How long is the small intestine in a child
Your Digestive System (for Kids)
So there you are, sitting at lunch, enjoying some grilled-chicken pizza and a few orange wedges. When you're finished, you take a last drink of milk, wipe your mouth, and head to your next class. In a few minutes you're thinking about the capital of Oregon or your science fair project. You've completely forgotten about that pizza lunch you just ate. But it's still in your stomach — sort of like a science experiment that happens all the time!
The Mouth Starts Everything Moving
Your digestive (say: dye-JES-tiv) system started working even before you took the first bite of your pizza. And the digestive system will be busy at work on your chewed-up lunch for the next few hours — or sometimes days, depending upon what you've eaten. This process, called digestion, allows your body to get the nutrients and energy it needs from the food you eat. So let's find out what's happening to that pizza, orange, and milk.
Even before you eat, when you smell a tasty food, see it, or think about it, digestion begins. Saliva (say: suh-LYE-vuh), or spit, begins to form in your mouth.
When you do eat, the saliva breaks down the chemicals in the food a bit, which helps make the food mushy and easy to swallow. Your tongue helps out, pushing the food around while you chew with your teeth. When you're ready to swallow, the tongue pushes a tiny bit of mushed-up food called a bolus (say: BO-luss) toward the back of your throat and into the opening of your esophagus, the second part of the digestive tract.
On the Way Down
The esophagus (say: ih-SOF-eh-guss) is like a stretchy pipe that's about 10 inches (25 centimeters) long. It moves food from the back of your throat to your stomach. But also at the back of your throat is your windpipe, which allows air to come in and out of your body. When you swallow a small ball of mushed-up food or liquids, a special flap called the epiglottis (say: ep-ih-GLOT-iss) flops down over the opening of your windpipe to make sure the food enters the esophagus and not the windpipe.
If you've ever drunk something too fast, started to cough, and heard someone say that your drink "went down the wrong way," the person meant that it went down your windpipe by mistake. This happens when the epiglottis doesn't have enough time to flop down, and you cough involuntarily (without thinking about it) to clear your windpipe.
Once food has entered the esophagus, it doesn't just drop right into your stomach. Instead, muscles in the walls of the esophagus move in a wavy way to slowly squeeze the food through the esophagus. This takes about 2 or 3 seconds.
See You in the Stomach
Your stomach, which is attached to the end of the esophagus, is a stretchy sack shaped like the letter J. It has three important jobs:
- to store the food you've eaten
- to break down the food into a liquidy mixture
- to slowly empty that liquidy mixture into the small intestine
The stomach is like a mixer, churning and mashing together all the small balls of food that came down the esophagus into smaller and smaller pieces. It does this with help from the strong muscles in the walls of the stomach and gastric (say: GAS-trik) juices that also come from the stomach's walls. In addition to breaking down food, gastric juices also help kill bacteria that might be in the eaten food.
It does this with help from the strong muscles in the walls of the stomach and gastric (say: GAS-trik) juices that also come from the stomach's walls. In addition to breaking down food, gastric juices also help kill bacteria that might be in the eaten food.
Onward to the small intestine!
22 Feet Isn't Small at All
The small intestine (say: in-TESS-tin) is a long tube that's about 1½ inches to 2 inches (about 3.5 to 5 centimeters) around, and it's packed inside you beneath your stomach. If you stretched out an adult's small intestine, it would be about 22 feet long (6.7 meters) — that's like 22 notebooks lined up end to end, all in a row!
The small intestine breaks down the food mixture even more so your body can absorb all the vitamins, minerals, proteins, carbohydrates, and fats. The grilled chicken on your pizza is full of proteins — and a little fat — and the small intestine can help extract them with a little help from three friends: the pancreas (say: PAN-kree-uss), liver, and gallbladder.
Those organs send different juices to the first part of the small intestine. These juices help to digest food and allow the body to absorb nutrients. The pancreas makes juices that help the body digest fats and protein. A juice from the liver called bile helps to absorb fats into the bloodstream. And the gallbladder serves as a warehouse for bile, storing it until the body needs it.
Your food may spend as long as 4 hours in the small intestine and will become a very thin, watery mixture. It's time well spent because, at the end of the journey, the nutrients from your pizza, orange, and milk can pass from the intestine into the blood. Once in the blood, your body is closer to benefiting from the complex carbohydrates in the pizza crust, the vitamin C in your orange, the protein in the chicken, and the calcium in your milk.
Next stop for these nutrients: the liver! And the leftover waste — parts of the food that your body can't use — goes on to the large intestine.
Love Your Liver
The nutrient-rich blood comes directly to the liver for processing.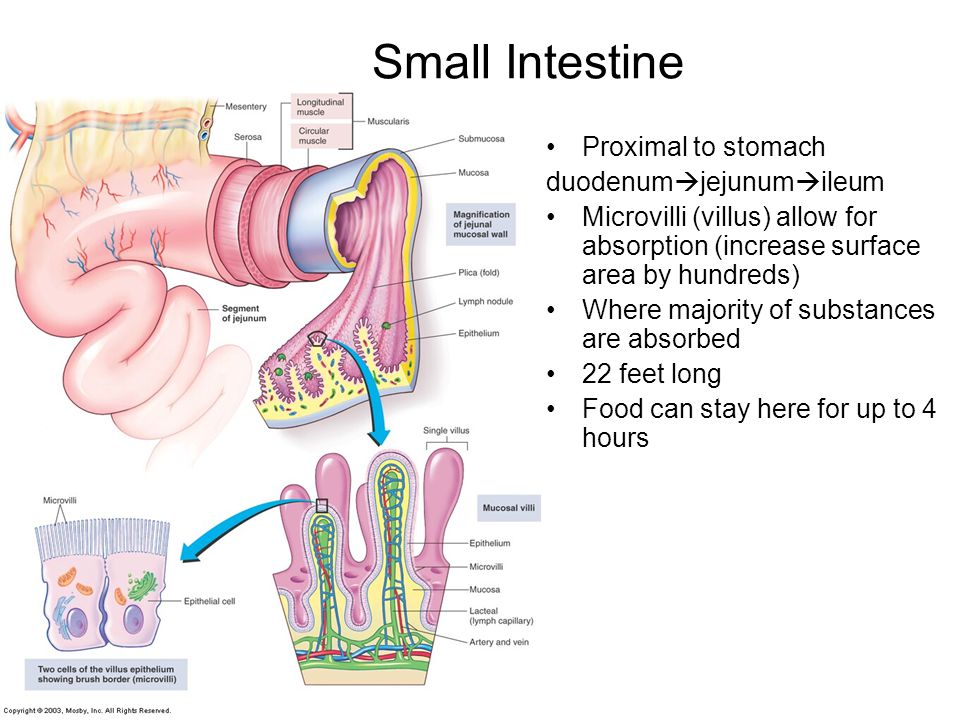 The liver filters out harmful substances or wastes, turning some of the waste into more bile. The liver even helps figure out how many nutrients will go to the rest of the body, and how many will stay behind in storage. For example, the liver stores certain vitamins and a type of sugar your body uses for energy.
The liver filters out harmful substances or wastes, turning some of the waste into more bile. The liver even helps figure out how many nutrients will go to the rest of the body, and how many will stay behind in storage. For example, the liver stores certain vitamins and a type of sugar your body uses for energy.
That's One Large Intestine
At 3 or 4 inches around (about 7 to 10 centimeters), the large intestine is fatter than the small intestine and it's almost the last stop on the digestive tract. Like the small intestine, it is packed into the body, and would measure 5 feet (about 1.5 meters) long if you spread it out.
The large intestine has a tiny tube with a closed end coming off it called the appendix (say: uh-PEN-dix). It's part of the digestive tract, but it doesn't seem to do anything, though it can cause big problems because it sometimes gets infected and needs to be removed.
Like we mentioned, after most of the nutrients are removed from the food mixture there is waste left over — stuff your body can't use. This stuff needs to be passed out of the body. Can you guess where it ends up? Well, here's a hint: It goes out with a flush.
This stuff needs to be passed out of the body. Can you guess where it ends up? Well, here's a hint: It goes out with a flush.
Before it goes, it passes through the part of the large intestine called the colon (say: CO-lun), which is where the body gets its last chance to absorb the water and some minerals into the blood. As the water leaves the waste product, what's left gets harder and harder as it keeps moving along, until it becomes a solid. Yep, it's poop (also called stool or a bowel movement).
The large intestine pushes the poop into the rectum (say: REK-tum), the very last stop on the digestive tract. The solid waste stays here until you are ready to go to the bathroom. When you go to the bathroom, you are getting rid of this solid waste by pushing it through the anus (say: AY-nus). There's the flush we were talking about!
Dig That Digestive System
You can help your digestive system by drinking water and eating a healthy diet that includes foods rich in fiber.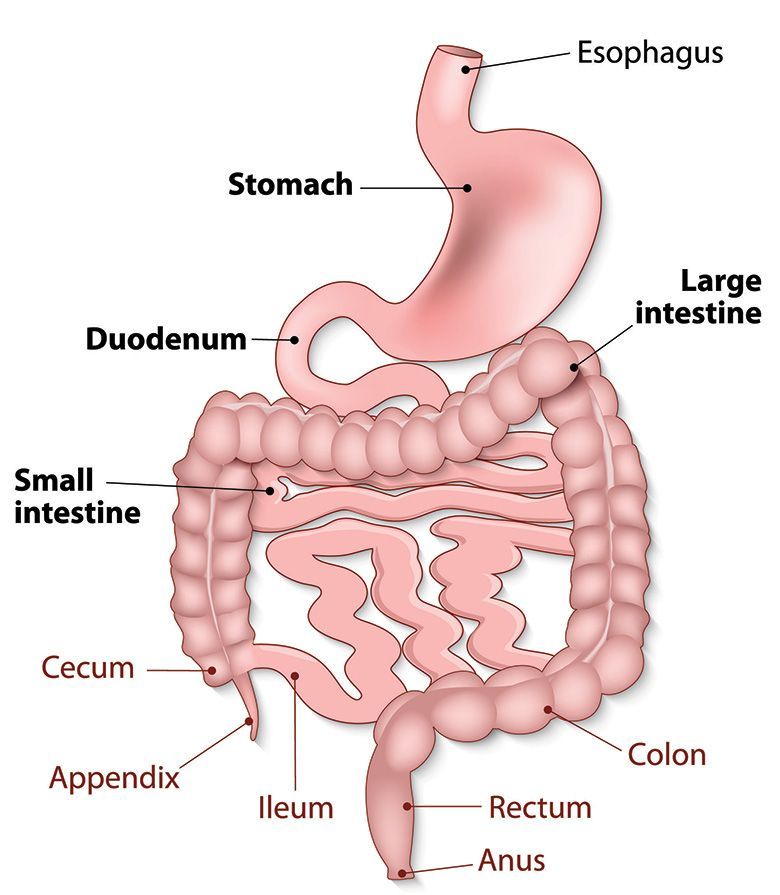 High-fiber foods, like fruits, vegetables, and whole grains, make it easier for poop to pass through your system.
High-fiber foods, like fruits, vegetables, and whole grains, make it easier for poop to pass through your system.
The digestive system is a pretty important part of your body. Without it, you couldn't get the nutrients you need to grow properly and stay healthy. And next time you sit down to lunch, you'll know where your food goes — from start to finish!
Small-Intestine Length in Infants and Children | JAMA Pediatrics
Small-Intestine Length in Infants and Children | JAMA Pediatrics | JAMA Network [Skip to Navigation]This Issue
- Download PDF
- Full Text
-
Share
Twitter Facebook Email LinkedIn
- Cite This
- Permissions
Article
June 1980
Joseph R. Siebert, MS
Siebert, MS
Author Affiliations
From the Department of Pathology, Children's Hospital of Pittsburgh. Mr Siebert is now with the Department of Laboratories, Children's Orthopedic Hospital and Medical Center, Seattle.
Am J Dis Child. 1980;134(6):593-595. doi:10.1001/archpedi.1980.02130180051015
Full Text
Abstract
• Small-intestine length from ligament of Treitz to ileocecal valve was measured in 183 infants and children ranging up to 15 years of age. Elongation of the intestine was rapid until crown-heel length was 60 cm and remained constant from 100 to 140 cm of body length. When patients were placed into three general diagnostic categories (congenital heart disease, abdominal lesions, and miscellaneous) no significant differences were found. However, several striking instances of abnormally long or short small intestines were encountered.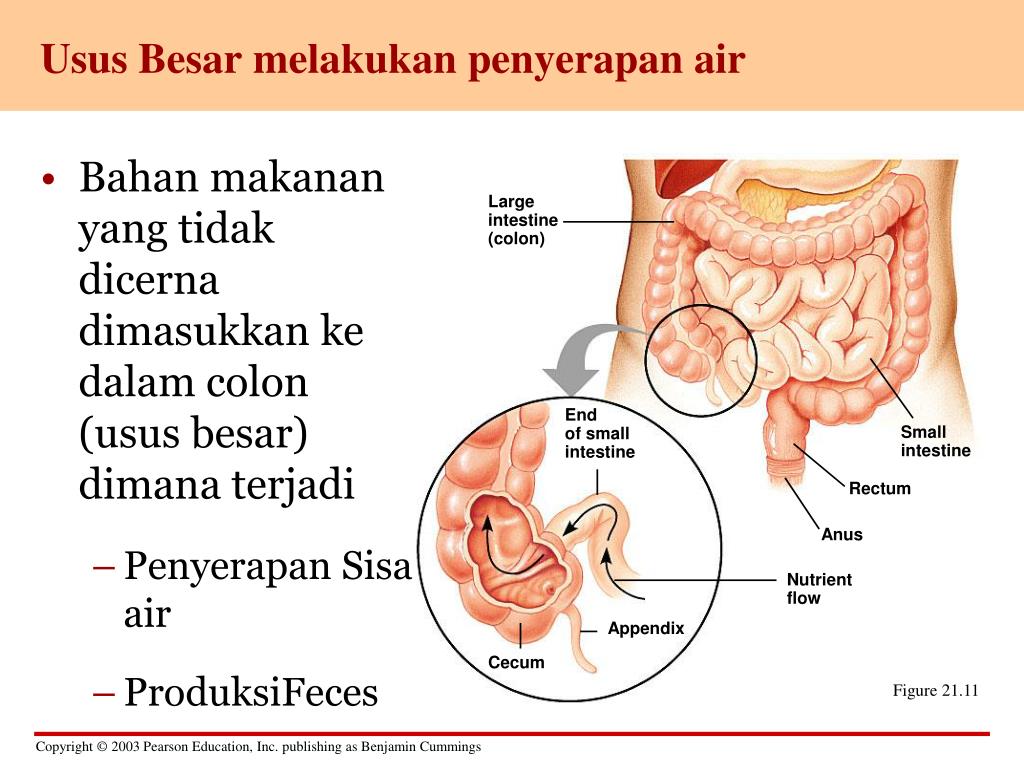
(Am J Dis Child 134:593-595, 1980)
Full Text
Add or change institution
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Bleeding and Transfusion
- Cardiology
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Diversity, Equity, and Inclusion
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life
- Environmental Health
- Ethics
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Geriatrics
- Global Health
- Guide to Statistics and Methods
- Guidelines
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Informatics
- Health Policy
- Hematology
- History of Medicine
- Humanities
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Melanoma
- Mobile Health and Telemedicine
- Narrative Medicine
- Nephrology
- Neurology
- Neuroscience and Psychiatry
- Notable Notes
- Nursing
- Nutrition
- Nutrition, Obesity, Exercise
- Obesity
- Obstetrics and Gynecology
- Occupational Health
- Oncology
- Ophthalmic Images
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Pediatrics
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Poetry
- Population Health
- Preventive Medicine
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Radiology
- Regulatory Agencies
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgery
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Toxicology
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Urology
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Violence
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Save Preferences
Privacy Policy | Terms of Use
Read online “Children's diseases.
 A complete guide” – LitRes, page 4
A complete guide” – LitRes, page 4 FEATURES OF VESSELS IN CHILDREN
Vessels supply and distribute blood to the organs and tissues of the child. Their clearance in young children is wide. Arteries are equal in width to veins. The ratio of their lumen is 1: 1, then the venous bed becomes wider, by the age of 16 their ratio is 1: 2. The growth of arteries and veins often does not correspond to the growth of the heart. Arterial walls are more elastic than vein walls. This is associated with lower indicators than in adults, peripheral resistance, blood pressure and blood flow velocity.
The structure of the arteries also changes. In newborns, the walls of the vessels are thin, they have poorly developed muscle and elastic fibers. Until the age of 5, the muscle layer grows rapidly, at the age of 5–8 all the membranes of the vessels are evenly developed, by the age of 12 the structure of the vessels in children is the same as in adults.
The pulse rate in children depends on age.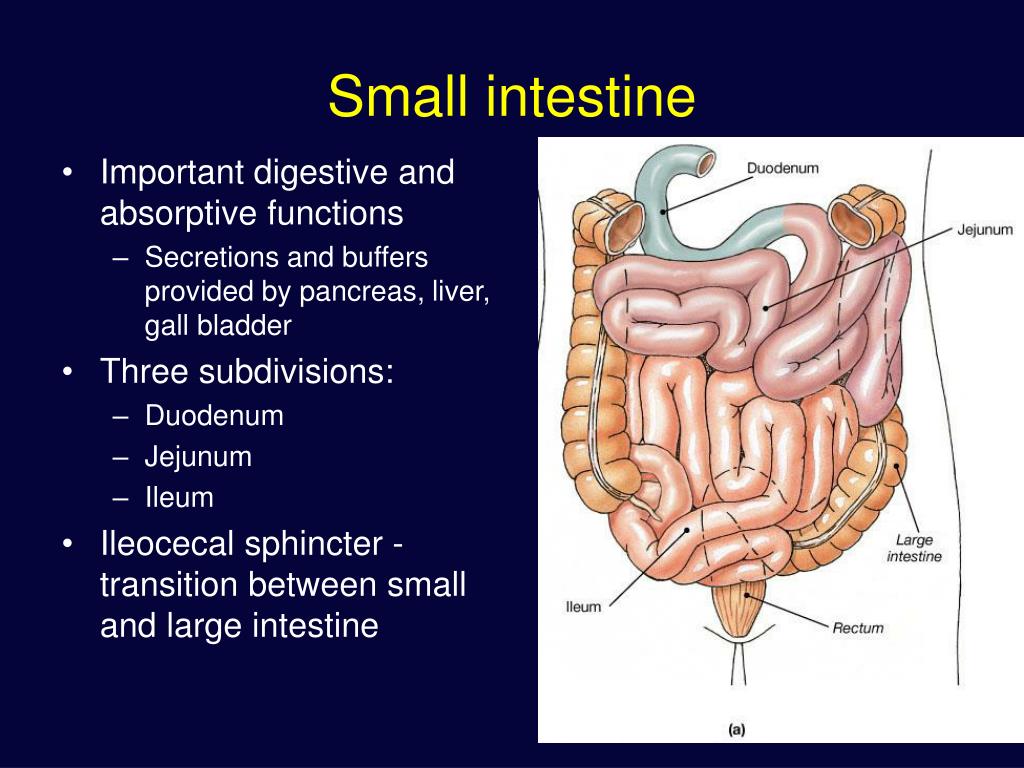 In a newborn it is 160-140 beats per minute, at 1 year old - 110-140, at 5 years old - 100, at 10 years old - 80-90, at 15 years old - 80. tendency to increase diastolic pressure.
In a newborn it is 160-140 beats per minute, at 1 year old - 110-140, at 5 years old - 100, at 10 years old - 80-90, at 15 years old - 80. tendency to increase diastolic pressure.
Systolic blood pressure is 90 + 2 × n, diastolic pressure is 60 + 2 × n, where n is the child's age in years. For children under 1 year old, systolic pressure is 75 + n, where n is the child's age in months. Diastolic blood pressure is equal to systolic pressure minus 10 mm Hg. Art.
HEART AND VESSELS DURING PUBERTY
At puberty there is an intensive growth of various organs and systems. During this period, there are violations of their functioning due to violations of their relationships and coordination of functions. In adolescents, due to the peculiarities of the growth of both the heart and the whole body, relatively small mass and volume of the heart are noted compared to the mass and volume of the body. The ratio of body volume to heart volume in children is 50%, in an adult - 60%, and in puberty is 90%.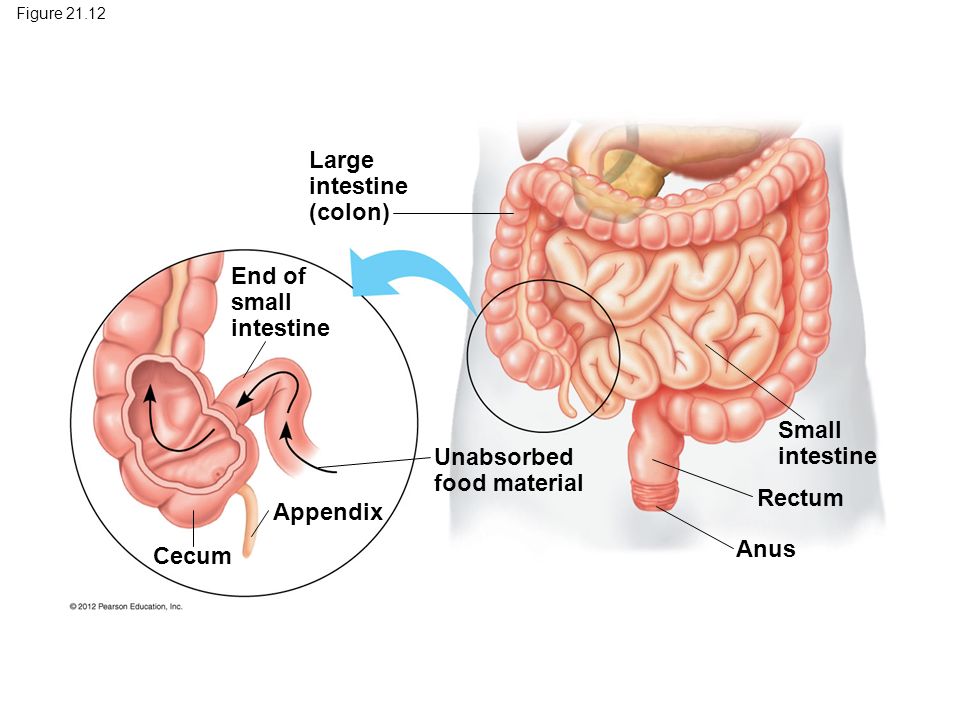 In addition, there are anatomical features of the cardiovascular system in adolescents, which are associated with the ratio of the volume of the heart and blood vessels.
In addition, there are anatomical features of the cardiovascular system in adolescents, which are associated with the ratio of the volume of the heart and blood vessels.
In adolescents, the volume of the heart increases faster than the capacity of the vasculature, this increases peripheral resistance, resulting in a hypertrophic variant of the adolescent heart.
Sympathetic regulation prevails in adolescents with deviations in the age evolution of the heart.
Thus, children have functional features of the circulatory organs, which are characterized by:
1) a high level of endurance of a child's heart due to its rather large mass, good blood supply;
2) physiological tachycardia caused by a small volume of the heart with a high need of the child's body for oxygen, as well as sympathotomy;
3) low blood pressure with a small volume of blood coming with each heartbeat, as well as low peripheral vascular resistance;
4) uneven growth of the heart and related functional disorders.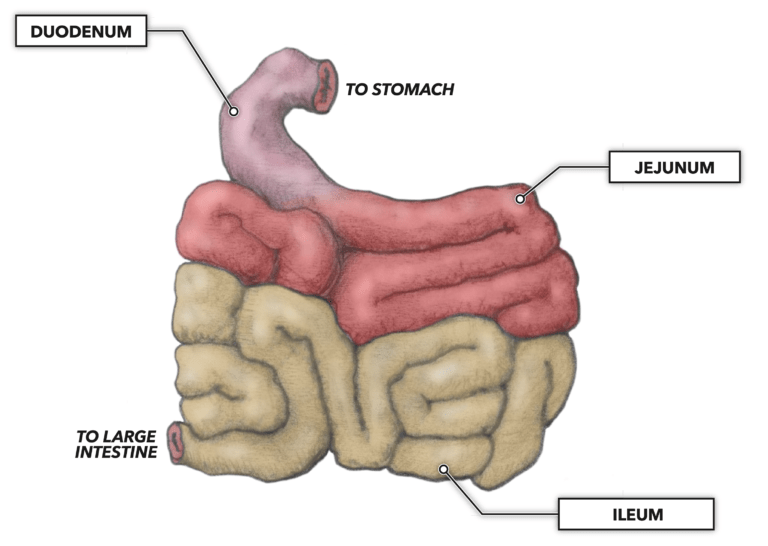
CHAPTER 6. ANATOMICAL AND PHYSIOLOGICAL FEATURES OF THE DIGESTIVE SYSTEM IN CHILDREN
The digestive organs include the oral cavity, esophagus, stomach and intestines. The pancreas and liver are involved in digestion. The digestive organs are laid in the first 4 weeks of the prenatal period, by 8 weeks of pregnancy all departments of the digestive organs are determined. The fetus begins to swallow amniotic fluid by 16-20 weeks of pregnancy. Digestive processes occur in the intestines of the fetus, where an accumulation of the original feces - meconium - is formed.
CHARACTERISTICS OF THE ORAL CAVITY
The main function of the oral cavity in a child after birth is to provide the act of sucking. These features are: small size of the oral cavity, large tongue, well-developed lip musculature and chewing muscles, transverse folds on the mucous membrane of the lips, ridge-like thickening of the gums, there are fat lumps (Bish lumps) in the cheeks, which give the cheeks elasticity.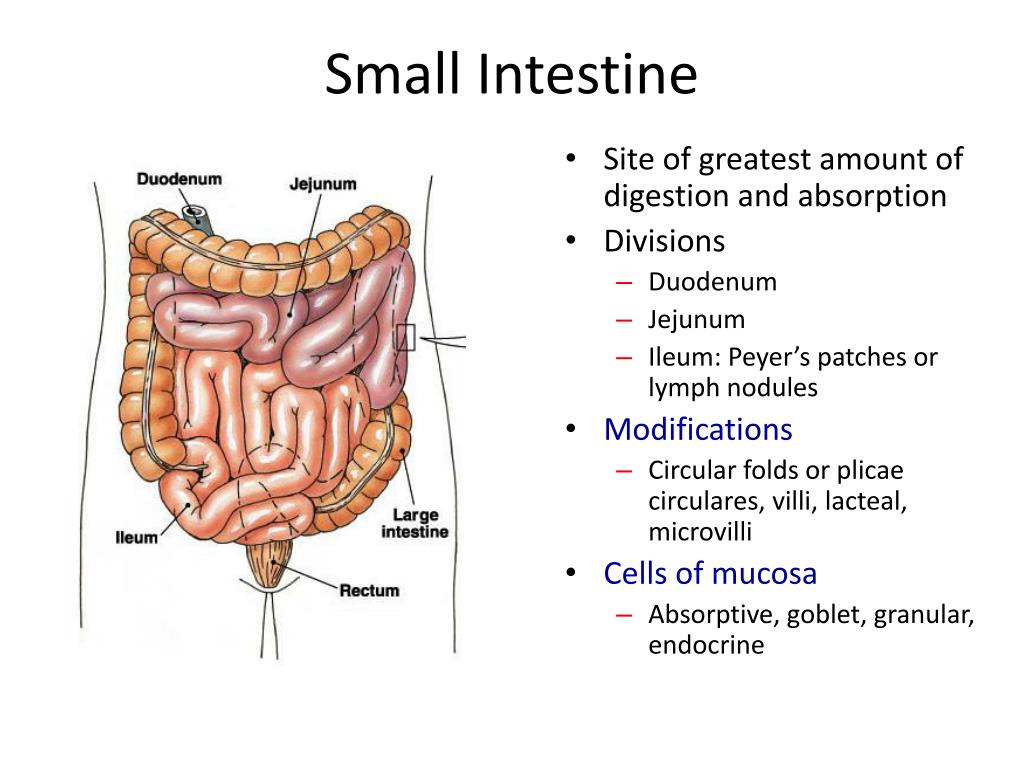
The salivary glands of children are underdeveloped after birth; little saliva is secreted in the first 3 months. The development of the salivary glands is completed by 3 months of age.
CHARACTERISTICS OF THE ESOPHAGUS
The esophagus in young children is spindle-shaped, narrow and short. In a newborn, its length is only 10 cm, in children at 1 year of age - 12 cm, at 10 years old - 18 cm. Its width, respectively, is 8 mm at 7 years old, and 15 mm at 12 years old.
There are no glands on the mucous membrane of the esophagus. It has thin walls, poor development of muscle and elastic tissues, and a good blood supply. The entrance to the esophagus is located high. He has no physiological constrictions.
STOMACH CHARACTERISTICS
In infancy, the stomach is horizontal. As the child grows and develops during the period when the child begins to walk, the stomach gradually assumes a vertical position, and by the age of 7-10 it is located in the same way as in adults.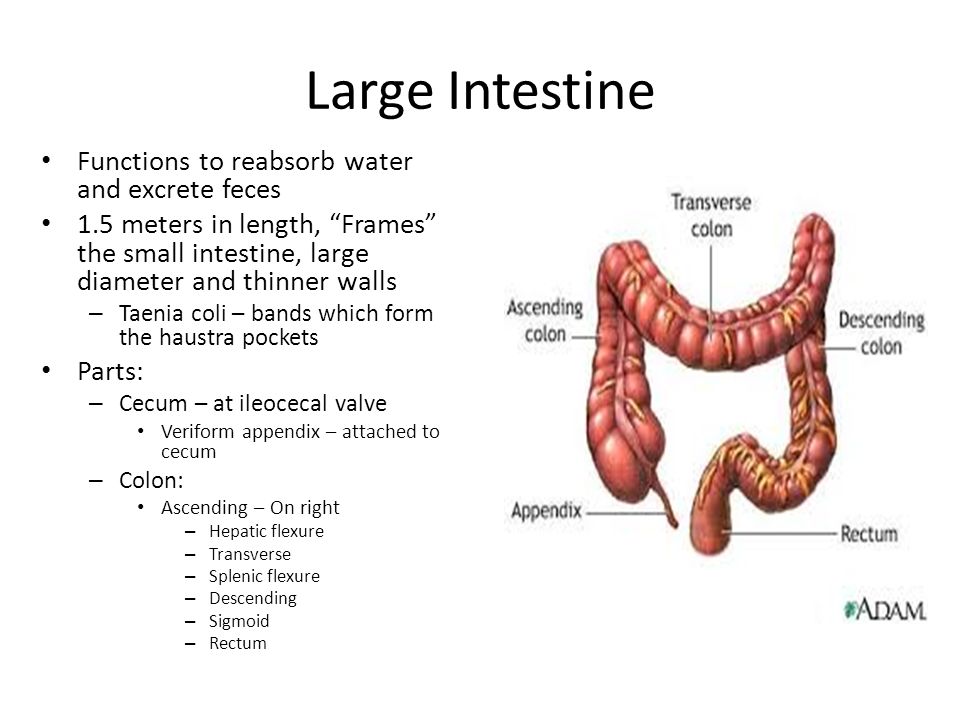 The capacity of the stomach gradually increases: at birth it is 7 ml, at 10 days - 80 ml, per year - 250 ml, at 3 years - 400–500 ml, at 10 years - 1500 ml.
The capacity of the stomach gradually increases: at birth it is 7 ml, at 10 days - 80 ml, per year - 250 ml, at 3 years - 400–500 ml, at 10 years - 1500 ml.
The volume of a single meal for children of the first year of life can be calculated using the formula of N. F. Filatov:
V = 30 ml + 30 × n,
where n is the age in months.
A feature of the stomach in children is the weak development of its fundus and cardiac sphincter against the background of a good development of the pyloric section. This contributes to frequent regurgitation in a child, especially when air enters the stomach during sucking.
The gastric mucosa is relatively thick, against which there is a weak development of the gastric glands. The active glands of the gastric mucosa, as the child grows, form and increase 25 times, as in the adult state. In connection with these features, the secretory apparatus in children of the first year of life is underdeveloped. The composition of gastric juice in children is similar to adults, but its acidic and enzymatic activity is much lower.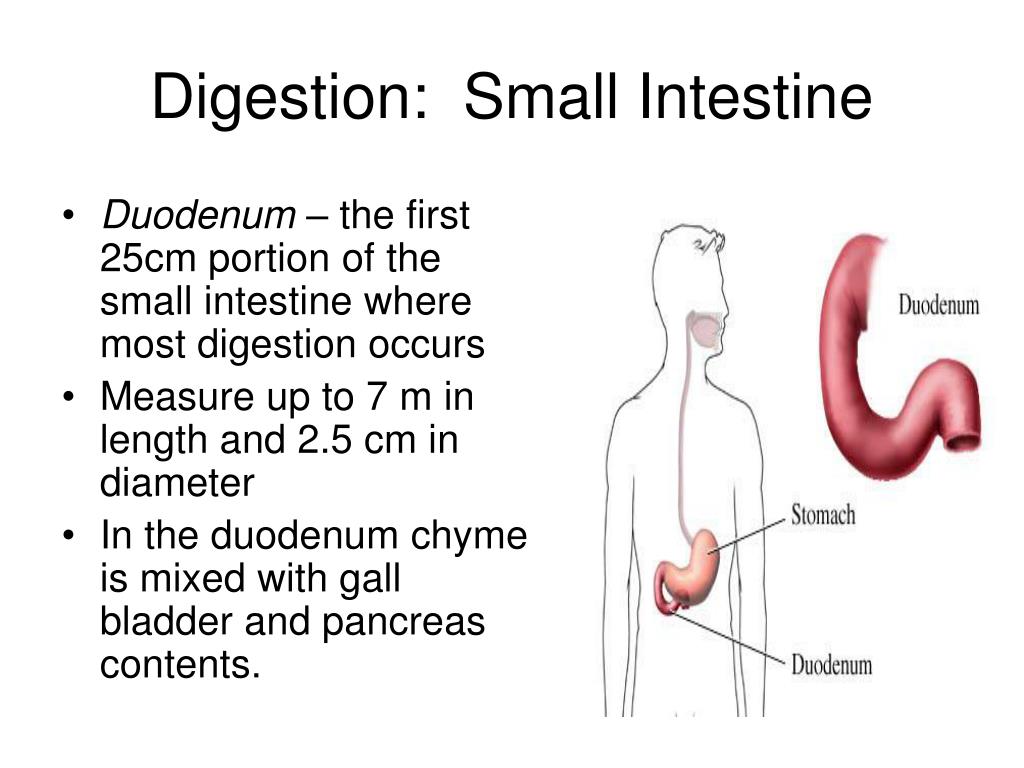 Barrier activity of gastric juice is low.
Barrier activity of gastric juice is low.
The main active enzyme of gastric juice is rennet (labenzyme), which ensures the first phase of digestion - milk curdling.
Very little lipase is excreted in the stomach of an infant. This deficiency is compensated by the presence of lipase in breast milk, as well as in the pancreatic juice of the child. If a child receives cow's milk, its fats in the stomach do not break down.
Absorption in the stomach is insignificant and concerns substances such as salts, water, glucose, and protein breakdown products are only partially absorbed. The timing of the evacuation of food from the stomach depends on the type of feeding. Women's milk lingers in the stomach for 2-3 hours.
FEATURES OF THE PANCREAS
The pancreas is small. In a newborn, its length is 5–6 cm, and by the age of 10 it triples. The pancreas is located deep in the abdominal cavity at the level of the X thoracic vertebra, at an older age it is located at the level of the I lumbar vertebra.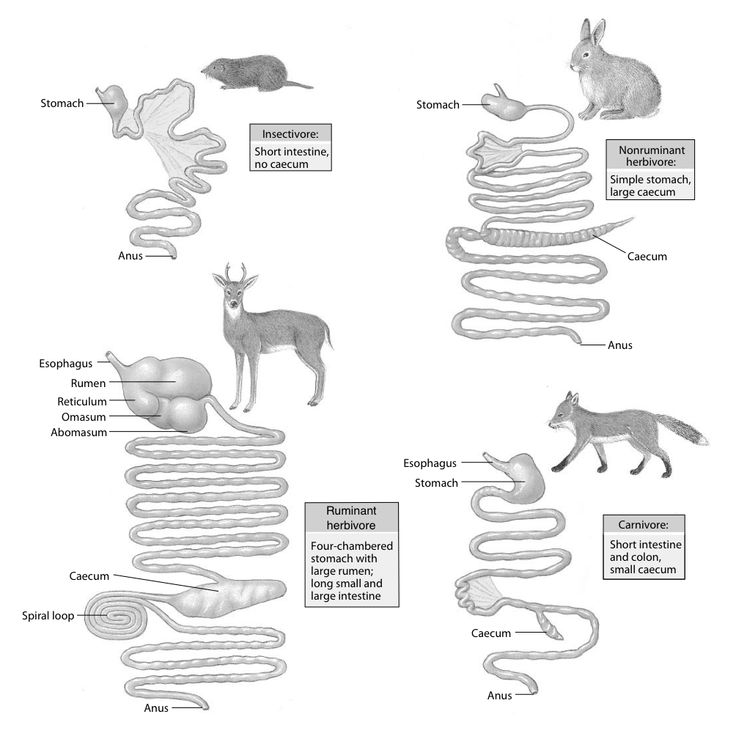 Its intensive growth occurs up to 14 years.
Its intensive growth occurs up to 14 years.
Dimensions of the pancreas in children in the first year of life (cm):
1) newborn - 6.0 × 1.3 × 0.5;
2) 5 months - 7.0 × 1.5 × 0.8;
3) 1 year - 9.5 × 2.0 × 1.0.
The pancreas is richly supplied with blood vessels. Its capsule is less dense than in adults, and consists of fine-fibrous structures. Its excretory ducts are wide, which provides good drainage.
The child's pancreas has exocrine and intrasecretory functions. It produces pancreatic juice, consisting of albumins, globulins, trace elements and electrolytes, enzymes necessary for the digestion of food. Enzymes include proteolytic enzymes: trypsin, chymotrypsin, elastase, as well as lipolytic enzymes and amylolytic enzymes. The regulation of the pancreas is provided by secretin, which stimulates the release of the liquid part of the pancreatic juice, and pancreozymin, which enhances the secretion of enzymes along with other hormone-like substances that are produced by the mucous membrane of the duodenum and small intestine.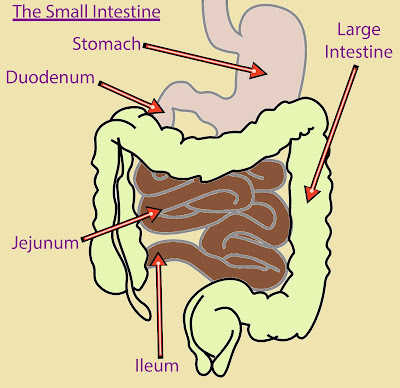
The intrasecretory function of the pancreas is carried out due to the synthesis of hormones responsible for the regulation of carbohydrate and fat metabolism.
LIVER
The newborn's liver is the largest organ, occupying 1/3 of the abdominal cavity. At 11 months, its mass doubles, by 2–3 years it triples, by 8 years it increases 5 times, by 16–17 years the mass of the liver is 10 times.
The liver performs the following functions:
1) produces bile involved in intestinal digestion;
2) stimulates intestinal motility, due to the action of bile;
3) stores nutrients;
4) performs a barrier function;
5) participates in metabolism, including the conversion of vitamins A, D, C, B 12 , K;
6) in the prenatal period is a hematopoietic organ.
After birth, further formation of liver lobules occurs. The functional capabilities of the liver in young children are low: in newborn children, the metabolism of indirect bilirubin is not completely carried out.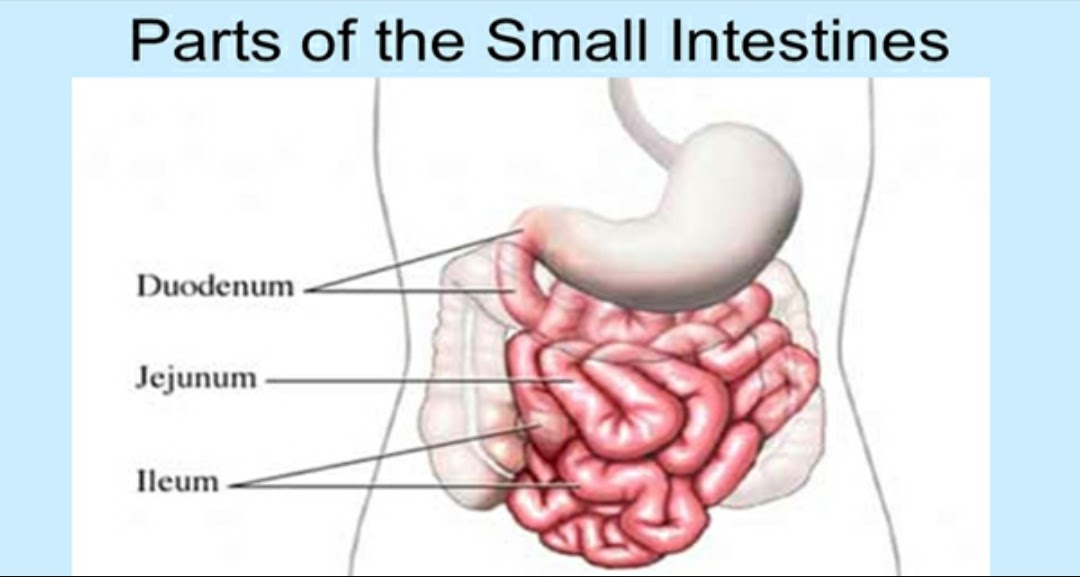
CHARACTERISTICS OF THE GALL BLADDER
The gallbladder is located under the right lobe of the liver and has a fusiform shape, its length reaches 3 cm. It acquires a typical pear-shaped shape by 7 months, by 2 years it reaches the edge of the liver.
The main function of the gallbladder is the accumulation and secretion of hepatic bile. The bile of a child differs in its composition from the bile of an adult. It has few bile acids, cholesterol, salts, a lot of water, mucin, pigments. In the neonatal period, bile is rich in urea. In the bile of a child, glycocholic acid predominates and enhances the bactericidal effect of bile, and also accelerates the separation of pancreatic juice. Bile emulsifies fats, dissolves fatty acids, improves peristalsis.
With age, the size of the gallbladder increases, bile of a different composition than in young children begins to be secreted. The length of the common bile duct increases with age.
Dimensions of the gallbladder in children (Chapova O.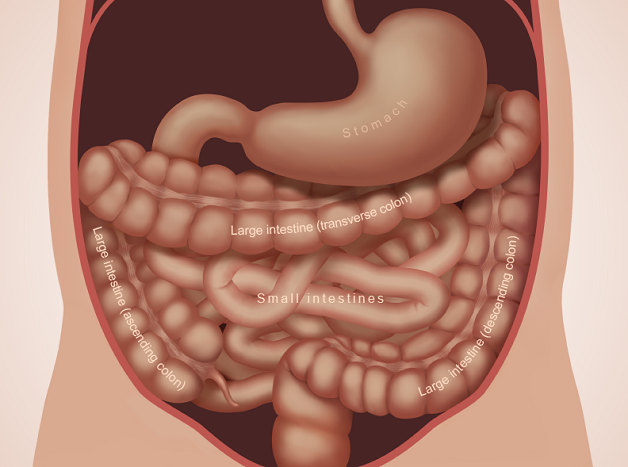 I., 2005):
I., 2005):
1) newborn - 3.5 × 1.0 × 0.68 cm;
2) 1 year - 5.0 × 1.6 × 1.0 cm;
3) 5 years - 7.0 × 1.8 × 1.2 cm;
4) 12 years - 7.7 x 3.7 x 1.5 cm.
FEATURES OF THE SMALL INTESTINE
The intestines of children are relatively longer than those of adults.
The ratio of the length of the small intestine and body length in a newborn is 8.3: 1, in the first year of life - 7.6: 1, at 16 years - 6.6: 1.
The length of the small intestine in a child of the first year of life is 1.2–2.8 m. The area of the inner surface of the small intestine in the first week of life is 85 cm 2 , in an adult - 3.3 × 103 cm 2 . The area of the small intestine increases due to the development of the epithelium and microvilli.
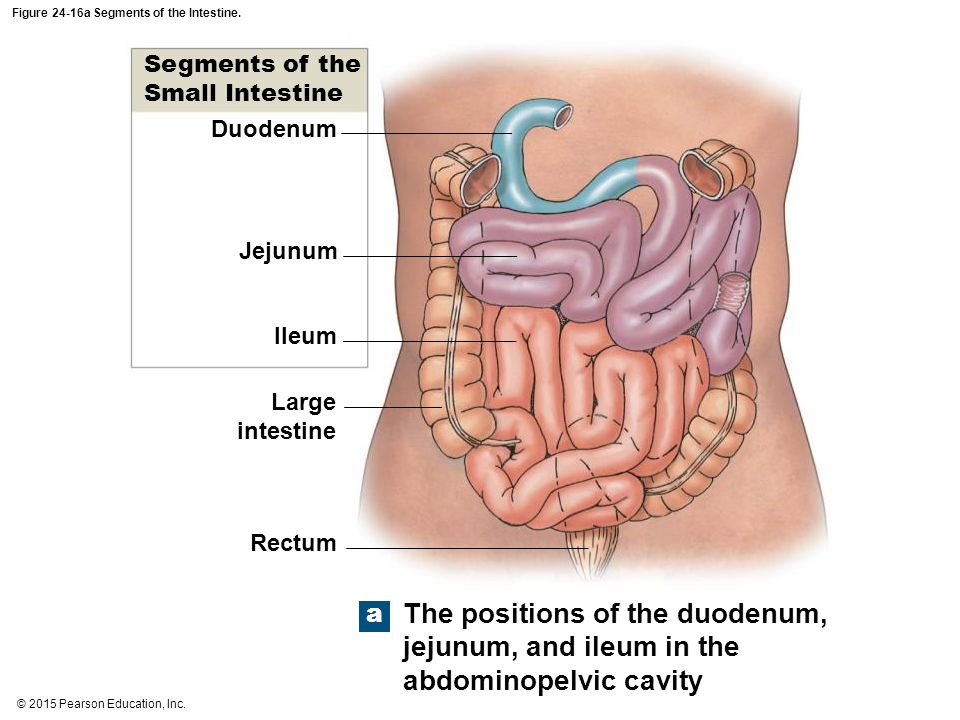
The small intestine is anatomically divided into 3 sections. The first section is the duodenum, the length of which in a newborn is 10 cm, in an adult it reaches 30 cm. It has three sphincters, the main function of which is to create an area of low pressure where food comes into contact with pancreatic enzymes.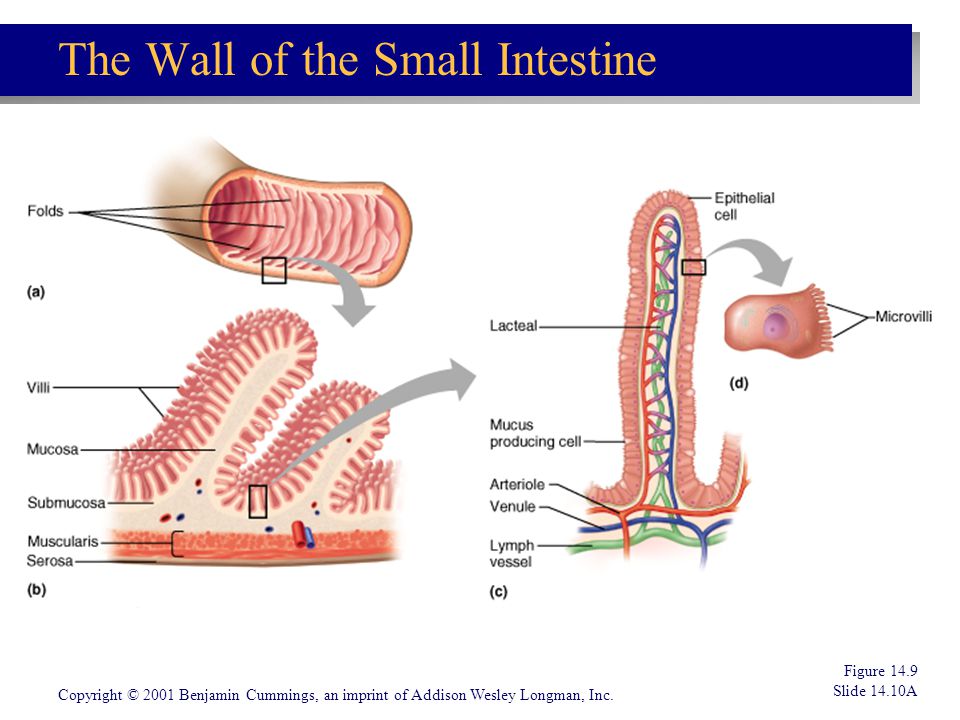
The second and third sections are represented by the small and ileal intestines. The length of the small intestine is 2/5 of the length to the ileocecal angle, the remaining 3/5 is the ileum.
Digestion of food, absorption of its ingredients occurs in the small intestine. The intestinal mucosa is rich in blood vessels, the epithelium of the small intestine is rapidly renewed. Intestinal glands in children are larger, lymphoid tissue is scattered throughout the intestine. As the child grows, Peyer's patches form.
FEATURES OF THE LARGE INTESTINE
The large intestine consists of various sections and develops after birth. In children under 4 years of age, the ascending colon is longer than the descending one. The sigmoid colon is relatively longer. Gradually, these features disappear. The caecum and appendix are mobile, the appendix is often located atypically.
Rectum in children of the first months of life is relatively long. In newborns, the rectal ampulla is undeveloped, the surrounding fatty tissue is poorly developed. By the age of 2, the rectum assumes its final position, which contributes to prolapse of the rectum in early childhood with straining, with persistent constipation and tenesmus in debilitated children.
By the age of 2, the rectum assumes its final position, which contributes to prolapse of the rectum in early childhood with straining, with persistent constipation and tenesmus in debilitated children.
Omentum in children under 5 years - short.
Juice secretion in children in the large intestine is small, but increases sharply with mechanical irritation.
In the large intestine, water is absorbed and feces are formed.
FEATURES OF THE INTESTINAL MICROFLORA
The gastrointestinal tract of the fetus is sterile. When a child comes into contact with the environment, it is populated by microflora. In the stomach and duodenum, the microflora is poor. In the small and large intestines, the number of microbes increases and depends on the type of feeding. The main microflora is B. bifidum, whose growth is stimulated by β-lactose in breast milk. With artificial feeding, opportunistic gram-negative E. coli dominates in the intestine. The normal intestinal flora has two main functions:
1) creation of an immunological barrier;
2) synthesis of vitamins and enzymes.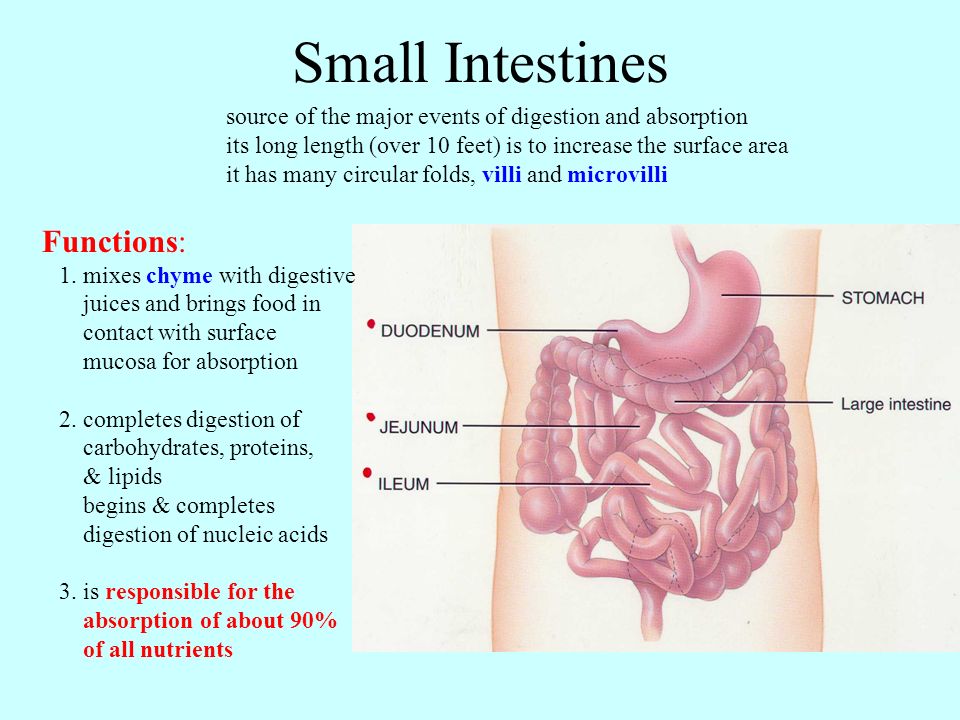
DIGESTIVE CHARACTERISTICS IN INFANTS
For children of the first months of life, nutrients that come with mother's milk and are digested due to substances contained in women's milk itself are of decisive importance. With the introduction of complementary foods, the mechanisms of the child's enzyme systems are stimulated. The absorption of food ingredients in young children has its own characteristics. Casein first curdles in the stomach under the influence of rennet. In the small intestine, it begins to break down into amino acids, which are activated and absorbed.
Digestion of fat depends on the type of feeding. Cow's milk fats contain long chain fats that are broken down by pancreatic lipase in the presence of fatty acids.
Fat absorption occurs in the terminal and middle portions of the small intestine. The breakdown of milk sugar in children occurs in the border of the intestinal epithelium. Human milk contains β-lactose, while cow's milk contains α-lactose.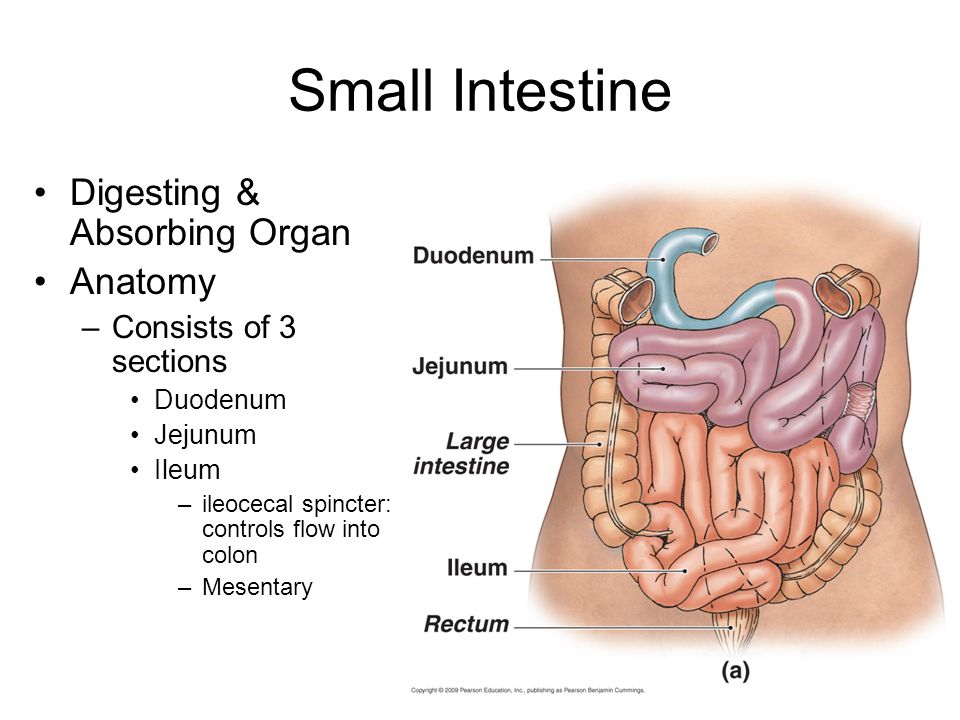 In this regard, with artificial feeding, the carbohydrate composition of food is changed. Vitamins are also absorbed in the small intestine.
In this regard, with artificial feeding, the carbohydrate composition of food is changed. Vitamins are also absorbed in the small intestine.
CHAPTER 7. ANATOMICAL AND PHYSIOLOGICAL FEATURES OF THE URINARY SYSTEM
By the time of birth, the maturation of the kidneys has not yet been completed. The glomeruli in newborns are much smaller than in adults, their filtering surface is 30% of the adult norm. The tubules are shorter and narrower. Compared to adults, urine reabsorption in children is reduced.
Urinary organs change with age. In young children, the size of the kidneys is relatively larger, the ratio of their mass to the body weight of the newborn is 1: 100, in an adult - 1: 200.
The upper pole of the kidney is at the level of the XI-XII thoracic vertebrae, the lower one is at the level of the IV lumbar vertebra. By the age of 2, these features of the location of the kidneys disappear. In subsequent years, the growth of the kidneys corresponds to the growth of the body.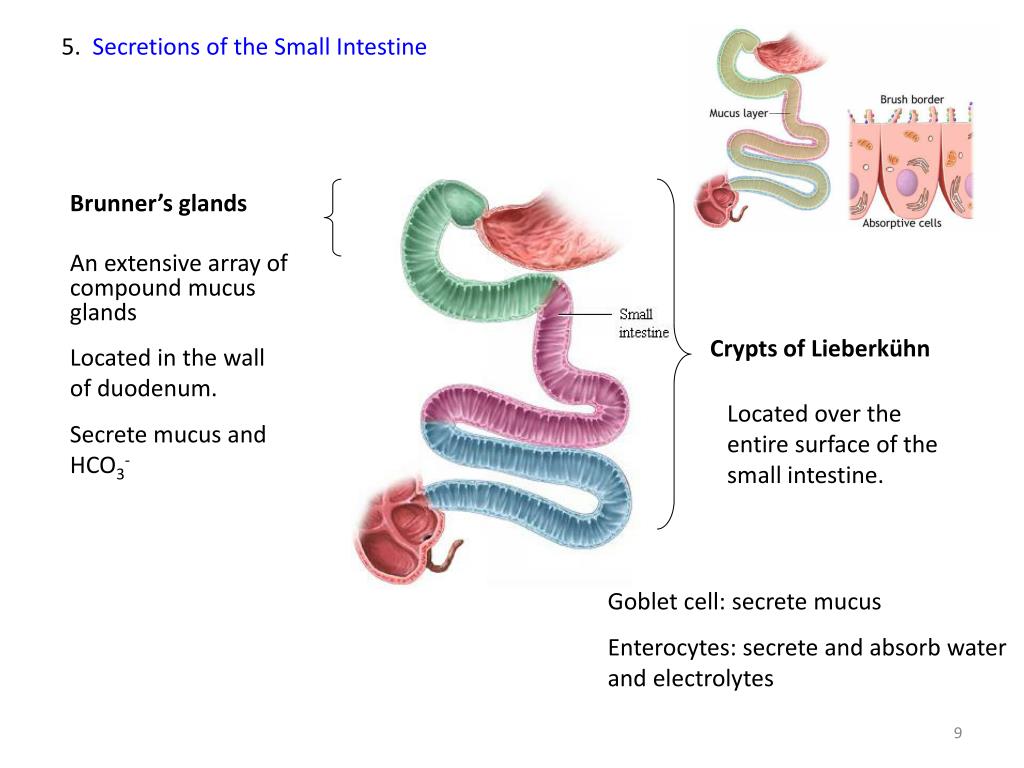
Kidneys in the first years of life have a lobular structure. The cortical layer is underdeveloped. The glomeruli in the newborn are compact. The amount of glomerular filtrate in children in the first months of life is reduced due to the fact that their filtering surface is much smaller than in adults (see Table 15).
Table 15
Dimensions of the kidneys in children (cm) (Fimin V.A., 2003)
With the growth of the kidney, a uniform development of nephrons is observed.
The amount of urine produced by a child can normally be approximately calculated by the formula:
V = 100 × (n + 5), where V is the volume of urine per day;
n is the number of years.
Or according to the formula:
V = 600 + 100 (n – 1),
where V is urine volume per day;
n is the number of years.
Children need more water to eliminate waste than adults. Dehydration in children occurs much faster. Breastfed babies digest it completely and there are very few products excreted through the kidneys.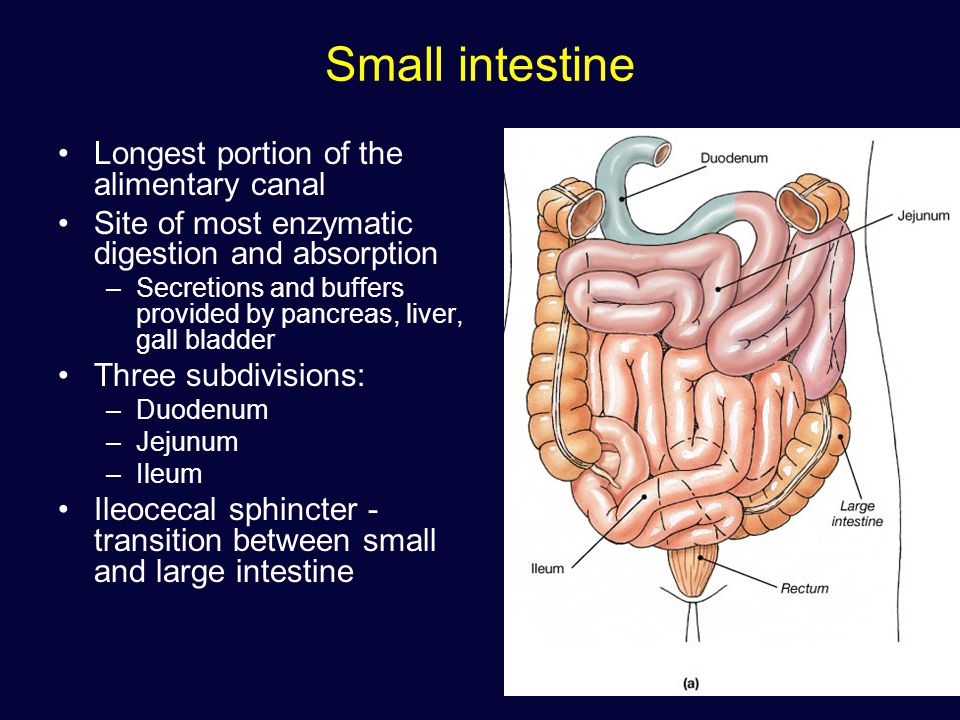 In this regard, with low functional capabilities, imperfection of the systems that regulate water-salt metabolism, the child maintains the constancy of the internal environment. When replacing breast milk with other products, the load on the kidneys increases, the amount of products to be removed increases, the kidneys work with great stress, the acidity of urine changes.
In this regard, with low functional capabilities, imperfection of the systems that regulate water-salt metabolism, the child maintains the constancy of the internal environment. When replacing breast milk with other products, the load on the kidneys increases, the amount of products to be removed increases, the kidneys work with great stress, the acidity of urine changes.
The kidneys are involved in maintaining the osmotic regulation of blood and extracellular fluid metabolism, maintaining acid-base balance.
Urine is formed as a result of the active function of the nephron, with the help of which plasma ultrafiltration occurs in the capillaries of the glomeruli, the reabsorption of water and glucose occurs in the tubules, the synthesis and secretion of compounds necessary for the body. Low-molecular water-soluble compounds pass through the filtering membrane of the glomeruli from the blood plasma. The kidney filter does not pass cellular elements and proteins.
Urine formation is regulated through the pituitary gland, adrenal glands, humoral and nervous pathways.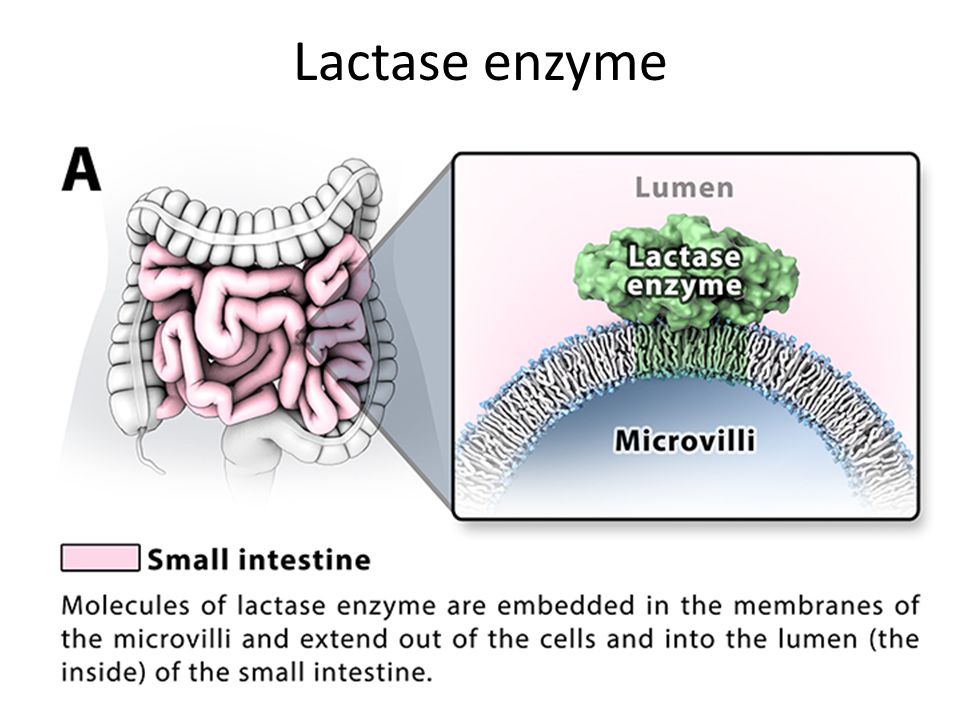 Water excretion is regulated by antidiuretic hormone. Aldosterone, a hormone of the adrenal cortex, increases sodium reabsorption and potassium excretion. In the first 3 months, 90 ml of urine per 1 kg of body weight is excreted, at the age of 10 years - 25–35 ml per 1 kg of body weight per day.
Water excretion is regulated by antidiuretic hormone. Aldosterone, a hormone of the adrenal cortex, increases sodium reabsorption and potassium excretion. In the first 3 months, 90 ml of urine per 1 kg of body weight is excreted, at the age of 10 years - 25–35 ml per 1 kg of body weight per day.
Ureters . The ureters in young children are relatively wider, more tortuous than in adults. The walls of the ureters are equipped with poorly formed muscle and elastic fibers.
Bladder . In newborns, the bladder is oval in shape and is higher than in adults. His mucosa is fully formed. With the age of the child, its muscle layer and elastic fibers thicken. The capacity of the bladder in a newborn is 50 ml, at 1 year - 200 ml.
Urethra . In boys, its length is 5–6 cm, in adult men it is 14–18 cm.0004 Urination of a newborn is produced due to congenital spinal reflexes. Upon reaching the age of 12 months, the conditioned reflex to urination is fully fixed (see Table 16).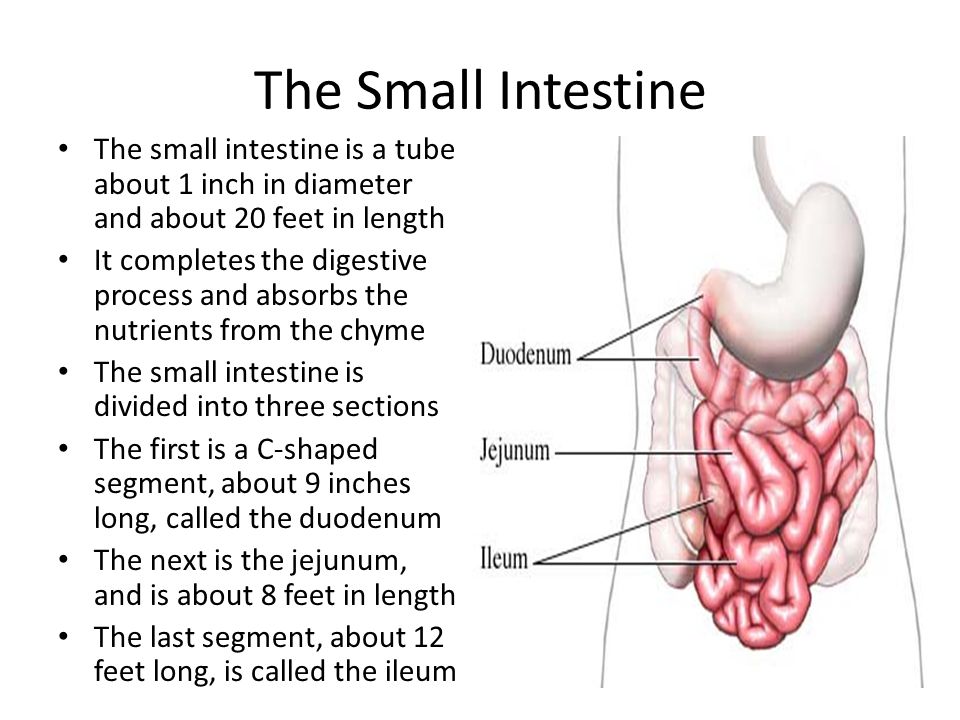
Table 16
The amount of urine and the frequency of urination in children (Papayan A.V., 1997)
The most informative indicator of the urinary system is urine analysis. The color of urine is normally yellow, the color of urine depends on the concentration of urinary elements. It can change with methylene blue, riboflavin, and food pigments.
Freshly passed urine is clear. Turbidity when standing urine depends on the presence of a large amount of salts, acidic elements, bacteria, mucus and fat.
Urine has a slightly acidic reaction, with artificial feeding - slightly alkaline.
Urine density ranges from 1002-1030. It depends on the amount of fluid drunk, diet, sweating. Urine in young children is less concentrated (see Table 17).
Table 17
Relative density of urine (Papayan A. V., 1997)
The density of urine is affected by the presence of protein, glucose and other substances in it. A decrease in the relative density of urine is observed in chronic renal failure, pituitary insufficiency and other diseases.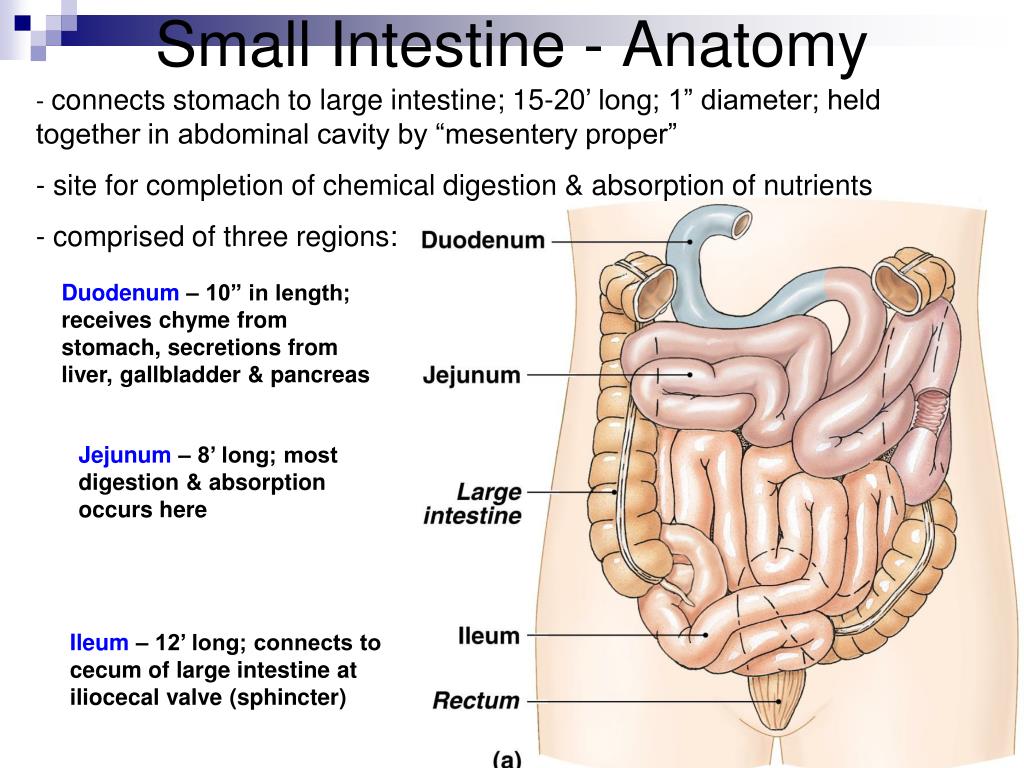 An increase in the density of urine occurs with large losses of fluid.
An increase in the density of urine occurs with large losses of fluid.
Usually 1-2 squamous cells are found in the urine sediment. In inflammatory processes, this indicator increases.
Cells of columnar epithelium are found in the urine sediment in single numbers.
Erythrocytes can be single: 0-1 per field of view, up to 2 in girls.
Leukocytes are also found in normal urine 5–6 per field of view.
Single hyaline and waxy casts can be found in healthy people during exercise.
Protein in the urine is found during physical stress, inflammatory and chronic kidney diseases, when the permeability of the membrane filter increases.
Glucose in the urine can be manifested in disorders of carbohydrate metabolism.
Ketonuria is found with frequent vomiting, metabolic disorders.
An increase in the amount of urine (polyuria) is typical for patients with diabetes mellitus, chronic nephritis, with edema discharge, after febrile illnesses.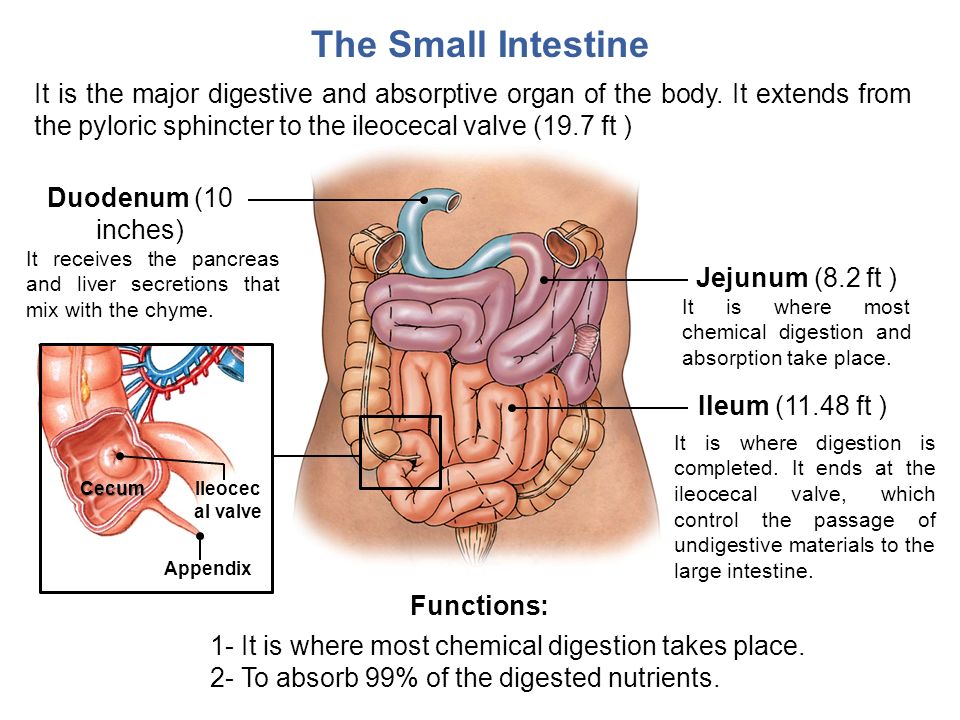
Oliguria (20-30% decrease in urine output) or absence of urine is due to a decrease or complete cessation of urine output by the kidneys, as well as reflex spasm and obstruction of outflow in the lower parts of the kidneys. Causes of oliguria can be diseases of the heart and kidneys, loss of fluid during vomiting, diarrhea, insufficient fluid intake.
Dysuria (impaired urination with urinary retention in the bladder) is most often associated with reflex spasm of the bladder sphincter in inflammatory diseases of the urinary tract, damage to the central nervous system and other diseases.
Pollakiuria (frequent urination) is observed in diabetes, chronic renal failure, cooling.
Painful urination may occur with cystitis and other urinary tract disorders.
Along with a general urine test, a quantitative determination of erythrocytes and leukocytes in the urine is carried out. To do this, a daily portion of urine is collected (Addis-Kakovsky test) or 1 ml of urine (Nechiporenko test).
16. Age features of the functioning of the small intestine in children (duodenum, jejunum and ileum, intestinal juice, enzymes, types of digestion)
Small the intestine is a tube 5-7 m, diameter 3-5 cm. Its length is newborn - 1.2-2.6 m, at 2-3 years 2.8 m, by 10 years - 5-6 m, as in an adult person. The diameter of the intestine in a one-year-old the child is 16 mm, at 3 years old - 23 mm. It distinguishes duodenal intestine (25-30 cm long), jejunum (2-2.5 m) and the ileum (2.5-3.5 cm). Duodenal gut - is the beginning of the small intestine begins immediately behind the stomach, covering horseshoe head of the pancreas. The length of the duodenum newborns 7.5-10 cm, in an adult - 25-30 cm (about 12 finger diameters, hence the name). Bowel position depends on the filling of the stomach.
Skinny and ileum
Mesenteric part of the small intestine is the lean intestine and ileum, occupying about 4/5 of the entire length of the digestive tract.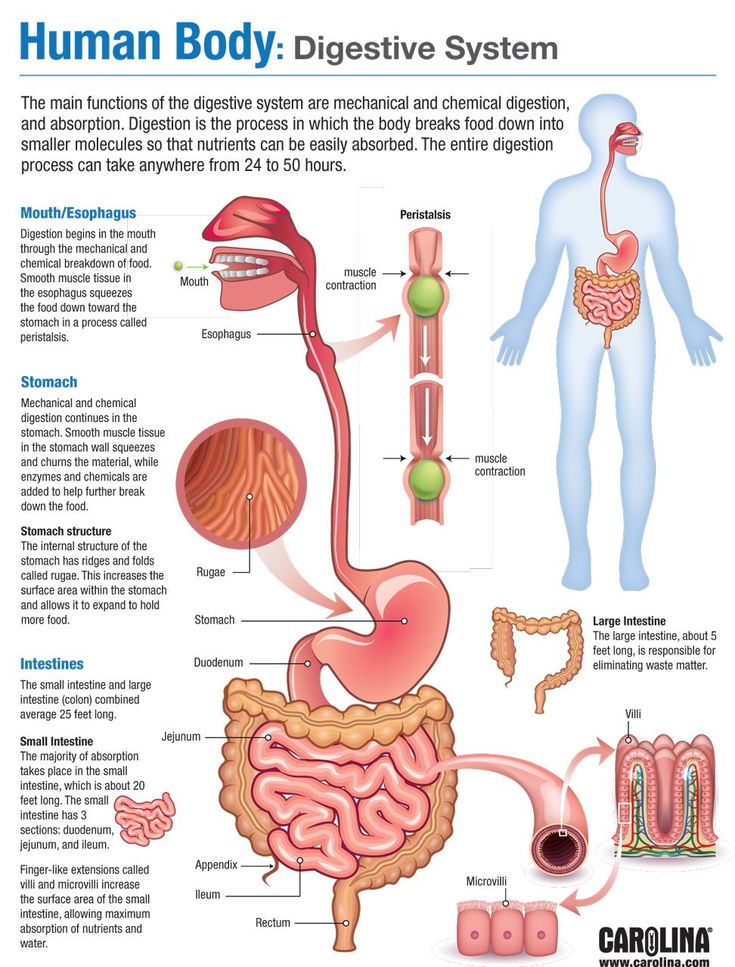 clear anatomical boundary between they are missing. This is the most mobile part of the intestine, as it is suspended on the mesentery and wrapped in the peritoneum. Digestive surface of the jejunum more than the iliac, this is due to its larger diameter, larger circular folds.
clear anatomical boundary between they are missing. This is the most mobile part of the intestine, as it is suspended on the mesentery and wrapped in the peritoneum. Digestive surface of the jejunum more than the iliac, this is due to its larger diameter, larger circular folds.
Length small intestine in a newborn is about 3 m, its intensive development lasts up to 3 years, after which growth slows down. In adults, the length of the thin intestines from 3 to 11 m; think that the length intestines is determined by the diet. In people who consume predominantly plant foods, the intestines are longer, than in people whose diet is dominated by products of animal origin. Diameter of the mesenteric part of the small intestine in the initial section is about 45 mm, and then gradually decreases to 30 mm.
Pleats The walls of the small intestine are made up of mucous membrane and submucosa, number reaches them in an adult 600-650. The villi in the jejunum are longer and more numerous (22-40 per 1 mm2) than iliac (18-31 per 1 mm2), the number the crypt is also larger.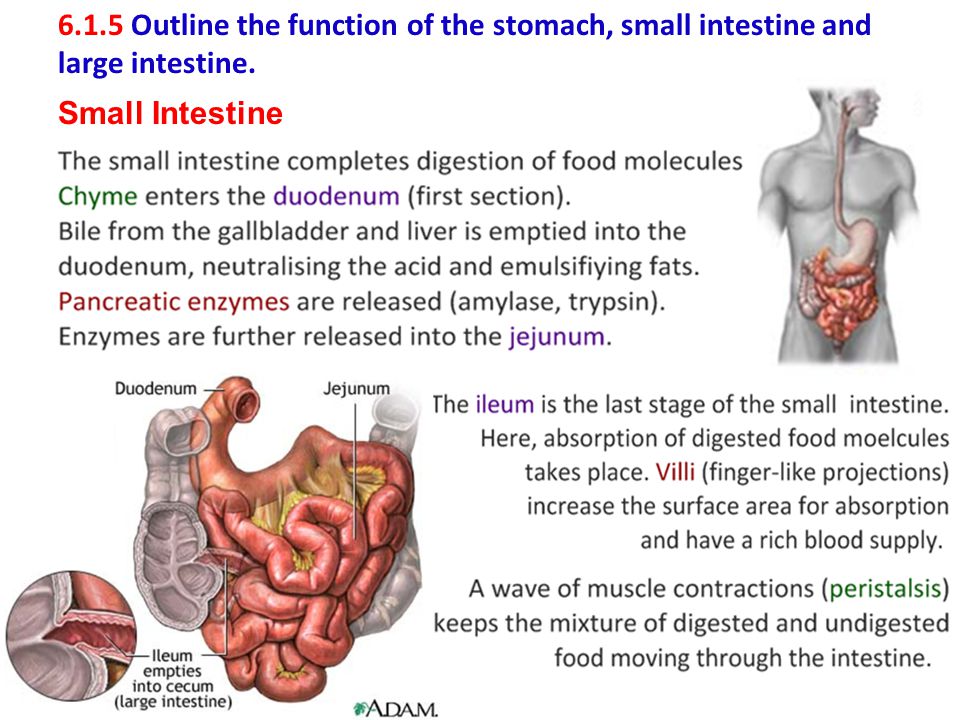 Total number of villi reaches 4 million total surface area small intestine including microvilli is 200 m2 for adults.
Total number of villi reaches 4 million total surface area small intestine including microvilli is 200 m2 for adults.
Mucous the lining of the small intestine contains up to 1000 glands per 1 mm2 that produce digestive juice. It includes numerous enzymes that act on proteins, fats and carbohydrates and products of their incomplete splits formed in the stomach . Intestinal juice consists of from the liquid part and sloughing cells intestinal epithelium. These cells are destroyed and release the contained enzymes. Over 20 enzymes found intestinal juice that can catalyze breakdown of almost any food organic substances to easily digestible products.
Types digestion. one. Abdominal digestion is carried out through digestive secretions and enzymes, passes into the intestinal cavity. Effective in splitting large food particles. Maximum at 12 - duodenal ulcer. 2. Parietal carried out by digestive enzymes fixed on cellular membranes of the mucous membrane of the thin intestines.