Fever and vomit 2 year old
Vomiting in children and babies
It's normal for babies and children to vomit occasionally. In most cases, it will last no longer than one to two days and isn't a sign of anything serious.
The most common cause of vomiting in children and babies is gastroenteritis. This is an infection of the gut usually caused by a virus or bacteria, which also causes diarrhoea. The symptoms can be unpleasant but your child will usually start to feel better after a few days.
However, persistent vomiting can sometimes cause your child to become severely dehydrated and occasionally it can be a sign of something more serious, such as meningitis.
This page outlines what to do if your child keeps vomiting and describes some of the common causes of vomiting in children and babies.
If your child has a high temperature, you can also read a separate page about fever in children.
What to do
If your child vomits, you should keep a close eye on them. Trust your instincts and contact your GP immediately if you're worried.
If the cause is just a tummy bug, your child should still be feeling well enough to eat, play and be their usual self. In this case, keep feeding them as normal and offer them regular drinks (see below).
But if they don't seem themself – for example, if they're floppy, irritable or less responsive – they may be seriously ill, so you should get medical help immediately.
When to get medical advice
You should contact your GP if:
- your child is repeatedly vomiting and is unable to hold down fluids
- you think they're dehydrated – symptoms of dehydration can include a dry mouth, crying without producing tears, urinating less or not wetting many nappies, and drowsiness
- their vomit is green or contains blood
- they have been vomiting for more than a day or two
Go to your nearest accident and emergency (A&E) department if your child is vomiting and develops sudden and severe tummy pain, or they're floppy, irritable or less responsive
Call 999 for an ambulance or go to your nearest A&E department immediately if they're vomiting and have a headache, stiff neck and a rash.
Looking after your child at home
In most cases, you can treat your child safely at home. The most important thing you can do is make sure they keep drinking fluids to prevent dehydration.
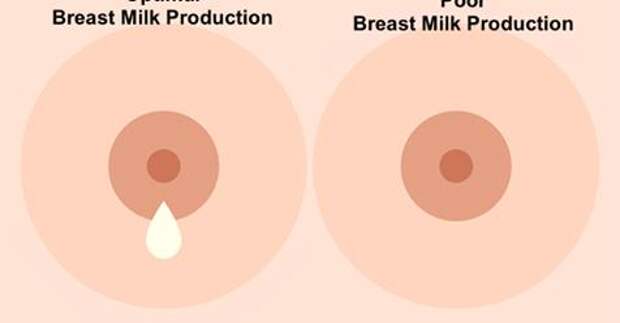
If your baby is vomiting, carry on breastfeeding or giving them milk feeds. If they seem dehydrated, they will need extra fluids. Ask your GP or pharmacist whether you should give your baby oral rehydration solution.
Oral rehydration solution is a special powder that you make into a drink. It contains sugar and salts to help replace the water and salts lost through vomiting and diarrhoea.
Children who are vomiting should keep taking small sips of clear fluid, such as water or clear broth. Fruit juice and fizzy drinks should be avoided until they're feeling better. If they're not dehydrated and haven't lost their appetite, it's fine for your child to eat solid foods as normal.
Again, speak to your GP or pharmacist if you're concerned about dehydration. They may recommend an oral rehydration solution for your child. Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
If your child has diarrhoea and is vomiting, they shouldn't go to school or any other childcare facility until 48 hours after the last episode of diarrhoea or vomiting.
Read more about treating gastroenteritis in children.
Causes of vomiting in children
There are a number of possible causes of vomiting in children, which are described below.
Gastroenteritis
Gastroenteritis is an infection of the gut. It's a common cause of vomiting in children and usually lasts a few days.
Food allergy
Food allergies can cause vomiting in children, as well as other symptoms, such as a raised, red, itchy skin rash (urticaria) and swelling of the face, around the eyes, lips, tongue or the roof of the mouth.
Watch out for foods that may bring on vomiting and see your GP for a diagnosis if you think your child may have a food allergy.
Other infections
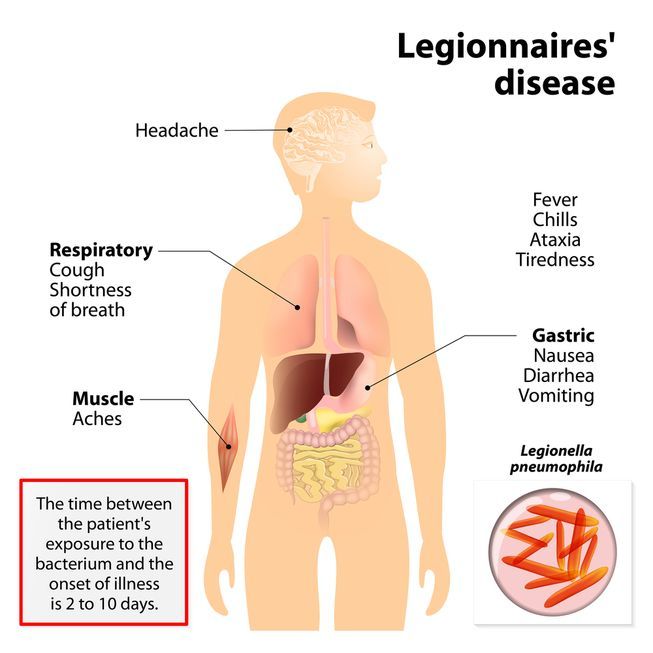
Vomiting can sometimes be a sign of an infection other than gastroenteritis, such as urinary tract infections (UTIs), middle ear infections, pneumonia or meningitis.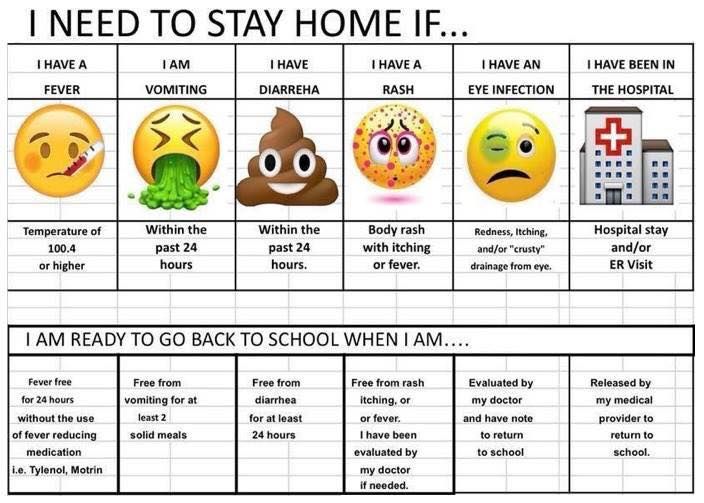
Contact your child's GP if they're vomiting and experiencing additional symptoms of an infection, such as a high temperature (fever) and irritability.
Appendicitis
Appendicitis is a painful swelling of the appendix, a finger-like pouch connected to the large intestine. It causes severe tummy pain that gets worse over time.
If your child has tummy pain that's gradually getting worse, contact your GP, or if they aren't open call NHS 24's 111 service immediately. You should call 999 for an ambulance if they have pain that gets worse quickly and spreads across their tummy.
In most cases of appendicitis, the appendix will need to be surgically removed as soon as possible.
Poison
Accidentally swallowing something poisonous can cause your child to vomit. If you think this is the case, contact your GP immediately or take your child to your nearest accident and emergency (A&E) department.
Causes of vomiting in babies
These include:
- gastroenteritis
- a food allergy or milk intolerance
- gastro-oesophageal reflux – where stomach contents escape back up the gullet
- too big a hole in the bottle teat, which causes your baby to swallow too much milk
- accidentally swallowing something poisonous
- congenital pyloric stenosis – a condition present at birth where the passage from the stomach to the bowel has narrowed, so food is unable to pass through easily; this causes projectile vomiting
- a strangulated hernia – your baby will vomit frequently and cry as if they are in a lot of pain; this should be treated as a medical emergency
- intussusception (where the bowel telescopes in on itself) – as well as vomiting, your baby may look pale, floppy and have symptoms of dehydration
Vomiting Without Diarrhea
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- It's normal for nausea (upset stomach) to come before each bout of vomiting
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis.
 Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours. - Food Poisoning. This causes rapid vomiting within hours after eating the bad food. Diarrhea may follow. Caused by toxins from germs growing in foods left out too long. An example is Staph toxin in egg salad.
- Ibuprofen. Ibuprofen products (such as Advil) can be a stomach irritant. If taken on an empty stomach, it can cause vomiting.
- Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Common foods are peanuts, tree nuts, fish and shellfish (such as shrimp).
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Motion Sickness. Vomiting and dizziness are triggered by motion.
 Sea sickness or fun-park ride sickness are the most common types. Strongly genetic.
Sea sickness or fun-park ride sickness are the most common types. Strongly genetic. - Migraine Headaches. In children, most migraine headaches also have vomiting.
- Serious Causes. Vomiting alone (without diarrhea) should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. Examples are appendicitis, a kidney infection, diabetes and head injury. A serious cause in young babies is pyloric stenosis. See below for more on this.
- Cyclic Vomiting. Cyclic vomiting is the most common cause of recurrent attacks of vomiting. Attacks have a sudden onset and offset. Often occur in children who later develop migraine headaches.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful. It becomes projectile and shoots out.
- Right after vomiting, the baby is hungry and wants to feed.
 ("hungry vomiter")
("hungry vomiter") - Cause: the pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: weight loss or dehydration
- Treatment: cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.

- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
- A child with severe dehydration becomes too weak to stand. They can also be very dizzy when trying to stand.
When to Call for Vomiting Without Diarrhea
Call 911 Now
- Can't wake up
- Not moving or too weak to stand
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected. No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Severe headache
- Diabetes suspected (drinking lots, frequent urine, weight loss)
- Kidney infection suspected (side or back pain, fever, painful to pass urine)
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Severe vomiting (vomits everything) more than 8 hours while getting clear fluids
- High-risk child (such as diabetes, stomach or head injury)
- Weak immune system. Examples are: sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age less than 1 year with vomiting
- Vomits for more than 24 hours
- Fever lasts more than 3 days
- Fever returns after being gone more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Vomiting is a frequent problem
- You have other questions or concerns
Self Care at Home
- Mild or moderate vomiting (most likely viral gastritis)
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting without Diarrhea
- What You Should Know About Vomiting Without Diarrhea:
- Most vomiting is caused by a viral infection of the stomach. Sometimes, mild food poisoning is the cause.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration.
 Dehydration means the body has lost too much fluid.
Dehydration means the body has lost too much fluid. - Here is some care advice that should help.
- Formula Fed Babies - Give Oral Rehydration Solution (ORS) for 8 Hours:
- If your child vomits more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drugstores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk.
 ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse.
ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse. - Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Older Children (over 1 Year Old) - Offer Small Amounts of Clear Fluids For 8 Hours:
- Water or ice chips are best for older children. Reason: Water is easily absorbed in the stomach.
- Other clear fluids: Use half-strength Gatorade. Make it by mixing equal amounts of Gatorade and water. Can mix apple juice the same way. ORS (such as Pedialyte) is usually not needed in older children. Popsicles work great for some kids.
- The key to success is giving small amounts of fluid. Offer 2-3 teaspoons (10-15 mL) every 5 minutes. Older kids can just slowly sip a clear fluid.
- After 4 hours without throwing up, increase the amount.
- After 8 hours without throwing up, return to regular fluids.
- Caution: If vomits over 12 hours, switch to ORS or half-strength Gatorade.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- Start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom). Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.

- Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to School:
- Your child can return to school after the vomiting and fever are gone.
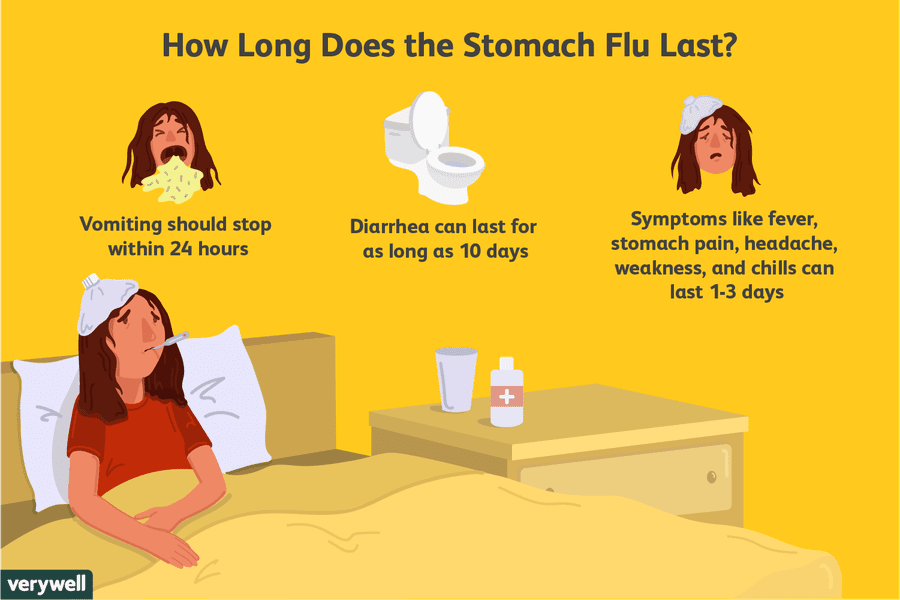
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach pain present even when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/27/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Viral gastroenteritis (children)
Most diarrhea and vomiting in children is caused by a virus. This is viral gastroenteritis. Many people call it "stomach flu" but it has nothing to do with the flu. This virus infects the stomach and intestinal tract. The disease lasts from 2 to 7 days. Diarrhea means loose or watery stools that are different from a baby's normal bowel movements.
The child may also have the following symptoms:
The main danger of this disease is that it leads to dehydration. This is the loss of a large amount of water and mineral salts by the body. In such cases, fluid loss by the body must be replenished. This is done with oral rehydration solution. These solutions are available from pharmacies and most grocery stores without a prescription.
These solutions are available from pharmacies and most grocery stores without a prescription.
Antibiotics do not help with this disease.
Home Care
Follow your pediatrician's instructions.
If you give medicine to your child:
-
Do not use over-the-counter diarrhea medications unless your doctor tells you to.
-
Acetaminophen or ibuprofen can be used for pain and fever. Or another medicine as prescribed.
-
Aspirin as an antipyretic is contraindicated in children under 18 years of age. Its use can lead to serious liver problems and a life-threatening condition called Reye's syndrome.
To prevent the spread of disease:
-
Remember that washing your hands with soap and clean running water or using an alcohol-based disinfectant is the best way to prevent the spread of infection.
-
Teach all family members when and how to wash their hands. Wet your hands with clean running water. Apply soap to the back of your hands, between your fingers and under your nails. Rub your hands for at least 20 seconds. If you need a timer, try singing "Happy Birthday to You!" twice. from the beginning to the end. Rinse your hands well and dry with a clean towel.
-
Wash your hands before and after caring for your sick child.
-
Clean the toilet after each use.
-
Dispose of soiled diapers in an airtight container.
-
Keep the child away from other people until the doctor says so.
-
Wash your hands before and after preparing food.
-
Wash hands and utensils after using cutting boards, countertops and knives that have been in contact with raw food.
-
Keep raw meat away from cooked and ready-to-eat foods.
-
Please note that people with diarrhea or vomiting should not prepare food for others.
How to properly water and feed
The main goal in the treatment of vomiting or diarrhea is to prevent dehydration. To do this, the child should often consume liquids in small portions.
-
Fluid is now more important than food. Give a small amount of liquid at a time, especially if the child has stomach cramps or is vomiting.
-
For diarrhea: If you are giving milk to a baby and the diarrhea does not stop, refuse the milk.
 In some cases, milk can make diarrhea worse. If this happens, use an oral rehydration solution. Eliminate apple juice, soda, sports or other sweetened drinks. Drinks with sugar can make diarrhea worse.
In some cases, milk can make diarrhea worse. If this happens, use an oral rehydration solution. Eliminate apple juice, soda, sports or other sweetened drinks. Drinks with sugar can make diarrhea worse. -
For vomiting: Start with oral rehydration solution at room temperature. Give 1 teaspoon (5 ml) every 5 minutes. Even if the child is vomiting, continue to give the solution. Most of the fluid will be absorbed despite vomiting. After 2 hours without vomiting, start with a small amount of milk or formula and other fluids. Increase the amount depending on tolerance. Do not give your child plain water, milk, formula, or other liquids until the vomiting stops. Give more oral rehydration solution as vomiting decreases. Increase the interval between doses. Continue until the child has urine and is no longer thirsty (no interest in drinking). If there has been no vomiting within 4 hours, resume feeding solid food.
 After 24 hours without vomiting, resume normal eating.
After 24 hours without vomiting, resume normal eating. -
As you feel better, you can gradually resume your child's normal diet. Don't force your child to eat, especially if they have stomach pain or cramps. Do not feed your baby large portions at a time, even if he is hungry. Tobacco smoke can make a child feel worse. Over time, the child can be given more food, provided it is tolerated. Foods that are allowed include cereals, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzel, rice or noodle soups, and cooked vegetables.
-
If symptoms return, return to a simple or no therapeutic diet.
Postoperative care
See your pediatrician or follow his instructions. If a stool or culture test is taken, see your doctor for results as directed.
Call 911
Call 911 if your child has any of these symptoms:
-
Labored breathing
-
Confusion
-
Extreme drowsiness or loss of consciousness
-
Trouble walking
-
Rapid pulse
-
Chest pains
-
Neck stiffness
-
Convulsions
When to seek medical help
Seek immediate medical attention in the following cases:
-
Abdominal pain worse
-
Constant pain in the right lower abdomen
-
Recurrent vomiting after first 2 hours of fluid intake
-
Episodic vomiting for more than 24 hours
-
Continuous severe diarrhea for more than 24 hours
-
Blood in stool or vomit
-
Child drinks less liquid than usual
-
Darkening or no urine for 6 to 8 hours in older children, 4 to 6 hours in toddlers
-
Whims or crying when the child cannot be soothed
-
Unusual drowsiness
-
New skin eruptions
-
Diarrhea lasting more than 10 days
-
Temperature (see Temperature and children below)
Temperature in children
Use a digital thermometer to take your child's temperature. Never use a mercury thermometer. There are various types and ways of using digital thermometers. For example:
Never use a mercury thermometer. There are various types and ways of using digital thermometers. For example:
-
Rectal. For children under 3 years of age, rectal temperature is the most accurate.
-
Frontal (temporal). It is used for children aged 3 months and older. If a child under 3 months of age has signs of illness, this method can be used for the first measurement. The doctor may also check the rectal temperature for confirmation.
-
Ear (tympanic). The ear method is accurate for children 6 months and older, but not younger.
-
Axillary (axillary). This is the least reliable method, but can be used for the first measurement to check on a child of any age who is showing signs of illness.
 The doctor may also check the rectal temperature for confirmation.
The doctor may also check the rectal temperature for confirmation. -
Oral (oral). Do not take oral temperature until the child is 4 years of age.
Use the rectal thermometer with care. For correct use, follow the manufacturer's instructions. Insert it carefully. Make a note on it and make sure it will not be used orally. It can carry germs from the stool. If a rectal thermometer doesn't work for you, ask your doctor which thermometer is best to use. When you tell a doctor about your child's temperature, tell him what type of thermometer you took it with.
Here are some tips to help you know if your baby has a fever. Your child's doctor may give you other values. Follow your healthcare provider's instructions.
Temperature values for infants up to 3 months:
-
Rectal or forehead thermometer: 38°C (100.
 4°F) or higher
4°F) or higher -
Underarm thermometer: temperature 37.2 °C (99 °F) or higher
Temperature readings for children aged 3 to 36 months (3 years):
-
Rectal, forehead or ear thermometer: temperature 38.9°C (102°F) or higher
-
Axillary thermometer: temperature 38.3 °C (101 °F) or higher
Call a doctor in the following cases:
-
Recurrent fever of 40°C (104°F) or more in a child of any age
-
Temperature 38°C (100.4°F) or higher in an infant under 3 months
-
Temperature lasting more than 24 hours in a child under 2 years of age
-
Temperature that persists for 3 days in a child 2 years of age or older
© 2000-2022 The StayWell Company, LLC.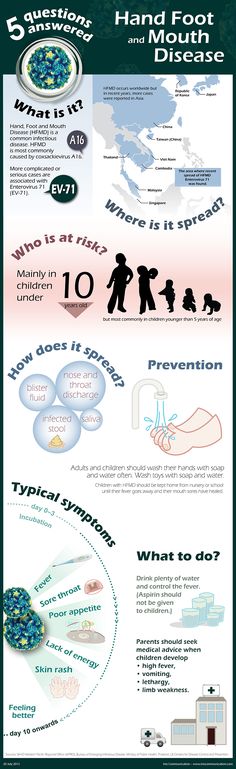 All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Was this helpful?
Yes no
Tell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.
I still don't know what to do next.
other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
symptoms and treatment (reminder for parents)
Enteroviral infections - is a group of diseases, the causes of which are based on several types of viruses.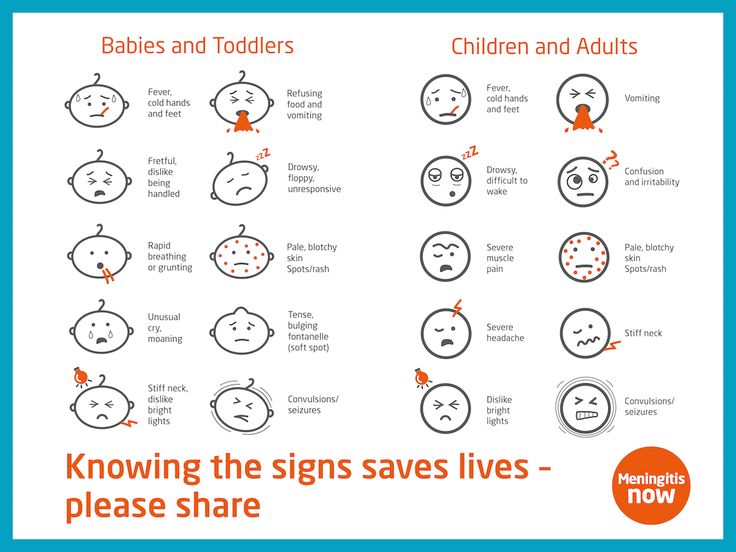 The disease is caused by Coxsackieviruses, polioviruses and ECHO (ECHO).
The disease is caused by Coxsackieviruses, polioviruses and ECHO (ECHO).
After an enterovirus infection, persistent lifelong immunity is formed, however, it is serospecific. This means that immunity is formed only to the serological type of virus that the child has had and does not protect him from other varieties of these viruses. Therefore, a child can get sick with an enterovirus infection several times in his life. Also, this feature does not allow the development of a vaccine to protect our children from this disease. The disease has a seasonality: outbreaks of the disease are most often observed in the summer-autumn period.
Causes of infection with enterovirus infection.
Infection occurs in several ways. Viruses can enter the environment from a sick child or from a child who is a carrier of the virus. Virus carriers do not have any manifestations of the disease, however, the viruses are in the intestines and are excreted into the environment with feces.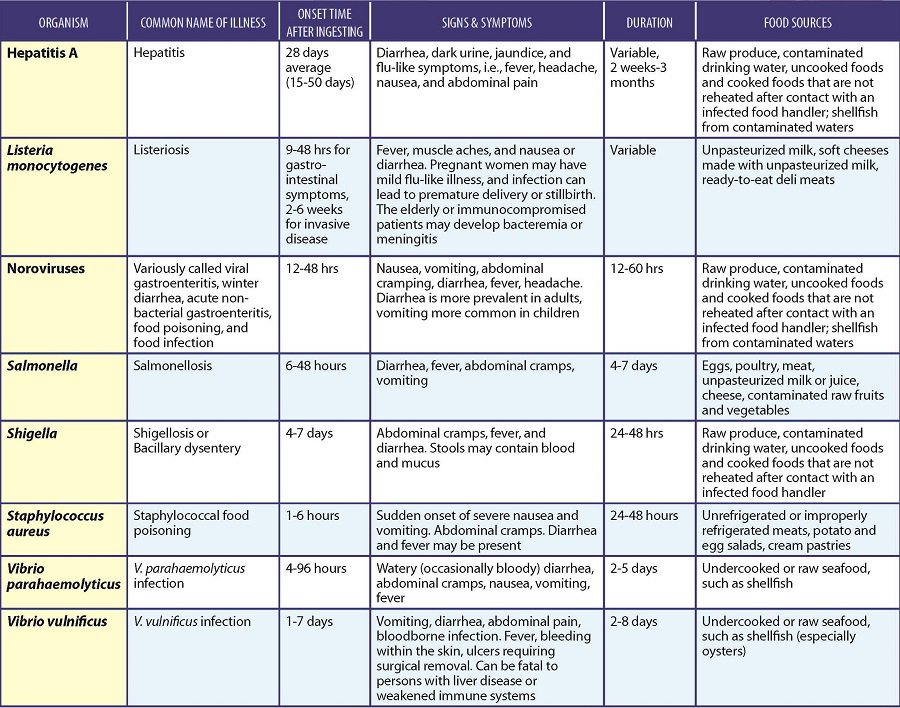 This condition can be observed in children who have been ill after a clinical recovery, or in children in whom the virus has entered the body, but could not cause the disease due to the strong immunity of the child. The virus carrier can persist for 5 months.
This condition can be observed in children who have been ill after a clinical recovery, or in children in whom the virus has entered the body, but could not cause the disease due to the strong immunity of the child. The virus carrier can persist for 5 months.
Once in the environment, viruses can persist for quite a long time, as they tolerate adverse effects well. Viruses are well preserved in water and soil; when frozen, they can survive for several years; heated to 45ºС die in 45-60 seconds).
How enterovirus infection is transmitted.
The transmission mechanism can be airborne (when sneezing and coughing with droplets of saliva from a sick child to a healthy one) and fecal-oral if personal hygiene is not followed. Most often, infection occurs through water, when drinking raw (not boiled) water. It is also possible to infect children through toys if children take them in their mouths. Most often, children aged 3 to 10 years are ill. In children who are breastfed, there is immunity in the body received from the mother through breast milk, however, this immunity is not stable and quickly disappears after the cessation of breastfeeding.
Symptoms of enterovirus infection.
Viruses enter the body through the mouth or upper respiratory tract. Once in the child's body, the viruses migrate to the lymph nodes, where they settle and begin to multiply. The further development of the disease is associated with many factors, such as virulence (the ability of the virus to resist the protective properties of the body), tropism (the tendency to infect individual tissues and organs) of the virus, and the state of the child's immunity.
Enteroviral infections have both similar manifestations and different ones, depending on the species and serotype. The incubation period (the period from the virus entering the child's body until the first clinical signs appear) is the same for all enterovirus infections - from 1 to 10 days (usually 2-5 days).
The disease begins acutely - with an increase in body temperature to 38-39º C. The temperature most often lasts 3-5 days, after which it drops to normal numbers.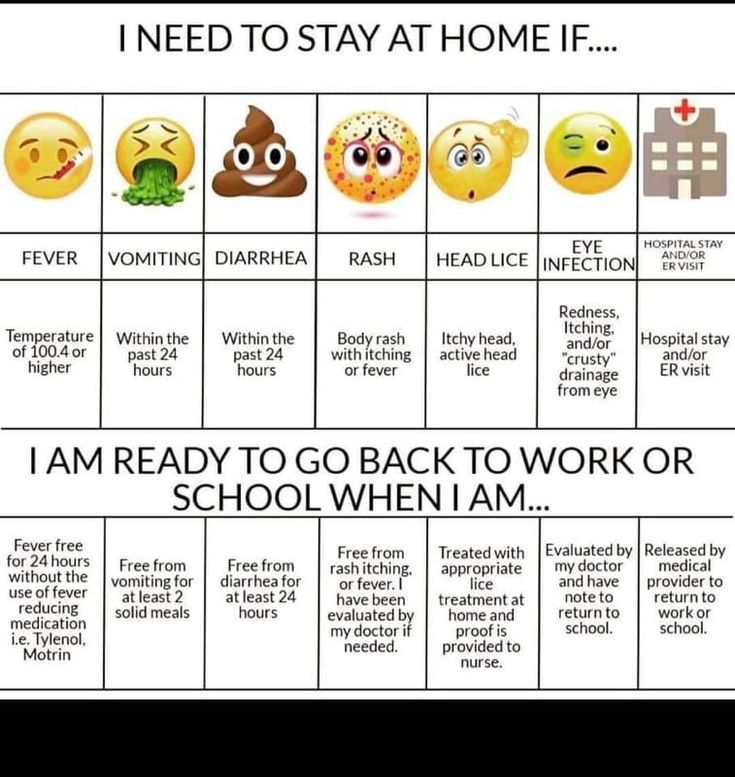 Very often, the temperature has a wave-like course: the temperature stays for 2-3 days, after which it decreases and stays at normal levels for 2-3 days, then rises again for 1-2 days and finally returns to normal. When the temperature rises, the child feels weakness, drowsiness, headache, nausea, and vomiting may occur. With a decrease in body temperature, all these symptoms disappear, but with a repeated increase, they may return. The cervical and submandibular lymph nodes also increase, as viruses multiply in them.
Very often, the temperature has a wave-like course: the temperature stays for 2-3 days, after which it decreases and stays at normal levels for 2-3 days, then rises again for 1-2 days and finally returns to normal. When the temperature rises, the child feels weakness, drowsiness, headache, nausea, and vomiting may occur. With a decrease in body temperature, all these symptoms disappear, but with a repeated increase, they may return. The cervical and submandibular lymph nodes also increase, as viruses multiply in them.
Depending on which organs are most affected, there are several forms of enterovirus infection. Enteroviruses can affect: the central and peripheral nervous systems, oropharyngeal mucosa, eye mucosa, skin, muscles, heart, intestinal mucosa, liver; in boys, testicular damage is possible.
When the mucous membrane of the oropharynx is affected, enterovirus angina develops. It is manifested by an increase in body temperature, general intoxication (weakness, headache, drowsiness) and the presence of a vesicular rash in the form of bubbles filled with liquid on the mucous membrane of the oropharynx and tonsils. These bubbles burst, in their place ulcers are formed, filled with white bloom. After recovery, no traces remain at the site of the sores.
These bubbles burst, in their place ulcers are formed, filled with white bloom. After recovery, no traces remain at the site of the sores.
When the eyes are affected, conjunctivitis develops. It can be one- or two-sided. It manifests itself in the form of photophobia, lacrimation, redness and swelling of the eyes. There may be hemorrhages in the conjunctiva of the eye.
With muscle damage, myositis develops - muscle pain. Pain appears on the background of an increase in temperature. Soreness is observed in the chest, arms and legs. The appearance of pain in the muscles, as well as temperature, can be undulating. When the body temperature decreases, the pain decreases or disappears completely.
With damage to the intestinal mucosa (enteritis), there is a liquid stool. Stools of normal color (yellow or brown), liquid, without pathological (mucus, blood) impurities. The appearance of loose stools can be both against the background of an increase in temperature, and isolated (without an increase in body temperature).
Enteroviral infections can affect various parts of the heart. So, if the muscle layer is damaged, myocarditis develops, if the inner layer is damaged with capture of the heart valves, endocarditis develops, if the outer shell of the heart is damaged, pericarditis develops. The child may experience: increased fatigue, weakness, palpitations, drop in blood pressure, rhythm disturbances (blockade, extrasystoles), pain behind the sternum.
With damage to the nervous system, encephalitis, meningitis can develop. The child has: severe headache, nausea, vomiting, fever, convulsions, paresis and paralysis, loss of consciousness.
With liver damage, acute hepatitis develops. It is characterized by an increase in the liver, a feeling of heaviness in the right hypochondrium, pain in this place. Perhaps the appearance of nausea, heartburn, weakness, fever.
When the skin is damaged, exanthema may appear - hyperemia (red coloration) of the skin, most often on the upper half of the body (head, chest, arms), does not rise above the level of the skin, appears simultaneously.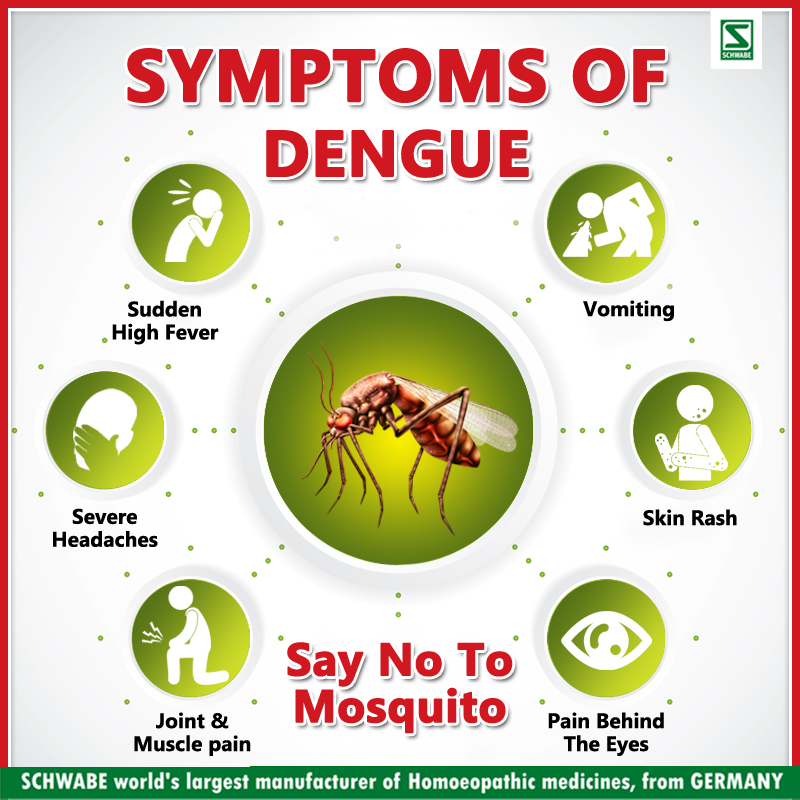
Boys may have inflammation in the testicles with the development of morchitis. Most often, this condition develops 2-3 weeks after the onset of the disease with other manifestations (tonsillitis, loose stools, and others). The disease passes quite quickly and does not bear any consequences, however, in rare cases, the development of aspermia (lack of sperm) in adulthood is possible.
There are also congenital forms of enterovirus infection, when viruses enter the child's body through the placenta from the mother. Usually, this condition has a benign course and is cured on its own, however, in some cases, an enterovirus infection can cause an abortion (miscarriage) and the development of a sudden death syndrome in a child (the death of a child occurs against the background of complete health).
Very rarely, damage to the kidneys, pancreas, lungs is possible. The defeat of various organs and systems can be observed both isolated and combined.
Treatment of enterovirus infection
There is no specific treatment for enterovirus infection. Treatment is carried out at home, hospitalization is indicated in the presence of damage to the nervous system, heart, high temperature, which cannot be reduced for a long time when using antipyretics. The child is shown bed rest for the entire period of fever.
Treatment is carried out at home, hospitalization is indicated in the presence of damage to the nervous system, heart, high temperature, which cannot be reduced for a long time when using antipyretics. The child is shown bed rest for the entire period of fever.
Meals should be light, rich in proteins. A sufficient amount of liquid is needed: boiled water, mineral water without gases, compotes, juices, fruit drinks.
Treatment is carried out symptomatically, depending on the manifestations of the infection - tonsillitis, conjunctivitis, myositis, loose stools, heart damage, encephalitis, meningitis, hepatitis, exanthema, orchitis. In some cases (tonsillitis, diarrhea, conjunctivitis ...) bacterial complications are prevented.
Children are isolated for the entire period of the disease. In the children's team may be after the disappearance of all symptoms of the disease.
Prevention of enterovirus infection.
For prevention, it is necessary to observe the rules of personal hygiene: wash hands after going to the toilet, walking on the street, drinking only boiled water or water from a factory bottle, it is unacceptable to use water from an open source (river, lake) to drink a child.