Common weeks for miscarriage
Miscarriage Rates by Week: Causes and Risks
Miscarriage Rates by Week: Causes and RisksMedically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
Overview
Miscarriage is a word used to describe the early loss of a pregnancy before 20 weeks of pregnancy. It usually happens in the first trimester.
Unfortunately, between 10 and 15 percent of known pregnancies end in miscarriage.
You may have heard of couples waiting to announce a pregnancy until the risk of having a miscarriage is lower. The further you are into the pregnancy, the less likely you are to miscarry.
Read on to learn about what causes miscarriages and the risk for miscarriage during pregnancy.
Causes
Dr. Kaylen Silverberg, a Texas-based fertility specialist, says miscarriages are very common.
“Women think that when they have one miscarriage, they are doomed to miscarry again,” he says. However, the likelihood of having recurrent miscarriages (at least 2 or 3) is low, only occurring in about 1 percent of women.
Studies have shown an increased risk for miscarriage in women who have had recurrent miscarriages in the past. Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Several factors have to be accounted for in these cases, however. This includes maternal age and other medical conditions present. Most doctors will begin to investigate for a cause after you have had two to three losses. This will include reviewing your medical history in detail and performing certain tests.
Here are the five most common miscarriage causes.
Genetics
When the sperm and egg meet, the cells come together. They then begin to divide to start forming the genetic material that makes up a person.
Each of us is supposed to have 46 total chromosomes. That’s 23 from one parent and 23 from the other. If something goes wrong when the cells are dividing, a chromosome may be missing or repeated.
About 50 percent of all first trimester miscarriages are because of chromosomal abnormalities. This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
Infections
Uterus or cervix infections can be dangerous to a developing baby and lead to miscarriage. Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Some of these infections include:
- listeria
- parvovirus B19
- toxoplasma gondii
- rubella
- herpes simplex
- cytomegalovirus
Anatomic problems
This refers to defects of the uterus cavity. If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
Clotting disorders
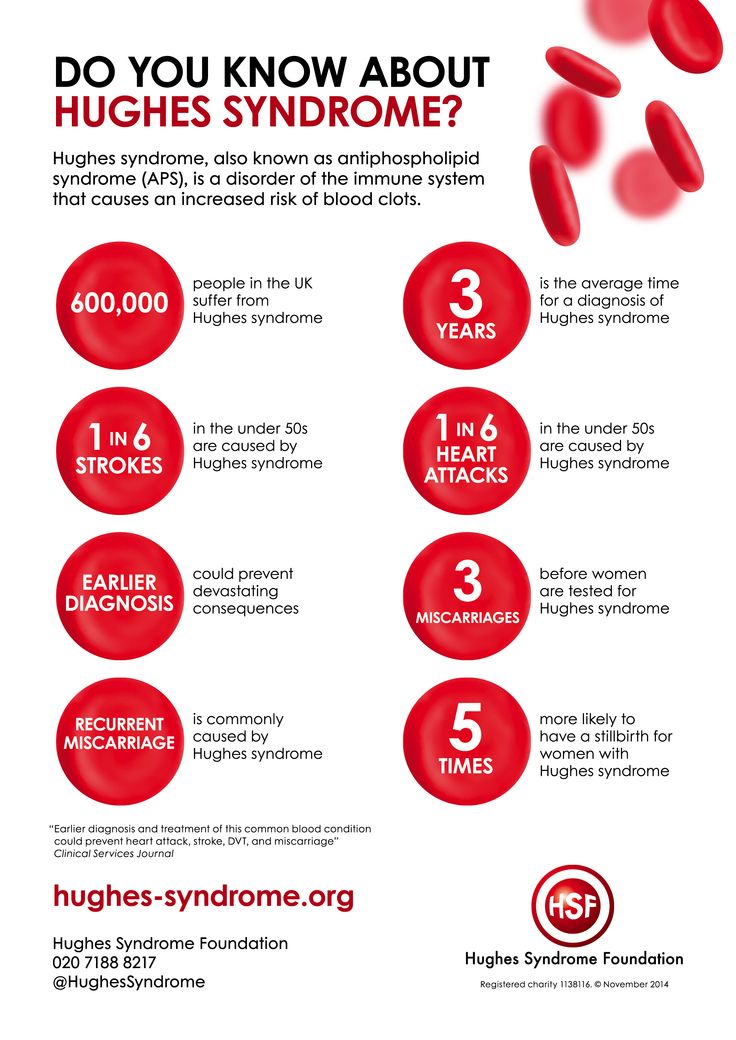
Clotting disorders are conditions that cause your body to form more blood clots than normal. Examples include lupus anticoagulant and antiphospholipid syndrome.
In the case of pregnancy, blood clots can form in the placenta. This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
Risk rates
The first trimester of pregnancy is considered weeks 0 to 13. About 80 percent of miscarriages happen in the first trimester. Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Weeks 0 to 6
These early weeks mark the highest risk of miscarriage. A woman can have a miscarriage in the first week or two without realizing she’s pregnant. It may even seem like a late period.
Age plays a role in a woman’s risk factor. One study indicated that compared to women younger than 35:
- Women ages 35 to 39 have a 75 percent increase in risk
- Women ages 40 and older are at 5 times the risk
Weeks 6 to 12
Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent.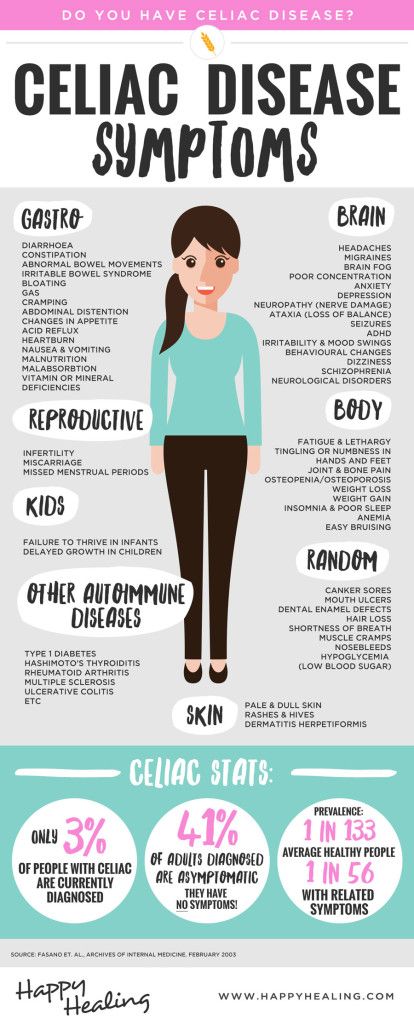 According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
Weeks 13 to 20
By week 12, the risk may fall to 5 percent. But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
Signs and symptoms
The most common signs of a miscarriage are bleeding and cramping that are felt in the abdomen, pelvis, or lower back.
Some women have spotting (light bleeding) during pregnancy. A few drops or light flow of brown or dark red doesn’t necessarily mean trouble. But call your doctor right away if you see bright red blood, particularly in large amounts.
Cramping can also happen in normal pregnancies. But if it’s severe or occurring more on one side of the pelvis, you should call your doctor.
Prevention
The majority of miscarriages are the result of genetic abnormalities or other health factors that are beyond our control. For that reason, there isn’t a whole lot you can do for prevention.
For that reason, there isn’t a whole lot you can do for prevention.
The best thing you can do is to keep yourself as healthy as possible before trying to conceive and throughout your pregnancy. Here are some tips to staying healthy during pregnancy:
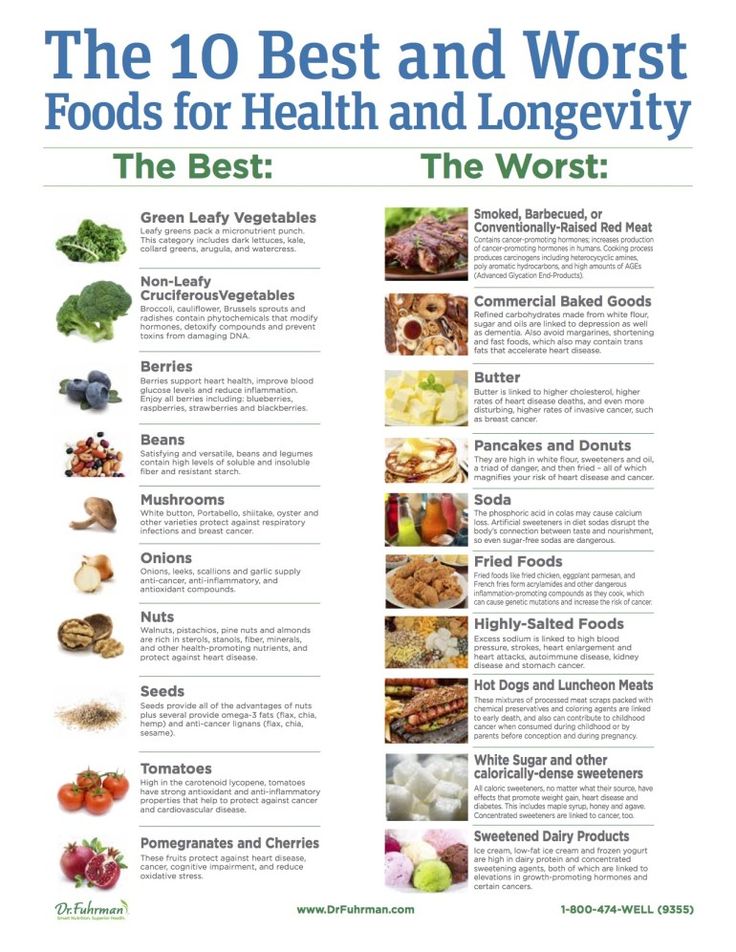
- Eat a well-balanced diet.
- Exercise regularly.
- Avoid alcohol, recreational drugs, and cigarette smoking.
- Reduce caffeine to 200 mg or less per day.
- Get regular prenatal visits.
If you’re worried about your risk of having a pregnancy affected by chromosomal issues, you can speak to your doctor about genetic testing before trying to conceive. A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
The takeaway
The experience of a miscarriage can be physically and emotionally painful. But it’s important to remember that it’s not your fault. Talk to trusted friends and family, and ask for help when you need it.
Talk to trusted friends and family, and ask for help when you need it.
Your doctor may be able to recommend a support group or therapist in your area. There are also many online organizations and support groups like March of Dimes that offer a safe place to share your story and grieve with others.
Share on Pinterest
Rena Goldman is a journalist and editor who lives in Los Angeles. She writes about health, wellness, interior design, small business, and the grassroots movement for campaign finance reform. When she’s not glued to a computer screen, Rena likes to explore new hiking spots in Southern California. She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
Last medically reviewed on October 3, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chromosomal conditions. (2018).
marchofdimes.org/baby/chromosomal-conditions.aspx - Early pregnancy loss: FAQs. (2015).
acog.org/Patients/FAQs/Early-Pregnancy-Loss - Early pregnancy loss: Practice bulletin. (2015).
acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Early-Pregnancy-Loss - Ford HB, et al. (2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy.
ncbi.nlm.nih.gov/pmc/articles/PMC2709325/ - Maconochie N, et al. (2007). Risk factors for first-trimester miscarriage—results from a UK-population-based case-control study.
obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2006.01193.x - Miscarriage. (2017).
marchofdimes.org/complications/miscarriage.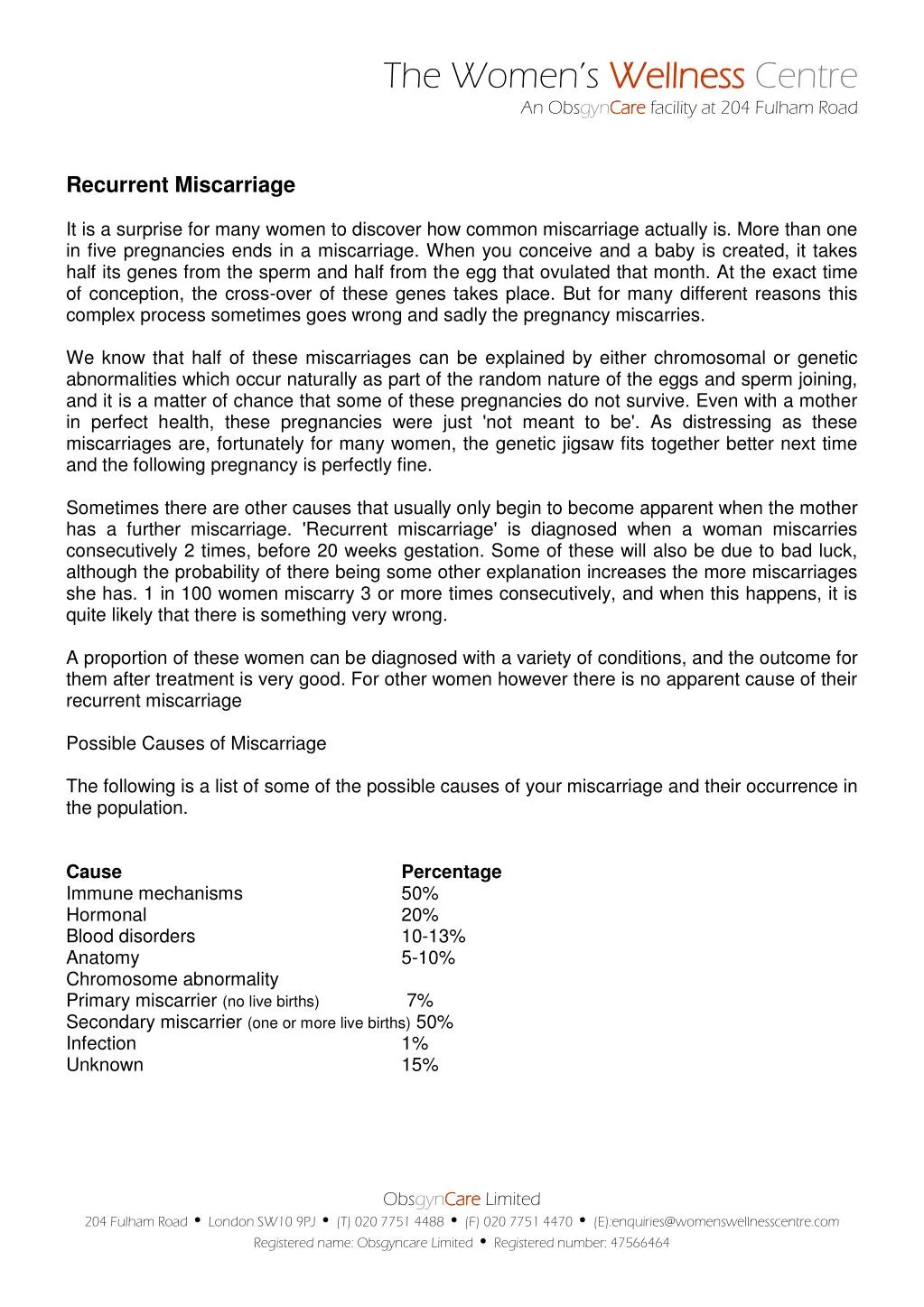 aspx
aspx - Regan L, et al. (1989). Influence of past reproductive performance on risk of spontaneous abortion.
uptodate.com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19 - Repeated miscarriages. (2016).
acog.org/Patients/FAQs/Repeated-Miscarriages - Tong S, et al. (2008). Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit.
ncbi.nlm.nih.gov/pubmed/18310375 - Tulandi T. (2018). Patient information: Miscarriage (beyond the basics).
uptodate.com/contents/miscarriage-beyond-the-basics
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Rena Goldman
Medically Reviewed By
Holly Ernst, PA-C
Share this article
Medically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
related stories
How to Tell if You’re Having a Miscarriage Without Bleeding
When Is the Best Time to Announce Your Pregnancy?
What’s a Chemical Pregnancy?
How Long Does a Miscarriage Last?
Late Miscarriage: Symptoms and Finding Support
Read this next
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
When Is the Best Time to Announce Your Pregnancy?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
If you’re expecting, you might be wondering when it’ll be safe to tell family and friends. Here’s how to decide when to share the news of your…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Late Miscarriage: Symptoms and Finding Support
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
It can be devastating to experience a miscarriage in your second trimester. Find support and information here.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
Threatened Abortion (Threatened Miscarriage)
Threatened abortion refers to vaginal bleeding during the first 20 weeks of pregnancy. Learn about its symptoms, risk factors, and diagnosis.

READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
Miscarriage Rates by Week: Causes and Risks
Miscarriage Rates by Week: Causes and RisksMedically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
Overview
Miscarriage is a word used to describe the early loss of a pregnancy before 20 weeks of pregnancy. It usually happens in the first trimester.
It usually happens in the first trimester.
Unfortunately, between 10 and 15 percent of known pregnancies end in miscarriage.
You may have heard of couples waiting to announce a pregnancy until the risk of having a miscarriage is lower. The further you are into the pregnancy, the less likely you are to miscarry.
Read on to learn about what causes miscarriages and the risk for miscarriage during pregnancy.
Causes
Dr. Kaylen Silverberg, a Texas-based fertility specialist, says miscarriages are very common.
“Women think that when they have one miscarriage, they are doomed to miscarry again,” he says. However, the likelihood of having recurrent miscarriages (at least 2 or 3) is low, only occurring in about 1 percent of women.
Studies have shown an increased risk for miscarriage in women who have had recurrent miscarriages in the past. Conversely, some studies indicate that having a successful pregnancy before a current pregnancy may decrease the risk for miscarriage in the current pregnancy.
Several factors have to be accounted for in these cases, however. This includes maternal age and other medical conditions present. Most doctors will begin to investigate for a cause after you have had two to three losses. This will include reviewing your medical history in detail and performing certain tests.
Here are the five most common miscarriage causes.
Genetics
When the sperm and egg meet, the cells come together. They then begin to divide to start forming the genetic material that makes up a person.
Each of us is supposed to have 46 total chromosomes. That’s 23 from one parent and 23 from the other. If something goes wrong when the cells are dividing, a chromosome may be missing or repeated.
About 50 percent of all first trimester miscarriages are because of chromosomal abnormalities. This can occur more frequently in women who are considered advanced maternal age, or greater than 35 years old at pregnancy term.
Infections
Uterus or cervix infections can be dangerous to a developing baby and lead to miscarriage. Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Other infections that may pass to the baby or placenta can also affect a developing pregnancy and may lead to loss.
Some of these infections include:
- listeria
- parvovirus B19
- toxoplasma gondii
- rubella
- herpes simplex
- cytomegalovirus
Anatomic problems
This refers to defects of the uterus cavity. If a woman’s uterus didn’t form correctly when she was developing, it may be unable to support a healthy pregnancy.
Clotting disorders
Clotting disorders are conditions that cause your body to form more blood clots than normal. Examples include lupus anticoagulant and antiphospholipid syndrome.
In the case of pregnancy, blood clots can form in the placenta. This prevents nutrition and oxygen from getting to the baby-to-be, and prevents waste from being carried away.
Risk rates
The first trimester of pregnancy is considered weeks 0 to 13. About 80 percent of miscarriages happen in the first trimester.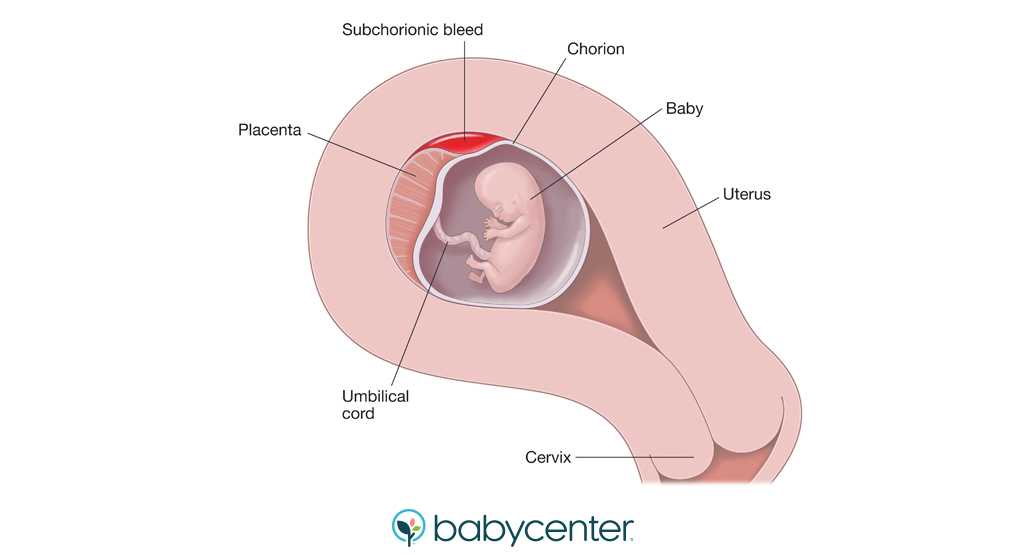 Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Losses after this time occur less often. March of Dimes reports a miscarriage rate of only 1 to 5 percent in the second trimester.
Weeks 0 to 6
These early weeks mark the highest risk of miscarriage. A woman can have a miscarriage in the first week or two without realizing she’s pregnant. It may even seem like a late period.
Age plays a role in a woman’s risk factor. One study indicated that compared to women younger than 35:
- Women ages 35 to 39 have a 75 percent increase in risk
- Women ages 40 and older are at 5 times the risk
Weeks 6 to 12
Once a pregnancy makes it to 6 weeks and has confirmed viability with a heartbeat, the risk of having a miscarriage drops to 10 percent. According to a 2008 study, the risk for miscarriage falls quickly with further gestational age. However, this was not specifically studied in patients with other risk factors for miscarriage.
Weeks 13 to 20
By week 12, the risk may fall to 5 percent. But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
But keep in mind that it doesn’t really fall below that because complications can happen during pregnancy.
Signs and symptoms
The most common signs of a miscarriage are bleeding and cramping that are felt in the abdomen, pelvis, or lower back.
Some women have spotting (light bleeding) during pregnancy. A few drops or light flow of brown or dark red doesn’t necessarily mean trouble. But call your doctor right away if you see bright red blood, particularly in large amounts.
Cramping can also happen in normal pregnancies. But if it’s severe or occurring more on one side of the pelvis, you should call your doctor.
Prevention
The majority of miscarriages are the result of genetic abnormalities or other health factors that are beyond our control. For that reason, there isn’t a whole lot you can do for prevention.
The best thing you can do is to keep yourself as healthy as possible before trying to conceive and throughout your pregnancy.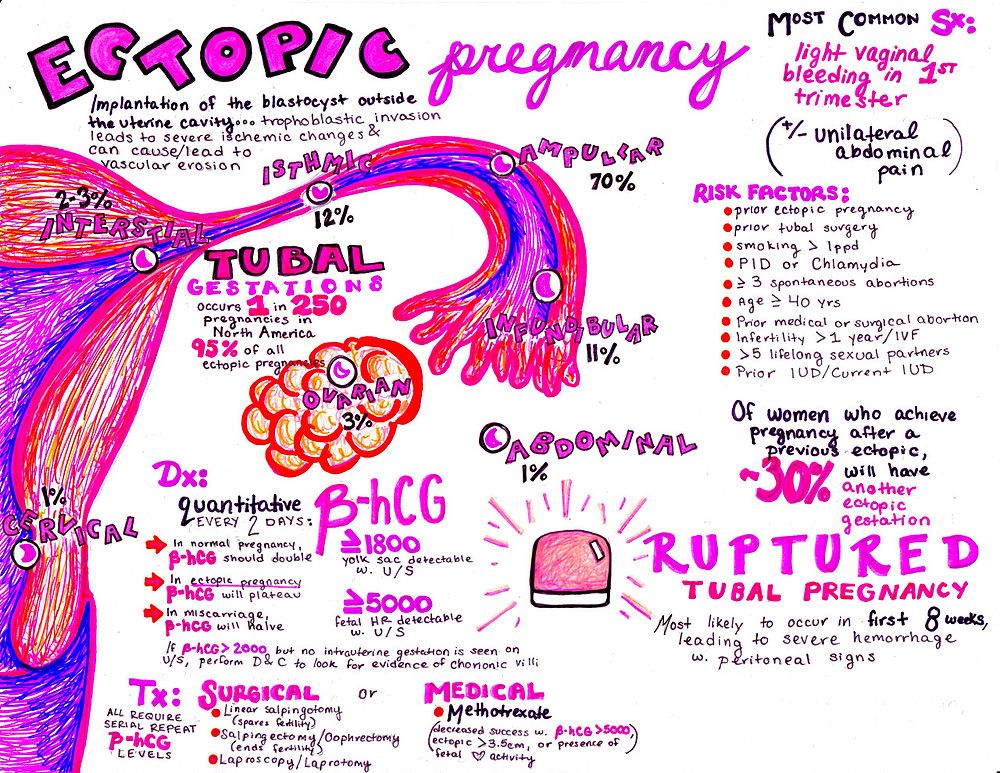 Here are some tips to staying healthy during pregnancy:
Here are some tips to staying healthy during pregnancy:
- Eat a well-balanced diet.
- Exercise regularly.
- Avoid alcohol, recreational drugs, and cigarette smoking.
- Reduce caffeine to 200 mg or less per day.
- Get regular prenatal visits.
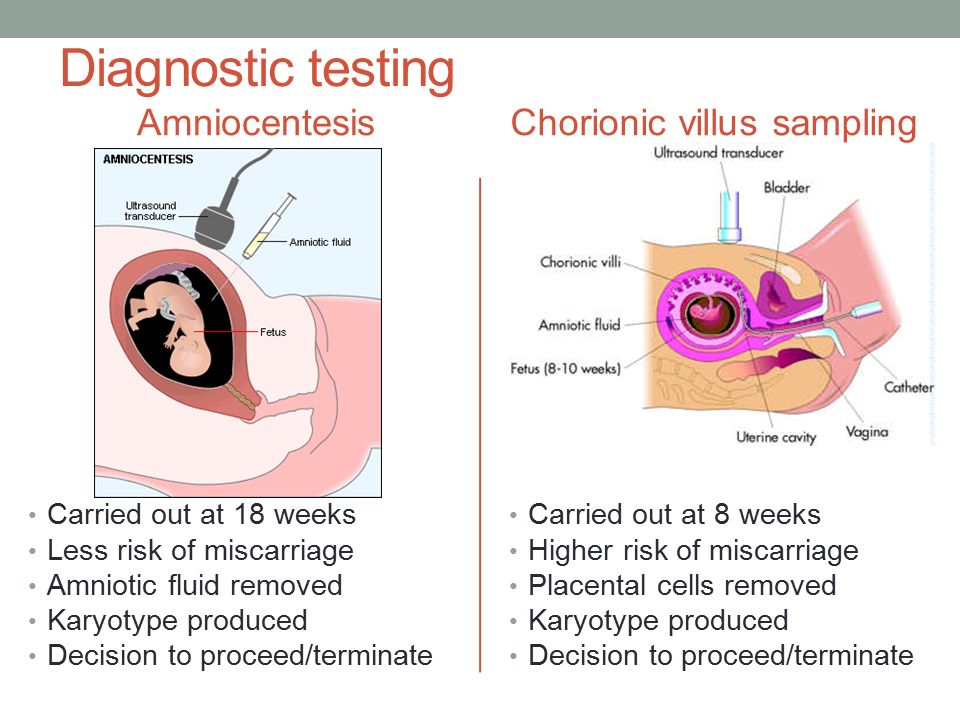
If you’re worried about your risk of having a pregnancy affected by chromosomal issues, you can speak to your doctor about genetic testing before trying to conceive. A blood sample will be taken from one or both partners, and then sent to a laboratory to be evaluated for major genetic disorders. This testing and other evaluation are generally done after someone has recurrent losses.
The takeaway
The experience of a miscarriage can be physically and emotionally painful. But it’s important to remember that it’s not your fault. Talk to trusted friends and family, and ask for help when you need it.
Your doctor may be able to recommend a support group or therapist in your area. There are also many online organizations and support groups like March of Dimes that offer a safe place to share your story and grieve with others.
Share on Pinterest
Rena Goldman is a journalist and editor who lives in Los Angeles. She writes about health, wellness, interior design, small business, and the grassroots movement for campaign finance reform. When she’s not glued to a computer screen, Rena likes to explore new hiking spots in Southern California. She also enjoys walking in her neighborhood with her dachshund, Charlie, and admiring the landscaping and architecture of LA homes she can’t afford. Follow her on Twitter: @ReeRee_writes
Last medically reviewed on October 3, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Chromosomal conditions. (2018).
marchofdimes.org/baby/chromosomal-conditions.aspx - Early pregnancy loss: FAQs. (2015).
acog.org/Patients/FAQs/Early-Pregnancy-Loss - Early pregnancy loss: Practice bulletin. (2015).
acog.org/Resources-And-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Early-Pregnancy-Loss - Ford HB, et al. (2009). Recurrent pregnancy loss: Etiology, diagnosis, and therapy.
ncbi.nlm.nih.gov/pmc/articles/PMC2709325/ - Maconochie N, et al. (2007). Risk factors for first-trimester miscarriage—results from a UK-population-based case-control study.
obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2006.01193.x - Miscarriage. (2017).
marchofdimes.org/complications/miscarriage.aspx - Regan L, et al. (1989). Influence of past reproductive performance on risk of spontaneous abortion.
uptodate. com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19
com/contents/definition-and-etiology-of-recurrent-pregnancy-loss/abstract/19 - Repeated miscarriages. (2016).
acog.org/Patients/FAQs/Repeated-Miscarriages - Tong S, et al. (2008). Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit.
ncbi.nlm.nih.gov/pubmed/18310375 - Tulandi T. (2018). Patient information: Miscarriage (beyond the basics).
uptodate.com/contents/miscarriage-beyond-the-basics
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
Written By
Rena Goldman
Medically Reviewed By
Holly Ernst, PA-C
Share this article
Medically reviewed by Holly Ernst, PA-C — By Rena Goldman on October 3, 2018
related stories
How to Tell if You’re Having a Miscarriage Without Bleeding
When Is the Best Time to Announce Your Pregnancy?
What’s a Chemical Pregnancy?
How Long Does a Miscarriage Last?
Late Miscarriage: Symptoms and Finding Support
Read this next
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIA miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
When Is the Best Time to Announce Your Pregnancy?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
If you’re expecting, you might be wondering when it’ll be safe to tell family and friends. Here’s how to decide when to share the news of your…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
A chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
Late Miscarriage: Symptoms and Finding Support
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
It can be devastating to experience a miscarriage in your second trimester. Find support and information here.
READ MORE
Everything You Need to Know About Miscarriage
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
A miscarriage is the loss of a fetus during pregnancy. It’s also an event that’s more common than you think. Learn about causes, types, symptoms, and…
READ MORE
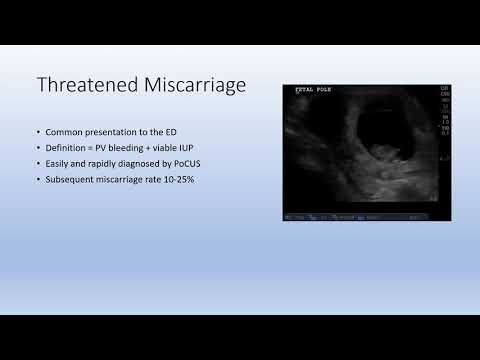
Threatened Abortion (Threatened Miscarriage)
Threatened abortion refers to vaginal bleeding during the first 20 weeks of pregnancy. Learn about its symptoms, risk factors, and diagnosis.
READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
Depression After a Miscarriage
Medically reviewed by Janine Kelbach, RNC-OB
It’s not uncommon to experience depression after the sudden loss of a pregnancy. Learn how to cope with the depression associated with miscarriage.
READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
Pregnancy: Terrible word THREAT! Let's save ourselves!
Our today's conversation will touch upon recommendations for a pregnant woman who is faced with such a complication of pregnancy as a threatened abortion.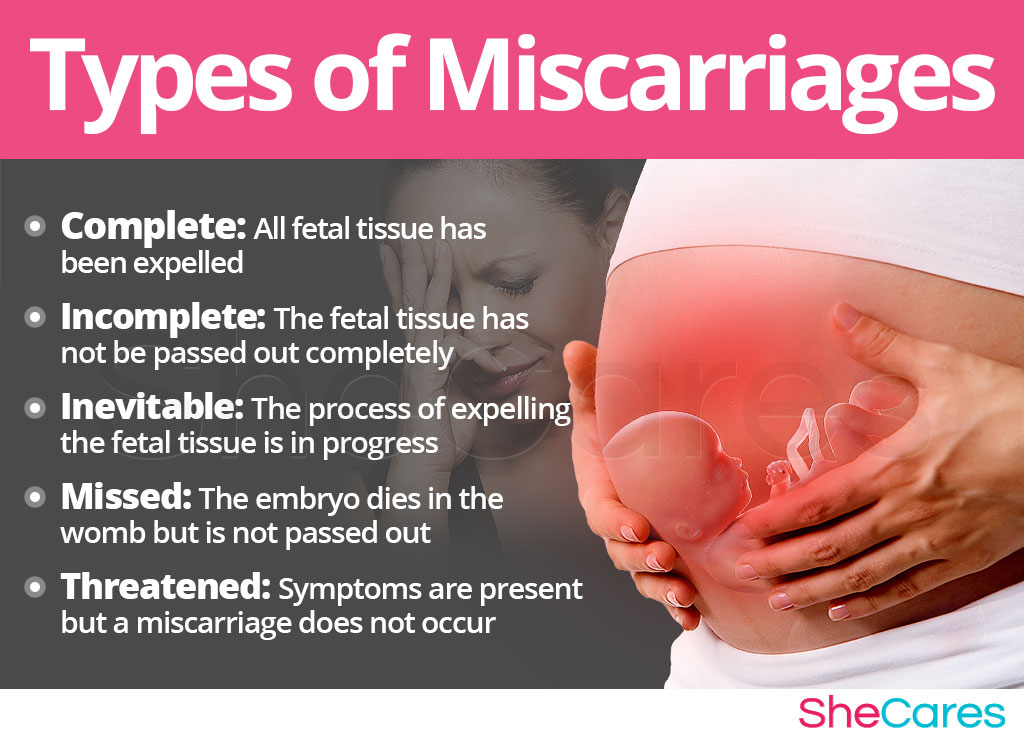
Pregnancy is a physiological process for the female body. If a woman is young (18-30 years old) and healthy, then, as a rule, pregnancy proceeds without complications. Recently, in the world and in our country, there has been a sharp deterioration in the health of women of reproductive age.
Complications of pregnancy can be divided into 3 groups for a better understanding of the reader (these are not standards).
- Firstly, the complications associated with the pregnancy itself, if it were not for this condition, then there would be no complication - the threat of abortion (the threat of premature birth).
- Secondly, these are complications associated with a disease (for example, rubella) that occurred during pregnancy.
- Thirdly, these are complications that arose in a woman who suffered from a particular disease before pregnancy (perhaps the first exacerbation of this disease is associated with pregnancy).
The most unpleasant psychological and physical complications are threatened miscarriage . If this happens in the early stages, then the term is used, the threat of termination of pregnancy ", if in the later stages (after 28 weeks), then " the threat of premature birth.
If this happens in the early stages, then the term is used, the threat of termination of pregnancy ", if in the later stages (after 28 weeks), then " the threat of premature birth.
What to do if there is a threat of termination of pregnancy
In some countries, including Russia, it is customary to keep a pregnancy of any term; accordingly, if a woman notes spotting during pregnancy, then she immediately should see a doctor during the daytime or seek help from the emergency team at night. But the question of the expediency of maintaining pregnancy with the onset of bleeding up to 12 weeks remains open, because. it is known that 70-80% of pregnancies terminated during this period are associated with chromosomal pathologies, sometimes incompatible with life. Those. It can be said that the body itself corrects its mistakes.
Reasons for termination of pregnancy
Termination of pregnancy may also be associated with cervical incompetence . Those. its upper part may not be tightly closed, i.e. unable to play the role of a "castle". This condition may be caused by trauma during previous births or during abortions ( even if it was a single ). In this case, treatment is carried out in a hospital, and in the future, pregnancy is observed by an outpatient doctor. A woman can be stitched on the cervix if such a diagnosis is made at 16-20 weeks or a special retaining ring is placed if complaints appear later than this period. The suture or ring is removed at the time of the onset of labor, i.e. with the appearance of regular contractions or the outflow of amniotic fluid. However, this procedure can be performed two weeks before the expected date of birth.
Those. its upper part may not be tightly closed, i.e. unable to play the role of a "castle". This condition may be caused by trauma during previous births or during abortions ( even if it was a single ). In this case, treatment is carried out in a hospital, and in the future, pregnancy is observed by an outpatient doctor. A woman can be stitched on the cervix if such a diagnosis is made at 16-20 weeks or a special retaining ring is placed if complaints appear later than this period. The suture or ring is removed at the time of the onset of labor, i.e. with the appearance of regular contractions or the outflow of amniotic fluid. However, this procedure can be performed two weeks before the expected date of birth.
Termination of pregnancy may be associated with the hormonal status of a woman , therefore hormones play a leading role in the treatment of this complication. In order to clarify the diagnosis in the antenatal clinic, they can take the so-called “threat smear” (this is not a 100% confirmation of the diagnosis). Of course, hormones play one of the main roles in the regulation of pregnancy. The problem of treatment of miscarriage is very complex and multifaceted. I repeat that in our country it is customary to preserve early pregnancy. For this purpose, hormone therapy is used, based on the physiological and pathogenetic processes of the onset and development of pregnancy. A woman diagnosed with threatened miscarriage or threatened miscarriage is admitted to the hospital for appropriate therapy in severe condition, or may be observed on an outpatient basis and given hormonal therapy, as in inpatient treatment.
Of course, hormones play one of the main roles in the regulation of pregnancy. The problem of treatment of miscarriage is very complex and multifaceted. I repeat that in our country it is customary to preserve early pregnancy. For this purpose, hormone therapy is used, based on the physiological and pathogenetic processes of the onset and development of pregnancy. A woman diagnosed with threatened miscarriage or threatened miscarriage is admitted to the hospital for appropriate therapy in severe condition, or may be observed on an outpatient basis and given hormonal therapy, as in inpatient treatment.
Symptoms of a threatened miscarriage
As for the threat of preterm labor, the first symptoms may not be bloody discharge, but simply heavy discharge (sometimes a woman thinks that she has urinary incontinence). This may be a signal that the integrity of the fetal bladder is broken. Of course, in this case, you should immediately consult a doctor.![]() If it is daytime, then a doctor of antenatal clinic is enough. At night, it is better to call an ambulance or get to the maternity hospital on your own.
If it is daytime, then a doctor of antenatal clinic is enough. At night, it is better to call an ambulance or get to the maternity hospital on your own.
In later pregnancy there may also be spotting . The reason for them may be a low-lying placenta and constant uterine contractions (uterine tone). It is the tone of the uterus that can cause placental abruption and, accordingly, bleeding. Contacting a doctor should be in the same mode as described above.
Separate mention should be made of ectopic pregnancy . This condition can also be associated with the threat of termination, only the consequences of the termination of an ectopic pregnancy can adversely affect the woman's health. An ectopic pregnancy is a condition in which a fertilized egg attaches itself outside the uterine cavity. This place is most often tubes, but an ectopic pregnancy can also be found directly in the ovary or in the abdominal cavity. The diagnosis of "ectopic pregnancy" requires immediate surgical intervention. The scope of the operation and operative approach (cavitary or laparoscopic) can only be decided in a hospital setting and depends on many factors, including complications that have arisen at the time of admission to the hospital. Very often, an ectopic pregnancy occurs when there is a malfunction of the villi that are in the tubes and push the fertilized egg into the uterine cavity. It is impossible to predict this state. However, it can occur most often in chronic inflammatory diseases of the pelvic organs.
The diagnosis of "ectopic pregnancy" requires immediate surgical intervention. The scope of the operation and operative approach (cavitary or laparoscopic) can only be decided in a hospital setting and depends on many factors, including complications that have arisen at the time of admission to the hospital. Very often, an ectopic pregnancy occurs when there is a malfunction of the villi that are in the tubes and push the fertilized egg into the uterine cavity. It is impossible to predict this state. However, it can occur most often in chronic inflammatory diseases of the pelvic organs.
What to do in case of termination of pregnancy
If the pregnancy could not be maintained, then the question arises of the reasons for this situation. After what happened, an examination is necessary, which will include an examination of both spouses. It is necessary to obtain the results of a histological examination and consult a geneticist .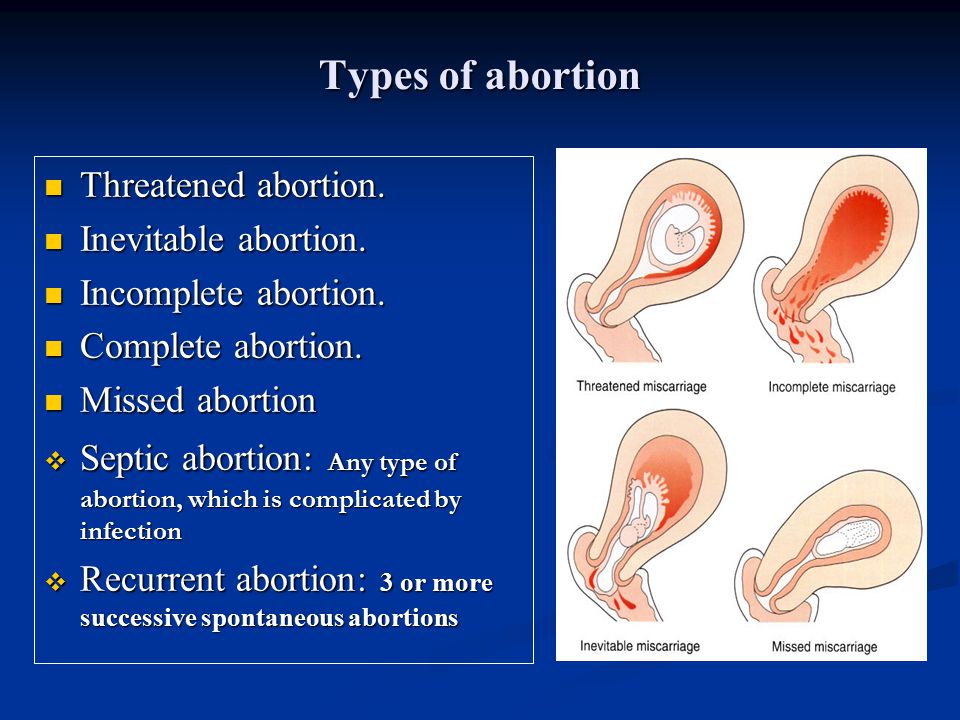 A woman will be examined by a gynecologist for infections or hormonal disorders, a man needs to consult a urologist (andrologist) for the same examination.
A woman will be examined by a gynecologist for infections or hormonal disorders, a man needs to consult a urologist (andrologist) for the same examination.
Sometimes it is very difficult to find the cause, but this is not a reason to despair. Subsequent pregnancies can pass without complications, and the first unsuccessful attempt is quickly forgotten. With a successful examination of , it is recommended to plan the next pregnancy in 4-6 months .
Everything we have talked about should draw attention to the health of a pregnant woman and help her navigate in the event of a particular situation. A desired pregnancy is a joyful state for a woman and her family. The task of the doctor is to prevent and, as far as possible, solve the problem with a positive result.
Doctors of the Fetal Medicine Center are one of the leading specialists in prenatal diagnostics, candidates of medical sciences, doctors of the highest categories with a narrow specialization and extensive experience in prenatal medicine.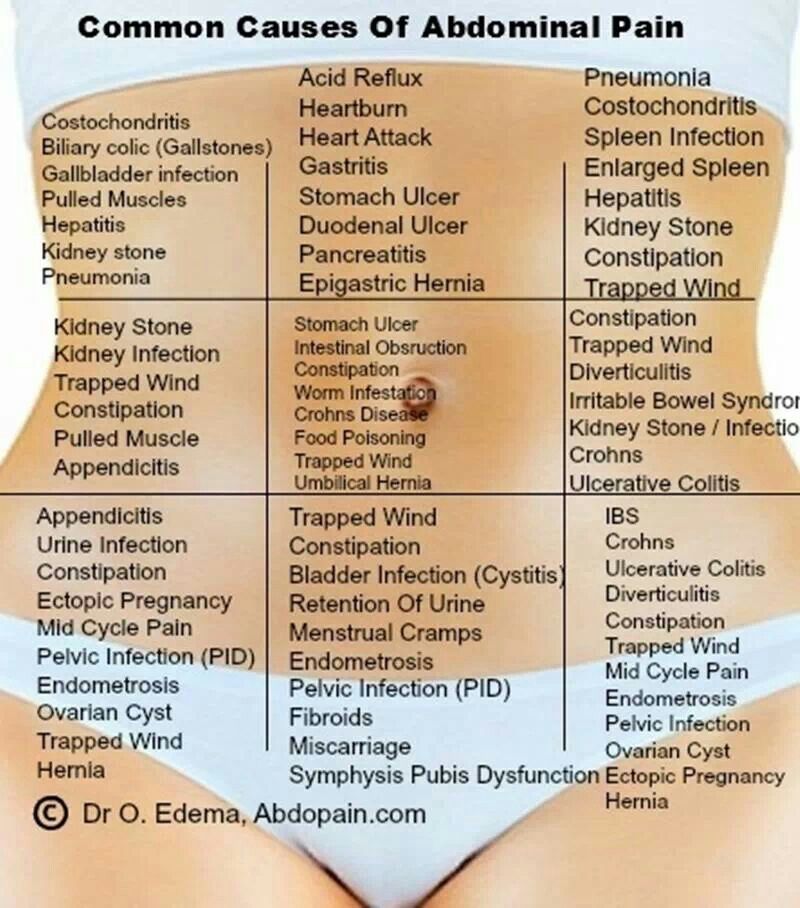
All ultrasound examinations in the center are carried out according to the international standards FMF (Fetal Medicine Foundation) and ISUOG (International Society for Ultrasound in Obstetrics and Gynecology).
Ultrasound doctors have international certificates from the Fetal Medicine Foundation (Fundamental Medicine, UK), which are are confirmed annually.
We take care of the most complex cases and, if necessary, it is possible to consult with specialists from King's College Hospital, King's College Hospital (London, UK).
The pride of our Centers - modern and high-tech medical equipment from General Electric: expert-class ultrasonic devices Voluson E8 / E10
The capabilities of these devices allow us to talk about a new level of information content.
You can make an appointment and get an expert opinion of our ultrasound diagnostics specialists by calling the single contact center +7 (812) 458-00-00
The threat of miscarriage: how to recognize and prevent
important for any woman. However, it is at this stage that the body loses most of its protective properties, becoming more vulnerable to adverse factors, especially in the case of existing health problems. According to disappointing statistics, about 15% of all clinically confirmed pregnancies end in the loss of a baby, and with a diagnosis of “ threat of miscarriage “every second expectant mother is familiar firsthand.
However, it is at this stage that the body loses most of its protective properties, becoming more vulnerable to adverse factors, especially in the case of existing health problems. According to disappointing statistics, about 15% of all clinically confirmed pregnancies end in the loss of a baby, and with a diagnosis of “ threat of miscarriage “every second expectant mother is familiar firsthand.
What is a miscarriage?
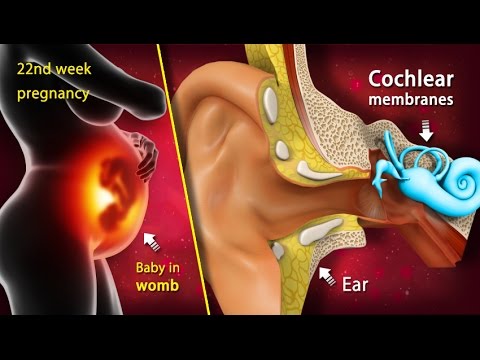
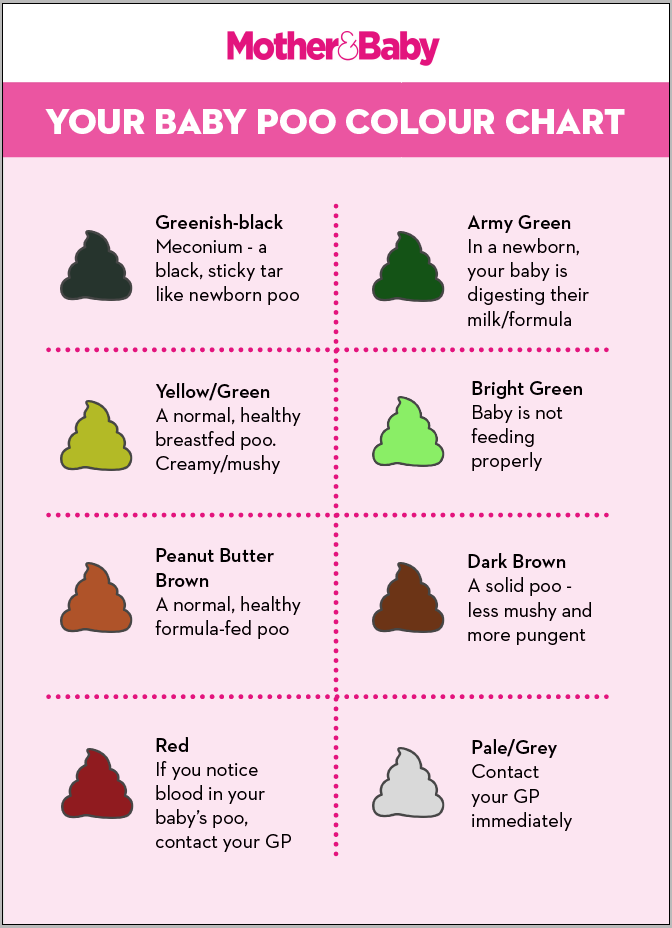
Miscarriage is an involuntary termination of pregnancy that occurs before 20 weeks of gestation, when the weight of the fetus does not exceed 500 grams. More than 80% of miscarriages occur early up to 12 weeks. It is at this time that the initial laying of the organs of the fetus occurs, and therefore any impact can be negative. Often, the woman herself, not knowing about her pregnancy, perceives the bleeding that has arisen as the monthly onset of the menstrual cycle. This situation is dangerous and can cause serious complications in case of incomplete expulsion from the fetus.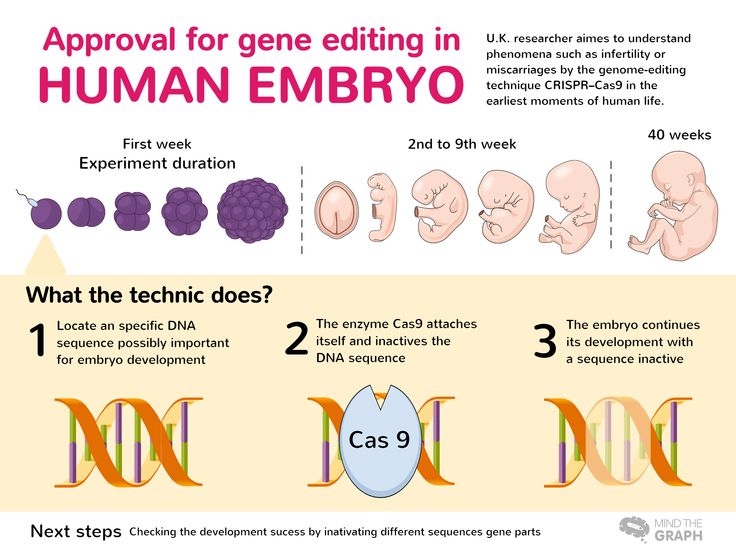
If the threat of miscarriage occurs after 22 weeks, then we are talking about premature birth and born babies weighing more than 650 grams. can be successfully cared for thanks to the achievements of modern medicine and the experience of doctors.
Symptoms that must not be ignored
The fact that the pregnancy is at risk of miscarriage is indicated by the onset of vaginal bleeding. Whatever its intensity, duration and color saturation, this is a signal that you should immediately seek help from a specialist.
No less alarming sign is a pulling pain that has appeared in the lower abdomen. Painful sensations radiating to the sacrum or inguinal region indicate the presence of uterine hypertonicity and an attempt by the body to get rid of the developing fetus.
The causes of bleeding and discomfort may be less serious, but these symptoms should definitely not be ignored. If the expectant mother is given a disappointing diagnosis, the task of the doctors is to do everything possible to keep the pregnancy until a safe period.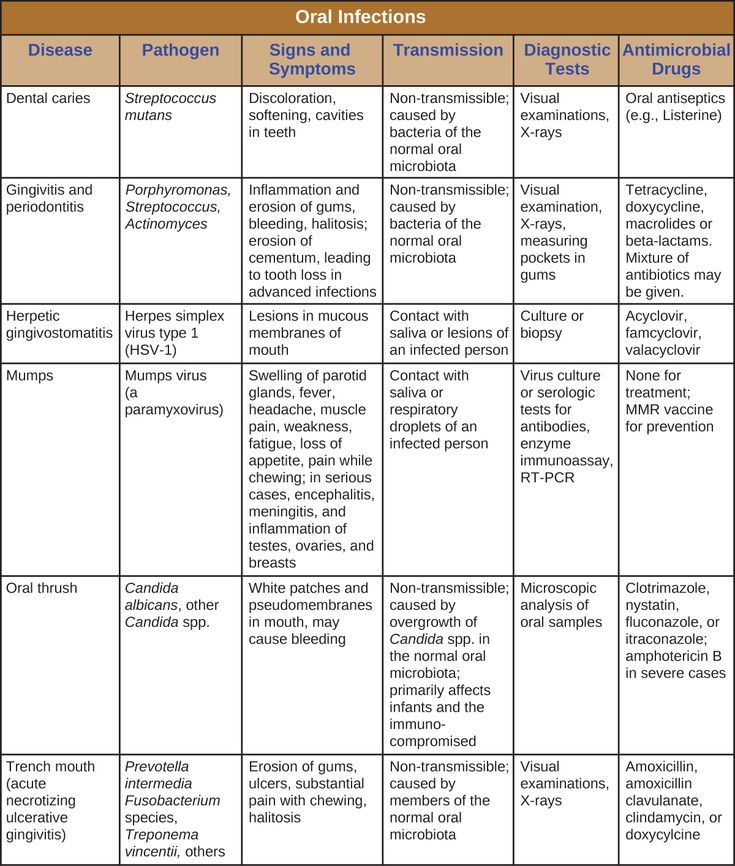
The main reasons causing the threat of miscarriage
The threat of miscarriage can be provoked by a number of reasons and not in every case it is possible to establish the true problem. And, nevertheless, every woman should be aware of the factors that can lead to termination of pregnancy:
- Any inflammatory and infectious diseases in which the body temperature rises above 38'C is a serious threat to pregnancy. The leaders who appear among the first in this list are rubella, chlamydia, hepatitis, taxoplasmosis, syphilis. Even the sore throat familiar to everyone at the initial stage can be fatal.
- Progesterone, a hormone produced initially by the yellow egg and subsequently by the placenta, is essential for maintaining pregnancy and fetal development. A lack of progesterone can lead to the rejection of an already fertilized egg. An excess of male hormones is another reason for abortion, as it suppresses the production of female hormones.

- Severe stress, along with heavy physical labor and an unhealthy lifestyle, deplete the body of the expectant mother, making it unable to bear the fetus for the required period. In case of excessive emotional stress, the doctor decides on the need to prescribe sedatives.
- A variety of gynecological problems, such as the presence of sutures or abnormal development of the uterus, pose a serious threat to gestation. The non-standard shape (two-horned, saddle-shaped) does not allow the fertilized egg to gain a foothold and stay in the endometrium.
- Uncontrolled use of various medications during pregnancy can cause miscarriage. Even seemingly safe herbs should be used only in advance, after consulting with an experienced doctor.
- Genetic anomalies in the development of the fetus - the main reason why there is a threat of miscarriage . Pathology is the result of a single mutation, in which the development of the embryo stops, which leads to its subsequent death.
 The development of such pathologies is perhaps the only one of the factors listed above, in which medicine is powerless.
The development of such pathologies is perhaps the only one of the factors listed above, in which medicine is powerless.
Who is at extra risk?
No woman is insured against involuntary termination of pregnancy, and yet there are a number of factors that increase the risk and require more attention from the expectant mother and additional control from the attending physician:
- If the expectant mother's age exceeds 35 years, the risk of miscarriage increases significantly. After a series of studies, doctors say that the risk of abortion after 30 years increases by 2 times, after 40 years the probability of carrying a child decreases to 20%. Doctors attribute this problem to the aging of the eggs, which nature endows a woman at birth and lose their vitality as they get older. Past diseases, the accumulation of toxic substances adversely affect the ability of eggs to conceive.
- If a woman has chronic and endocrine diseases, it is necessary to inform the supervising doctor even before the moment of pregnancy.
 Often such a problem as diabetes develops in parallel with the growth of the fetus. Being under the constant supervision of a specialist, a woman increases the chances of bringing a long-awaited child to a safe date.
Often such a problem as diabetes develops in parallel with the growth of the fetus. Being under the constant supervision of a specialist, a woman increases the chances of bringing a long-awaited child to a safe date. - A new pregnancy shortly after a recent birth is a serious factor that can lead to the inability of the body to bear the baby. According to doctors, you should beware of a new pregnancy for at least three months after giving birth.
- If a woman previously faced the problem of spontaneous termination of pregnancy, the threat of miscarriage will be present during the subsequent conception. According to the observations of experts, in the case of two miscarriages following each other, almost every new pregnancy cannot be saved until the end, if the necessary examination has not been carried out beforehand and the appropriate treatment has not been received.
- Medicine knows many cases when the genetic incompatibility of the father and mother led to the rejection of the fetus.
 At the highest risk are parents who do not match the Rh factor of the blood. If the mother has a negative and the father has a positive Rh factor, a situation may arise in which the female body, perceiving the developing fetus as a foreign body, tries by all means to get rid of it.
At the highest risk are parents who do not match the Rh factor of the blood. If the mother has a negative and the father has a positive Rh factor, a situation may arise in which the female body, perceiving the developing fetus as a foreign body, tries by all means to get rid of it. - Modern women prefer to lead an active lifestyle and work until late. On the one hand, such activity can only be welcomed, since physical mobility helps the expectant mother to more easily endure the rather difficult process of the upcoming birth. However, if a woman has to constantly experience excessive loads, lift weights, then this is a serious reason to think about changing jobs or going on maternity leave as soon as possible.
What should I do if I suspect a threatened miscarriage?
Even with the slightest suspicion, a specialist should be contacted immediately. It is very important to maintain a sober mind and not panic. Your calmness and timely medical care in most cases help to keep the pregnancy.
If you notice bloody discharge, indicating a possible detachment of the chorion - the membranes of the embryo, with which it is held on the walls of the uterus, you should lie down and call an ambulance. Trying to get to a medical facility on your own in such a state is not worth it.
If a doctor suspects a threatened miscarriage , a series of tests and examinations will help clarify the situation and identify the degree of danger. First of all, the specialist will check the heartbeat of the developing fetus. Ultrasound examination will help to find out about the condition of the placenta and embryo, as well as show possible pathologies of the structure of the uterus. Examination by a gynecologist will determine the presence of tone.
Methods of treatment
After a thorough examination and determination of the level of danger, the doctor will prescribe maintenance therapy. In the case when the risk of miscarriage is particularly high, the expectant mother is left for treatment in a hospital until her condition stabilizes and the threat of miscarriage is eliminated.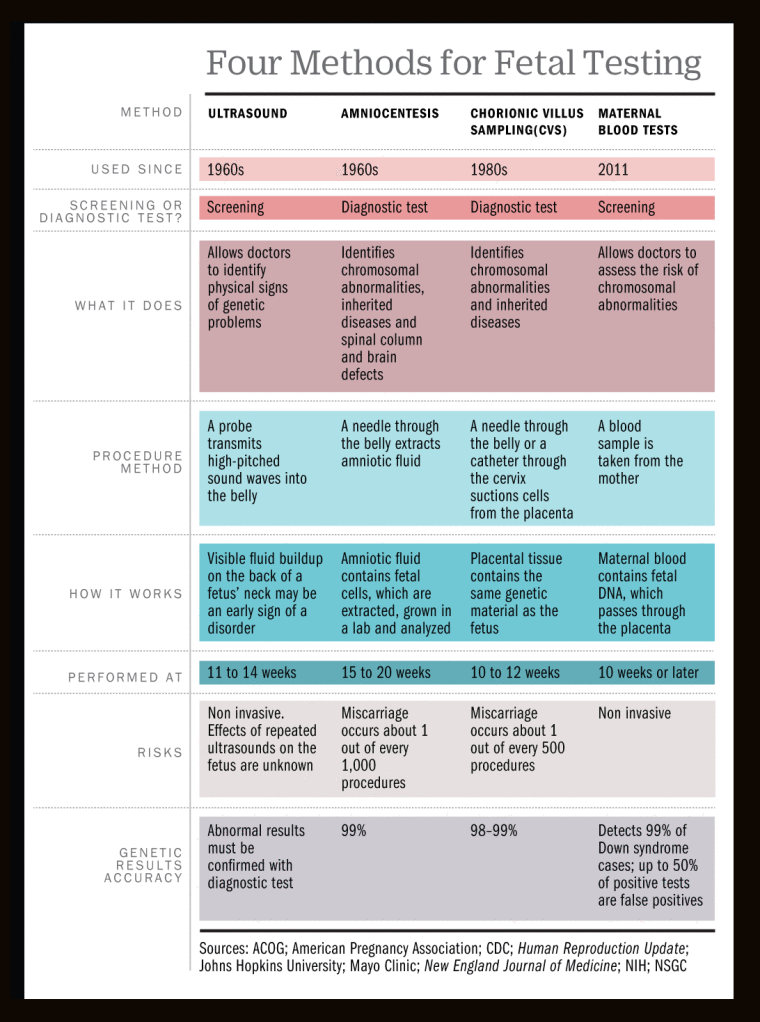 If the condition does not cause serious concern, a woman can be treated at home, subject to the doctor's instructions and maintaining complete calm, for which she will be prescribed sedatives on a natural basis.
If the condition does not cause serious concern, a woman can be treated at home, subject to the doctor's instructions and maintaining complete calm, for which she will be prescribed sedatives on a natural basis.
Treatment aimed at preserving pregnancy, includes the following stages:
1. Hormonal therapy
If the threat of miscarriage was caused by hormonal disorders, the pregnant woman will be prescribed by the main necessary hormone - progesterone. Taking drugs (usually "Utrozhestan" or "Dufaston") is prescribed according to a special scheme and is used until a period of 16 weeks is reached. By this time, the mature placenta begins to produce the necessary hormones on its own.
There is no need to obtain hormones artificially, but it is very important to know that the abrupt cessation of progesterone use can cause spontaneous abortion. Cancellation of the drug should occur in stages, by reducing the dose entering the body weekly.
2. Decreased tone
Prescribing antispasmodics can reduce uterine tone and reduce pain. The most common drugs that can be used until the pain disappears completely are papaverine (candles) and drotaverine (tablets).
3. Vitamin support
The expectant mother will be required to take vitamins, which will not only strengthen the body as a whole, but also contribute to the fact that the threat of miscarriage will be minimized. The use of folic acid during the first trimester as a separate drug or as part of a vitamin complex will prevent the development of neural tube defects in the embryo.
How to avoid the threat of miscarriage: prevention measures
Given the number of factors that affect the course of pregnancy, it is impossible to find a magic formula that reduces the risk of miscarriage to zero. And yet, some preventive measures will help reduce the risk of complications to a possible minimum: Problems.