Contractions for weeks
Prodromal Labor: Definition, Symptoms, and More
Prodromal Labor: Definition, Symptoms, and MoreMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Becky Young on August 22, 2017
What is prodromal labor?
Prodromal labor is labor that starts and stops before fully active labor begins. It’s often called “false labor,” but this is a poor description. Medical professionals recognize that the contractions are real, but they come and go and labor may not progress.
So, prodromal labor is real in terms of contraction pain and regularity. What makes these contractions different from contractions seen in active labor is that they start and stop.
Prodromal labor contractions will often come and go at the same time each day or at regular intervals. Many mothers, even experienced ones, end up calling their birth team or going to the hospital, thinking labor has begun.
Prodromal labor is really common and can start days, weeks, or even a month or more before active labor begins. Your health care provider will want you to deliver as close to 40 weeks (your due date) as possible. Prodromal labor isn’t an indication for induction or cesarean delivery.
Prodromal labor vs. Braxton-Hicks
Prodromal labor is often mistaken for Braxton-Hicks contractions, but they’re not the same thing. The majority of pregnant women will experience this type of contraction at some stage during their pregnancy. Braxton-Hicks are essentially practice contractions. They’re your body’s way of preparing for labor.
Braxton-Hicks contractions can cause a very tight, uncomfortable sensation, but they’re not typically regular or intense. They rarely last a long time or grow in intensity. Prodromal labor can follow a very regular pattern. The contractions can vary and grow in intensity.
It’s sometimes possible to ease Braxton-Hicks contractions by drinking water, eating, or relaxing. These activities won’t help ease prodromal labor contractions. Your cervix can also slowly dilate or efface during prodromal labor.![]() This doesn’t usually happen with Braxton-Hicks contractions.
This doesn’t usually happen with Braxton-Hicks contractions.
Prodromal labor vs. active labor
Prodromal labor contractions usually occur less than every five minutes and may stop for long periods. Once active labor begins, your contractions will become more and more frequent and will no longer start and stop.
The closer together your contractions are, the closer you are to meeting your baby. Real labor contractions get longer, stronger, and closer together and progress to delivery without stopping or slowing. Once labor is progressing well (usually once the mother is over 4 centimeters dilated), the labor won’t stop.
What causes prodromal labor?
There are several theories as to what causes prodromal labor, but the medical community hasn’t identified a specific cause. Most researchers seem to agree that prodromal labor is the body’s way of preparing for active labor. There are several potential contributing factors:
- The position of your baby: You may be more likely to experience prodromal labor if your baby is in breech position.
 The theory is that the uterus attempts to move the baby with contractions for a period of time and then stops if it doesn’t work.
The theory is that the uterus attempts to move the baby with contractions for a period of time and then stops if it doesn’t work. - Physical factor: An uneven pelvis or uterine abnormality may lead to these contractions.
- Feeling anxious or afraid: Apprehensive emotions either about your pregnancy or other things in your life may cause prodromal labor.
- History of previous pregnancies: This may be related to the way the uterus changes or relaxes after multiple pregnancies.
Prodromal labor isn’t usually a cause for concern and doesn’t mean that your baby is in distress. But if you do have concerns, you should always contact your healthcare provider.
Does prodromal labor mean active labor is near?
Prodromal labor can occur any time within the last month of your pregnancy. However, it doesn’t necessarily mean active labor is going to happen in the next day or even week. Labor and birth are unpredictable, so there’s really no good way to predict exactly when it will begin. Here are some common telltale signs that may signal that baby will soon be on the way.
Here are some common telltale signs that may signal that baby will soon be on the way.
Seeking help
Whether or not you need to contact your doctor or midwife will depend on your individual situation. In general, if your pregnancy is low risk, you likely won’t need to contact your healthcare provider if you’re experiencing prodromal labor.
However, it may be difficult to tell if your contractions are a sign of active labor or prodromal labor. You should always reach out to your healthcare providers if you have concerns and to rule out other problems.
What you can do to manage this condition
If you are close to your due date, try to stay active during contractions. This could include:
- staying upright
- walking around
- using a birthing ball
- dancing
Rest during periods where contractions have ceased. Remember to stay hydrated and nourished to keep your energy levels up. Use this time to practice your coping mechanisms for getting through each contraction. Breathing and relaxation techniques can be really useful.
Breathing and relaxation techniques can be really useful.
Last medically reviewed on August 22, 2017
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Angelini DJ, et al. (2013). Obstetric triage and emergency care protocols.
books.google.com/books?hl=en&lr=&id=A4f_gtPEOXcC&oi=fnd&pg=PA159&dq=prodromal+labor+pregnancy&ots=mrHcMRgTTI&sig=80ViknEOKy4VEvWp0OZr2gBaizw#v=onepage&q&f=false - Clark EAS, et al. (2015). Late preterm birth: An iatrogenic epidemic.
ajceog.us/files/ajceog0004598.pdf - True vs.
 false labor. (2016).
false labor. (2016).
my.clevelandclinic.org/health/articles/true-vs-false-labor
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Aug 22, 2017
Written By
Becky Young
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Becky Young on August 22, 2017
related stories
Abnormal Labor
When to Go to the Hospital for Labor
Labor and Delivery
6 Telltale Signs of Labor
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Read this next
Abnormal Labor
Medically reviewed by Nicole Galan, RN
Abnormal labor is labor that slows down or stops altogether.
 Learn why abnormal labor may occur and how it’s diagnosed.
Learn why abnormal labor may occur and how it’s diagnosed.READ MORE
When to Go to the Hospital for Labor
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Is it early labor or active labor? Is it true labor or false labor? Here are the signs that will tell you when to go to the hospital for labor.
READ MORE
Labor and Delivery
Medically reviewed by Bobbie Sue Whitworth, Ph.D., MSN, RNC
Labor and delivery tends to occupy the minds of expectant parents the most. Read on if you have questions about the signs and length of labor.
READ MORE
6 Telltale Signs of Labor
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
While every pregnancy and labor is different, here are six signs that labor is on the way.
 Talk to your doctor if you experience any of the following…
Talk to your doctor if you experience any of the following…READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt.
 Learn more about pregnancy after…
Learn more about pregnancy after…READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Does Swaddling Increase the Risk of SIDS?
Medically reviewed by Mia Armstrong, MD
Is swaddling safe, or is it a risk factor for SIDS? Here's what the most recent research says.

READ MORE
Prodromal Labor: Definition, Symptoms, and More
Prodromal Labor: Definition, Symptoms, and MoreMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Becky Young on August 22, 2017
What is prodromal labor?
Prodromal labor is labor that starts and stops before fully active labor begins. It’s often called “false labor,” but this is a poor description. Medical professionals recognize that the contractions are real, but they come and go and labor may not progress.
So, prodromal labor is real in terms of contraction pain and regularity. What makes these contractions different from contractions seen in active labor is that they start and stop.
Prodromal labor contractions will often come and go at the same time each day or at regular intervals. Many mothers, even experienced ones, end up calling their birth team or going to the hospital, thinking labor has begun.
Prodromal labor is really common and can start days, weeks, or even a month or more before active labor begins. Your health care provider will want you to deliver as close to 40 weeks (your due date) as possible. Prodromal labor isn’t an indication for induction or cesarean delivery.
Your health care provider will want you to deliver as close to 40 weeks (your due date) as possible. Prodromal labor isn’t an indication for induction or cesarean delivery.
Prodromal labor vs. Braxton-Hicks
Prodromal labor is often mistaken for Braxton-Hicks contractions, but they’re not the same thing. The majority of pregnant women will experience this type of contraction at some stage during their pregnancy. Braxton-Hicks are essentially practice contractions. They’re your body’s way of preparing for labor.
Braxton-Hicks contractions can cause a very tight, uncomfortable sensation, but they’re not typically regular or intense. They rarely last a long time or grow in intensity. Prodromal labor can follow a very regular pattern. The contractions can vary and grow in intensity.
It’s sometimes possible to ease Braxton-Hicks contractions by drinking water, eating, or relaxing. These activities won’t help ease prodromal labor contractions. Your cervix can also slowly dilate or efface during prodromal labor. This doesn’t usually happen with Braxton-Hicks contractions.
This doesn’t usually happen with Braxton-Hicks contractions.
Prodromal labor vs. active labor
Prodromal labor contractions usually occur less than every five minutes and may stop for long periods. Once active labor begins, your contractions will become more and more frequent and will no longer start and stop.
The closer together your contractions are, the closer you are to meeting your baby. Real labor contractions get longer, stronger, and closer together and progress to delivery without stopping or slowing. Once labor is progressing well (usually once the mother is over 4 centimeters dilated), the labor won’t stop.
What causes prodromal labor?
There are several theories as to what causes prodromal labor, but the medical community hasn’t identified a specific cause. Most researchers seem to agree that prodromal labor is the body’s way of preparing for active labor. There are several potential contributing factors:
- The position of your baby: You may be more likely to experience prodromal labor if your baby is in breech position.
 The theory is that the uterus attempts to move the baby with contractions for a period of time and then stops if it doesn’t work.
The theory is that the uterus attempts to move the baby with contractions for a period of time and then stops if it doesn’t work. - Physical factor: An uneven pelvis or uterine abnormality may lead to these contractions.
- Feeling anxious or afraid: Apprehensive emotions either about your pregnancy or other things in your life may cause prodromal labor.
- History of previous pregnancies: This may be related to the way the uterus changes or relaxes after multiple pregnancies.
Prodromal labor isn’t usually a cause for concern and doesn’t mean that your baby is in distress. But if you do have concerns, you should always contact your healthcare provider.
Does prodromal labor mean active labor is near?
Prodromal labor can occur any time within the last month of your pregnancy. However, it doesn’t necessarily mean active labor is going to happen in the next day or even week. Labor and birth are unpredictable, so there’s really no good way to predict exactly when it will begin.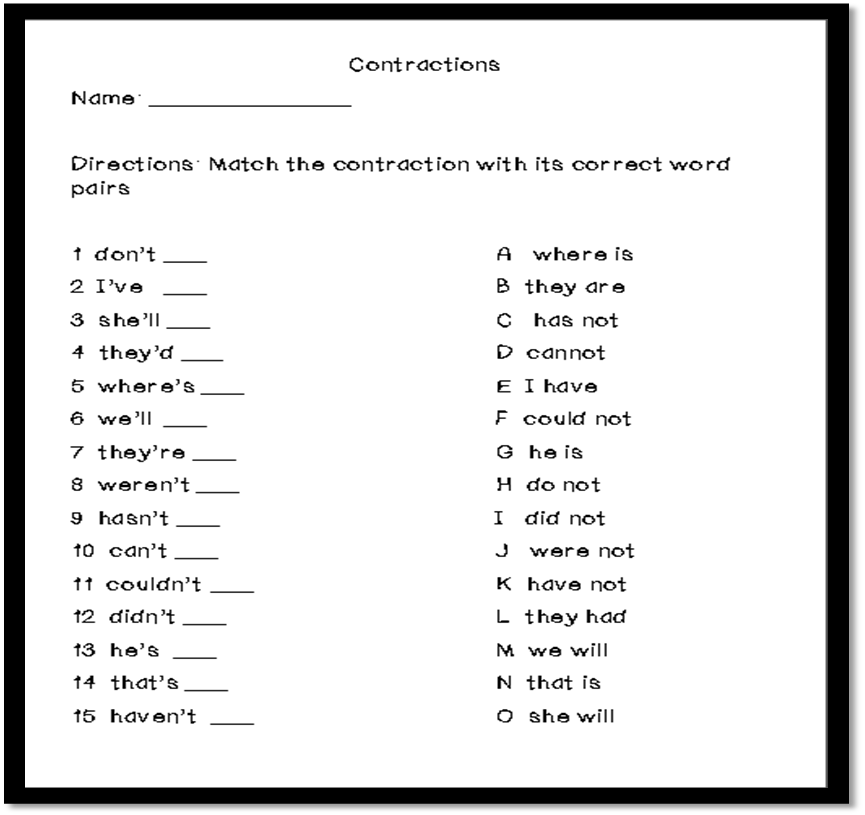 Here are some common telltale signs that may signal that baby will soon be on the way.
Here are some common telltale signs that may signal that baby will soon be on the way.
Seeking help
Whether or not you need to contact your doctor or midwife will depend on your individual situation. In general, if your pregnancy is low risk, you likely won’t need to contact your healthcare provider if you’re experiencing prodromal labor.
However, it may be difficult to tell if your contractions are a sign of active labor or prodromal labor. You should always reach out to your healthcare providers if you have concerns and to rule out other problems.
What you can do to manage this condition
If you are close to your due date, try to stay active during contractions. This could include:
- staying upright
- walking around
- using a birthing ball
- dancing
Rest during periods where contractions have ceased. Remember to stay hydrated and nourished to keep your energy levels up. Use this time to practice your coping mechanisms for getting through each contraction. Breathing and relaxation techniques can be really useful.
Breathing and relaxation techniques can be really useful.
Last medically reviewed on August 22, 2017
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Angelini DJ, et al. (2013). Obstetric triage and emergency care protocols.
books.google.com/books?hl=en&lr=&id=A4f_gtPEOXcC&oi=fnd&pg=PA159&dq=prodromal+labor+pregnancy&ots=mrHcMRgTTI&sig=80ViknEOKy4VEvWp0OZr2gBaizw#v=onepage&q&f=false - Clark EAS, et al. (2015). Late preterm birth: An iatrogenic epidemic.
ajceog.us/files/ajceog0004598.pdf - True vs.
 false labor. (2016).
false labor. (2016).
my.clevelandclinic.org/health/articles/true-vs-false-labor
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Aug 22, 2017
Written By
Becky Young
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Becky Young on August 22, 2017
related stories
Abnormal Labor
When to Go to the Hospital for Labor
Labor and Delivery
6 Telltale Signs of Labor
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Read this next
Abnormal Labor
Medically reviewed by Nicole Galan, RN
Abnormal labor is labor that slows down or stops altogether.
 Learn why abnormal labor may occur and how it’s diagnosed.
Learn why abnormal labor may occur and how it’s diagnosed.READ MORE
When to Go to the Hospital for Labor
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Is it early labor or active labor? Is it true labor or false labor? Here are the signs that will tell you when to go to the hospital for labor.
READ MORE
Labor and Delivery
Medically reviewed by Bobbie Sue Whitworth, Ph.D., MSN, RNC
Labor and delivery tends to occupy the minds of expectant parents the most. Read on if you have questions about the signs and length of labor.
READ MORE
6 Telltale Signs of Labor
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
While every pregnancy and labor is different, here are six signs that labor is on the way.
 Talk to your doctor if you experience any of the following…
Talk to your doctor if you experience any of the following…READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt.
 Learn more about pregnancy after…
Learn more about pregnancy after…READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Does Swaddling Increase the Risk of SIDS?
Medically reviewed by Mia Armstrong, MD
Is swaddling safe, or is it a risk factor for SIDS? Here's what the most recent research says.
READ MORE
Training bouts: sensations | How long do training contractions last during pregnancy
PreviousNext
- What are practice bouts?
- Why are they happening?
- What week do training bouts start?
- How long do practice bouts last?
- How does it feel during training bouts?
- Are training fights dangerous?
- How can I tell training contractions from labor contractions?
- Is it possible to calculate training bouts somehow easier?
- What to do?
Contents:
“I started having contractions, hurry to the maternity hospital!” yells the wife early Saturday morning. A sleepy husband drives a car through the streets of the city, and... at the next traffic light, it turns out that everything has passed. A happy but slightly bewildered couple stops by a nearby cafe for breakfast. Similar situations happen quite often, and training bouts are to blame. Let's figure out what they are and how to distinguish them from the real ones.
at the next traffic light, it turns out that everything has passed. A happy but slightly bewildered couple stops by a nearby cafe for breakfast. Similar situations happen quite often, and training bouts are to blame. Let's figure out what they are and how to distinguish them from the real ones.
What are practice bouts?
As the name suggests, they are not real. These contractions of the uterus are not directed to the beginning of the birth process. Usually they are irregular, rare and do not bring significant pain 1 .
This phenomenon has other names. Sometimes they are called even more obviously - false, as opposed to true labor pains. In specialized literature, you can find the term "Braxton-Hicks contractions" after the name of an English obstetrician-gynecologist 2 , who first drew attention to them and described them.
Why do they happen?
Medicine has no exact answer to this question. There is not even a consensus on whether they are part of the normal pregnancy process or a deviation from it. Most experts adhere to the first version, considering them to be a warm-up of the body before a real birth 3 .
Most experts adhere to the first version, considering them to be a warm-up of the body before a real birth 3 .
It is assumed that false contractions are needed to maintain the tone of the uterus - she, like any other muscular organ, requires periodic exercise. On the other hand, the time of arrival and the frequency of training contractions are very different for different women, and for some mothers who have successfully given birth, these sensations are not at all familiar.
What week do practice bouts start?
They can start already in the middle of pregnancy - from the 20th week 1 , in rare cases even earlier. 2–3 weeks before the planned date, their frequency often increases. In this period, they are called precursors, emphasizing that it is not long before the birth. However, even in the later stages, training contractions do not cause the cervix to open and continue to be only a preparation of the body for the main event.
Beginning of training bouts by weeks of pregnancy.
How long do practice bouts last?
Contractions last a few seconds, rarely up to 1 minute, and end as suddenly as 1 comes. Further, the expectant mother begins to listen to her feelings and wait for new ones, but they do not repeat. When the woman has already completely calmed down, the contractions can return after a considerable time - 4-5 hours.
After several unexpected cases, false contractions become habitual, and the expectant mother ceases to be afraid of them. However, in the last weeks until X hour, they can again surprise you - often training contractions before childbirth become longer and more intense.
In order not to confuse training contractions with real ones, you need to know about the harbingers of childbirth. We share all the necessary information here.
How does it feel during training bouts?
False contractions are not painful, but unfortunately, if this is your first pregnancy, you have nothing to compare. But there is another sure sign: all the muscles of the uterus participate in labor pains, and during training pain sensations are localized only in one area 4 .
But there is another sure sign: all the muscles of the uterus participate in labor pains, and during training pain sensations are localized only in one area 4 .
Periodicity and localization of training contractions of the second and the beginning of the third trimester, premonitory contractions, labor pains. Example.
False contractions usually present as muscle spasm in the back, front, or top of the uterus. The intervals between them are irregular, and it is impossible to predict where the attack will move next time. A few weeks before the birth, training contractions, which are now called precursor contractions, will become more frequent, but will retain their character - an attack localized in one area of the uterus. During labor pains, all the muscles of the uterus contract at the same time.
To know exactly how labor begins, read the signs and symptoms of labor.
Are training contractions dangerous?
There is no evidence that training contractions have any effect on fetal development. Their only danger is psychological. Some women, having felt unexpected contractions of the uterus, fall into a panic, and in this state they can do stupid things.
Their only danger is psychological. Some women, having felt unexpected contractions of the uterus, fall into a panic, and in this state they can do stupid things.
During pregnancy, you need to worry less. If something causes you mild anxiety, try to distract yourself. For example, take our fun quiz about what kind of mom you would be in the animal world.
Remember that the beginning of any contractions, even labor, does not mean that you will give birth in the next few minutes. There is time, so you need to calm down, take a deep breath, and listen to your feelings. If you're not sure if it's practice or real contractions, call your doctor and describe your symptoms. After listening to your answers, he will tell you what to do - go to the hospital or stay at home.
How to distinguish training contractions from labor contractions?
Expectant mothers almost accurately identify training contractions during the second and subsequent pregnancies.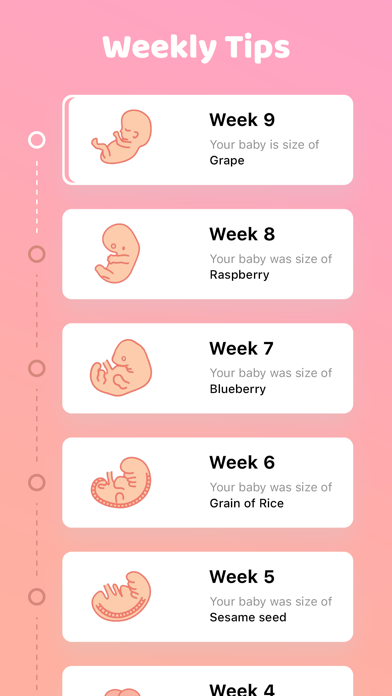 While you still have no experience, we recommend paying attention to the following signs 5 :
While you still have no experience, we recommend paying attention to the following signs 5 :
-
Training contractions are rarely painful, rather unexpected. What can not be said about labor - many women compare these sensations with very severe pain during menstruation.
-
Training contractions can usually be stopped. Leisurely walking around the room, breathing exercises and other calming exercises can completely eliminate discomfort in the uterus.
-
They do not differ in regularity and do not have obvious dynamics. In real fights, on the contrary, there is a regularity, a gradual increase in duration and a decrease in the interval between them.
For simplicity, we have collected the distinguishing features of false and true contractions in the table:
Is it possible to calculate training bouts somehow easier?
Mumlife contraction counter.
It just won't work. You still have to listen to your feelings and fix them. But you can get yourself an assistant - a special mobile application for calculating the duration and intervals between contractions. All of these apps work intuitively - all you have to do is press the big button each time an attack starts or ends.
In addition to recording and visualizing contractions, the application has useful additional functions. It tracks the dynamics of seizures and will tell you if it looks like a birth. And it will even show how much time you have left to get to the hospital.
What to do?
You can do nothing - after a while, the training bouts will pass by themselves. However, there are several proven methods 5 that help reduce the discomfort during false contractions and make them disappear quickly. Here are some of them:
-
Walk around the house.
Calm, slow walking in most cases allows you to get rid of unexpected uterine contractions.
 If the weather is good outside, and there is a place suitable for exercise nearby, you can get some fresh air at the same time - this will not be superfluous.
If the weather is good outside, and there is a place suitable for exercise nearby, you can get some fresh air at the same time - this will not be superfluous. -
Lie down and relax.
If you are not in the mood for walking right now, lie down on the couch or bed, take a comfortable position and think of something good. It is noticed that the best results are obtained by lying on the left side.
-
Take a bath or shower.
Water relaxes and is just what you need for training bouts. Fill the tub with water or stand under the shower and wait for the contractions to end there - most likely, this will happen very soon. But remember: only warm water, no hot baths and contrast showers!
-
Drink some water.
Dehydration can cause muscle cramps and is therefore also considered a factor in false contractions. Pour a glass of water and drink it slowly, alternating sips, inhales and exhales.
 Water can be replaced with some other drink, but only with a useful one, for example, berry juice or rosehip broth.
Water can be replaced with some other drink, but only with a useful one, for example, berry juice or rosehip broth. -
Do breathing exercises.
Proper breathing techniques are useful not only during training bouts. Before childbirth, they help to calm down, during childbirth - to relieve pain and better control your body. While the body is training the uterus, you are training your breathing.
-
Go to the toilet.
A full bladder is considered one of the culprits of false contractions: it puts pressure on the uterus, provoking its contractions. So before you settle into bed or go for a walk, do not forget to visit the toilet.
-
Walk around the house.
Calm, slow walking in most cases allows you to get rid of unexpected uterine contractions. If the weather is good outside, and there is a place suitable for exercise nearby, you can get some fresh air at the same time - this will not be superfluous.
-
Go to the toilet.
A full bladder is considered one of the culprits of false contractions: it puts pressure on the uterus, provoking its contractions. So before you settle into bed or go for a walk, do not forget to visit the toilet.
Sources:
-
Leah Hennen; Murray, Linda; Jim Scott (2005). The BabyCenter Essential Guide to Pregnancy and Birth: Expert Advice and Real-World Wisdom from the Top Pregnancy and Parenting Resource. Emmaus, Pa: Rodale Books. ISBN 1-59486-211-7.
-
John Braxton Hicks (1823-97) and painless uterine contractions.
-
Bhattacharya, Deepamala. Braxton Hicks Contractions.
-
The Physiological Difference Between Braxton Hicks and Labor Contractions.
-
Braxton Hicks or True Labor Contractions?
Follow us on Yandex Zen
what is happening, the development of pregnancy and fetus
Week by week
33 - 36 weeks of pregnancy
Elena Gevorkova
Obstetrician-gynecologist, Moscow
33rd week
BABY
At the 33rd week, the weight of the fetus is 1800-1900 g, and the body length is 43-44 cm. The amount of subcutaneous fat increases, due to which the folds and wrinkles on the baby's body are smoothed out, the skin turns pink. The fluffy hairs that cover the body of the fetus, which are called lanugo, become smaller, and the hair on the head darkens and thickens. The baby's skin is covered with a thin layer of cheese-like lubricant, its largest amount accumulates in the folds - axillary, cervical, inguinal - as well as on the back of the body and face. Grease is a viscous mass of white color, it is a secret of the sebaceous glands, mixed with skin scales. Its function is to protect the baby's skin from damage and facilitate its passage through the birth canal.
The amount of subcutaneous fat increases, due to which the folds and wrinkles on the baby's body are smoothed out, the skin turns pink. The fluffy hairs that cover the body of the fetus, which are called lanugo, become smaller, and the hair on the head darkens and thickens. The baby's skin is covered with a thin layer of cheese-like lubricant, its largest amount accumulates in the folds - axillary, cervical, inguinal - as well as on the back of the body and face. Grease is a viscous mass of white color, it is a secret of the sebaceous glands, mixed with skin scales. Its function is to protect the baby's skin from damage and facilitate its passage through the birth canal.
By this time, fetal movements gradually change their habitual character - they become more and more limited and less pronounced in amplitude due to insufficient space. However, the strength of the movements increases, since by this time the muscular system of the fetus is already sufficiently strengthened. Sharp and strong tremors of the fetus can be sensitive to the internal organs of a pregnant woman.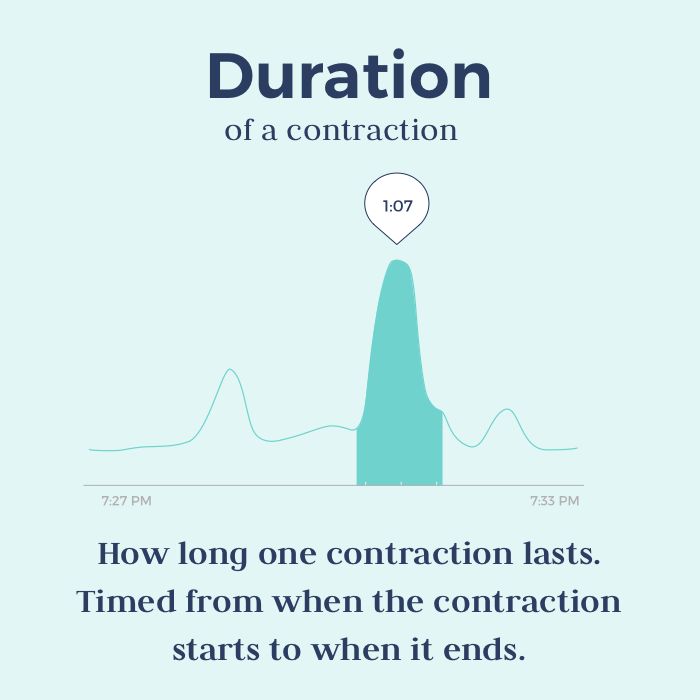 Depending on the position of the baby, the liver, stomach, bladder, ribs, etc. may “suffer”. By 33 weeks, the movements of the fetus are already quite coordinated.
Depending on the position of the baby, the liver, stomach, bladder, ribs, etc. may “suffer”. By 33 weeks, the movements of the fetus are already quite coordinated.
FUTURE MOTHER
The height of the fundus of the uterus from the level of the pubis at this time is 34 cm. The volume of the abdomen is increased due to the weight of the baby, placenta, amniotic fluid. The increase in uterine pressure and strong tremors of the fetus can cause some discomfort in the pregnant woman. Many movements previously available to the expectant mother, such as squats, become limited. Moderate physical activity - walking, fitness, etc. - Requires frequent respite.
A change in the center of gravity increases the load on the spine, which can manifest itself as pain in the lower back, sacrum, and pelvic region. The pressure of the uterus on the stomach can cause or increase nausea, heartburn, and a feeling of heaviness. An increase of almost 1 liter of the volume of circulating blood in the body of a pregnant woman increases the load on the kidneys, and the growing uterus puts pressure on the bladder. All this can be manifested by frequent urination.
All this can be manifested by frequent urination.
These ailments are usually associated with the mechanical pressure of the uterus on the surrounding organs; they are not symptoms of the disease and are temporary. And to relieve nausea, heartburn and a feeling of heaviness in the stomach, frequent meals in small portions are recommended.
34th week
BABY
By this time, the weight of the fetus is approximately 2100 g, and the height is 45 cm. From this period, the cheeks are very pronounced, because, developing a sucking reflex, the fetus often sucks its thumb. This leads to the fact that the baby strengthens the facial muscles, in particular the buccal. The total muscle mass of the fetus increases, the bones become denser.
The baby's internal organs are functioning intensively. During the day, he repeatedly swallows portions of amniotic fluid. Passing through the gastrointestinal tract, the amniotic fluid stimulates the work of the muscular wall. The dense part of the amniotic fluid, which is a suspension of skin flakes, lubricant, vellus hair, is processed by the enzymes of the liver and pancreas, and the liquid part is intensively excreted by the kidneys of the fetus.
The dense part of the amniotic fluid, which is a suspension of skin flakes, lubricant, vellus hair, is processed by the enzymes of the liver and pancreas, and the liquid part is intensively excreted by the kidneys of the fetus.
Approximately 500 ml of amniotic fluid is treated in this way per day. The production of bile continues, which accumulates in the gallbladder and, as the stomach fills with a suspension of amniotic water, enters the lumen of the small intestine. The functional development of the liver and pancreas during the prenatal period does not play a significant role, since the fetus does not have digestion; processes for the production of bile and enzymes: lipase, which breaks down fats; trypsin, which breaks down proteins; amylase, which breaks down carbohydrates, etc. - are preparatory in nature.
FUTURE MOTHER
Most pregnant women begin to feel rather intense false contractions at this time. Strictly speaking, false or training contractions, which are also called Braxton-Hicks contractions, can occur after the 20th week of pregnancy: the longer the period, the more frequent and pronounced the contractions.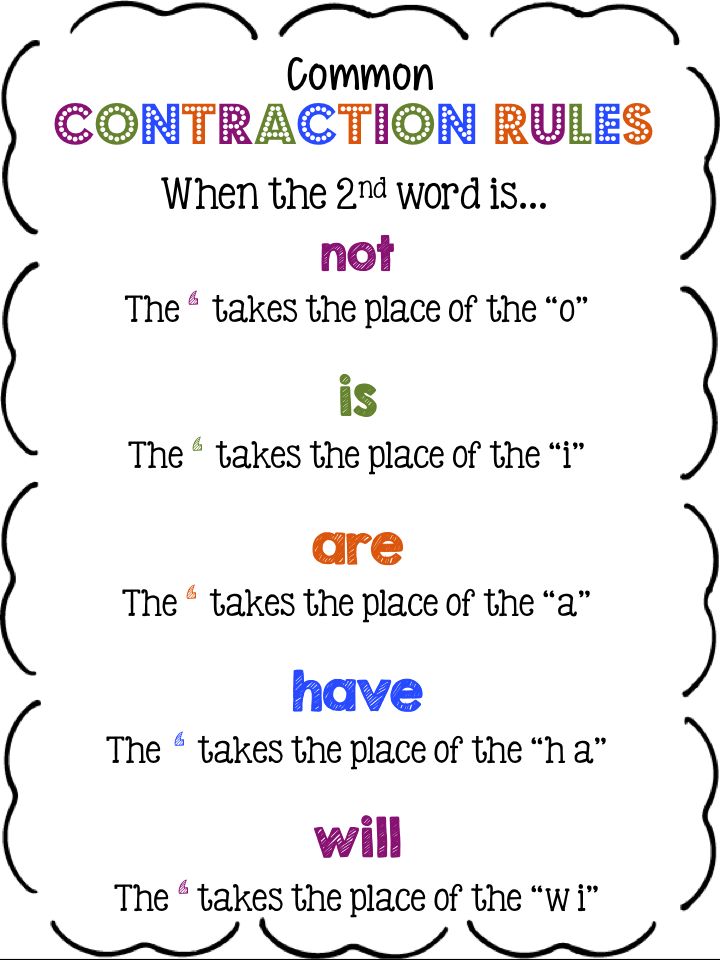 They are episodic contractions of the muscles of the uterus, lasting from a few seconds to 3-5 minutes. Braxton-Hicks contractions are not pathological - this is a completely normal process of preparing the muscles of the uterus for the difficult process of childbirth. This phenomenon with varying degrees of intensity is observed in almost all pregnant women.
They are episodic contractions of the muscles of the uterus, lasting from a few seconds to 3-5 minutes. Braxton-Hicks contractions are not pathological - this is a completely normal process of preparing the muscles of the uterus for the difficult process of childbirth. This phenomenon with varying degrees of intensity is observed in almost all pregnant women.
Many primiparas are concerned about the difference between preparatory contractions and labor.
Here are some differences:
- Frequency of contractions. Training bouts do not become more frequent, the intervals between them may be different. Labor pains are regular, the interval between them is reduced.
- Duration of contractions. Training bouts have different durations, from a few seconds to minutes, their duration does not increase over time. Labor pains tend to lengthen.
- Soreness. Preparatory contractions may not be accompanied by pain at all, or they may be quite noticeable, up to a feeling of sharp pain.
 However, their intensity weakens over time and the pain disappears. Labor pains are painful and constantly intensify.
However, their intensity weakens over time and the pain disappears. Labor pains are painful and constantly intensify. - Localization. Braxton-Hicks contractions can be felt in various places - in the lower part of the uterus, in the region of its bottom, along the side walls, covering the entire abdomen. Labor pains begin with a contraction of the lower abdomen, spreading to the front. Often in childbirth, pain in the lower back is felt, while the nature of the pain resembles menstrual pain.
- Relationship with body position. Preparatory contractions may disappear after walking or, on the contrary, rest. A change in body position can relieve the tension in some muscles, which also causes a decrease in the appearance of training contractions. Labor pains may be somewhat relieved in a certain position - when leaning forward, in the knee-elbow position, etc. - but their frequency and duration will still increase.
- Reaction to medication. The use of antispasmodic drugs - NO-ShPY, BUSCOPAN, PAPAVERIN, etc.
 - approved by the attending physician, can weaken or completely stop false contractions. The effect of antispasmodics on labor pains is minimal.
- approved by the attending physician, can weaken or completely stop false contractions. The effect of antispasmodics on labor pains is minimal.
Any pain or discomfort should be reported to the gynecologist: this will help the expectant mother to resolve doubts and cope with anxiety. Feeling safe is the best companion of pregnancy.
35th week
BABY
The body length of the fetus is 46-47 cm, weight - 2200-2300 g. These figures in the last weeks of pregnancy can vary greatly. The growth and weight of the fetus largely depend on heredity, individual parameters. Starting from 35 weeks, the baby will gain 200-250 g weekly. The fetus occupies almost the entire uterine cavity, its back is rounded, arms and legs are bent, brought to the body. The layer of subcutaneous fat increases significantly, which significantly “rounds” the body of the fetus. The closing of the eyelids and the contraction of facial muscles change the baby's facial expression quite often. The skin of the body becomes pink, smooth, the amount of cheese-like lubricant begins to decrease. Vellus hair covers separate small areas of the body - shoulders, back. The nails protrude beyond the tips of the fingers.
The skin of the body becomes pink, smooth, the amount of cheese-like lubricant begins to decrease. Vellus hair covers separate small areas of the body - shoulders, back. The nails protrude beyond the tips of the fingers.
FUTURE MOTHER
The fundus of the uterus is 35 cm higher from the pubis and 15 cm higher from the navel. particularly light. The growing uterus does not allow the lungs to expand, respiratory movements are limited, which is manifested by shortness of breath. Almost all pregnant women to one degree or another experience a feeling of shortness of breath - a feeling of lack of air, frequent and shallow breathing, a desire to take a deep breath. As a rule, these sensations occur for a period of 28 weeks and reach their peak at the 35-36th week. After 37 weeks of pregnancy, the abdomen droops, which greatly facilitates breathing.
Shortness of breath during pregnancy is associated not only with the mechanical pressure of the uterus on the diaphragm, but also with the relaxing effect of hormones on the muscles of the bronchi and lungs. Most often, it is provoked by physical activity - climbing stairs, a long walk, etc. However, it is not uncommon for shortness of breath to occur at rest, especially when lying down. Both prolonged lying in a horizontal position and excessive exercise can contribute to increased shortness of breath. To alleviate her condition, the expectant mother needs to be rational about the daily routine - it is reasonable to alternate rest and physical activity. It is important to monitor your posture, as slouching exacerbates shortness of breath, reducing the already insufficient lung capacity. If shortness of breath is accompanied by blue lips or nails, sensations of pain behind the sternum, darkening before the eyes, nausea or vomiting, fainting, then an urgent need to consult a doctor.
Most often, it is provoked by physical activity - climbing stairs, a long walk, etc. However, it is not uncommon for shortness of breath to occur at rest, especially when lying down. Both prolonged lying in a horizontal position and excessive exercise can contribute to increased shortness of breath. To alleviate her condition, the expectant mother needs to be rational about the daily routine - it is reasonable to alternate rest and physical activity. It is important to monitor your posture, as slouching exacerbates shortness of breath, reducing the already insufficient lung capacity. If shortness of breath is accompanied by blue lips or nails, sensations of pain behind the sternum, darkening before the eyes, nausea or vomiting, fainting, then an urgent need to consult a doctor.
36th week
BABY
The growth of the fetus by this term is approximately 47-48 cm, and the weight is about 2300-2500 g. The fetus enters a period of intensive preparation for childbirth. Each of the organs is already functionally mature enough to ensure the viability of the fetus. 36 weeks is the beginning of the preparatory journey, and the upcoming weeks of pregnancy are designed to finally form the baby's readiness for extrauterine life.
Each of the organs is already functionally mature enough to ensure the viability of the fetus. 36 weeks is the beginning of the preparatory journey, and the upcoming weeks of pregnancy are designed to finally form the baby's readiness for extrauterine life.
By 36 weeks, the fetus is in its final position in the uterus. As a rule, this is a longitudinal position, occipital presentation - in this case, the fetus is located head down, facing the mother's back. This is the most comfortable position that ensures the greatest safety of the baby during childbirth. More rarely, breech presentation is a condition in which the buttocks and legs of the fetus are located at the bottom of the uterus. This is a relative indication for operative delivery. The final decision on caesarean section or independent childbirth is made by doctors in each case individually.
A change in the position of the fetus in the uterus is possible, but this happens infrequently, since at this time the fetus occupies almost all the free space in the uterus, which significantly limits its motor activity. As a rule, if a change in the position of the fetus occurs, then only from the pelvic to the head. The reverse cases - the transition of the baby from the head position to the pelvic position - are practically impossible, since the head of the fetus is heavier than the buttocks and occupies the longitudinal position completely, by analogy with a float in water, the heavy part of which always outweighs.
As a rule, if a change in the position of the fetus occurs, then only from the pelvic to the head. The reverse cases - the transition of the baby from the head position to the pelvic position - are practically impossible, since the head of the fetus is heavier than the buttocks and occupies the longitudinal position completely, by analogy with a float in water, the heavy part of which always outweighs.
FUTURE MOTHER
The height of the uterus is 36 cm, the volume of the abdomen is maximally increased, the bottom reaches the costal arches. At this time, the pregnant woman's body also begins its journey of preparing for the upcoming birth. Changes begin with hormonal changes: the level of special hormones, oxytocin and prostaglandins, increases slightly in a woman. These active substances play a crucial role in the process of preparing for childbirth and directly during them. A slight increase in their level from the period of 36-37 weeks of pregnancy leads to an increase in Braxton-Hicks training contractions, an increase in urination and defecation, and the appearance of more abundant mucous discharge from the vagina.