Im 8 week pregnant
8 Weeks Pregnant | Pregnancy
When you're pregnant, you have lots of questions. Our week-by-week pregnancy guide is packed with lots of useful information. From what's happening inside your body, to how your baby is developing, and tips and advice on having a healthy pregnancy – this is your one-stop pregnancy guide!
- 1st trimester
- 2nd trimester
- 3rd trimester
Our week-by-week pregnancy guide is full of essential information. From early pregnancy symptoms to how your baby is growing and developing, you'll find it all here.
- Week 4
- Week 5
- Week 6
- Week 7
- Week 8
- Week 9
- Week 10
- Week 11
- Week 12
You might be feeling bloated and you may have slightly swollen breasts, but it will probably be a few more weeks before you start looking pregnant.
What's happening in my body?
Your baby is growing very quickly. The placenta is getting ready to provide nutrients and oxygen and take away the waste. As part of this process, your placenta is sprouting little branches that will enable it to attach itself to the wall of your womb.
Beating the pregnancy blues
There may be times when you feel anxious and stressed. Look after yourself and get as much rest as you can. Try to eat 6 small healthy meals a day. You could also experiment with mindfulness. You can read NHS advice on how to cope with feelings and relationships during your pregnancy. The important thing is to share your worries, as there is lots of support available. A good start would be to talk to your midwife or doctor.
Early pregnancy symptoms (at 8 weeks)
You may be feeling tired and sick, you could find yourself peeing more often as your expanding womb pushes onto your bladder. If this starts to affect your sleep, try to drink lots of fluids in the day but less in the evenings.
Your symptoms could also include:
- a metallic taste in your mouth
- sore breasts
- morning sickness (read some ways to cope with morning sickness on week 6's page
- headaches
- mood swings
- new likes and dislikes for food and drink
- a heightened sense of smell
- a milky white pregnancy discharge from your vagina
- light spotting (see your doctor if you get bleeding in pregnancy)
- cramping, a bit like period pains
- darkened skin on your face or brown patches – this is known as chloasma faciei or the "mask of pregnancy"
- thicker and shinier hair
- bloating and the feeling of being bloated (read ways to cope with bloating on week 10's page)
Read Tommy's guide to common pregnancy symptoms.
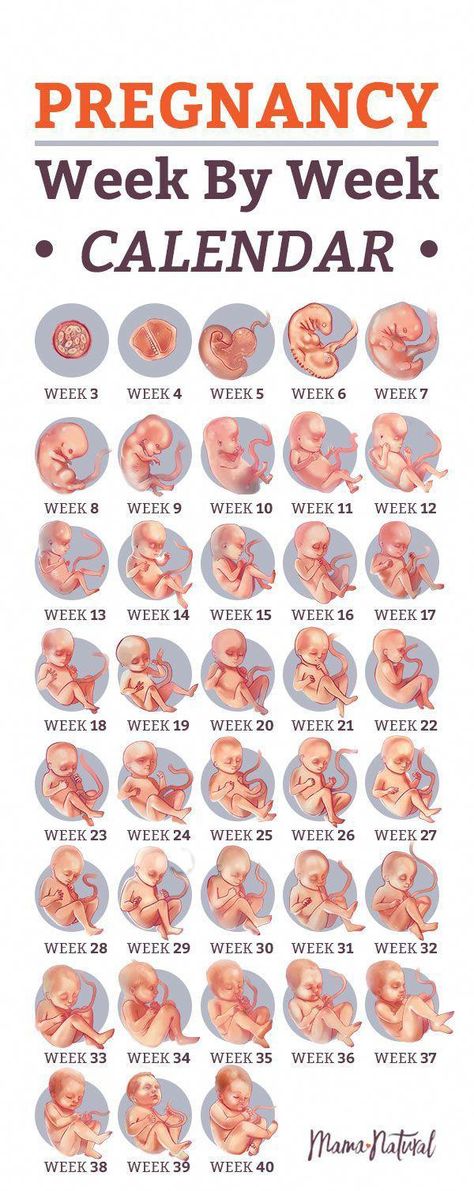
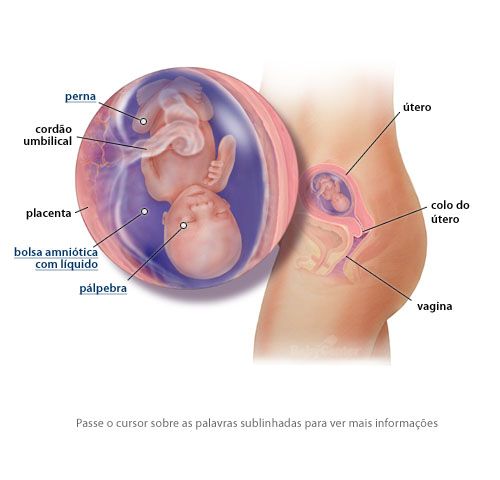
What does my baby look like?
Your baby is now around 16mm long, which is about the size of a raspberry. By next week, they will be twice the size!
The tiny head has started to uncurl a bit. Their arms are getting longer and are bigger than the legs as the upper part of the body grows faster than the lower part. The legs are getting longer too, although the knees, ankles, thighs and toes have not developed yet.
Their arms are getting longer and are bigger than the legs as the upper part of the body grows faster than the lower part. The legs are getting longer too, although the knees, ankles, thighs and toes have not developed yet.
Around now, your embryo becomes a “foetus”, which means offspring in Latin.
Action stations
Share the news with your GP or ask for an appointment with a midwife at your doctors' surgery. Alternatively you can refer yourself to your local hospital – look for contact details on their website.
You'll need to arrange a booking appointment. This usually takes place between weeks 8 and 12, and takes around an hour. You can talk about the options for your pregnancy and the birth. You'll also be offered screening tests for infectious diseases, and conditions such as Down's syndrome. You could ask about the Maternity Transformation Programme and how it could benefit you.
You will be offered your first dating scan at 8 to 14 weeks.
If it's your first pregnancy, you will probably have around 10 appointments and 2 scans in total.
Ask your midwife or doctor about online antenatal classes – they may be able to recommend one. The charity Tommy's has lots of useful information on antenatal classes and preparing you for birth.
Antenatal classes will give you the chance to meet other people and prepare you for parenthood. The NCT offers online antenatal classes with small groups of people that live locally to you.
Take prenatal vitamins. You're advised to take 400mcg of folic acid every day, until at least week 12. This helps your baby's nervous system to form and offers some protection from conditions such as spina bifida.
To keep bones and muscles healthy, we need vitamin D. From late March/early April to the end of September, most people make enough vitamin D from sunlight on their skin. However, between October and early March, you should consider taking a daily vitamin D supplement because we cannot make enough from sunlight.
Some people should take a vitamin D supplement all year round, find out if this applies to you on the NHS website. You just need 10 micrograms (it's the same for grown-ups and kids). Check if you're entitled to free vitamins.
You just need 10 micrograms (it's the same for grown-ups and kids). Check if you're entitled to free vitamins.
Do you think you or your partner could have a sexually transmitted infection (STI)? If so, get checked out, as this could affect your baby's development. Talk to your midwife or GP, or visit a sexual health clinic.
It's recommended that you do 150 minutes of exercise a week while pregnant. You could start off with just 10 minutes of daily exercise - perhaps take a brisk walk outside. Check out Sport England's #StayInWorkOut online exercises (scroll to the pregnancy section). Listen to your body and do what feels right for you.
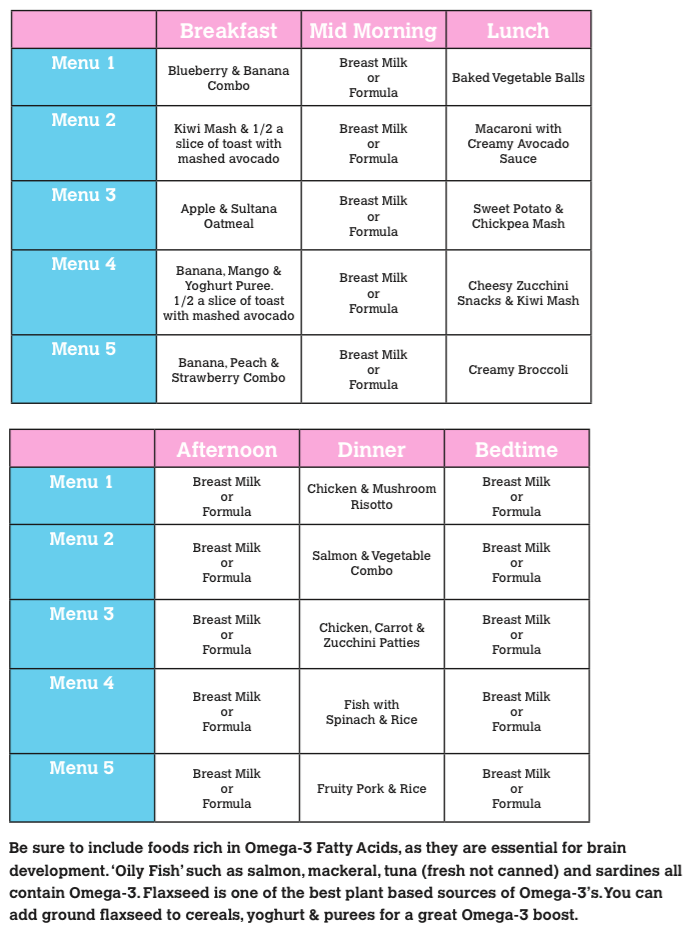
There's no need to eat for 2. If you pile on the pounds, you could put yourself and your baby at risk of health problems such as high blood pressure. Eat healthily, with plenty of fresh fruit and veg, and avoid processed, fatty and salty foods. You may be able to get free milk, fruit and veg through the Healthy Start scheme.
If you have a long-term health condition, then let your specialist or GP know you're pregnant as soon as possible. Don't stop taking any regular medication without discussing it with your doctor first.
Don't stop taking any regular medication without discussing it with your doctor first.
How are you today? If you're feeling anxious or low, then talk to your midwife or doctor. They can point you in the right direction to get all the support that you need. You could also discuss your worries with your partner, friends and family.
You may be worried about your relationship, or money, or having somewhere permanent to live. Don't keep it to yourself. It's important that you ask for help if you need it.
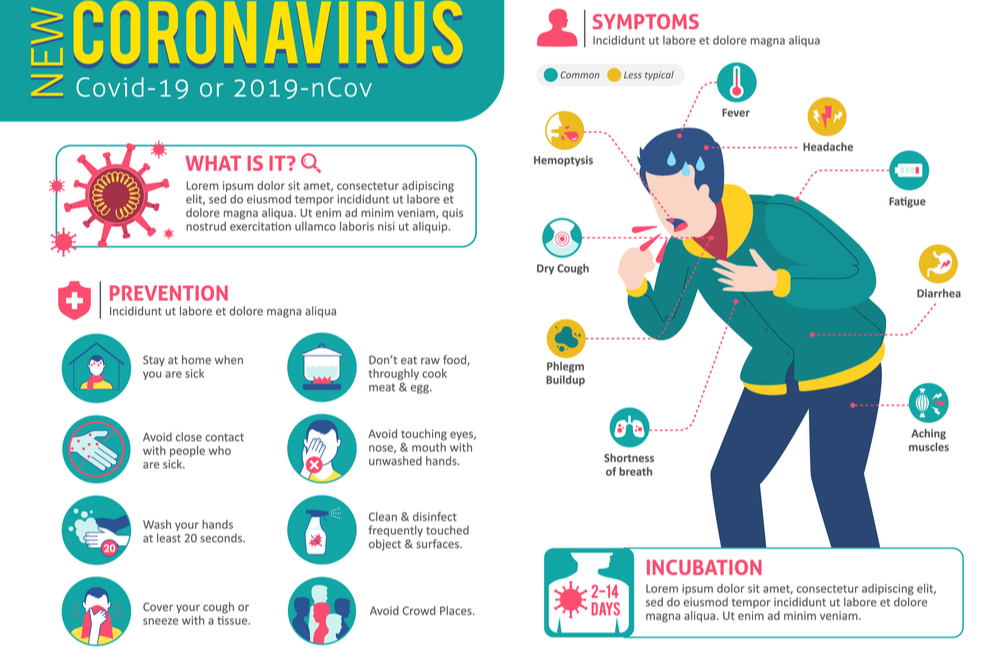
You and your family should follow the government and NHS guidance on coronavirus (COVID-19):
To find out about about COVID-19 and pregnancy, childbirth and breastfeeding, have a look at advice on the:
Want to know when the baby's due?
Use the NHS's pregnancy due date calculator.
You'll get a more accurate date from your doctor or midwife when you have a dating scan (usually at 8 to 14 weeks).
Go back to week 7
Go to week 9
8 weeks pregnant: baby's development, symptoms and your first midwife appointment
Your pregnancy symptoms in week 8
Early pregnancy symptoms
Read more about early pregnancy symptoms, such as tiredness, needing to wee more often and mood swings.
Find out more tips for getting through the first trimester.
Anxiety after pregnancy loss
Anxiety in pregnancy is very common. If you’ve lost a baby before, this can make anxiety worse.
Be kind to yourself about how you’re feeling. It’s completely understandable to feel this why. You could try some of our top tips for looking after your emotional wellbeing.
Tell your midwife or GP how you feel. They can help support you and offer treatment, if needed. If you need more help, you may be referred to a specialist mental health team for pregnant women. Find out more about anxiety in pregnancy.
Find out more about anxiety in pregnancy.
Having a safer pregnancy
No one can guarantee a perfect pregnancy. But there are certain things you can do to reduce the risk of pregnancy loss and complications. Read about the dos and don’ts of pregnancy.
What to do in week 8
To tell or not to tell
Telling people is such a personal thing to decide. Many people decide not to go public with their pregnancy until they have their gone past 12 weeks. This is because the risk of having a miscarriage goes down dramatically after 3 months.
If you do have an early miscarriage, though, you will probably need the support of close family and friends, so you could consider telling just a few people before the end of the first 3 months. You can read more about the symptoms of early miscarriage.
“I told my parents at six weeks, mainly because if anything had gone wrong at that point I would have wanted their support without having to explain that I was pregnant in the first place.
We told everyone else after the 12-week scan.”
Abby
Are you at risk at work?
If you’re worried that your job could be a risk to your health, tell your manager you’re pregnant. Your work will need to remove these risks, or perhaps offer you different work.
Things that may make it difficult to manage work and pregnancy include:
- heavy lifting or carrying
- standing or sitting for long periods without enough breaks
- being exposed to toxic substances
- long working hours.
If your employer can't remove any risks, they should suspend you on full pay. You can read more about your rights at work during pregnancy on this government website.
Find out more about having a working pregnancy.
Your first midwife appointment
In the next few weeks, you will have your booking appointment. This is your first antenatal appointment with a midwife. You’ll be asked for lots of information about your physical and emotional health, your family’s health, any medical conditions you have and your lifestyle.
You will also be offered routine blood and urine tests, which can help any potential problems, such as high blood pressure, gestational diabetes and urinary tract infections. Find out more about what tests you will have during pregnancy.
This first visit may take up to an hour, so allow plenty of time.
“I would recommend writing down a list of questions/concerns and not being afraid to ask them all however rushed others seem to be. I wish I had spoken up a bit more at appointments and I often found myself going home with questions.”
Jenni
Your answers can help make sure the antenatal team offers the right support for you. After all, their job is to ensure you have the best possible care during your pregnancy.
Your booking appointment is also a great chance for you to ask any questions you may have about your pregnancy and birth. For example, you might want to know about the screening and diagnostic tests you’d like to have or to discuss where you’d like to give birth.
It is also a chance to ask your midwife for your free prescriptions form (FW8) which enables you to apply for an NHS 'maternity exemption' certificate. Your midwife will need to sign it so you can get your prescriptions free of charge.
Read more about your booking appointment.
How likely is a miscarriage and can I prevent it?
Unfortunately, miscarriages are common. 1 in 5 women will have a miscarriage in the first 3 months of pregnancy (an early miscarriage), for no apparent reason. But most miscarriages are a one-off and there’s a very good chance that a next pregnancy would be successful. You are not at higher risk of another miscarriage if you have had 1 or 2 early miscarriages.
We still don’t always know why miscarriages happen, so this makes it very difficult to prevent them. It is important to know that miscarriages very rarely happen because of something you did or didn’t do. The most common cause of early miscarriages (the most common type of miscarriage) is chromosomal abnormalities in the baby, and these happen by chance.
Many women who do everything they can to have a healthy pregnancy still, sadly, lose their baby. But there are some lifestyle choices, such as drinking heavily or smoking during pregnancy, that can increase the risk of miscarriage.
Find out more about preventing miscarriage.
what happens to the woman's body and the fetus
7 weeks Week 9
Formation of important organs
On the 8th week, the embryonic period takes place, which is extremely important for the development of the human body. During this period, all the most important organs of the future person are laid and all systems begin to function. In the first and second weeks of pregnancy, three germ layers were formed in the zygote. At the eighth week, they differentiate - each begins its development: from the ectoderm, the outer leaf, the placenta and fetal membranes are formed; from the endoderm, the inner leaf, - the internal organs and tissues; and from the mesoderm, the middle layer, which is between the outer and inner layers, the skeleton, muscles and skin. The embryonic period is considered critical, because it is so easy to break all these subtle mechanisms! nine0003
New period
By the end of the week, the embryonic period will be over and the fertile period will begin. Now the unborn baby is called a fetus. By this time, the fetus has formed the main organs and systems: the stomach, intestines, pancreas, liver, as well as the circulatory, nervous and respiratory systems. These systems are starting to work. The brain grows so fast that the size of the head is almost half the size of the body. The face becomes similar to a human, the superciliary arches are clearly visible, the eyes are expressed, not completely covered with eyelids, the nose and auricles, the formation of the lips ends, the lungs form in the chest cavity. There is ossification of the long arms and legs, the membranes between the fingers are no longer there. The length of the tail sharply decreases, the division of the limbs into three sections is being prepared. The external genital organs and gonads develop: in boys, testicles appear, in girls, ovaries. nine0003
The external genital organs and gonads develop: in boys, testicles appear, in girls, ovaries. nine0003
Time to visit a doctor
Some women in the days of missed menstruation may feel sipping pains in the lower abdomen. If the pain becomes intense, you should consult a doctor. It is necessary to pass primary tests, undergo an ultrasound examination, and also be examined by specialist doctors in all organs and systems, if the expectant mother did not do this before pregnancy. Periodic blood and urine tests, vaginal and urethral discharges, body weighing to determine internal edema - this must be done throughout pregnancy. If there are no concomitant diseases and a woman does not suffer from colds during pregnancy, then the pregnancy prognosis will be good and a visit to the gynecologist with whom you are registered will not take much time and effort. In case of complications, there is no need to despair - just contact your doctor more often and follow all his recommendations. At this time, the placenta is only being formed, and early toxicosis may intensify: in the morning it is sick, it is difficult to get up, weakness. These symptoms may also occur during the day. A woman may want to sleep all the time. Since the embryo develops rapidly in the first weeks, the growing uterus begins to put pressure on the bladder, and this causes the woman to urinate frequently. nine0003
At this time, the placenta is only being formed, and early toxicosis may intensify: in the morning it is sick, it is difficult to get up, weakness. These symptoms may also occur during the day. A woman may want to sleep all the time. Since the embryo develops rapidly in the first weeks, the growing uterus begins to put pressure on the bladder, and this causes the woman to urinate frequently. nine0003
7 week Week 9
Pregnancy calendar Week 8 - Miracle Doctor multidisciplinary clinic in Moscow
Compared to last week, the 8-week-old baby has grown significantly. Its length is already 1.5-2 cm, and it weighs up to 3 grams. The auricles stand out on the head, the process of formation of the upper lip is underway, during which its individual parts are gradually approaching. The salivary glands are also laid. The ultrasound shows that the tail has almost completely disappeared, the eyelids almost close their eyes, and the embryo itself makes the first spontaneous movements. Tiny webbed fingers have already finally formed on the arms and legs. The arms of the embryo bend at the elbows and wrists, as there is an intensive development of the bones of the skeleton and joints. The formation of the musculoskeletal system requires the intake of nutrients in a large volume. If a woman still does not take vitamins for pregnant women, the building material is scooped from the body of the expectant mother. Therefore, do not neglect the vitamins recommended by the gynecologist. You should also follow a healthy diet rich in natural minerals and trace elements. nine0003
Tiny webbed fingers have already finally formed on the arms and legs. The arms of the embryo bend at the elbows and wrists, as there is an intensive development of the bones of the skeleton and joints. The formation of the musculoskeletal system requires the intake of nutrients in a large volume. If a woman still does not take vitamins for pregnant women, the building material is scooped from the body of the expectant mother. Therefore, do not neglect the vitamins recommended by the gynecologist. You should also follow a healthy diet rich in natural minerals and trace elements. nine0003
The formation of the heart during the 8th week of pregnancy is completed by sealing the septum between its sections. There is an improvement in the communication of the heart with the main blood vessels.
The stomach of the embryo moves down into the abdominal cavity, where it will now remain forever. Nerve elements are formed in the tissues of the muscular layer of the stomach, which subsequently ensure the correct passage of food through the stomach further into the intestines. At the 8th week of pregnancy, the formation of the testicles in the unborn boy begins. nine0003
Most moms-to-be feel exhausted at this stage. Constant fatigue is present due to ongoing hormonal changes. In the body, the level of the so-called pregnancy hormone human chorionic gonadotropin increases. An increase in hCG stimulates the corpus luteum to produce progesterone and estrogen, which are required to maintain pregnancy. The role of progesterone is to strengthen the walls of the cervix, the development of the milk ducts for subsequent breastfeeding. Progesterone is present in the body of a woman outside of pregnancy, but in a smaller amount. Under the influence of estrogen, the lining of the uterus prepares for pregnancy. It increases the number of glands and blood vessels. The restructuring of the hormonal background, necessary for the preservation and development of pregnancy, also has negative consequences. An increase in the amount of progesterone worsens intestinal motility, as a result of which a woman suffers from heartburn. The hCG hormone causes toxicosis with accompanying nausea and vomiting. Estrogen is the cause of frequent nosebleeds, bleeding gums, fever and increased sweating of pregnant women. nine0003
The hCG hormone causes toxicosis with accompanying nausea and vomiting. Estrogen is the cause of frequent nosebleeds, bleeding gums, fever and increased sweating of pregnant women. nine0003
The uterus of a woman at the 8th week of pregnancy is already enlarged, but not so much that it could be noticeable even to herself. The processes occurring in the uterus make themselves felt with weak spasms. These irregular spasms are not dangerous. Attention should be drawn to uterine contractions, accompanied by bleeding. They can be harbingers of a miscarriage.
A gynecologist can determine the increase in the volume of the uterus during examination. If you have not yet consulted a doctor, then it's time to do it now. Your pregnancy specialist will create an individual follow-up plan based on your family and obstetric history. A woman is assigned a number of laboratory tests, among which the following are common to all: nine0003
- urinalysis for hCG, protein and leukocytes,
- complete blood count,
- blood for HIV,
- blood on RW,
- determination of the Rh factor of blood,
- smear for vaginal microflora.