How to check a child for diabetes
Type 1 diabetes in children - Diagnosis and treatment
Diagnosis
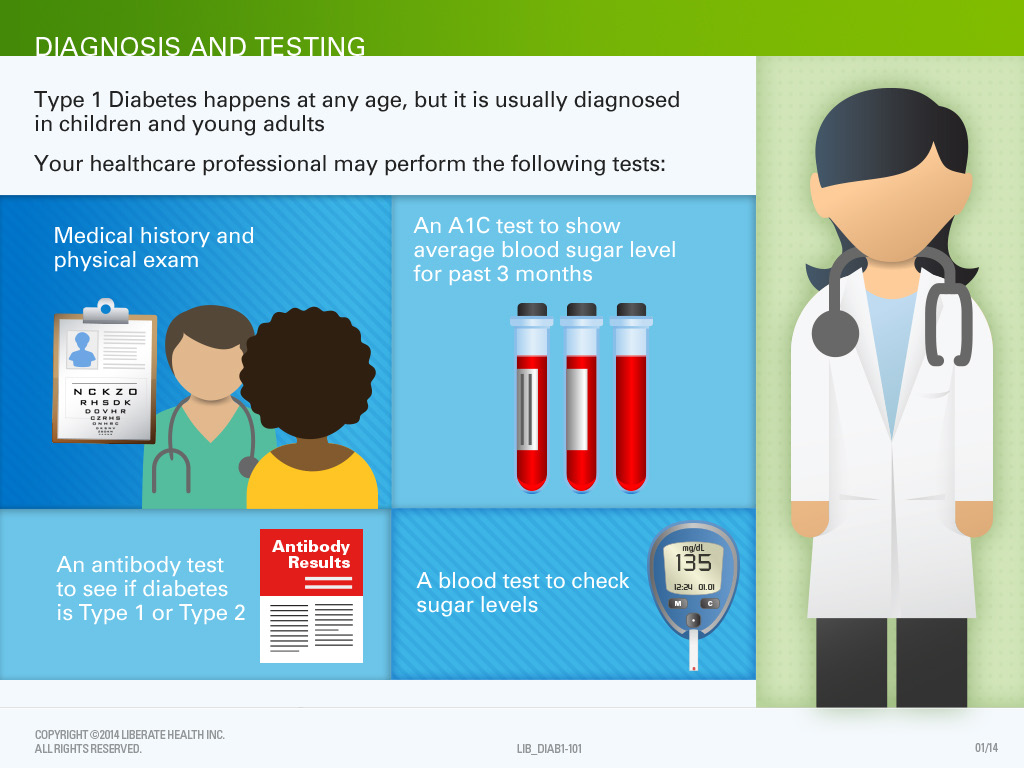
There are several blood tests for type 1 diabetes in children. These tests are used to diagnose diabetes and to monitor diabetes management:
- Random blood sugar test. This is the primary screening test for type 1 diabetes. A blood sample is taken at a random time. A blood sugar level of 200 milligrams per deciliter (mg/dL), or 11.1 millimoles per liter (mmol/L), or higher, along with symptoms, suggests diabetes.
- Glycated hemoglobin (A1C) test. This test indicates your child's average blood sugar level for the past 3 months. An A1C level of 6.5% or higher on two separate tests indicates diabetes.
- Fasting blood sugar test. A blood sample is taken after your child hasn't eaten (fasted) for at least 8 hours or overnight. A fasting blood sugar level of 126 mg/dL (7.
0 mmol/L) or higher suggests type 1 diabetes.
Additional tests
If blood sugar testing indicates diabetes, your health care provider may recommend additional tests to distinguish between type 1 diabetes and type 2 diabetes because treatment strategies differ by type. Additional tests include blood tests to check for antibodies that are common in type 1 diabetes.
More Information
- A1C test
Treatment
Treatment for type 1 diabetes includes:
- Taking insulin
- Monitoring blood sugar
- Eating healthy foods
- Exercising regularly
You'll work closely with your child's diabetes treatment team — health care provider, certified diabetes care and education specialist, and registered dietitian. The goal of treatment is to keep your child's blood sugar within certain numbers. This target range helps to keep your child's blood sugar level as close to normal as possible.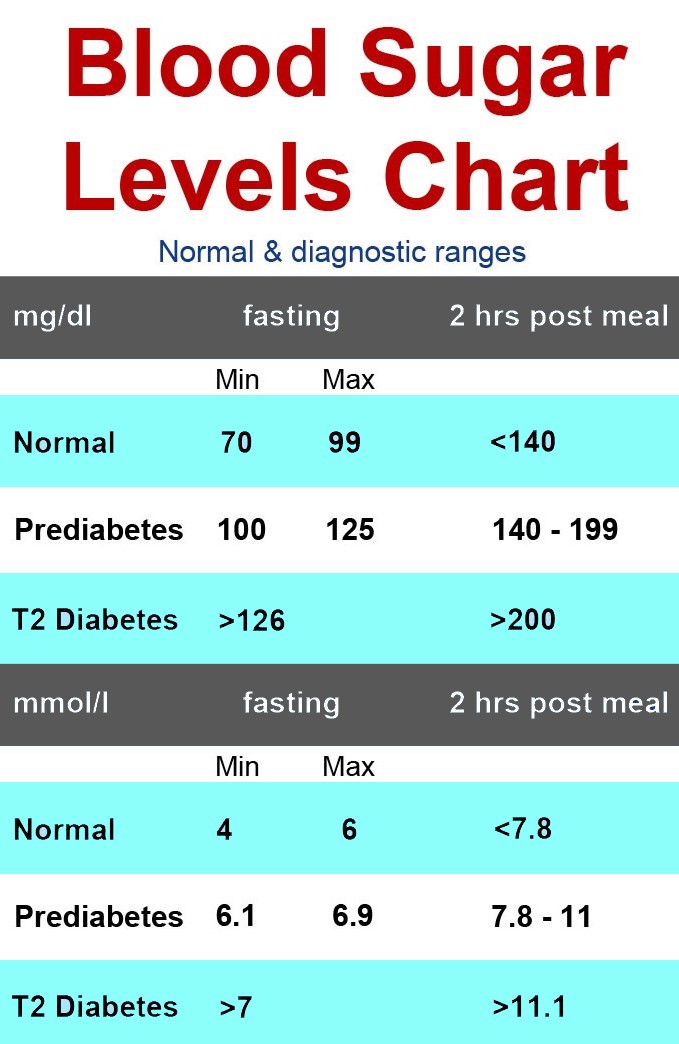
Your child's health care provider will let you know what your child's blood sugar target range is. This range may change as your child grows and changes.
Insulin
Anyone who has type 1 diabetes needs lifelong treatment with one or more types of insulin to survive.
Many types of insulin are available, including:
- Rapid-acting insulin. This type of insulin starts working within 15 minutes. It reaches peak effect at 60 minutes and lasts about 4 hours. This type is often used 15 to 20 minutes before meals. Examples are lispro (Humalog, Admelog), aspart (NovoLog, Fiasp) and glulisine (Apidra).
- Short-acting insulin. Sometimes called regular insulin, this type starts working around 30 minutes after injection. It reaches peak effect at 90 to 120 minutes and lasts about 4 to 6 hours. Examples are human insulin (Humulin R, Novolin R).
- Intermediate-acting insulin. Also called NPH insulin, this type of insulin starts working in about 1 to 3 hours.
 It reaches peak effect at 6 to 8 hours and lasts 12 to 24 hours. Examples are NPH insulin (Humulin N, Novolin N).
It reaches peak effect at 6 to 8 hours and lasts 12 to 24 hours. Examples are NPH insulin (Humulin N, Novolin N). - Long- and ultra-long-acting insulin. This type of insulin may provide coverage for as long as 14 to 40 hours. Examples are glargine (Lantus, Toujeo, other), detemir (Levemir) and degludec (Tresiba).
Insulin delivery options
Insulin delivery options include:
- Fine needle and syringe. This looks like a shot you might get in a health care provider's office, but with a smaller syringe and a much thinner, shorter needle.
- Insulin pen with fine needle. This device looks like an ink pen, except the cartridge is filled with insulin. A needle is attached for injection.
-
An insulin pump. This is a small device worn on the outside of your body that you program to deliver specific amounts of insulin throughout the day and when you eat.
 A tube connects a reservoir of insulin to a catheter that's inserted under the skin of your abdomen.
A tube connects a reservoir of insulin to a catheter that's inserted under the skin of your abdomen.There's also a tubeless pump option that involves wearing a pod containing the insulin on your body combined with a tiny catheter that's inserted under your skin.
Blood sugar monitoring
You or your child will need to check and record your child's blood sugar at least four times a day. Typically, you or your child test his or her blood glucose before every meal and at bedtime and occasionally during the middle of the night. But you or your child may need to check it more often if your child doesn't have a continuous glucose monitor.
Frequent testing is the only way to make sure that your child's blood sugar level remains within the target range.
Continuous glucose monitoring (CGM)
Continuous glucose monitor and insulin pump
Continuous glucose monitor and insulin pump
A continuous glucose monitor, on the left, is a device that measures blood sugar every few minutes using a sensor inserted under the skin. An insulin pump, attached to the pocket, is a device that’s worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen. Insulin pumps are programmed to deliver specific amounts of insulin continuously and with food.
An insulin pump, attached to the pocket, is a device that’s worn outside of the body with a tube that connects the reservoir of insulin to a catheter inserted under the skin of the abdomen. Insulin pumps are programmed to deliver specific amounts of insulin continuously and with food.
Continuous glucose monitoring (CGM) devices measure your blood sugar every few minutes using a temporary sensor inserted under the skin. Some devices show your blood sugar reading at all times on a receiver or your smartphone or smartwatch, while others require that you check your blood sugar by running the receiver over the sensor.
Closed loop system
A closed loop system is a continuous glucose sensor, which checks blood sugar levels every five minutes, and an insulin pump that communicate with each other. The device uses a sophisticated algorithm to automatically deliver the correct amount or withhold insulin when the monitor indicates it's needed.
This is considered a hybrid closed loop system. You or your child still have to tell the device how many carbohydrates are eaten, and periodically confirm blood sugar levels, but the device adjusts insulin delivery throughout the day automatically.
You or your child still have to tell the device how many carbohydrates are eaten, and periodically confirm blood sugar levels, but the device adjusts insulin delivery throughout the day automatically.
Available devices continue to be refined, and there are more systems currently in clinical trials.
Healthy eating
Food is a big part of any diabetes treatment plan, but that doesn't mean your child has to follow a strict "diabetes diet." Just like the rest of the family, your child's diet should regularly include foods that are high in nutrition and low in fat and calories, such as:
- Vegetables
- Fruits
- Lean protein
- Whole grains
Your child's registered dietitian can help you create a meal plan that fits your child's food preferences and health goals, as well as help you plan for occasional treats. The dietitian will also teach you how to count carbohydrates in foods so that you can use that information when figuring out insulin doses.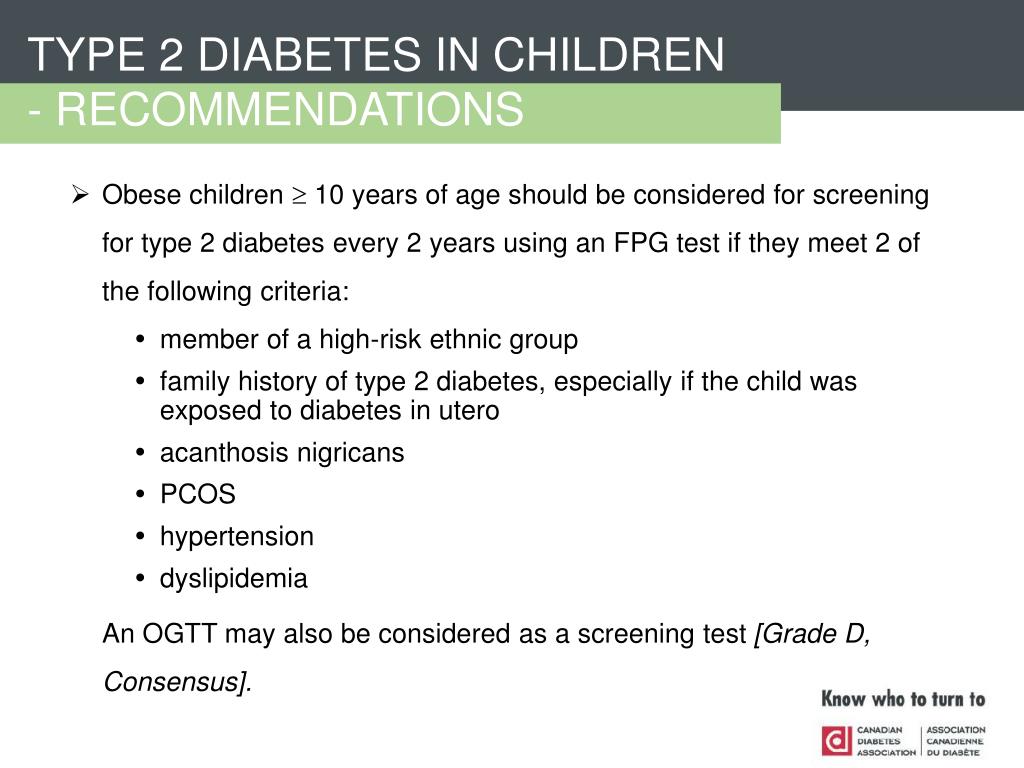
Physical activity
Everyone needs regular aerobic exercise, and children who have type 1 diabetes are no exception.
But remember that physical activity can affect blood sugar. This effect on blood sugar levels can remain for hours after exercise, possibly even overnight. You or your child might need to adjust your child's meal plan or insulin doses for the increased activity.
If your child begins a new activity, check your child's blood sugar more often than usual until you and your child learn how his or her body reacts to the activity.
Make physical activity part of your child's daily routine. Encourage your child to get at least 60 minutes of physical activity daily or, better yet, exercise with your child.
Handling challenges
Blood sugar can sometimes change unpredictably. During these challenges, more frequent blood sugar testing can help identify problems and guide treatment. Ask your child's diabetes treatment team how to handle these and other challenges:
- Picky eating.
 Very young children with type 1 diabetes might not finish what's on their plates, which can be a problem if they've already received insulin for that food.
Very young children with type 1 diabetes might not finish what's on their plates, which can be a problem if they've already received insulin for that food. - Illness. Sickness has varying effects on children's insulin needs. Hormones produced during illness raise blood sugar levels, but reduced carbohydrate intake due to poor appetite or vomiting lowers the insulin requirement. Your child's health care provider will recommend a flu shot for your child every year and may recommend the pneumonia vaccine as well as the COVID-19 vaccine if your child is age 5 or older.
- Growth spurts and puberty. Just when you've mastered your child's insulin needs, he or she sprouts up seemingly overnight, and suddenly isn't getting enough insulin. Hormones also can affect insulin requirements, particularly for teenage females as they begin to menstruate.
- Sleep. To avoid problems with low blood sugar during the night, you might need to adjust your child's insulin routine and snack times.

- Temporary changes in routine. Despite planning, days don't always stay the same. Check blood sugars often when schedules change unexpectedly. Plan ahead for holidays, special occasions and vacations.
Ongoing medical care
Your child will need regular appointments to ensure good diabetes management. This can include a review of your child's blood sugar patterns, insulin needs, eating and physical activity.
Your health care provider also checks your child's A1C levels. The American Diabetes Association generally recommends an A1C of 7% or lower for all children and teens with diabetes.
Your health care provider also will periodically check your child's:
- Blood pressure
- Growth
- Cholesterol levels
- Thyroid function
- Kidney function
- Feet
- Eyes
Signs of trouble
Despite your best efforts, sometimes problems will arise. Certain short-term complications of type 1 diabetes require immediate care or they could become very serious, including:
Certain short-term complications of type 1 diabetes require immediate care or they could become very serious, including:
- Low blood sugar (hypoglycemia)
- High blood sugar (hyperglycemia)
- Diabetic ketoacidosis (DKA)
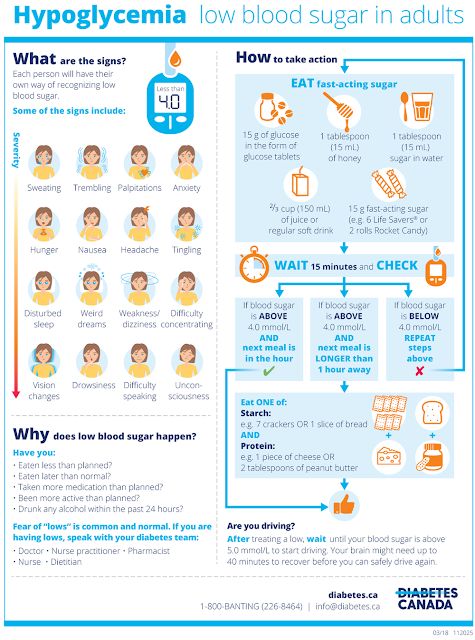
Low blood sugar (hypoglycemia)
Hypoglycemia is a blood sugar level below your child's target range. Blood sugar levels can drop for many reasons, including skipping a meal, getting more physical activity than typical or injecting too much insulin. Low blood sugar is not uncommon in people with type 1 diabetes, but if it isn't treated quickly, symptoms will get worse.
Signs and symptoms of low blood sugar include:
- Pallor
- Shakiness
- Hunger
- Sweating
- Irritability and other mood changes
- Difficulty concentrating or confusion
- Dizziness or lightheadedness
- Loss of coordination
- Slurred speech
- Loss of consciousness
- Seizures
Teach your child the symptoms of low blood sugar. When in doubt, he or she should always do a blood sugar test. If a blood glucose meter isn't readily available and your child is having symptoms of a low blood sugar, treat for low blood sugar, and then test as soon as possible.
When in doubt, he or she should always do a blood sugar test. If a blood glucose meter isn't readily available and your child is having symptoms of a low blood sugar, treat for low blood sugar, and then test as soon as possible.
If your child has a low blood sugar reading:
- Give a fast-acting carbohydrate. Have your child consume 15 to 20 grams of a fast-acting carbohydrate, such as fruit juice, glucose tablets, hard candy, regular (not diet) soda or another source of sugar. Foods with added fat, such as chocolate or ice cream, don't raise blood sugar as quickly because fat slows down the absorption of the sugar.
- Retest blood sugar. Retest your child's blood sugar in about 15 minutes to make sure it's back in the target range. If it's not, repeat giving a fast-acting carbohydrate and testing in 15 minutes as needed until you get a reading in your child's target range.
- Follow up with a snack or meal. Once the blood sugar is back in the target range, have your child eat a healthy snack or a meal to help prevent another low blood sugar level.

If a low blood sugar causes your child to lose consciousness, an emergency injection of a hormone that stimulates the release of sugar into the blood (glucagon) may be necessary.
High blood sugar (hyperglycemia)
Hyperglycemia is a blood sugar level above your child's target range. Blood sugar levels can rise for many reasons, including illness, eating too much, eating certain types of foods and not taking enough insulin.
Signs and symptoms of high blood sugar include:
- Frequent urination
- Increased thirst or dry mouth
- Blurred vision
- Fatigue
- Nausea
If you suspect a high blood sugar level, test your child's blood sugar. If the blood sugar is higher than the target range, follow your child's diabetes treatment plan or check with your child's health care provider. High blood sugar levels don't come down quickly, so ask how long to wait until you check the blood sugar again.
If your child has a blood sugar reading above 240 mg/dL (13. 3 mmol/L), your child should use an over-the-counter ketone test kit to check for ketones.
3 mmol/L), your child should use an over-the-counter ketone test kit to check for ketones.
Diabetic ketoacidosis (DKA)
A severe lack of insulin causes your child's body to break down fat for energy. This causes the body to produce a substance called ketones. Excess ketones build up in your child's blood, creating a potentially life-threatening condition known as diabetic ketoacidosis.
Signs and symptoms of DKA include:
- Thirst or very dry mouth
- Increased urination
- Dry or flushed skin
- Nausea, vomiting or abdominal pain
- A sweet, fruity smell on your child's breath
- Confusion
If you suspect DKA, check your child's urine for excess ketones. If the ketone levels are high, call your child's health care provider or seek emergency care.
More Information
- Pancreas transplant
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.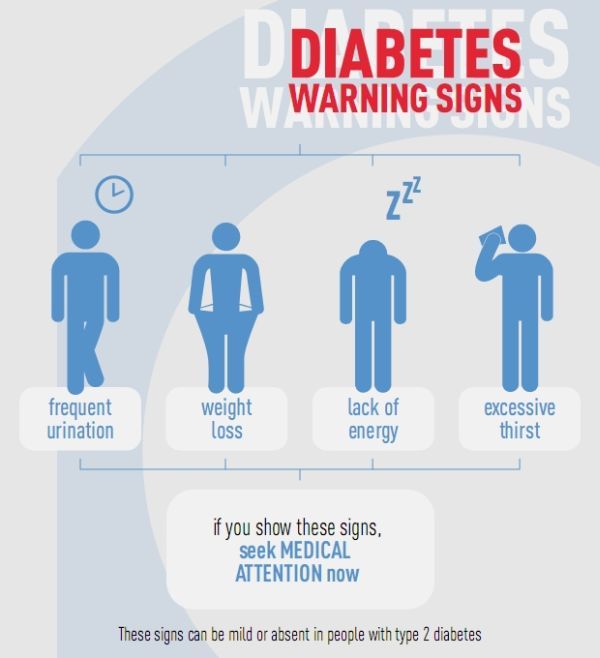
Lifestyle and home remedies
Following a diabetes treatment plan requires 24-hour care and significant lifestyle changes. Careful management of type 1 diabetes helps reduce your child's risk of serious complications.
As your child gets older:
- Encourage him or her to take an increasingly active role in diabetes management
- Stress the importance of lifelong diabetes care
- Teach your child how to test his or her blood sugar and inject insulin
- Help your child make wise food choices
- Encourage your child to remain physically active
- Foster a relationship between your child and his or her diabetes treatment team
- Make sure your child wears a medical identification tag
The habits you teach your child today will help him or her enjoy an active and healthy life with type 1 diabetes.
School and diabetes
You'll need to work with your child's day care provider or school nurse and teachers to make sure they know the signs and symptoms of high and low blood sugar levels. The school nurse might need to administer insulin or check your child's blood sugar levels.
The school nurse might need to administer insulin or check your child's blood sugar levels.
Federal law protects children with diabetes, and schools must make reasonable accommodations to ensure that all children get a proper education.
Ask your health care provider
Contact your child's health care provider, certified diabetes care and education specialist, or registered dietitian between appointments if you have questions.
Coping and support
If managing your child's diabetes seems overwhelming, take it one day at a time. Some days you'll manage your child's blood sugar ideally and on other days, it may seem as if nothing works well. No one can do it perfectly. But your efforts are worthwhile. Don't forget that you're not alone and that your diabetes treatment team can help.
Your child's emotions
Diabetes can affect your child's emotions both directly and indirectly. Poorly controlled blood sugar can cause behavior changes, such as irritability.
Diabetes can also make your child feel different from other kids. Having to draw blood and give shots sets kids with diabetes apart from their peers. Getting your child together with other children who have diabetes or spending time at a diabetes camp may help your child feel less alone.
Mental health and substance abuse
People with diabetes have an increased risk of depression, anxiety and diabetes-related distress. That's why some diabetes specialists regularly include a social worker or psychologist as part of their diabetes care team.
If you notice that your child or adolescent is persistently sad or pessimistic, or experiences dramatic changes in sleeping habits, weight, friends or school performance, have your child screened for depression.
Rebellion also may be an issue, particularly for teens. A child who has been very good about sticking to his or her diabetes treatment plan may rebel in the teen years by ignoring his or her diabetes care. Additionally, experimenting with drugs, alcohol and smoking can be even more dangerous for people with diabetes.
Support groups
Talking to a counselor or therapist may help your child or you cope with the dramatic lifestyle changes that come with a diagnosis of type 1 diabetes. Your child may find encouragement and understanding in a type 1 diabetes support group for children. Support groups for parents also are available.
If you're interested, your health care provider may be able to recommend a group in your area. Websites that offer support include:
- The American Diabetes Association (ADA). The ADA also offers diabetes camp programs that provide education and support for children and teens with diabetes.
- Juvenile Diabetes Research Foundation (JDRF).
Putting information in perspective
The threat of complications from poorly managed diabetes can be frightening. If you and your child work with your child's health care provider and do your best to manage your child's diabetes, your child will likely live a long and enjoyable life.
Preparing for your appointment
Your child's primary care provider will probably make the initial diagnosis of type 1 diabetes. Hospitalization may be needed to stabilize your child's blood sugar levels.
Your child's long-term diabetes care will likely be handled by a pediatric endocrinologist. Your child's health care team also generally includes a certified diabetes care and education specialist, a registered dietitian, and a social worker.
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment take these steps:
- Make a list of any concerns you have about your child's well-being.
- Ask a family member or friend to join you. Managing diabetes requires you to remember a lot of information. Someone who accompanies you may recall something that you missed or forgot.
- Make a list of questions to ask your health care provider.
 Ask your health care provider for a referral to a certified diabetes care and education specialist and a registered dietitian to provide additional education about managing diabetes.
Ask your health care provider for a referral to a certified diabetes care and education specialist and a registered dietitian to provide additional education about managing diabetes.
Topics you might want to discuss with your health care team include:
- Blood sugar monitoring — frequency and timing and continuous glucose monitors
- Insulin therapy — types of insulin used, dose timing and amount
- Insulin administration — shots versus pumps and new diabetes technology
- Low blood sugar — how to recognize and treat
- High blood sugar — how to recognize and treat
- Ketones — testing and treatment
- Nutrition — types of food and their effects on blood sugar
- Carbohydrate counting
- Exercise — adjusting insulin and food intake for activity
- Dealing with special situations ⸺ such as at day care, school or summer camp; during illness; and on special occasions, such as sleepovers, holidays and vacations
- Medical management — how often to visit the health care provider and other diabetes care specialists
What to expect from your doctor
Your health care provider is likely to ask you a number of questions, such as:
- How comfortable are you with managing your child's diabetes?
- How often does your child have low blood sugar episodes?
- What's a typical day's diet like?
- How often does your child participate in physical activity?
By Mayo Clinic Staff
Type 2 diabetes in children - Diagnosis and treatment
Diagnosis
If diabetes is suspected, your child's health care provider will likely recommend a screening test. There are several blood tests to diagnose type 2 diabetes in children.
There are several blood tests to diagnose type 2 diabetes in children.
- Random blood sugar test. A blood sample is taken at a random time, regardless of when your child last ate. A random blood sugar level of 200 milligrams per deciliter (mg/dL), or 11.1 millimoles per liter (mmol/L), or higher suggests diabetes.
- Fasting blood sugar test. A blood sample is taken after your child hasn't had anything to eat or drink but water for at least eight hours or overnight (fasting). A fasting blood sugar level of 126 mg/dL (7.0 mmol/L) or higher suggests diabetes.
- Glycated hemoglobin (A1C) test. This test indicates your child's average blood sugar level for the past 3 months. An A1C level of 6.5% or higher indicates diabetes.
- Oral glucose tolerance test. Your child will need to fast overnight and then drink a sugary liquid at the health care provider's office or a laboratory testing site.
 Blood sugar levels are tested periodically for the next two hours. A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher generally means your child has diabetes.
Blood sugar levels are tested periodically for the next two hours. A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher generally means your child has diabetes.
Additional tests
Your health care provider may recommend additional tests to distinguish between type 1 diabetes and type 2 diabetes, because treatment strategies for each type differ.
More Information
- A1C test
- Glucose tolerance test
Treatment
Treatment for type 2 diabetes is lifelong and can include:
- Healthy eating
- Regular physical activity
- Insulin or other medications
- Blood sugar monitoring
- Weight-loss surgery, in some cases
You'll work closely with your child's diabetes treatment team — including a health care provider, certified diabetes care and education specialist, registered dietitian, and other specialists as needed. The goal of treatment is to keep your child's blood sugar within a certain range. This target range helps to keep your child's blood sugar level as close to the standard range as possible.
The goal of treatment is to keep your child's blood sugar within a certain range. This target range helps to keep your child's blood sugar level as close to the standard range as possible.
Your child's health care provider will let you know what your child's blood sugar target range is, and may also set an A1C target. These numbers may change as your child grows and changes and so will your child's diabetes treatment plan.
Healthy eating
Food is a big part of any diabetes treatment plan, but that doesn't mean your child has to follow a strict "diabetes diet." Your health care provider may recommend weight loss to achieve and maintain a healthy weight. Blood sugar levels can improve with weight loss.
Your child's dietitian will likely suggest that your child — and the rest of the family — consume foods that are high in nutritional value and low in fat and calories.
Healthy eating includes a diet high in fruits, vegetables, nuts, whole grains and olive oil. Choose foods low in fat and calories and high in fiber. Eat a variety of foods to help achieve your child's goals without compromising taste or nutrition.
Choose foods low in fat and calories and high in fiber. Eat a variety of foods to help achieve your child's goals without compromising taste or nutrition.
Your child's dietitian can help you create a meal plan that fits your child's food preferences and health goals, as well as help you plan for occasional treats. Your dietitian is also likely to recommend that your child:
- Reduce portion sizes and not feel a need to finish everything on the plate
- Substitute a fruit or vegetable for a carbohydrate-rich food
- Replace high-calorie beverages, such as soft drinks or fruit juices, with water
- Eat at home more frequently instead of eating at restaurants or getting food to carry out from restaurants
- Help make meals
- Eat at the dinner table instead of in front of the TV
Physical activity
Everyone needs regular aerobic exercise, and children who have type 2 diabetes are no exception. Physical activity helps children control their weight, uses up sugar for energy, and makes the body use insulin more effectively. This can lower blood sugar.
This can lower blood sugar.
Make physical activity part of your child's daily routine. Activity time doesn't have to be all at once — it's OK to break it down into smaller chunks of time. Encourage your child to get at least 60 minutes of physical activity daily or, better yet, exercise with your child.
Medication
There are three medications that have been approved by the Food and Drug Administration (FDA) for treating type 2 diabetes in children.
- Metformin (Glumetza, others). This pill reduces the amount of sugar a child's liver releases into the bloodstream between meals and helps the body's cells use insulin more effectively.
- Liraglutide (Victoza). This medication is taken by injection. Liraglutide helps the body release more insulin from the pancreas after meals, when blood sugar levels are higher. This medication may have digestive system side effects, such as nausea or diarrhea.
-
Insulin.
 Sometimes, insulin may be needed if your child's blood sugar levels are very high. Insulin allows sugar into the cells for energy, reducing the amount of sugar in the bloodstream.
Sometimes, insulin may be needed if your child's blood sugar levels are very high. Insulin allows sugar into the cells for energy, reducing the amount of sugar in the bloodstream.There are a number of different insulins, but a long-acting insulin once a day, along with a short- or rapid-acting insulin with meals, is often used for type 2 diabetes in children. Insulin is typically delivered via a syringe or an insulin pen.
With lifestyle changes and other medications, your child may be able to be weaned off insulin.
Blood sugar monitoring
Your health care provider will let you know how often you or your child need to check and record your child's blood sugar. Children who take insulin usually need to test more frequently, possibly four times a day or more.
Depending on treatment needs, continuous glucose monitoring may be an option. Frequent testing is the only way to make sure that your child's blood sugar level remains within the target range.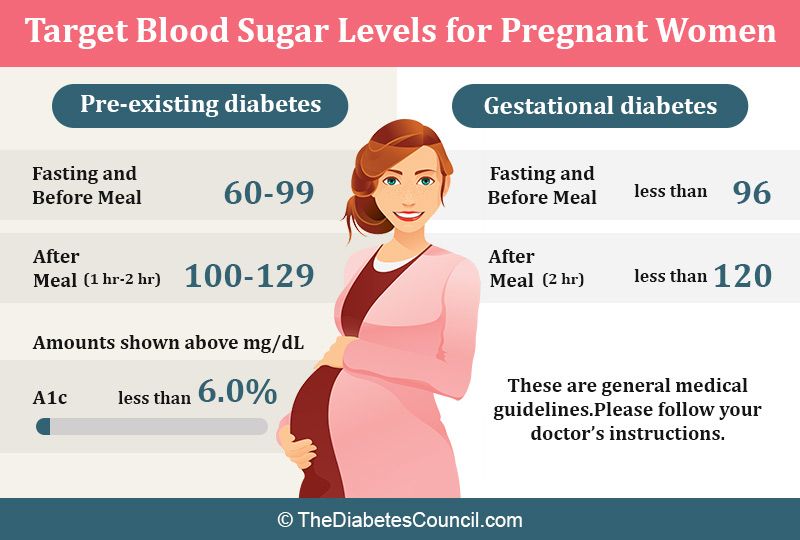
Weight loss surgery
These procedures are not an option for everyone. But for teens who are significantly obese — a body mass index (BMI) at or above 35 — having weight-loss surgery may lead to improved management of type 2 diabetes.
Ongoing medical care
Your child will need regular appointments to ensure good diabetes management. Visits with your child's health care provider can include a review of your child's blood sugar patterns, typical eating habits, physical activity, weight and medication if taken. Healthy-lifestyle changes can reduce the need for medications.
Your health care provider may check your child's A1C levels. The American Diabetes Association generally recommends an A1C of 7% or lower for all children and teens with diabetes.
Your health care provider will also periodically check your child's:
- Growth
- Blood pressure
- Cholesterol levels
- Kidney and liver function
- Eyes ⸺ usually annually
- Feet
- Risk of polycystic ovary syndrome and obstructive sleep apnea
Your child's health care provider will likely recommend a flu shot for your child every year, and may recommend the pneumonia vaccine and the COVID-19 vaccine if your child is age 5 or older.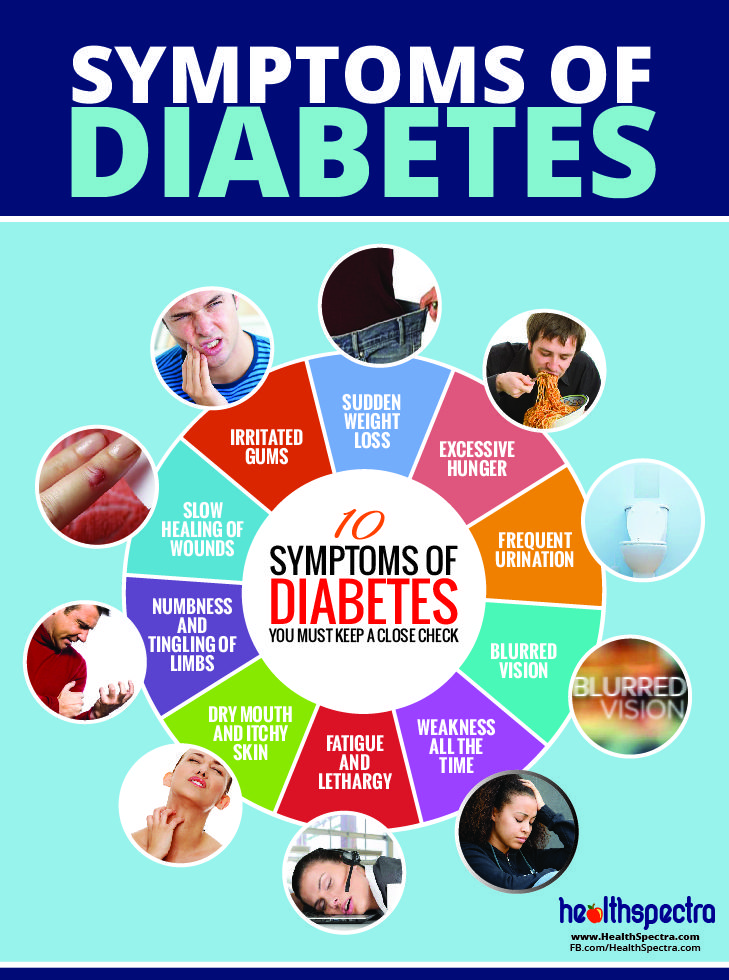
Signs of trouble
Despite your best efforts, sometimes problems will arise. Certain short-term complications of type 2 diabetes — such as low blood sugar, high blood sugar, diabetic ketoacidosis and hyperosmolar hyperglycemic state — require immediate care.
Low blood sugar (hypoglycemia)
Hypoglycemia is a blood sugar level below your child's target range. Blood sugar levels can drop for many reasons, including skipping a meal, eating fewer carbohydrates than planned, getting more physical activity than typical or injecting too much insulin. Children with type 2 diabetes have less risk of low blood sugar than do kids with type 1 diabetes.
Signs and symptoms of low blood sugar include:
- Pallor
- Shakiness
- Hunger
- Sweating
- Irritability and other mood changes
- Difficulty concentrating or confusion
- Dizziness or lightheadedness
- Loss of coordination
- Slurred speech
- Loss of consciousness
- Seizures
Teach your child the symptoms of low blood sugar. When in doubt, your child should always do a blood sugar test. If a blood glucose meter isn't readily available and your child is having symptoms of a low blood sugar, treat for low blood sugar and then test as soon as possible.
When in doubt, your child should always do a blood sugar test. If a blood glucose meter isn't readily available and your child is having symptoms of a low blood sugar, treat for low blood sugar and then test as soon as possible.
If your child has a low blood sugar reading:
- Give a fast-acting carbohydrate. Have your child consume 15 to 20 grams of a fast-acting carbohydrate, such as fruit juice, glucose tablets, hard candy, regular (not diet) soda or another source of sugar. Foods with added fat, such as chocolate or ice cream, don't raise blood sugar as quickly because fat slows down the absorption of the sugar.
- Retest blood sugar. Retest your child's blood sugar in about 15 minutes to make sure it's back in the target range. If it's not, repeat giving a fast-acting carbohydrate and testing in 15 minutes as needed until you get a reading in your child's target range.
High blood sugar (hyperglycemia)
Hyperglycemia is a blood sugar level above your child's target range. Blood sugar levels can rise for many reasons, including illness, eating too much, eating certain types of foods, and not taking enough diabetes medication or insulin.
Blood sugar levels can rise for many reasons, including illness, eating too much, eating certain types of foods, and not taking enough diabetes medication or insulin.
Signs and symptoms of high blood sugar include:
- Frequent urination
- Increased thirst or dry mouth
- Blurred vision
- Fatigue
- Nausea
If you suspect hyperglycemia, check your child's blood sugar. You might need to adjust your child's meal plan or medications. Contact your child's health care provider if your child's blood sugar is regularly above his or her target range.
Diabetes ketoacidosis
A severe lack of insulin causes your child's body to produce certain toxic acids (ketones). If excess ketones build up, your child may develop a potentially life-threatening condition known as diabetic ketoacidosis (DKA). DKA is more common in children with type 1 diabetes but can sometimes occur in children with type 2 diabetes.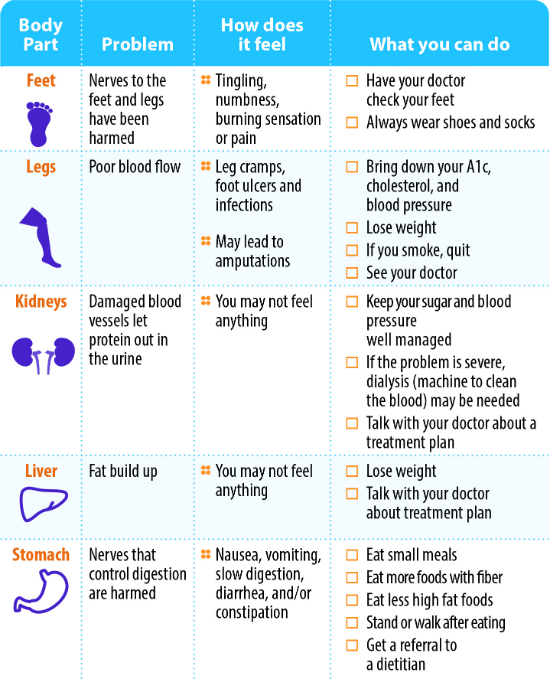
Signs and symptoms of DKA include:
- Thirst or very dry mouth
- Increased urination
- Dry or flushed skin
- Nausea, vomiting or abdominal pain
- A sweet, fruity smell on your child's breath
- Confusion
If you suspect DKA, check your child's urine for excess ketones using an over-the-counter ketone test kit. If the ketone levels are high, call your child's health care provider or seek emergency care.
Hyperosmolar hyperglycemic state
Hyperosmolar hyperglycemic state (HHS) may develop over a period of a few days in children with type 2 diabetes. The extremely high blood sugar level of HHS ⸺ 600 mg/dL or higher ⸺ may develop with severe infections, illness or other medical conditions. The body's attempt to get rid of the high level of sugar by passing it in the urine results in severe dehydration.
Signs and symptoms of HHS include:
- No or minimal ketones in the urine
- Increased urination
- Increased thirst
- Dry mouth and warm, dry skin
- Confusion or combativeness
- Seizures
- Coma
HHS can be life-threatening and requires emergency care.
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Helping your child follow the diabetes treatment plan takes round-the-clock commitment. But careful management of type 2 diabetes can reduce your child's risk of serious complications.
As your child gets older:
- Encourage your child to take an increasingly active role in diabetes management
- Stress the importance of lifelong diabetes care
- Teach your child how to test blood sugar levels and to take medication and inject insulin if needed
- Help your child make healthy food choices
- Encourage your child to remain physically active and limit electronic screen time
- Foster a relationship between your child and the diabetes treatment team
- Make sure your child wears a medical identification tag
School and diabetes
You'll need to work with your child's school nurse and teachers to make sure they know the symptoms of high and low blood sugar levels. The school nurse might need to administer insulin or check your child's blood sugar.
The school nurse might need to administer insulin or check your child's blood sugar.
Federal law protects children with diabetes, and schools must make reasonable accommodations to ensure that all children get a proper education.
When to contact your diabetes care team
Contact your child's health care provider, certified diabetes care and education specialist, or registered dietitian between appointments if your child's blood sugar is consistently out of the target range your health care provider recommended. Also contact the care team if you're not sure what to do in a certain situation.
Coping and support
Living with type 2 diabetes isn't easy — for you or for your child. Good diabetes management requires a lot of changes, especially in the beginning. That's why some diabetes specialists regularly include a social worker or psychologist as part of their diabetes care teams. Don't forget that you're not alone and your diabetes treatment team can help.
If you notice that your child or adolescent is persistently sad or pessimistic, or experiences dramatic changes in sleeping habits, friends or school performance, have your child assessed for depression.
Rebellion also may be an issue, particularly for teens. A child who has been very good about sticking to the diabetes treatment plan may rebel in the teen years by ignoring diabetes care. Additionally, experimenting with drugs, alcohol and smoking can be even more dangerous for people with diabetes.
Talking to a counselor or therapist may help your child or you cope with the dramatic lifestyle changes that come with a diagnosis of type 2 diabetes. Websites that offer support include the American Diabetes Association (ADA).
Preparing for your appointment
Your child's family health care provider or pediatrician will probably make the initial diagnosis of diabetes. However, you'll likely then be referred to a specialist in metabolic disorders in children (pediatric endocrinologist).
Your child's health care team also generally includes a certified diabetes care and education specialist and a registered dietitian.
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment take these steps:
- Ask about any pre-appointment restrictions. If the health care provider is going to test your child's blood sugar, your child might need to fast for eight hours, depending on the type of test.
- Make a list of any symptoms your child is experiencing, including any that may seem unrelated to the reason for your appointment.
- Ask a family member or friend to join you, if possible. Managing diabetes requires you to remember a lot of information. Someone who accompanies you may recall something that you missed or forgot.
- Make a list of questions to ask your health care provider.
Some basic questions to ask your child's health care provider include:
- How often do I need to monitor my child's blood sugar?
- What should my child's blood sugar levels be during the day and before bedtime?
- What changes need to be made in the family diet?
- How much exercise should my child get each day?
- Will my child need to take medication? If so, what kind and how much?
- What signs and symptoms of complications should I look for?
- My child has another health condition.
 How can we best manage them together?
How can we best manage them together? - How often does my child need to be monitored for diabetes care? What specialists do we need to see?
Don't hesitate to ask additional questions during the appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- How comfortable are you with managing your child's diabetes?
- What's a typical day's eating like for your child?
- Is your child exercising? If so, how often?
- How do you feel your child is coping with diabetes and its treatment?
By Mayo Clinic Staff
Childhood diabetes | Prevention | GBUZ "City Polyclinic No. 6 of Novorossiysk" MH KK
Diabetes in children: causes, symptoms and signs, diagnosis, treatment.
) in the blood. Diabetes mellitus ranks first among all endocrine diseases in children. Diabetes mellitus in children is relatively acute and without appropriate treatment, as a rule, acquires a severe, progressive course.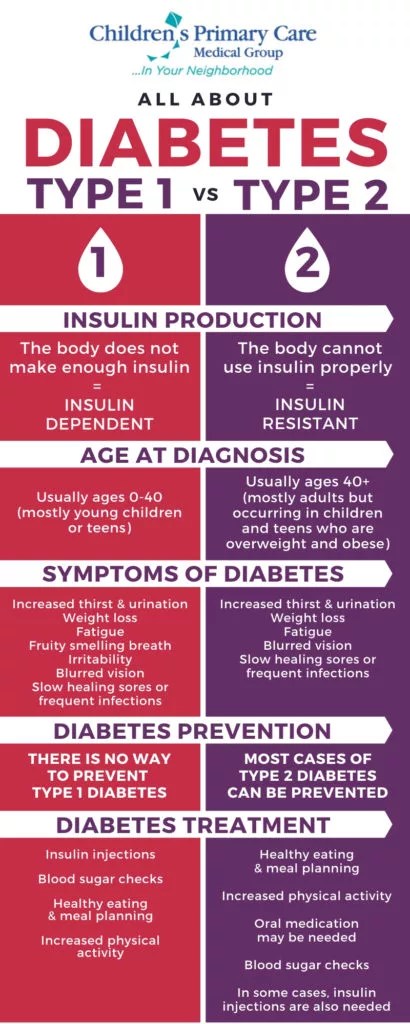 This development of diabetes in children is due to the intensive growth of the child's body and, accordingly, increased metabolism
This development of diabetes in children is due to the intensive growth of the child's body and, accordingly, increased metabolism
Diagnosis of diabetes in children is based on identifying the symptoms of the disease and determining the concentration of glucose and insulin in the blood. Treatment of diabetes mellitus in children includes diet, dosed exercise, treatment with insulin preparations.
Forms of diabetes in children. There are two main types of diabetes mellitus:
- Insulin-dependent diabetes (type 1 diabetes).
- Non-insulin dependent diabetes (type 2 diabetes).
While type 2 diabetes mellitus predominates among adults, type 1 diabetes mellitus (insulin-dependent) predominates among children.
Type 1 diabetes mellitus is characterized by very low levels of insulin in the blood, as a result of which the diabetic child is dependent on insulin treatment.
Features of the development of diabetes in children
A child's pancreas (an organ that produces the hormone insulin) is very small. By the age of 10, the mass of the child's pancreas doubles, reaching a size of 12 cm and a weight of just over 50 g. The production of insulin by the pancreas is one of its most important functions, which is finally formed by the fifth year of a child's life. It is from this age and up to about 11 years that children are especially susceptible to diabetes. All metabolic processes in a child's body proceed much faster than in an adult. Carbohydrate metabolism (assimilation of sugars) is no exception. Accordingly, a child needs to consume 10 g of carbohydrates per 1 kg of weight per day. Therefore, all children are very fond of sweets - this is a natural need of their body. The metabolism of carbohydrates is also affected by the nervous system of the child, which is not yet fully formed, therefore it can malfunction and also affect blood sugar levels. Contrary to popular belief, even the consumption of significant amounts of sweets in childhood does not lead to the development of diabetes.
By the age of 10, the mass of the child's pancreas doubles, reaching a size of 12 cm and a weight of just over 50 g. The production of insulin by the pancreas is one of its most important functions, which is finally formed by the fifth year of a child's life. It is from this age and up to about 11 years that children are especially susceptible to diabetes. All metabolic processes in a child's body proceed much faster than in an adult. Carbohydrate metabolism (assimilation of sugars) is no exception. Accordingly, a child needs to consume 10 g of carbohydrates per 1 kg of weight per day. Therefore, all children are very fond of sweets - this is a natural need of their body. The metabolism of carbohydrates is also affected by the nervous system of the child, which is not yet fully formed, therefore it can malfunction and also affect blood sugar levels. Contrary to popular belief, even the consumption of significant amounts of sweets in childhood does not lead to the development of diabetes.
In general, the risk of developing diabetes is higher in premature, underdeveloped children, or adolescents during puberty. Also, the risk of developing diabetes is higher in children subject to significant physical exertion (for example, in pupils of sports schools).
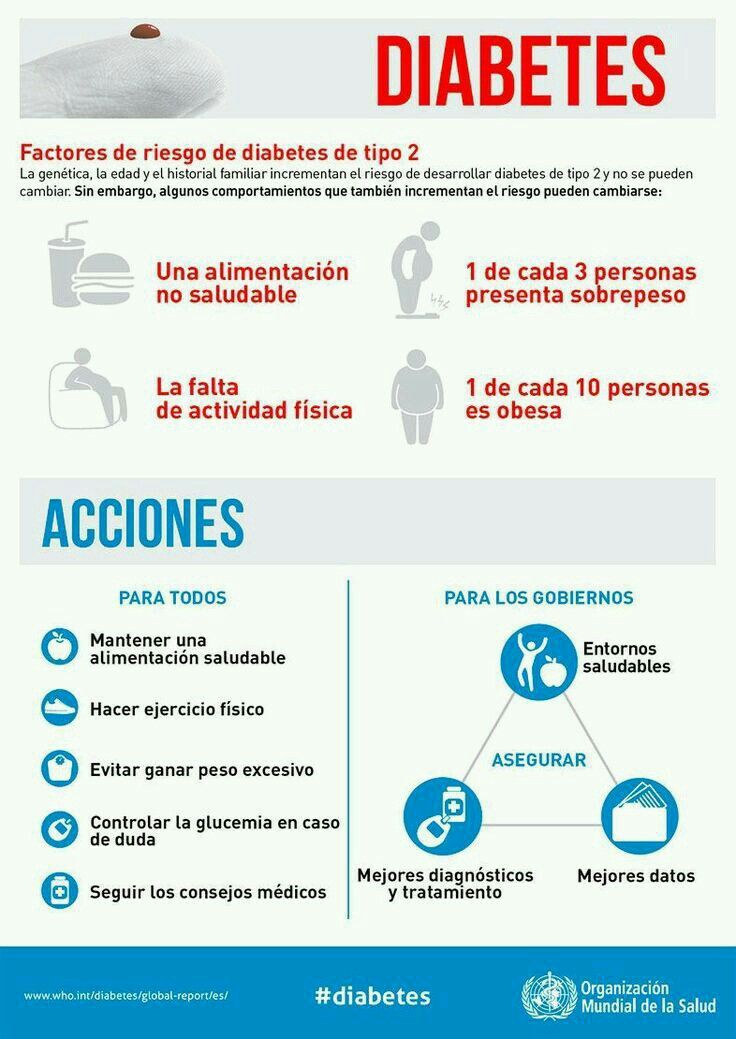
The main cause of diabetes in children is a viral infection that destroys insulin-producing cells in the pancreas. Among childhood infections, many can cause the development of diabetes (mumps, rubella, measles, etc.). In this regard, one of the most important measures to prevent the development of diabetes in children is the timely vaccination of the child.
The course of diabetes mellitus in children also depends on the age of the child at which the disease began. The younger the child with diabetes, the more severe it is and the greater the risk of various complications. As a rule, once having arisen, diabetes in a child never goes away. A child with diabetes will need supportive care throughout his life.
Risk factors for diabetes in children
There are a number of risk factors that contribute to the development of diabetes in children. The presence of one or more risk factors greatly increases a child's chances of developing diabetes. Risk factors for diabetes in children:
- children born to diabetic mothers
- both parents of the child have diabetes mellitus
- frequent acute viral diseases
- birth weight exceeded 4.5 kg
- other metabolic disorders (hypothyroidism, obesity)
- immunosuppression
Symptoms of diabetes in children are almost the same as in adults:
- thirst
- weight loss
- excessive urine output (more than 2-3 liters per day)
- severe infections
- fatigue, inability to concentrate
Parents do not always notice these symptoms, which makes it difficult to detect diabetes in children.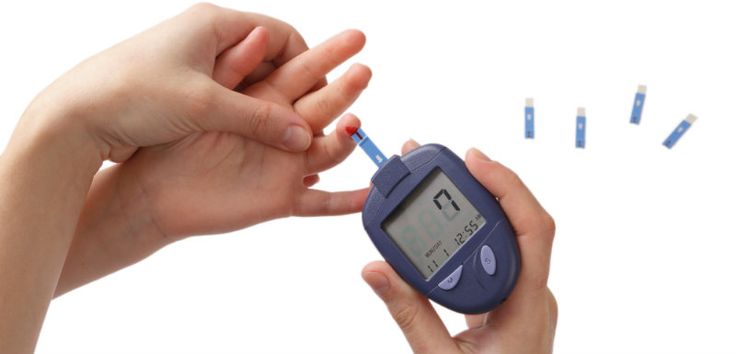 Despite the difficulty in identifying the symptoms of diabetes in a child, there are characteristic signs of diabetes in children that make it easier to identify the disease. So, for example, an important symptom of diabetes is bedwetting. Children with diabetes produce 2-4 times more urine than healthy children. Also, in children with diabetes, skin lesions (furunculosis), itching of the skin, etc. often occur. In infants, diabetes mellitus is accompanied by indigestion (diarrhea, constipation, vomiting), anxiety. A diabetic child suckles a lot and greedily at the breast or drinks water. From sweet urine, linen and diapers become hard, crispy. These symptoms are often observed in moderate or severe diabetes mellitus. In mild diabetes mellitus, sick children may have little to no complaints or signs of illness, and the diagnosis is based on blood and urine sugar levels.
Despite the difficulty in identifying the symptoms of diabetes in a child, there are characteristic signs of diabetes in children that make it easier to identify the disease. So, for example, an important symptom of diabetes is bedwetting. Children with diabetes produce 2-4 times more urine than healthy children. Also, in children with diabetes, skin lesions (furunculosis), itching of the skin, etc. often occur. In infants, diabetes mellitus is accompanied by indigestion (diarrhea, constipation, vomiting), anxiety. A diabetic child suckles a lot and greedily at the breast or drinks water. From sweet urine, linen and diapers become hard, crispy. These symptoms are often observed in moderate or severe diabetes mellitus. In mild diabetes mellitus, sick children may have little to no complaints or signs of illness, and the diagnosis is based on blood and urine sugar levels.
Treatment of diabetes in children.
Treatment of diabetes in a child includes: exercise, diet, medication.
Exercise for children with diabetes
Exercise increases the sensitivity of body tissues to insulin and lowers blood sugar levels. In this regard, dosed physical activity is an important part of the treatment of children with diabetes. It should be emphasized that only dosed physical activity is useful in diabetes, while uncontrolled physical activity in patients with diabetes mellitus contributes to the development of hypoglycemic conditions.
Proper exercise management in diabetic children necessarily includes the use of additional carbohydrates before, during and after exercise in accordance with the recommendations given by your doctor, as well as periodic monitoring of blood glucose levels.
It is important to measure blood glucose before, during and after exercise in order to correctly dose insulin with a short or intermediate duration of action.
Nutrition of a sick child plays an important role in the treatment of diabetes mellitus. The nutrition of a child with diabetes should meet all the requirements that are currently imposed on the nutrition of a healthy child: the diet should be as balanced as possible in all the most important ingredients (proteins, fats, carbohydrates and vitamins). Compliance with this condition allows children with diabetes to grow and develop normally. At the same time, a special diet eliminates the carbohydrate load and thus facilitates the course and treatment of diabetes.
Compliance with this condition allows children with diabetes to grow and develop normally. At the same time, a special diet eliminates the carbohydrate load and thus facilitates the course and treatment of diabetes.
In diabetes mellitus, they limit the use of such foods and dishes as bakery products made from wheat flour, potatoes, cereals (semolina, rice). Porridge is given to the child no more than once a day, using coarse grinding cereals (buckwheat, oatmeal, corn) for their preparation.
Rice, semolina and pasta should be used in limited quantities. The consumption of bread should not exceed 100g per day. Vegetables (everything except potatoes) can be offered to the child without restrictions. Moreover, dishes from various vegetables should make up a significant part of the daily diet of children.
Fruits and berries – unsweetened varieties of apples, black currants, cherries, etc. – are also widely included in the diet for diabetes. Occasionally, you can give your child citrus fruits (oranges, tangerines), strawberries, wild strawberries, raspberries. A child can eat fruits raw and in the form of compotes prepared with sugar substitutes.
A child can eat fruits raw and in the form of compotes prepared with sugar substitutes.
Fatty, spicy and salty sauces, sweet sauces are excluded from the menu. If the child does not have liver diseases associated with diabetes, it is allowed to add a small amount of onion to food as a seasoning.
It is necessary to feed a child with diabetes 6 times a day and more often. The greatest satisfaction for the child, as a rule, brings his usual food. In view of this, when compiling a diet, the features of the family nutrition stereotype should be taken into account: the hours and volume of each meal, the child's eating habits. The composition of the child's diet should be agreed with the doctor observing the child.
Drug treatment of diabetes in children.
Almost all children with diabetes receive insulin. Thanks to the introduction of long-acting insulin preparations into medical practice, as a rule, one injection of insulin per day is sufficient.
The choice of insulin preparation, its dosage and administration schedule are also determined by the attending physician. Tablets for diabetes (Maninil, Glipizide, etc.) are quite effective in treating diabetes in adults, but very rarely give good results in children. They are used in mild forms of the disease or prescribed as an adjuvant to reduce the number of injections or the dose of insulin.
Children and adolescents who are regularly treated, adhere to the diet exactly, develop well physically and mentally.
Properly selected and organized therapy with insulin preparations and constant monitoring of the child's condition greatly alleviate the course of the disease and allow children with diabetes to lead a full life.
Material taken from the site: Cherepovets City Maternity Hospital
Diabetes mellitus in children and adolescents
Category: Useful information.
Type 1 diabetes mellitus (insulin-dependent) predominates among children.
 Although in recent years, type 2 diabetes occurs in obese children older than 8 years. A child can get sick at any age, often diabetes develops in children under 5 years of age.
Although in recent years, type 2 diabetes occurs in obese children older than 8 years. A child can get sick at any age, often diabetes develops in children under 5 years of age. What contributes to the development of diabetes in children?
- genetic predisposition.
- Early refusal of breastfeeding, improper introduction of complementary foods,
- Overweight.
- Infectious diseases transferred in early childhood.
- Stress.
The symptoms of diabetes mellitus in children are almost the same as in adults: severe thirst, bedwetting appears, the child loses weight, fatigue, poor performance at school, skin infections (boils, barley) often recur, and vaginal candidiasis in girls.
Diabetes in children of the first year of life is rare, but it still happens sometimes. An infant cannot complain. If the baby is in a diaper, then parents are unlikely to notice that he has begun to excrete much more urine. Diabetes can be suspected if the child is not gaining or losing weight; greedily drinks water; frequent diaper rash; after the urine dries, the diapers become as if starched; if urine gets on the floor, then sticky spots remain there. Acute symptoms of diabetes in children: vomiting, intoxication, severe dehydration.
Diabetes can be suspected if the child is not gaining or losing weight; greedily drinks water; frequent diaper rash; after the urine dries, the diapers become as if starched; if urine gets on the floor, then sticky spots remain there. Acute symptoms of diabetes in children: vomiting, intoxication, severe dehydration.
The diagnosis is usually quickly confirmed by detecting an increase in blood glucose (greater than 11.1 mmol/L). If ketone bodies are detected in the blood or urine, urgent therapy is indicated. Waiting the next day to confirm hyperglycemia can be life-threatening. Children with diabetes need lifelong hormone replacement therapy. Diabetes never goes away. A child with diabetes will need maintenance treatment with insulin for the rest of his life.
Prevention of diabetes.
- Control of blood glucose levels, if among close relatives there are patients with diabetes mellitus.
- Breastfeeding up to 12 months, timely introduction of complementary foods.