How much is a placenta
What is your Placenta Worth?
Home » News » What is your Placenta Worth?
March 2019
Russ Schweizer, CEO of AmnioChor
Unique, to say the least
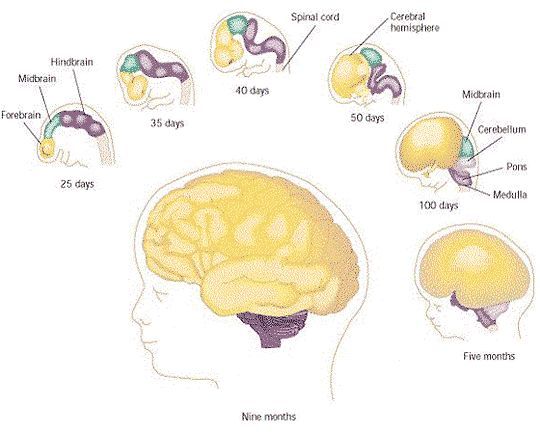
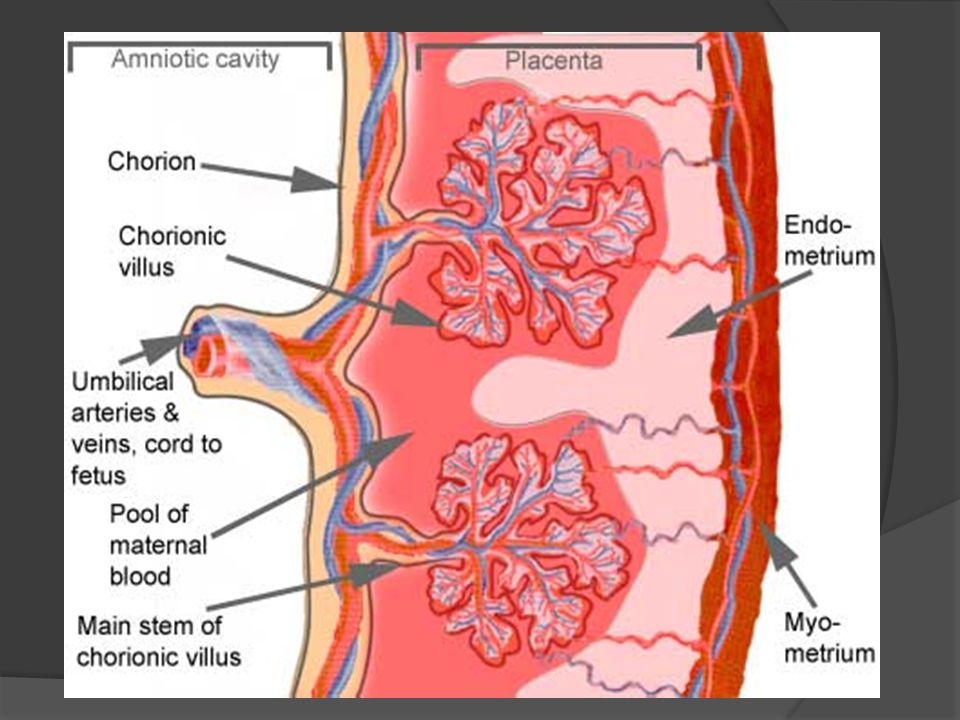
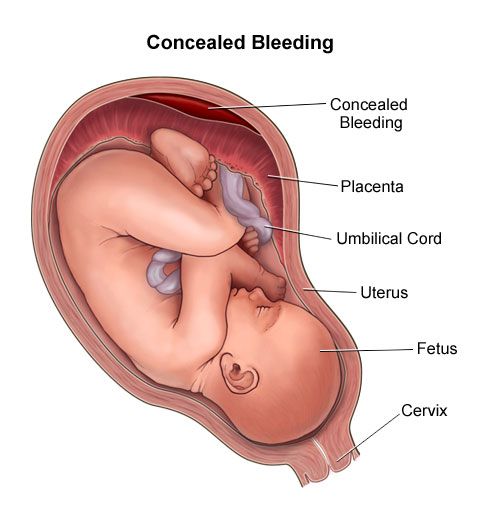
The placenta remains the least understood human organ. But thanks to organizations like The Centre For Trophoblast Research1, and scientists like Professor Y.W. Loke of Cambridge University2, we are beginning to understand the flawless organization and intricate performance of our placenta. For example, few people are aware that the placenta is derived from the baby. It becomes closely embedded in the mother’s womb such that the baby can “borrow” everything it needs to develop1. We are learning that many of the medical problems encountered later in life are a direct result of placenta dysfunction2. The hope is that a better understanding of the placenta will lead to broader knowledge in other critical areas of healthcare.
The Placenta’s 2nd Life
Your placenta can continue to provide therapeutic value and have a 2nd life if the afterbirth is not discarded as medical waste. Components isolated from the placenta, such as the umbilical cord blood, and the amniotic membrane, are already serving a valuable role in medicine today. Research continues to develop the therapeutic value of other components of the placenta. With our skills in cryopreservation, your placenta can be preserved for future applications in personalized medicine. The placenta’s 2nd life encompasses new treatments today and bio-banking for the future. We are rapidly moving into a new paradigm where the placenta is transitioning from biological waste to becoming a biological toolbox for cures.
Therapies for Today and Tomorrow
We consider the following to be the therapeutic components of the placenta, either today or tomorrow:
- Cord/Placental blood – Over 35,000 cord blood transplants have been performed worldwide3, with thousands more joining the list each year4.
 Cord blood transplants comprise living cells and are performed under FDA approval.
Cord blood transplants comprise living cells and are performed under FDA approval. - Amniotic Membrane of the Placenta (AMP) – Both viable (living) and non-viable (freeze dried) AMP tissue products are used every day as skin substitutes for wound care. AMP products also have well-established applications in ophthalmology, orthopedics, gynecology and urology.
- Mesenchymal stem/stromal cells (MSC’s) can be derived from the tissue of the placenta, amnion, and chorion, as well as the Wharton’s Jelly that fills the body of the umbilical cord. There are currently about 150 new clinical trials each year that utilize MSC for regenerative medicine5, and perinatal tissues provide the largest percentage of MSC in clinical trials6.
- Epithelial stem cells are found in the amnion. They are precursors to growing skin and have cell markers similar to pluripotent stem cells.
- Endothelial cells – These are derived from the lining of blood vessels in the umbilical cord and are currently studied for applications in vascular diseases.

- Extracellular Matrix (ECM) of the placenta has value as a decellularized scaffold material for biological engineering.
- Chorion tissue – Like the AMP, chorion tissue isolated from the placental sac has been used whole in wound care products.
- Umbilical Cord Tissue – Thicker and stronger than AMP, this tissue can be used in surgical applications as an allograft or stent wrap.
- Conditioned Media – There are numerous beneficial factors that are secreted by perinatal cells and tissues, including cytokines, hyaluronic acid, growth factors, etc.
The Placenta Paradigm Shift
As we become mindful of the placenta’s broader therapeutic future, organizations that collect birth tissues have become more ‘whole placenta’ minded. We need to isolate and utilize as much of the placenta as possible for research, clinical study, and current product fulfillment. However, distribution is typically fragmented, and many companies justifiably focus on only one type of product, so consequently there is waste. Also, the ability to successfully cryopreserve several of these components, such as ECM, is still in development.
Also, the ability to successfully cryopreserve several of these components, such as ECM, is still in development.
Hype will always precede the commercialization of a breakthrough technology, and placenta-based products and therapies are no exception. Saving a life is certainly priceless and cannot be monetized, but today thousands of dollars in value are being attached to placenta donations. When we include our AmnioChor model of bio-banking for future use, the placenta becomes the gift that will keep on giving.
Placenta Valuation
We know that falsely marketed products and treatments are running rampant today and people are getting wealthy at the expense of the good name of the placenta. An accurate valuation of what your placenta is worth must include the following considerations:
- By AmnioChor's estimate, the AMP market, which is a significant contributor to placenta value today, will grow to over $600M in 2020. Although insurance reimbursement exists for many AMP products, at present these products are only sourced from donations of C-Section placentas.
- The price of placenta products is driven up by the multi-tiered structure of the procurement chain: One company collects birth tissues, a second company manufactures products, and a third delivers them as therapy.
- The laboratory processing of the placenta is highly variable right now, can be costly, and this will continue for quite some time as new methods and efficiencies are developed.
- Valuation of the placenta should contemplate both today and tomorrow products. The ability to bank placenta tissue and cells and derive multiple personalized therapies will drive the valuation higher, but the costs of tomorrow products are obviously not yet known.
- We are dealing with potentially lifesaving products in a market that today is largely an unregulated ‘what-the-market-will-bear’ environment. Tomorrow’s market will be more regulated and FDA compliance will lead to higher product costs.
- As therapeutic benefits are realized, we believe that more placenta products will be covered by insurance reimbursement, and this will drive a leveling of the valuations.
- With any new technology there is great value fluctuation as the industry strives to achieve economy of scale and cost effectiveness. Hence we caution against runaway inflation of placenta valuations.
Given all these caveats, we estimate a conservative street value of the placenta today at around $50,000, and that could double or triple in five to ten years.
A recent blog by Dr. Chris Centeno placed the value of all afterbirth products at over half a million dollars per birth7. However, the majority of that high valuation was driven by amniotic fluid, which we do not include here. Although research indicates that amniotic fluid can be collected on a large scale during C-section births and contains valuable cells, the cells are present at low concentrations compared to cells isolated from cord blood or perinatal tissues8.
How to Incentivize Placenta Donors
Donation is the backbone of life saving organ and stem cell transplants as well as regenerative medicine.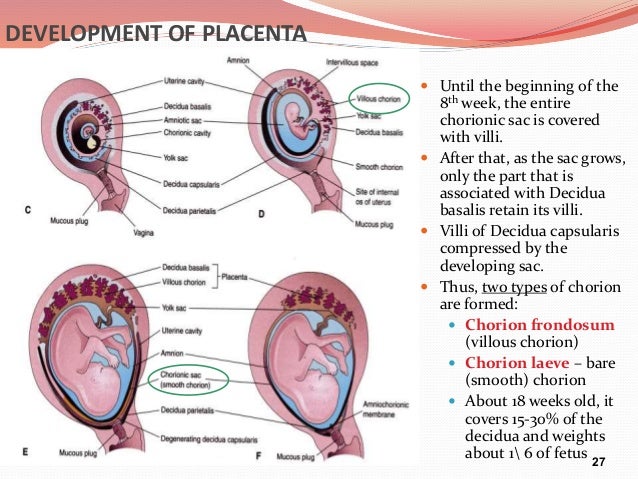 To stifle that caring and sharing human dynamic would be catastrophic. As a society we have an ethical responsibility to both advance medical technology and to further grow donation networks to build the community transplant capacity that will save lives. Most people agree that providing mothers with an incentive to donate their placenta would be a good thing, if it is done in an ethical way.
To stifle that caring and sharing human dynamic would be catastrophic. As a society we have an ethical responsibility to both advance medical technology and to further grow donation networks to build the community transplant capacity that will save lives. Most people agree that providing mothers with an incentive to donate their placenta would be a good thing, if it is done in an ethical way.
We must be aware of The National Organ Transplant Act of 1984 (NOTA)9-11. NOTA made it illegal to compensate organ donors, but did not prevent payment for other forms of donations, such as blood, sperm, and eggs. Since the placenta is considered an organ, now and for the foreseeable future, financial compensation for placenta donation is illegal and carries stiff punishment for violation.
In lieu of financial compensation, some have suggested that donating mothers should receive a gift or service12. A better option is to give the donating mother something of substantial future value: storage of her child’s stem cells. What if we provide donors with a level of private banking at little to no cost? As a business there is an opportunity to leverage two capabilities: both donation for product development as well as personal storage for the family, and this can be done for multiple cell lineages found in the placenta and umbilical cord. When we achieve launch, AmnioChor will offer an Omnibank that operates on the philosophy to “leave no cell behind”.
What if we provide donors with a level of private banking at little to no cost? As a business there is an opportunity to leverage two capabilities: both donation for product development as well as personal storage for the family, and this can be done for multiple cell lineages found in the placenta and umbilical cord. When we achieve launch, AmnioChor will offer an Omnibank that operates on the philosophy to “leave no cell behind”.
Russ Schweizer serves as Chief Executive Officer in building AmnioChor, a biotech startup based in perinatal stem cell and tissue technologies. Employing their proprietary AmnioCept technology for the recovery of the human placenta, AmnioChor will transpose the organ’s paradigm from medical waste to medical wonder, and commence the human placenta’s second and everlasting life in providing therapies. AmnioChor’s whole placenta-focused business will create and develop many new paths to cures, made available to everyone. For more information, visit www. AmnioChor.com, or follow us on Twitter @AmnioChor or email [email protected].
AmnioChor.com, or follow us on Twitter @AmnioChor or email [email protected].
References
- Centre for Trophoblast Research
- Loke YW. Life’s Vital Link: The Astonishing Role of the Placenta Oxford University Press 2013; ISBN: 978-0199694518
- Ballen KK, Verter F, Kurtzberg J. Umbilical cord blood donation: public or private? Bone Marrow Transplantation 2015; 50:1271–1278
- World Marrow Donor Assocation
- CellTrials.org blog 31 March 2018: Counting Keywords is not Compiling Clinical Trials: Mesenchymal
- CellTrials.org data package: MSC Trials 2011-2018
- Centeno C. Regenexx blog 25 January 2019: What Are the Bioethics of Sourcing Birth Tissues and Selling Them for Huge Money?
- Moraghebi R, Kirkeby A, Chaves P, et al. Term amniotic fluid: an unexploited reserve of mesenchymal stromal cells for reprogramming and potential cell therapy applications Stem Cell Research & Therapy 2017; 8:190
- NIH Legislative History: National Organ Transplant Act
- National Living Donor Assistance Center: National Organ Transplant Act
- Wikipedia: National Organ Transplant Act of 1984
- Medium Magazine 25 July 2018: Should We Pay Mothers to Donate Placentas?
Placenta Donation is Organ Donation
Home » News » Placenta Donation is Organ Donation
November 2019
Parent's Guide to Cord Blood Foundation
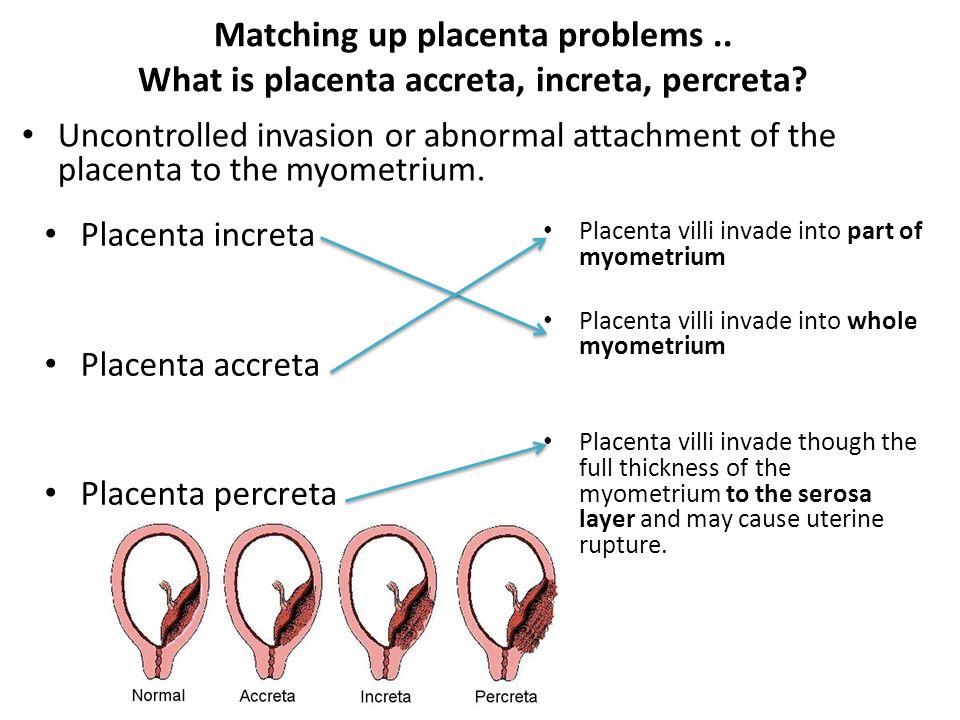
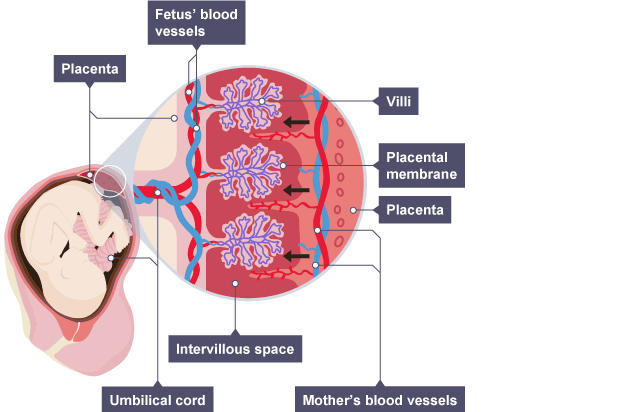
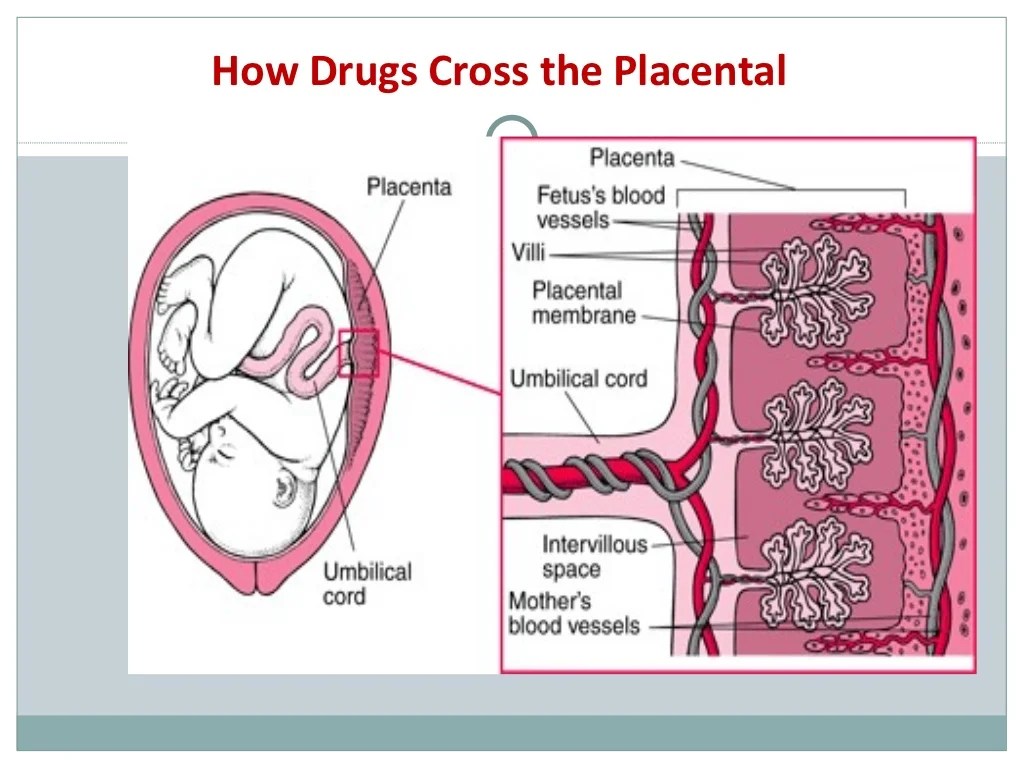
The placenta is considered to be an organ1. It is one of the most remarkable human organs, because it is only designed to survive over the course of pregnancy. The placenta’s purpose is to support and protect the baby in the womb. The mother and the baby have separate blood supplies, and the placenta enables the migration of nutrition and oxygen from the mother’s blood to the baby’s blood. Also important, the placenta mediates between their immune systems, so that the mother’s immune system does not recognize the baby as foreign and attack the baby with antibodies.
It is one of the most remarkable human organs, because it is only designed to survive over the course of pregnancy. The placenta’s purpose is to support and protect the baby in the womb. The mother and the baby have separate blood supplies, and the placenta enables the migration of nutrition and oxygen from the mother’s blood to the baby’s blood. Also important, the placenta mediates between their immune systems, so that the mother’s immune system does not recognize the baby as foreign and attack the baby with antibodies.
Many people reading this article may have a little “organ donor” symbol on their driver’s license, signaling that in the event of death they want to donate their organs, tissues, and eyes. Our society has a very positive attitude towards organ donation; most people consider it a gift to save or enhance lives. Some countries have passed laws ruling that organ donation is the presumed choice upon death, unless the individual opts out2.
But some recent media reports have demonized placenta donations3,4. They have told the story of a mother giving consent on the operating table, they have assumed that the donations are funneled to unregulated stem cell clinics, and they have implied that it is wrong for procurement organizations to make money from tissue that was donated for free. Let’s take a deeper look at the similarities and differences between placenta donation and organ donation.
They have told the story of a mother giving consent on the operating table, they have assumed that the donations are funneled to unregulated stem cell clinics, and they have implied that it is wrong for procurement organizations to make money from tissue that was donated for free. Let’s take a deeper look at the similarities and differences between placenta donation and organ donation.
In the United States, we have a network of regional “Organ Procurement Organizations” (OPOs) that collect organs, tissues, and eyes from deceased donors5. We also have a national organization named United Network for Organ Sharing (UNOS) that assigns transplantable organs to patients on the waiting list6. As a result of this network, 2018 was the 6th consecutive year in which organ transplants broke previous records: there were 145 million adults registered to donate, there were over 113,000 patients on the wait list, donations were made by 10,722 deceased donors and 6,831 living donors, but over 5,800 patients on the wait list died6.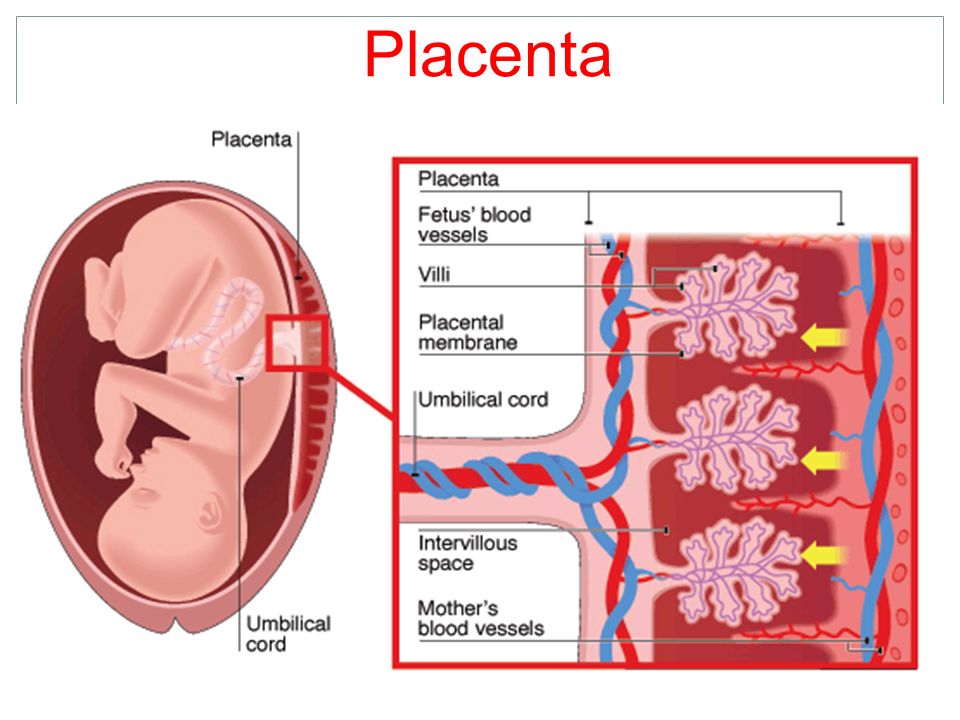 In 2019 there has been a court battle over changes to the rules of organ allocation, changes that hopefully will save more lives, but will also cause financial losses to some transplant hospitals7.
In 2019 there has been a court battle over changes to the rules of organ allocation, changes that hopefully will save more lives, but will also cause financial losses to some transplant hospitals7.
It is well known that organ transplants are very expensive, in terms of charges billed by the hospital to the patient’s insurance. The accompanying graphic shows the average charge per type of transplant, based on 2017 data researched by Milliman8 and presented in Fortune9. Some of the billed charges go to reimburse the OPO that provided the organ(s).
At present, there are over 50 OPOs operating in the United States that are accredited by the agency AOPO5. Parent’s Guide to Cord Blood Foundation looked up the most recently filed IRS financials for 43 of these OPOs that are registered as non-profits. Their annual revenue ranged from $5.4 to $376 million, and averaged $47 million. The assets of these OPOs averaged $46 million. It requires highly trained staff and advanced laboratory facilities to operate a successful OPO, which justifies the big budgets of the most highly accredited organizations.
How does placenta donation compare to organ donation? We have prepared a table that compares the steps to each process, and demonstrates that medically they are very similar. Parent’s Guide to Cord Blood Foundation is aware of at least 20 organizations that are collecting placenta donations in the United States. We were not able to summarize their financials, because most of them are subsidiaries of larger organizations: either they are part of a pharma company that develops products from the placenta, or they are a program at one of the non-profit OPOs that we have already described.
Procurement | Placenta Donation | Organs, Tissues, & Eyes from Deceased Donors |
Timing of Consent | Mother should not be in labor or under the influence of medication15 | Either donor registered before death or immediate family member gives consent15 |
Alternative fate of the organ | Discarded as medical waste. | Disposed by donor family. |
Checks on donor health | Questionnaire & Maternal blood test15 | Questionnaire if possible & Donor blood test15 |
Testing of the organ | Checked for diseases & external sterility15 | Checked for diseases & external sterility15 |
Handling and processing | Laboratory meets cGMP standards. | Organs tested in hospital. Tissues and eyes go to laboratory that meets cGMP standards. |
Time window from recovery to produce viable product | Within 48 hours | Some organs must be transplanted within a few hours. |
Medical products | Amniotic membrane, tissue matrix, tissue fragments. Cells that are Mesenchymal, Epithelial, Endothelial. Various combinations of the above. | Transplantable organs & corneas. |
Product applications that are already standard of care | Eye diseases and surgery. Wound dressings. Nerve wraps. Dental implants. Enhanced surgical recovery. Scar prevention. | Transplants of organs & corneas. Grafts of bone, tendons, ligaments. |
Research to increase clinical applications | Trials16 of perinatal stem cells for auto-immune diseases, neurologic disorders, and orthopedic procedures, among others. | Organ perfusion17,18 to keep the organ viable longer. Transplants19 that combine the organ with stem cells from donor bone marrow to decrease rejection. |
Examples of financial value | Public banks charge $36K to release donated cord blood13. The estimated value of a placenta is $50K14. | Health insurance companies pay8,9 $1. |
Lives impacted in USA | Potential use: diabetic foot ulcers20-22 about 1 million per year; corneal ulcers23-25 about 34,000 per year. | 10,722 deceased donor organ transplants6 in 2018, over 1.5 million musculoskeletal allografts26 per year. |
In a recent article about placenta donation titled, The Afterlife of the Afterbirth, a bioethicist at the University of Minnesota told MedPage Today4: "What if women were given the full account, that some biobank is going to acquire it, process it, assign it value, and then it's going to be marked up and sold again…. Some women might think twice."
As part of informed consent, mothers giving birth should receive a full account of how their placenta donation might be used. It is illegal for the mother or her healthcare provider to be offered any financial incentive to donate.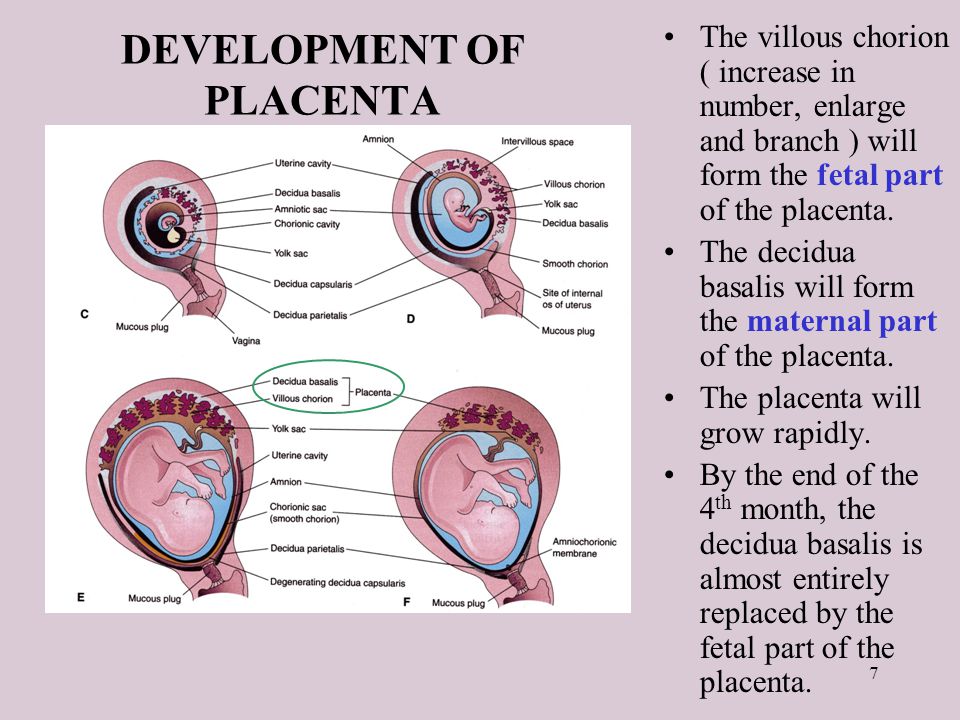 Accreditation standards require that the mother should not be in active labor or under the influence of drugs at the time of informed consent15. But it is unreasonable to expect that a biobank can acquire a donation, process it, and release it for patients without charging for their services. That is how procurement organizations stay in business and make it possible for patients to receive transplants and grafts of donated tissue.
Accreditation standards require that the mother should not be in active labor or under the influence of drugs at the time of informed consent15. But it is unreasonable to expect that a biobank can acquire a donation, process it, and release it for patients without charging for their services. That is how procurement organizations stay in business and make it possible for patients to receive transplants and grafts of donated tissue.
The OPO industry used to have a problem with the perception that donated body parts get “marked up and sold again”. Back in 2012 the website MedicalTranscription.net provided data for an Infographic about organ values that was titled You Are Worth More Dead Than Alive10. Since it first appeared on the internet, this graphic has been reproduced and quoted in the media countless times. The OPO industry overcame that negative perception by producing lots of educational materials that emphasized the lives saved and the patient benefits realized from organ donations. For example, we have embedded an animated video from the US government promoting organ donation that was uploaded in Sept 201911. Nowhere over the course of this 5 minute video is anything shown about the finances involved. The entire focus is on saving lives.
For example, we have embedded an animated video from the US government promoting organ donation that was uploaded in Sept 201911. Nowhere over the course of this 5 minute video is anything shown about the finances involved. The entire focus is on saving lives.
This is the bottom line throughout the industries that process medical donations. It costs a lot of money to test and prepare donations for patients, and in the end the supplier must be reimbursed. When the Red Cross delivers blood transfusions to a hospital, they are paid for the product12. When Be The Match releases donated cord blood for a transplant, they get paid13. When OPOs provide organs for transplant, they get paid5-10. And yes, when companies provide products made from donated placentas, they are also paid14.
Placenta donation deserves the same respect accorded to donations of organs, tissues, and eyes. There are numerous medical products manufactured from placentas that are routinely used in FDA-approved treatments and clinical trials (see the table). The birth tissue industry has to push back against the media perception that placenta donation is a scam perpetuated on mothers at a vulnerable time. They need to produce more educational materials about how patients are helped by the donations, and stress their adherence to quality guidelines around informed consent and handling of tissues. Through improved public education, hopefully placenta donation will come to be regarded in the same positive light as organ donation.
DOWNLOAD this article as a pdf file.
References
- Loke YW. Life’s Vital Link: The Astonishing Role of the Placenta Oxford University Press 2013; ISBN: 978-0199694518
- Willis BH, Quigley M. Opt-out organ donation: on evidence and public policy.
 J R Soc Med. 2014; 107(2): 56–60.
J R Soc Med. 2014; 107(2): 56–60. - Chen C. The Birth-Tissue Profiteers. 7 May 2019. ProPublica
- Fiore K. The Afterlife of Afterbirth - Placenta donations may be feeding stem-cell scams. 15 Oct. 2019. MedPage Today
- Association of Organ Procurement Organizations (AOPO)
- United Network for Organ Sharing (UNOS)
- Farmer B. As Thousands Wait For Transplants, Medical Centers Fight To Keep Livers Close To Home. 14 May 2019. NPR All Things Considered
- Bentley TS, Phillips SJ. 2017 U.S. organ and tissue transplant cost estimates and discussion. 3 August 2017. Milliman Research Report
- Rapp N, VanderMey A. Here’s What Every Organ in the Body Would Cost to Transplant. 14 Sept. 2017. Fortune
- You Are Worth More Dead Than Alive. MedicalTranscription.net 2012. [Infographic]
- OrganDonor.gov (U.S. Government Information on Organ Donation and Transplantation) Organ Donation and Transplantation: How Does it Work? 2019. [Video]
- American Red Cross.
 What happens to donated blood? 2019. [Video]
What happens to donated blood? 2019. [Video] - Kapinos KA, Briscombe B, Gracner T, Strong A, Whaley C, Hoch E, Hlavka JP, Case SR, Chen PG. Challenges to the Sustainability of the U.S. Public Cord Blood System. 29 Sept. 2017. RAND Research Report
- Schweizer R. What is your Placenta Worth? 2019; Parent’s Guide to Cord Blood Foundation. March 2019 newsletter
- American Association of Tissue Banks (AATB) Guidance Documents
- Couto PS, Bersenev A, Verter F. The first decade of advanced cell therapy clinical trials using perinatal cells (2005–2015). Regenerative Medicine 2017; 12(8):953-968
- Pan X, Yang J, Fu S, Zhao H. Application of ex vivo lung perfusion (EVLP) in lung transplantation. J Thorac Dis. 2018; 10(7):4637-4642.
- Ex Vivo Lung Perfusion (EVLP) - webpage for patients from Penn Medicine
- Leventhal J, Abecassis M, Miller J, Gallon L, Ravindra K, Tollerud DJ, King B, Elliott MJ, Herzig G, Herzig R, Ildstad ST. Chimerism and Tolerance Without GVHD or Engraftment Syndrome in HLA-Mismatched Combined Kidney and Hematopoietic Stem Cell Transplantation.
 Science Translational Medicine 2012; 4(124):124ra28
Science Translational Medicine 2012; 4(124):124ra28 - American Diabetes Association (ADA) Statistics About Diabetes
- DiabeticFootOnline - 1 Day with #Diabetes in USA: Every 1.2 seconds someone develops a diabetic foot ulcer (DFU). From the Southwestern Academic Limb Salvage Alliance (SALSA). 2017.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. NEJM 2017; 376:2367-2375
- Holt Y. Amniotic Membrane uses in Ophthalmology. Parent’s Guide to Cord Blood Foundation. September 2017 newsletter
- Cason JB. Amniotic Membrane Transplant. American Association of Ophthalmology. 19 August 2019. EyeWiki
- Chang DC & Fusarium Keratitis Investigation Team. Multistate Outbreak of Fusarium Keratitis Associated With Use of a Contact Lens Solution. (34M people wear contacts USA, incidence microbial keratitis 5-21 per 10,000). JAMA. 2006; 296(8):953-963.
- Giedraitis A, Arnoczky SP, Bedi A. Allografts in Soft Tissue Reconstructive Procedures.
 Sports Health. 2014; 6(3):256–264.
Sports Health. 2014; 6(3):256–264.
What to do with the placenta? 10 uses
The placenta (baby place, afterbirth, storage) is a unique organ. It appears only for 8-9 months to provide the unborn child with oxygen and all the necessary nutrients, but after the third stage of labor it becomes unnecessary. What can be done with the placenta after the doctor examined it and said that everything is in order? There are at least 10 options, and each has its supporters.
Eat. This is exactly what female placental mammals do after giving birth, even herbivores. After all, the afterbirth contains many valuable nutrients, and after giving birth in the wild, you need to restore strength as soon as possible in order to be able to run and get food again.
Women still do this too, especially in parts of Asia. Some experts recommend eating the placenta for the prevention of postpartum depression and anemia. However, in our time, placentophagy has acquired many exotic forms: since it is rather problematic for a civilized person to simply eat a raw afterbirth, as in the wild, the placenta is either heat-treated, like ordinary meat, or smoothies are prepared, or encapsulated.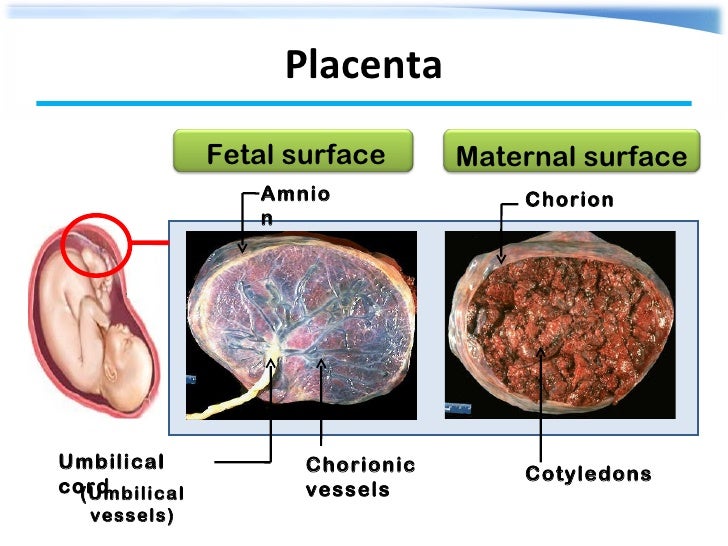 To do this, the placenta must be steam-dried, turned into powder, and then taken in the form of capsules. Of course, only those who have the appropriate technical capabilities resort to such methods. However, you should be aware of the risks: the placenta contains hormones, is not sterile, and may even be infected.
To do this, the placenta must be steam-dried, turned into powder, and then taken in the form of capsules. Of course, only those who have the appropriate technical capabilities resort to such methods. However, you should be aware of the risks: the placenta contains hormones, is not sterile, and may even be infected.
Bury. In our climatic latitudes, the placenta was most often buried in the ground. This could be accompanied by rituals: the placenta was washed, sprinkled with fragrant herbs, spices, put in an embroidered bag (they could cover it with a layer of wet clay and dry it so that it would not become food for wild animals), and only then they put it in a specially prepared hole - under the house, in a wasteland but most often under a tree. If a girl was born, the placenta was buried under a "female" tree - for example, an apple tree. If the family was replenished with a boy, the children's place was buried under a maple or oak tree so that the guy would grow up strong and powerful.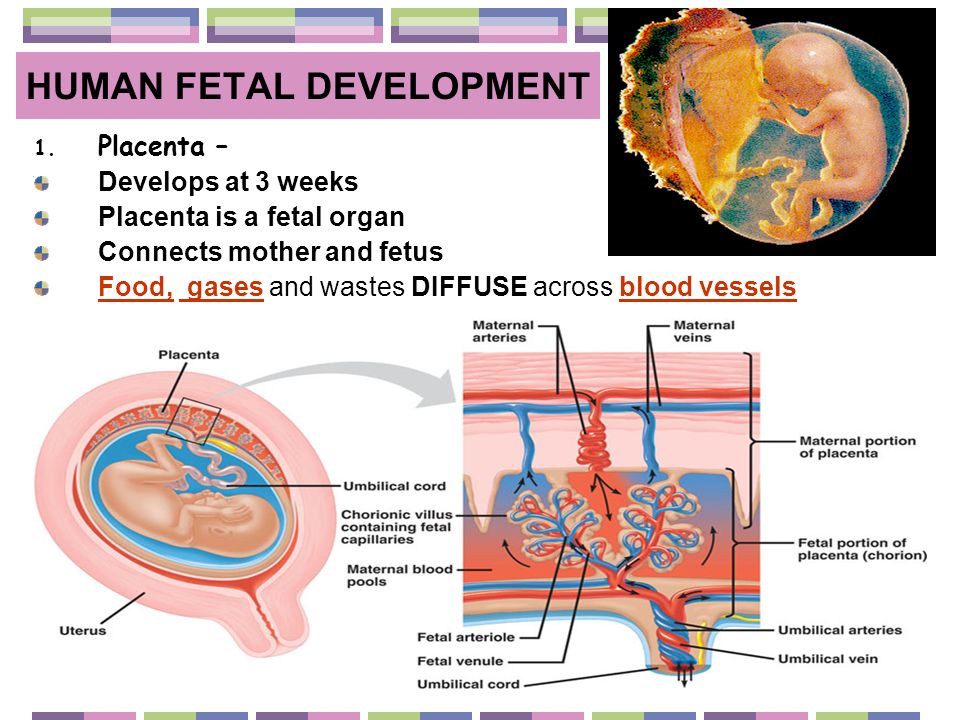 Nowadays, the placenta can be buried under the so-called "family tree" to ensure the baby's health and well-being, or they can simply be buried in a flower bed - they say, this is how flowers grow better.
Nowadays, the placenta can be buried under the so-called "family tree" to ensure the baby's health and well-being, or they can simply be buried in a flower bed - they say, this is how flowers grow better.
Bury. In some countries (particularly on the island of Bali), it is customary not just to bury the placenta, but to ritually hide it in a cemetery, believing that it is a living being.
Make a decoration. The placenta looks good in epoxy, so some women order a pendant, bracelet, ring or necklace from their own placenta from jewelers. Such decoration should symbolize the bond between mother and child.
Dry for memory. Dried placentas are sometimes used in art compositions or sewn into toys.
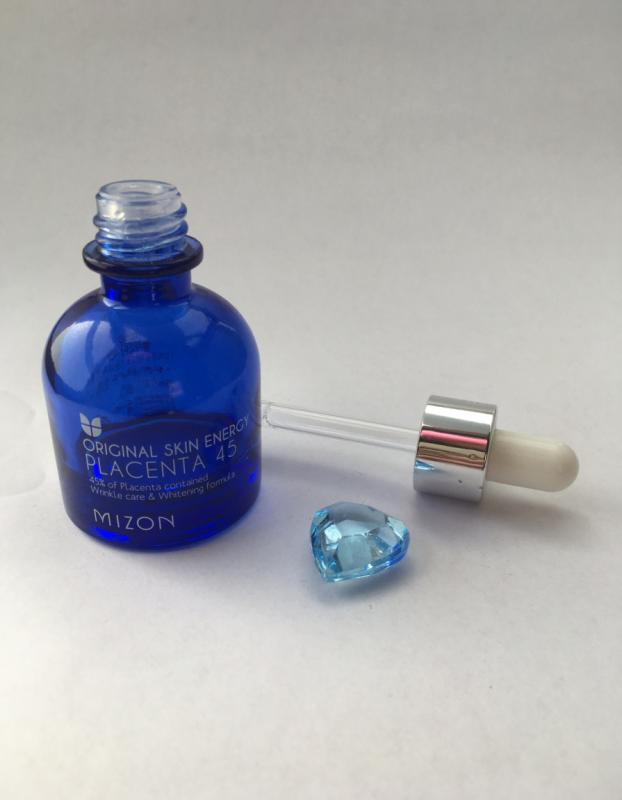
Sell. Cosmetics made using the placenta are very popular on the market - creams, gels, serums, shampoos, etc. Especially effective are products with a placenta in anti-aging cosmetology - because in this way you can stimulate the appearance of new cells, as well as activate the production of collagen and elastin, and the skin becomes more elastic.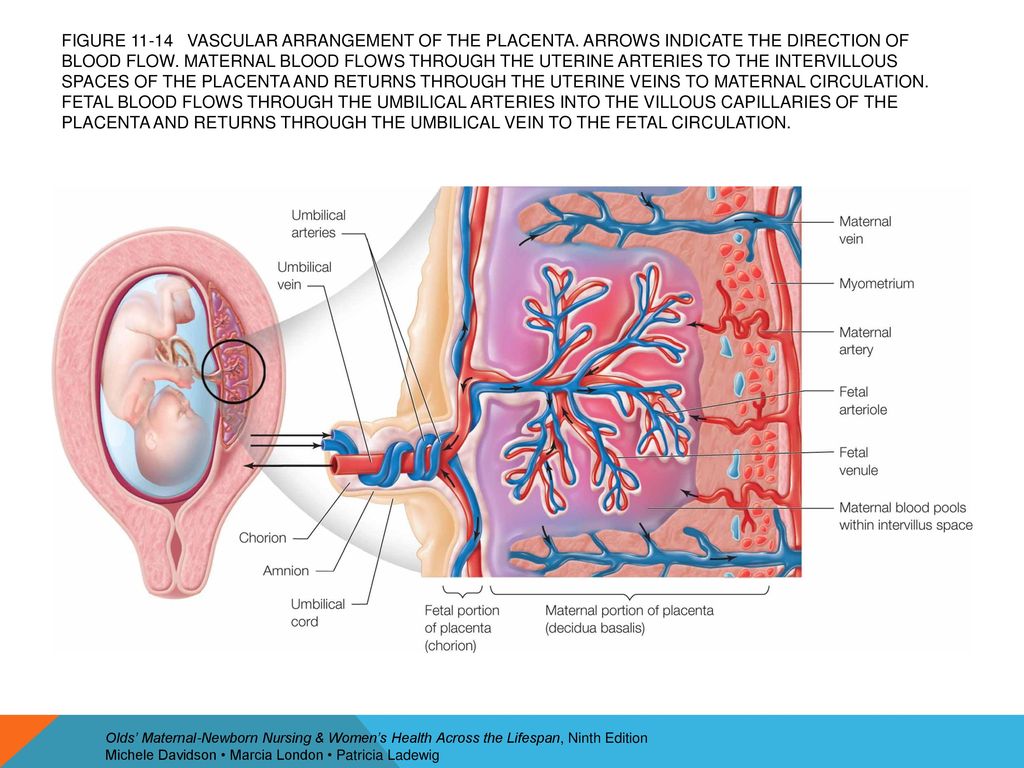 Therefore, some women sell their afterbirth. Although, of course, you won’t earn a lot of money this way.
Therefore, some women sell their afterbirth. Although, of course, you won’t earn a lot of money this way.
Use in homemade skin cream. However, a cream that will help heal the skin, reduce scars and stretch marks, and even heal sore or cracked nipples is even made independently. To do this, placenta powder is added to other components.
Dispose of. In Ukraine, this is the most common scenario for the development of events. Maternity hospitals are guided by a protocol for handling biowaste: after the completion of the third stage of labor, the placenta is examined and sent for freezing in a special chamber. When it is full, the placentas are taken for disposal - more often they are buried, less often they are burned.
Deposit in the cryobank. Today, the placenta - like cord blood - is used to isolate the most valuable mesenchymal stem cells. Even now, stem cells are successfully used for the treatment of various diseases and in cosmetology, this area is rightly called "medicine of the XXI century. " Therefore, such a “contribution” can be a very profitable investment in the health of the child and the longevity of the parents. Interestingly, stem cells are obtained from a smaller part of the placenta, from the amnion and chorion, which are genetically related to the child. The remains of the placenta can be used as the family decides, because everyone has their own opinion and traditions of the family.
" Therefore, such a “contribution” can be a very profitable investment in the health of the child and the longevity of the parents. Interestingly, stem cells are obtained from a smaller part of the placenta, from the amnion and chorion, which are genetically related to the child. The remains of the placenta can be used as the family decides, because everyone has their own opinion and traditions of the family.
Read also 10 unique facts about the placenta.
Nikki Reed
In 2017, the star of the vampire saga "Twilight" Nikki Reed and her husband Ian Somerhalder became the parents of a girl named Bodhi Soleil. After giving birth, the actress decided to transform the placenta into special capsules in order to use it as a biological supplement. Apparently, the pills lasted only a few months - at the end of the same year, a photo with a half-empty jar appeared on Reed's Instagram. In a message attached to the post, the actress noted that "every mom should do what she thinks will be good for her health.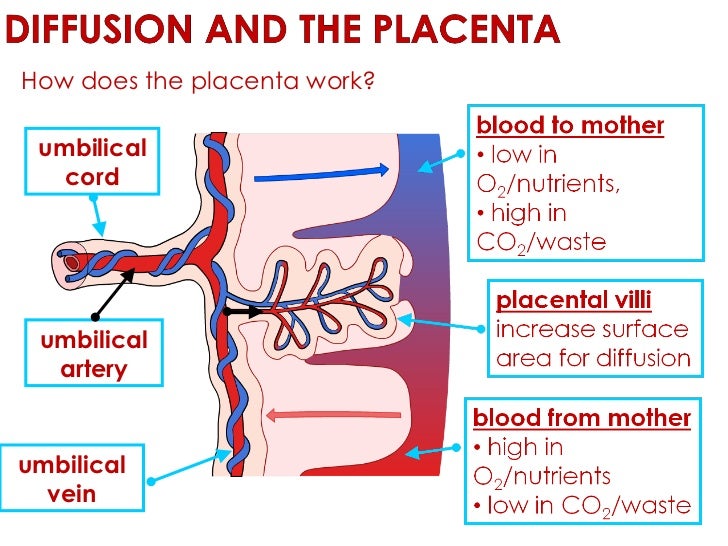 " However, she still did not advertise pills from the placenta.
" However, she still did not advertise pills from the placenta.
Hilary Duff
While recording a pregnancy health podcast, Lizzie Maguire actress Hilary Duff revealed that she decided to turn her daughter Banks Violet's placenta into a smoothie. Recall that the girl was born in October 2015.
"It was the most delicious cocktail I've ever had," the actress told podcast host Dr. Elliot Berlin. She also admitted that for a long time she was extremely skeptical about the idea of consuming the placenta, but decided to go on an experiment when she learned that postpartum depression could be prevented in this way.
Katherine Heigl
Comedian Katherine Heigl, known to many from the films "The Naked Truth" and "Knocked Up", also joined the list of celebrities who decided to use the placenta after the birth of a child. During her third pregnancy, Heigl worked extensively with a naturopath who urged her to encapsulate the organ.
During a conversation with People, the actress noted that immediately after the completion of the caesarean section, a man approached her and offered his services in the manufacture of capsules based on the placenta.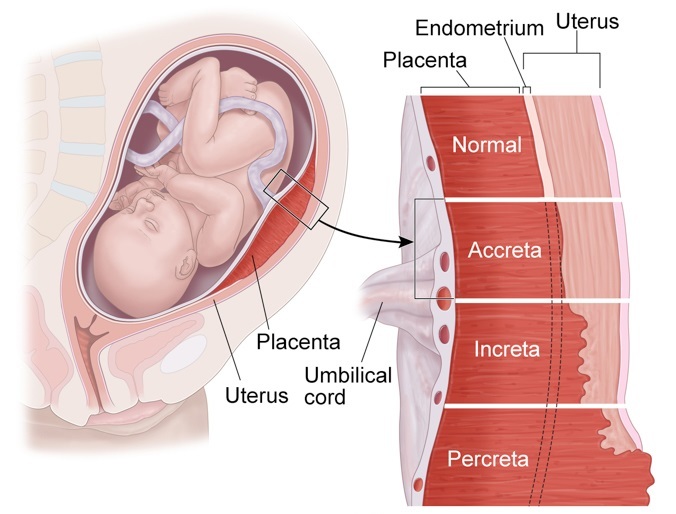 Apparently, some clinics already officially carry out such a service.
Apparently, some clinics already officially carry out such a service.
Alicia Silverstone
"Clueless" and "Batman & Robin" star Alicia Silverstone took placental capsules from the birth of her first and so far only daughter, Bear Blue. During a conversation with reporters, Silverstone admitted that she was not originally going to experiment with her health. The idea to encapsulate the placenta came from one of Alicia's fans, who gave her a bottle of pills as an exclusive gift. When asked if she enjoyed the experience, the actress stated that "it was love at first sight."
“I was very upset when they ended. These capsules really helped, ”said Silverstone.
Mayim Bialik
Star of the cult comedy series The Big Bang Theory, Mayim Bialik has come under fire after she publicly admitted to eating a placenta. Sheldon Cooper's on-screen sweetheart spoke about the experience of natural childbirth and breastfeeding in one of the popular health blogs.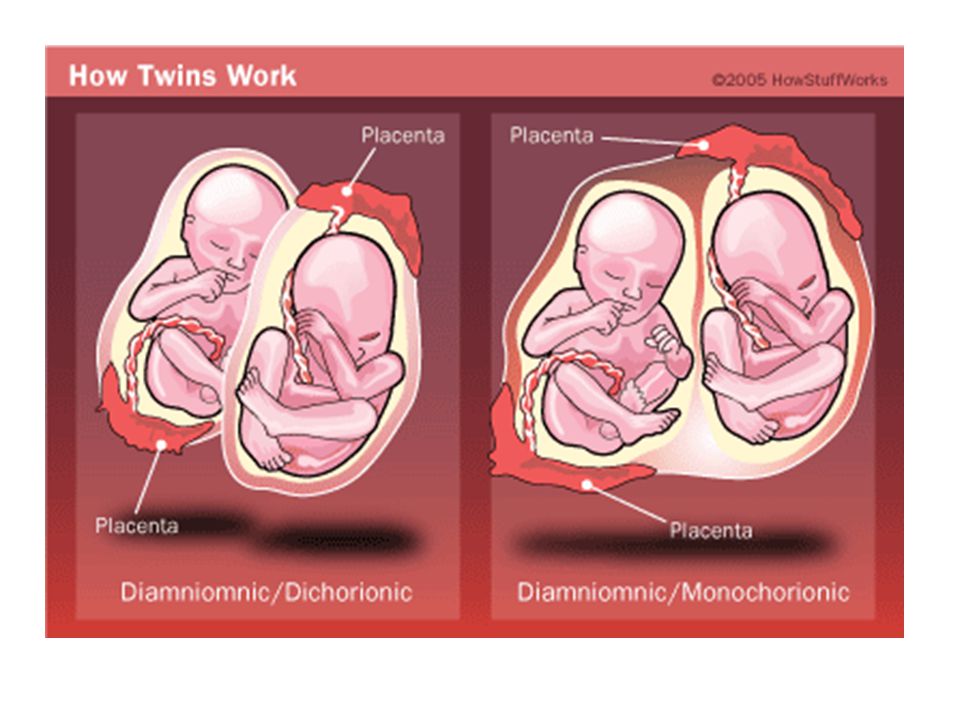
“Humans are the only mammals that choose not to eat the placenta. While in the animal kingdom it is still a natural process. Animals eat the placenta for an extra dose of protein and iron, which help the body recover from a difficult birth,” Bialik wrote.
January Jones
American actress January Jones of Mad Men fame has also come under public scrutiny after her decision to capsule her placenta. It happened in 2011, when the trend for the use of the placenta was not yet particularly relevant. So, ABC News released an entire article with the subtitle "Crazy Mom?", clearly alluding to the mental problems of the actress.
Nevertheless, January herself believes that it was the placenta that helped her quickly recover after childbirth. According to her, already seven weeks after the birth of her son Xander, she was able to return to active work.
Tom Cruise
The famous Hollywood actor Tom Cruise remains the only famous man who decided to use the placenta of his child.
 Grafts of bone, tendons, and ligaments. Stem cells from bone marrow.
Grafts of bone, tendons, and ligaments. Stem cells from bone marrow. 4M for heart transplant, $893K bone marrow transplant, $415K kidney, etc.
4M for heart transplant, $893K bone marrow transplant, $415K kidney, etc.