How to treat mouth ulcers in child
Canker Sores (for Parents) - Nemours KidsHealth
What Are Canker Sores?
Canker sores are small sores that happen inside the cheeks and lips, at the base of the gums, and on or under the tongue. They can make it painful to eat, drink, or even brush teeth.
Canker sores are different from cold sores (fever blisters), which are caused by a virus and found outside the mouth around the lips, on the cheeks or chin, or inside the nostrils. Cold sores are contagious, but canker sores are not.
What Are the Signs & Symptoms of Canker Sores?
Canker sores usually appear as round, painful open sores that have a white or yellowish coating and a red "halo" around them. Most are small (¼ inch, or 6 millimeters across) and shallow, but occasionally can be larger and deeper.
Most often, canker sores pop up alone, but they can appear in small clusters. Sometimes an area will tingle or burn before a canker sore starts to develop.
It takes about 2 weeks for canker sores to heal. During this time, the sores can be painful, although the first 3 to 4 days are usually the worst. Unless they are very large or deep, they usually heal without scarring.
What Causes Canker Sores?
No one knows exactly what causes canker sores, also known as aphthous (AF-thiss) ulcers. Many things are thought to put a person at risk for them. Diet may play a part. People whose diets are low in folic acid, vitamin B12, and iron seem to develop canker sores more often, as do people with food allergies.
Mouth injuries (like biting the inside of the lip or even brushing too hard and damaging the delicate lining inside the mouth) also seem to bring on canker sores. Sodium lauryl sulfate (SLS), an ingredient in many toothpastes and mouthwashes, has been linked to canker sores, and sometimes the sores can be a sign of an immune system problem.
Even emotional stress could be a factor. One study of college students showed that they had more canker sores during stressful periods, such as around exam time.
Young people in their teens and early twenties seem to get them most often, and women are twice as likely to develop them as men. Some girls and women find that they get canker sores at the start of their menstrual periods.
Although canker sores aren't contagious, the tendency to have outbreaks of canker sores can run in a family.
How Are Canker Sores Diagnosed?
Just because canker sores are fairly common doesn't mean they should be ignored.
If your child has canker sores that last longer than 2 weeks or can't eat or drink because of the pain, call your doctor. Also call if the sores appear more than two or three times a year.
Usually, no tests are needed to diagnose canker sores.
If your child gets canker sores a lot or they're severe, the doctor may want to do tests to look for possible nutrition problems (which can be corrected with dietary changes or prescription vitamin supplements), immune system problems, and food or other allergies.
How Are Canker Sores Treated?
Most canker sores will heal on their own in a few days to a couple of weeks. If they're painful, you can give your child an over-the-counter pain reliever like ibuprofen or acetaminophen.
If they're painful, you can give your child an over-the-counter pain reliever like ibuprofen or acetaminophen.
If a sore doesn't get better after a few weeks or sores keeps coming back, see a doctor or dentist. They may prescribe a topical medicine, special mouthwash, or home remedy to help heal the sores.
For medicines that are applied directly to the sore, first blot the area dry with a tissue. Use a cotton swab to apply a small amount of the medicine, and make sure your child doesn't eat or drink for at least 30 minutes to make sure it isn't washed away.
How Can I Help My Child Feel Better?
To help make canker sores less painful and keep them from coming back, encourage your child to:
- avoid eating abrasive foods, such as potato chips and nuts, which can irritate gums and other delicate mouth tissues
- try brushing and rinsing with toothpastes and mouthwashes that don't contain SLS
- use only soft-bristle toothbrushes and be careful not to brush too hard
- avoid any foods they're allergic to
- avoid spicy, salty, and acidic foods (such as lemons and tomatoes), which can irritate tender mouth sores
Reviewed by: Rachel S. Schare, MD
Schare, MD
Date reviewed: September 2021
Mouth ulcers - NHS
Mouth ulcers are common and should clear up on their own within a week or 2. But see a GP or dentist if you have a mouth ulcer that lasts longer than 3 weeks.
How you can treat mouth ulcers yourself
Mouth ulcers are rarely a sign of anything serious, but may be uncomfortable to live with.
They need time to heal and there's no quick fix.
Avoiding things that irritate your mouth ulcer should help:
- speed up the healing process
- reduce pain
- reduce the chance of it returning
Do
-
use a soft-bristled toothbrush
-
drink cool drinks through a straw
-
eat softer foods
-
get regular dental check-ups
-
eat a healthy, balanced diet
Don’t
-
do not eat very spicy, salty or acidic food
-
do not eat rough, crunchy food, such as toast or crisps
-
do not drink very hot or acidic drinks, such as fruit juice
-
do not use chewing gum
-
do not use toothpaste containing sodium lauryl sulphate
A pharmacist can help with mouth ulcers
A pharmacist can recommend a treatment to speed up healing, prevent infection or reduce pain, such as:
- antimicrobial mouthwash
- a painkilling tablet, mouthwash, gel or spray
- corticosteroid lozenges
- a salt (saline) mouthwash
You can buy these without a prescription, but they may not always work.
- Dissolve half a teaspoon of salt in a glass of warm water – warm water helps salt dissolve.
- Rinse your mouth with the solution, then spit it out – do not swallow it.
- Repeat as often as you like.
Non-urgent advice: See a dentist or GP if your mouth ulcer:
- lasts longer than 3 weeks
- keeps coming back
- grows bigger than usual or is near the back of your throat
- bleeds or becomes more painful and red – this may be a sign of an infection
Although most mouth ulcers are harmless, a long-lasting mouth ulcer is sometimes a sign of mouth cancer. It's best to get it checked.
Treatment from a dentist or GP
A GP or dentist may prescribe stronger medicine to treat severe, persistent or infected mouth ulcers.
Possible treatments include:
- steroid mouth spray or steroid tablets that dissolve in your mouth
- painkilling gels, ointments, sprays or tablets
- mouthwashes to kill or remove any germs in your mouth
Check if you have a mouth ulcer
Mouth ulcers usually appear inside the mouth, on the cheeks or lips.Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/832116/view
Ulcers can also appear on the tongue.Credit:
DR P. MARAZZI/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/115960/view
You may have more than 1 ulcer at a time, and they can change in size.
Mouth ulcers are not contagious and should not be confused with cold sores.
Cold sores appear on the lips or around the mouth and often begin with a tingling, itching or burning sensation.
Causes of mouth ulcers
Most single mouth ulcers are caused by things you can try to avoid, such as:
- biting the inside of your cheek
- badly fitting dentures, braces, rough fillings or a sharp tooth
- cuts or burns while eating or drinking – for example, hard food or hot drinks
- a food intolerance or allergy
- damaging your gums with a toothbrush or irritating toothpaste
- feeling tired, stressed or anxious
Sometimes they're triggered by things you cannot always control, such as:
- hormonal changes – such as during pregnancy
- your genes – some families get mouth ulcers more often
- a vitamin B12 or iron deficiency
- medicines – including some NSAIDs, beta blockers or nicorandil
- stopping smoking – people may develop mouth ulcers when they first stop smoking
If you have several mouth ulcers, it can be a symptom of:
- hand, foot and mouth disease, which also causes a rash on the hands and feet
- oral lichen planus, which causes a white, lacy pattern inside the cheeks
- Crohn's disease and coeliac disease (conditions that affect the digestive system)
- a weakened immune system from having a condition like HIV or lupus
Page last reviewed: 19 January 2021
Next review due: 19 January 2024
How to treat stomatitis in a child?
Children's stomatitis
Stomatitis is an inflammation in a child's mouth that can cause sores on the tongue, gums, cheeks and throat. This situation is more common in children under 3 years of age, but can also occur in adolescence. In most cases, stomatitis is caused by the herpes virus, and in this case is called herpetic gingivostomatitis.
This situation is more common in children under 3 years of age, but can also occur in adolescence. In most cases, stomatitis is caused by the herpes virus, and in this case is called herpetic gingivostomatitis.
Treatment is provided by a pediatrician who recommends that the child's mouth be kept clean at all times and that medications be used to relieve symptoms and, in some cases, relieve discomfort.
What can cause stomatitis in children?
Stomatitis can occur for several reasons, but the most common causes are:
- reduced immune system defenses,
- habit of putting dirty hands and objects (toys) in the mouth,
- as a result of infection with influenza viruses, herpes simplex or varicella, Coxsackie, enteroviruses,
- candidiasis (thrush).
Other pathogens are bacteria and fungi. Also, the cause may be temperature or mechanical injuries of the oral cavity, allergic reactions. Vitamin B or C deficiency plays a role.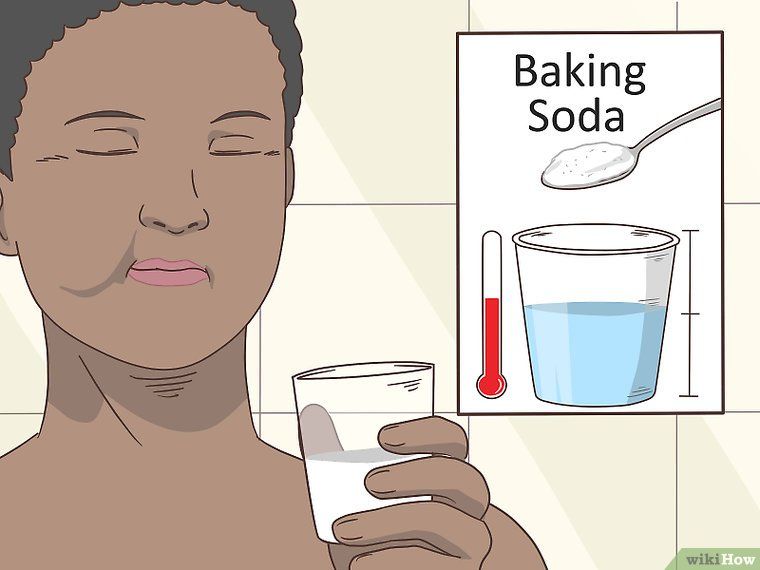
Main symptoms
Children's stomatitis usually presents with symptoms such as irritability and poor appetite because when food enters the wound, it causes pain. Other symptoms that may occur with stomatitis:
- Mouth ulcers or inflammation of the gums;
- Pain in mouth and throat when swallowing;
- May be above 38 °C;
- Wounds on the lips;
- Bad breath.
These symptoms may appear simultaneously, but most often only ulcers appear. In addition to stomatitis, there are other diseases that can cause mouth ulcers, such as the Coxsackie virus, which causes foot-and-mouth disease. Therefore, it is important that the pediatrician assess the symptoms in time and do tests in order to correctly diagnose.
What is observed in the mouth of a child with stomatitis?
On examination, there may be painful erosions, ulcers, and blisters on the lining of the inside of the cheeks, gums, lips, tongue, and, rarely, in the back of the throat. Enlarged lymph nodes in the neck and under the lower jaw are also common.
Enlarged lymph nodes in the neck and under the lower jaw are also common.
Gums may be slightly swollen, red, ulcerated and bleed easily.
When the cause is viral, oral lesions may last 7 to 10 days, although general symptoms resolve sooner.
Can the pathogen be easily diagnosed?
Microbiological examination can be carried out, but the methods used are not simple.
Samples must be transported and cultured in a suitable medium. Results will be available in approximately 15 days. Rapid diagnostic methods are also available, such as direct staining of the contents of the vesicles with fluorescent antibodies.
Is there any specific treatment?
Treatment of stomatitis should be prescribed by a pediatrician or dentist and last about 2 weeks. However, it is important to be careful with the food the child eats and maintain proper oral hygiene to avoid the multiplication of microorganisms in the ulcer.
Most often, gingivostomatitis resolves spontaneously and requires only symptomatic pain management or antiseptics to aid local healing. In children, special attention should be paid to their hydration by offering them liquids in fractional form, cold or at room temperature. Sour, salty or spicy foods should be avoided.
In children, special attention should be paid to their hydration by offering them liquids in fractional form, cold or at room temperature. Sour, salty or spicy foods should be avoided.
Discomfort can be reduced with paracetamol or ibuprofen taken by mouth. If a yeast infection is suspected, topical application or antifungal rinses are usually effective. In some cases, the use of antiviral drugs such as acyclovir may be recommended for gingivostomatitis caused by herpes viruses. This medication helps heal wounds in the mouth, but should only be used with a pediatrician's prescription. Therapy of herpes infection with acyclovir is not required for mild infection in children with sufficiently strong immunity.
How to feed an infant or child with stomatitis?
It is important that the baby's feeding is not interrupted when there is an illness. However, it is important to be careful to avoid aggravating symptoms:
- Avoid acidic foods such as orange, kiwi or pineapple;
- Offer cold liquids such as fruit juices or smoothies;
- Eating pureed or liquid foods, such as soups;
- Choose cold foods such as yogurt, fruit compotes and gelatin.

How can stomatitis be prevented?
Herpes simplex infections are common in schoolchildren. Most of these infections are asymptomatic, the virus is shed in saliva in the absence of clinical manifestations of the disease. Children with this disease should stay at home until the end of treatment.
The best form of prevention is strict handwashing, avoiding direct body contact with other people, and not sharing glasses or utensils.
Stomatitis in a child - what is it? . Official site of KGAUZ "Norilsk GSP"
Stomatitis is an inflammation of the oral mucosa. The name comes from the Latin word “stoma” (mouth). Stomatitis occurs in both children and adults, but most often it appears in infants and preschoolers. This is because the mucosa at this age is thinner and more tender. It’s more common for everyone to say “stomatitis”, but it would be more correct to say “stomatitis”, since this is a generalizing concept for a whole group of diseases.
Causes of stomatitis in children
Causes of stomatitis in children are different. These are dirty hands, and fragile children's immunity, and the features of thermoregulation, on which the respiratory system directly depends. You need to understand that the children's mucosa, unlike the adult one, is a very thin and vulnerable substance, so the attachment of any infection occurs very quickly. At an early age, salivation is not yet fully formed in a child, and saliva enzymes play a very important role in protecting the body. As a result, the mucous membrane often dries up, cracks appear, an infection occurs, and stomatitis follows it. It is impossible not to take into account the long-term use of medications, such as antibiotics, as well as neuropsychiatric disorders, unfavorable living conditions, poor child care and inadequate oral hygiene by the parents themselves.
These are dirty hands, and fragile children's immunity, and the features of thermoregulation, on which the respiratory system directly depends. You need to understand that the children's mucosa, unlike the adult one, is a very thin and vulnerable substance, so the attachment of any infection occurs very quickly. At an early age, salivation is not yet fully formed in a child, and saliva enzymes play a very important role in protecting the body. As a result, the mucous membrane often dries up, cracks appear, an infection occurs, and stomatitis follows it. It is impossible not to take into account the long-term use of medications, such as antibiotics, as well as neuropsychiatric disorders, unfavorable living conditions, poor child care and inadequate oral hygiene by the parents themselves.
It is often the parents who help the doctor to find out the cause of the disease. Only they can try to analyze what caused the appearance of a bubble, sore or plaque. For example, the child ate something wrong, bought a new toothpaste or toothbrush, or maybe the baby suffered a temperature drop.
Depending on the causes of occurrence, stomatitis can be divided into several types, each of which has a number of features.
Viral, herpes, or herpetic stomatitis in children is one of the most common types of childhood stomatitis. Usually a child becomes infected with it by airborne droplets. The virus is also transmitted through dishes, toys, household items. Most often, herpetic stomatitis in a child appears at the age of one to 4 years. The disease begins as a cold and is accompanied by a rash on the lips, lethargy, and fever. Sometimes there is a runny nose and cough. Around the second day, aphthae appear on the lips, tongue, and inside of the cheeks - small round or oval sores of light yellow color with a bright red border. They exude an unpleasant odor, are easily torn off and then bleed. These ulcers are the main symptom of this type of stomatitis. Therefore, such stomatitis in children is also called aphthous, or ulcerative. This is a particularly unpleasant type of disease, as it can be severe and accompanied by severe intoxication. Viral stomatitis in children also often occurs against the background of other viral diseases, such as influenza, chickenpox or measles.
Viral stomatitis in children also often occurs against the background of other viral diseases, such as influenza, chickenpox or measles.
Infectious stomatitis occurs in children of both school and preschool age. Most often they occur with tonsillitis, sinusitis, pneumonia. The main symptom is a thick yellow crust on the lips. At the same time, the lips stick together, the mouth opens with difficulty. The temperature usually rises. Bacterial stomatitis in a child most often occurs due to weakened immunity in the autumn-winter period.
Traumatic stomatitis in a child is caused by mechanical trauma to the oral cavity. For example, burns from hot food, a too hard nipple, the habit of chewing on a pencil. Also, traumatic stomatitis often occurs in children with malocclusion due to frequent biting of the cheeks and tongue.
Candidal stomatitis occurs in children under one year old. The cause is Candida fungus. The milk left in the baby's mouth after breastfeeding is an excellent breeding ground for them.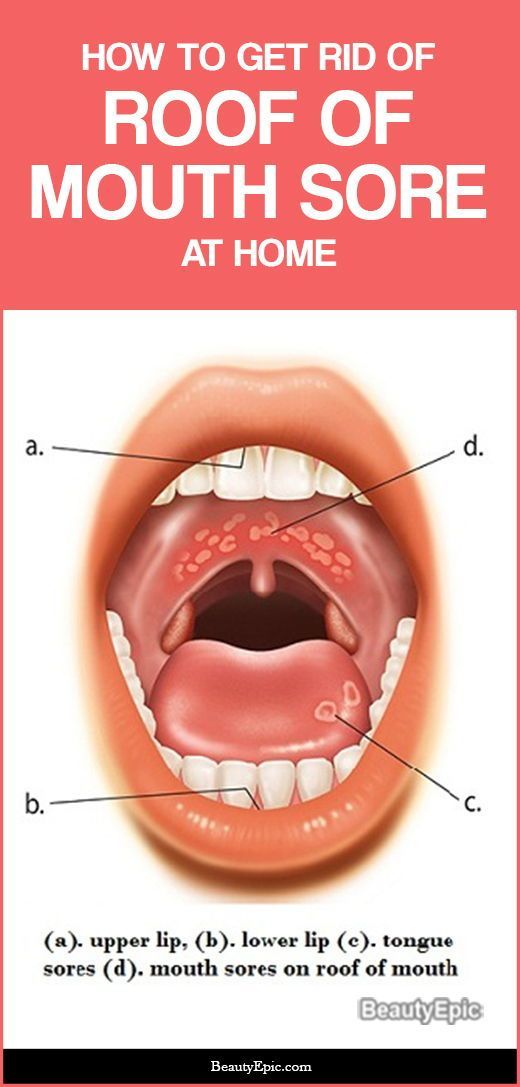 Therefore, parents call candidal stomatitis in children thrush. The main symptom is the appearance of white plaque in the baby's mouth. It is worth noting that this plaque should not be confused with the usual plaque after feeding. A cause for alarm is if the plaque does not go away, and the child refuses to eat.
Therefore, parents call candidal stomatitis in children thrush. The main symptom is the appearance of white plaque in the baby's mouth. It is worth noting that this plaque should not be confused with the usual plaque after feeding. A cause for alarm is if the plaque does not go away, and the child refuses to eat.
Drug-induced or allergic stomatitis in children is caused by some type of allergy or drug reaction. In case of suspicion of this type of disease, the allergen should be identified and removed, otherwise there is a risk of getting unpleasant consequences, up to anaphylactic shock.
Symptoms of stomatitis in children
For all types of stomatitis, a common and defining symptom is inflammation of the oral mucosa and the appearance on any of its parts, such as the tongue, the inside of the lips, cheeks, throat of various formations in the form of sores, vesicles, characteristic plaque, vesicles (blistering rashes) and in cases of traumatic stomatitis - burns, bites, injuries. It is important to understand that stomatitis is not one acute or chronic disease with certain classic symptoms, each type has its own special cause, and they manifest themselves in the oral cavity in different ways, therefore, they need to be treated differently.
It is important to understand that stomatitis is not one acute or chronic disease with certain classic symptoms, each type has its own special cause, and they manifest themselves in the oral cavity in different ways, therefore, they need to be treated differently.
Treatment of stomatitis in children
There is no single algorithm for the treatment of stomatitis in children. Each case is individual in its own way. It often happens when a mother comes in the hope that the doctor will prescribe an ointment, and she will immediately cure her child with it. This does not happen! It is necessary to understand what preceded the inflammation, taking into account the age of the child, the stage and severity of the disease. Treatment is carried out both locally and symptomatically, i.e. symptoms are relieved. Doctors dentist-therapist and pediatrician give their recommendations, it is possible to involve highly specialized specialists, such as ENT, mycologist, dermatologist. Of course, there are some textbook principles that guide specialists in order to relieve or relieve pain or prevent complications.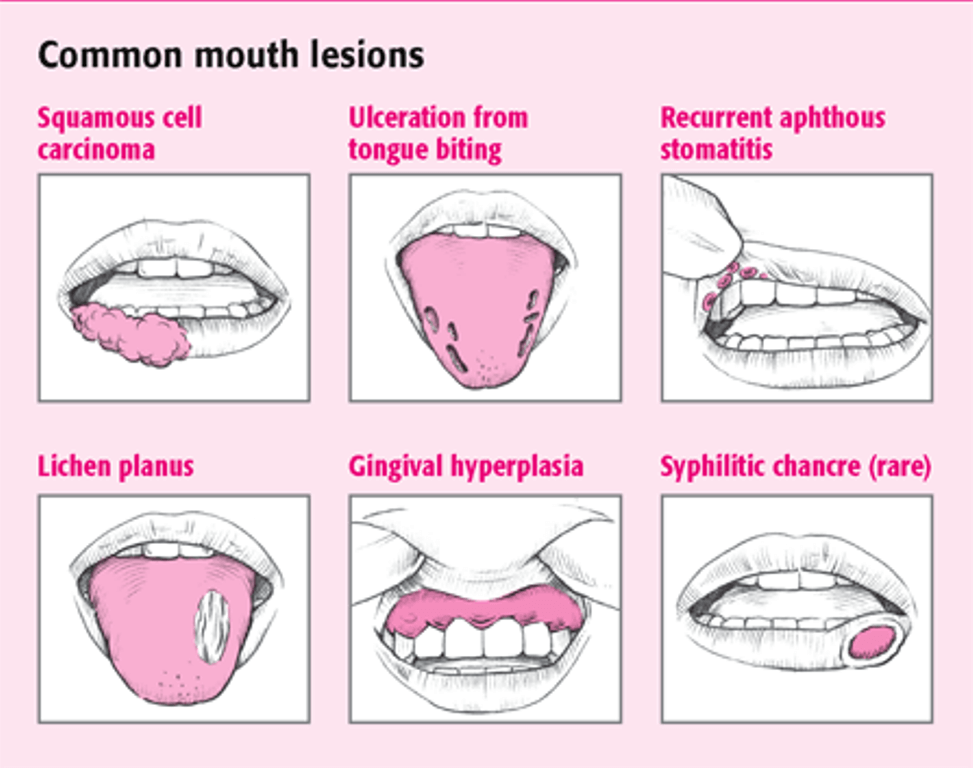 We are talking about compliance with the rules of oral hygiene, diet and sleep, treatment of the mucous membrane with special gels, solutions and applications. For example, with allergic stomatitis in children, antihistamines are recommended, with herpetic forms - antiviral, if there is a temperature - it is antipyretic. It is important that when you find a problem, contact a specialist without delay.
We are talking about compliance with the rules of oral hygiene, diet and sleep, treatment of the mucous membrane with special gels, solutions and applications. For example, with allergic stomatitis in children, antihistamines are recommended, with herpetic forms - antiviral, if there is a temperature - it is antipyretic. It is important that when you find a problem, contact a specialist without delay.
Caring for a child with stomatitis
Parental involvement in treatment and proper care of the child are not only important, they are decisive. With stomatitis, it is necessary to strictly follow the treatment plan, which is often very laborious, so the result depends on parental care and control. The oral cavity is a kind of epicenter of pain, so it is not surprising that the child will be capricious a lot. Therefore, it is important for parents to stock up on patience and perseverance.
Most moms and dads are concerned about how to feed a child with stomatitis. Firstly, it is necessary to consume only soft, warm (not hotter than 30 degrees) and mushy food, for example, in the form of mashed potatoes. The main thing is that the food is high-calorie and positive, because the child's immunity is already weakened. After eating, it is imperative to rinse your mouth so as not to provoke the development of stomatitis and not to attach any additional infection. A diet for stomatitis in a child should be with the exclusion from the diet of spicy, sour, sweet foods and citrus fruits.
The main thing is that the food is high-calorie and positive, because the child's immunity is already weakened. After eating, it is imperative to rinse your mouth so as not to provoke the development of stomatitis and not to attach any additional infection. A diet for stomatitis in a child should be with the exclusion from the diet of spicy, sour, sweet foods and citrus fruits.
Children with stomatitis need to be anesthetized. It is carried out with the help of various medications in order to avoid refusal of food and deterioration of sleep. In addition, with stomatitis in children, proper treatment of the oral cavity is very important. How to handle and rinse the child's mouth should be recommended by the doctor.
Prevention of stomatitis in children
If a person had stomatitis at least once in his life, there will always be a risk of its recurrence, so prevention comes to the fore - in general, strengthening immunity in order to prevent the disease from returning.