How to get rid of a back cramp
Causes, Treatment & What Is It
Overview
What are back spasms?
A spasm is when your muscles suddenly and against your will. They may painfully twinge, seize or contract. The muscles in your upper, middle and lower back are divided into three types: intrinsic/deep muscles, superficial muscles and intermediate muscles. Lower back spasms are more common, but any muscle can contract.
How common are back spasms?
Around 80% of people in the U.S. have had or will have some sort of back pain in their lives. Back spasms and other back pain are, unfortunately, common.
How do back spasms start?
Back spasms can start with no warning, or they may begin as a mild twitch that builds to agonizing pain.
Who is more likely to get back spasms?
Athletes, those who do heavy lifting and anyone with other types of back pain are more likely to experience back spasms.
How do back spasms affect the rest of my body?
Sometimes pain from a back spasm can “radiate. ” This means that the pain starts in your back but moves to other parts of your body like your legs or hips.
Are back spasms a sign of multiple sclerosis?
No, but back spasms are a symptom of other serious diseases like gallstones and ankylosing spondylitis.
Are back spasms a sign of labor?
No. If you’re in labor you’ll feel the muscles in your uterus contract, not your back. But you may have back pain in your lower back as part of back labor.
Symptoms and Causes
What causes back spasms?
There are a number of possible causes for back spasms:
- Not using your muscles enough. If you sit too much, have poor posture, don’t exercise or rarely use your back or stomach muscles, those muscles can get weak and spasm.
- Using your muscles too much. Athletes and those who do a lot of heavy lifting may experience back spasms. Such activities can cause a muscle strain, which is a tear, and that can cause inflammation.

- Dietary issues. Back spasms can be caused by too little water, potassium and/or calcium in your diet.
- Mental/emotional health issues. Anxiety and stress can tense up your muscles.
- Trauma. You may injure your back in a fall or car accident.
Sometimes, your back spasms may mean that you have a serious condition, including:
- Epidural abscess.
- Gallstones.
- Stiff person syndrome.
- Ankylosing spondylitis.
- Kidney stones.
- Kidney infection.
- Tumor.
You’re more likely to experience pain that’s like a back spasm — but isn’t actually a back spasm — if you have any of the following disorders:
- Spinal arthritis.
- Herniated disk.
- Spinal stenosis.
- Curvature of the spine: scoliosis or lordosis.
- Spondylolysis or spondylolisthesis.
Can stress cause back spasms?
Yes. Talk to your healthcare provider about a referral to a therapist who can help you manage your stress and anxiety.
Can back spasms cause chest pain?
You should always go to the emergency room if you have chest pain. Pain in your back can sometimes radiate to other parts of your body, but it’s usually to your hips or legs.
What are the symptoms of back spasms?
A back spasm may feel mild like a dull ache or twitch, or it can get so sharp and painful that it’s debilitating.
If you experience any of the following symptoms in addition to back spasms, you should see your healthcare provider right away:
- Loss of bladder or bowel control.
- Muscle weakness in arms or legs.
- Odd sensations, numbness or weakness on one side of your body.
- Loss of balance and coordination.
- Loss of a sense of feeling in a limb/limbs.
How long do back spasms last?
If you use your back muscles too much, you may have spasms for a few days. It may take several weeks if there’s a muscle strain.
Diagnosis and Tests
How are back spasms evaluated and diagnosed?
After talking to you about your symptoms and getting a list of your medications, your healthcare provider may ask about your entire medical history. Be sure to mention any trauma to your back. Your provider may diagnose your back spasms based on the symptoms you describe.
Be sure to mention any trauma to your back. Your provider may diagnose your back spasms based on the symptoms you describe.
Which healthcare providers evaluate and diagnose back spasms?
You can see your primary healthcare provider about your back spasms. If needed, they may send you to a specialist.
What questions might a healthcare provider ask to help diagnose back spasms?
- What does the pain feel like?
- Where is the pain located?
- Have you ever loss control of your bowel or bladder?
- How long do the spasms last?
- How often do you have back spasms?
- Any stiffness?
- Do you get any tingling or numbness in your body?
- Do you ever feel weak or uncoordinated when you’re having back spasms?
- What medications are you taking?
Management and Treatment
How are back spasms treated?
Healthcare providers used to prescribe bed rest for those who deal with back spasms. Such inactivity is no longer recommended. Instead, follow your provider's instructions about the following:
Instead, follow your provider's instructions about the following:
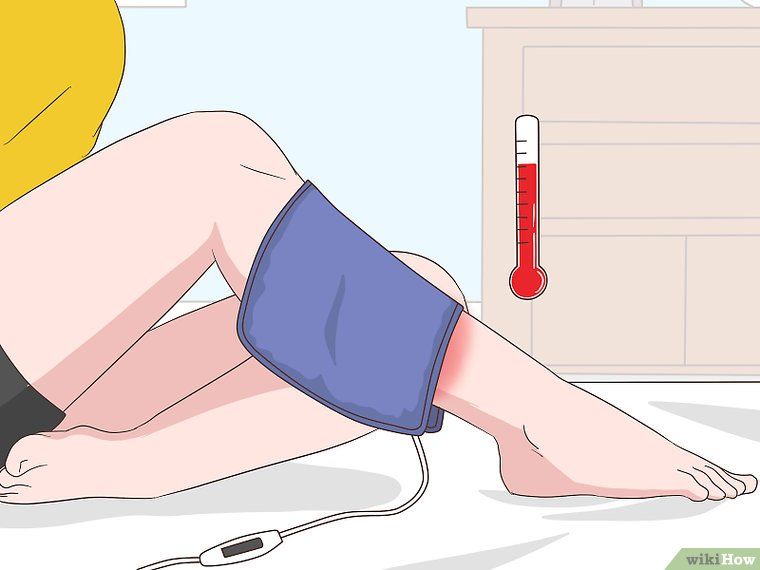
- Ice/heat: Apply ice or heat to the location of your back spasms. Wrap the ice pack or heating pad in a towel or pillowcase and apply it to your skin for 20 to 30 minutes. Then reapply after 20 to 30 minutes.
- Over-the-counter pain medications: Over-the-counter pain medications, including acetaminophen (Tylenol®), naproxen (Aleve®) or ibuprofen (Advil®, Motrin®).
- Muscle relaxants: Your provider may recommend taking a muscle relaxant like cyclobenzaprine, metaxalone or methocarbamol. If you do take them, take them at night (or when you're not operating a car or heavy machinery) and only for 72 hours or less.
- Physical therapy: Your healthcare provider might prescribe physical therapy, where you can learn relaxation techniques and stretches for your back muscles.
Are there any side effects of the medications prescribed for back spasms?
The side effects of muscle relaxants include:
- Confusion.
- Drowsiness.
Refer to the instructions that come with your prescription regarding dosages and when you can operate a vehicle.
What kind of healthcare provider treats back spasms?
Your primary healthcare provider can recommend at-home treatments, refer you to physical therapy and prescribe muscle relaxants, if necessary.
What happens if I don’t get treatment for my back spasms?
It’s possible that your back spasms may go away on their own, but it depends on what caused them. Talk to your healthcare provider about the best treatment plan for your situation.
Prevention
How can I prevent back spasms?
Back spasms aren’t 100% preventable. But you can consistent self-care can help, including:
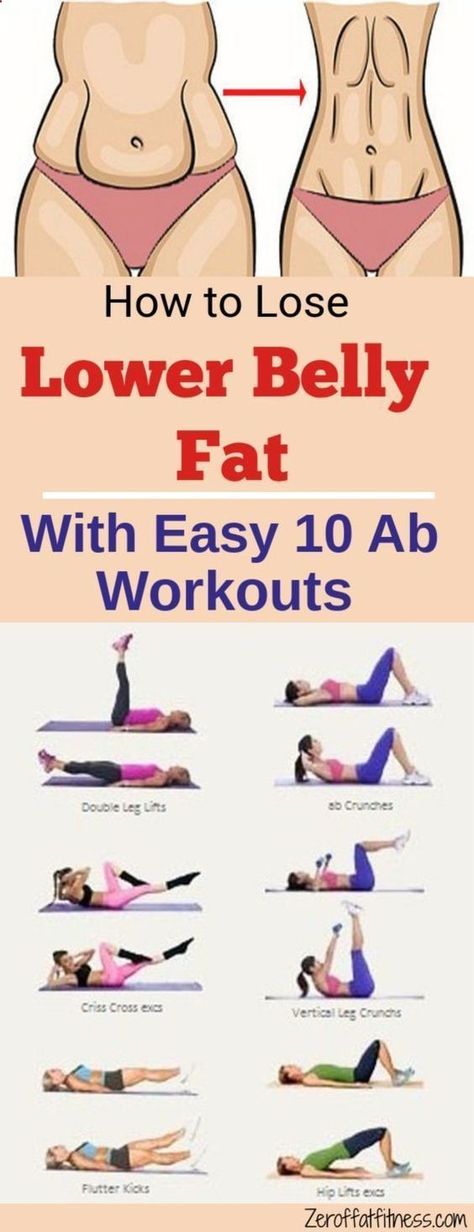
- Exercising.
- Sitting with good posture.
- Stress management.
- Getting up and stretching after you’ve been sitting for 30 minutes.
Outlook / Prognosis
Can back spasms go away on their own?
Yes, but they may also come back.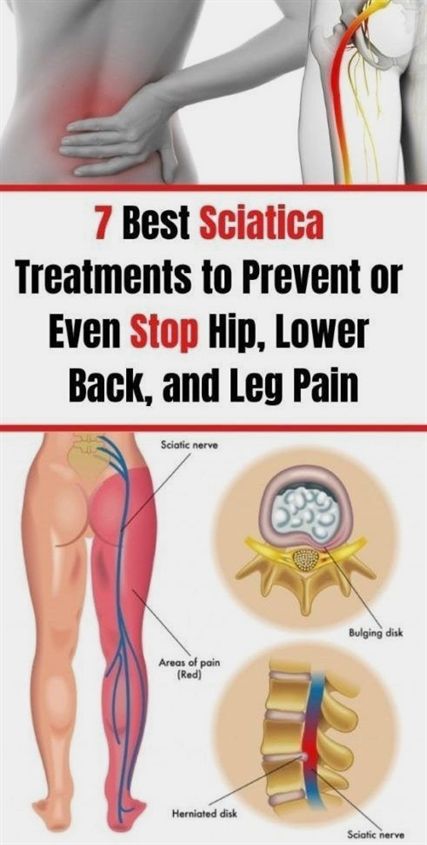
When can I return to my normal activities?
You might heal after a couple days, or it could be weeks. Talk to your healthcare provider about a recovery plan.
Are there any complications of back spasms?
Although back spasms don’t cause and aren’t caused by the following symptoms, they sometimes happen at the same time.
Other pain
- Backache.
- Shoulder pain.
- Arm pain.
- Headache.
- Hip pain.
- Buttock pain.
- Sciatica.
Stiffness
- Neck.
- Spine.
Other conditions
- Leg weakness.
- A curved spine.
- Numbness.
- Tingling.
Living With
When should I contact my healthcare provider?
You don’t have to live with back spasms and other types of back pain. Talk to your healthcare provider about your symptoms to receive treatment.
When should I go to the emergency department?
Call 911 if you’re unable to move because of the pain.
Back spasms are sometimes a symptom of a serious condition. See your healthcare provider right away if you also experience:
- Loss of bladder or bowel control.
- Muscle weakness in arms or legs.
- Odd sensations or numbness or weakness on one side of your body.
- Loss of balance and coordination.
- Loss of a sense of feeling in a limb/limbs.
What questions should I ask my healthcare provider about back spasms?
- What’s the best treatment for me?
- Do my back spasms mean that I have a serious disorder?
- Should I see a therapist for help with my stress?
- Should I try a muscle relaxant?
A note from Cleveland Clinic
Remember that it’s important to stay active even when you’re in pain (as long as that pain isn’t caused by over-using your muscles)! Get up and stretch every 30 minutes and exercise three times a week. To help with your pain, take over-the-counter medications and muscle relaxants and get a massage. Always discuss your symptoms with your healthcare provider so that you can get the best care.
Always discuss your symptoms with your healthcare provider so that you can get the best care.
Keep in mind that back spasms are sometimes a symptom of a serious disorder. Notice other symptoms you might have alongside them and go to the emergency department if you have tingling/numbness on one side, weakness or if you lose your ability to control your bowel or bladder. If you’re debating whether or not to go to the emergency department, it’s better to go and be told you’re not in serious condition than to stay home.
Gallstones (Cholelithiasis): Symptoms, Causes & Treatment
Overview
Do You Have Gallstone Pain?What are gallstones?
Gallstones form in your gallbladder, the small, pear-shaped organ where your body stores bile. They are pebble-like pieces of concentrated bile materials. Bile fluid contains cholesterol, bilirubin, bile salts and lecithin. Gallstones are usually made up of cholesterol or bilirubin that collect at the bottom of your gallbladder until they harden into “stones. ”
”
Gallstones can be as small as a grain of sand or as big as a golf ball. They grow gradually, as bile continues to wash over them and they collect extra materials. Actually, it’s the smaller stones that are more likely to cause trouble. That’s because smaller stones can travel, while bigger ones tend to stay put. Gallstones that travel may get stuck somewhere and create a blockage.
What is cholelithiasis?
Cholelithiasis is the condition of having gallstones. Many people have cholelithiasis and don’t know it. Gallstones won’t necessarily cause any problems for you. If they don’t, you can leave them alone. But gallstones can sometimes cause problems by creating a blockage. This will cause pain and inflammation in your organs. If it goes untreated, it can cause serious complications.
How common are gallstones?
Gallstones are common in developed countries, affecting about 10% of adults and 20% of those over the age of 65. Only 20% of people diagnosed with gallstones will need treatment.
How does having gallstones (cholelithiasis) affect me?
Your gallbladder is part of your biliary system. It belongs to a network of organs that pass bile between each other. These organs are connected by a series of pipelines called bile ducts. Bile travels through the bile ducts from your liver to your gallbladder, and from your gallbladder to your small intestine. Your pancreas also uses the bile ducts to deliver its own digestive juices.
A gallstone that travels to the mouth of your gallbladder can obstruct the flow of bile in or out. A gallstone that makes its way out of your gallbladder and into the bile ducts could block the flow of bile through the ducts. This will cause bile to back up into the nearby organs. When bile backs up, it builds pressure and pain in your organs and bile ducts and causes inflammation.
This can lead to a variety of complications, including:
- Gallbladder disease. Gallstones are the most common cause of gallbladder diseases.
 When they get stuck, they cause bile to back up into your gallbladder, causing inflammation. This can do long-term damage to your gallbladder over time, scarring the tissues and stopping it from functioning. The stalled flow of bile also makes infections in your gallbladder more likely.
When they get stuck, they cause bile to back up into your gallbladder, causing inflammation. This can do long-term damage to your gallbladder over time, scarring the tissues and stopping it from functioning. The stalled flow of bile also makes infections in your gallbladder more likely. - Liver disease. A blockage anywhere in the biliary system can cause bile to back up into your liver. This will cause inflammation in your liver, leading to an increased risk of infection and long-term scarring over time (cirrhosis). If your liver stops functioning well, your whole biliary system breaks down. You can live without a gallbladder but not without a liver.
- Gallstone pancreatitis. A gallstone that blocks the pancreatic duct will cause inflammation in your pancreas. As with your other organs, temporary inflammation causes pain, and chronic inflammation causes long-term damage that can stop your organ from functioning.
- Cholangitis.
 Inflammation in your bile ducts can lead to infections in the short term and scarring in the long term. Scarring in your bile ducts causes them to narrow, which restricts the flow of bile. This can cause long-term bile-flow problems even after the blockage has been removed.
Inflammation in your bile ducts can lead to infections in the short term and scarring in the long term. Scarring in your bile ducts causes them to narrow, which restricts the flow of bile. This can cause long-term bile-flow problems even after the blockage has been removed. - Jaundice. Backed-up bile will leak into your bloodstream, making you sick. Bile carries toxins that your liver has filtered from your body. The bilirubin content has a yellow color, which will be visible in the whites of your eyes.
- Malabsorption. If bile can’t travel to your small intestine as intended, you might have difficulty breaking down and absorbing nutrients from your food. Bile is particularly important for breaking down fats and for absorbing fat-soluble vitamins in your small intestine.
Symptoms and Causes
What is the main cause of gallstones?
As much as 75% of the gallstones healthcare providers discover are made up of excess cholesterol. So, we could say that having excess cholesterol in your blood is the leading cause of gallstones. You might have extra cholesterol for a variety of reasons. Some of the most common reasons include metabolic disorders, such as obesity and diabetes.
So, we could say that having excess cholesterol in your blood is the leading cause of gallstones. You might have extra cholesterol for a variety of reasons. Some of the most common reasons include metabolic disorders, such as obesity and diabetes.
High blood cholesterol leads to higher cholesterol content in your bile. Your liver filters cholesterol from your blood and deposits it in bile as a waste product before sending the bile to your gallbladder. Chemicals in bile (lecithin and bile salts) are supposed to dissolve cholesterol. But if there’s too much of it, these chemicals might not be up to the task.
What else causes cholelithiasis?
Other factors that contribute to gallstones include:
- Excess bilirubin: About 25% of gallstones are made up of excess bilirubin instead of cholesterol. Bilirubin is a byproduct that’s produced when your liver breaks down red blood cells. Certain medical disorders can cause your liver to produce extra bilirubin while doing its job.
 Some of these include infections, blood disorders and liver disease.
Some of these include infections, blood disorders and liver disease. - Gallbladder stasis: Your small intestine signals to your gallbladder to send bile when it has fats to digest. When your gallbladder is healthy, it contracts to efficiently move bile out when necessary. But if your gallbladder doesn’t contract well enough, some bile may be left behind. This bile gradually concentrates into a kind of sludge at the bottom of your gallbladder, which then crystallizes.
Who gets gallstones?
Anyone can get gallstones, including children, but they are more common after the age of 40. That’s because gallstones grow very gradually. It may take 10 to 20 years for gallstones to grow large enough to cause an obstruction. They are also more common in people assigned female at birth than in those assigned male at birth, by a ratio of 3:1. This is due to the effects of female hormones.
Other common risk factors include:
- Native American or Mexican descent.
 These peoples share a genetic profile of higher cholesterol levels.
These peoples share a genetic profile of higher cholesterol levels. - Metabolic syndrome. A constellation of metabolic risk factors, including overweight, high blood triglycerides and insulin resistance, contribute to the risk of cholesterol gallstones.
Why are women more at risk of developing gallstones?
Estrogen increases cholesterol, and progesterone slows down gallbladder contractions. Both hormones are especially high during certain periods in your reproductive life, such as menstruation and pregnancy. When hormone levels begin to drop in menopause, many people use hormone therapy (HT) to replace them, which elevates them again.
Women and people assigned female at birth are also more likely to gain and lose body fat more frequently. Excessive body fat can translate to extra cholesterol in your blood. Having obesity increases estrogen. On the other hand, rapid weight loss has a similar effect to weight gain. When you lose a lot of body fat at once, it sends an unusually large load of cholesterol to your liver for processing, which ends up in your bile.
What are the first signs of having gallstones?
You won’t notice your gallstones unless one gets stuck somewhere and causes a blockage. When that happens, the most typical symptom is a type of abdominal pain, in the right upper quadrant of your abdomen, called biliary colic. It occurs in episodes that last for one to several hours, usually after a large or rich meal. That’s when your gallbladder contracts to send bile to your small intestine for digestion.
If you have occasional episodes of biliary colic, it means that a gallstone is causing a partial blockage, but you can’t feel it until your gallbladder contracts. The contraction forces pressure through your bile ducts and causes that pressure to build up inside when it meets resistance. This is a warning sign. When the blockage becomes more severe, your pain will too.
What is gallstone pain like?
Gallbladder pain most often occurs in the upper right side of your abdomen, under your ribcage, where your gallbladder is located. But sometimes it feels more vaguely located in your abdomen. The pain can also radiate somewhere else, most often to your right arm or shoulder blade. It starts as an ache and then steadily increases in intensity over the first hour before receding again.
But sometimes it feels more vaguely located in your abdomen. The pain can also radiate somewhere else, most often to your right arm or shoulder blade. It starts as an ache and then steadily increases in intensity over the first hour before receding again.
Despite the name, biliary colic is not “colicky pain,” which is sharp and comes in waves. It has a slow and steady arc, and it’s usually dull but severe. It may bring you to the emergency room for relief. You may also notice that your upper right abdomen is tender to the touch. Biliary colic is often accompanied by nausea and vomiting. It’s also called a “gallbladder attack.”
Do gallstones cause other symptoms?
When a gallstone causes a persistent blockage or an infection, you’ll have symptoms of acute inflammation. This may include:
- Constant pain.
- Fever and chills.
- Heart rate accelerations.
You may also begin to show symptoms of bile accumulating in your bloodstream, such as:
- Jaundice.

- Sunken eyes.
- Dark-colored pee.
Diagnosis and Tests
How are gallstones diagnosed?
If you’re experiencing symptoms of biliary colic, your healthcare provider will investigate with blood tests and imaging tests. Blood tests can detect inflammation, infection or jaundice. They can also give your healthcare provider clues about which organs are being affected. Imaging tests will help locate the source of the blockage. They will usually start with an ultrasound.
What tests are used to diagnose cholelithiasis?
Ultrasound: An abdominal ultrasound is a simple and noninvasive test that requires no preparation or medication. It’s usually all that’s needed to locate gallstones. However, it doesn’t visualize the common bile duct very well. If your healthcare provider suspects there’s a gallstone hidden in there, they might need to use another type of imaging test to find it.
MRCP: Magnetic resonance cholangiopancreatography (MRCP) is a type of MRI that specifically visualizes the bile ducts. It’s non-invasive and creates very clear images of your biliary system, including the common bile duct. Your provider might use this test first to find a suspected gallstone there. But if they’re already pretty sure it’s there, they might skip it and go straight to an ERCP.
It’s non-invasive and creates very clear images of your biliary system, including the common bile duct. Your provider might use this test first to find a suspected gallstone there. But if they’re already pretty sure it’s there, they might skip it and go straight to an ERCP.
ERCP: ERCP stands for endoscopic retrograde cholangiopancreatography. This test is a little more invasive, but it’s a useful one for finding gallstones because it can also be used to remove them from the ducts if they are stuck there. It uses a combination of X-rays and endoscopy, which means passing a tiny camera on the end of a long tube down your throat and into your upper GI tract. (You’ll have medication to make this easier.)
When the camera (endoscope) reaches the top of your small intestine, your healthcare provider will slide another, smaller tube into the first one to reach farther down into your bile ducts. They will inject a special dye through the tube and then take video X-rays (fluoroscopy) as the dye travels through the ducts. They can insert tools through the tube to remove the stones they find.
They can insert tools through the tube to remove the stones they find.
_
_Endoscopic retrograde cholangiopancreatography (ERCP) can diagnose and sometimes treat gallstones.
Endoscopic ultrasound passes through the mouth to the common bile duct and gall bladder.
Management and Treatment
Incision locations for a laparoscopic cholecystectomy.Does cholelithiasis require surgery?
Most people with gallstones will never need treatment. But if your gallstones cause problems, your healthcare provider will want to remove them. Usually, they will want to remove all of your gallstones, even if only one of them is currently causing trouble. If a blockage happens once, it’s likely to happen again. The risk isn’t worth waiting around for.
Since there’s no way to access the gallstones inside your gallbladder without removing it, the standard treatment for problematic gallstones is to remove the gallbladder entirely. This is a minor surgery, and you can live well without a gallbladder. If you have gallstones in your bile ducts, your healthcare provider will have to remove those separately as well.
If you have gallstones in your bile ducts, your healthcare provider will have to remove those separately as well.
Can gallstones go away without surgery?
Gallstones in your bile ducts that aren’t stuck can successfully pass through them and into your intestines. You can pass them out through your poop. That's a lucky scenario, but in general, you don’t want to risk having gallstones in your bile ducts in the first place. If they don’t pass all the way out of you, they will only grow bigger over time.
There are some medications that can help to dissolve smaller gallstones. These take many months to work, so they aren’t the most practical option for people experiencing symptoms. But they offer an alternative for people who may not be in a safe health condition for surgery. They may also be practical for people who have gallstones but don’t have symptoms yet.
How are gallstones removed?
There are a few different ways to remove gallstones.
Endoscopy
Gallstones in your bile ducts are removed by endoscopy (ERCP). This doesn’t require any incisions. The gallstones come out through the long tube that’s been passed down your throat. Gallstones in your gallbladder are removed by removing the gallbladder (cholecystectomy). This can usually be done by laparoscopy, a minimally-invasive surgery technique.
This doesn’t require any incisions. The gallstones come out through the long tube that’s been passed down your throat. Gallstones in your gallbladder are removed by removing the gallbladder (cholecystectomy). This can usually be done by laparoscopy, a minimally-invasive surgery technique.
Laparoscopy
A laparoscopic cholecystectomy uses small, “keyhole incisions” in your abdomen to operate with the aid of a small camera called a laparoscope. Your surgeon inserts the laparoscope through one keyhole and removes your gallbladder through another. Smaller incisions make for less post-operative pain and a faster recovery time than conventional, “open” surgery.
Open surgery
Some people may have more complicated conditions that require open surgery to manage. If you have open surgery, you’ll have a longer hospital stay afterward and a longer recovery at home for your larger incision. Some laparoscopic cholecystectomies may need to convert to open surgery if your surgeon runs into complications during the procedure.
What are the complications or side effects of gallstone surgery?
After laparoscopic surgery, you may have some abdominal gas and gas pain. You can have this after ERCP too. Both methods pump gas into your organs to expand them and help them show up better in images. It will pass in a day or so. Complications during the operation are rare but include bleeding, infection, and injury to nearby organs.
How long is the recovery from gallstone surgery?
If you have a laparoscopic cholecystectomy, you can be home within 24 hours. You can recover in about two weeks. If you have open surgery, you’ll need to stay in the hospital for three to five days afterward. Your recovery at home will be six to eight weeks. Your digestive system may take two to eight weeks to adjust after the operation.
What happens when you don’t have a gallbladder anymore?
Your digestive system can still function without a gallbladder. Your gallbladder is mostly a holding place for the bile your liver makes. It delivers bile to your small intestine to help with digestion. When your surgeon removes your gallbladder, they’ll redirect your bile ducts so that bile can flow directly from your liver to your small intestine.
It delivers bile to your small intestine to help with digestion. When your surgeon removes your gallbladder, they’ll redirect your bile ducts so that bile can flow directly from your liver to your small intestine.
Will I need to change my diet after gallstone surgery?
Your digestive system may take some weeks to adjust to the lack of a gallbladder. Some people may experience temporary indigestion or diarrhea during the transition period. Your healthcare provider will advise you not to eat anything too rich or fatty while you recover. Most people can return to a normal (but reasonably healthy) diet after a few weeks.
Prevention
Can diet help to prevent gallstones?
You can reduce your risk of cholesterol gallstones, which are the most common type, by reducing cholesterol in your diet. Here are some quick tips:
- Limit fried and fast foods. These foods are usually fried in saturated fats, which promote LDL cholesterol (the “bad” type).
 If you cook with oil, choose plant oils instead of animal fats.
If you cook with oil, choose plant oils instead of animal fats. - Replace red meat with fish. Red meat is high in saturated fats, while fish is high in omega-3 fatty acids, which promote HDL cholesterol (the “good” type). The good type helps balance the bad type.
- Eat more plants. High-fiber fruits, vegetables and whole grains help to clear out excess cholesterol from your body. Eating more plants can also help you keep your overall weight down.
- Lose weight gradually. Dieting to lose weight can help reduce the cholesterol content in your blood. But it’s better to lose weight at a slow, steady pace of one to two pounds a week. Rapid weight loss can encourage gallstones.
Outlook / Prognosis
What is my prognosis if I have gallstones (cholelithiasis)?
If you have gallstones but they haven’t caused you any problems yet, they probably never will. About 2% of asymptomatic gallstones become symptomatic each year. Once they begin to cause symptoms, they are likely to keep doing so. About 2% of people with symptomatic gallstones develop complications each year, such as acute inflammation and infection.
Once they begin to cause symptoms, they are likely to keep doing so. About 2% of people with symptomatic gallstones develop complications each year, such as acute inflammation and infection.
Cholecystectomy is a definitive treatment for most gallstones, and most people recover quickly and completely from it. Some people may still have gallstones show up in their bile ducts again afterward. These can be treated by an endoscope. If you use medicine to dissolve your gallstones, this works about 75% of the time, but the gallstones will often come back again.
Living With
When should I seek care for gallstones?
If you experience anything like biliary colic, seek immediate attention. Biliary pain is dull and persistent, growing for about 20 minutes and lasting for one to several hours. It’s usually in the upper right quadrant of your abdomen, but sometimes it’s referred elsewhere. It’s often accompanied by nausea and vomiting, but vomiting doesn’t relieve it.
A note from Cleveland Clinic
Gallstones are common, and most people will never be bothered by them.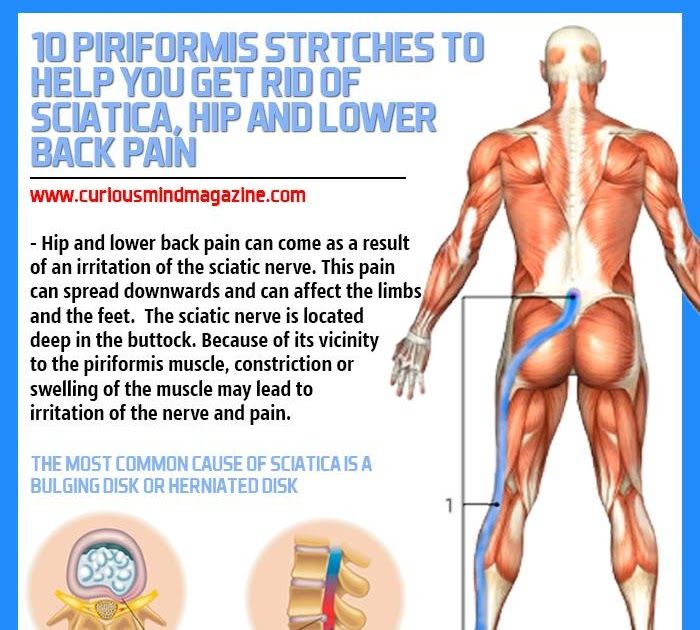 If they stay put in your gallbladder, you’ll probably never know they’re there. But once they begin to move, they become dangerous. These tiny, pebble-like pieces can do a lot of damage when they get into the tight spaces of your delicate biliary system.
If they stay put in your gallbladder, you’ll probably never know they’re there. But once they begin to move, they become dangerous. These tiny, pebble-like pieces can do a lot of damage when they get into the tight spaces of your delicate biliary system.
A gallbladder attack can be intense and scary, especially if you didn’t know you had gallstones to begin with. It may be alarming to find out that the recommended treatment is surgery. But laparoscopic gallbladder removal is a common procedure with an excellent prognosis. Your whole ordeal may be over within hours of your first symptoms.
Muscle spasm: description of the disease, causes, symptoms, cost of treatment in Moscow
Muscle spasm in the back is a contraction of muscle tissue in an involuntary manner and in an accelerated mode. A person during its occurrence experiences significant pain, which can completely deprive him of his ability to work for some time. According to the general sensations, the attack resembles a convulsive convulsion, reminiscent of a high-frequency discharge.
Spasm in the muscles of the back has its own scheme of formation: the occurrence of an electrical heating wave (nerve impulse) - an active effect on the muscle - muscle contraction in the absence of its relaxation - spasm. Its formation is easy to predict, because initially a person feels discomfort in the area of the shoulder blades, which rapidly or undulatingly develops into pain. The occurrence of excruciating compression is cyclical or once manifested discomfort.
Varieties of back pain with muscle spasm:
1. Tonic. Pathology arises from the professional activity of a person. Office workers (programmers, assistant secretaries, accountants, etc.) cannot refuse sedentary work due to the specifics of their profession. Tonic pains also sometimes occur in students and pupils. These seizures last for a short time.
2. Clonic. A sign by which they can be identified is frequent muscle twitching. The main reason for their occurrence is damage to the nervous system of an organic nature. Clonic back spasm is dangerous because it is able to provoke paralysis.
Clonic back spasm is dangerous because it is able to provoke paralysis.
3. Tonic-clonic. The voiced variety of pathology in most cases means that a person has a serious illness. It can be epilepsy, in which the attack of tonic-clonic spasm lasts a long time. The attack is fast and frightening. In a person, the back bends into an arc, and after the end of the attack it hurts for a long time.
Localization of backaches
At the place of their dislocation, the affected zones can be located in the following areas of the back:
1. Its upper part. Spasm of the back muscles in the thoracic region has different causes of formation. It is characterized by intense pain in the central zone of the back or in the shoulder blades.
2. Its lower part. Spasm of the back muscles in the lumbar region is often diagnosed by specialists. In everyday life, it is called sciatica and they are in no hurry to visit a specialist.
Causes of muscle spasms in the back, which often recur:
1. Problems with posture. In scoliosis, lordosis and kyphosis, spasms of the back muscles occur due to the fact that the tissues are tensed in order to straighten the curved part of the skeleton. The same process occurs during destruction in articular cartilage during osteochondrosis and intervertebral hernia.
Problems with posture. In scoliosis, lordosis and kyphosis, spasms of the back muscles occur due to the fact that the tissues are tensed in order to straighten the curved part of the skeleton. The same process occurs during destruction in articular cartilage during osteochondrosis and intervertebral hernia.
2. Pathological processes in the spinal cord. Such neurological diseases adversely affect nerve cells and contribute to the formation of inflammatory processes in muscle tissues. The scheme is repeated: the muscles tense up and provoke a spasm in the back.
3. Transferred shock. With the release of prolactin - the stress hormone - the nerve endings and muscles come into hypertonicity. The more often people get into critical situations, the more they are then disturbed by back spasms.
4. Serious injury. Injury to the spinal region causes significant pain to a person. An alarm signal enters the brain, and the body instantly activates all protective reserves. The result is a chain reaction. The tissues in the lesion are compressed in order to create a barrier against increased spasm, creating an additional load on the vessels and nerve endings. The result is a rapid increase in pain.
The result is a chain reaction. The tissues in the lesion are compressed in order to create a barrier against increased spasm, creating an additional load on the vessels and nerve endings. The result is a rapid increase in pain.
Separately, cases should be highlighted when spasm in the back occurs due to:
-
neurological and mental disorders;
-
pelvic bone problems;
-
dysfunction of internal organs.
Triggers causing one-time spasm:
-
performing heavy physical work during the day;
-
slight bruising without health consequences;
-
weakened muscles when loaded;
-
hypothermia without signs of frostbite;
-
sudden movements, turns or fast running.
Reasons for immediate medical attention:
1. The duration of the attack.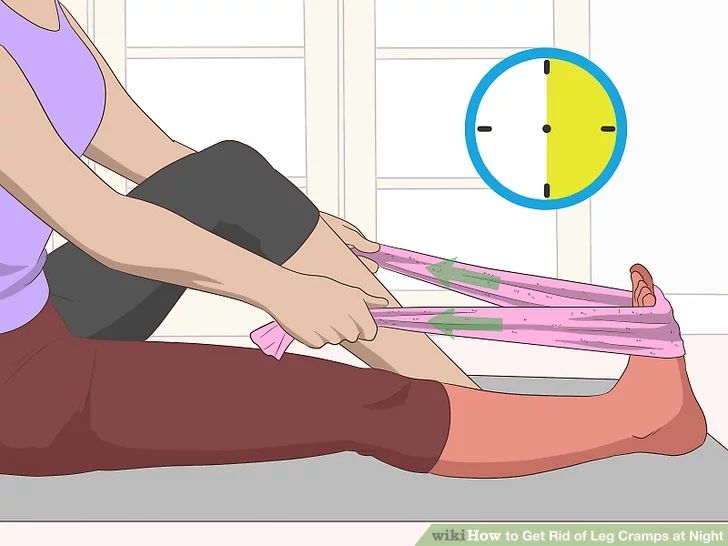 It should not last more than 2-3 days. Otherwise, we are talking about the inflammatory process in the body.
It should not last more than 2-3 days. Otherwise, we are talking about the inflammatory process in the body.
2. Intensity of spasm. An alarming sign is an increase in pain after taking analgesics and antispasmodics. An emergency call is the only help in this case.
3. Restriction in movements. Should alert the inability to move the legs and arms. Move your hand towards the glass on the table
4. The appearance of additional symptoms. These include severe weakness, nausea, and numbness of the extremities.
Disease diagnosis:
1. Donating blood for analysis. The specialist will need the results of the UAC and a decoding of its biochemical composition.
2. Fluorography. A standard procedure is necessary to detect pathologies of the chest organs.
3. MRI. Magnetic resonance imaging is needed for detailed monitoring of the state of the spinal column.
4. Electrocardiogram. Assign it in the presence of spasms in the thoracic region.
Prevention of sudden spasms in the back:
1. Regular stretching. It is important not to overdo it in your endeavors, so as not to damage the ligaments. For insurance, it is better to seek help from a specialist who will develop an individual complex for the patient.
2. Massage sessions. It is recommended to lightly stretch the chest, neck and shoulders when numbing the back. Regular massage by a professional will significantly increase the chances of preventing painful spasms.
3. Active lifestyle. It is not necessary to immediately pick up a barbell or make many hours of cross-country. It is enough to purchase a subscription to the swimming pool, take walks and do gymnastic exercises.
4. Change of work activity. With weakened muscles, it is forbidden to work as a loader, miner and builder. To perform tasks with the use of power loads, special training is needed.
5. Correct daily routine. You should correctly distribute your schedule by periods of work-rest. With physical exertion or sedentary work, you need to take a short break for a couple of minutes.
With physical exertion or sedentary work, you need to take a short break for a couple of minutes.
6. Rational menu. It is better to compile it with the help of a specialist in the presence of back problems. The uniform rules for the diet in this case are the inclusion of lean meat, dairy products, cereals, vegetables and fruits in the menu.
7. Tracking the water balance. With its lack of problems with dry skin, it will not work. To prevent muscle hypertonicity, you should drink at least two liters of fluid per day. Alcohol is prohibited.
8. Water aerobics. A visit to the swimming pool should be made as useful as possible. Water exercises are recommended even for pregnant women, so this method is absolutely safe for the back muscles.
9. Safety net during sedentary work. The back will not greatly disturb those people who let it warm up every half an hour. If it is impossible to leave the office, it is enough to walk around the working room.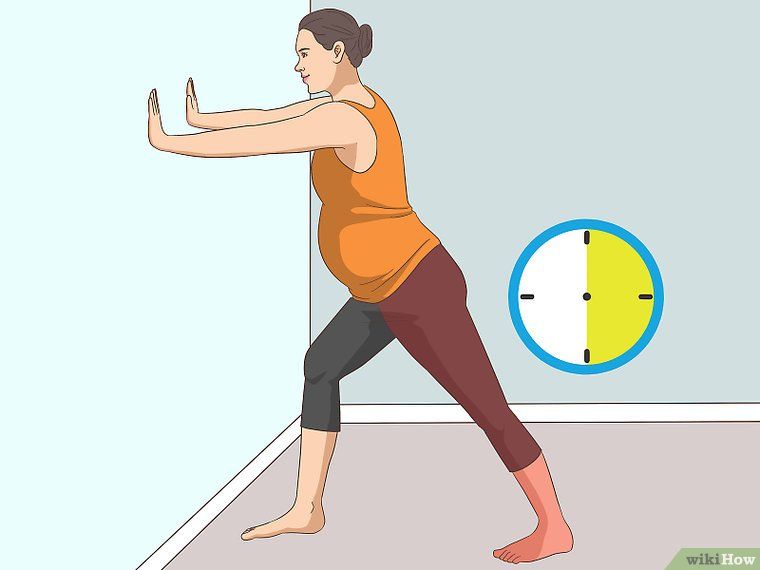 When moving, you should make rotational movements with your neck, shoulders and arms.
When moving, you should make rotational movements with your neck, shoulders and arms.
10. Proper layout of the recreation and work areas. Soft featherbed and voluminous pillows are the first enemies for the spine. At the first sign of pain in the back, you need to purchase an orthopedic mattress
Self first aid
If it is impossible to urgently visit a neurologist, you need to perform the following actions:
1. Lie down on the bed. Any hard surface without cavities will do. Ideally, you should use an orthopedic mattress.
2. Place your feet correctly. The lower limbs are placed on a small roller. In its absence, any flat and solid object can be used as a supporting base.
3. Take a pill. With a strong spasm, No-shpa, Spazmolgon will do, and during pain of moderate intensity, Diclofenac will come in handy.
4. Massage the problem area. If possible, it is recommended to treat it with a Kuznetsov applicator.
5. Put on a bandage. A corset will be needed for a person with a prolonged spasm if necessary to move around. With a tough work schedule, you can use a corset on a rigid basis.
Put on a bandage. A corset will be needed for a person with a prolonged spasm if necessary to move around. With a tough work schedule, you can use a corset on a rigid basis.
6. Use contrast compresses. They need to be changed every 15 minutes. You should monitor the reaction of the body during the procedure. For more relief from pain with a cold compress, it is recommended to opt for it.
7. Stick to bed rest. Its maximum duration is 3 days. Otherwise, there is a possibility of the formation of muscle atrophy.
Non-stop, if desired, to block back spasms
In case of recurrence of the disease with severe muscle spasms in the back, it is recommended:
1. Refusal of exercise therapy. The recommendation is limited to the period of recurrence of the disease. The vibrocouch is also contraindicated for the period of exacerbation of the pathology.
2. Turn on the brake light. With excessive body weight, it is impossible to independently control the plan for further treatment.
3. Refusal to plan pregnancy. In this case, the mechanism of Russian roulette starts. Without verification, there will be a reconciliation with the reaction of the body. Without consulting a gynecologist with serious back pain is indispensable.
How treatment methods work
Injections. With an injection, it is easier and faster to relieve severe pain. Of the analgesics, Baralgin is most often prescribed, but it is purchased by prescription. Amateurs are not recommended to administer the drug. It is better for the patient to seek medical help. You can replace Baralgin with Aspirin. At a low price and the ability to buy a medicine without a prescription, the remedy helps to eliminate the inflammatory process, lower body temperature and alleviate the human condition. In case of spasm, which Aspirin and Baralgin are not able to block, Dexamethasone and Prednisolone are prescribed. In a critical situation, blockade with Novocain is used.
Tablets. After consulting a doctor, tension in the back is removed with Mydocalm and Tizalud. With pain of moderate intensity, it is enough to take antispasmodics in the form of Spasmalgon. For the relief of more serious discomfort, Diclofenac and Ortofen are prescribed. This form of release of the drug can cause pain and cramps in the stomach. The way out of the situation is the use of painkillers along with Omeprazole or Omega.
After consulting a doctor, tension in the back is removed with Mydocalm and Tizalud. With pain of moderate intensity, it is enough to take antispasmodics in the form of Spasmalgon. For the relief of more serious discomfort, Diclofenac and Ortofen are prescribed. This form of release of the drug can cause pain and cramps in the stomach. The way out of the situation is the use of painkillers along with Omeprazole or Omega.
Ointments. It is not recommended to intensively treat an area with hypersensitivity with such a tool. With discomfort in the lumbar region, Radiculin is used (the second name is Valentin Dikul's gel). During spasms in the spine, which are given to the neck, Fastum-gel and Traumeel S will help.
Plasters. They do not have a strong effect, but they can alleviate the symptoms of the disease. Patch therapy involves the use of warming patches (pepper), orthopedic stickers (Zb Pain Relief) and plastic mass with anesthesia (Voltaren).
Muscle cramps - treatment, symptoms, causes, diagnosis
- Muscle cramps are involuntary and intense muscle contractions without a period of relaxation.

- Almost everyone has experienced a seizure episode at least once in their life.
- There are different types of seizures and different causes.
- Many different medications can cause muscle cramps.
- In most cases, muscle cramps can be stopped by relaxing (stretching) the muscle.
- Muscle cramps can often be prevented by measures such as a nutritious diet with sufficient micronutrients and adequate fluid intake.
Muscle cramps is an involuntary and violent contraction of a muscle without a period of relaxation. When muscles that can be controlled voluntarily, such as the muscles of the arms or legs, are used, they alternately contract and relax as certain movements are made in the limbs. The muscles that support the head, neck and torso work in synchrony and maintain the position of the body. A muscle (or even a few muscle fibers) can be involuntarily in a state of spasm. If the spasm is strong and persistent, then this leads to the appearance of convulsions. Muscle cramps are often visualized or palpated in the region of the muscle involved.
Muscle cramps are often visualized or palpated in the region of the muscle involved.
Muscle cramps can last from a few seconds to a quarter of an hour, and sometimes longer. It is also not uncommon for the seizures to recur until the muscle relaxes. The spasmodic contractions may involve part of a muscle, the entire muscle, or several muscles that usually contract at the same time when performing movements, such as flexing several fingers. In some cases, cramps can be simultaneously in the antagonist muscles responsible for movements in opposite directions. Muscle cramps are widespread. Almost all people (according to some studies about 95% of people) have experienced seizures at some point in their lives. Muscle cramps are common in adults and become more common with age, but cramps can still occur in children. In any muscle (skeletal) in which voluntary movements are performed, there may be cramps. Cramps of the limbs, legs and feet, and especially the calf muscle, are very common.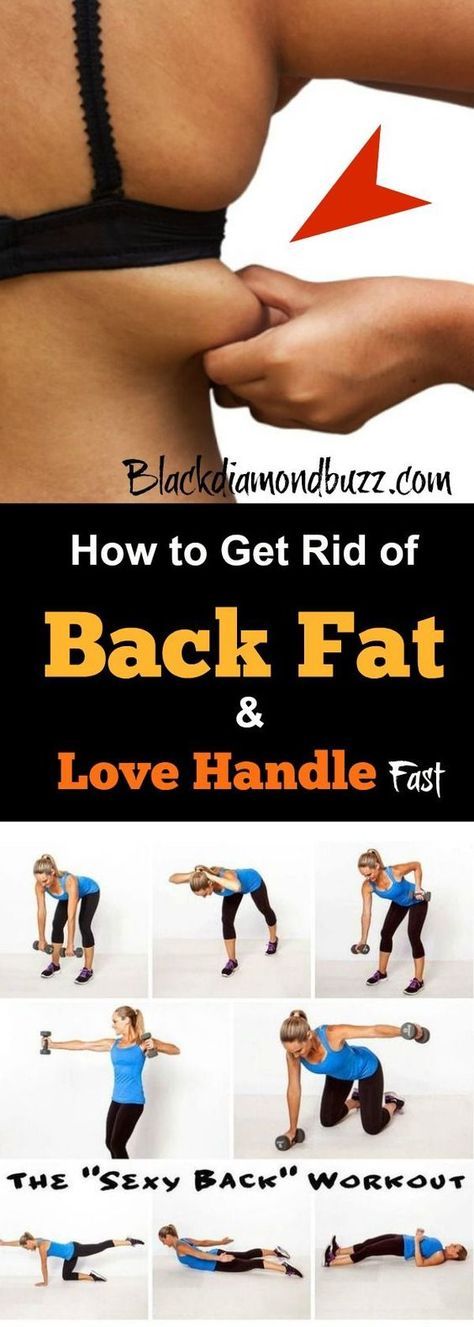
Types and causes of muscle cramps
Skeletal muscle cramps can be divided into four main types. These include "true" seizures, tetanic seizures, contractures, and dystonic seizures. Seizures are classified according to the causes of the seizures and the muscle groups they affect.
Types of muscle cramps
True cramps . True cramps involve part or all of a muscle or group of muscles that normally function together, such as the muscles involved in flexing several adjacent fingers. Most researchers agree that true cramps are caused by increased excitability of nerves that stimulate muscle contractions. They are overwhelmingly the most common type of skeletal muscle cramps. True seizures can occur in a variety of circumstances.
Injuries : Persistent muscle spasms may occur as a defense mechanism after an injury such as a broken bone. In this case, as a rule, spasm allows you to minimize movement and stabilize the area of injury. Injury to just the muscle can also lead to muscle spasm.
Injury to just the muscle can also lead to muscle spasm.
Vigorous activity: true cramps are usually associated with active muscle loading and muscle fatigue (during sports or unusual activities). Such convulsions can occur both during the activity and after, sometimes many hours later. In addition, muscle fatigue from sitting or lying down for a long period of time in an awkward position or any repetitive movement can also cause cramps. Older people are more at risk of seizures during vigorous or strenuous physical activity.
Rest seizures : Rest seizures are very common, especially in the elderly, but can occur at any age, including childhood. Rest spasms often occur at night. Night cramps, while not life threatening, can be painful, disrupt sleep, and may recur frequently (i.e., many times a night and/or many nights a week). The actual cause of nighttime cramps is unknown. Sometimes these cramps are initiated by a movement that contracts the muscles. An example would be stretching the foot in bed, which shortens the calf muscle, where cramps are most common.
An example would be stretching the foot in bed, which shortens the calf muscle, where cramps are most common.
Dehydration : Sports and other strenuous exercise may cause excessive fluid loss through sweat. With this type of dehydration, the likelihood of true seizures increases. These cramps most often occur in warm weather and may be an early sign of heat stroke. Chronic dehydration due to diuretics and poor fluid intake can similarly lead to seizures, especially in the elderly. Seizures can also be associated with a lack of sodium.
Redistribution of fluids in the body: true convulsions can also be noted in conditions where there is an unusual distribution of fluid in the body. An example is cirrhosis of the liver, in which there is an accumulation of fluid in the abdominal cavity (ascites). Similarly, seizures are a relatively common complication of the rapid changes in body fluids that occur during dialysis for kidney failure.
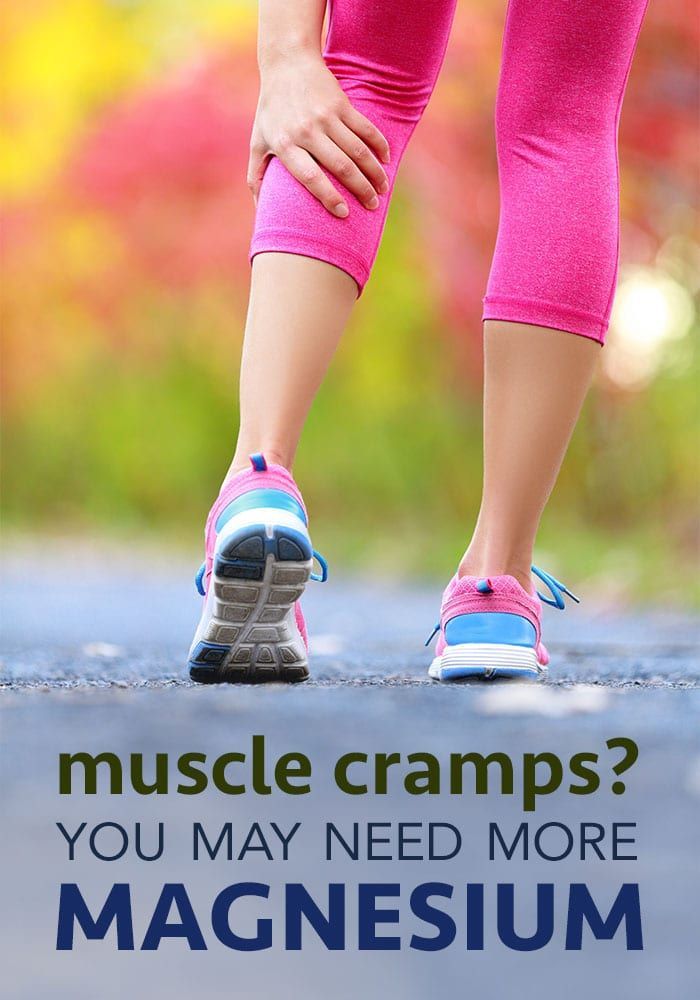
Low levels of electrolytes in the blood (calcium, magnesium): low blood levels of calcium or magnesium directly increase the excitability of the nerve endings innervating the muscles. This may be a predisposing factor for the spontaneous true seizures that many older people experience, and these seizures are also common in pregnant women. Low levels of calcium and magnesium are common in pregnant women, especially if these minerals are not getting enough from the diet. Seizures occur in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, insufficient absorption of calcium due to vitamin D deficiency, reduced parathyroid function.
This may be a predisposing factor for the spontaneous true seizures that many older people experience, and these seizures are also common in pregnant women. Low levels of calcium and magnesium are common in pregnant women, especially if these minerals are not getting enough from the diet. Seizures occur in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, insufficient absorption of calcium due to vitamin D deficiency, reduced parathyroid function.
Low potassium levels: Low blood potassium levels sometimes cause muscle cramps, although muscle weakness is more common in hypokalemia.
Tetany
Tetany activates all nerve cells in the body, which then stimulate muscle contraction. In this type, convulsive contractions occur throughout the body. The name tetany comes from the spasms that occur when tetanus toxin affects the nerves. However, this name for this type of cramp is now widely used to refer to muscle cramps in other conditions, such as low blood levels of calcium and magnesium. Low levels of calcium and magnesium increase the activity of the nervous tissue non-specifically, which can lead to the appearance of tetanic seizures. Often these seizures are accompanied by signs of hyperactivity of other nerve functions in addition to muscle hyperstimulation. For example, low blood calcium not only causes muscle spasm in the hands and wrists, but it can also cause numbness and tingling sensations around the mouth and other areas of the body.
However, this name for this type of cramp is now widely used to refer to muscle cramps in other conditions, such as low blood levels of calcium and magnesium. Low levels of calcium and magnesium increase the activity of the nervous tissue non-specifically, which can lead to the appearance of tetanic seizures. Often these seizures are accompanied by signs of hyperactivity of other nerve functions in addition to muscle hyperstimulation. For example, low blood calcium not only causes muscle spasm in the hands and wrists, but it can also cause numbness and tingling sensations around the mouth and other areas of the body.
Sometimes, tetanic convulsions are indistinguishable from true convulsions. Additional changes in sensation or other nerve function may not be noticeable, as the pain of a cramp may mask other symptoms.
Contractures
Contractures occur when muscles cannot relax for an even longer period than with the main types of muscle cramps.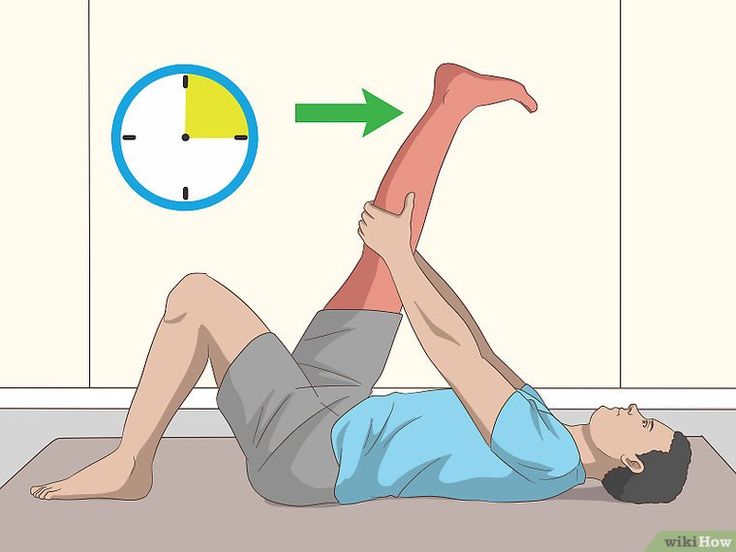 Constant spasms are caused by the depletion of adenosine triphosphate (ATP) - the energy intracellular substrate of the cell. This prevents relaxation of the muscle fibers. The nerves are inactive in this type of muscle cramp.
Constant spasms are caused by the depletion of adenosine triphosphate (ATP) - the energy intracellular substrate of the cell. This prevents relaxation of the muscle fibers. The nerves are inactive in this type of muscle cramp.
Contracture may be the result of genetic inheritance (eg, McArdle disease, which is a defect in the breakdown of glycogen to sugar in muscle cells) or acquired conditions (eg, hyperthyroid myopathy, which is a muscle disease associated with an overactive thyroid gland) . Convulsions of the type of contractures are rare.
Dystonic seizures
The last category of seizures are dystonic seizures, in which muscles not involved in the intended movement are affected and contracted. Muscles that are involved in this type of cramp include antagonistic muscles that usually work in the opposite direction of the intended movement and/or others that enhance the movement. Some dystonic spasms usually affect small muscle groups (eyelids, cheeks, neck, larynx, etc.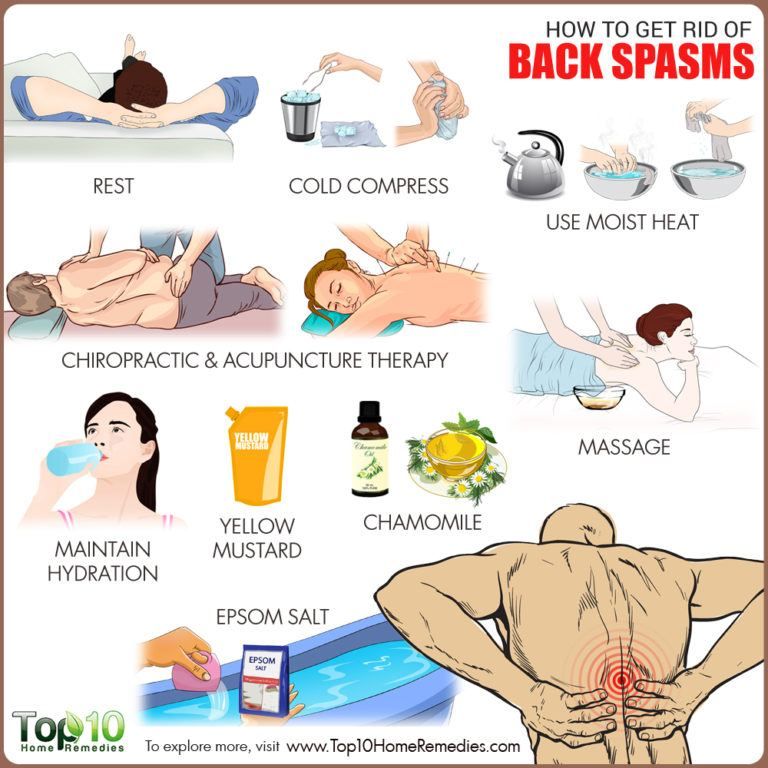 ). The arms and hands may be affected during repetitive movements such as writing (writer's cramp), playing a musical instrument. These activities can also lead to true cramps due to muscle fatigue. Dystonic seizures are not as common as true seizures.
). The arms and hands may be affected during repetitive movements such as writing (writer's cramp), playing a musical instrument. These activities can also lead to true cramps due to muscle fatigue. Dystonic seizures are not as common as true seizures.
Other types of convulsions
Some convulsions are caused by a number of nervous and muscular diseases. For example, these are diseases such as amyotrophic lateral sclerosis (Lou Gehrig's disease), accompanied by muscle weakness and atrophy; radiculopathy in degenerative diseases of the spine (hernia, disc protrusion, osteophytes), when root compression is accompanied by pain, impaired sensitivity and sometimes convulsions. Seizures can also occur with peripheral nerve damage, such as diabetic neuropathy.
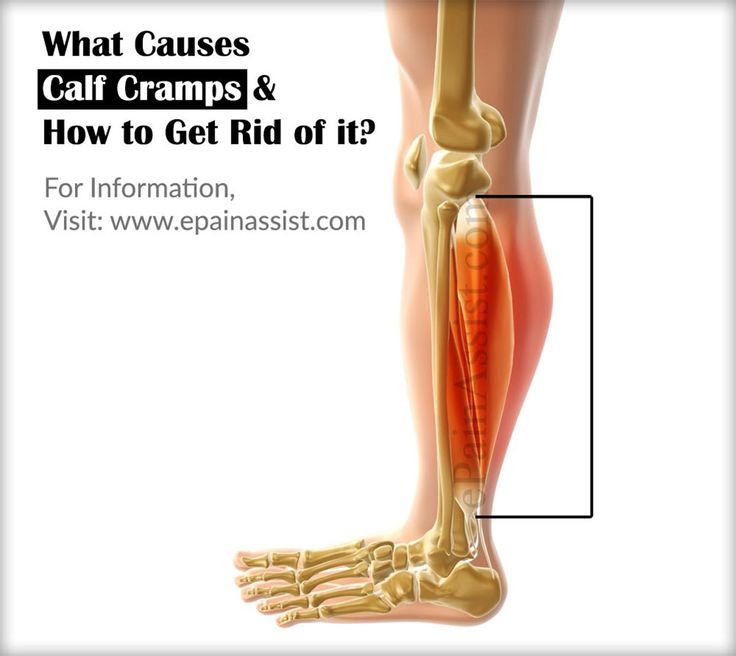
Crumpy . This type of cramps, as a rule, describes cramps in the calf muscle, and associate their appearance with muscle overstrain and the presence of degenerative changes in the spine (osteochondrosis of the lumbar spine, lumbar ischialgia). In addition, cramps are possible with disorders of the vascular circulation in the lower extremities (with obliterating endarteritis or post-thrombophlebitic syndrome). Also, various biochemical disorders in the triceps muscle of the leg can be the cause of cramps.
In addition, cramps are possible with disorders of the vascular circulation in the lower extremities (with obliterating endarteritis or post-thrombophlebitic syndrome). Also, various biochemical disorders in the triceps muscle of the leg can be the cause of cramps.
Many medicines can cause seizures. Strong diuretics such as furosemide or vigorous fluid removal from the body, even with less potent diuretics, can induce seizures as dehydration and sodium loss occur. At the same time, diuretics often cause loss of potassium, calcium and magnesium, which can also cause seizures.
Medicines such as donepezil (Aricept, which is used to treat Alzheimer's disease) and neostigmine (Prostigmine, used for myasthenia gravis), asraloxifene (Evista) is used to prevent osteoporosis in postmenopausal women - may cause seizures. Tolcapone (Tasmar), which is used to treat Parkinson's disease, has been shown to cause muscle cramps in at least 10% of patients. True seizures have been reported with nifedipine and the drugs Terbutaline (Brethine) and albuterol (Proventil, Ventolin). Some medicines used to lower cholesterol, such as lovastatin (Mevacor), can also cause seizures.
Some medicines used to lower cholesterol, such as lovastatin (Mevacor), can also cause seizures.
Seizures are sometimes observed in addicts during cessation of sedatives.
Lack of certain vitamins can also lead directly or indirectly to muscle cramps. These include deficiencies in thiamine (B1), pantothenic acid (B5), and pyridoxine (B6). The exact role of deficiency of these vitamins in causing seizures is unknown.
Poor circulation in the legs leads to a lack of oxygen in the muscle tissue and can cause severe muscle pain (intermittent claudication) that occurs when walking. It usually occurs in the calf muscles. But the pain in vascular disorders in such cases is not caused by the muscle cramp itself. This pain may be more related to the buildup of lactic acid and other chemicals in muscle tissue. Cramps in the calf muscles can also be associated with a violation of the outflow of blood in varicose veins and, as a rule, cramps in the calf muscles occur at night.
Symptoms and diagnosis of muscle cramps
Characteristically, a cramp is often quite painful. As a rule, the patient has to stop activities and urgently take measures to relieve seizures; the person is unable to use the affected muscle during the seizure. Severe cramps may be accompanied by soreness and swelling, which can sometimes persist for up to several days after the cramp has subsided. At the time of the cramp, the affected muscles will bulge, feel hard and tender to the touch.
Diagnosis of seizures is usually not difficult, but finding out the causes may require both a thorough history of the disease and instrumental and laboratory examinations.
Treatment
Most seizures can be interrupted by stretching the muscle. For many leg and foot cramps, this stretch can often be achieved by standing up and walking. With cramps in the calf muscles, it is possible to bend the ankle with the help of the hand, while lying in bed with the leg extended straight. In writing spasm, pressing the hand against the wall with the fingers down will stretch the flexors of the fingers.
In writing spasm, pressing the hand against the wall with the fingers down will stretch the flexors of the fingers.
Gentle muscle massage can also be done to help relax a cramped muscle. If the cramp is associated with fluid loss, as is often the case with strenuous exercise, rehydration and restoration of electrolyte levels is necessary.
Muscle relaxants may be used in the short term in certain situations to allow muscles to relax during injury or other conditions (eg, radiculopathy). These drugs include cyclobenzaprine (Flexeril), orphenadrine (NORFLEX), and baclofen (Lioresal).
In recent years, injections of therapeutic doses of botulinum toxin (Botox) have been successfully used for certain dystonic muscle disorders that are localized to a limited muscle group. A good response may last several months or more, and injections may be repeated.
Treatment of seizures that are associated with specific diseases, usually focuses on the treatment of the underlying disease.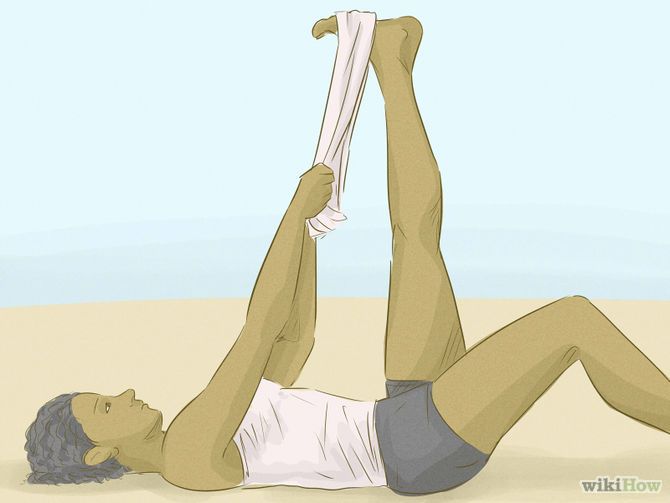
In cases where seizures are severe, frequent, prolonged, difficult to treat, or not associated with an obvious cause, then in such cases, both additional examination and more intensive treatment are required.
Prevention of seizures
Adequate nutrition with sufficient fluids and electrolytes is essential to prevent possible seizures, especially during strenuous exercise or during pregnancy.
Night cramps and other rest cramps can often be prevented with regular stretching exercises, especially if performed before bed.
Magnesium and calcium supplements are also a good way to prevent seizures, but caution is required when prescribing them in the presence of renal insufficiency. In the presence of hypovitaminosis, it is necessary to take vitamins of group B, vitamin D, E.
If the patient is taking diuretics, it is necessary to take potassium supplements.
Recently, the only drug that is widely used for the prevention, and sometimes for the treatment of seizures, is quinine.