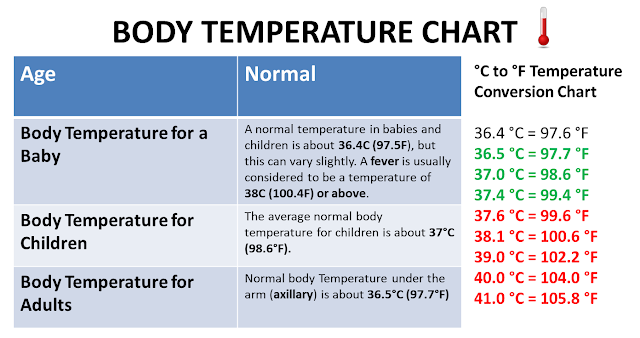
Fever for a baby under arm
How to Take a Temperature (0-12 Months)
When Does Your Baby Have a Fever??
- Rectal, Forehead or Ear temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
Where to Take the Temperature
- Rectal temps are the most accurate. Forehead temps are the next most accurate. Ear temps are also accurate if done properly. Temps done in the armpit are the least accurate. Armpit temps are useful for screening at any age.
- Age under 3 months old (90 days old). An armpit temp is the safest and is good for screening. If the armpit temp is above 99° F (37.2° C), re-check it. Use a rectal reading. Reason: If young babies have a fever, they need to see a doctor now. New research shows that forehead temps may also be accurate under 3 months of age.
- Age 3 months to 1 year old. Rectal or forehead temps are accurate.
An ear thermometer can be used after 6 months old. An armpit temp is good for screening if it is taken right.
- Digital (electronic) thermometers are easily found in stores. They do not cost very much. They can be used for rectal and armpit temps. Most of them give an accurate temp in 10 seconds or less. The AAP suggests you replace any glass thermometer in the house with one of these products.
Rectal Temperature: How to Take
- Age: Birth to 1 year old
- Have your child lie stomach down on your lap. Another way is on the back with the legs pulled up to the chest.
- Put some petroleum jelly on the end of the thermometer and the anus.
- Slide the thermometer gently into the anus no more than 1 inch. If your child is less than 6 months old, put it in no more than ½ inch. That means until you can no longer see the silver tip.
- Be gentle. There should not be any resistance. If there is, stop.
- Hold your child still. Leave a digital thermometer in until it beeps (about 10 seconds).
- Your child has a fever if the rectal temp is above 100.4° F (38° C).
- Warning: do not take rectal temperatures in young children with leukemia or other cancers. Also avoid in other children with weak immune systems such as organ transplant, HIV or sickle cell disease.
Armpit Temperature: How to Take
- Age: Any age for screening
- Put the tip of the thermometer in an armpit. Make sure the armpit is dry.
- Close the armpit by holding the elbow against the chest. Do this until it beeps (about 10 seconds). The tip of the thermometer must stay covered by skin.
- Your child has a fever if the armpit temp is above 99.0° F (37.2° C). If you have any doubt, take your child's temp by rectum or forehead.
Digital Pacifier Temperature: How to Take
- Age: Birth to 1 year. Only good for screening. Requires the baby to suck on it, which is not always possible.
- Have your child suck on the pacifier until it beeps (about 10 seconds).

- Your child has a fever if the pacifier temp is above 100° F (37.8° C).
Ear Temperature: How to Take
- Age: 6 months and older (not accurate before 6 months)
- This thermometer reads the heat waves coming off the eardrum.
- A correct temp depends on pulling the ear backward. Pull back and up if over 1 year old.
- Then aim the tip of the ear probe between the opposite eye and ear.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution. Being outdoors on a cold day will cause a low reading. Your child needs to be inside for 15 minutes before taking the temp. Earwax, ear infections and ear tubes do not keep from getting correct readings.
Forehead (Temporal Artery) Temperature: How to Take
- Age: Any age
- This thermometer reads the heat waves coming off the temporal artery. This blood vessel runs across the forehead just below the skin.

- Place the sensor head at the center of the forehead.
- Slowly slide the thermometer across the forehead toward the top of the ear. Keep it in contact with the skin.
- Stop when you reach the hairline.
- Read your child's temp on the display screen.
- Note: some newer forehead thermometers don't need to slide across the forehead. Follow the box directions on how to take the temp.
- Used in more doctor's offices than any other thermometer.
- Parents like this thermometer because it takes less than 2 seconds. It also does not need the child to cooperate. It does not cause any discomfort.
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Last Reviewed: 12/04/2022
Last Revised: 03/17/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Fever and temperature taking | Caring for kids
When your child is sick with an infection (viral or bacterial), it is common to also have a fever. Fever will not hurt your child. Usually, it goes away after 72 hours (3 days).
Babies younger than 6 months old should see a doctor when they have a fever. Babies younger than 3 months old should be seen urgently.
Older children can be treated at home, as long as they get enough liquids and seem well otherwise. However, they should see a doctor if their fever lasts for more than 48-72 hours.
There are several methods for taking your child’s temperature:
- rectal (by the rectum or ‘bum’)
- oral (by the mouth)
- axillary (under the armpit)
- tympanic (in the ear)
- temporal artery (forehead)
Which method should I use?
The right method depends on your child’s age. It’s important that the measurement is accurate.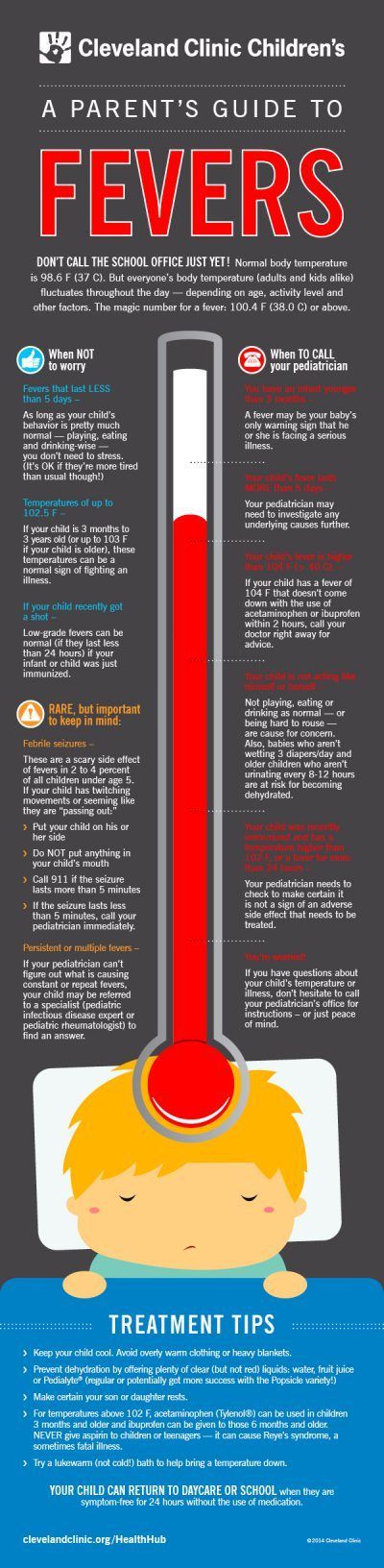 The most accurate measurement by age is shown below. However, some parents or caregivers will first check for fever using an alternative method. Use this chart to help you decide which method to use:
The most accurate measurement by age is shown below. However, some parents or caregivers will first check for fever using an alternative method. Use this chart to help you decide which method to use:
| Age | Recommended method |
|---|---|
| Birth to 2 years | Most accurate: Rectum Alternative: Armpit |
| Between 2 and 5 years | Most accurate: Rectum Alternative: Ear, armpit |
| Older than 5 years | Most accurate: Mouth Alternative: Ear, armpit |
Temperature-taking tips
- Do not use a mercury thermometer. If it breaks, you could be exposed to the toxic substance.
- A digital thermometer can be used for both rectal and oral temperature taking. It’s made of unbreakable plastic, is easy to read, easy to clean, and measures temperature quickly.

- Do not use the same thermometer for rectal and oral temperature taking.
- A non-contact infrared thermometer can display a reading quickly and reduce the risk of spreading disease. But head coverings, sweat, environment (direct sunlight, humidity, cold air, etc.), and positioning on forehead may influence the measurement.
- Fever strips are not recommended because they do not give accurate readings.
- Touching your child's skin (e.g., forehead) is not a reliable way to check for fever. If you suspect a fever, confirm it by using one of the methods above.
To get an accurate reading of your child’s temperature, you will need to make sure it’s done right. Here’s how:
Rectum
This is the most reliable way to measure body temperature. Only use a rectal thermometer if you are comfortable doing so and if a health care provider has shown you how to do it safely.
- Clean the thermometer with cool, soapy water and rinse.
- Cover the silver tip with petroleum jelly (such as Vaseline).
- Place your baby on their back with their knees bent.
- Gently insert the thermometer in the rectum, about 2.5 cm (1 inch), holding it in place with your fingers.
- When ready, remove the thermometer and read the temperature.
- Clean the thermometer.
Mouth
The oral method is not recommended for children younger than 5 years old because it is hard for them to hold the thermometer under their tongue for long enough.
- Clean the thermometer with cool, soapy water and rinse.
- Carefully place the tip of the thermometer under your child’s tongue.
- With your child’s mouth closed, leave the thermometer in place for about 1 minute, until you hear the beep.
- Remove the thermometer and read the temperature.
- Clean the thermometer.
Armpit
The armpit (axillary) method is usually used to check for fever in newborns and young children, but it’s not as accurate as a rectal temperature. If an axillary temperature does not show a fever but your child feels warm and seems unwell, take a rectal measurement.
If an axillary temperature does not show a fever but your child feels warm and seems unwell, take a rectal measurement.
- Use a rectal or oral thermometer.
- Clean the thermometer with cool, soapy water and rinse.
- Place the tip of the thermometer in the centre of your child’s armpit.
- Make sure your child’s arm is tucked snugly against their body.
- When ready, remove the thermometer and read the temperature.
- Clean the thermometer.
Ear
Though quick to use, the ear (tympanic) method can give temperature readings that are too low, even when the manufacturer’s directions are followed. It is not as reliable or accurate as rectal temperature taking. If a tympanic temperature does not show a fever but your child feels warm and seems unwell, take a rectal measurement.
- Use a clean probe tip each time, and follow the manufacturer’s instructions carefully.
- Gently tug on the ear, pulling it back. This will help straighten the ear canal, and make a clear path inside the ear to the eardrum.
- Gently insert the thermometer until the ear canal is fully sealed off.
- When ready, remove the thermometer and read the temperature.
What is a normal temperature?
The following chart lists normal temperatures. The range varies and depends on the way you took your child’s temperature. Any temperature above this range is considered a fever.
| Method | Normal temperature range |
|---|---|
| Rectum | 36.6°C to 37.9°C (97.9°F to 100.2°F) |
| Mouth | 35.5°C to 37.5°C (95.9°F to 99.5°F) |
| Armpit | 36.5°C to 37.5°C (97.8°F to 99.5°F) |
| Ear | 35.8°C to 37.9°C (96.4°F to 100.2°F) |
The degree (height) of a fever does not tell you how serious your child’s illness is—how your child looks and acts is usually a better sign. A child with a mild infection can have a high fever, while a child with a severe infection might have no fever at all.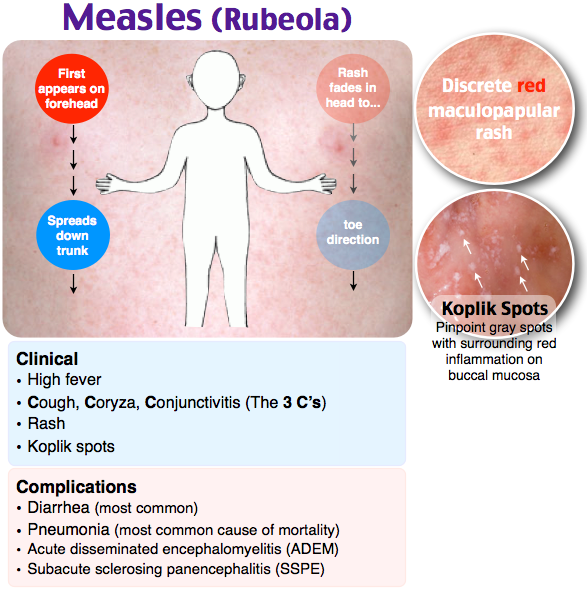
What can I do if my child has a fever?
- Keep your child comfortable, and offer plenty of fluids.
- Remove extra blankets and clothing so heat can leave their body and help lower the body temperature. But don’t take off all your child’s clothes because they may become too cold and start shivering, which makes more body heat and will cause their temperature to rise again.
What about medications?
Medications are not always needed to reduce a child’s temperature. They can be used to relieve any aches and pains, and to make your child more comfortable.
Medications such as acetaminophen (Tylenol or Tempra) and ibuprofen (Advil or Motrin) do not treat the underlying cause of the fever but can help temporarily lower a temperature. Sometimes a fever continues even after giving medication. That’s ok.
Unless your doctor says otherwise, you can give the dose recommended on the medication package. The correct dose should be based on your child’s body weight. Never exceed the recommended dose.
Ibuprofen should only be given if your child is drinking reasonably well. Do not give ibuprofen to babies under 6 months without first talking to your doctor or health care provider.
Acetaminophen and ibuprofen have different doses and different lengths of time between doses. They are safe to take at the same time, but because the dose and time are different, it is important to keep track when using both for your child.
Do not use aspirin [acetylsalicylic acid (ASA)] to treat a child’s fever. If the fever is due to chickenpox, influenza or certain other viral infections, taking aspirin can increase the risk of Reye’s syndrome. This is a very serious condition that can damage the liver and brain.
Contact your health care provider if your child
- has a fever and is less than 6 months old.
- has a fever for more than 48-72 hours.
- is excessively cranky, fussy or irritable.

- is excessively sleepy, lethargic or does not respond.
- is persistently wheezing or coughing.
- has a fever combined with a rash or any other signs of illness that worry you.
More information from the CPS
Additional resources
Reviewed by the following CPS committees
- Community Paediatrics Committee
Last updated: June 2022
Mouse fever (Hemorrhagic fever) in children and adults: symptoms, signs, treatment
Hemorrhagic fever with renal syndrome (the second name is mouse fever) is a disease of the infectious group, often associated with the beginning of the summer season and agricultural work. Every year, about 7,000 cases of infection are recorded in the country, which makes itself felt with characteristic symptoms - a hemorrhagic rash, vascular damage, malfunctioning of the kidneys and a general deterioration in a person's condition. In the absence of timely assistance, the disease can cause serious complications and death. Only timely seeking medical help will help preserve the health of the patient and return him to normal life.
In the absence of timely assistance, the disease can cause serious complications and death. Only timely seeking medical help will help preserve the health of the patient and return him to normal life.
Causes of mouse fever
For a long time, the beginning of the summer season was marked by a sharp increase in patients who went to the doctor with the same symptoms - impaired excretory function, skin rashes, changes in blood composition, weakness and malaise. Detailed studies have identified the culprits who are carriers of a dangerous infection.
These are rodents, in the body of which there is a sufficient amount of pathogenic microflora. Together with secretions, it enters the soil and on the skin of a person during summer work, digging the soil, outdoor recreation and sports. Through dirty hands, pathogens enter the body, penetrate the respiratory system and blood vessels, causing the appearance of characteristic symptoms. Most of the sick are lovers of summer holidays and employees of agricultural enterprises involved in planting plants and harvesting in the fields and gardens.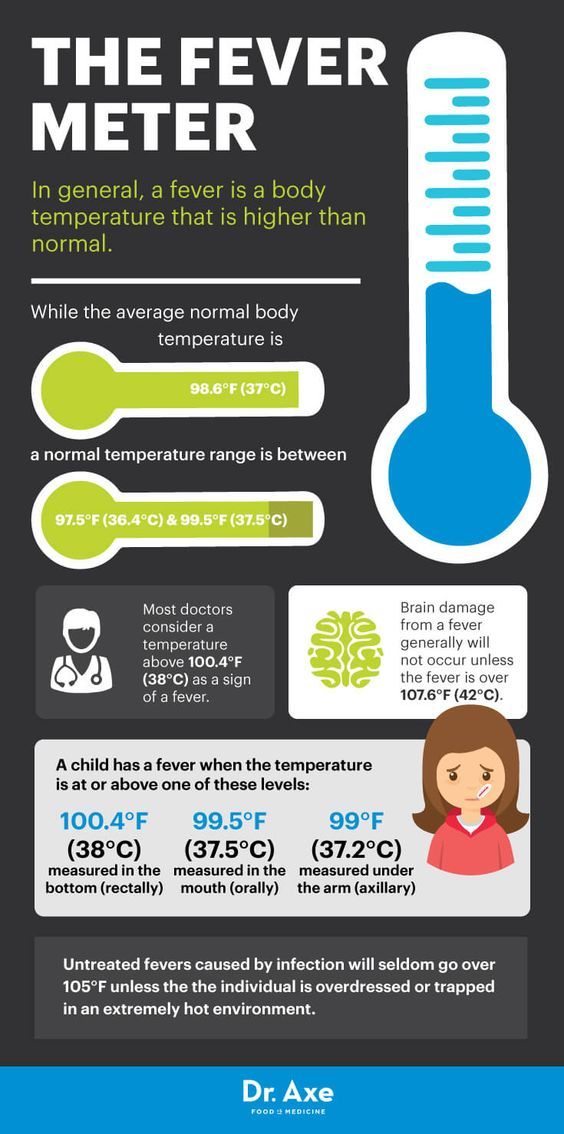
A significant part of the rodents that are carriers of hemorrhagic fever infection move through fields, broad-leaved forests, garden plots, abandoned agricultural land, auxiliary buildings, etc. With the onset of cold weather, they tend to penetrate into houses, where they continue to actively breed. Their waste products remain on the surfaces of the floor and walls, tables and shelves, which significantly increases the risk of infection during cleaning and tidying up.
Routes of infection include:
- airborne - inhalation of dust containing small particles of excrement;
- alimentary - consumption of water contaminated by rodents;
- contact - in contact with human skin of the remains of waste products and contaminated soil.
Cases of transmission of the disease from an infected person to healthy people have not been registered.
Mouse Fever Symptoms
The disease manifests itself in several stages:
In the initial stage, which takes about 3 days, the first signs of mouse fever resemble the flu or an acute viral infection.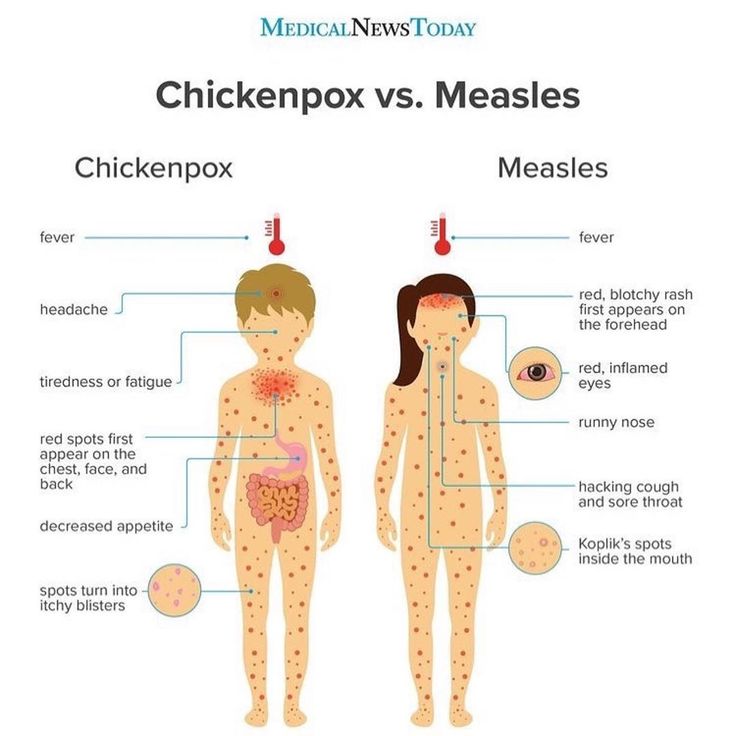 There is an increase in temperature, aches and pain in the muscles, chills and weakness, thirst, a decrease in pressure and a slowing of the pulse. Many patients complain of inflammation of the mucous membrane of the eyes, conjunctivitis, and a rash.
There is an increase in temperature, aches and pain in the muscles, chills and weakness, thirst, a decrease in pressure and a slowing of the pulse. Many patients complain of inflammation of the mucous membrane of the eyes, conjunctivitis, and a rash.
At the next stage, the patient has nausea and vomiting, swelling of the face and body, bloating of the abdominal cavity, back pain in the lumbar region. The duration of this period is about 10-11 days. In the absence of medical attention, with symptoms of mouse fever, there is a risk of internal bleeding with subsequent death.
Thanks to timely medical care, the patient's recovery takes about one to one and a half months. Complete disposal of the body from the pathogen and symptoms of mouse fever in men and women is observed after 4-6 months.
Consequences of mouse fever
The presence in the body of complex diseases of internal organs, the general depressed state of the immune system and the rapid development of the disease against the background of the lack of timely medical care can cause the development of the following pathologies:
- pancreatitis;
- myocarditis;
- sepsis;
- edematous phenomena in the lungs;
- meningitis, cerebral hemorrhage;
- renal failure.
The combination of the listed consequences of mouse fever contributes to the rapid deterioration of the patient's condition and can lead to irreversible consequences in the body.
Diagnostic methods
Some signs of an infectious disease can be detected at the stage of visual examination and history taking. Confirm the doctor's assumptions allow the analysis of PCR (polymerase chain reaction) enzyme immunoassay, showing the presence of antibodies to the pathogen in the blood. Radiography, ultrasound diagnostics and urinalysis allow to clarify the state of internal organs.
How to treat?
Putting off going to the doctor, hoping for the results of folk methods, is a serious risk. The result of such a decision can be a significant deterioration in the patient's condition up to the failure of internal organs, extensive internal bleeding and death. Moreover, the medical institution will offer comprehensive treatment aimed at eliminating the symptoms and causes of the pathology:
- intravenous injections of ribavirin;
- the introduction of saline and glucose solution to restore the basic functions and nutrition of the body;
- a course of multivitamin preparations;
- blood transfusion, excluding the consequences of its infection with a pathogen.
A therapeutic diet with the complete exclusion of spicy and spicy foods, alcohol, vinegar and seasonings can speed up recovery.
Ways to Prevent Infection with Mouse Fever
You can avoid infection by following these guidelines:
- regular cleaning of the premises of a country house and an agricultural enterprise using automatic equipment and disinfectants;
- protection of the skin of the hands and respiratory tract when cleaning or working with open ground;
- destruction of products spoiled by rodents;
- sealing joints and seams through which uninvited vectors of infection can enter the room;
- storage of foodstuffs in hermetically sealed containers;
- thorough heat treatment of food before eating.
Other recommendations for infection prevention can be obtained from the attending physician who supervises the treatment of murine fever.
Diagnosis and treatment of mouse fever in Moscow
The qualified staff of the clinic of JSC "Medicina" in the Central Administrative District of Moscow invites patients with the first signs of the disease for an initial consultation, diagnosis and treatment of mouse fever. All the necessary examinations and procedures can be done at the medical center, equipped with advanced equipment from leading world manufacturers. Each patient is guaranteed an attentive attitude, careful development of an individual treatment course, control of specialists and confidentiality of personal information. You can make an appointment on the clinic's website or by calling the indicated numbers in Moscow.
All the necessary examinations and procedures can be done at the medical center, equipped with advanced equipment from leading world manufacturers. Each patient is guaranteed an attentive attitude, careful development of an individual treatment course, control of specialists and confidentiality of personal information. You can make an appointment on the clinic's website or by calling the indicated numbers in Moscow.
Questions and answers
What is mouse fever?
Mouse fever is the second name for hemorrhagic fever with renal syndrome. This is a human infectious disease that occurs after contact with the waste products of rodents that are carriers of the virus. Direct contact, drinking contaminated water or inhaling the smallest particles of excrement during field or country work often cause infection to enter the body and cause dangerous symptoms of infection.
How do you get mouse fever?
Most of the reported cases are the consequences of being in nature or country work in violation of personal hygiene requirements.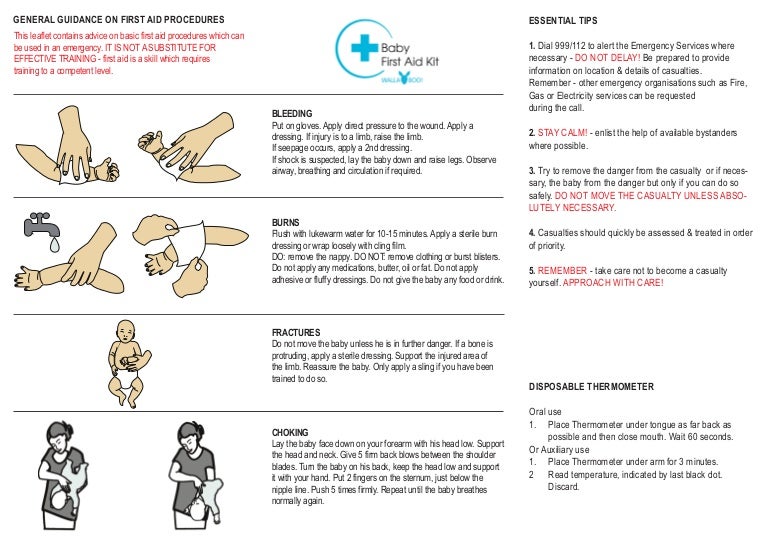 The pathogen enters the body through dirty hands, respiratory tract, minor injuries on the skin. Quickly spreading throughout the body, it manifests itself with a rash, a violation of the excretory function of the kidneys, changes in the composition of the blood and other signs. More often, mouse fever is infected by holidaymakers, farm workers, soil explorers and residents of old houses who are forced to deal with uninvited guests and clean up traces of their life.
The pathogen enters the body through dirty hands, respiratory tract, minor injuries on the skin. Quickly spreading throughout the body, it manifests itself with a rash, a violation of the excretory function of the kidneys, changes in the composition of the blood and other signs. More often, mouse fever is infected by holidaymakers, farm workers, soil explorers and residents of old houses who are forced to deal with uninvited guests and clean up traces of their life.
Is mouse fever transmitted?
The main carrier of the disease are rodents, who prefer to settle in abandoned houses, warehouses, and old buildings. Most of the infected are summer residents or employees of agricultural enterprises working with soil or harvesting. Cases of mutual infection of people have not been identified.
Mouse fever
Hemorrhagic fever with renal syndrome (HFRS) or "mouse fever" is an acute viral natural focal disease characterized by fever, general intoxication, a kind of kidney damage.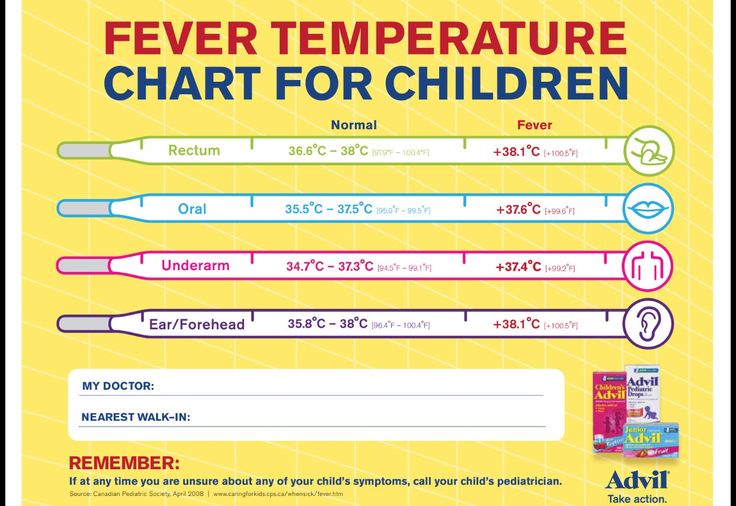 It is dangerous because if treatment is not started in time, the disease will hit the kidneys and can even be fatal.
It is dangerous because if treatment is not started in time, the disease will hit the kidneys and can even be fatal.
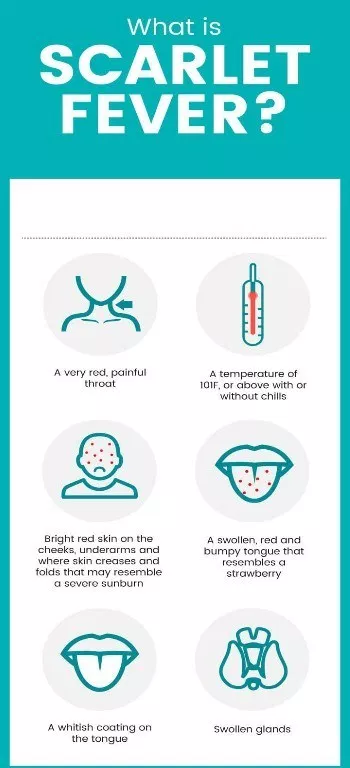
The disease begins suddenly - the temperature rises sharply to 38 - 40 degrees, the head hurts a lot. On the 3-4th day, a rash on the skin may appear in the form of small hemorrhages. There are bleeding from the gums, nose. Due to kidney damage, there are pains in the lower back, abdomen.
The virus is transmitted to humans mainly by airborne dust. When infecting people in the summer, the alimentary route is most common (infection of products with secretions of infected rodents or dirty hands while eating). The disease is not transmitted from person to person. Most often, rural residents and tourists get sick.
Diagnosis:
In the first period of the disease, it can be difficult to recognize. It can be distinguished from acute respiratory diseases by the absence of a runny nose, cough and other symptoms of respiratory tract damage, and from intestinal infections by the late onset of abdominal pain and vomiting, which only intensify with the course of the disease.
The main diagnostic sign is a sharp decrease in the amount of urine and a deterioration in the patient's condition after normalization of body temperature. It is also possible laboratory confirmation of the diagnosis of HFRS
Symptoms and course :
The incubation period lasts from 7 to 46 days (most often from 21 to 25 days). During the course of the disease, the following periods are distinguished: initial, oliguric (the period of renal and hemorrhagic manifestations), polyuric and convalescence.
The initial period lasts from 1 to 3 days and is characterized by an acute onset, an increase in body temperature up to 38-40 ° C, which is sometimes accompanied by chills. There is a severe headache (but no pain in the superciliary arches and eyeballs), weakness, dry mouth, signs of inflammation of the upper respiratory tract are not observed. When examining patients, there is hyperemia of the skin of the face, neck, upper chest.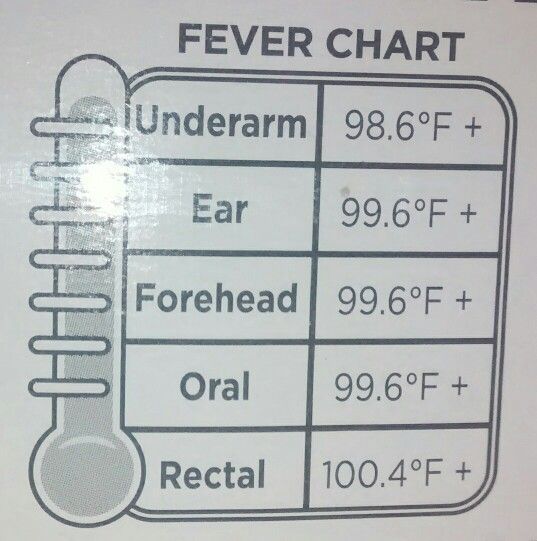 The conjunctiva appears sometimes you can notice a hemorrhagic rash. In some patients, the onset of the disease may be gradual, and 2-3 days before the illness, there may be prodromal phenomena (weakness, malaise, catarrhal phenomena from the upper respiratory tract). From the side of the internal organs in the initial period, no special changes can be identified.
The conjunctiva appears sometimes you can notice a hemorrhagic rash. In some patients, the onset of the disease may be gradual, and 2-3 days before the illness, there may be prodromal phenomena (weakness, malaise, catarrhal phenomena from the upper respiratory tract). From the side of the internal organs in the initial period, no special changes can be identified.
Period from 2-4 to 8-11 days of illness. The body temperature remains at the level of 38-40°C and lasts until the 4th-7th day of illness, however, a decrease in body temperature is not accompanied by an improvement in the patient's condition, more often it even worsens. The most typical manifestation of this period is lower back pain of varying severity (sometimes they begin at the end of the initial period). The absence of pain after the 5th day of illness with the severity of fever and symptoms of intoxication casts doubt on the diagnosis of HFRS. In most patients, 1-2 days after the onset of back pain, vomiting occurs up to 6-8 times a day or more. It has nothing to do with food or medication. At the same time, there are pains in the abdomen, bloating is often noted.
It has nothing to do with food or medication. At the same time, there are pains in the abdomen, bloating is often noted.
When examined during this period, the skin is dry, the face and neck are hyperemic, hyperemia of the mucous membranes of the pharynx and conjunctiva persists, there may be a slight swelling of the upper eyelid, the vessels of the sclera are injected. Hemorrhagic symptoms appear.
The characteristic manifestations of the disease include kidney damage. It manifests itself in puffiness of the face, pastosity of the eyelids, a positive symptom Oliguria develops from the 2nd-4th day, in severe cases it can reach anuria. The protein content in the urine increases significantly (up to 60 g / l), at the beginning of the oliguric period there may be microhematuria, hyaline and granular casts are found in the sediment, sometimes long coarse "fibrinous" Dunayevsky casts appear. Residual nitrogen builds up. The most pronounced azotemia occurs by the 7-10th day of illness.