How to help a newborn with reflux
Soothing Your Baby’s Reflux
If baby burp cloths are in heavy rotation at your house, you might wonder whether all’s well in your baby’s GI tract. But spitting up, also called gastroesophageal reflux (GER), is a typical part of babyhood. If your infant is eating well, growing, and not in pain, there’s no reason to worry about it.
“Stomach content coming back up into the esophagus is a normal physiologic process in everyone -- even adults -- that happens multiple times per day,” says Andrew Singer, MD, assistant clinical professor of pediatric gastroenterology at University of Michigan Health C.S. Mott Children’s Hospital.
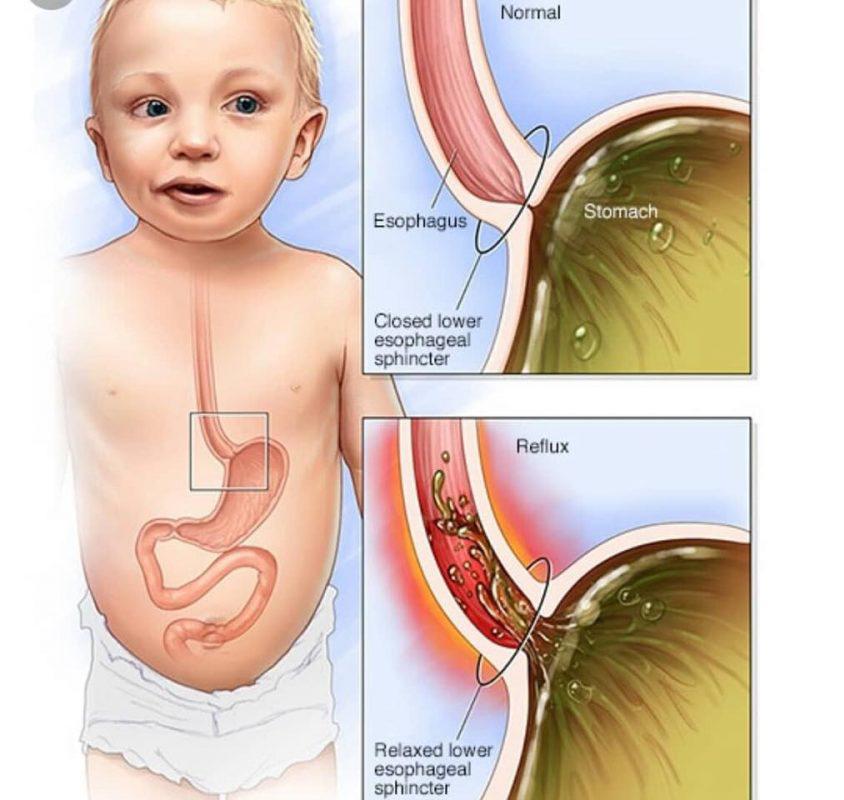
Reflux happens often in babies because the muscle that separates their esophagus from their stomach (the lower esophageal sphincter) isn’t yet strong enough to keep contents inside their tummy. And with feedings every 2-3 hours, there’s almost constantly something there to come up.
“It's just very easy for things to sneak up into the esophagus where they're not intended to be,” Singer says.
As babies get older, the lower esophageal sphincter stays tightly closed except when they swallow, and food and liquids stay in the stomach where they belong.
Signs of a Problem
Run-of-the-mill spitting up shouldn’t cause any upsetting symptoms in your baby. So if you notice these worrisome signs, it could mean their reflux has enough acid that it’s damaging the lining of your baby’s esophagus, a condition called gastroesophageal reflux disease (GERD):
- Weight loss
- Forceful (projectile) spitting up
- Spit up that’s green, yellow, bloody, or looks like coffee grounds
- Refusal to eat
- Bloody poop
- Trouble breathing or constant cough
- Spitting up that suddenly starts after 6 months old
- Fussiness after eating
“If you have an infant who spits up after a feed, and then they fuss for 5-10 seconds afterwards, that's not that big of a deal,” Singer says. “But if every time they spit up, they just seem like they go from totally calm to really uncomfortable and in pain, that suggests that there may be a problem.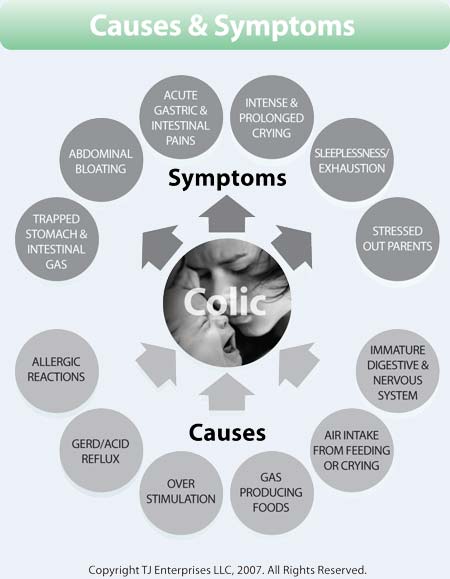 ”
”
Ani Perrault of Winnipeg, Manitoba, Canada, says her infant daughter was a generally happy baby most of the time -- until she spit up. “She exorcist-style projectile-vomited everywhere constantly, and often wailed about it,” she says.
Another clue that things weren’t right was her baby’s acidic-smelling breath. Perrault took her to the pediatrician to get it checked out.
“His first response was that if she was gaining weight well it was ‘more of a laundry problem’ than anything else,” she says. “But when it didn’t improve after starting solids, we got a [GERD] diagnosis.”
Home Help for Reflux
Whether your baby has GERD or is simply spitting up often, you can help reduce reflux by paying attention to how and when you feed them. Try these tips:
- Feed your baby smaller amounts more often. Be sure they’re taking in enough for healthy growth, but don’t overfeed. “Often parents feed a fussy baby because they think the problem is hunger,” Singer says.
 “But if kids are eating too much, that increases the likelihood that reflux is going to occur.”
“But if kids are eating too much, that increases the likelihood that reflux is going to occur.” - Burp baby mid-feed. Pause at natural points during feeding and get a good burp out of your baby. “Babies will swallow a lot of air when they're feeding, and that competes for room in the stomach,” Singer says. “The more full and distended the stomach gets, the more likely things are to come up.”
- Hold off on tummy time after feeding. Keep your baby upright for about 20-30 minutes post-meal. That way gravity can help hold things down while digestion happens.
- Thicken baby’s formula. If your baby is at least 4 months old, ask your pediatrician about the adding a small amount of infant cereal to their bottle. “The idea is that if things are a little bit thicker, they'll stay down in the stomach a little bit better,” Singer says.
Although there are a couple of over-the-counter acid reflux medications for infants, they won’t treat typical reflux. But they may help reduce some symptoms of GERD caused by acid damage in the esophagus.
But they may help reduce some symptoms of GERD caused by acid damage in the esophagus.
“Medication for reflux only serves to decrease the amount of acid that the stomach is secreting in the first place,” Singer says. “It doesn't actually keep reflux from happening.”
Perrault says ultimately if your baby is clearly unhappy or uncomfortable, don’t hesitate to tell your doctor. You may catch a potential problem that could have long-term effects on your baby’s diet. As an older toddler her daughter couldn’t tolerate many textures in her food. And though she doesn’t take daily medication for GERD today at age 9, she does still need an antacid a few times a week.
“In our case, our baby was always ahead of the curve for height and weight and she ate well, even when it looked like she was vomiting most of it back up,” Perrault says. “But she was late meeting milestones, and it has definitely had a lasting impact on her relationship with food.”
Reflux in Infants: MedlinePlus
What are reflux (GER) and GERD?
The esophagus is the tube that carries food from your mouth to your stomach. If your baby has reflux, his or her stomach contents come back up into the esophagus. Another name for reflux is gastroesophageal reflux (GER).
If your baby has reflux, his or her stomach contents come back up into the esophagus. Another name for reflux is gastroesophageal reflux (GER).
GERD stands for gastroesophageal reflux disease. It is a more serious and long-lasting type of reflux. Babies may have GERD if their symptoms prevent them from feeding or if the reflux lasts more than 12 to 14 months.
What causes reflux and GERD in infants?
There is a muscle (the lower esophageal sphincter) that acts as a valve between the esophagus and stomach. When your baby swallows, this muscle relaxes to let food pass from the esophagus to the stomach. This muscle normally stays closed, so the stomach contents don't flow back into the esophagus.
In babies who have reflux, the lower esophageal sphincter muscle is not fully developed and lets the stomach contents back up the esophagus. This causes your baby to spit up (regurgitate). Once his or her sphincter muscle fully develops, your baby should no longer spit up.
In babies who have GERD, the sphincter muscle becomes weak or relaxes when it shouldn't.
How common are reflux and GERD in infants?
Reflux is very common in babies. About half all babies spit up many times a day in the first 3 months of their lives. They usually stop spitting up between the ages of 12 and 14 months.
GERD is also common in younger infants. Many 4-month-olds have it. But by their first birthday, only 10% of babies still have GERD.
What are the symptoms of reflux and GERD in infants?
In babies, the main symptom of reflux and GERD is spitting up. GERD may also cause symptoms such as:
- Arching of the back, often during or right after eating
- Colic - crying that lasts for more than 3 hours a day with no medical cause
- Coughing
- Gagging or trouble swallowing
- Irritability, especially after eating
- Poor eating or refusing to eat
- Poor weight gain, or weight loss
- Wheezing or trouble breathing
- Forceful or frequent vomiting
NIH: National Institute of Diabetes and Digestive and Kidney Diseases
How do doctors diagnose reflux and GERD in infants?
In most cases, a doctor diagnoses reflux by reviewing your baby's symptoms and medical history.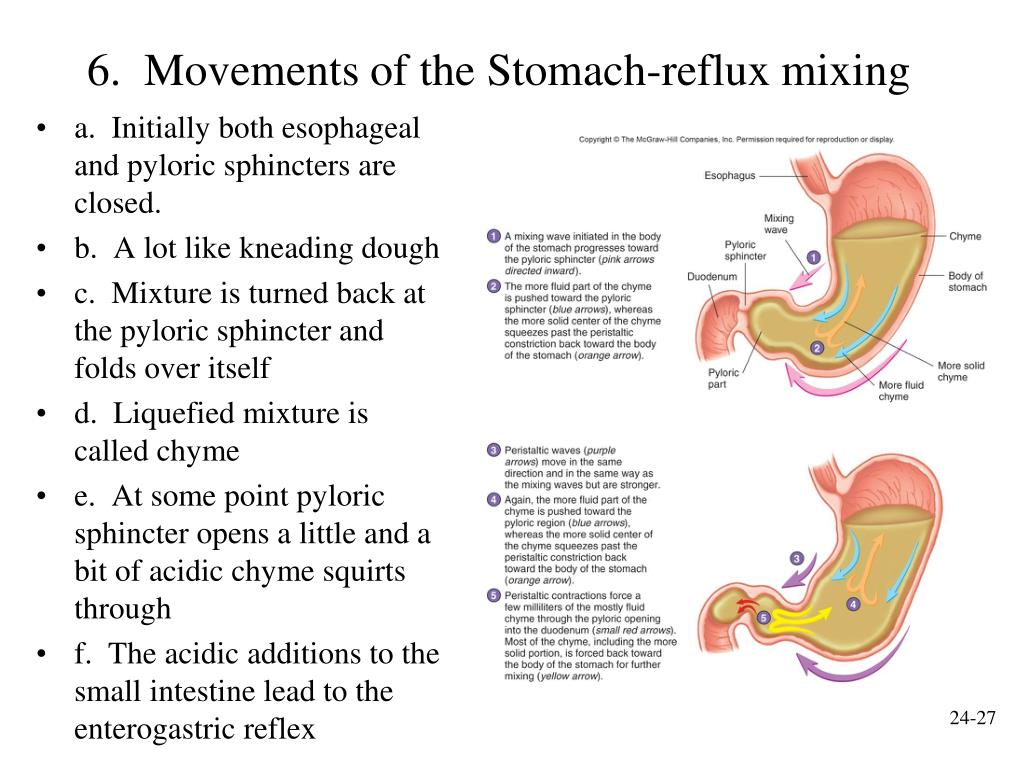 If the symptoms do not get better with feeding changes and anti-reflux medicines, your baby may need testing.
If the symptoms do not get better with feeding changes and anti-reflux medicines, your baby may need testing.
Several tests can help a doctor diagnose GERD. Sometimes doctors order more than one test to get a diagnosis. Common tests include:
- Upper GI series, which looks at the shape of your baby's upper GI (gastrointestinal) tract. Your baby will drink or eat a contrast liquid called barium. The barium is mixed in with a bottle or other food. The health care professional will take several x-rays of your baby to track the barium as it goes through the esophagus and stomach.
- Esophageal pH and impedance monitoring, which measures the amount of acid or liquid in your baby's esophagus. A doctor or nurse places a thin flexible tube through your baby's nose into the stomach. The end of the tube in the esophagus measures when and how much acid comes up into the esophagus. The other end of the tube attaches to a monitor that records the measurements.
 Your baby will wear this for 24 hours, most likely in the hospital.
Your baby will wear this for 24 hours, most likely in the hospital. - Upper gastrointestinal (GI) endoscopy and biopsy, which uses an endoscope, a long, flexible tube with a light and camera at the end of it. The doctor runs the endoscope down your baby's esophagus, stomach, and first part of the small intestine. While looking at the pictures from the endoscope, the doctor may also take tissue samples (biopsy).
What feeding changes can help treat my infant's reflux or GERD?
Feeding changes may help your baby's reflux and GERD:
- Add rice cereal to your baby's bottle of formula or breastmilk. Check with the doctor about how much to add. If the mixture is too thick, you can change the nipple size or cut a little "x" in the nipple to make the opening larger.
- Burp your baby after every 1 to 2 ounces of formula. If you breastfeed, burp your baby after nursing from each breast.
- Avoid overfeeding; give your baby the amount of formula or breast milk recommended.
- Hold your baby upright for 30 minutes after feedings.
- If you use formula and your doctor thinks that your baby may be sensitive to milk protein, your doctor may suggest switching to a different type of formula. Do not change formulas without talking to the doctor.
What treatments might the doctor give for my infant's GERD?
If feeding changes do not help enough, the doctor may recommend medicines to treat GERD. The medicines work by lowering the amount of acid in your baby's stomach. The doctor will only suggest medicine if your baby still has regular GERD symptoms and:
- You already tried some feeding changes
- Your baby has problems sleeping or feeding
- Your baby does not grow properly
The doctor will often prescribe a medicine on a trial basis and will explain any possible complications. You shouldn't give your baby any medicines unless the doctor tells you to.
Medicines for GERD in babies include:
- h3 blockers, which decrease acid production
- Proton pump inhibitors (PPIs), which lower the amount of acid the stomach makes
If these don't help and your baby still has severe symptoms, then surgery might be an option. Pediatric gastroenterologists only use surgery to treat GERD in babies in rare cases. They may suggest surgery when babies have severe breathing problems or have a physical problem that causes GERD symptoms.
Pediatric gastroenterologists only use surgery to treat GERD in babies in rare cases. They may suggest surgery when babies have severe breathing problems or have a physical problem that causes GERD symptoms.
- Acid Reflux (GER & GERD) in Infants (National Institute of Diabetes and Digestive and Kidney Diseases)
- Gastroesophageal reflux in infants (Medical Encyclopedia) Also in Spanish
- Infant Reflux: Diagnosis and Treatment (Mayo Foundation for Medical Education and Research)
- Infant Reflux: Symptoms and Causes (Mayo Foundation for Medical Education and Research)
- Parent's Take Home Guide to GERD (Gastroesophogeal Reflux Disease) (North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition) - PDF Also in Spanish
- Reflux and GERD in Infants (North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition)
- Spitting Up in Babies (American Academy of Family Physicians) Also in Spanish
- Spitting up in Babies: What's Normal, What's Not (Mayo Foundation for Medical Education and Research) Also in Spanish
- ClinicalTrials.
 gov: GERD in Infants (National Institutes of Health)
gov: GERD in Infants (National Institutes of Health)
- Article: Pathogenesis, diagnosis, dietary management, and prevention of gastrointestinal disorders in the.
 ..
.. - Article: Laparoscopic fundoplication after oesophageal atresia repair.
- Article: Impact of esophageal mucosal permeability markers on provocation-induced esophageal reflexes in.
 ..
.. - Reflux in Infants -- see more articles
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is a common occurrence in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.
How do I know if my child has acid (gastroesophageal) reflux?
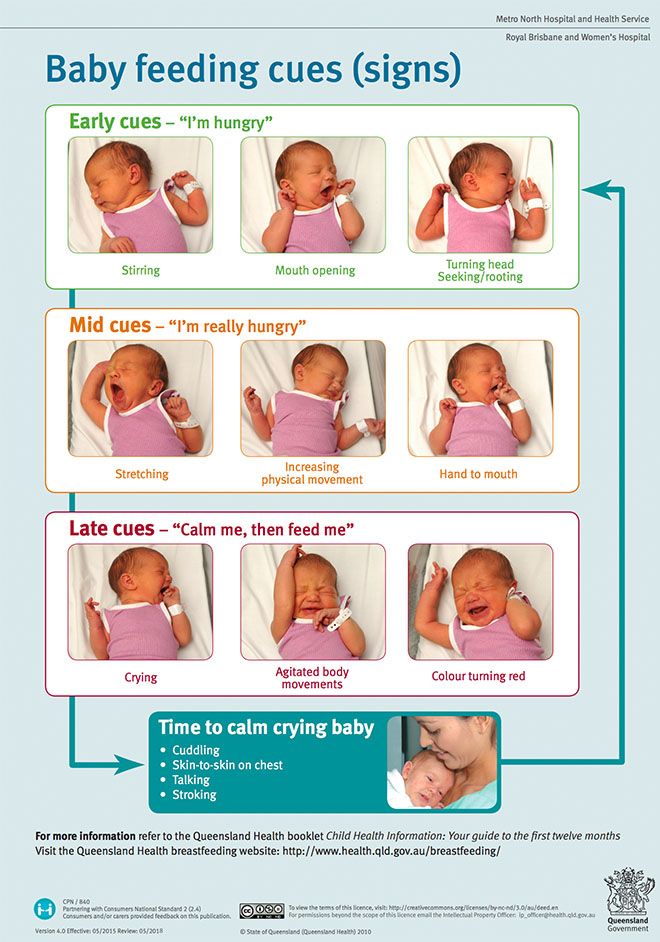
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting.
GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of the baby's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
The following are some of the symptoms of laryngopharyngeal reflux:
- breathing problems;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD.
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet.
It may be worth eliminating acidic foods from your diet.
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD?
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.

4. Let the baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer.
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.
4 Seattle Children’s Hospital
5 The National Institute of Diabetes and Digestive and Kidney Diseases - Treatment for GER & GERD in Infants
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
You are about to visit the Philips USA website.
Reflux in newborns - Articles about baby food from pediatricians and experts MAMAKO
- Valeria Maksimovna, what is reflux in newborns and what problems of the digestive system is it associated with?
— Reflux is the return of contents from the stomach or from the intestines and stomach into the esophagus and then into the oral cavity. Reflux causes various causes, but in infants it is more often functional disorders in the digestive organs. Regurgitation due to intrauterine hypoxia and congenital metabolic defects are extremely rare.
Regurgitation due to intrauterine hypoxia and congenital metabolic defects are extremely rare.
Nonpathological causes of reflux:
- non-compliance with the diet and dosage;
- improper breastfeeding and bottle feeding, resulting in swallowing large amounts of air;
- Incorrectly selected mixture, early complementary foods.
Organic disorders are formed, for example, against the background of congenital anomalies of the digestive organs and injuries of the cervical spine. They can cause pathological regurgitation.
— How can you tell reflux from vomiting?
- Between the concepts of "reflux" and "vomiting" you can put an equal sign. Vomiting refers to gastrointestinal reflux, the so-called gastroesophageal reflux in infants. But reflux is not just the backflow of fluid from the stomach into the esophagus. They also distinguish cystic reflux during the outflow of bile, vesicoureteral in the urinary system, and others.
Regurgitation is physiological and occurs in almost all children under three months of age. They appear within twenty minutes after feeding due to the child swallowing a large amount of air during sucking. This condition is accompanied by a characteristic sound of belching and a slight release of milk eaten: up to 3-5 ml.
— What are the most striking symptoms and signs of reflux? Is it always necessary to consult a pediatrician with the appearance of reflux, or can a child “outgrow” the problem?
- Clinical assessment of reflux syndrome is given on a 5-point scale, which takes into account the frequency and abundance of regurgitation. Often, regurgitation is not regarded as a disease, since it does not affect the health of the baby.
Medical intervention is necessary for severe forms of reflux to prevent the problem from progressing. The risk group for the formation of various pathologies includes children with a characteristic of reflux according to the table from three to five points.
Reflux in infants: how to identify
Any mother can independently determine the symptoms according to the table and decide on the need to visit a doctor. However, if the score is less than 3 points, but the mother does not like something or the child is lethargic, inactive, then, of course, you also need to visit a specialist.
- Can infantile reflux be caused by allergies or brain disorders?
- Food allergies, especially to cow's milk proteins, can lead to reflux. Neurological causes of reflux are less common: they may be based on damage to the central nervous system, suffered due to hypoxia or birth trauma. Therefore, it is very important to understand the cause of reflux in order to make the right decision about the treatment of the child. Of course, food allergies and problems with the central nervous system are two diametrically opposed causes, and the approach to these conditions is completely different.
How to help a baby with reflux
Interview with parents
- First of all, it is necessary to work with parents, give them full information about this pathology, tell them about first aid for reflux and aspiration prevention. Parents should be aware of this, because spitting up always causes panic.
Parents should be aware of this, because spitting up always causes panic.
Medications
- Post-syndromic therapy is used for reflux, which may include painkillers, probiotics, enzyme preparations, drugs that improve cerebral blood flow and act on the nervous system, motor function of the stomach and pancreas.
Medications are prescribed exclusively by the attending physician. Self-medication will be not only useless, but also dangerous.
Thickeners and breast-milk substitutes
- If reflux of unknown origin and non-drug methods of overcoming the problem do not help, then the next step will be diet therapy - breastfeeding milk thickeners are introduced, formula-fed milk thickener mixtures labeled AR (AP).
Breastfeeding mother's diet
— Reflux in infants due to food intolerance may be treated with a hypoallergenic mother's diet.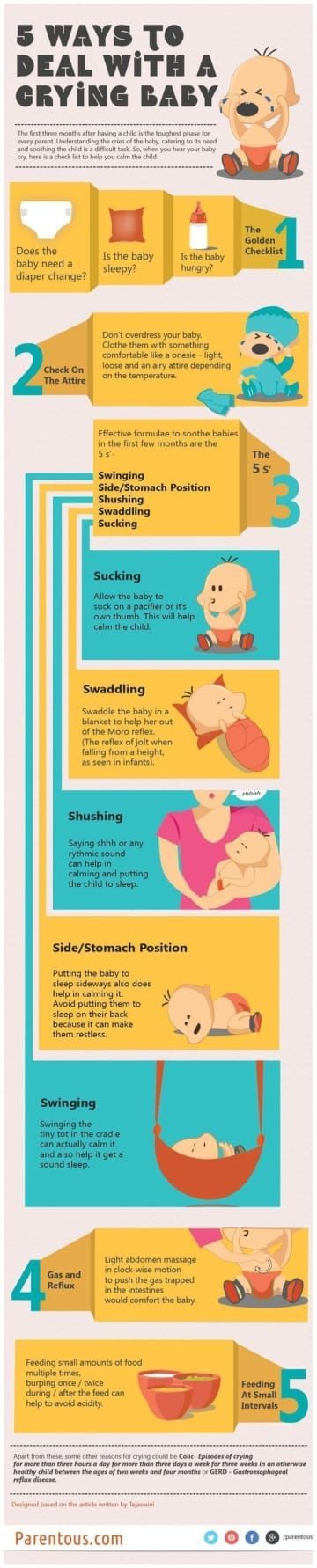 The doctor will try to identify the allergen in order to act on the cause of the reflux and fight it.
The doctor will try to identify the allergen in order to act on the cause of the reflux and fight it.
Massage
- Classical massage techniques are not suitable - on the contrary, they can cause reflux. There are non-drug techniques that can be conditionally attributed to physiotherapy exercises - exercises in water, positional therapy.
- Valeria Maksimovna, the sleep of a newborn with reflux is restless. How to help a baby with reflux sleep?
- We need to direct all our efforts to fight the cause of reflux. If it is not possible to cope with the root cause, general recommendations are applied to normalize the feeding regimen and activity of the child, non-drug methods. But the idea is simple - you need to try to identify and eliminate the cause of restless sleep. The baby's sleep will improve if the reflux is eliminated.
Preventive measures to help minimize symptoms of reflux
— What to feed a child with reflux and how does nutrition change depending on the state of his health?
- Breast-fed and bottle-fed babies can equally suffer from reflux. But help with reflux will be provided depending on how the mother feeds her child.
But help with reflux will be provided depending on how the mother feeds her child.
Breastfed
- With a proven food allergy in a child, a nursing mother is recommended to follow a hypoallergenic diet (the doctor determines the allergen and prescribes a diet).
- If the baby does not feel better after changing the diet, a thickener is added to the breast milk. Usually by the age of three months, the number of reflux episodes decreases significantly.
- If persistent regurgitation persists, additional laboratory and instrumental examinations are carried out, and therapeutic nutrition is prescribed.
Formula-fed
- Initially, they try to solve the problem by non-drug methods.
- If the cause of the reflux is unclear and nothing helps, the doctor will prescribe an anti-reflux mixture. It is more viscous due to special thickeners and is better retained in the stomach, so regurgitation stops.
Learn more





