How to read nipt results
Interpreting a result | Sonic Genetics
-
Clinicians
- Patients
- Our tests
- Locations
- About
- Contact
- Pathologists
-
Featured tests
- Welcome to Sonic Genetics
- Our tests
- Incidental findings
- Resources
- Education (medical)
- Electronic newsletter
- Request forms
- Sonic Education
-
Non-invasive prenatal testing
- Reproductive carrier screening
- Cancer genetics
- Pharmacogenomics
- Lactose intolerance
- Familial hypercholesterolaemia
-
Interpreting a result
-
Selecting non-invasive prenatal.
..
- High quality
- Arranging a test
- Inconclusive results
- FAQS
- Resources
- NIPT genetic counselling
-
Selecting non-invasive prenatal.
- Selecting the highest quality NIPT
- NIPT methods used by Sonic Genetics
- Arranging a test
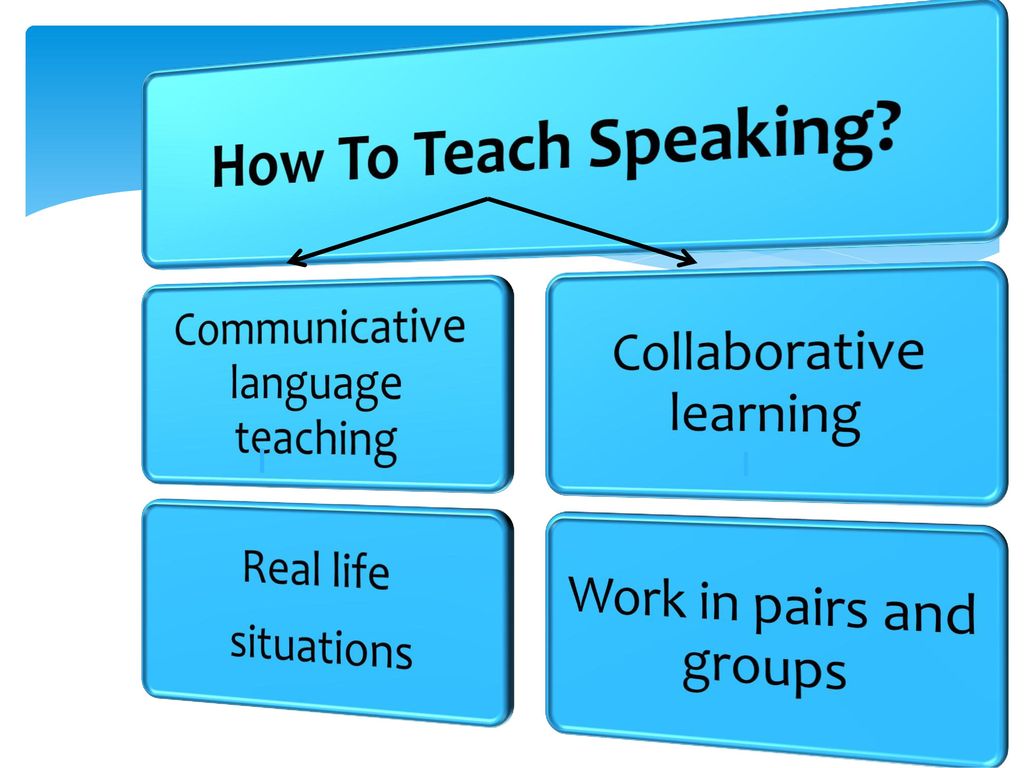
- Interpreting the NIPT result
- Inconclusive results
- Genetic counselling
- FAQs
- Resources
The non-invasive prenatal test (NIPT) is an accurate screening test for common trisomies, sex chromosome aneuploidies and other selected chromosome abnormalities.
NIPT differs from conventional prenatal screening methods in two important ways. First, conventional screening methods which use the concentration of serum proteins in maternal blood and on ultrasound have higher false-positive rates (incorrect “high risk” results in an unaffected pregnancy) and false negatives rates (incorrect “low risk” results in an affected pregnancy) than NIPT. Second, conventional screening methods report an individual risk score for a patient which takes into account ultrasound findings, the results of other screening tests and relevant family history. NIPT relies primarily on the relative concentrations of DNA fragments from different chromosomes in the mother’s blood.
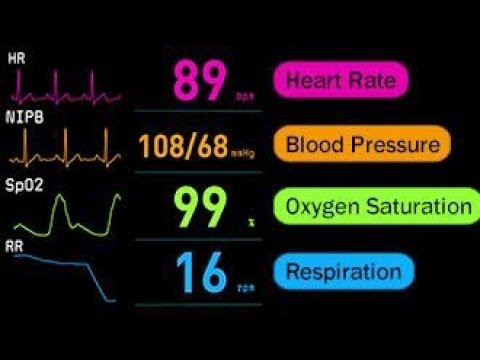
NIPT results are reported as either ‘High Probability’ or ‘Low Probability’ for the chromosome abnormality being tested. The accuracy of this result can be viewed in two ways:
- The accuracy of the test in general i.e. the proportion of pregnancies in which the test correctly identifies the fetus as having (or not having) the disorder in question.
 This refers to the sensitivity and specificity (respectively) of the test for that disorder. These measures of test performance are based on the analysis of thousands of pregnancies. For example, the Table shows the sensitivity and specificity of Sonic’s NIPT for different autosomal trisomies:
This refers to the sensitivity and specificity (respectively) of the test for that disorder. These measures of test performance are based on the analysis of thousands of pregnancies. For example, the Table shows the sensitivity and specificity of Sonic’s NIPT for different autosomal trisomies:
- The accuracy of this test in a particular woman i.e. the chance that her own result correctly identifies whether the fetus has (or does not have) the disorder in question. This refers to the positive and negative predictive value (respectively) of the test for that woman. The answers depend both on the sensitivity and specificity (as above) and the chance that this particular woman could have an affected fetus.
For example, some general scenarios are considered below.
Woman who is at a very low prior risk, e.g. 1 in 5,000 (0.02%) of her fetus having trisomy 21.
This may apply to a young woman with normal fetal ultrasound, or a woman with a low probability result from conventional first trimester screen.
If the NIPT result is LOW PROBABILITY of trisomy 21
The negative predictive value of the test for this patient would be >99.99% i.e. it is almost certain that the result is correct, and that the fetus does not have trisomy 21. However, there is a very small chance (less than 1 in 10,000) that this normal test result is incorrect.
If the NIPT result is HIGH PROBABILITY of trisomy 21
The positive predictive value of the test for this patient would be approximately 20% i.e. it is possible but not definite that the result is correct, and that the fetus has trisomy 21. However, there is an 80% chance that this abnormal test result is incorrect.
A high probability NIPT result is more likely to be correct than a high probability conventional first trimester screen. Nonetheless, a high probability NIPT result must be confirmed by invasive testing by CVS or amniocentesis before making major medical decisions regarding the pregnancy.
Nonetheless, a high probability NIPT result must be confirmed by invasive testing by CVS or amniocentesis before making major medical decisions regarding the pregnancy.
Woman who is at low prior risk, e.g. 1 in 1,000 (0.1%) of her fetus having trisomy 21.
This may apply to a young woman with normal fetal ultrasound, or a woman with a low probability result from conventional first trimester screen.
If the NIPT result is LOW PROBABILITY of trisomy 21
The negative predictive value of the test for this patient would be approximately 99.99% i.e. it is almost certain that the result is correct, and that the fetus does not have trisomy 21. However, there is a very small chance (approximately 1 in 10,000) that this normal test result is incorrect.
If the NIPT result is HIGH PROBABILITY of trisomy 21
The positive predictive value of the test for this patient would be approximately 50% i. e. it is likely but not definite that the result is correct, and that the fetus has trisomy 21. However, there is a 50% chance that this abnormal test result is incorrect.
e. it is likely but not definite that the result is correct, and that the fetus has trisomy 21. However, there is a 50% chance that this abnormal test result is incorrect.
A high probability NIPT result is more likely to be correct than a high probability conventional first trimester screen. Nonetheless, a high probability NIPT result must be confirmed by invasive testing by CVS or amniocentesis before making major medical decisions regarding the pregnancy.
Woman who is at increased prior risk, e.g. 1 in 100 (1%) of her fetus having trisomy 21.
This may apply to an older woman, or a woman with a high probability result from conventional first trimester screen.
If the NIPT result is LOW PROBABILITY of trisomy 21
The negative predictive value of the test for this patient would be >99. 9% i.e. it is highly likely that the result is correct, and that the fetus does not have trisomy 21. However, there is a very small chance (approximately 1 in 5,000) that this normal test result is incorrect.
9% i.e. it is highly likely that the result is correct, and that the fetus does not have trisomy 21. However, there is a very small chance (approximately 1 in 5,000) that this normal test result is incorrect.
If the NIPT result is HIGH PROBABILITY of trisomy 21
The positive predictive value of the test for this patient would be approximately 90% i.e. it is very likely that the result is correct, and that the fetus has trisomy 21. However, there is a 10% chance that this abnormal test result is incorrect.
A high probability NIPT result is more likely to be correct than a high probability conventional first trimester screen. Nonetheless, a high probability NIPT result must be confirmed by invasive testing by CVS or amniocentesis before making major medical decisions regarding the pregnancy
Woman who is at high probability, e.g. 1 in 10 (10%) of her fetus having trisomy 21.
This may apply to an older woman, or a woman with a very high probability result from conventional first trimester screen, or evidence of fetal malformations on ultrasound.
If the NIPT result is LOW PROBABILITY of trisomy 21
The negative predictive value of the test for this patient would be 99% i.e. it is likely that the result is correct, and that the fetus does not have trisomy 21. However, there is an approximately 1% chance that this result is incorrect for trisomy 21. In addition, this result does not preclude a chromosome disorder other than trisomy 21 being the underlying cause of her being identified as “high prior probability”. Invasive testing by CVS or amniocentesis with cytogenetic studies may still be warranted to check for a chromosome abnormality other than trisomy 21.
If the NIPT result is HIGH PROBABILITY of trisomy 21
The positive predictive value of the test for this patient would be approximately 99% i. e. it is very likely that the result is correct, and that the fetus has trisomy 21. Invasive testing by CVS or amniocentesis with cytogenetic studies would be warranted to confirm the diagnosis of trisomy 21.
e. it is very likely that the result is correct, and that the fetus has trisomy 21. Invasive testing by CVS or amniocentesis with cytogenetic studies would be warranted to confirm the diagnosis of trisomy 21.
Given that both a “low probability” result and a “high probability” result yield the same recommendation for invasive genetic testing, NIPT is not recommended as a screening test in women if there is a high prior probability of a chromosome abnormality.
Why is NIPT sometimes incorrect?
It is important to note the DNA fragments that are tested by NIPT are derived from the placenta and not the fetus. The placenta and fetus develop from the same cell i.e. the fertilised egg, and almost always have the same number of chromosomes. However, there are exceptions, and these can account for those uncommon situations in which the NIPT result does not match the fetal chromosomes.
For this reason, NIPT must be regarded as a screening test i.e. there is a small well-defined possibility that the NIPT will not reflect the actual chromosome status of the fetus. A “high probability” result should be confirmed by invasive genetic testing (CVS or amniocentesis) before taking irreversible steps in the management of the pregnancy. Conversely, a “low probability” result may still warrant invasive genetic testing if there are other indicators of a fetal chromosome disorder.
A “high probability” result should be confirmed by invasive genetic testing (CVS or amniocentesis) before taking irreversible steps in the management of the pregnancy. Conversely, a “low probability” result may still warrant invasive genetic testing if there are other indicators of a fetal chromosome disorder.
For details about the test, please click here.
Non-invasive prenatal testing (NIPT) | Pregnancy Birth and Baby
Non-invasive prenatal testing (NIPT) | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- The non-invasive prenatal test (NIPT) screens your baby for genetic health conditions.
- You may want to consider genetic counselling before having an NIPT to help you make an informed decision.
- If your NIPT result shows that your baby is likely to have a chromosomal difference, a diagnostic test such as chorionic villus sampling or amniocentesis can confirm your result.
What is the non-invasive prenatal test (NIPT)?
The non-invasive prenatal test (NIPT) is a very accurate screening test. Screening tests are used to see if your baby has a high chance of a genetic health condition. These conditions include Down syndrome and other chromosomal differences. The NIPT involves a simple blood test that is done in your first trimester of pregnancy.
There are different kinds of prenatal testing available to check the health of your baby. It’s your choice if you would like to have these tests. Talk about your options with your doctor or genetic counsellor and give yourself some time to make your decision.
Screening tests are different to diagnostic tests. Diagnostic tests are often more invasive. However they confirm for certain if the result is positive.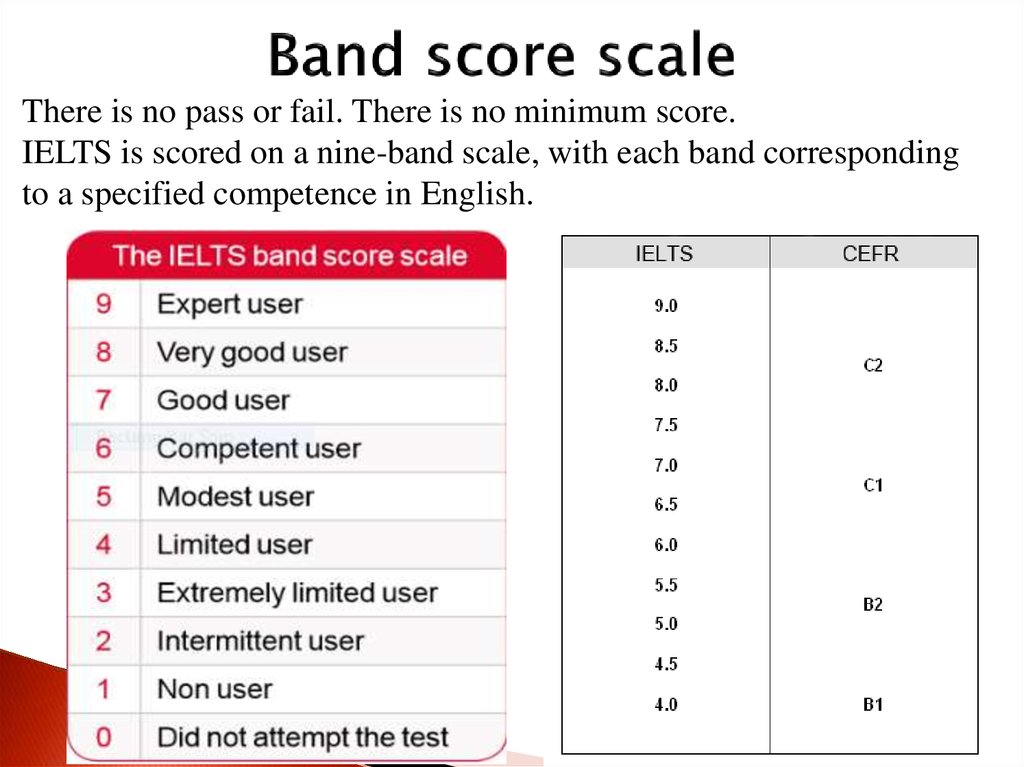
During pregnancy, some of the baby’s DNA passes into your bloodstream. The non-invasive prenatal test analyses the genetic information contained in this DNA. It’s used to screen for a number of genetic conditions. The test is particularly sensitive to Down syndrome. It was first offered in Australia in 2012.
In Australia, NIPTs are offered in private centres and involve an out-of-pocket cost. They are sometimes referred to by different names, depending on the company that makes them. They might be called: Harmony, Generation or Percept.
An NIPT is done from 10 weeks into the pregnancy. Before the test you will be asked to give consent.
What does it test for?
The NIPT is a safe and very effective way of screening for certain conditions. These include:
- Down syndrome (also called trisomy 21)
- Edwards syndrome (trisomy 18)
- Patau syndrome (trisomy 13)
- Turner syndrome
Some laboratories also test the sex of your baby and look for differences with the sex chromosomes.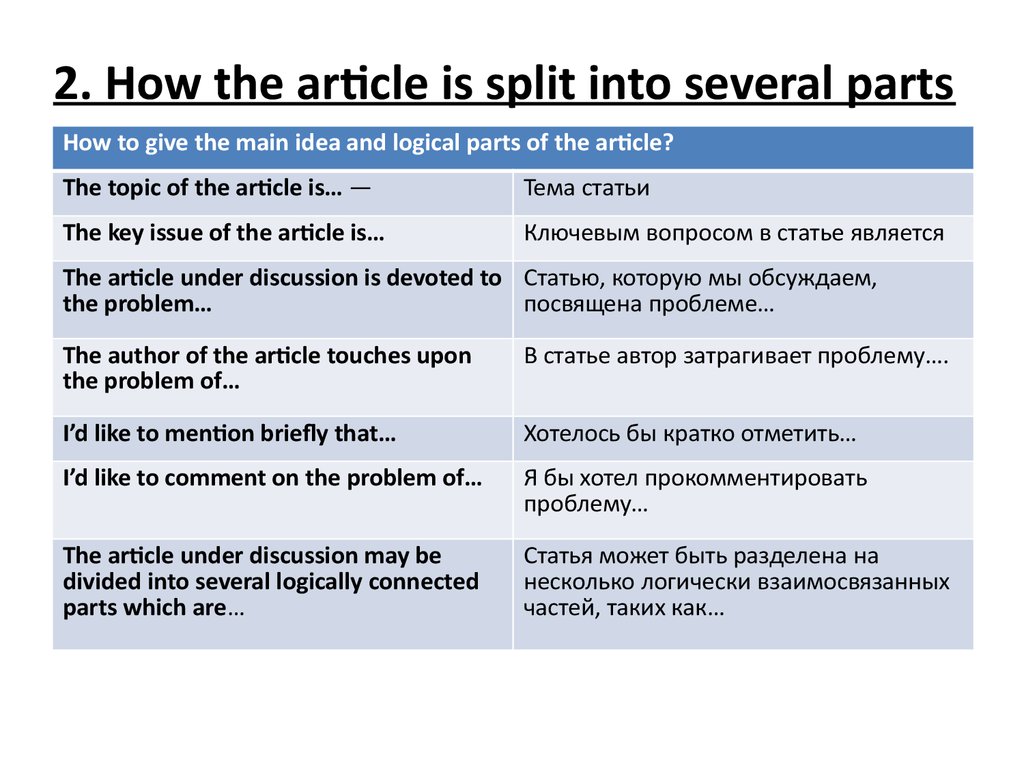
The test identifies many chromosomal anomalies. It doesn’t screen for genetic disorders such as:
- cystic fibrosis
- thalassaemia
- sickle cell anaemia
Screening will tell you how likely it is that your baby has a chromosomal difference. The only way of knowing for sure is to have a diagnostic test such as:
- chorionic villus sampling (CVS)
- amniocentesis
Should I have an NIPT?
The NIPT is very sensitive. It picks up more than 99% of cases of Down syndrome. But it is a screening test rather than a diagnostic test.
It can tell you whether there is an increased chance of having a baby with a genetic condition. It doesn’t give you a definitive answer. For some parents, information from screening tests can help them decide about whether to have diagnostic testing.
You might choose to have an NIPT test if:
- Your first trimester combined screening test shows you have an increased chance of having a baby with Down syndrome (this test combines results from a blood test at 10 to 12 weeks and an ultrasound at 11 to 13 weeks).

- You did not have the first trimester combined screening test because it was too late or the test wasn't available in your area.
- You want to understand your chance of having a baby with Down syndrome before considering diagnostic tests such as amniocentesis or CVS.
- You have an increased chance of having a baby with Down syndrome because you are older or you or your partner already have a baby with Down syndrome or another genetic condition.
It’s a good idea to consider genetic counselling before you have an NIPT to help you make an informed decision. It’s important to understand the risks and benefits of having the test.
Genetic counsellors can:
- review your family and medical history
- give you information about genetic tests
- help you learn about how the condition is inherited
- offer advice on support services
If your pregnancy is affected by a genetic condition, your genetic counsellor can:
- help support you
- help you understand what the results mean for you and your family
What can I expect from my NIPT results?
It can take up to 2 weeks to get the result of your NIPT.
If your NIPT result shows that your baby is likely to have a chromosomal difference, a diagnostic test such as: CVS or amniocentesis can confirm the result.
You should discuss your options with your doctor, midwife or genetic counsellor.
How much does the NIPT cost?
The NIPT is not covered by Medicare or private health insurance in Australia. You can expect to pay about $400 to $500 for an NIPT.
You may also need to pay for: an appointment with your doctor to get a referral, as well as an ultrasound.
You should speak with your doctor or a genetic counsellor before getting an NIPT. You can find genetic counselling services near you using the healthdirect Service Finder here.
You can read more about genetic counselling here.
If you have any questions about the NIPT, you can call the Pregnancy Birth and Baby helpline.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call.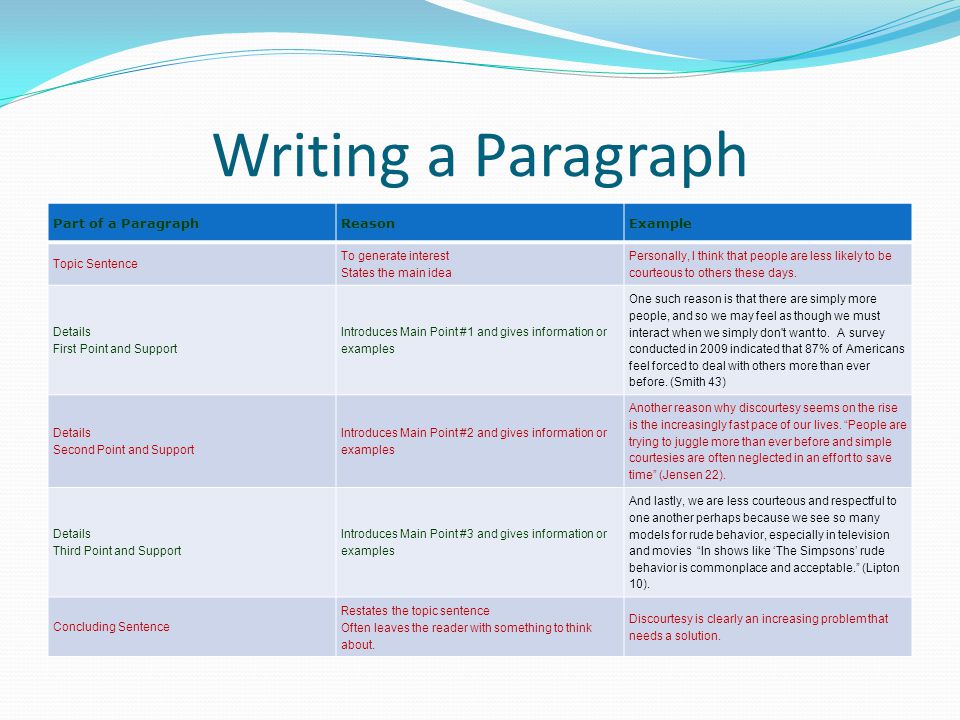 Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Women's Hospital Victoria (Genetic testing in pregnancy), NSW Health (Genetic and genomic testing for intellectual disability and childhood syndromes), O&G Magazine (Developments in non-invasive prenatal testing: is bigger better?), Allied Health Professions Australia (Genetic Counselling)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Questions to ask your doctor about tests and scans
- Antenatal care during your pregnancy
- Your first antenatal visit
- Blood tests during pregnancy
- Prenatal screening and testing
Need more information?
NIPT - non-invasive prenatal testing - Pathology Tests Explained
Learn about why, when and how NIPT testing is done
Read more on Pathology Tests Explained website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
What is prenatal screening?
Prenatal screening won't tell you if your baby has a health condition, but it can assess your risk. Learn more here about deciding whether to have a prenatal screening test.
Learn more here about deciding whether to have a prenatal screening test.
Read more on Pregnancy, Birth & Baby website
A guide to blood tests in pregnancy | Know Pathology Know Healthcare
The following guide outlines the different pathology tests available throughout each trimester, and the purpose of your prenatal blood tests.
Read more on Know Pathology Know Healthcare website
Screening for carrier status
Screening for carrier status assesses whether you and your partner carry genes that could mean your baby is born with a health condition. Find out more here about whether the test might be right for you.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 10
Think about the prenatal screening tests you might have, and whether you want a dating scan to confirm your due date.
Read more on Pregnancy, Birth & Baby website
Prenatal Screening for Chromosomal and Genetic Conditions
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Nuchal translucency scan
A nuchal translucency scan is an ultrasound scan that helps in estimating your risk of having a baby with chromosomal abnormality.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 12
By week 12, your baby is the size of a plum but fully formed, with their organs, muscles, limbs and bones in place.
Read more on Pregnancy, Birth & Baby website
Screening for Down syndrome
Down syndrome is a chromosomal disorder that affects 1 in 1,00 babies. Find out about the screening and diagnostic tests that can detect the condition.
Find out about the screening and diagnostic tests that can detect the condition.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What NIPT results might look like and what they mean
THE MAIN TEST OF YOUR PREGNANCY
Prenatal DNA Testing (NIPT) Accurate and Safe
Get Tested Today ,
get the result
Select date Order a test
The term of the study is from 2 to 7
calendar days from the date of receipt of
biomaterial to the laboratory in Moscow
Traditional prenatal screening methods using serum proteins and ultrasound (combined screening) produce many false positives, so an additional invasive procedure (chorionic biopsy or amniocentesis) is often required to distinguish false positives from true ones.
Equally dangerous are false-negative results of combined screening, which do not reveal a chromosomal pathology, which leads to the birth of a sick child. nine0003
NIPT results contain important information about the health of the unborn child, which in most cases is understandable and does not require additional comments.
Consider the main options for conclusions based on the results of NIPT:
1. Low risk of chromosomal abnormality in the fetus
This result means that the probability of encountering the investigated chromosomal abnormalities is extremely low. It is necessary to continue observation by an obstetrician-gynecologist with the implementation of planned ultrasound examinations of the fetus. nine0003
Separate consideration should be given to the low risk of NIPT results in the presence of ultrasound markers or fetal malformations.
Since there are many more possible causes of these abnormalities than NIPT can detect, we recommend that you discuss prenatal chromosome microarray testing with your geneticist and OB/GYN.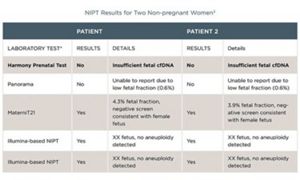
We do not recommend NIPT if ultrasound markers or fetal malformations were identified prior to NIPT and there are no contraindications for chorion biopsy or amniocentesis. nine0003
2. High risk of chromosomal abnormality in the fetus
If a high risk is identified, it is necessary to consult a geneticist.
Available data suggest that out of 1000 patients at high risk of having a child with Down syndrome, this chromosomal abnormality is confirmed in 999 during invasive diagnostics.
Since NIPT is a screening test, confirmation of the result by prenatal chromosome microarray analysis is required when a high risk is detected, especially if it is a continuation of the pregnancy. nine0003
3. No result. Low fetal fraction
Thanks to the measurement of the level of the fetal fraction during all NIPT in the Genomed laboratory, it is possible to avoid false results.
However, in some cases, the amount of fetal DNA is not enough to conduct the study.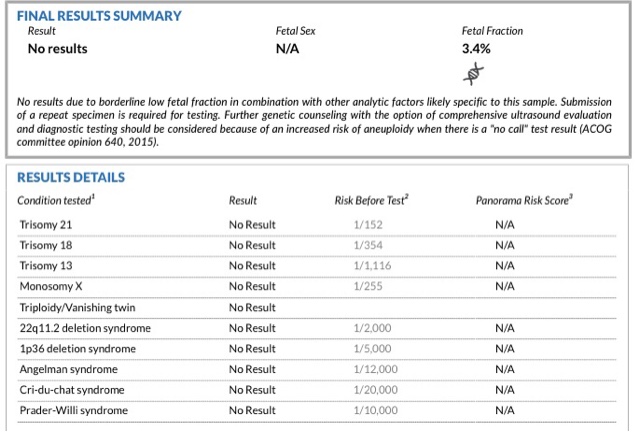
This may be due to various reasons, including those related to the weight of the pregnant woman and the characteristics of her placenta.
If there is no result due to a low fetal fraction, we will offer to test a new blood sample free of charge. nine0003
The non-invasive prenatal test is not diagnostic. If a high risk of chromosomal pathology is established, before a decision is made to terminate or maintain the pregnancy, it is necessary to confirm the diagnosis by an invasive method.
Still have questions?
Call us on the federal hotline 8-800-333-45-38
NIPT test Prenetics | Non-invasive prenatal fetal test
Contents
There is a discount for those who take NIPT. Call and ask about the amount of the current discount.
What is the Prenetix non-invasive prenatal fetal test, how long does it take
Non-invasive prenatal fetal test (NIPT) is an early opportunity to identify the risk of developing the most common genetic diseases in the fetus: Down, Edwards, Patau, Turner syndromes.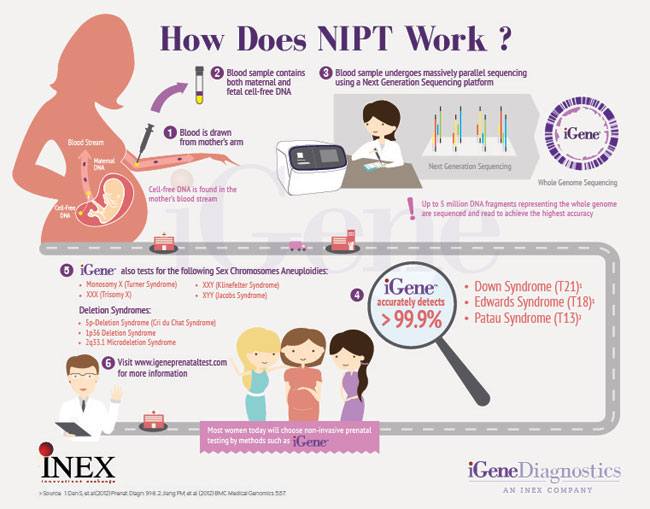
- Performed after ten completed obstetric weeks of pregnancy
- Results within 12 business days
- Safe for the health of women and children
- Available in all regions of Russia
- Recognized as the most objective and accurate in the world
| > 22,000 Number of patients who participated in technology testing | 99.9% Research-backed test accuracy | >1,000,000 Number of women from different countries who trusted the Prenetics test |
Why take the Prenetix test
Prenetix is a safe detection of risks of chromosomal abnormalities in the fetus with an accuracy of 99.9%. Before the invention of non-invasive tests, there were three ways to confirm the pregnancy specialist's suspicions about such disorders: draw indirect conclusions from fetal ultrasound (not accurate enough), examine the fetal tissue obtained after the “puncture” (more accurately), or wait for delivery. Although the probability of abortion with invasive diagnostics is low, not everyone was willing to risk the life of a child. Waiting for childbirth and remaining in the dark is stressful for the family. nine0008 Now there is an excellent screening study - a non-invasive prenatal DNA test. Since the technology is new, testing is not yet considered mandatory in Russia. But the World Health Organization recommends it to every pregnant woman: even a low risk of 1:10,000 at the first screening means that one out of ten thousand children is born sick.
Although the probability of abortion with invasive diagnostics is low, not everyone was willing to risk the life of a child. Waiting for childbirth and remaining in the dark is stressful for the family. nine0008 Now there is an excellent screening study - a non-invasive prenatal DNA test. Since the technology is new, testing is not yet considered mandatory in Russia. But the World Health Organization recommends it to every pregnant woman: even a low risk of 1:10,000 at the first screening means that one out of ten thousand children is born sick.
What does Prenetix show?
Non-invasive prenatal test reveals the risk of the following pathologies: Severe mental retardation and congenital malformations. The most common chromosomal pathology. nine0018
What Prenetix will not show
Prenetix examines only the risk of pathology of chromosomes 21, 18, 13, X and Y. Violations of other chromosomes, hereditary diseases, the analysis does not determine. NIPT test will not show a reliable result in the following cases:
- Pregnancy with more than two fetuses;
- Maternal chromosomal mutations;
- Malignant tumors;
- Donated maternal bone marrow or organs;
- Recent blood donation; nine0018
- The death of one of the twins.
Why Prenetix is up to 99.9% accurate: screening using new technology
It is impossible to study DNA molecules in their entirety, therefore, when testing them, they are divided into sections.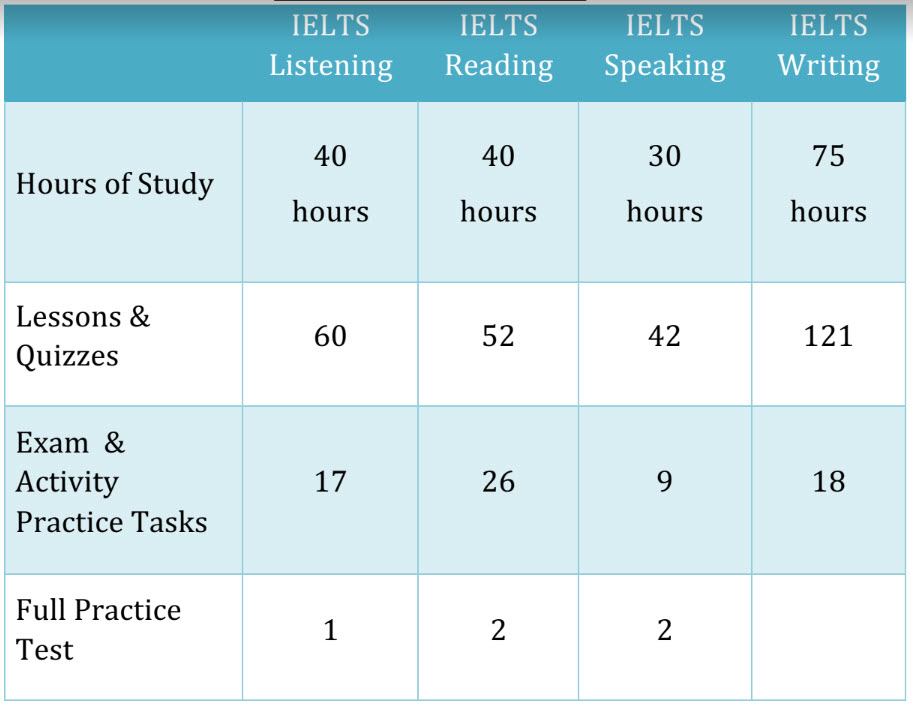 In each section, the sequence of structural blocks of the molecule - nucleotides - is studied. Violations in the order of nucleotides cause deviations in human development.
In each section, the sequence of structural blocks of the molecule - nucleotides - is studied. Violations in the order of nucleotides cause deviations in human development.
Sequencing - reading the sequence of nucleotides in DNA. There are two methods of sequencing: the study of random and sample sites. A random study is ineffective: all DNA sections are studied, the risk of not detecting pathology in the right ones increases. Selective sequencing examines only those regions whose mutations lead to common malformations. nine0008 Prenetix is based on a selective study of DNA fragments, with each section being read more times than in other similar technologies. Then the computer program evaluates the data of the study, the height, weight, age of the pregnant woman, the concentration of fetal DNA in the mother's blood and gives the results.
Benefits of Prenetix antenatal screening
| Exact result | Eleven clinical studies, of which three are independent, showed Prenetix to be reliable in 99. 9% of cases. For other non-invasive tests, the total number of studies is less than for Prenetix, so the result is not guaranteed. 9% of cases. For other non-invasive tests, the total number of studies is less than for Prenetix, so the result is not guaranteed. |
| Early term | Prenetics is carried out at the full 10th week of pregnancy. A prenatal DNA test will give the most accurate answer possible about the risks of chromosomal abnormalities at the earliest stage of pregnancy. |
| Any type of pregnancy | Prenetix will show a true result in twin pregnancy, surrogacy, IVF, if donor sperm or eggs are used. Other tests may fail or work incorrectly. nine0102 |
| Testing throughout Russia | Genetico operates in every region. It is enough to take a blood test in Moscow or any other city and get the result in 12 working days. |
| Recheck result | Test results are reviewed by two physicians before they are released to ensure a correct diagnosis. |
| Early sex determination | A non-invasive blood test will show the exact sex of the baby from ten weeks, including twin pregnancies. On ultrasound, sexual signs are noticeable no earlier than 23 weeks. nine0102 |
| No risks | Blood for analysis is taken from a vein, so there is no risk of miscarriage or infection, as is the case with invasive diagnostics. |
| Reliability | More than 1,000,000 women worldwide have taken the test. More than 22,000 people participated in the studies. |
Who is recommended to test
The use of the non-invasive prenatal test Prenetix allows to increase the reliability of traditional 1 screening for chromosomal pathologies and to conduct pregnancy with greater awareness. nine0008 Non-invasive prenatal test Prenetix is also effective in special cases.