
- severe abdominal pain or shoulder pain
- fever or chills
- dizziness or fainting
- vaginal discharge that smells unpleasant
- diarrhoea or pain when you open your bowels.
What to do while you are waiting
- You can try to rest and relax at home.
- Usual activity that is not too strenuous will not be harmful. You can go to work if you feel up to it.
- If you have pain you can take paracetamol.
- If there is bleeding, use sanitary pads rather than tampons.
After a miscarriage
- It is usual to have pain and bleeding after a miscarriage.
 It will feel similar to a period and will usually stop within two weeks. You can take ordinary painkillers for the pain. Your next period will usually come in four to six weeks after a miscarriage.
It will feel similar to a period and will usually stop within two weeks. You can take ordinary painkillers for the pain. Your next period will usually come in four to six weeks after a miscarriage. - See a doctor or attend a hospital emergency department if you have strong pain and bleeding (stronger than period pain), abnormal discharge, (especially if it is smelly), or fever. These symptoms may mean that you have an infection or that tissue has been left behind.
- Try and avoid vaginal sex until the bleeding stops and you feel comfortable.
- Use sanitary pads until the bleeding stops (do not use tampons).
- All contraceptive methods are safe after a miscarriage
- See a GP (local doctor) in four to six weeks for a check-up.
Anti-D injection after a miscarriage
It is important to have your blood group checked. If you’re RhD negative and the fetus is RhD positive this can cause problems for future pregnancies. This is because the fetus’s blood cells have RhD antigen attached to them, whereas yours do not. If small amounts of the fetus’s blood mixes with your blood, your immune system may perceive this difference in blood cells as a threat and produce antibodies to fight against the fetus’s blood. Once your body has made these antibodies they can’t be removed. This is unlikely to have caused your miscarriage and is more likely to affect future pregnancies. Women with a negative blood type usually need an Anti-D injection, which will stop the antibodies forming.
If small amounts of the fetus’s blood mixes with your blood, your immune system may perceive this difference in blood cells as a threat and produce antibodies to fight against the fetus’s blood. Once your body has made these antibodies they can’t be removed. This is unlikely to have caused your miscarriage and is more likely to affect future pregnancies. Women with a negative blood type usually need an Anti-D injection, which will stop the antibodies forming.
Future pregnancies after a miscarriage
One of the most common concerns following a miscarriage is that it might happen again. However, if you have had one miscarriage the next pregnancy will usually be normal.
If you do try for another pregnancy, try and avoid smoking, alcohol and excess caffeine as they increase the risk of miscarriage. It is recommended that all women take folic acid while trying to conceive, and continue until three months of pregnancy. In your next pregnancy you are encouraged to see your GP and have an ultrasound at about seven weeks.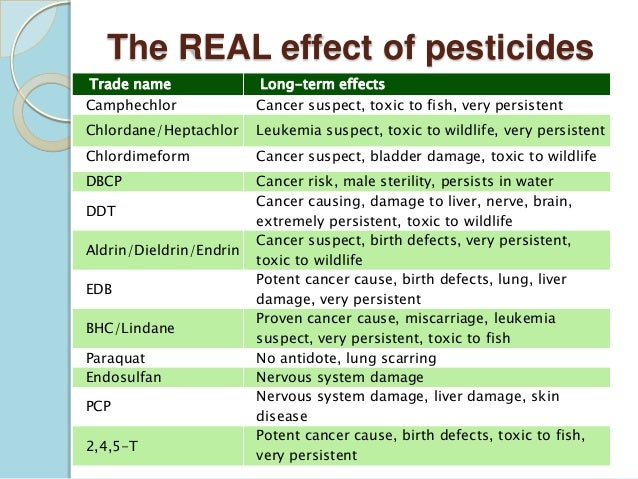 If ultrasound is done too early in pregnancy the findings are often uncertain and cause unnecessary worry.
If ultrasound is done too early in pregnancy the findings are often uncertain and cause unnecessary worry.
Feelings and reactions
There is no ‘right’ way to feel following a miscarriage. Some degree of grief is very common, even if the pregnancy wasn’t planned. Partners may react quite differently, just as people can respond differently to a continuing pregnancy. Feelings of loss may persist for some time and you may have mixed feelings about becoming pregnant again. Some friends and family may not understand the depth of emotion that can be attached to a pregnancy and may unreasonably expect for you to move on before you are ready.
Some couples decide that they want to try for a pregnancy straight away, while others need time to adjust to their loss. If you feel anxious about a possible loss in future pregnancies, you may find it helpful to talk to someone about this. If it’s difficult to speak with your friends and family about these issues, your doctor, community support group and counsellors can provide information and assistance.
Related Health Topics
-
- Treatment for miscarriage
Treatment for miscarriage is aimed at avoiding heavy bleeding and infection. It is also aimed at looking after you, physically and emotionally.
-
- (English) PDF (302 KB)
- Treatment for miscarriage
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner.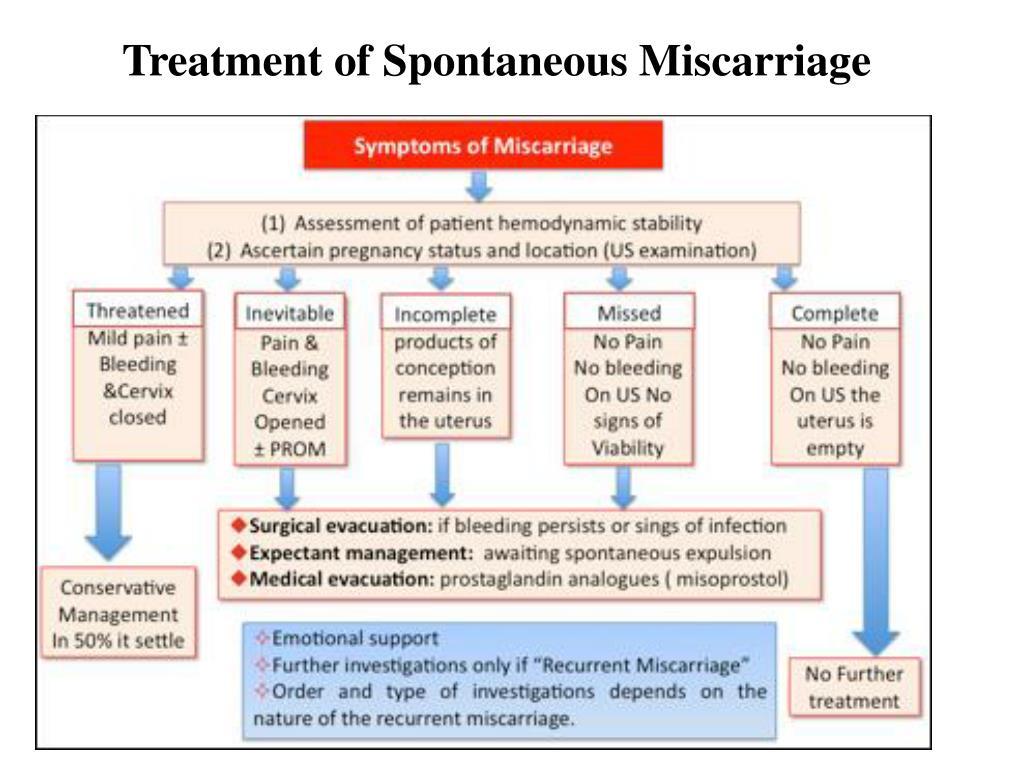 If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
Incomplete miscarriage | Tommy's
An incomplete miscarriage is when a miscarriage begins, but the pregnancy doesn’t completely come away from the womb.
What is an incomplete miscarriage?
Sometimes not all of the pregnancy comes away after a miscarriage. An incomplete miscarriage is when a miscarriage begins, but some pregnancy tissue stays in the womb.
Signs of an incomplete miscarriage
All women have some bleeding or pain during and after a miscarriage. But if you have an incomplete miscarriage, you may have these symptoms:
- heavy bleeding – get medical help if you’re soaking through a pad in an hour
- bleeding that carries on and doesn’t settle down
- passing blood clots
- increasing tummy pain, which may feel like cramps or contractions
- a raised temperature (fever) and flu-like symptoms.
Get medical help straightaway if you experience any of these warning signs.
Treatment for an incomplete miscarriage
If you have an incomplete miscarriage, you’ll need to have treatment. There are 3 options available:
- waiting for the miscarriage to happen by itself naturally (expectant management)
- taking medicine to help things along (medical management)
- having surgery to remove the pregnancy (surgical management).
Your doctor should talk with you about what may be the best option for you. You should be given some time for the diagnosis to sink in and to think about what you want to do.
“It's OK to take your time over making a decision. You may have a gut feeling about how to manage the miscarriage, you may not. Talk through your options with the medical professionals. I know they are incredibly busy, but we needed and wanted answers. I phoned the number we were given after our second missed miscarriage and asked all the questions I had.
This helped us make a decision.”
Catherine
How you are treated is your choice. However, you may be advised to have surgery immediately if there are any problems, such as infections.
Find out more about how your miscarriage will be managed.
Your emotional health
Miscarriage can be devastating. You may be struggling with grief, anxiety and shock, but you do not need to go through this alone. There are lots of organisations that can provide advice and support.
If you’re worried that you or your partner are struggling to cope after losing a baby, please talk to your GP. They will be able to help you get the support you need.
You can also talk to a Tommy’s midwife for free. You can call them Monday-Friday, 9am-5pm on 0800 0147 800 or you can email them at [email protected]. Our midwives are trained in bereavement support so will be able to talk to you about what you’re going through.
Find out more about support after a miscarriage.
Back to top
Spontaneous miscarriage and miscarriage
Over the past 10 years, the number of spontaneous miscarriages has been growing rapidly. The International Histological Classification Organization (FIGO) has declared the situation with an increase in the frequency of miscarriages an epidemic.
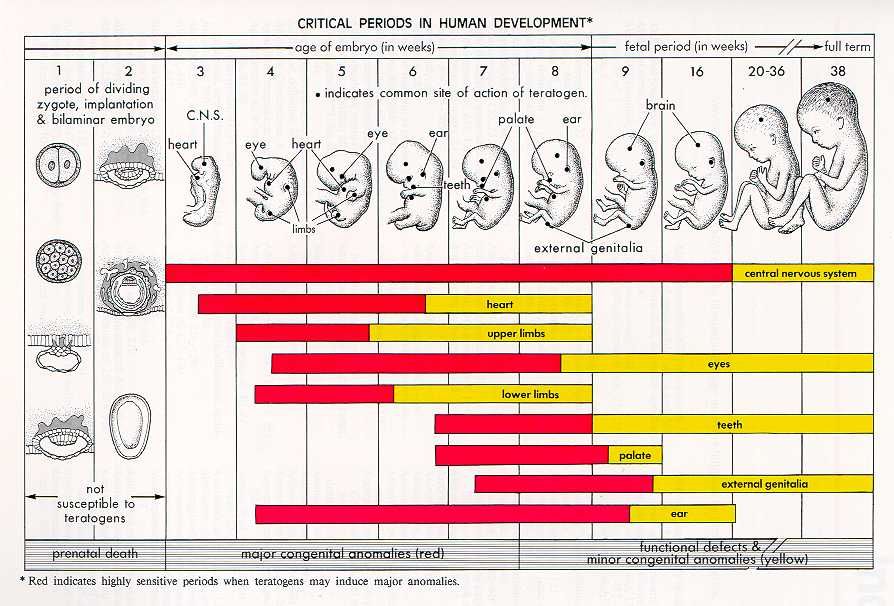
Spontaneous miscarriage is the termination of pregnancy before the fetus reaches a viable term (up to 22 weeks of pregnancy and fetal weight 500 g.).
Most miscarriages (about 80%) occur before 12 weeks of gestation. Moreover, in the early stages up to 8 weeks of pregnancy, the cause of miscarriage is chromosomal abnormalities in 50% of cases. It turns out that nature eliminates the defective product of conception. And these causes are difficult to prevent, especially in the presence of hereditary diseases. Fortunately, accidental breakdowns are much more common than genetically determined ones. Therefore, subsequent pregnancies usually end happily. nine0003 But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
Therefore, subsequent pregnancies usually end happily. nine0003 But the remaining 50% of miscarriages have completely real and removable causes. They can be easily identified at the stage of preparation for pregnancy by a gynecologist.
What are the reasons?
- chronic diseases: inflammatory diseases of the uterus and appendages, polycystic ovary syndrome, uterine fibroids, endometriosis, malformations of the genital organs.
- infections: toxoplasmosis, listeriosis, genital tuberculosis, sexual infections - chlamydia, mycoplasma, ureaplasma, syphilis. nine0007 - antiphospholipid syndrome.
- endocrine diseases: diabetes, thyroid disease.
- metabolic disorders in the body: obesity, folic acid deficiency, iron deficiency, vitamin D deficiency.
- male factor.
Of course, these causes are identified and eliminated before the planned conception.
There are harmful factors that can affect the development of the fetus in the early stages of pregnancy and lead to miscarriage:
- alcohol consumption. nine0007 - caffeine use (4-5 cups of coffee per day).
nine0007 - caffeine use (4-5 cups of coffee per day).
- smoking (more than 10 cigarettes a day).
- drug use.
- taking medications with a teratogenic effect (for example: aspirin, nise and others from this group of drugs; antifungals; antidepressants; some antibiotics and a number of other drugs).
- toxins and occupational hazards: ionizing radiation, pesticides, inhalation of anesthetic gases.
What are the signs of possible pregnancy loss? nine0004
These are complaints of pain in the lower abdomen and lower back, bloody discharge from the genital tract. It is necessary to consult a doctor to rule out an ectopic pregnancy and conduct an additional examination (hCG test, blood test for progesterone, ultrasound).
In early pregnancy, with dubious ultrasound data or suspected non-developing (missing) pregnancy, expectant management is chosen with a repeat examination by a gynecologist, ultrasound, tests after 7-10 days. If the diagnosis was made and the fact of uterine pregnancy was confirmed, with a threatened miscarriage, preservation therapy is carried out in an outpatient day hospital.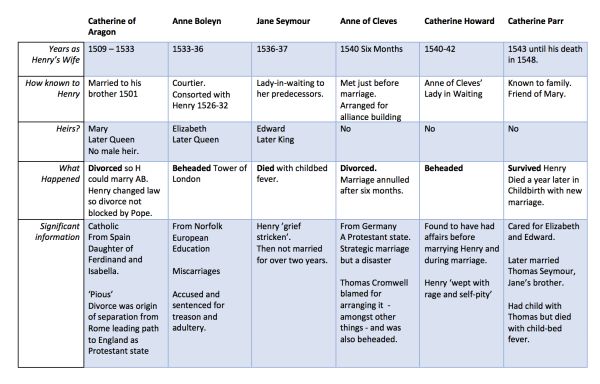 A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed. nine0005
A miscarriage that has begun requires hospitalization in the gynecological department. In the case of a non-developing pregnancy, an abortion is performed. nine0005
In accordance with the clinical treatment protocol approved by the Ministry of Health of the Russian Federation dated 07.06.2016. Preference is given to drug therapy aimed at terminating pregnancy with prostaglandin analogues (misoprostol) with or without prior use of an antiprogestin (mifepristone). In case of need for surgical treatment (with incomplete miscarriage with infected miscarriage), it is recommended to use aspiration curettage (with an electric vacuum source or a manual vacuum aspirator). What has a significant advantage over curettage of the uterine cavity because it is less traumatic and can be performed on an outpatient basis. nine0005
All women who have had a miscarriage need treatment to prevent complications and prevent recurrent miscarriages. Why is rehabilitation therapy necessary?
According to the decision of the XVIII World Congress of Obstetricians and Gynecologists , the diagnosis of chronic endometritis should be made to absolutely all women who have had an undeveloped pregnancy. Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy. nine0007 If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome). nine0007 In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist).
Two out of three miscarriages according to Professor V.E. Radzinsky are caused by this disease. When examining the material from the uterine cavity, infectious pathogens were isolated: ureaplasmas, mycoplasmas, streptococci, staphylococci, Escherichia coli, viruses (herpes, HPV). Therefore, it is very important to carry out treatment immediately after the termination of pregnancy. nine0007 If time is lost, it is necessary to carry out additional diagnostics: a pipel biopsy of the endometrium with a histological examination and a study for infections, including tuberculosis. Then, taking into account the results obtained, symptomatic anti-inflammatory therapy is carried out (immunomodulators, antibacterial drugs, physiotherapy, gynecological massage, mud therapy). In parallel, an examination is prescribed to identify other causes of miscarriage (male factor, chronic maternal diseases, genital infections, antiphospholipid syndrome). nine0007 In the medical center "Mifra-Med" at the level of modern requirements of medicine, all the possibilities for a complete adequate examination have been created: all types of tests, ultrasound, hysteroscopy, aspiration biopsy, consultations of narrow specialists (endocrinologist, therapist, neurologist, urologist). Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage. nine0005
Our gynecologists of the highest category Melko O.N., Novitskaya E.L., Tikhonova T.N. and urologist of the highest category Kanaev S.A. have sufficient experience in the rehabilitation and preparation of couples for the next pregnancy with a successful outcome. Treatment is carried out in a day hospital with the use of drugs, physiotherapy, gynecological massage, prostate massage. nine0005
WE WILL HELP YOU!
st. Yakovleva, 16 st. Kirova 47 B
tel. 244-744 tel. 46-43-57
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor. nine0005
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams.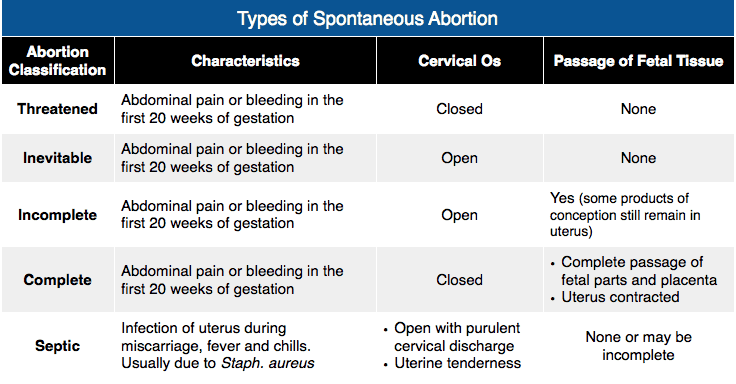 and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.
and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.
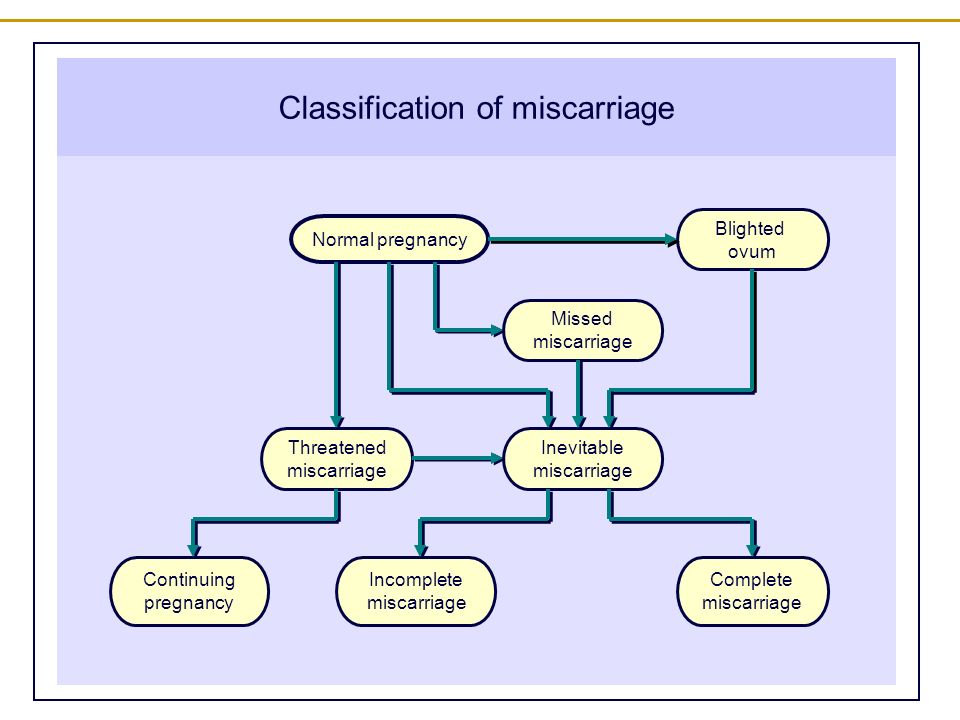
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen. nine0005
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.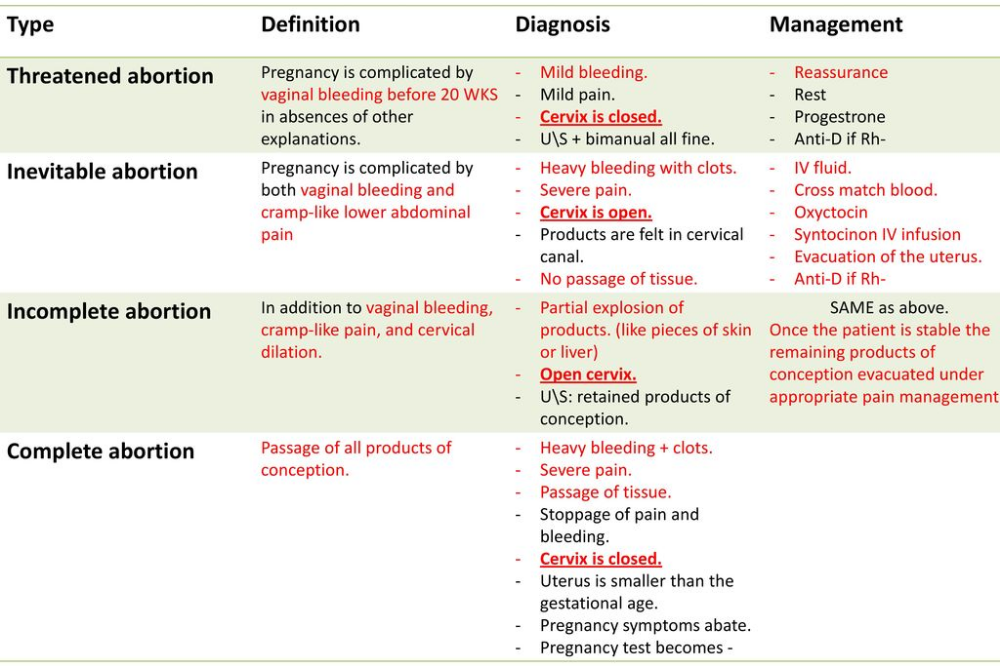
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy; nine0005
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, drawing pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization. nine0005
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin. Pregnancy cannot be saved, cleaning is required; nine0005
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them. nine0005
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.