Baby with umbilical cord attached
Umbilical cord care | Pregnancy Birth and Baby
Umbilical cord care | Pregnancy Birth and Baby beginning of content3-minute read
Listen
In the womb, the umbilical cord delivers the oxygen and nutrients needed to allow your baby to grow. After birth, the cord is clamped and cut, leaving a stump. This eventually falls off, healing to form the umbilicus (belly button). There are ways for you to prevent problems during healing.
What happens immediately after the birth?
After birth, the doctor or midwife cuts your baby’s cord from the placenta and puts a clamp on the remaining stump to pinch it off. After a couple of days, once the cord has dried, you can take the clamp off.
How long does the cord stay attached for?
The cord stump usually stays attached for 5 to 15 days. Over this time, the cord dries, shrinks and turns black. Sometimes, especially in the day or so before it falls off, the stump can ooze a little and may leave marks on your baby’s clothes.
Do not pull the cord stump off, even if it looks like it will come off easily, as this can prolong healing time and cause scarring. Let the cord stump fall off by itself in its own time.
When the stump falls off, there is sometimes a little bleeding at the stump site. This is normal and it should stop quickly.
Please see your doctor or maternal and child health nurse if you have any concerns, or speak to Pregnancy, Birth and Baby on 1800 882 436.
Caring for the umbilical cord
Wash the cord stump as part of your baby’s usual bathing routine.
Make sure you wash your hands first. Use only water and cotton pads, and dry it carefully. If wee or poo gets on the stump, you can use a mild soap to help clean it off. You don’t need to use antiseptics and alcohol.
Let the cord sit out of the nappy so it dries out in the air; this can be done by folding the nappy under the cord stump.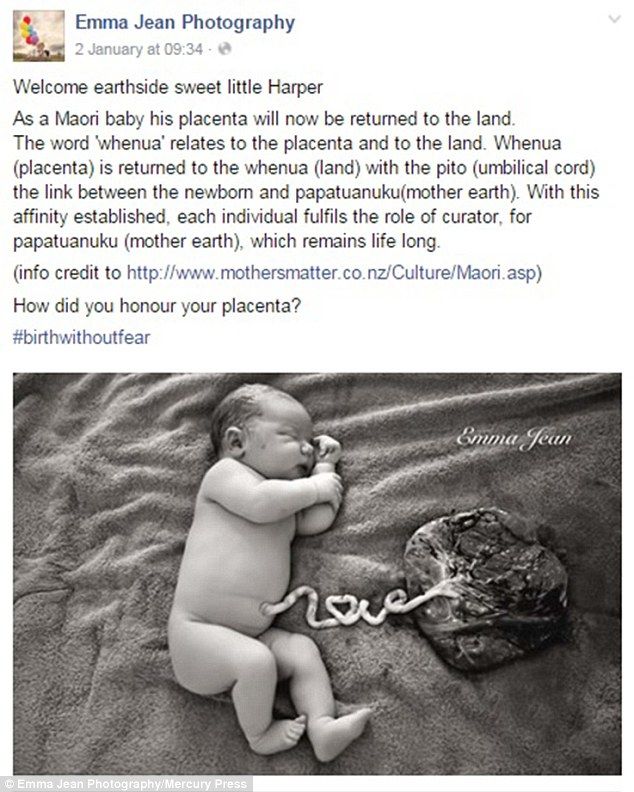 There is no need to cover the cord stump with Band-Aids or bandages, as this stops airflow around the stump.
There is no need to cover the cord stump with Band-Aids or bandages, as this stops airflow around the stump.
If you’re not washing the cord stump, try not to handle it.
How long does the belly button take to heal?
The belly button should heal completely in days. It may bleed or ooze a little after the cord falls off, but if there is continuous stickiness or discharge, it may be infected and you should show your doctor or maternal and child health nurse.
Sometimes the belly button does not heal completely and moist red tissue forms over the stump site, often with a lump present. This is called a ‘granuloma’. It is usually harmless, but you should ask your doctor or child and family nurse to have a look at it.
How to tell if the cord is infected
Signs of an infection of the belly button may include:
- redness, swelling, stickiness or a bad smell on or around the belly button
- fevers, poor feeding and tiredness in your baby
If you think your baby’s cord stump or belly button is infected, see your doctor as soon as possible.
Sources:
Victorian Agency for Health Information (Umbilical cord care for neonates), Raising Children Network (Umbilical care), Royal Children’s Hospital Melbourne (Umbilical granuloma – pre-referral), Cochrane (Topical umbilical cord care at birth)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: December 2020
Back To Top
Related pages
- Baby's first 24 hours
- Mum's first 24 hours after birth
- About the placenta
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.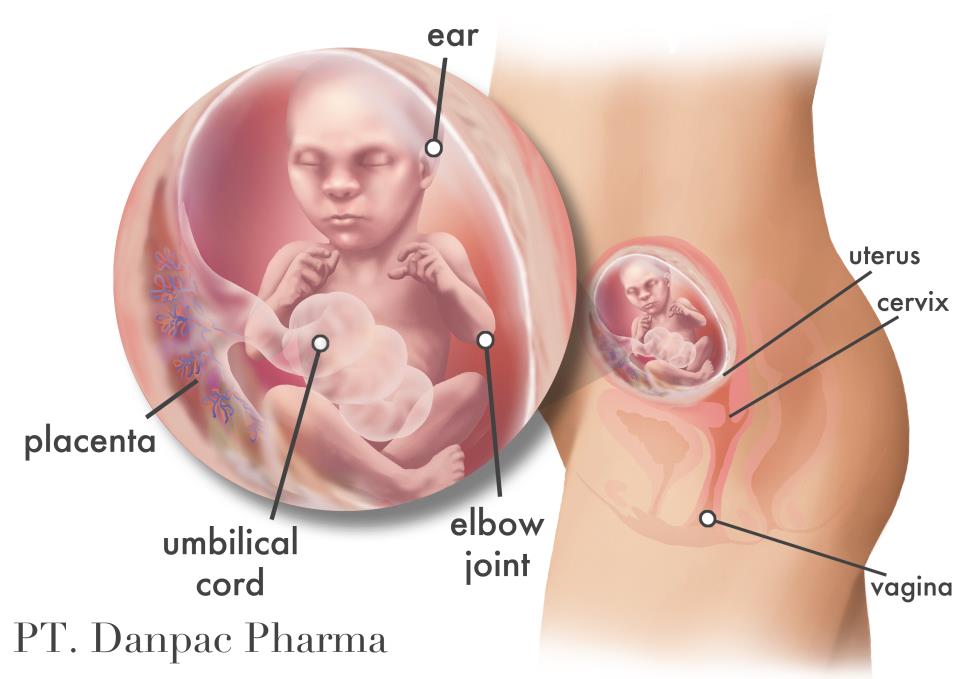
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
4 Reasons to Consider Delayed Cord Clamping
Choosing to delay clamping the umbilical cord after giving birth can give a newborn baby’s health a boost.
OB/GYN Courtney Barnes, MD, explains the benefits of this simple change in the birthing process.
What is delayed cord clamping?
During pregnancy, the umbilical cord connects the fetus to the placenta. The placenta allows nutrients and oxygen to pass from the mother to the baby. After the birth of the baby, the umbilical cord is still attached from the baby’s belly button to the placenta, and nutrient-rich blood remains within the umbilical cord and the placenta.
Delayed cord clamping means that doctors don’t immediately clamp and cut the umbilical cord. Instead, they allow extra time for the blood in the cord and placenta to flow to the baby. Eventually, the placenta, also known as afterbirth, detaches from the uterus and is also delivered. The baby then receives oxygen through his or her lungs and nutrition from the mother’s milk.
“Until recently, hospitals immediately clamped and cut the umbilical cord after delivery of the baby,” Barnes says. “By delaying the clamping of the cord, more blood travels from the cord and placenta to the baby. ”
”
Delayed cord clamping is now standard practice at MU Health Care for most births. Here’s why:
Courtney Barnes, MD
1. It decreases the risk of anemia
“For full-term babies, delayed cord clamping increases the baby’s blood volume and iron stores,” Barnes says. “Because iron is poorly transferred into breast milk, this extra iron helps prevent anemia.”
Anemia is a condition characterized by low red blood cell volume. Increased red blood cell count can lead to better development as the baby grows.
2. The benefits are even greater for preterm babies
Babies born prematurely are at risk for serious health problems, and an extra boost of healthy blood from the umbilical cord can help lower that risk.
According to Barnes, delayed cord clamping in preterm babies has been shown to decrease the number of needed blood transfusions and reduce the risk of necrotizing enterocolitis (a severe complication involving the intestines of a preterm baby) and interventricular hemorrhage (a bleed in the baby’s brain that can cause lifelong neurologic problems).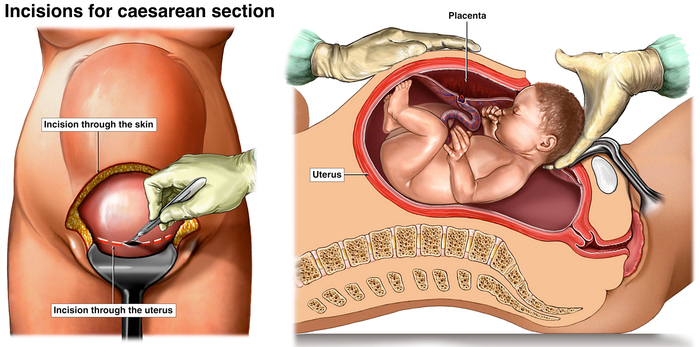
3. It can be performed with a C-section
Because cord clamping can take place after the placenta has been removed from the mother’s uterus, there is no added risk to the mother or child to delay cord clamping after a cesarean birth.
“Since the operating rooms are often quite chilly, special attention needs to be paid to ensure that the babies stay warm,” Barnes says.
4. It’s a very safe procedure
There are very few risks associated with delayed cord clamping for healthy mothers and babies.
“The main risk to delayed cord clamping is that the increased blood volume may result in jaundice,” Barnes says. “Because all babies are monitored for jaundice, this is a complication that we would be able to detect.”
Treatment for jaundice involves placing the baby under a light that helps break down excess bilirubin in the blood.
When you should avoid delayed cord clamping
“There are some reasons that delayed cord clamping should be avoided,” Barnes says.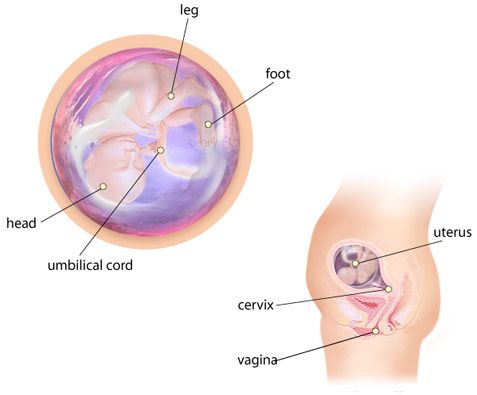 “For example, in women with abnormal placentas, women experiencing a hemorrhage or babies who are born needing immediate medical care, delayed cord clamping is not recommended.”
“For example, in women with abnormal placentas, women experiencing a hemorrhage or babies who are born needing immediate medical care, delayed cord clamping is not recommended.”
In these cases, doctors will clamp the cord immediately to focus on the health of mother and child.
Learn more
Family Birth Center
Read more stories like this
Women's Health
Child Health
Wrapping the baby's umbilical cord | What to do if the umbilical cord is wrapped around the baby
Pregnancy
Article
5/5 1 reviews
Cord entanglement is a fairly common diagnosis, which is made by approximately 25-30% of pregnant women. Why this happens, is it dangerous for the fetus and what to do - read further in the article.
4 min. for reading Feb. 17, 2022
Pregnancy is an exciting and joyful state, but often it is associated with a whole range of worries and anxieties. Most often, expectant mothers worry in vain, but sometimes there is still cause for concern. For example, when an ultrasound shows that the fetus is wrapped around the umbilical cord.
Such a diagnosis is not always considered a pathology and occurs in about every third pregnant woman. If this became known in the early stages of pregnancy, there is nothing to be afraid of. The size of the fetus at this time is quite small, it has a lot of space, it can freely roll over and swim in the amniotic fluid, getting entangled in the umbilical cord several times a day and successfully unraveling from it. However, if a problem is found in the later stages of pregnancy, especially when the baby has already taken its place and prepared for the birth, measures should be taken immediately.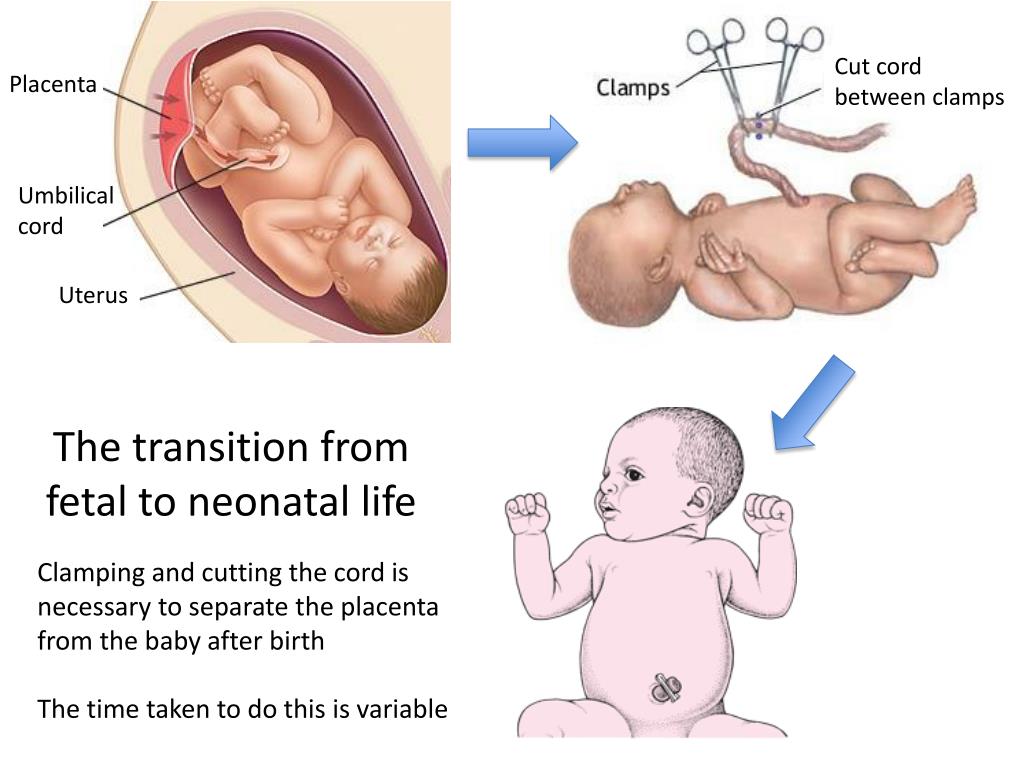
Why umbilical cord entanglement occurs
The umbilical cord is an organ that connects the fetus to the placenta and is a kind of transporter of blood and nutrients from the mother's body to the child's. It is formed starting from the 11th week of pregnancy, its length is normally 40-70 centimeters, and its thickness is up to 2 centimeters. Cord entanglement occurs for a number of reasons:
- The umbilical cord is too long.
The length of this organ is genetically determined and does not depend on such external factors as a woman's lifestyle, her weight, and so on. If the umbilical cord is longer than 70 centimeters, it forms loops that the baby can get into. An umbilical cord around the neck during pregnancy is the most common option. But the limbs of the child can also get into the loops of the umbilical cord.
- Excessive activity of the child.
Some babies are too active in the womb, which increases the risk of cord entanglement.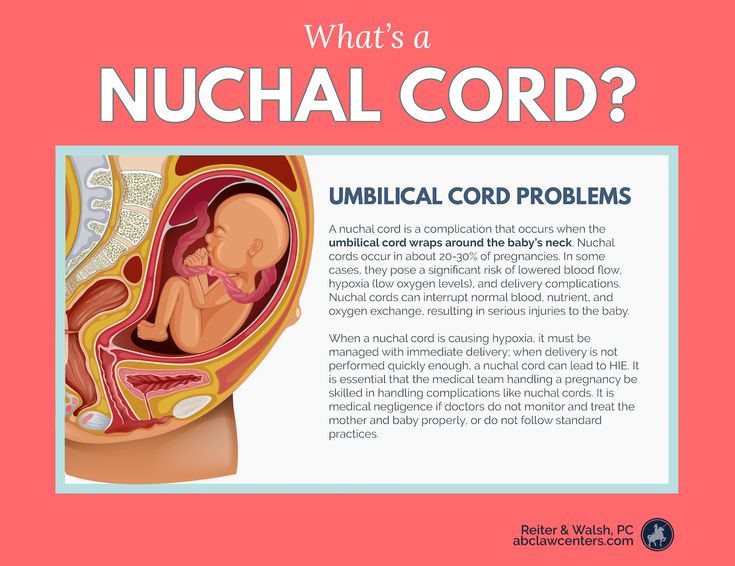 Such mobility can be a manifestation of the restless nature of the crumbs, or maybe a symptom of chronic hypoxia (oxygen starvation). When the child does not have enough oxygen, he begins to worry and inform his mother about his condition with active movements. Therefore, doctors recommend listening very carefully to the child's jolts and monitoring their intensity.
Such mobility can be a manifestation of the restless nature of the crumbs, or maybe a symptom of chronic hypoxia (oxygen starvation). When the child does not have enough oxygen, he begins to worry and inform his mother about his condition with active movements. Therefore, doctors recommend listening very carefully to the child's jolts and monitoring their intensity.
Normally, the number of movements during the day should be no less than 6 and no more than 10. If you notice that the number of shocks significantly exceeds this figure, or vice versa - there are too few of them, you should immediately consult a doctor.
- Polyhydramnios.
An excessive amount of amniotic fluid, especially in the later stages, is considered a complication of pregnancy. The abundance of amniotic fluid creates conditions in the womb under which the baby continues to actively move around while it should already take a place and prepare for birth. The condition is also dangerous because the child runs the risk of becoming entangled in the umbilical cord.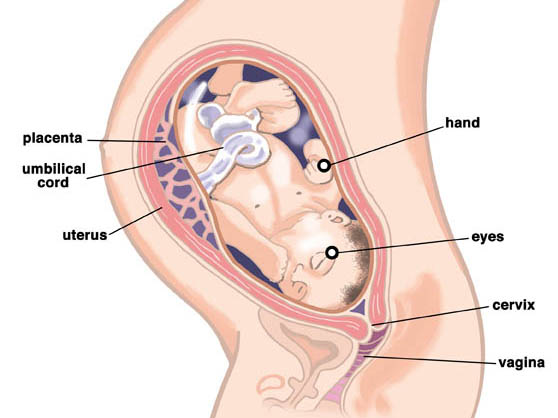
Is cord entanglement dangerous?
The fact that the umbilical cord is entangled is established during an ultrasound examination, as a rule, as part of one of the routine screenings. To determine the multiplicity of entanglement, an additional Doppler study is prescribed. A single, non-tight entanglement is the most common and safest. But it happens that the umbilical cord also forms several loops around the fetus. Is it dangerous? Explain and debunk myths.
- Can a baby suffocate in the womb if the umbilical cord is wrapped around the neck?
Many mothers-to-be are convinced that wrapping the cord around the neck can cause the baby to suffocate in the womb. This is not true. The baby begins to breathe on its own only after birth, when mucus is removed from its oral cavity. Prior to this, his airways are not involved, and oxygen is supplied through the umbilical cord.
- Does umbilical cord entanglement affect intrauterine development of the fetus?
In certain cases, yes.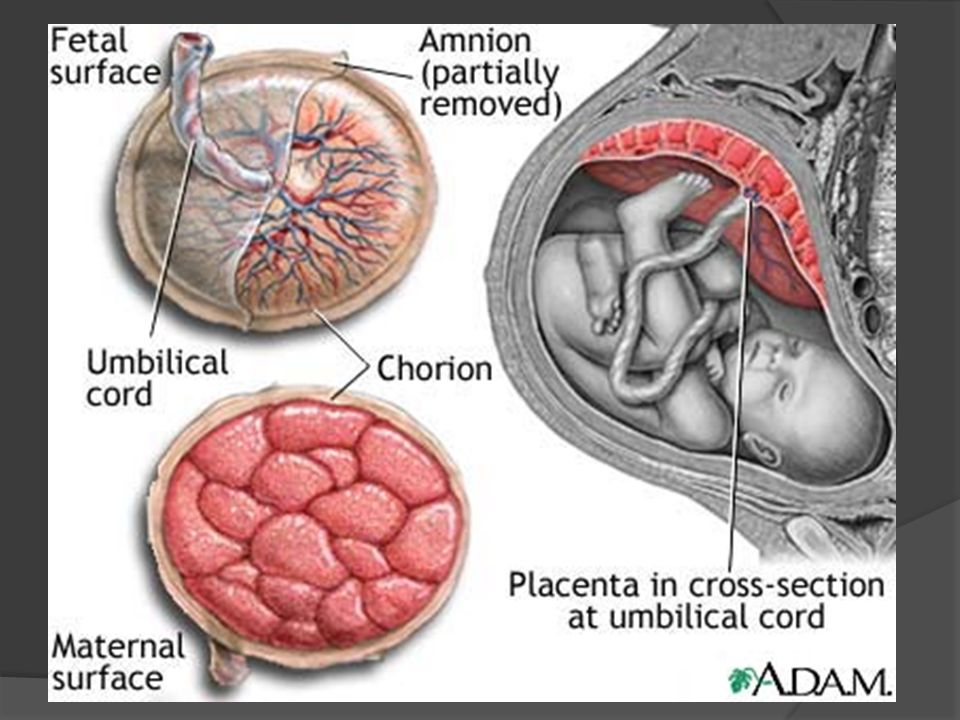 To understand if there is a risk for the child, cardiotocography is performed, which allows you to evaluate the work of his heart. If the study recorded a decrease in the number of heartbeats, this is a reason to take action. A slow heartbeat and impaired blood flow can provoke oxygen starvation of the fetus. The consequences of this can be irreparable.
To understand if there is a risk for the child, cardiotocography is performed, which allows you to evaluate the work of his heart. If the study recorded a decrease in the number of heartbeats, this is a reason to take action. A slow heartbeat and impaired blood flow can provoke oxygen starvation of the fetus. The consequences of this can be irreparable.
- Is it possible to untangle the umbilical cord while still in the womb?
There are no medical manipulations that can be used to eliminate the entanglement of the umbilical cord - there is no. But you can still do something. Try a special set of exercises for pregnant women.
- Is cord entanglement an indication for caesarean section?
The entanglement of the umbilical cord itself cannot be a reason for surgical intervention during childbirth. However, it carries a danger to the baby precisely in the process of birth. If the entanglement of the umbilical cord is multiple and tight, there is a risk that its length will not be enough to allow the baby to pass unhindered through the birth canal.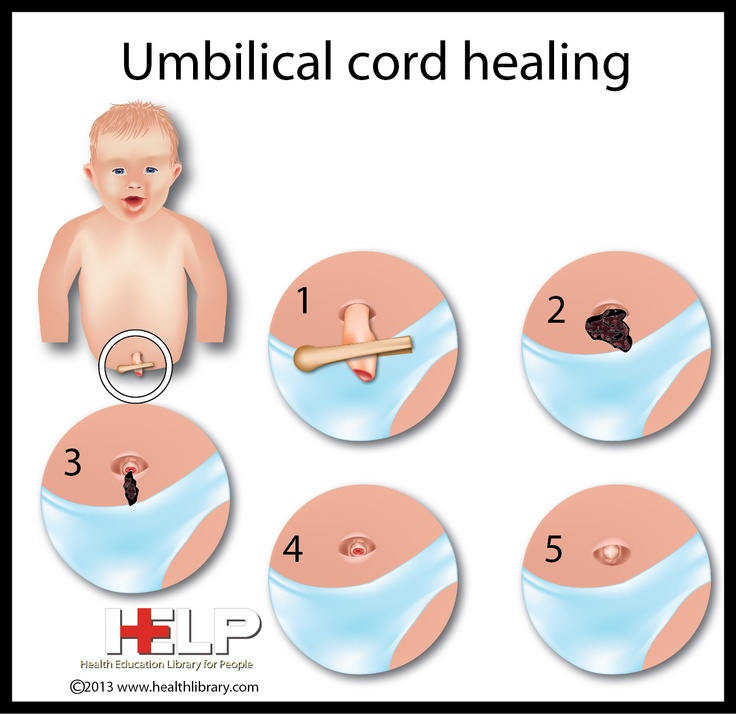 In addition, in such a situation, premature detachment of the placenta is possible - the most dangerous complication during childbirth. Until the baby begins to breathe on his own, he will receive oxygen through the placenta. Its detachment ahead of time is fraught with hypoxia for the baby.
In addition, in such a situation, premature detachment of the placenta is possible - the most dangerous complication during childbirth. Until the baby begins to breathe on his own, he will receive oxygen through the placenta. Its detachment ahead of time is fraught with hypoxia for the baby.
Cord entanglement does not always pose a risk to the baby. But this condition should not be neglected. If the doctor has made such a diagnosis, it is worth more closely monitoring the course of pregnancy and contacting a specialist at the slightest suspicion that something is wrong.
Related articles:
How the baby behaves before childbirth
Enema before childbirth: how and when to do it
Latest reviews
Average customer rating
1 customer ratings
Snapshot of community ratings
- 5 1
- 4 0
- 3 0
- 2 0
- 1 0
The Morozov hospital saved the life of a newborn by applying the unique EXIT procedure
A child with a severe anomaly in the development of the respiratory tract was born in the Morozov Children's Hospital. During labor, the multidisciplinary team performed a unique EXIT procedure on the newborn, which was the only way to ensure the baby could breathe effectively.
During labor, the multidisciplinary team performed a unique EXIT procedure on the newborn, which was the only way to ensure the baby could breathe effectively.
Soft tissue formation in the neck of the fetus was detected in utero during a routine ultrasound examination. According to the results of an MRI performed at the 33rd week of the mother's pregnancy, the tumor was about 5 cm in diameter, displaced the neck organs and completely squeezed the trachea . It was impossible to ensure the patency of the airways in the usual way, as is done in maternity hospitals, therefore, at the city perinatal council, it was decided to conduct delivery in a pediatric hospital, where there are all technologies to ensure the respiratory function and patency of the respiratory tract of a newborn ,” said Valery Gorev, chief physician of the Morozov Children’s Hospital .
A planned caesarean section was performed at a gestational age of 38 weeks in the Morozov hospital by the chief obstetrician-gynecologist of the DZM, head of the Perinatal Center of the City Clinical Hospital No.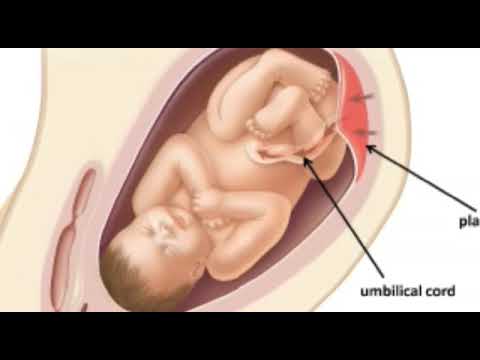 24, Ph.D. Anton Sergeevich Olenev together with the obstetric team and the chief neonatologist of the DZM, chief physician of the Morozov Children's Hospital, Ph. Valery Viktorovich Gorev . A multidisciplinary team of doctors from the Morozov Hospital participated in the operative delivery: Deputy Chief Physician for Surgical Care Alexander Pavlovich Kurkin , Head of the Department of Maxillofacial Surgery, Ph.D. Irina Gennadievna Bazina , Head of the Thoracic Surgery Department Oleg G. Topilin , Head of the Department of Resuscitation and Intensive Care for Newborns Mikhail Mikhailovich Kamenev , Professor, MD, otorhinolaryngologist Yuri Lvovich Soldatsky , anesthesiologist-resuscitator, Ph.D. Semyon Sergeevich Mezhinsky , anesthesiologist-resuscitator Anton Aleksandrovich Glazunov , anesthesiologist-resuscitator Nikolai Nikolaevich Selevich .
24, Ph.D. Anton Sergeevich Olenev together with the obstetric team and the chief neonatologist of the DZM, chief physician of the Morozov Children's Hospital, Ph. Valery Viktorovich Gorev . A multidisciplinary team of doctors from the Morozov Hospital participated in the operative delivery: Deputy Chief Physician for Surgical Care Alexander Pavlovich Kurkin , Head of the Department of Maxillofacial Surgery, Ph.D. Irina Gennadievna Bazina , Head of the Thoracic Surgery Department Oleg G. Topilin , Head of the Department of Resuscitation and Intensive Care for Newborns Mikhail Mikhailovich Kamenev , Professor, MD, otorhinolaryngologist Yuri Lvovich Soldatsky , anesthesiologist-resuscitator, Ph.D. Semyon Sergeevich Mezhinsky , anesthesiologist-resuscitator Anton Aleksandrovich Glazunov , anesthesiologist-resuscitator Nikolai Nikolaevich Selevich .
“The only option for effective breathing after birth was EXIT. This is a specific surgical intervention performed on a newborn with partial birth and preservation of uteroplacental blood flow to ensure gas exchange through the placenta. While the baby remained attached to the placenta by the umbilical cord, the surgeons performed a tracheostomy followed by tracheal intubation. To ensure effective and safe stabilization of breathing, restoration of tidal volume, a special type of artificial lung ventilation was performed for a small patient during the procedure, infusion therapy was started, and anesthesia was continued. After the completion of the EXIT procedure, the umbilical cord was cut without the risk of destabilization of the condition, and the baby was born ", - said the anesthesiologist-resuscitator Semyon Mezhinsky .
The complexity of the EXIT procedure lies in the organization of work on multidisciplinary coordination between obstetrician-gynecologists, neonatologists and specialists operating on a newborn. For the successful implementation of the intervention, doctors developed an algorithm that involves the phased application of various methods of ensuring airway patency, depending on the clinical situation.
For the successful implementation of the intervention, doctors developed an algorithm that involves the phased application of various methods of ensuring airway patency, depending on the clinical situation.
According to doctors, the peculiarity of managing a newborn in the early postoperative period, taking into account separate intubation (right bronchus and trachea), was the use of a unique method of respiratory support - intrapulmonary pneumopercus ventilation. This made it possible to effectively and safely stabilize gas exchange and prepare the child for the next stage of treatment - removal of a neck tumor and tracheal plasty.
The operation was performed using the extracorporeal membrane oxygenation (ECMO) technique with subsequent stabilization of vital functions using targeted inotropic and vasotonic support and high-frequency ventilation in the early postoperative period.
Histological examination confirmed the malignant nature of the tumor - it was an immature teratoma.