Immunisation for babies
Immunization Schedule (for Parents) - Nemours KidsHealth
Reviewed by: Elana Pearl Ben-Joseph, MD
Primary Care Pediatrics at Nemours Children's Health
en español Calendario de vacunación
This schedule of recommended immunizations may vary depending upon where you live, your child's health, the type of vaccine, and the vaccines available.
Some of the vaccines may be given as part of a combination vaccine so that a child gets fewer shots. Talk with your doctor about which vaccines your kids need.
Birth
- HepB: Hepatitis B vaccine. Ideally, the first dose is given within 12–24 hours of birth, but kids not previously immunized can get it at any age. Some low birth weight infants will get it at 1 month or when they're discharged from the hospital.
1–2 months
- HepB: Second dose should be given 1 to 2 months after the first dose.
2 months
- DTaP: Diphtheria, tetanus, and acellular pertussis vaccine
- Hib: Haemophilus influenzae type b vaccine
- IPV: Inactivated poliovirus vaccine
- PCV: Pneumococcal conjugate vaccine
- RV: Rotavirus vaccine
4 months
- DTaP
- Hib
- IPV
- PCV
- RV
6 months
- DTaP
- Hib: This third dose may be needed, depending on the brand of vaccine used in previous Hib immunizations.
- PCV
- RV: This third dose may be needed, depending on the brand of vaccine used in previous RV immunizations.
6 months and annually
- Influenza (Flu): The flu vaccine is recommended every year for children 6 months and older:
- Kids younger than 9 who get the flu vaccine for the first time (or who have only had 1 dose before July 2022) will get it in 2 separate doses at least a month apart.
- Those younger than 9 who have had at least 2 doses of flu vaccine previously (before July 2022) will only need 1 dose.
- Kids older than 9 need only 1 dose.
- The vaccine is given by injection with a needle (the flu shot) or by nasal spray. Both types of vaccine can be used this flu season (2022–2023) because they seem to work equally well. Your doctor will recommend which to use based on your child's age and general health. The nasal spray is only for healthy people ages 2–49.
 People with weak immune systems or some health conditions (such as asthma) and pregnant women should not get the nasal spray vaccine.
People with weak immune systems or some health conditions (such as asthma) and pregnant women should not get the nasal spray vaccine.
6–18 months
- HepB
- IPV
12–15 months
- Hib
- MMR: Measles, mumps, and rubella (German measles) vaccine. Sometimes given together with the varicella vaccine and called MMRV.
- PCV
- Varicella (chickenpox)
12–23 months
- HepA: Hepatitis A vaccine; given as 2 shots at least 6 months apart
15–18 months
- DTaP
4–6 years
- DTaP
- MMR
- IPV
- Varicella
9–16 years
- Dengue vaccine: This vaccine is given in 3 doses to children who have already had dengue fever and who live in areas where it is common (such as Puerto Rico, American Samoa, and the U.
 S. Virgin Islands).
S. Virgin Islands).
11–12 years
- HPV: Human papillomavirus vaccine, given in 2 shots over a 6- to 12-month period. It can be given as early as age 9. For teens and young adults (ages 15–26), it is given in 3 shots over 6 months. It's recommended for both girls and boys to prevent genital warts and some types of cancer.
- Tdap: Tetanus, diphtheria, and pertussis booster. Also recommended during each pregnancy a woman has.
- MenACWY: Meningococcal vaccine. Protects against meningococcal bacteria types A, C, W, and Y. A booster dose is recommended at age 16.
16–18 years
- MenB: Meningococcal vaccine. Protects against meningococcal bacterium type B. The MenB vaccine may be given to kids and teens in 2 or 3 doses, depending on the brand. Unlike the meningococcal conjugate vaccine, which is recommended for all, the decision to get the MenB vaccine is made by the teens, their parents, and the doctor.
 It is only recommended as routine for kids 10 years and older who have specific conditions that weaken their immune system, or during an outbreak.
It is only recommended as routine for kids 10 years and older who have specific conditions that weaken their immune system, or during an outbreak.
Other Things to Know
- The HepA vaccine can be given as early as 6 months of age to babies who will travel to a place where hepatitis A is common (they will still need routine vaccination after their first birthday). It's also recommended for older kids who did not get it in the past.
- The MMR vaccine can be given to babies as young as 6 months old if they will be traveling internationally. These children should still get the recommended routine doses at 12–15 months and 4–6 years of age, but can get the second dose as early as 4 weeks after the first if they will still be traveling and at risk.
- The flu vaccine is especially important for kids who are at risk for health problems from the flu. High-risk groups include, but aren't limited to, kids younger than 5 years old and those with chronic medical conditions, such as asthma, heart problems, sickle cell disease, diabetes, or HIV.

- Pneumococcal vaccines can be given to older kids (age 2 and up) who have conditions that affect their immune systems, such as asplenia or HIV infection, or other conditions, like a cochlear implant, chronic heart disease, or chronic lung disease.
- The meningococcal vaccines can be given to kids as young as 8 weeks old (depending on the vaccine brand) who are at risk for a meningococcal infection, such as meningitis. This includes children with some immune disorders. Kids who live in (or will travel to) countries where meningitis is common, or where there is an outbreak, also should get the vaccine.
- COVID- 19 vaccines and booster shots are recommended for adults and kids 6 months of age and older. Everyone who is eligible should get these as soon as possible.
- Adults who were fully vaccinated against polio as children can get a polio vaccine booster dose if they're at risk for exposure to polio.
 This can include people who:
This can include people who: - travel to areas where there's a high risk for catching polio
- might be exposed to poliovirus at work
- have close contact at home with someone who has polio
Note: An outbreak is when a disease happens in greater numbers than expected in a particular area. If you have questions about vaccinating your family during an outbreak, ask your health care provider or contact your state or local health department.
Reviewed by: Elana Pearl Ben-Joseph, MD
Date reviewed: December 2022
Your Child's Immunizations: Pneumococcal Vaccines (PCV, PPSV) (for Parents)
Reviewed by: Elana Pearl Ben-Joseph, MD
en español Las vacunas de su hijo: Vacunas antineumocócicas (PCV y PPSV)
The pneumococcal conjugate vaccine (PCV13) and the pneumococcal polysaccharide vaccine (PPSV23) protect against pneumococcal infections.
The bacteria that cause these infections spread through person-to-person contact.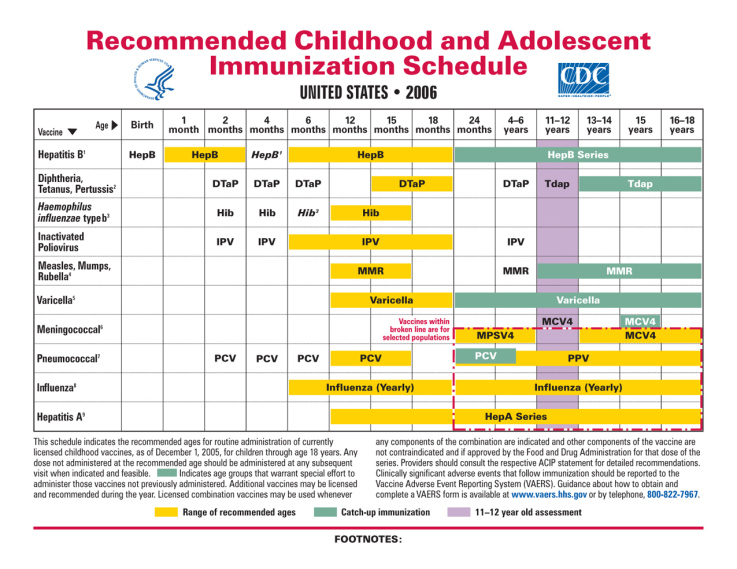 They can lead to serious infections like pneumonia, blood infections, and bacterial meningitis.
They can lead to serious infections like pneumonia, blood infections, and bacterial meningitis.
PCV13 protects against 13 types of pneumococcal bacteria, which cause the most common pneumococcal (new-muh-KOK-uhl) infections in kids. PPSV23 protects against 23 types. These vaccines prevent infections in children who get them, and help stop the infections from spreading to others.
When Are PCV and PPSV Immunizations Given?
Infants get PCV13 immunizations as a series of four injections:
- the first at 2 months of age
- then at 4 months, 6 months, and 12–15 months
Some kids older than age 2 also might need a shot of PCV13 if they have missed one or more shots, especially if they have a chronic health condition or a condition that weakens the immune system.
A doctor can decide when and how often a child should get PCV13.
Doctors also recommend PPSV23 immunizations for kids 2–18 years old with some kinds of chronic health conditions.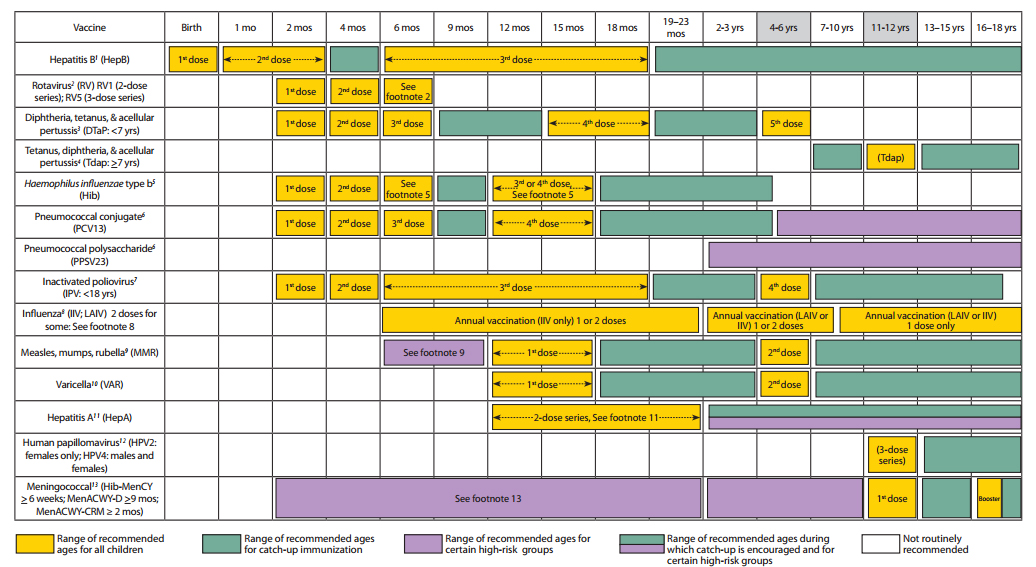 These include:
These include:
- heart, lung, or liver disease
- diabetes
- kidney failure
- a weak immune system (such as from cancer, HIV infection, or problems with the spleen)
- cochlear implants
- cerebrospinal fluid leak
Why Are the PCV and PPSV Vaccines Recommended?
Children younger than 2 years old, adults over 65, and people with some medical conditions are at high risk for serious pneumococcal infections. These vaccines are very effective at preventing severe disease, hospitalization, and even death.
What Are the Possible Side Effects of PCV and PPSV Vaccines?
Kids may have redness, tenderness, or swelling where the shot was given. A child also might have a fever after getting the shot. There is a very small chance of an allergic reaction with any vaccine.
The pneumococcal vaccines contain only a small piece of the germ and so cannot cause pneumococcal disease.
When to Delay or Avoid PCV and PPSV Immunization
These vaccines are not recommended if your child:
- is currently sick.
 But simple colds or other minor illnesses should not prevent immunization.
But simple colds or other minor illnesses should not prevent immunization. - had a serious allergic reaction to an earlier dose of a pneumococcal vaccine or to the DTaP vaccine
Caring for Your Child After PCV and PPSV Immunization
These vaccines may cause mild fever and soreness or redness in the injection area. Check with your doctor to see if you can give either acetaminophen or ibuprofen for pain or fever and to find out the right dose.
When Should I Call the Doctor?
Call the doctor if:
- Your child missed a dose in the series.
- Your child has a serious allergic reaction or high fever after immunization.
Reviewed by: Elana Pearl Ben-Joseph, MD
Date reviewed: February 2022
Vaccination - prices, paid vaccinations for children and newborns in Moscow
Vaccination according to the additional calendar of preventive vaccinations
Vaccination calendar nine0003
Registration of medical documentation
Routine vaccination according to the national vaccination schedule
Center for Immunoprophylaxis nine0003
Children's emergency room
Operations on the soft palate (treatment of snoring) in children
Tympanoplasty in children nine0003
Removal of adenoids in children
Removal of palatine tonsils (tonsillectomy) in children
Removal of neoplasms of the larynx in children nine0003
Removal of polyps in the nasal cavity in children
Shunting of the tympanic cavity in children
Clinical examination nine0003
Comprehensive pre-kindergarten examination
Comprehensive examination before school
exercise therapy nine0003
Swimming
Emergency Pediatric Care
Removal of kidney stones nine0003
Comprehensive examination before the summer camp
Comprehensive Child Health Surveillance Programs
Note to mom nine0003
Monitoring children at home
Observation of children with special needs
Psychomotor development in the first year of life nine0003
Favorable conditions for the baby
Breast-feeding
When and how to wean a baby nine0003
Children's first aid kit
Do you need a pacifier
Hygiene and wellness procedures nine0003
Massage
Treatment of temporary teeth after trauma
Treatment of caries in temporary teeth nine0003
Treatment of periodontitis of temporary teeth
Treatment of permanent teeth with an unformed root system
Treatment of pulpitis of temporary teeth nine0003
Professional dental hygiene
Prevention of caries in children's teeth
Remineralizing therapy nine0003
Vestibuloplasty
Plastic to move the bridles
Removal of temporary teeth nine0003
Removal of temporary teeth during exacerbation of a chronic process in bone tissue
Removal of the germs of wisdom teeth
Extraction of supernumerary permanent teeth
Resuscitation and intensive care for newborns
Caring for low birth weight babies nine0003
Treatment of neonatal pathology
Observation of newborns (physiological department)
Vaccination and immunoprophylaxis of children and adolescents
What is immunization?
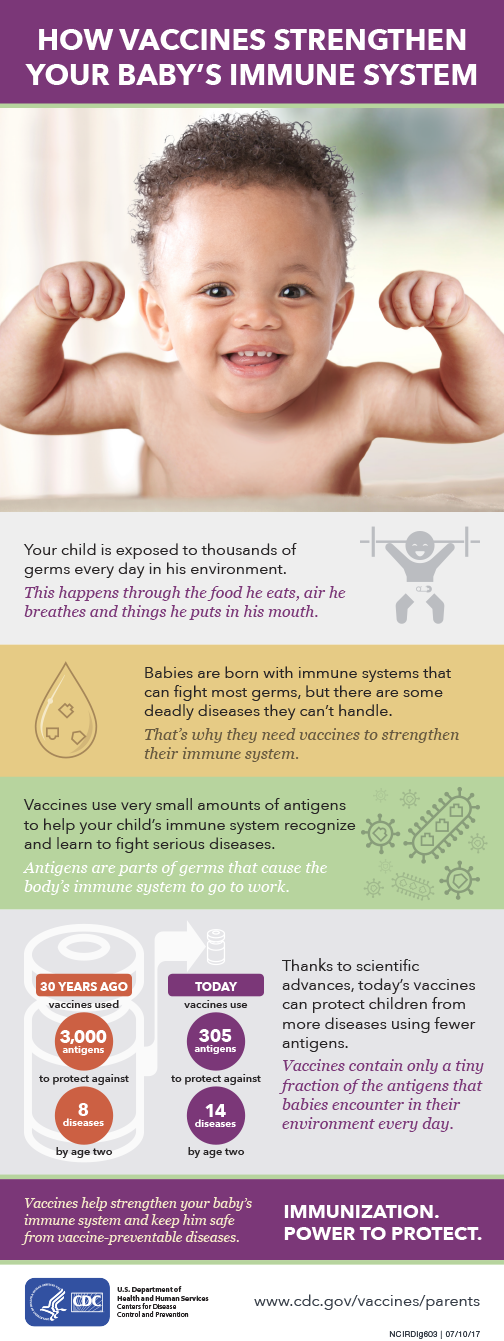
Immunization (immunoprophylaxis, vaccination) is the process by which a person acquires immunity, or becomes immune to an infectious disease, usually by administering a vaccine. Vaccines stimulate the body's own immune system to protect a person from the corresponding infection or disease.
Immunization is widely recognized as one of the most successful and effective public health interventions to save lives and health in existence. It helps to prevent 2 to 3 million deaths from infectious diseases in the world every year. nine0003
Types of vaccinations that you can get in the children's polyclinic GAUZ YaO KB No. 2
-
flu shot
-
Vaccinations against hepatitis A and hepatitis B
-
Tetanus shot
-
Tuberculosis vaccination nine0121
-
Diphtheria vaccination
-
whooping cough vaccine
-
Rubella vaccine
-
measles vaccine
nine0122
The relevance of childhood immunization
According to WHO, one in five children in the world are not covered by vaccination, which is the cause of high infant mortality in countries where public programs for immunization against infectious diseases do not have sustainable funding.
Immunization plays an important role in the fight against pulmonary tuberculosis. Parents are well aware that for many years now all newborns have been immunized to prevent the development of this dangerous infection in them. Of course, it is not yet possible to achieve a 100% result here, but doctors have managed to reduce the incidence of tuberculosis. nine0003
In the group of intestinal infections, immunization is especially effective in preventing poliomyelitis. A radical measure for the prevention of brucellosis is the improvement of the herd of domestic animals, from which this infection can pass to humans, for example, with milk. Excellent results were obtained in the immunization of the population against typhus.
Immunization is carried out in a planned manner and according to epidemic indications. The list of infectious diseases for immunization in a planned manner and the timing of vaccinations are determined by the Ministry of Health of Russia. This takes into account the need to observe a 2-month interval between vaccinations against certain infectious diseases. nine0003
It is well known that children are routinely vaccinated against tuberculosis on the 5th-7th day of a child's life, against poliomyelitis - from the 2nd month of life, against diphtheria and whooping cough - from the 5th-6th month, against smallpox - from 1 -th year to 2 years and against measles - from the 10th month of life. Repeated vaccinations are also carried out according to indications.
Antibodies provide immunity
Infection is the introduction of pathogens into the human body, accompanied by a complex of reactive processes. After the penetration of microbes, the body begins to "defend itself" - it produces antibodies that actively "fight" against pathogens. After the infection, antibodies remain in the body, i.e. immunity is developed. If pathogens of the same disease enter the body again, antibodies neutralize them. A person who has had a certain infectious disease develops immunity to it, i.e. its natural “vaccination” takes place. After the transfer of certain diseases, lifelong immunity is developed. nine0003
Sometimes vaccinations need to be repeated several times in order to develop permanent immunity. Some vaccines only last a few years and therefore need to be repeated. Before doing this, you should consult with your doctor.
History of vaccination
The first vaccination took place in 1796. The English physician E. Dhenner vaccinated several patients with cowpox, as he noticed that people who had cowpox did not get smallpox. At 1977 was the last case of smallpox.
Principles of immunization
Active immunization uses live or non-live vaccines. Live vaccines are pathogens that have retained the ability to reproduce, but their effect is very weakly expressed. Such a vaccine is vaccinated against smallpox, polio, tuberculosis, yellow fever, measles, rubella and mumps.
Non-live vaccine contains pathogens that cannot reproduce but remain active enough to cause antibodies to form in the body. Such a vaccine is vaccinated against cholera, typhoid, paratyphoid, whooping cough and influenza. nine0003
Passive immunization is based on the introduction to the patient of foreign antibodies taken from vaccinated people or animals. The action of such a vaccine begins in a few hours and ends in four weeks, since foreign antibodies, once in the human body, are split. Passive immunization is usually used in cases where a person has already contracted a certain disease or the likelihood of infection is very high. A classic example of the use of passive immunization is rabies vaccination. nine0003
Passive immunization does not protect against a specific disease, but only mitigates its course. The immune sera used to treat tetanus, measles, rubella, mumps, hepatitis and rabies are obtained from vaccinated people. Diphtheria, botulism, gas gangrene, poisoning with snake venoms are treated with animal immune serum.
When is vaccination required?
The answer to this question mainly depends on the circumstances of the individual's life.
Is vaccination dangerous?
In children, the vaccine often causes a mild vaccination reaction, such as mild fever, mild soreness, redness and swelling at the injection site, and loss of appetite. Severe lesions are less common and usually occur in children with chronic illnesses. Such children are vaccinated in a hospital under the supervision of a doctor.
In the presence of hypersensitivity to a foreign protein, serum sickness may occur. In mild cases, serum sickness symptoms such as swollen lymph nodes and urticaria are observed. In addition, allergic shock is possible, which is a common cause of patient death. nine0003
Who pays for vaccination costs?
Vaccination according to the National Immunization Schedule or according to epidemiological indications (for example, with routine vaccinations of children or the use of a tetanus vaccine in case of injury, etc.) is free of charge. Other special vaccines, for example, when traveling abroad, must be paid for by yourself.
If you care about your health and your future - make the right decision about immunization now. nine0003
National Immunization Schedule - a document approved by the order of the Ministry of Health of the Russian Federation, which determines the timing and types of vaccinations (prophylactic vaccinations) carried out free of charge and on a mass basis in accordance with the Compulsory Medical Insurance (CHI) program.
The vaccination calendar is developed taking into account all age characteristics, including the most dangerous infectious diseases in children of the first year of life. Vaccinations that are given within the framework of the National Calendar can significantly reduce the risk of disease in children. And if the child does get sick, then the vaccine made will contribute to the course of the disease in a milder form and relieve severe complications, many of which are extremely life-threatening. nine0003
National Immunization Schedule
The National Immunization Schedule is a system of the most rational use of vaccines that ensures the development of intense immunity at the earliest (vulnerable) age in the shortest possible time. The vaccination calendar can be divided into two parts.
The first part is the National Immunization Schedule, which provides for vaccination against ubiquitous infections that affect almost the entire human population (airborne infections - measles, rubella, mumps, whooping cough, chicken pox, diphtheria, influenza), as well as infections, which are characterized by a severe course with high mortality (tuberculosis, hepatitis B, diphtheria, tetanus, poliomyelitis, hemophilic infection type b). nine0003
The second part - vaccinations according to epidemic indications - against natural focal infections (tick-borne encephalitis, leptospirosis, etc.) and zoonotic infections (brucellosis, tularemia, anthrax). The same category can include vaccinations carried out in risk groups - people with both a high possibility of infection and a high danger to others in case of their illness (such diseases include hepatitis A, typhoid fever, cholera).
The National Calendar is an authoritative source of information that will help parents find out what diseases they can protect their child from and when is the best time to do so.