How to heal cut on nipple while breastfeeding
Healing Tips for Nipple Cracks or Abrasions • KellyMom.com
By Kelly Bonyata, BS, IBCLC
The following measures can be very helpful if the skin on the nipple is broken for any reason (cracked nipple due to shallow latch, tongue-tie/lip-tie or other anatomical variations, thrush, a bite, milk blister, etc.).
Keep in mind that one of the most important factors in healing is to correct the source of the problem.
.
Continue to work on correct latch and positioning, thrush treatment, etc. as you treat the symptoms, and talk to a La Leche League Leader and/or board certified lactation consultant (IBCLC) if what you’re doing is not working.
During the nursing session | After nursing | Between nursings | Additional information
- Breastfeed from the uninjured (or less injured) side first. Baby will tend to nurse more gently on the second side offered.
- The initial latch-on tends to hurt the worst – a brief application of ice right before latching can help to numb the area.
- Experiment with different breastfeeding positions to determine which is most comfortable.
- If breastfeeding is too painful, it is very important to express milk from the injured side to reduce the risk of mastitis and to maintain supply. If pumping is too painful, try hand expression.
After nursing
Salt water rinse
This special type of salt water, called normal saline, has the same salt concentration as tears and should not be painful to use.
To make your own normal saline solution:
Mix 1/2 teaspoon of salt in one cup (8 oz) of warm water. Make a fresh supply each day to avoid bacterial contamination. You may also buy individual-use packets of sterile saline solution.
- After breastfeeding, soak nipple(s) in a small bowl of warm saline solution for a minute or so–long enough for the saline to get onto all areas of the nipple. Alternately, put the saline solution into a squeeze bottle and squirt it on gently; use plenty of saline, making sure to get it on all areas of broken skin.

- Avoid prolonged soaking (more than 5-10 minutes) that “super” hydrates the skin, as this can promote cracking and delay healing.
- Pat dry very gently with a soft paper towel.
- If baby objects to the taste of the residual salt from the saline rinse, rinse directly before nursing by dipping nipple(s) into a bowl of plain water. Pat dry gently.
After the salt water rinse
- Apply expressed breastmilk to the nipples to promote healing–this can be done in addition to other treatments.
- To promote “moist wound healing” (this refers to maintaining the internal moisture of the skin, not keeping the exterior of the skin wet) apply a medical grade lanolin ointment (e.g., Lansinoh, Purelan), soft paraffin/vaseline or a hydrogel dressing (e.g., ComfortGel, Soothies).
- If you have thrush, follow the saline soak with an antifungal ointment or other thrush treatment.
- If needed, apply an antibiotic ointment (e.g. Bactroban/mupirocin, Polysporin) or Dr.
 Jack Newman’s All Purpose Nipple Ointment(APNO; an antibiotic/anti-inflammatory/anti-yeast combo) sparingly after each feeding.
Jack Newman’s All Purpose Nipple Ointment(APNO; an antibiotic/anti-inflammatory/anti-yeast combo) sparingly after each feeding. - Per Hale, Bactroban ointment (mupirocin; lactation risk category L1/safest), available only by prescription, may be the best choice for nursing mothers.
- Of the over-the-counter treatments, Polysporin (Polymyxin B Sulfate and Bacitracin Zinc) may be preferred for topical use in the nipple area of nursing moms over antibiotic ointments containing neomycin (such as Neosporin or triple antibiotic ointment). Neomycin carries a small risk (1-2% of the general population) of contact dermatitis (see The Role of Topical Antibiotics in Dermatologic Practice by J.J. Leyden, MD).
- It is not necessary to wash small amounts of antibiotic or APNO ointment from the nipple prior to nursing, even if baby nurses again within minutes (see Dr. Jack Newman’s Sore Nipples info). If too much ointment was used and there is an obvious amount remaining when baby is ready to nurse again, gently wipe the excess off with a damp cloth.

Between nursings
- Keep nipples exposed to air when possible. When wearing a bra, use fresh disposable pads (change when damp). Some mothers use breast shells to protect the nipple from the dampness and friction of the bra.
- If there is a specific injury–like a bite–cold compresses (ice packs over a layer of cloth) may help: 20 minutes on, 20 minutes off; repeat as needed.
- Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) is compatible with breastfeeding.
- Once a day, use a non-antibacterial, non-perfumed soap to gently clean the wounded area, then rinse well under running water. Using soap on the nipple area is not recommended unless the skin is broken.
Contact your health care provider if you notice:Fever, inflammation/redness, swelling, oozing, pus, or other signs of infection. It is possible to have multiple infections (both fungal and bacterial). If the nipple is obviously infected, then talk to your health care provider about the possibility of using an oral (systemic) antibiotic. One study indicated that topical antibiotics and good breastfeeding techniques might not be sufficient if infection is present. (See Livingstone V, Stringer LJ. The treatment of Staphyloccocus aureus infected sore nipples: a randomized comparative study. J Hum Lact. 1999 Sep;15(3):241-6.) See also Oral antibiotic use for sore, cracked nipples and Staphylococcus aureus and sore nipples.) |
Additional information
Treatment of Sore, Cracked, or Bleeding Nipples by Becky Flora, IBCLC
Sore Nipples by Jack Newman, MD, FRCPC
Nipple Pain by Paula Yount
Sore Nipples in the Breastfeeding Mother from Lactation Education Resources
Barton A. Oral Antibiotics and Positioning Are Effective in Decreasing Morbidity in Breastfeeding Mothers. Critically-Appraised Topic from University of Michigan Evidence-Based Pediatrics Web Site, February 14, 2000.
Buchanan P, Hands A, Jones W. Assessing the evidence: Cracked Nipples and Moist Wound Healing. Paisley, Scotland: The Breastfeeding Network, March 2002.
Livingstone V, Stringer LJ. The treatment of Staphyloccocus aureus infected sore nipples: a randomized comparative study. J Hum Lact. 1999 Sep;15(3):241-6.
Martin J. Nipple Pain: Causes, Treatments, and Remedies. Leaven. February-March 2000;36(1):10-11.
Morland-Schultz K, Hill PD. Prevention of and therapies for nipple pain: a systematic review. J Obstet Gynecol Neonatal Nurs. 2005 Jul-Aug;34(4):428-37.
Cracked nipple Wikipedia
Cracked Nipples and Moist Wound Healing
This information is also available in a printer-friendly PDF format by clicking here.
Updated (2019) by Agnès Léger, BfN Supporter
Reviewed by Phyll Buchanan, Anthea Tennant-Eyles, Sarah Turner, Wendy Jones. Registered BfN Supporters
The original version of this leaflet was produced in 2002 and can be found below.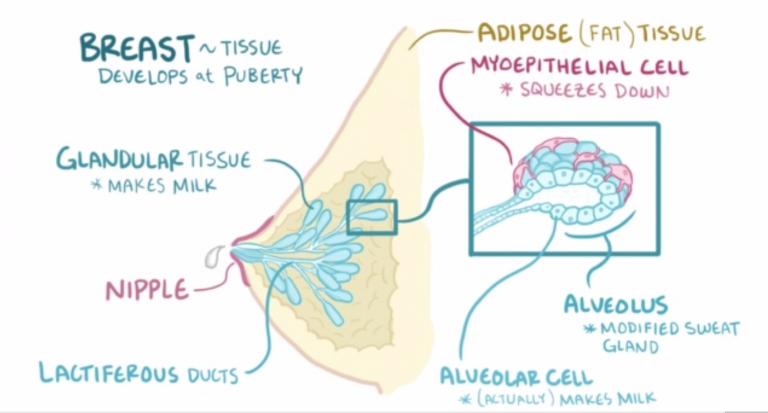 Although some further research has been conducted since, the conclusions mostly haven’t changed. This is still an area in urgent need of further systematic reviews and independent research, especially distinguishing sore and damaged nipples. Nipple pain is usually poorly defined in the studies, without distinction between broken and unbroken skin (see Section “Sore or cracked?”). It could be the case that those different types of issues benefit from different treatments.
Although some further research has been conducted since, the conclusions mostly haven’t changed. This is still an area in urgent need of further systematic reviews and independent research, especially distinguishing sore and damaged nipples. Nipple pain is usually poorly defined in the studies, without distinction between broken and unbroken skin (see Section “Sore or cracked?”). It could be the case that those different types of issues benefit from different treatments.
A review of most of the recent studies that assessed the efficacy of treatments for painful nipples was produced in 2014, and we recommend readers to refer to this document to help them understand the evidence supporting the use of various treatments. Note that it does not separate treatment of recent and established wounds. This Cochrane review is entitled “Interventions for treating painful nipples among breastfeeding women” and was conducted by C‐L Dennis, K Jackson and J Watson. It can be accessed at the following link:
https://doi. org/10.1002/14651858.CD007366.pub2
org/10.1002/14651858.CD007366.pub2
Most of the content of this leaflet is still as relevant today. The amendment highlights some of the main updates of the last 17 years throughout the text (in boxes). The BfN is investigating paths to either produce an updated leaflet or support further systematic reviews.
Summary of the key points
· Cause of soreness
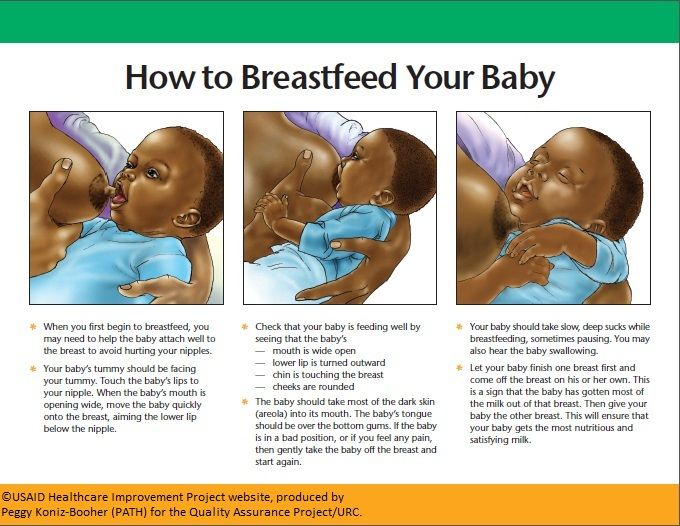
Addressing the cause of the nipple soreness is the most effective way of solving it! Correcting positioning and attachment is paramount in allowing a damaged nipple to heal and enable pain free, effective breastfeeding. Positioning and attachment should always be investigated, including for older babies, because even a good latch can be improved. There are resources on the subject here:
www.breastfeedingnetwork.org.uk/positioning-attachment
· How to treat sore nipples
Nipples can be air dried or kept moist using a few drops of expressed milk. To this date, there isn’t satisfactory evidence than any other treatment is as effective in helping nipples heal, including purified lanolin and vaseline (Dennis et al. , 2014). If using creams, apply after feeds. Most do not need to be washed off before the next feed, though if using creams/gauze containing antibiotics its worth wiping off any excess before a feed. You can also check our section “A few things to try”.
, 2014). If using creams, apply after feeds. Most do not need to be washed off before the next feed, though if using creams/gauze containing antibiotics its worth wiping off any excess before a feed. You can also check our section “A few things to try”.
· How long does healing take
The duration of the healing will vary. Superficial and recent soreness may clear in a matter of hours or days. However, long-established and profound wounds may require a up to 2 or 3 weeks to be entirely resolved even after the cause of the soreness has been eliminated. Long-established wounds usually close from the bottom to the top, so creams applied to the wound in order to prevent a scab forming is likely to aid healing, see section on “Two ways of wound healing”.
· Continuing breastfeeding
If positioning and attachment is adjusted so that pain is minimised with no new damage visible after a feed, you can continue breastfeeding. The wound will continue to heal. See our section “Expressing versus continued breastfeeding”.
· When to contact a medical professional
You should speak to your health visitor or GP if you have signs of infection (like abnormal swelling, inflammation, [pus – check description] discharge, fever and/or chills, or feeling ill), or if your wound doesn’t heal after a few weeks, even after adjusting attachment to a pain free latch. You can also check our section on “Other medical considerations”.
Supporting women with cracked nipples is such a large part of our work, it is surprising how little certainty there is on the best method of healing them. We know that adjusting positioning is crucial to avoid any further damage. An established wound that is slow to heal may be a sign of continued friction. So, start with watching a whole feed to see whether fresh injury is happening and if so, at what stage. Sometimes it’s when latching on, other times during a feed, or maybe it’s towards the end when the baby is getting sleepy and the mother’s arm relaxes downwards. Watching for any changes in suckling and swallowing will give further clues. Usually a more comfortable position can be found, but the wound may have been established for some weeks before we become involved. In these circumstances we can offer support while working towards comfortable feeding. Part of the feeding assessment should include looking into the baby’s mouth to check for a high palate or tongue-tie.
Watching for any changes in suckling and swallowing will give further clues. Usually a more comfortable position can be found, but the wound may have been established for some weeks before we become involved. In these circumstances we can offer support while working towards comfortable feeding. Part of the feeding assessment should include looking into the baby’s mouth to check for a high palate or tongue-tie.
Many women with cracked nipples want to know if there is anything they can put on the wound to speed up healing. A typical response might have been to suggest air drying or expressed breastmilk (EBM). However, when looking at the research we have a dilemma. A few years ago the available information on treatments was clear: In the Royal College of Midwives handbook, Successful Breastfeeding (2nd edition,1991, page 58), the section on treatment of sore nipples states “No randomised trial has yet been done to assess the usefulness of any of the creams, sprays, lotions or ointments [in current use] ….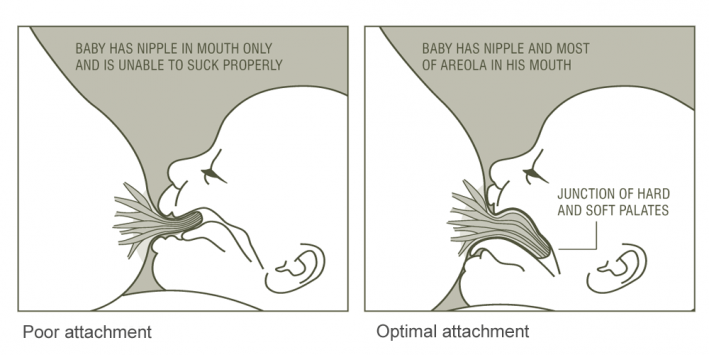 there is no scientific basis for their use. Nor is there any scientific evidence to support the use of expressed breastmilk or colostrum on the nipples after feeding.” The 3rd edition (2002) now agrees that there is a strong theoretical basis for moist wound healing techniques though they have yet to be evaluated in the context of RCT’s. Murray Enkin’s A Guide to Effective Care in Pregnancy and Childbirth’ (3rd edition 2000, p507), still relegates nipple creams and ointments to forms of care likely to be ineffective or harmful. However Renfrew, Woolridge, and Ross McGill (2000) consider new evidence that the presence of ‘epidermal growth factor’ in breastmilk has potential therapeutic benefit in promoting the growth and repair of skin cells. This growth factor appears to be passively transported from the circulation into breastmilk as levels measured are constant over weeks and throughout a day’s feeds.
there is no scientific basis for their use. Nor is there any scientific evidence to support the use of expressed breastmilk or colostrum on the nipples after feeding.” The 3rd edition (2002) now agrees that there is a strong theoretical basis for moist wound healing techniques though they have yet to be evaluated in the context of RCT’s. Murray Enkin’s A Guide to Effective Care in Pregnancy and Childbirth’ (3rd edition 2000, p507), still relegates nipple creams and ointments to forms of care likely to be ineffective or harmful. However Renfrew, Woolridge, and Ross McGill (2000) consider new evidence that the presence of ‘epidermal growth factor’ in breastmilk has potential therapeutic benefit in promoting the growth and repair of skin cells. This growth factor appears to be passively transported from the circulation into breastmilk as levels measured are constant over weeks and throughout a day’s feeds.
Mohrbacher and Stock (1997) retract information in the previous edition on keeping the skin dry when sore, cracked or bleeding and add that research into moist wound healing results in wounds healing 50% faster when the internal moisture of the skin is maintained.
All books agree that no product is a substitute for finding and correcting the cause of soreness. The aim of this article is to help women achieve pain free effective breastfeeding.
Sore or cracked?
There is a move towards using moist wound healing for cracked nipples. At this point it is worth distinguishing between sore (unbroken skin) or cracked (wounded, broken skin) nipples. Many of the text books discuss sore, rather than cracked nipples or include sore and cracked nipples together (see above). This is reflected in the design of many research studies into moist wound healing, so it is perhaps not surprising that results are often inconclusive.
Mohrbacher and Stock (1997) now say, ‘keeping the skin dry is no longer recommended for nipple soreness’ while reminding us that many creams and ointments sold for the treatment of sore nipples may actually contribute to the problem (page 394). Yet sore nipples should be able to heal without creams, providing help is given with positioning to prevent a crack developing. Renfrew, Woolridge, Ross McGill (2000) find it plausible that this process (of moist wound healing) may have contributed to the previously reported claims by women that oil-based formulations (eg lanolin, ‘Calendula’, ‘Kamillosan’) are beneficial with nipple soreness.
Renfrew, Woolridge, Ross McGill (2000) find it plausible that this process (of moist wound healing) may have contributed to the previously reported claims by women that oil-based formulations (eg lanolin, ‘Calendula’, ‘Kamillosan’) are beneficial with nipple soreness.
Any study which suggests that using a moisturiser would help women with sore nipples should compare subsequent rates of cracked nipples in each group, as well as levels of pain. There appears to be no such study. It seems probable that the main use of moisturisers (or other forms of skin care) should be when the skin is broken as a result of nipple trauma, especially when prevented from healing by repeated damage. Renfrew, Woolridge, Ross McGill (2000) agree that no controlled studies of adequate size have been published to date.
Compare this with general health care, where the principles of moist wound healing are well established. The importance of a moist environment for wound healing was identified by the work of George Winter (Nature, 1962, 193, 293-294.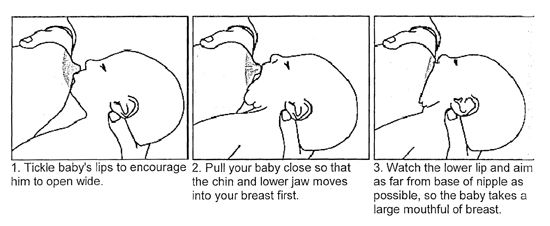 ). He compared the effect of leaving superficial wounds exposed to form a scab, with the effect of applying a vapour-permeable film dressing (on a pig). The wounds healed twice as quickly when kept humid. The dressing maintained humidity on the wound surface, allowing skin cells to slide across the surface of the wound. With a scab, the cells had to go deeper under all the dry crust and dead skin to find a moist layer (ref 6, p79).
). He compared the effect of leaving superficial wounds exposed to form a scab, with the effect of applying a vapour-permeable film dressing (on a pig). The wounds healed twice as quickly when kept humid. The dressing maintained humidity on the wound surface, allowing skin cells to slide across the surface of the wound. With a scab, the cells had to go deeper under all the dry crust and dead skin to find a moist layer (ref 6, p79).
Ideal skin care would allow moisture to be retained, without making the skin ‘soggy’ (or macerated) – like when a plaster has been on the skin too long, or feet go wrinkly in the bath. This moisture prevents a hard scab forming. When applying this to cracked nipples, a softer wound has an extra advantage. There is less risk of further damage happening during breastfeeding as there is no hard scab to pull off during a feed, taking the new skin cells lying underneath with it.
Keeping the wound moist also reduces pain by keeping air from drying out the exposed nerve endings (then more pain as it rehydrates) (ref 6, p80). Just as grazed knees are really nippy when going into the bath, but don’t hurt so much once underwater, keeping a cracked nipple moist avoids it being re-wetted every time the baby latches on. We are, however, unaware of any study that has looked at this specifically.
Just as grazed knees are really nippy when going into the bath, but don’t hurt so much once underwater, keeping a cracked nipple moist avoids it being re-wetted every time the baby latches on. We are, however, unaware of any study that has looked at this specifically.
Two ways of wound healing
Normally a new wound heals when the edges close together. An established wound heals from the base upwards, with the new skin growing over the edges, so they look smooth – often described as a rolled edge. As these wounds look like they are healing relatively slowly, women can feel disheartened. It helps to explain this and to look for the wound getting shallower. These wounds are most likely to benefit from moist wound healing, reducing any scab formation and allowing the skin cells to glide over each other.
| Amendment – Sept 2019 This is sometimes referred to as secondary wound healing, as opposed to the primary wound healing that occurs for more recent and superficial wounds. |
Newly healed wounds are not as strong as normal skin, so can re-open if the baby slips when feeding. This is more likely to happen when the mother or baby is sleepy. Feeding lying side-on may help reduce the chance of this happening during night-time feeds.
While the wound is healing, it sometimes helps to talk about a pain scale – imagine a ruler numbered 0 to 10, with 10 being unbearable pain. Suggest trying to drop down the scale at each feed so the mother can see a progression towards no pain at all. Correcting the position should give her an instant drop someway down the scale but not necessarily to 0. Depending on the extent of the wound, it may take some time before she reaches 0. If pain stays the same, or increases, ask her to contact you again.
Expressing versus continued breastfeeding
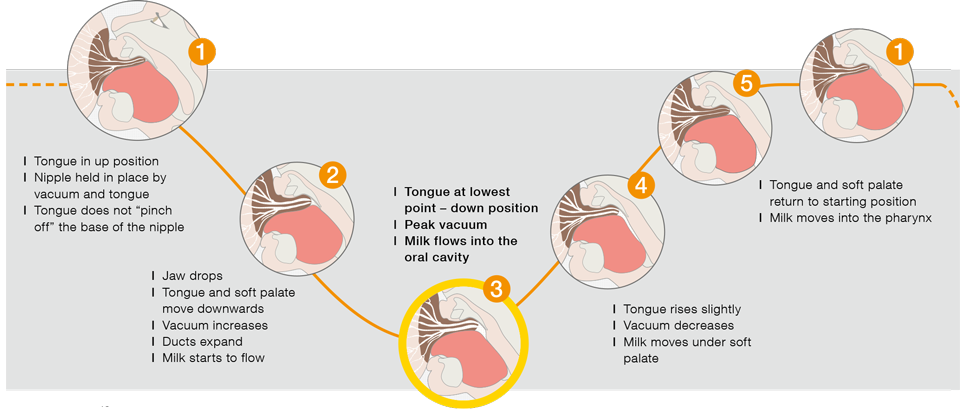
Expressing is sometimes suggested as an option to ‘rest’ the nipple. Finding a comfortable feeding position however, is usually less trouble than expressing milk, which puts suction on the wound. Breastfeeding only involves suction at the very beginning of the feed, as the nipple and areola are drawn into the baby’s mouth to form a teat. Once the milk begins to flow the negative pressure is relieved and the nipple should be well into the baby’s mouth, safe from any further damage (ref 12, Chap 80, p1362).
Possible treatments
The table below reviews the different moist wound healing treatments available. Choosing a moisturiser is not easy. Perhaps the first suggestion for mothers would be either white soft paraffin (Vaseline) or purified lanolin (such as Lansinoh ®). Vaseline is widely used in wound care, either directly, or as a base for other creams. Lanolin is also used as a base but concerns over allergic responses and high levels of contaminants (ref 2 and 7) limit its use. Purified lanolin is a purified anhydrous version. The revised edition of the Breastfeeding Answer Book warns that Vaseline is unsuitable because it “keeps out air” (ref 2, page 163) and is “not safe for ingestion” (page 395). Unfortunately, these comments are not referenced and the standard reference book for drugs, Martindales Pharmacopoeia, makes no reference to this. Softened paraffin is likely to stay on the surface of the skin longer than purified lanolin but this is what makes it so useful in preventing hard scab formation. It is worth noting that white soft paraffin, or its unbleached version yellow soft paraffin, has been widely used over many years for lip care in special care baby units – if it was unsafe for ingestion why is it used directly on babies lips? White soft paraffin is widely available and cheap (a small tin currently costs 99p) while purified lanolin cost between £5-£10.
Purified lanolin is a purified anhydrous version. The revised edition of the Breastfeeding Answer Book warns that Vaseline is unsuitable because it “keeps out air” (ref 2, page 163) and is “not safe for ingestion” (page 395). Unfortunately, these comments are not referenced and the standard reference book for drugs, Martindales Pharmacopoeia, makes no reference to this. Softened paraffin is likely to stay on the surface of the skin longer than purified lanolin but this is what makes it so useful in preventing hard scab formation. It is worth noting that white soft paraffin, or its unbleached version yellow soft paraffin, has been widely used over many years for lip care in special care baby units – if it was unsafe for ingestion why is it used directly on babies lips? White soft paraffin is widely available and cheap (a small tin currently costs 99p) while purified lanolin cost between £5-£10.
Sue Huml, Lactation Consultant for Lansinoh ®, believes “Petrolatum [Vaseline] is occlusive (prevents any air reaching the wound/skin). Lansinoh ® is semi-occlusive, allowing oxygen and water transpiration. Petrolatum remains on the surface of the skin. Lansinoh ® penetrates the stratum corneum and in a study was found to penetrate into the stratum granulosum, where in can hold moisture already in the skin …… In lanolin sensitive patients researchers were unable to elicit a single allergic response.”
Lansinoh ® is semi-occlusive, allowing oxygen and water transpiration. Petrolatum remains on the surface of the skin. Lansinoh ® penetrates the stratum corneum and in a study was found to penetrate into the stratum granulosum, where in can hold moisture already in the skin …… In lanolin sensitive patients researchers were unable to elicit a single allergic response.”
| Amendment – Sept 2019 A 2014 feasibility study (https://doi.org/10.1891/2158-0782.5.1.28) investigated if breastfeeding women using purified lanolin may have a higher rate of infections than others – however the results weren’t conclusive. Further research is required to answer this question. |
A few things to try
- Get a breastfeeding supporter to watch a whole feed, even good positioning may be made better.
- Use only water when washing, because soap will dry the skin further.
- Massage the breast gently and/or hand express a little milk to shorten the time between the baby latching on and the milk beginning to flow.
- Feed when the baby at the first stirs rather than when really wide awake – so the baby feeds in a more relaxed way.
- Feed from the least painful side first.
- After a feed, try expressing some milk, and let it dry on the nipple.
- You can try anaesthetising the nipple with ice wrapped in a cloth before a feed.
- Consider pain relief, e.g. Paracetamol or Ibuprofen at least 30mins before a feed is expected, and at regular intervals.
- Change breast pads at each feed.
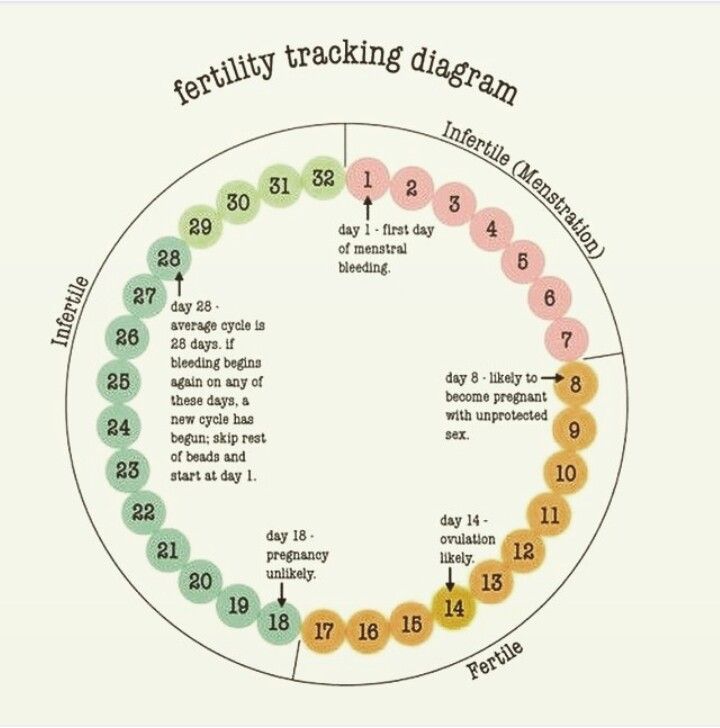
| Amendment – Sept 2019 Other medical considerationsNipple soreness can sometimes be caused by factors other than breastfeeding, such as the following. If in doubt, contact a medical professional.
|
Conclusion
Correcting positioning is paramount in allowing a damaged nipple to heal and enable pain free, effective breastfeeding. Sore nipples alone are unlikely to need further treatment, no evidence exists to support the use of creams, sprays or ointments to prevent or treat nipple soreness (11). Cracked nipples may benefit from applying a moisturiser such as white soft paraffin (Vaseline®) or purified lanolin. Some women may not like a particular choice of treatment. It may be useful to check whether they have any allergies to creams or cosmetics. Creams can be tested on their inner arm, but bear in mind that healthy skin is often less likely to react than damaged skin.
This is certainly an area in urgent need of systematic review and further, independent, research. We would like to hear from anyone with any experience of moist wound healing, with examples of what worked or not. We would like to collect this information. It’s your experiences that will help us learn.
It’s your experiences that will help us learn.
Moist Wound Healing Treatments: a review (November 1999, revised May 2001)
| Amendment – Sept 2019 For an update on this table, please refer to the Cochrane review “Interventions for treating painful nipples among breastfeeding women”, published in 2014 by C‐L Dennis, K Jackson and J Watson (https://doi.org/10.1002/14651858.CD007366.pub2). The authors of this review conclude that
|
| Product | Use/comment | Evidence |
| Expressed breast milk | Expressed breast milk has no risk of allergy, contains antibodies and ‘epidermal growth factor’ which potentially may promote the growth and repair of skin cells (1). Using expressed breastmilk encourages hand expressing – may have benefits not considered in studies of nipple healing. Is used in many cultures on skin irritations (2). | USP-modified lanolin, warm compresses, and expressed breast milk with air drying were compared to a control group (177 women with sore nipples) (3). Results No differences in pain or duration of breastfeeding. Exclusive breastfeeding rather than partial was a better predictor of breastfeeding beyond 6 weeks. Conclusion Clinicians should discontinue recommending creams and ointments, since these have not been proved to be effective… and may only present an unnecessary nuisance and expense for the mother. |
| White soft paraffin (Vaseline®) Widely available.
| Might try next after breast milk. Good at preventing scab formation which may be pulled off during a feed causing further damage. | Compared white soft paraffin to antibiotic creams in general wound healing (884 women) (4). Results No skin reaction to Vaseline® was found when confirmed by patch tests. Only 0.9% reacted in the antibiotic group. |
| Yellow soft paraffin Available in hospitals and pharmacies. | This is used in special care baby units as a moisturiser on babies’ lips. See above re scab formation | Not tested on nipple wounds although in common usage. Compared reactions to yellow and white soft paraffin on 3 people with known sensitivity to yellow soft paraffin (5). Results Within each brand purification meant less sensitivity, may mean white soft paraffin is preferable to yellow. |
| Jelonet® Available on prescription, or from pharmacies. | Useful on open, established cracks; should help stop the wound sticking to a breast pad. Use folded in double layer to stop drying out, if it still sticks try something else. Change at each feed. See illustration in (6) | Has been used as a wound dressing for many years. |
| Purified lanolin (e.g. Lansinoh ®) Substitutes are widely available in high street chemists and supermarkets and unlikely to be effective. | Claims to be absorbed more effectively than Vaseline® and that Vaseline® needs to be washed off – no evidence of this. Advertised in baby magazines. Look out for various substitutes purporting to be pure lanolin – some are diluted by other compounds i.e. liquid paraffin | Several studies published but have design shortcomings. No study found which compared purified lanolin to the soft paraffin group. One unpublished thesis compared purified lanolin to expressed breast milk (8) and (9). Results Cracked nipples took on average 1-2 days quicker to heal with purified lanolin. Delay in publication has been prolonged which must cast doubts on its methodology. |
| Creams Widely available | No scientific evidence exists for their use. Look for ingredients that should not be ingested by babies – vitamins, peanut oil. Many stores have own brand versions. Kamillosan® no longer contains peanut oil. | Referred to in (1) (11) (12) and (13).
|
| Hydrogel Expensive. Available from pharmacies e.g. as NuGel®, market is still developing | Various papers warn of the risk of the baby choking if the mother is sleepy enough to forget to take it off. Seems remote given that it would be held in place by a bra and breast pad which would have to be removed. Will absorb some wound fluid/ milk. Good at moistening a dry wound. Used for open and established wounds (granulating wounds). New dressings designed and marketed specifically for breastfeeding are being marketed in some countries. Some advantages are claimed for dressings containing glycerine, as these residues are considered safer. | Compared hydrogel dressings with standard hospital care of lanolin plus breast shells. (10) Results Stopped early because of increased infections in the hydrogel dressing group. |
| Sprays | Sprays have an alcohol base which is drying to the skin, may be more likely to cause cracking. May alter the normal skin bacteria | (1) (11) (12) (13) |
| Antibiotic creams Only available from GP’s.
Antibiotic dressings | Not in general use in the UK but is more common in America and through information found on internet sites. Expensive, can cause skin reactions, increase the risk of bacterial resistance. Wipe off excess cream before the next feed but don’t wash off or it may further damage skin. Tulle gauze used like Jelonet® – doubled over and kept under breast pad. May be used instead of a Jelonet® type dressing if the wound is superficially infected (11). | Study A randomised trial with 922 patients divided into 440 having white petrolatum (wsp) and 444 Bacitracin® – an antibiotic cream(ac) Results The rate of infection was similar in both groups (2%wsp v 0.9%ac, not sig). Antibiotic creams were associated with infections that were more serious and expensive to treat. No patient in the wsp group developed an allergic reaction but 4 did in the antibiotic group (4). In a study of treatments for infected sore nipples (confirmed by lab culture) better healing was achieved in the group taking antibiotic tablets rather than creams (14). Letter states study was too small to be conclusive (15). |
If using any of the above creams, apply after feeds. They do not need to be washed off before the next feed, though if using creams/gauze containing antibiotics its worth wiping off any excess before a feed (see above).
Phyll Buchanan, Anabel Hands and Wendy Jones, Breastfeeding Network Supporters
(2019 amendment also by Agnès Léger, Anthea Tennant-Eyles and Sarah Turner.)
Cracked nipples | Medela
Amir, L.H. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Jacobs, A. et al. S3-Guidelines for the Treatment of Inflammatory Breast Disease during the Lactation Period: AWMF Guidelines, Registry No. 015/071 (short version) AWMF Leitlinien-Register Nr. 015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs A. et al., "Recommendations S -3 for the management of inflammatory breast disease during breastfeeding: guidelines AWMF , registration number 015/071 (abbreviated version)" Leitlinjen- Registration number 015/071 (Kurzfassung). Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding handbook for physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
Lawrence , R . A . & Lawrence , R . M . Breastfeeding : a guide for the medical profession ( Elsevier Mosby , Maryland Heights , MO , 2011). - Lawrence R. A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
McClellan, H.L. et al. Infants of mothers with persistent nipple pain exert strong sucking vacuums. Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." Pediatrics 97, 1205–1209 (2008).
McClellan, H.L. et al. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeed Med 7, 275–281 (2012). — McClellan H.L. et al., "Breastfeeding frequency, milk quantity and duration of feedings in case of persistent sore nipples in the mother", Brestfeed Med (Breastfeeding Medicine) 7, 275–281 (2012).
McClellan, H.L. et al. Nipple pain during breastfeeding with or without visible trauma.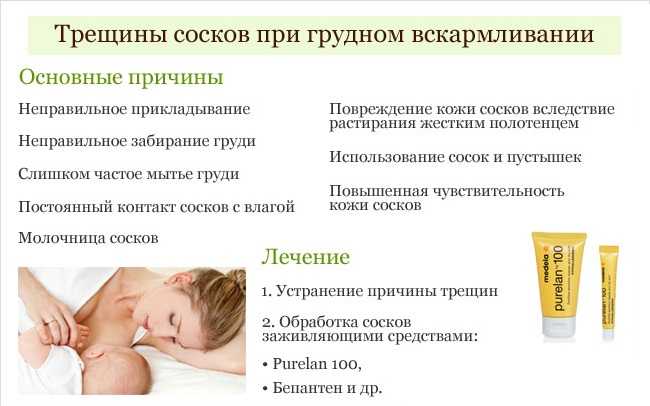 J Hum Lact 28, 511–521 (2012). — McClellan H.L. et al., "Nipple pain during breastfeeding with or without visible lesions." J Hum Lakt (Journal of the International Association of Lactation Consultants" 28, 511–521 (2012).
J Hum Lact 28, 511–521 (2012). — McClellan H.L. et al., "Nipple pain during breastfeeding with or without visible lesions." J Hum Lakt (Journal of the International Association of Lactation Consultants" 28, 511–521 (2012).
Hale, T.W., & Rowe H.E., Medications and mothers' Milk 2014 (Hale Publishing, Plano, 2014). - Hale T . and Row X . and ., " medicinal Preparations in Maternal ". Publishing Hale
Nipple fissure - health articles
11/10/2022
Nipple fissure - defect, damage to the integrity of the skin on the nipples of the mammary glands. It is manifested by a sharp soreness with irradiation to the shoulder blade when feeding a child. It can be complicated by infection of wounds, the development of candidiasis on the nipple, mastitis. If cracks become infected, there is a risk of infection of the child during feeding.
It can be complicated by infection of wounds, the development of candidiasis on the nipple, mastitis. If cracks become infected, there is a risk of infection of the child during feeding.
Treatment of cracked nipples begins with the elimination of their cause. In parallel, they carry out the prevention of their infection, use means that promote the speedy healing.
Causes
The main reason for the appearance of cracks is the lack of breastfeeding during feeding. When properly applied to the breast, the nipple rests against the baby's palate in a fixed motionless position, the child squeezes the areola with its jaws, contributing to the outflow of milk. In this case, the lower lip of the child is tucked up. If the nipple is not inserted to the proper depth, then it ends up on the tongue, gaining mobility, the lower lip injures the nipple and areola, and the jaws compress the breast in the most sensitive and easily damaged place. As a result of constant irritation of the nipple and areola areas, damage to the skin occurs - cracks form.
The second most common cause of cracked nipples can be improper weaning. Often, when feeding, mothers do not support the child's head, and also place his stomach not towards himself, but up. As a result, at the end of feeding, the child turns away from the breast, pinching the nipple in the jaws. There is pressure on areas of the nipple that are not intended for this.
Another common cause is washing your nipples too often. Modern medicine does not support the need to wash the breast after each feeding. With frequent washing, the nipples are washed off their natural lubricant, which is secreted by special glands in the skin of the areola (Montgomery's glands) and the nipples lose one of their natural protective mechanisms.
Fissures can also develop when feeding older children as a result of bites from erupted teeth.
The development of thrush contributes to the occurrence of cracked nipples.
Symptoms
Symptoms that may appear both in the early periods of feeding and later:
- single or multiple lesions of the skin of the breast, nipples and areals;
- superficial cracks that will show up on contact with underwear;
- subcutaneous fissures, characterized by severe pain;
- bleeding;
- slight suppuration;
- increased sensitivity and soreness of the nipples;
- Excessively dry skin around the nipples and areolas.
Even if you notice that at least one of the above symptoms appears from time to time and then disappears, this can also be an important signal of a possible infection or the presence of some other disease.
Treatment of cracked nipples
If it is a small cracked nipple, treatment can be started at home. The first step is to prevent infection. Change your underwear every day, iron your bra after washing with a hot iron. Put disposable sterile pads inside the bra and change them when they become damp.
Do not wash your breasts after each feeding, so as not to violate the natural protection. Mother's milk itself is a good antiseptic, so it can be used as a cream for cracked nipples, squeezing a few drops after feeding. Be sure to let the milk dry, hold your chest open for a few minutes.
Previously, when nipple cracks appeared, treatment was started with brilliant green. You should not do this, as it has been proven that brilliant green is quite toxic.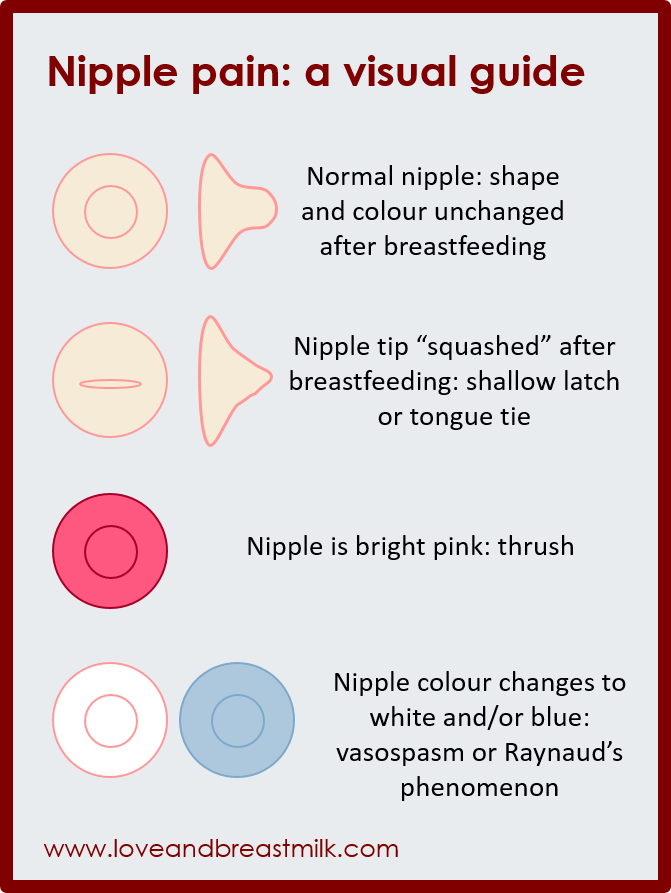 It is better to use a methylene blue aqueous or alcohol solution as an antiseptic, this antiseptic will also serve to prevent thrush in a child. It should be noted that antiseptics cannot solve the problem of how to treat nipple cracks, they only prevent infection.
It is better to use a methylene blue aqueous or alcohol solution as an antiseptic, this antiseptic will also serve to prevent thrush in a child. It should be noted that antiseptics cannot solve the problem of how to treat nipple cracks, they only prevent infection.
Cracked nipples can be lubricated with castor oil to soften the skin and heal quickly. It can be replaced with sea buckthorn or rosehip oil. Oil is applied to cracked nipples after feeding. Be sure to wait until it dries, and only then put on a bra.
Compresses for cracked nipples can be made from butter and applesauce. Apples need to be rubbed on a grater, add butter to them in a ratio of 1: 1 and attach to the chest. Hold the compress for 2-3 hours.
Kalanchoe or aloe juice has an excellent healing effect. The leaves of the plants are cut in half and smeared with pulp on the cracks in the nipples. Juice can be squeezed out and compresses can be made from it.
Cracked nipples during feeding can also be treated with products from a pharmacy.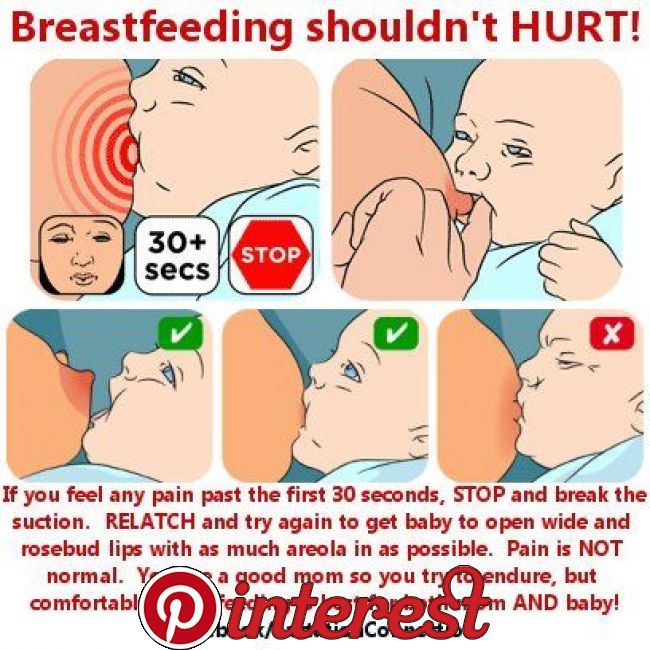
 Chronic wounds are more likely to heal “by secondary intention”, which means that they heal bottom to top. This process takes longer, and the wound is more susceptible to infection and scab formation in the meantime.
Chronic wounds are more likely to heal “by secondary intention”, which means that they heal bottom to top. This process takes longer, and the wound is more susceptible to infection and scab formation in the meantime.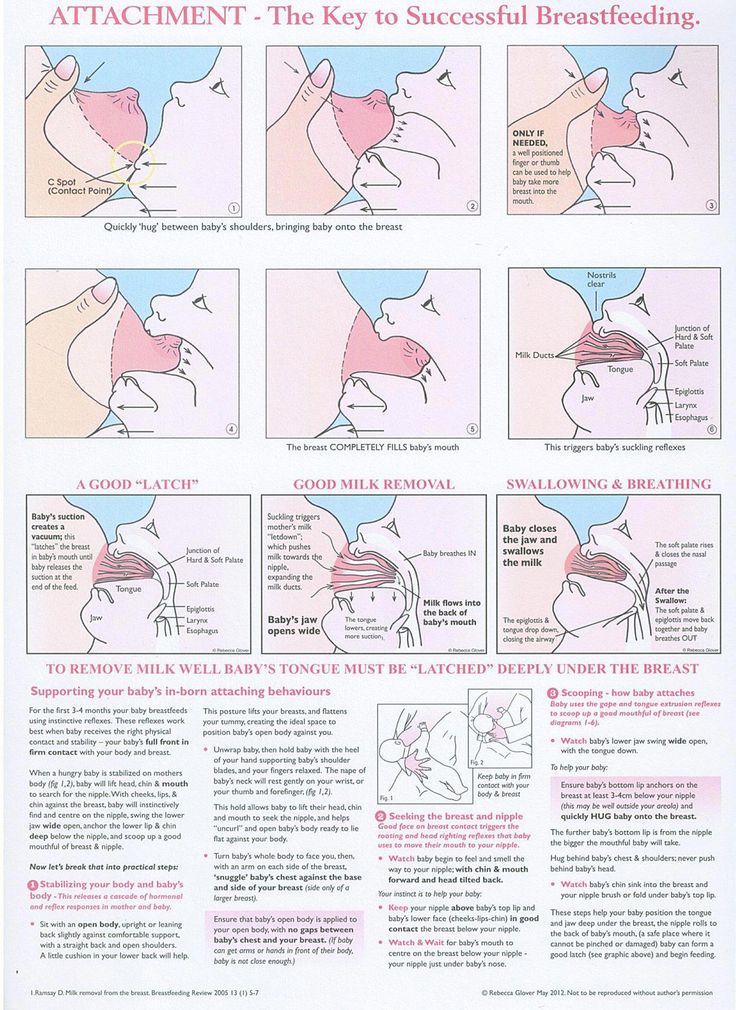 nhs.uk/conditions/breast-cancer/)
nhs.uk/conditions/breast-cancer/)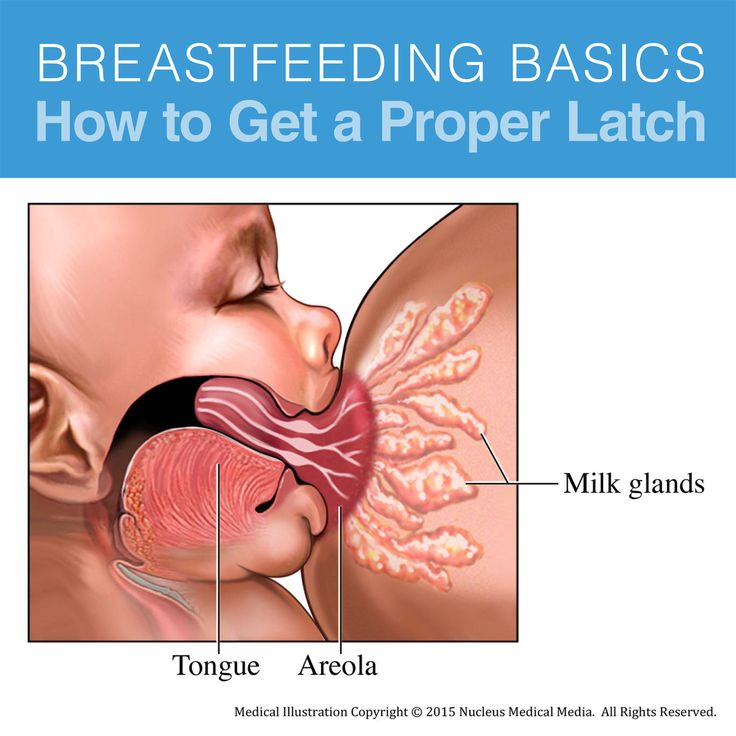

 Comes in foil pack or tin
Comes in foil pack or tin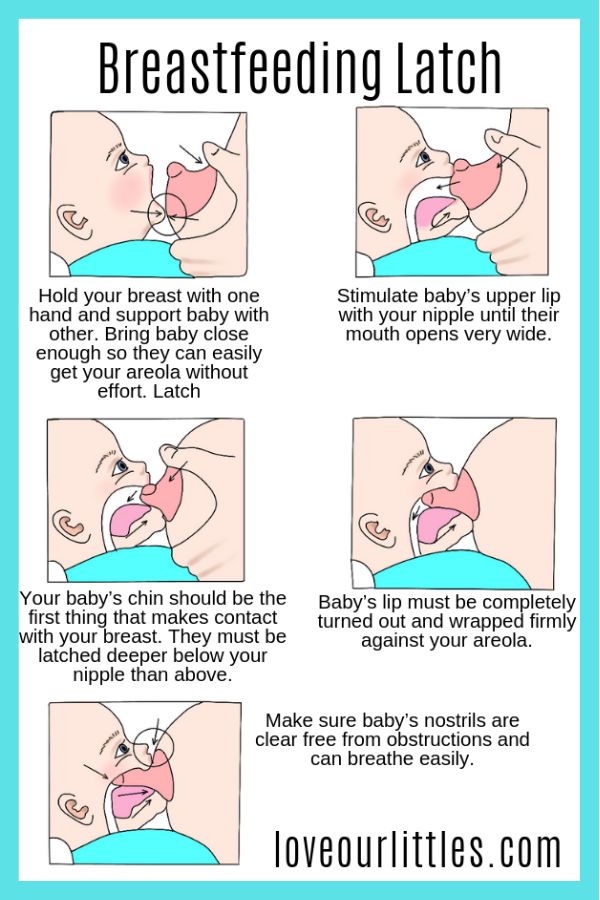
 Two groups each with
Two groups each with