How to increase breast milk supply while pregnant
5 Ways to Prepare for Breastfeeding While Pregnant – Nourisher
Breastfeeding feels like the first test of motherhood. It’s quite unfair actually. You’ve JUST made it to the finish line of your pregnancy, gone through labor and dealt with the emotional shock of meeting a tiny human that is half of your DNA. Instead of taking a good nap (or having that long awaited glass of wine) there is a startling jolt of reality that this baby is 100% dependent on you. He or she will be placed on your breast and before you know it, it’s go time!
Here are five ways to prepare for breastfeeding before your baby arrives.
Learn (and Practice!) the Main Breastfeeding Positions
We here stories like this from Nourisher moms all of the time!
“Minutes after my son was born a nurse hovered over me watching me try and latch him on for the first time. I knew what to look for in a latch, but unsurprisingly, he didn’t get it right away. “Maybe try him in the football hold,” she recommended.
Panic set in. The football hold? I had no idea what she was talking about! How could I already be bad at this, it had only been ten minutes? I mumbled something incoherent before she gracefully lifted him up and placed his body under my arm with his head in my palm. Baby latched and I breathed a sigh of relief.”
Case in point, study the various breastfeeding positions so that you know the different ways to hold your baby right from the start.
Take an In Person or Online Breastfeeding Class
The first time you hear the words “latch” “engorgement” “let down” and “colostrum” should be in an environment where you can absorb information — i.e. not in a hospital room with a screaming hungry newborn.
Learn the basics of breastfeeding before your baby arrives. This way the process will get off to a less-chaotic start. Most hospitals hold classes on breastfeeding and lactation consultants offer in-person training. But if getting dressed and out the door at 8 or 9 months pregnant doesn’t sound like your thing, take an online class! Nourisher friend Lindsey Shipley of the Lactation Link offers amazing online tutorials and webinars.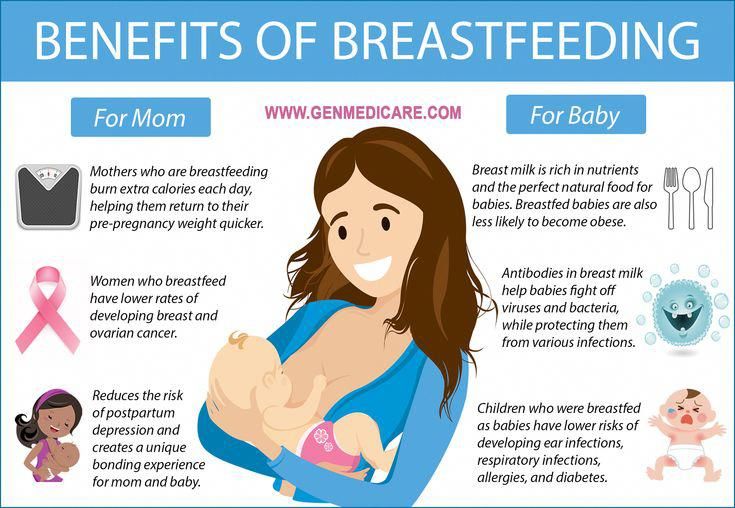
Understand Where Your Milk Supply Comes From
You don’t know it yet, but your milk supply will become a focal point of your day in a few weeks or months. Unfortunately you have no way of knowing if your milk supply will be abundant, just right, or if you’ll have a low supply. Regardless of where your body will fall on the milk-supply spectrum, it’s important to know where your supply comes from and how you can influence production.
Supply and Demand
The greatest way to maintain a healthy milk supply is to feed or pump frequently. Your body will produce on a supply and demand basis, so the more demand, the more supply.
Meeting Calorie Goals
Breastfeeding mothers don’t have to eat one specific type of diet, but they do need to be hitting the correct calorie amount in order to make milk. It’s all too easy to stop taking care of your body when your baby arrives.
Milkful Nursing Bars are a wholesome, convenient, energy-packed snack made specifically for breastfeeding moms. Eating one or two bars a day ensures you’re eating healthy ingredients and not snacking on cheap sugar products or failing to meet your calorie count. We recommend buying bars ahead of time (they have a shelf life of 5 months) and keeping several in your hospital bag for when baby arrives.
Eating one or two bars a day ensures you’re eating healthy ingredients and not snacking on cheap sugar products or failing to meet your calorie count. We recommend buying bars ahead of time (they have a shelf life of 5 months) and keeping several in your hospital bag for when baby arrives.
Additionally, learn what foods you can and can’t eat when breastfeeding. Hint: It’s more relaxed than pregnancy!
Hydrating
Drinking water to thirst is extremely important for breastfeeding women. Always keep a water bottle on hand so that your body is never straining for liquid to make milk.
Order Your Breast Pump, Necessary Accessories and Milk Storage Solution
Pumping is an entirely different facet of breastfeeding. Some women are exclusive pumpers, meaning their baby primarily drinks expressed breastmilk from a bottle rather than from their bodies. Some women pump breastmilk once or twice a day so that they have a bottle on-hand for occasional feedings from other people. And then some women never pump breastmilk because they are never separated from their child.
And then some women never pump breastmilk because they are never separated from their child.
How do you know which category you will fall into? For starters, consider what will happen at the end of your maternity leave. If there is a set date that you will be returning to work and you still want to continue breastfeeding, you’ll need to pump.
If your plans don’t involve daily separation from your child but you think you’ll want an occasional break from feeding, you’ll need to pump.
Now, you don’t need to feel pressure to pump right away. In fact, many lactation consultants recommend holding off on pumping until a breastfeeding routine is established. But we recommend having your pumping gear ready so that you can easily transition to this next stage of breastfeeding.
Here’s what we recommend purchasing during your pregnancy in preparation for pumping:
1. An electric or manual pump
A dual pump means you can pump from both breasts at the same time (a massive timesaver!)
2. A hands-free pumping bra
A hands-free pumping bra
This bra is not necessary if you’re going the manual route, but a hands-free bra means you aren’t sitting there holding your breast shields up to your body for 20 minutes at a time.
3. A breast milk storage solution
If you know pumping will eventually be a big part of your routine, go straight for the breast milk bags. These store up to 6 ounces of breast milk and are cost effective. You can also purchase 2.7 ounce vials that are easier to fill and defrost for feedings in the early weeks.
4. Bottles
Some babies prefer one style of bottle to another so you can either purchase a few different styles or borrow from a mommy-friend. Once your baby sets a preference, it’s a good idea to stick to one brand so you’re not trying to mix and match parts in the middle of the night.
5. Bottle brush and sanitizing steam bags
Have a new clean brush ready that is only dedicated to washing bottles, and buy a steam sanitizer bag for easy sterilization.
Mentally Prepare Yourself For a Newborn’s Breastfeeding Schedule
Alright mamas-to-be it’s time to buckle in. Breastfeeding is a job, and most likely the routine is going to kick your butt the first couple of weeks.
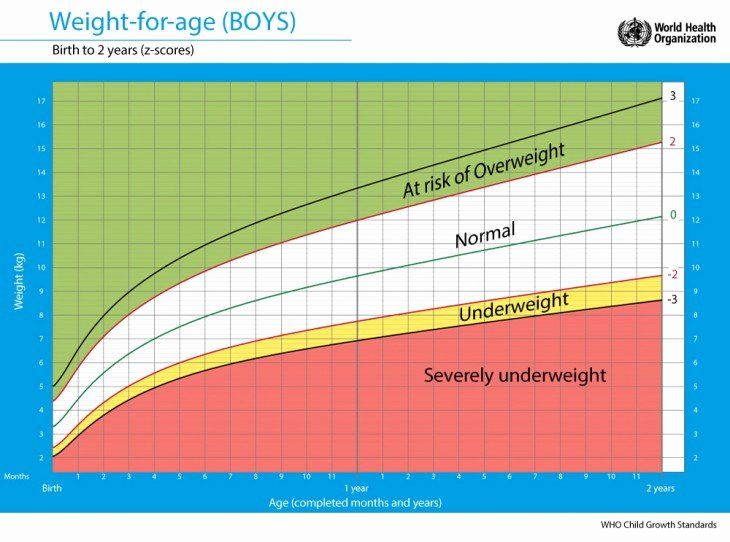
Newborn babies need to eat at every two hour mark until they get back up to their birth weight. Every two hours, 24/7. That means a typical day could have feedings at 6 a.m., 8 a.m., 10 a.m., 12 p.m., 2 p.m., 4 p.m., 6 p.m., 8 p.m., 10 p.m. 12 a.m., 2 a.m., 4 a.m.
The good news is that it is over quickly. The bad news is when you’re in that schedule, it feels like there is no way can you keep going. Trust us, you can!
Psych Yourself Up for the Routine
Go into that crazy feeding schedule knowing you will be challenged but you will make it through. Try to think of each feeding as a positive because it means your child is gaining weight quickly. Once you are given the go-ahead by your pediatrician you can relax into 3-4 hour stretches between feedings.
Know Pain is Only Temporary
Understand that it’s natural for breastfeeding to feel painful at first, but your body toughens up and it gets easier. Many women fail when they begin breastfeeding because it’s uncomfortable. When a baby latches in the first few weeks there is about a 10 second “ow ow ow” where you hold your breath and tense up while your nipples sting. (We would equate it to the pain of a clothespin on your finger.)
Pretty soon you’ll stop having to hold your breath and before you know it, latching is no big deal. Breastfeeding can feel uncomfortable at first, but with all new things, it becomes the norm quickly as your body and mind adjust.
Keep Reading 9 Healthy and Delicious Recipes for Eating Milkful Nursing Bars ›
Disclaimer: Some portions of this site may provide you with health-related information or information about Nourisher products based upon information that you provide. However, that information and other content provided through the site (collectively, “Content”) are presented in a summary fashion and intended to be used for educational purposes only. The Content is not intended to be and should not be interpreted as a recommendation for a specific treatment plan or course of action. Your use of this site or the Content does not create a doctor/patient relationship. This site does not offer medical advice and nothing provided through this site, including any content, is intended to constitute professional advice for medical diagnosis or treatment. You should not use this site or any Content to diagnose a health or fitness problem or disease. Use of this site or any Content does not replace medical consultations with a qualified health or medical professional to meet the health and medical needs of you or any other party. Do not disregard the medical advice of a physician or health professional, or delay in seeking such advice, because of any information you obtain from the Site.
The Content is not intended to be and should not be interpreted as a recommendation for a specific treatment plan or course of action. Your use of this site or the Content does not create a doctor/patient relationship. This site does not offer medical advice and nothing provided through this site, including any content, is intended to constitute professional advice for medical diagnosis or treatment. You should not use this site or any Content to diagnose a health or fitness problem or disease. Use of this site or any Content does not replace medical consultations with a qualified health or medical professional to meet the health and medical needs of you or any other party. Do not disregard the medical advice of a physician or health professional, or delay in seeking such advice, because of any information you obtain from the Site.
How to increase breast milk supply
How to increase breast milk supply | Pregnancy Birth and Baby beginning of content6-minute read
Listen
The best way to establish a healthy supply of breast milk is to start early, breastfeed frequently and make sure your baby is latching on correctly.
Some women have low supply, particularly during the early weeks of breastfeeding. This is the main reason some mothers start weaning or move to formula feeding. However, it's rare for a mother to produce less milk than her baby needs.
What are some reasons for a low supply?
There are many different reasons why some women have low supply including:
- delays in breastfeeding after delivery or separations of mother and baby such as if the baby needs to be admitted to the special care nursery or if the mother is unwell after delivery
- poor attachment to the breast, which can be caused by flat or inverted nipples, a tongue or lip tie, a sleepy baby because of jaundice, or a difficult or prolonged delivery
- if the mother is unwell due to problems like mastitis, retained placental tissue or large blood loss after the baby is born
- scheduled or timed feeding, rather than feeding baby on demand
- taking an oral contraceptive pill that contains oestrogen
- formula feeding as well as breastfeeding
- skipping breast feeds and offering a supplement formula feed but not expressing breast milk at that time to ensure that supply continues to meet baby's demand
- long-term use of dummies or nipple shields
- smoking
Breast milk supply can be low if the woman has medical problems such as polycystic ovarian syndrome, hypothyroidism, diabetes and pre-diabetes, or takes some blood pressure medications and cold and flu preparations, or has taken the contraceptive pill or has been infertile.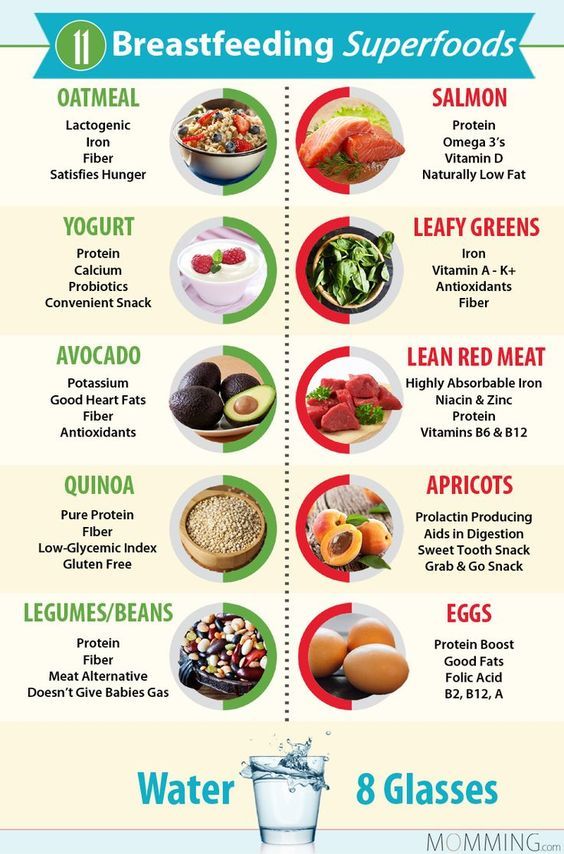
In some women, breast or nipple surgery makes breastfeeding difficult. In a few women, the breasts did not change during puberty and early pregnancy in a way that makes breastfeeding easier.
Typical baby behaviour
Some health professionals and mothers have an unrealistic expectation of how the baby will behave and might be concerned that what is normal baby behaviour could indicate low supply.
If your baby is having a good number of wet nappies each day, low supply is not a likely cause.
Some issues with breastfeeding include:
- wanting to be fed often — breast milk is digested in about 1.5 to 2 hours, whereas formula takes longer to digest
- being more fussy in the evening; you might produce less milk at this time and your baby will request fewer feeds or will 'cluster feed' (feed frequently at certain times of the day)
- liking to suck even if they have had a good breastfeed — sucking comforts them
- wanting lots of cuddles and skin to skin contact — this makes them feel secure and ensures that baby's needs are being met
- wanting to feed more frequently, which will happen when a baby is having a growth spurt — increased feeding will increase your supply
- reduced amount of sucking time at the breast — this often happens after 2 or 3 months as your baby becomes more efficient at the breast
What is normal for mum?
Although breastfeeding is different for every woman, the following do not mean that you have a low supply:
- your breasts suddenly seem softer — this is normal as your milk supply adjusts to your baby's needs
- your breasts do not leak milk, stop leaking or only leak a little
- you don’t feel a 'let-down' when milk pushes out of the breast
- you are unable to pump very much with an electric pump — remember the baby is much more efficient and will always get more than a pump
- how much you pump decreases over time
How do I know that baby is getting enough milk?
Always look at the whole picture to ensure that baby's growth and development is with normal limits. The baby is getting enough milk if they:
The baby is getting enough milk if they:
- go through 6 to 8 wet nappies in a 24-hour period including at least a few dirty nappies
- wake for feeds by themselves and feed vigorously at the breast
- have 8 to 12 breastfeeds in 24 hours
- pass a soft yellow stool
- settle and sleep fairly well after most feeds
- is back to birth weight in about 2 weeks
- gain on average 150g or more every week for the first 3 months
If your supply is low
Milk supply is considered to be low if you are not producing enough milk to meet your baby's normal growth and development needs.
Low milk supply is usually a temporary situation that will improve with appropriate breastfeeding support and management. Making more milk is all about supply and demand — the more milk is removed from the breast, the more milk is made. The less milk removed, the less made.
How to increase your supply
The following may help increase your breastmilk supply:
- ensure that baby is attaching well and removing milk efficiently from the breast
- be prepared to feed your baby more frequently — breastfeed on demand every 2-3 hours at least 8 times in 24 hours
- switch your baby from one breast to the other; offer each breast twice
- ensure your breasts are emptied well at each feed or pumping session; you can express after breastfeeds to make sure
- do not go longer than 5 hours without milk removal — your baby at the breast sucking is the most effective way to do this, but otherwise use a hand or electric pump
- when your baby is feeding, compress your breast to aid milk flow as this will also encourage more effective sucking
- make sure you are drinking a lot of water, eating a healthy balanced diet and not missing any meals
- also ensure you are resting as much as possible between feeds
Other options that can help with a low supply include:
- a supplemental nursing system or 'supply line'
- herbal and pharmacological remedies that are known to increase milk supply (galactogogues)
Some cultures use food or herbs to increase breast milk supply but many of these have not been formally studied. Domperidone is a prescription medicine that can increase the hormone prolactin, which can help stimulate breast milk production. Your doctor may discuss if this medicine is right for you. The main way to increase breast milk supply is through breastfeeding or expressing milk more than you currently do.
Domperidone is a prescription medicine that can increase the hormone prolactin, which can help stimulate breast milk production. Your doctor may discuss if this medicine is right for you. The main way to increase breast milk supply is through breastfeeding or expressing milk more than you currently do.
If you think you have low milk supply, talk to your doctor, lactation consultant, breastfeeding counsellor or child health nurse. You can call Pregnancy Birth and Baby on 1800 882 436 for advice and support.
Sources:
Australian Breastfeeding Association (Increasing supply), Karitane (Breastfeeding), Royal Women's Hospital (Low milk supply)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2021
Back To Top
Related pages
- Sore, cracked or bleeding nipples
- Breastfeeding your baby
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.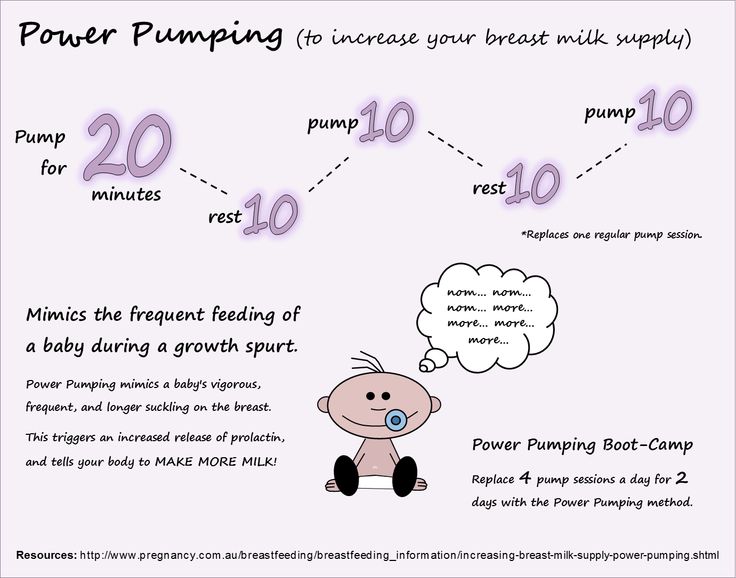
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
obstetrician-gynecologist Starostina Antonina Viktorovna.
For the normal development of lactation, first of all, it is necessary to organize the feeding of the child (feeding on demand, without a night break, the absence of nipples and pacifiers that suppress the suckling reflex of the baby), properly care for the breast, use a breast pump to stimulate and increase lactation, use according to indications other accessories for breastfeeding.
Sleep should be at least 10 hours a day - night and day. Outdoor walks for at least 2 hours. Frequent breastfeeding from birth (at least 10 times a day) with obligatory night feedings. Good nutrition and an increase in the amount of fluid consumed up to 1.5 - 2 liters per day (this is tea, soups, decoctions, milk, dairy products). Shower-massage: after feeding the baby and expressing milk, pour hot water (45 degrees) from the shower over the mammary gland that was fed, while massaging in circular motions from the nipple to the periphery and from top to bottom, while expressing milk. Duration 5-10 minutes.
Perform the procedure 2 times for the left and 2 times for the right breast during the day. Drink hot tea with milk 30 minutes before feeding.
Drink in small sips throughout the day.
- Steep 3 teaspoons of dry nettle with 2 cups of boiling water and infuse for 10-15 minutes (we only infuse fresh herb for 2 minutes). The resulting drink should be used during the day.

- A very effective remedy that stimulates the flow of milk and helps increase lactation is an infusion of walnuts, which is prepared as follows: brew 0.5 cups of peeled walnuts with 0.5 liters of boiling milk in a thermos and infuse for 3-4 hours. Infusion take 1/3 cup 20 minutes before each feeding, but not daily, but every other day.
- A mixture that promotes lactation is very good: 100 g dried apricots, 100 g raisins, 100 g figs, 1 glass of walnuts. Grind everything and mix with 100 g of honey and 100 g of butter. Use 1 tbsp. spoon 15-20 minutes before feeding. Watch your child's reaction! Allergy is possible.
- Useful green tea with dill seeds, raspberry leaves, linden, oregano, lemon balm.
Be sure to use special multivitamin complexes for pregnant and lactating women, which also help improve lactation. They will improve the quality of milk and increase its quantity:
- Hipp tea for nursing mothers.
- Apilac 0.01 under the tongue and dissolve.
 Take 2-3 times a day. Pay attention to the child's reaction! Allergy is possible.
Take 2-3 times a day. Pay attention to the child's reaction! Allergy is possible. - Vitamin E capsules 0.1-0.2 - 2 times a day.
- Ascorbic acid (vitamin C) up to 1 g per day.
- Brewer's yeast - liquid 60 g 3 times a day, dry 1 tsp. 4 times a day.
- Calcium pantothenate 1 tab. 3 times a day.
- Asparkam 1 tab. 3 times a day
In European countries, homeopathic remedies are widely used to stimulate lactation. Of the many homeopathic remedies to enhance lactation, the following remedies can be recommended: before each feeding of the child (20 minutes) \ Urtika urens 3 and Agnus castus 3 alternately and at night - Pulsatilla 6. Take 5 grains until the effect is obtained (from 3 days to 3 weeks). But in any case, you need to consult a doctor.
Too much milk? Reduced lactation
Sometimes you may feel like you are producing too much milk, especially during the first weeks of breastfeeding. After reading our article, you will find out if you really have too much milk, and what can be done to reduce it.
Share this information
Breast milk is very healthy, so it's good to have a lot of it, right? However, this is not always the case. Babies can sometimes have a hard time coping with the rapid rush of milk that usually accompanies excess lactation. And mothers who have too much milk often experience discomfort due to the constant leakage of milk and often suffer from mastitis.
Fortunately, there are a number of ways to help in this situation. But before using them, answer two important questions:
Do I really have too much milk?
Some of the symptoms of over-lactation (listed below) may occur for very different reasons. You should not try to reduce the production of breast milk, if you are not sure that it is the overabundance of it that is the main problem. Otherwise, this can lead to the fact that your baby will produce less milk than your baby needs, especially in the critical first month when production is just being established.
Is being overweight a problem for me or my baby?
If you are sure that you have an excess of milk, but this does not cause problems for you and your baby, you do not need to do anything. In most cases, everything returns to normal within the first few months. As the baby grows, he will learn to better cope with the rapid flow of milk and will feed with pleasure.
Leakage is not always a sign of too much milk
During the first four to six weeks of your baby's birth, the level of prolactin, the hormone responsible for milk production, will rise every time you have a bowel movement. In these first weeks, the breast learns to produce milk in the amount that the baby needs, depending on the time of day. Therefore, excessive leakage, rapid filling of the breast, and even splashing of milk during a rush are the norm. 1
At the same time, your baby is learning to suck and swallow milk, so you should not be surprised if he suddenly coughs or chokes when he suckles.
After about four to six weeks, the spikes in prolactin levels will begin to fade and milk production will become more balanced, adjusting to your baby's needs on a supply and demand basis. 2 However, given the many hormonal changes that occur in the body of a young mother, such a restructuring may take some time. In some mothers, milk production is established quickly, in others a little longer.
Behavior of the child, which may indicate an excess of milk
When overproduced, milk is usually released very quickly, especially during the first flush. As a result, the baby may cough or choke at the beginning of a feed, push back, or hold the breast loose in the mouth. The baby may pull away from the chest, frightened by a quick rush, and then cry because he hasn’t eaten. He can swallow milk in large volumes and with a lot of air, and after that he will spit up a lot. Try to be as careful as possible when you help him burp - sudden movements combined with a full tummy can cause the baby to vomit and scare him even more.
At the start of a feed, milk is relatively low in fat and consists mainly of lactose (sugar) and proteins. As the breast is fed and emptied, the fat content constantly increases. In the case of excess milk production, your baby may feel full before he completely empties his breast. This means that he will get a lot of lactose-rich milk, but not enough fat-rich milk that comes towards the end of a feed. Excess lactose instead of a balanced diet can make digestion difficult and cause hard, frothy, and greenish stools.
Oddly enough, in such a situation, the baby may constantly want to eat and behave restlessly between feedings. Despite the high calorie content, the low fat content of milk prevents it from being fully satiated. It is the fat contained in food that gives us a feeling of satiety. What happens if you eat a few dozen rice crackers or a slice of cheese with a cookie instead? You will fill up on cheese faster, as it is more saturated with fats.
However, all these symptoms can be caused by completely different problems, such as reflux, allergies, or even vice versa, insufficient milk production. An excess of breast milk can indeed cause these symptoms, but only if they are accompanied by excessive weight gain. Children usually dial around 900 g per month, but in the case of an excess of milk, they can gain much more, often almost twice as much. 1 If you feel like you are having too much milk but your baby is gaining weight normally, contact your lactation consultant or your healthcare provider.
An excess of breast milk can indeed cause these symptoms, but only if they are accompanied by excessive weight gain. Children usually dial around 900 g per month, but in the case of an excess of milk, they can gain much more, often almost twice as much. 1 If you feel like you are having too much milk but your baby is gaining weight normally, contact your lactation consultant or your healthcare provider.
Symptoms that may indicate an excess of milk in mothers
Mothers with an excess of breast milk often experience swelling and tightness in the breast, which constantly seems full. 3 As already noted, the leakage of breast milk in the first six weeks does not indicate its excess. However, if this continues at every feeding and after this period, it may be that the problem is in the overabundance.
A baby cannot always empty a full breast, so when there is an excess of breast milk, blockage of the milk ducts or periodic bouts of mastitis often occur. However, these problems can also be caused by other reasons.
However, these problems can also be caused by other reasons.
How to reduce milk production
If you have found that you have too much breastmilk and this is causing you concern, here are a few simple things you can do to help. For some mothers, they are enough.
- Try feeding in a relaxed position. Reclining or lying down feeding will allow the baby to better control the process. In this position, the baby sets the rhythm of feeding himself and can always raise his head to take a break if the milk is released too quickly. Don't forget to put a towel over to soak up spilled milk.
- Release the pressure. If full breasts make you uncomfortable, try expressing some milk by hand or with a breast pump, but try to express as little milk as possible. Every time you empty your breast, you send a signal to her to produce even more milk. Therefore, pumping provides short-term relief, but with prolonged use, it can only aggravate the situation.
 If you need to express and store milk to feed your baby when you are not around, it is best to address the problem of excess production first.
If you need to express and store milk to feed your baby when you are not around, it is best to address the problem of excess production first. - Try bra pads. If you have milk leaks, put special pads or pads in your bra to collect milk* to keep your underwear dry. If your milk leakage is moderate and already decreasing, or your breasts leak slightly during pregnancy, ultra-thin disposable pads will help you feel confident in any life situation.
- Avoid teas and lactation supplements. If you have been drinking teas, eating special biscuits, or taking supplements to improve breast milk production, this should be stopped now to resolve the problem.
Breast Watch to reduce milk production
If all the above methods fail, you can try a technique called breast watch, which allows you to better control milk production. However, before trying this method, check with a lactation consultant or healthcare provider.
On breastfeeding, you feed your baby on demand, but only on one breast for four hours. The second breast during this time is strongly filled. Since breast milk contains what is known as a "feedback lactation inhibitor", due to overfullness, the body sends a signal to that breast to slow down milk production. This is a natural way to protect the breast from endless filling.
The second breast during this time is strongly filled. Since breast milk contains what is known as a "feedback lactation inhibitor", due to overfullness, the body sends a signal to that breast to slow down milk production. This is a natural way to protect the breast from endless filling.
This technique must be applied for 24 hours, changing breasts every four hours. If the milk does not become less, try increasing the duration of the "watch" to six hours.
Complete emptying and “breast duty” technique
If after another day there is still a lot of milk produced,
you can try another version of this technique, which is recommended in cases of extreme overabundance. It is called "complete emptying and duty of the breast." 3
In this method, both breasts must be completely emptied in the morning with an electric breast pump and breastfeeding should be started immediately. The flow of milk will be weaker and allow the baby to eat calmly. In addition, he will get more fat-rich milk, which comes at the end of feeding, which means he will feel more full.
After that, you can continue the "breast watch" for four hours, as described above. If that doesn't help, try increasing the interval to six, eight, or twelve hours the next day, depending on the extent of the problem. Before using this technique, be sure to consult with your doctor.
You may not need to completely empty your breasts after the first use of this technique, but some mothers have to do this once or twice. Improvement usually occurs within the first two days or a little later, but in no case should "breast watch" be used for more than five days.
Literature
1 Morbacher N. Breastfeeding answers made simple. Amarillo TX , USA : Hale Publishing ; 2010. - Morbacher N., "Simple answers to questions about breastfeeding." Amarillo, Texas, USA: Publishing Hale 0146 et al . Blood and milk prolactin and the rate of milk synthesis in women.