How to relieve varicose veins during pregnancy
Treat Varicose Veins Naturally During Pregnancy
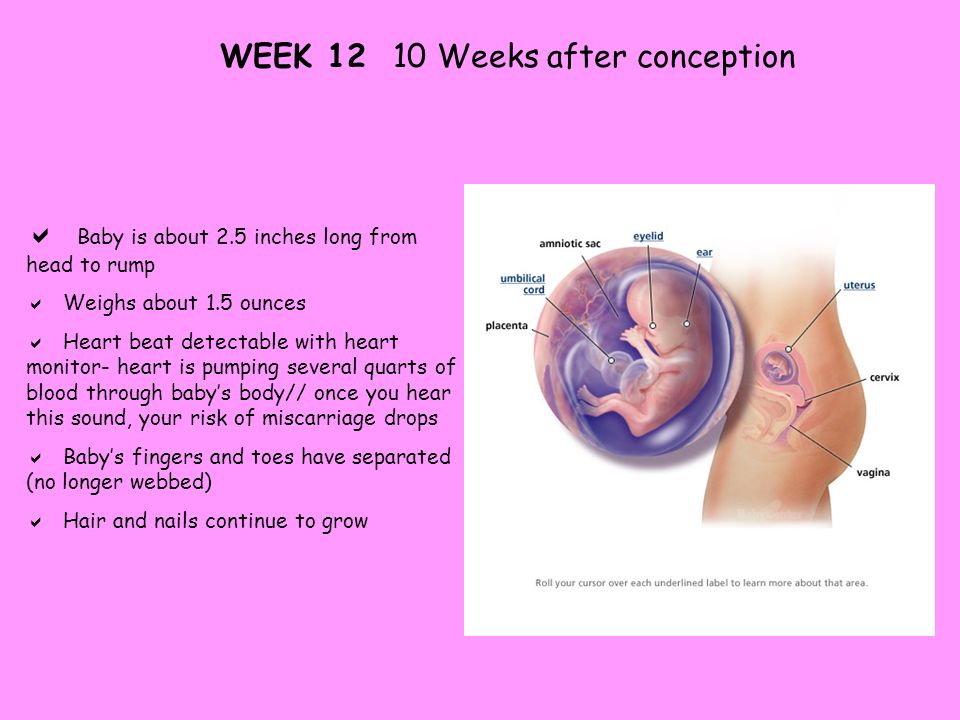
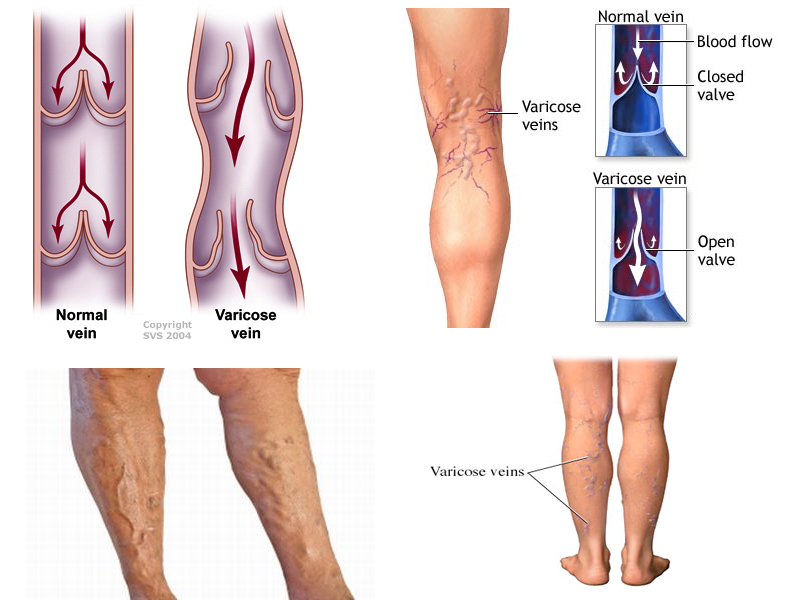
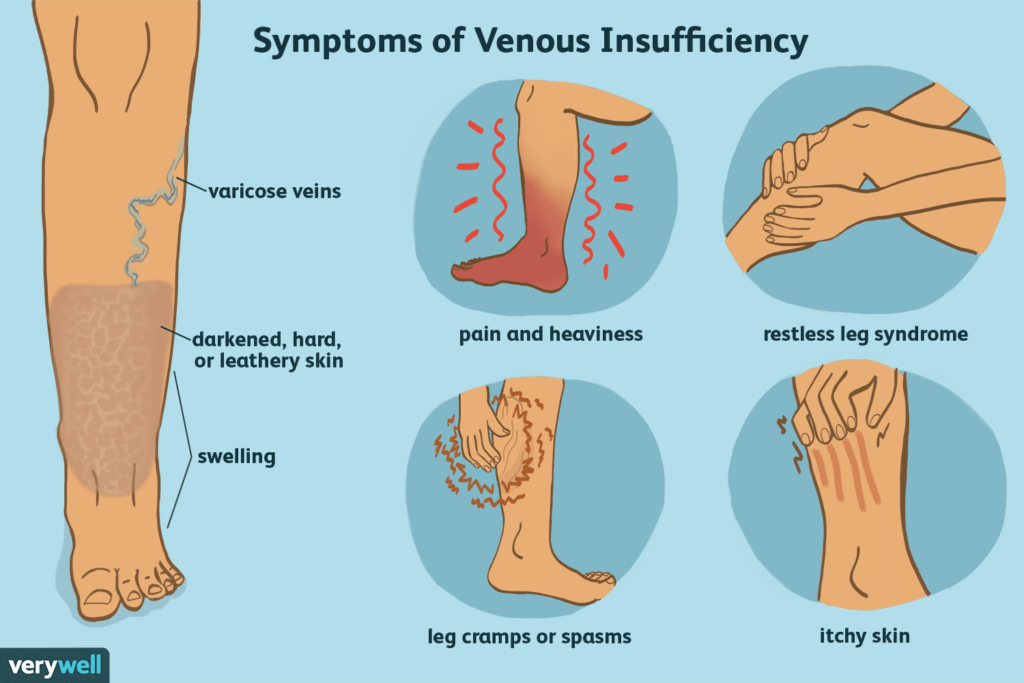
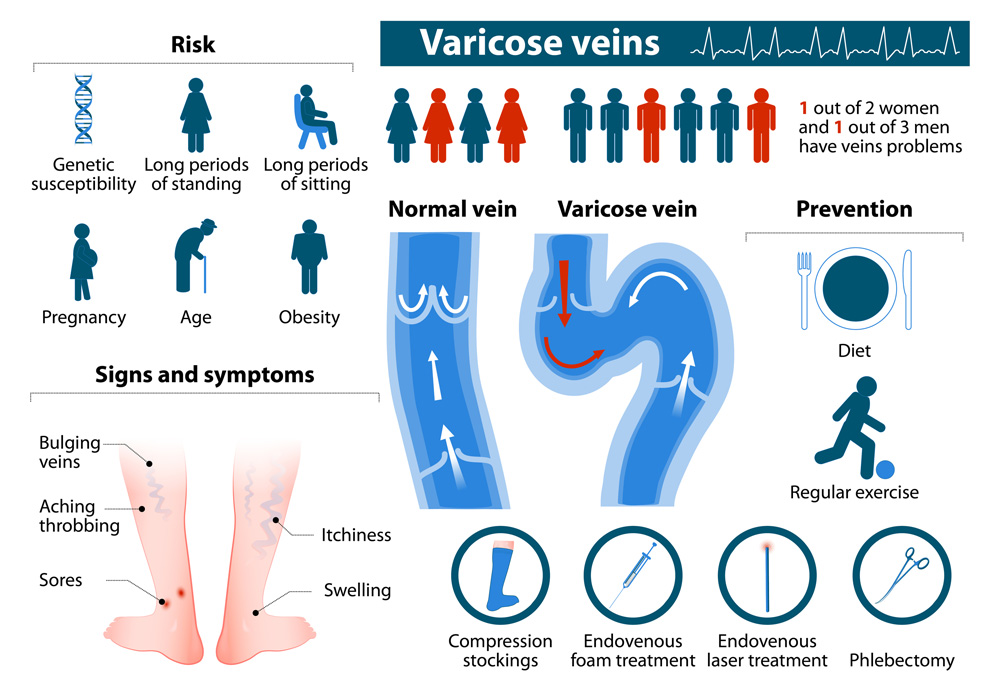
Varicose veins during pregnancy are caused by blood volume increases that put pressure on the veins. Varicose veins are enlarged veins that commonly occur in the legs, although during pregnancy they can also appear on the buttocks and vaginal area. Hormonal changes can also lead to varicose veins during pregnancy as increased progestin levels can dilate or open the veins. In addition, during pregnancy the uterus puts pressure on the inferior vena cava (the vein that carries blood from the legs and feet to the heart), further contributing to varicose veins.
Varicose veins are generally harmless, although they may become itchy and uncomfortable. The good news is they typically diminish within three months to a year after giving birth.
Hemorrhoids are another kind of varicose vein in the anus or rectum that occurs during pregnancy and is oftentimes a result of constipation.
While varicose veins can be hereditary, and you can’t prevent the circulatory changes that occur during pregnancy, there are some ways you can prevent or minimize varicose veins.
These preventative measures are ultimately your best treatment option during pregnancy:
- Avoid sitting or standing in the same position for long periods of time. Make sure to take breaks to change your position.
- Avoid wearing high heels. It is better to wear lower-heel or flat shoes as this works your calf muscles, fostering healthy circulation.
- Get regular exercise. Talk with your doctor to confirm if it is safe for you to exercise during pregnancy.
- Wear maternity support hosiery. These put pressure on the legs, stimulating blood flow up the leg towards the heart. However, avoid wearing tight hose that cut off circulation.
- Avoid crossing your legs while sitting.
- Elevate your legs periodically to improve circulation.
- Sleep on your left side. This will help relieve pressure on the inferior vena cava.
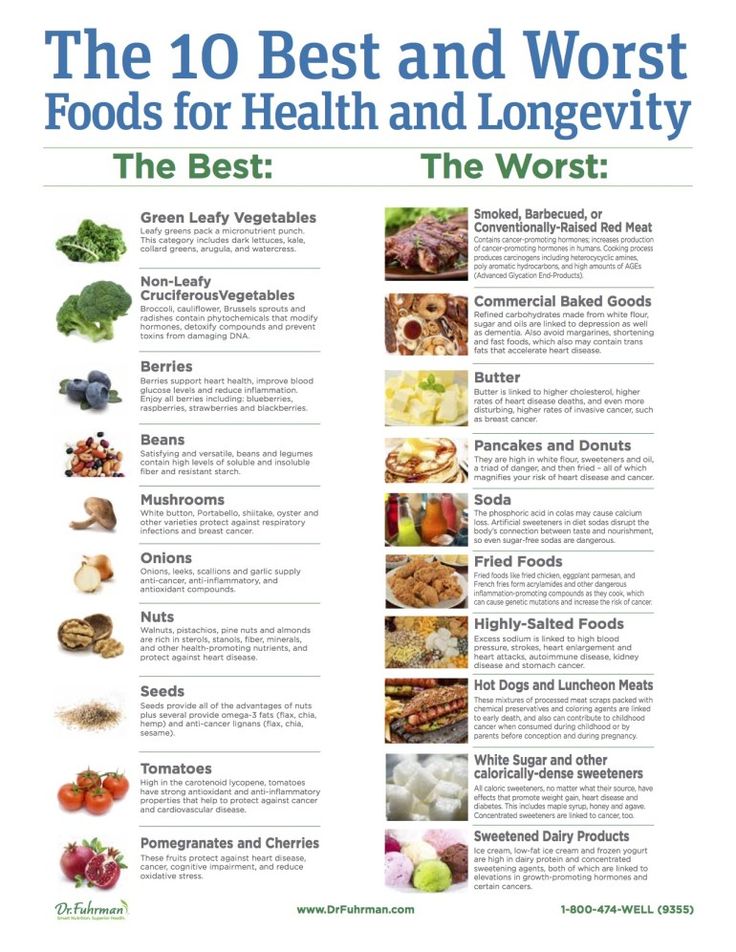
- Reduce sodium intake to minimize swelling of the veins.
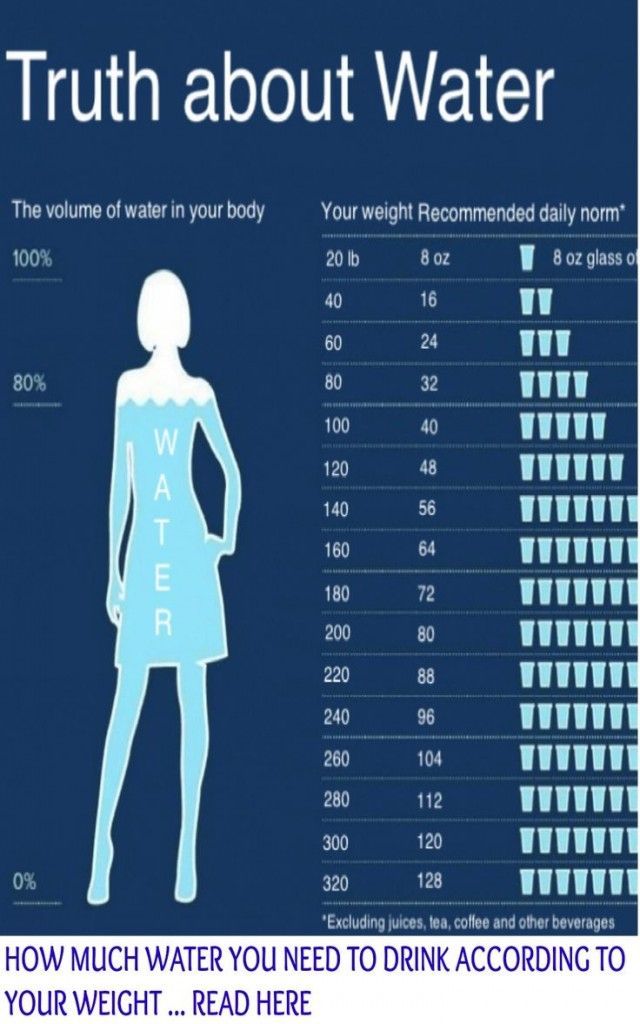
- Drink plenty of water and eat enough fiber to prevent constipation.
Warning: Some have used horse chestnut seed extract (with the poisonous esculin removed) to treat varicose veins. However, consuming the raw bark, flower, seed, or leaf of this plant is poisonous and can cause death. The safety of using horse chestnut extract with the esculin removed during pregnancy remains unknown.
Therefore, it is best to avoid using it if you are pregnant or breastfeeding.
How to Treat Varicose Veins Naturally During Pregnancy When Naturally Does Not Work
Varicose vein surgery is not recommend during pregnancy as varicose veins generally improve after giving birth. Contact your doctor if the veins become swollen, warm, tender, or red, if they bleed, if you have a rash on your leg or ankle, or if the skin on leg changes color or thickens.
- Skin Changes During Pregnancy
Compiled using information from the following sources:
1. Aetna Inc. (2015). Clinical policy bulletin: Varicose veins, Number 0050.
Aetna Inc. (2015). Clinical policy bulletin: Varicose veins, Number 0050.
2. Mayo Clinic Staff. (2013, January 31). Varicose veins.
https://www.mayoclinic.org/diseases-conditions/varicose-veins/basics/definition/con-20043474
3. MedlinePlus. (2014) Horse chestnut.
https://www.nlm.nih.gov
4. Murry, M. M. (2013, April 10. Varicose veins and pregnancy: Legs and more.
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-blog/varicose-veins-and-pregnancy/bgp-20055799
5. Nemours. (2013). Why do some pregnant women get varicose veins?
https://kidshealth.org/parent/question/infants/veins.html
6. Office on Women’s Health, U.S. Department of Health and Human Services. (2012). Varicose veins and spider veins fact sheet.
How to Treat Varicose Veins While Pregnant| Vein Clinics of America
Did you know pregnancy is one of the top 5 leading causes of varicose veins? Learn how to keep your veins healthy during pregnancy on our blog here.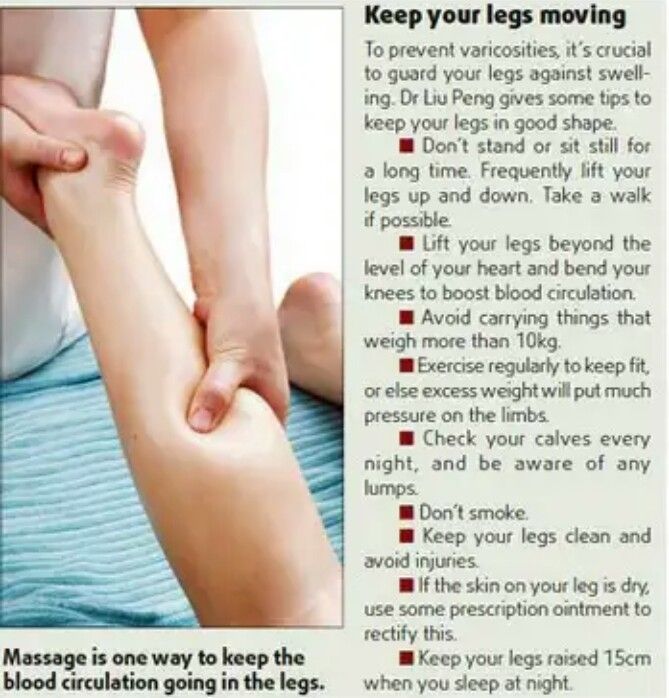
Pregnancy comes with its challenges, and one of those that isn’t always on people’s radar is varicose veins.
Varicose veins during pregnancy are more common than people think, however. Studies show that nearly 50% of pregnant women suffer from vein disease.
In fact, one of the top 5 leading causes of varicose veins is pregnancy. While not every woman will suffer from vein issues while pregnant or following her pregnancy, it is very common.
Why does pregnancy sometimes lead to varicose veins?
Here we will answer that question, and share with you how you can decrease your risk of developing this vein problem during and after your pregnancy.
Why You May See Varicose Veins When Pregnant
1. Hormone changesThe minute you become pregnant, your hormones immediately start changing.
The flux in your hormones can cause a number of things to happen. You may find you’re more irritable, that you have strange food cravings — some of the typical things you hear about with pregnant women.
However, you may be surprised to find out that your changing hormones also affect your veins.
How does that happen?
Progesterone production in a pregnant woman’s ovaries skyrockets during pregnancy. And, because of this, her blood vessels struggle to contract like they did pre-pregnancy.
Though this sounds like a bad thing — there is a reason for it. A pregnant woman’s body needs her blood vessels to be more lax in order to deliver the baby in a healthy way. The downside of this is the fact that it increases your risk of developing varicose veins.
2. Blood levelsPregnancy causes the amount of blood in a woman’s body to increase massively in order to support the growing baby.
As a result of that increase in blood, your veins will become enlarged.
3. GenesWhen not pregnant, your chances of suffering from varicose veins increases if vein problems are in your genes.
And, the same is true if your family history shows that varicose veins developed in your mom or your grandmother during pregnancy.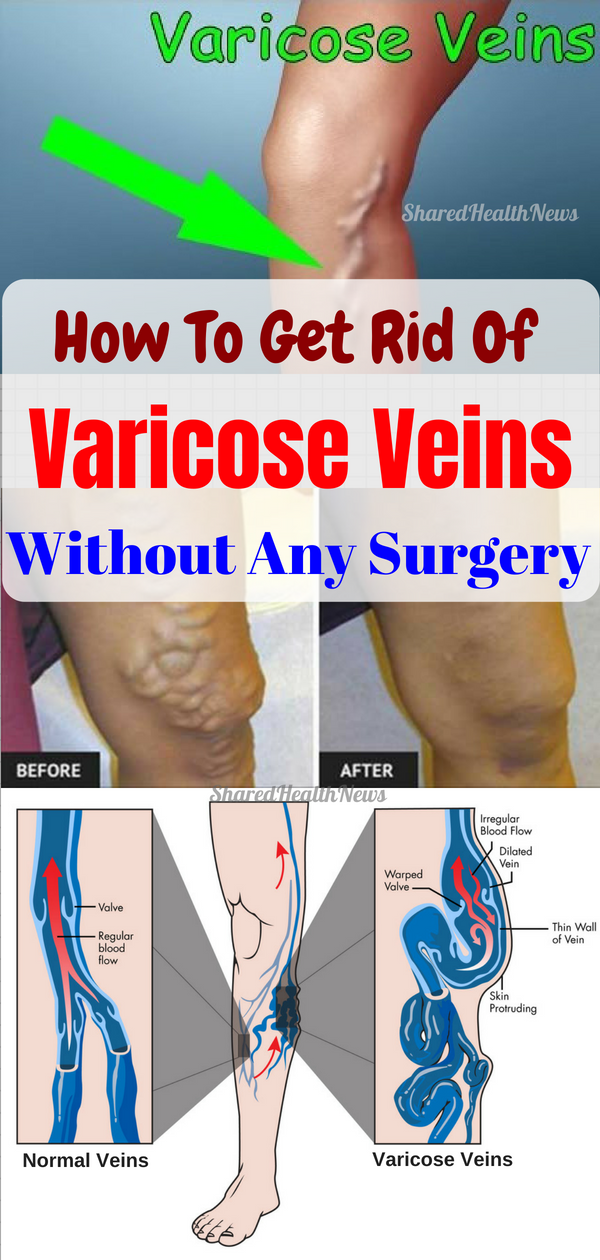
As your due date becomes closer and closer, your body must work harder and harder to go against gravity and circulate blood from your legs up to your heart.
And, as your baby inside continues to grow, your pelvis will be experiencing new levels of pressure, thus affecting the veins that pass through your pelvic area working to circulate your blood.
With this added pressure, you may find that your veins just aren’t working like they used to, and you may see those dreaded blue varicose veins make an appearance.
How To Keep Veins Healthy During Pregnancy
There are things that you can do to help keep your veins healthy during pregnancy, and possibly offset the risk of you developing varicose veins. The key in all of the below is starting to manage your health as soon as possible — the longer you wait, the harder it will be.
Stay in motionOne of the worst things you can do for your veins is sitting or standing in the same place for too long. Take breaks every 30 minutes or so to get moving and get your blood flowing again.
Take breaks every 30 minutes or so to get moving and get your blood flowing again.
Setting up a workout routine at the beginning stages of your pregnancy will do you wonders.
Not only will the extra endorphins help you during a time when your hormones are going to be off-balance, but exercise is also a great way to keep your blood flow consistent and healthy.
The exercise that you choose to do is up to you and your doctor, though if you weren’t much into working out prior to pregnancy, don’t worry — it’s not as if you’ll have to develop an intense workout regimen.
Something as simple as walking for 30-60 minutes a day is a great way to keep your veins healthy, and also help manage your weight.
Compression
StockingsThough far from anything you’ll see in the catwalks of Fashion Week, compression stockings are a fabulous tool during pregnancy.
If you are sitting or standing for long periods of time while pregnant, pop on these socks to keep your circulation moving.
You may also want to throw compression stockings on when heading out for your daily walk.
Elevate Your LegsYou will find during pregnancy that you feel exhausted. Not just mentally, but also physically.
Many women say their legs have just had it by the end of the day, and sometimes aches immensely.
To combat this, and the vein issues that may result, lay down with your legs elevated above your heart.
Elevating your legs helps take the pressure off of your veins and aids your body in the natural blood flow from the veins of your lower legs all the way up to your heart.
Aim to sleep on your left sideDoing this will help keep pressure off of your main veins and help keep your circulation strong.
Stay hydratedDrink plenty of water. This will help prevent the discomfort and strain of constipation.
Avoid high heels and other uncomfortable shoesThe muscles in your calves help to pump blood from your legs and feet back to your heart. Wearing shoes, such as high heels, restricts the movement of your calf muscles which slows circulation and causes blood to pool in your legs, so be sure to keep yourself in comfortable shoes that allow your feet and your veins to breathe.
Wearing shoes, such as high heels, restricts the movement of your calf muscles which slows circulation and causes blood to pool in your legs, so be sure to keep yourself in comfortable shoes that allow your feet and your veins to breathe.
Vein Treatment after Childbirth
If, despite your best efforts, varicose veins appear during pregnancy, do not lose heart. The same methods of prevention can also be used to keep varicose veins from worsening and to alleviate uncomfortable symptoms. And for many women, the varicose veins of pregnancy will disappear on their own in the months following the baby’s birth.
If your varicose veins look like they’re going to stick around, you can pursue minimally invasive treatments to eliminate unsightly vessels for good. At Vein Clinics of America, we offer two of the most popular methods for addressing varicose veins:
Sclerotherapy – During sclerotherapy, a solution is injected into varicose veins, causing them to seal off from the other veins in your leg.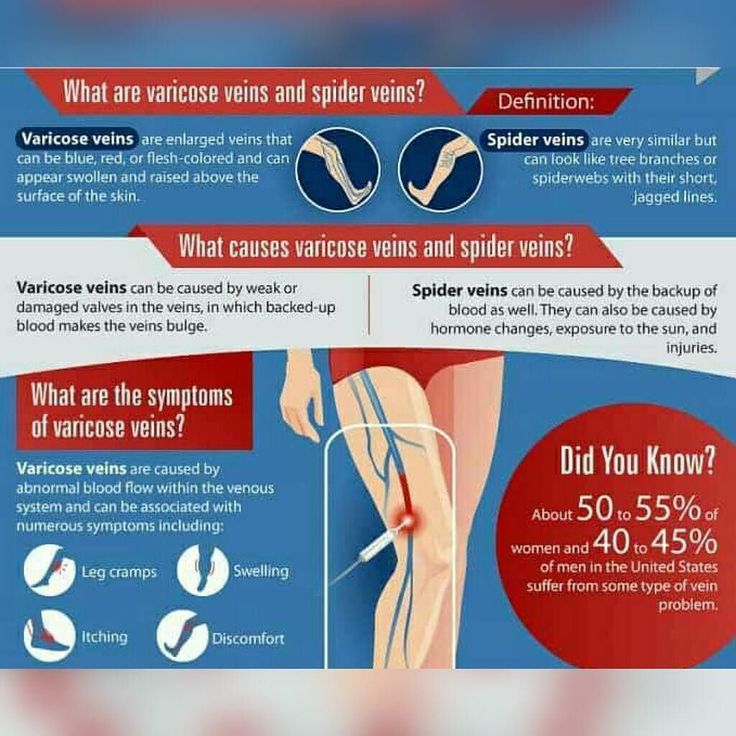 The vein closes over time and is eventually absorbed into your body.
The vein closes over time and is eventually absorbed into your body.
Endovenous Laser Treatment – With ELT, laser energy is delivered into the diseased vein, causing the vein to seal closed and collapse. The vein is reabsorbed by the body, while blood is rerouted to other vessels.
Varicose veins and pregnancy may be a common combination, but you don’t have to take those swollen vessels lying down.
Interested in reading more about varicose veins for women? Explore our collection of topics.
- Why Women Are More Likely To Develop Varicose Veins
- Risk Factors of Chronic Venous Insufficiency (CVI)
- The Stages of Chronic Venous Insufficiency
- Is There a Cure for Venous Insufficiency?
- 8 Signs It’s Time to See a Vein Specialist
Medically Reviewed by
Dr. Satish Vayuvegula
Dr. Satish Vayuvegula is the National Medical Director at Vein Clinics of America. Certified by the American Board of Venous & Lymphatic Medicine, Dr.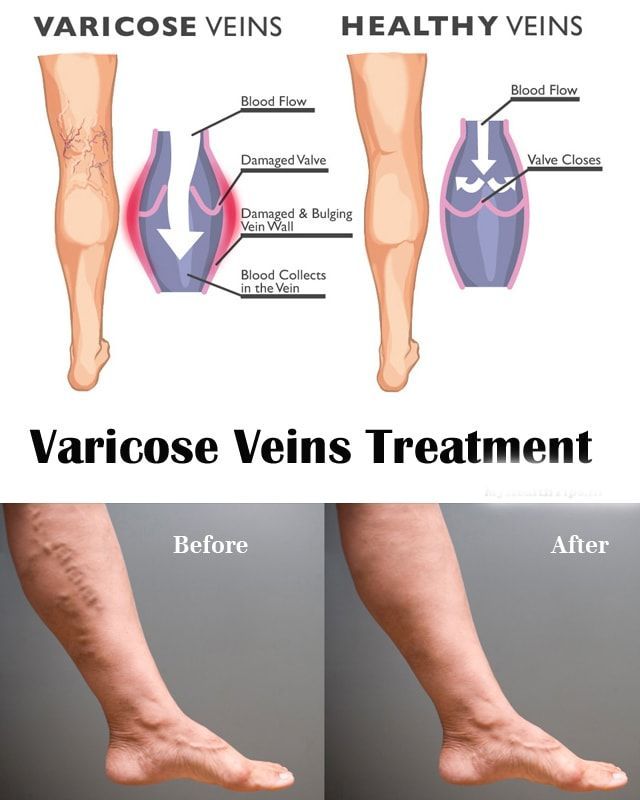 Satish Vayuvegula is recognized as a physician who has met rigorous standards of knowledge and extensive training in phlebology, the diagnosis and treatment of varicose vein disease and related disorders. Dr. Satish also shares his passion and expertise by serving as a board member of the American Vein and Lymphatic Society, the predominant national organization for venous and lymphatic disease.
Satish Vayuvegula is recognized as a physician who has met rigorous standards of knowledge and extensive training in phlebology, the diagnosis and treatment of varicose vein disease and related disorders. Dr. Satish also shares his passion and expertise by serving as a board member of the American Vein and Lymphatic Society, the predominant national organization for venous and lymphatic disease.Varicose veins during pregnancy - what to do and how to treat varicose veins in the legs
Varicose veins are persistent and irreversible enlargement resulting from pathological changes in the walls and valves of blood vessels. The superficial veins in the legs most often expand, since they have increased pressure when standing and walking. Varicose veins during pregnancy is one of the diseases that can appear or progress during the period of gestation. Because of this, women get sick 4 times more often than men.
Causes
The following reasons contribute to the occurrence of varicose veins during pregnancy:
- Violation of the outflow of blood from the veins of the lower extremities.
 This is because the growing uterus presses on the inferior vena cava - a large abdominal vein that collects blood from the lower half of the trunk and lower extremities.
This is because the growing uterus presses on the inferior vena cava - a large abdominal vein that collects blood from the lower half of the trunk and lower extremities. - During pregnancy, the blood is more viscous, flows more slowly, this also contributes to venous congestion.
- The increase in body weight during gestation increases the load on the legs.
The development of varicose veins is promoted by wearing high-heeled shoes, prolonged work in a standing position, lifting weights, and overweight.
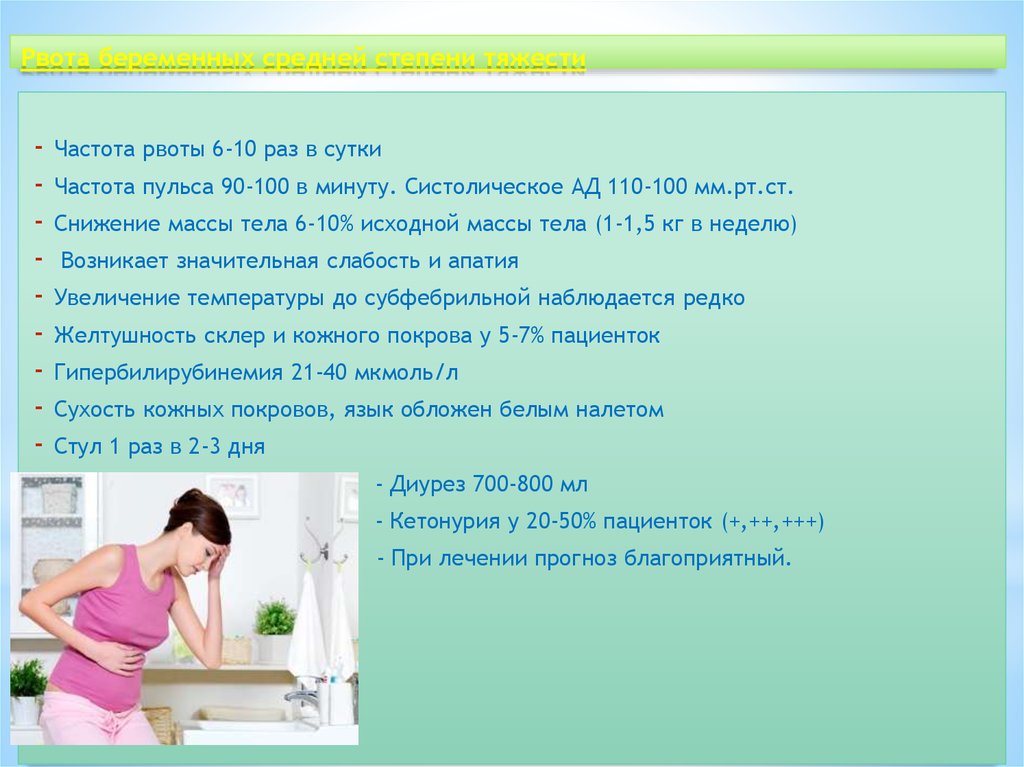
Symptoms
The first symptom is a visible increase in the vessels of the lower extremities. The veins are blue or purple, tortuous, protrude above the surface of the skin, may be serpentine or knobby (nodular) in shape. At the initial stage of the disease, a woman is only concerned about a cosmetic defect.
Other complaints follow. Edema appears, increasing in the evening and decreasing or completely disappearing after rest and a night's sleep. At night, convulsions may disturb. When walking, rapid fatigue is observed, there may be a feeling of fullness and pain.
At night, convulsions may disturb. When walking, rapid fatigue is observed, there may be a feeling of fullness and pain.
Varicose veins of the lower extremities are observed in 50% of pregnant women, but not all of them suffer from true varicose veins, when irreversible changes appear in the venous wall. For most, the disease is functional in nature, that is, it is temporary, and after childbirth, when the factors that prevent normal venous outflow are eliminated, the tubes return to normal. This usually happens within a year.
Regression does not occur if the predisposition is independent of pregnancy. In this case, close relatives usually have varicose veins, or the woman herself had some symptoms even before conception.
Diagnostics
As you know, the “gold standard” for diagnosing pathology is ultrasound duplex scanning (USDS) of the veins of the lower extremities. This is a safe procedure for the expectant mother. Experienced obstetricians and gynecologists strongly recommend that pregnant women visit a phlebologist in the early stages of pregnancy, which contributes to the early prevention of complications of varicose veins in the postpartum period.
Stockings for varicose veins during pregnancy
During pregnancy, it is recommended to wear special compression (anti-varicose) tights and stockings. They need to be put on in a prone position, slightly lifting the leg up. There are 4 compression classes (pressure levels):
- 18-21 mmHg
- 23-32 mmHg
- 33-48 mmHg
- over 49 mmHg
During pregnancy, it is recommended to use compression class 1-2. The third class of compression hosiery is used for the late stage of leg varicose veins, the fourth class - only for severe congenital anomalies of the venous system.
Tights should be specially designed for expectant mothers so that they do not put pressure on the growing belly, but support it.
How much to wear?
After 20 weeks, you need to wear a bandage. It supports the uterus and reduces pressure on the large vessels of the abdominal cavity, thereby improving the outflow of blood from the lower half of the body.
Compression underwear and a bandage should be bought in pharmacies, it is important to choose the right size for them.
Exercise
It is recommended to attend gymnastics for pregnant women or do exercises at home. Particularly good prevention of varicose veins are classes in the pool. Sports strengthen the walls of blood vessels and improve blood flow. In addition, gymnastics is the prevention of overweight.
A contrast shower on the calf muscles is useful.
If you think you have a predisposition to varicose veins, you should avoid saunas and thermal treatments.
As often as possible, try to give your legs an elevated position. Don't sit cross-legged for long periods of time.
Wear comfortable shoes with small heels.
You can use creams for pregnant women "to relieve fatigue from the legs", such creams usually contain plant substances that, with regular use, strengthen the walls of superficial veins.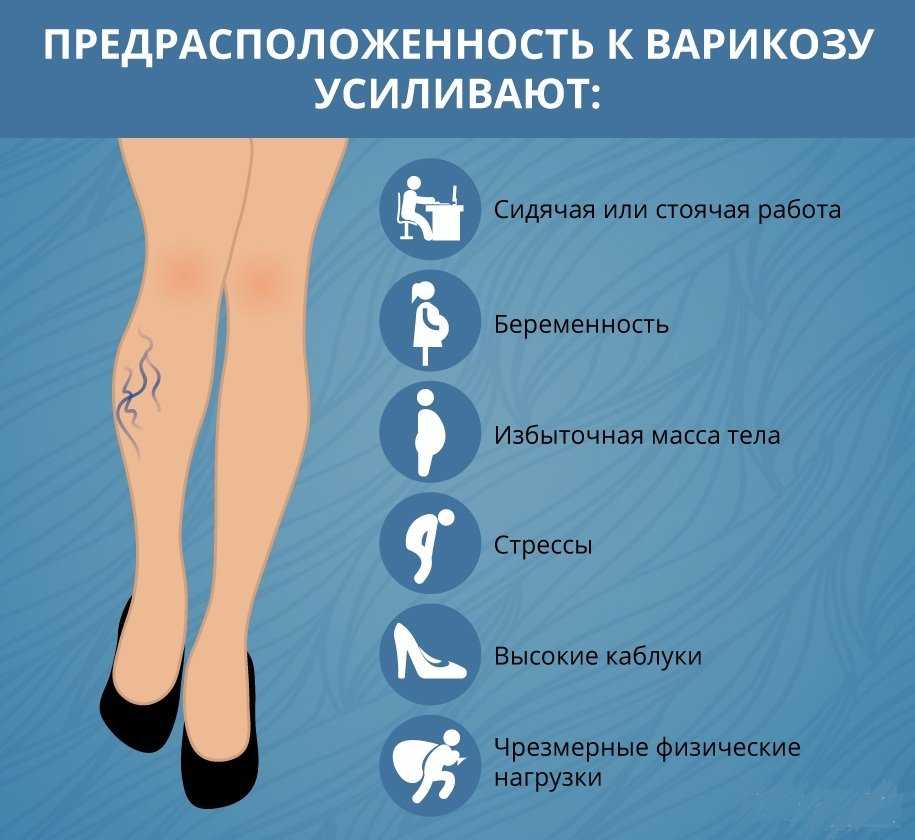
Treatment
Treatment of true varicose veins is surgical. During pregnancy, surgical treatment is carried out only for emergency indications, in view of the development of complications (thrombophlebitis).
A modern method of treatment is sclerotherapy, when a chemical substance is injected into the lumen of the vein, which leads to sclerosis and closure of its lumen. Endovasal methods are also minimally invasive treatments performed on an outpatient basis (described in the relevant sections of our website). They may be an alternative to surgical treatment. However, during pregnancy and lactation are also contraindicated.
All other methods are aimed only at preventing the disease from developing and temporarily reducing symptoms.
Most often, various ointments and gels are used, which are applied to the affected limb. For example, heparin-containing ointments reduce blood clotting and prevent the formation of blood clots. Venotonics (allowed only from the second trimester of pregnancy) have a decongestant and anti-inflammatory effect and strengthen the walls of blood vessels.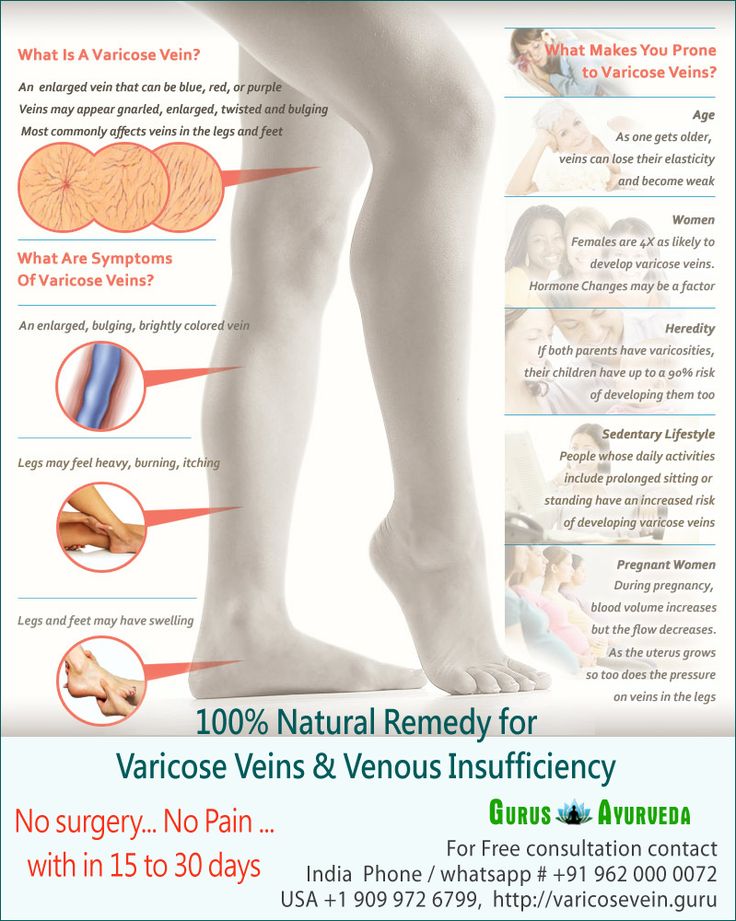
The diagnostic equipment used in our center has been tested in ROSTEST and has an appropriate conclusion about the absence of contraindications for use in pregnant women and children.
In the medical center "Yuzhny" they are very kind to expectant mothers and experienced phlebologists are well versed in the methods of diagnosing CVI and the secrets of preserving your beautiful legs after childbirth.
Varicose veins during pregnancy - what to do and how to treat
Veins are actively involved in the complex 9-month pregnancy process, and their changes are significant. Even with complete medical supervision, there is a risk of developing venous insufficiency.
Pregnancy is accompanied by profound changes throughout the female body. One of the first effects of pregnancy is an increase in the load on the veins of the pelvis and lower extremities. Therefore, many pregnant women develop varicose veins, which sometimes disappear after childbirth.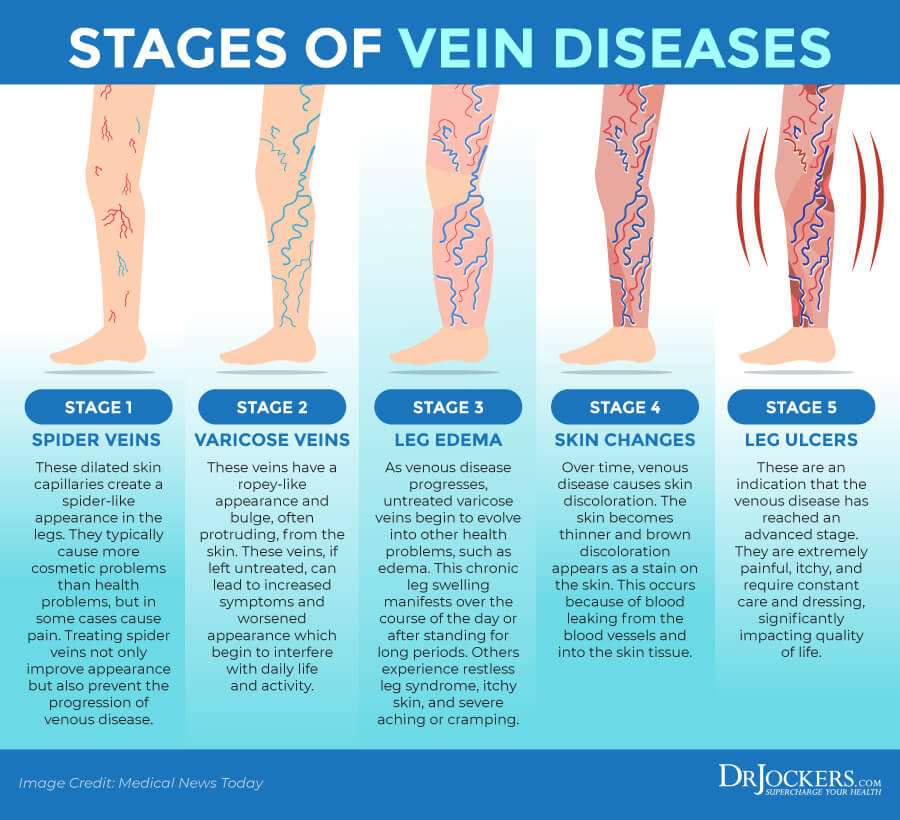 This varicose vein is accompanied by discomfort, a feeling of heaviness, pain when walking, but women are mainly concerned with noticeable skin changes and varicose coloration of the legs and ankles, which remain after pregnancy.
This varicose vein is accompanied by discomfort, a feeling of heaviness, pain when walking, but women are mainly concerned with noticeable skin changes and varicose coloration of the legs and ankles, which remain after pregnancy.
From sickness to sickness
Many pregnant women are familiar with the feeling of malaise, accompanied by discomfort in the lower extremities. Functional chronic venous insufficiency is the first stage of venous disease with a feeling of heaviness in the lower extremities, sometimes with itching, paresthesias and, in some cases, convulsions, often nocturnal.
The possibility of thrombosis in pregnant women is 3-5 times higher than in other women. Sometimes blockage of the veins leads to their inflammation - thrombophlebitis. Blood clots that form in this case in the veins can cause a serious and dangerous disease - pulmonary embolism. In addition, the risk of developing thrombosis remains for another 1.5 months after childbirth, especially if they are severe.
Should I go to the doctor?
There are five groups of factors that affect the body of a pregnant woman, which explain the need for observation by a phlebologist.
Mechanical factor
An enlarged uterus is a barrier to blood circulation, as it compresses the inferior vena cava, pressing it against the spinal column and iliac muscle. This is of particular importance at rest, when a sharp decrease in venous outflow can lead to postural shock, well known to gynecologists. The anatomical structure of the iliac vein, which crosses the right iliac artery, explains the high incidence of thrombosis of the left limb (Cocket's syndrome).
Circulatory factor
An increase in blood volume and outflow of blood from the heart leads to an increase in the load on the vessels, especially veins, and their expansion. This is especially important for the veins of the lower extremities and the vaginal area.
Hormonal factors
Progesterone, due to its relaxing effect on smooth muscle fibers, leads not only to a decrease in the tone of the venous wall, but also to a decrease in the tone of the urethra, bladder and small intestine.
Hemostatic factors
Changes in the hemostasis system always occur in the direction of increased coagulability (increased fibrinogen and factor III levels, increased platelet activity and decreased fibrinolytic activity).
Hemorheological factors
Blood viscosity increases despite a decrease in hematocrit.
Other contributing factors
In addition to the above factors associated with pregnancy, there are other contributing factors such as family history, sedentary lifestyle, immobile posture while working, driving, too low or high thin heels, obesity, underfloor heating, hot baths, and multiple pregnancies with short intervals between them.
How to prevent illness?
Pregnant women, regardless of risk factors and venous manifestations, always need lifestyle modification: avoidance of standing still, sitting in a low chair, hot baths and sunbathing, adaptive exercises such as easy walking, leg movement when sitting, contrast showers, elevated the position of the lower extremities in a state of rest.