How long does it take to stop bleeding after birth
Bleeding after birth: 10 things you need to know | Life as a parent articles & support
It may be one of the few things you haven’t discussed with friends. Here’s an honest, clear account of what you can expect with bleeding after birth.
1. Every woman bleeds after they give birth
You will have vaginal bleeding after you’ve given birth(NHS, 2021). This bleeding is known as lochia. The lochia is a combination of mucous, tissue and blood that your womb sheds as it replaces its lining after you’ve given birth (UHS NHS Foundation Trust, 2020).
2. Bleeding after birth may last for a while
Bleeding often lasts for around for four to six weeks, but could last up to 12 weeks after your baby's born (RCOG, 2016). If you’re worried, you can talk to a health professional.
Bleeding will start off heavy and red to browny red. It will become lighter in colour and flow over time (NHS, 2021).
Here’s what you can expect:
- Day 1: Fresh red to brownish-red blood.
Heavy flow that probably soaks one maternity pad every few hours, with one or two clots or several smaller ones.
- Day 2 to 6: Darker brown or pinkish red blood. Moderate flow with 7 cm to 12 cm stains on your maternity pads and smaller blood clots.
- Day 7 to 10: Darker brown or pinkish red blood, becoming lighter. Variable but lighter flow, with less than a 7 cm stain on your pads.
- Days 11 to 14: Darker brown or pinkish red blood, becoming lighter. Lighter flow, you may have some sanitary towels that are hardly stained.
- Week 3 to 4: Paler, possibly a creamy white blood loss. Lighter flow.
- Week 5 to 6: Brown, pinkish red, or creamy yellow stains, possibly for several weeks, and possibly only on some days (UHS NHS Foundation Trust, 2020).
3. Don’t keep quiet about clots
They’re common. Discuss any clots with your midwife as she’ll want to keep track of what’s happening. Save your maternity pads to show your midwife if possible. Passing a lot of large clots can flag up something more serious (NHS, 2021).
Passing a lot of large clots can flag up something more serious (NHS, 2021).
4. If you pass a lot of large blood clots or more than a pint of blood in the first 24 hours, talk to a health professional immediately
Passing lots of large blood clots or more than a pint of blood in the first 24 hours after birth are symptoms of primary postpartum haemorrhage (RCOG, 2016).
Severe postnatal blood loss can make you feel even more exhausted than is normal after giving birth but it can also be life threatening. Getting quick treatment is essential before it becomes a major haemorrhage.
Treatment normally involves helping your uterus to contract through massaging the belly, an injection to contract the uterus, and a catheter into your bladder. The doctors will check to make sure all of the placenta has come out, and may have to do this under general anaesthetic. You will also have a drip in your arm and blood taken for tests.
5. The risk factors for primary postpartum haemorrhage
Before labour, risk factors are:
- Previous postpartum haemorrhages
- A body mass index (BMI) above 35
- A twin or triplet pregnancy
- Low-lying placenta (placenta previa)
- Placenta coming away early (placental abruption)
- Pre-eclampsia or high blood pressure
- Anaemia
- Growths in or around the womb (e.
 g. fibroids)
g. fibroids) - Taking blood-thinning medication
- Blood clotting problems.
During labour, risk factors are:
- Caesarean section birth
- Induced labour
- Retained placenta
- Episiotomy
- Forceps or vacuum-assisted vaginal delivery (ventouse) birth
- Your labour lasted longer than 12 hours
- Having a baby that weighs more than 4kg (9lbs)
- Having your first baby when you’re over 40 years old
- Having a raised temperature during labour
- Having a general anaesthetic.
(RCOG, 2016)
6. Think about postpartum bleeding when you pack your hospital bag
Pack maternity pads rather than menstrual pads as they’ll be more absorbant and allow the area between the vagina and anus (perineum) to heal with the least irritation. Describing the number of maternity pads you’re using also gives your midwife a clear picture of how much blood loss you’re experiencing.
7. Lots of things can affect the amount of blood loss
Breastfeeding makes your body release oxytocin. This makes your womb contract so it releases the lochia blood more quickly (but it will be the same amount of blood overall).
This makes your womb contract so it releases the lochia blood more quickly (but it will be the same amount of blood overall).
Any sort of gentle exercise – even a quick vacuum of the lounge – could also make bleeding heavier. This is especially true in the first two weeks.
Bleeding will tend to be heavier in the morning too. This is because blood pools when you lay down sleeping.
8. It’s important to keep an eye on your blood loss in the weeks after giving birth
It’s possible to get secondary postpartum haemorrhage, which is abnormal or heavy bleeding between 24 hours and 12 weeks after giving birth. It’s often associated with an infection, and sometimes with part of the placenta remaining in the womb (RCOG, 2016).
Symptoms include:
- Feeling shaky, feverish, and generally ill.
- Having lochia with an offensive smell.
- Heavier than expected bleeding, or bleeding that becomes heavier rather than lighter over time. (UHS NHS Foundation Trust, 2015; RCOG, 2016)
If you have any of these symptoms, you should speak to your GP or health visitor immediately (RCOG, 2016). Treatment for an infection includes antibiotics, so remind the health professional if you are breastfeeding so they can select the most appropriate antibiotic.
Treatment for an infection includes antibiotics, so remind the health professional if you are breastfeeding so they can select the most appropriate antibiotic.
Severe pain in the womb in the six weeks after birth could be a sign of a serious infection called sepsis, and should be treated with urgency because it can be life-threatening (RCOG, 2012). Other symptoms of sepsis include a high or low temperature, vomiting, diarrhoea, a rash and offensive discharge (RCOG, 2012). If you are experiencing these symptoms, go straight to the emergency department, say that you have recently given birth, and ask if this could be sepsis.
9. It’s important to reduce your risk of infection
Wash your hands thoroughly before and after using the toilet and changing your maternity pad (NICE, 2021).
10. Always speak to your GP or health visitor if anything doesn’t feel right
In the end, trust your judgement. If you have any worries about your bleeding after you give birth, talk to a health professional. They’re there to help.
They’re there to help.
This page was last reviewed in November 2021
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
You might find attending one of our Early Days groups helpful as they give you the opportunity to explore different approaches to important parenting issues with a qualified group leader and other new parents in your area.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby.
What's Normal, What's Not, Causes, Treatment
Written by Paige Fowler
In this Article
- What's Normal
- When to Call Your Doctor
- What Causes It?
- How It's Treated
If you have a vaginal delivery or Cesarean section, you’ll have vaginal bleeding and discharge after birth. This is known as lochia. It’s how your body gets rid of the extra blood and tissue in your uterus that helped your baby grow.
This is known as lochia. It’s how your body gets rid of the extra blood and tissue in your uterus that helped your baby grow.
Bleeding is heaviest the first few days after your baby is born. But if heavy bleeding continues after that, you may need to call your doctor.
What's Normal
Your blood will be bright red, and you may see some clots for the first few days after you give birth. They shouldn’t be bigger than a quarter. You’ll have to wear a hospital-grade pad at first. But you should be able to go back to a regular pad later.
You might bleed a little more when you bring your baby home. This may be because you’re moving around a lot. If this happens, try to stay off your feet and rest a little.
It’s also normal to sometimes feel a gush of blood when you stand. This is because of the way your vagina is shaped. The blood collects in a cup-like area while you’re sitting or lying down. When you stand, it comes out.
After about 10 days, you should see less blood. You may have light bleeding or spotting for up to 6 weeks after delivery. You can only use sanitary pads during this time. Tampons could lead to an infection.
You may have light bleeding or spotting for up to 6 weeks after delivery. You can only use sanitary pads during this time. Tampons could lead to an infection.
When to Call Your Doctor
Heavy bleeding after giving birth is called postpartum hemorrhage. It affects up to 5% of women who give birth. It’s most likely to happen the first 24 hours after delivery. But it can happen anytime within the first 12 weeks after your baby is born.
Postpartum hemorrhage is serious. It can cause a big drop in your blood pressure. If the pressure gets too low, your organs won’t get enough blood. This is shock, and it can cause death. That’s why it’s important to get medical help right away.
Tell your doctor or call 911 if you have any of these symptoms or signs:
- Bright red bleeding beyond the third day after birth
- Blood clots bigger than a plum
- Bleeding that soaks more than one sanitary pad an hour and doesn’t slow down or stop
- Blurred vision
- Chills
- Clammy skin
- Rapid heartbeat
- Dizziness
- Weakness
- Nausea
- Faint feeling
What Causes It?
Certain things can raise your chance of postpartum hemorrhage. You’re at higher risk if you’ve had it before. For unknown reasons, Asian and Hispanic women are more likely to have it.
You’re at higher risk if you’ve had it before. For unknown reasons, Asian and Hispanic women are more likely to have it.
The most common cause of postpartum hemorrhage is something called uterine atony. Normally, the uterus squeezes after delivery to stop bleeding where the placenta was. The placenta is an organ that grows in your uterus during pregnancy and nourishes your baby. With uterine atony, the uterus doesn’t contract as well as it should. This can cause heavy bleeding after you give birth.
You may be more likely to have this if you:
- Give birth to more than one child at a time (twins, for example)
- Have a baby bigger than 8 pounds 13 ounces
- Are in labor for a long time
- Have given birth several times before
Other conditions can raise your risk for postpartum hemorrhage. These include:
- Uterine rupture -- when the uterus tears during labor
- Cesarean section -- your risk for postpartum hemorrhage is higher compared with a vaginal delivery
- Tears in the vagina or cervix during delivery
- General anesthesia -- this may be used if you have a Cesarean section
- Oxytocin (Pitocin) -- a medicine that makes you go into labor
- Preeclampsia -- high blood pressure and protein in your urine that develops during pregnancy
- Obesity
- Issues that affect the placenta
How It's Treated
There are many different treatments for postpartum hemorrhage. The cause of your bleeding will help your doctor decide what may be best for you.
The cause of your bleeding will help your doctor decide what may be best for you.
They could:
- Give you medicine to help your uterus contract
- Massage your uterus
- Remove pieces of the placenta still in your uterus
- Perform a laparotomy -- surgery to open your abdomen to find out the cause of bleeding and stop it
- Give you a blood transfusion -- blood is given to you through a tube that goes in a vein to help replace blood you've lost
- Perform a hysterectomy -- surgical removal of the uterus
- Give you a shot of a special medicine to stop the bleeding
- Have a radiologist do what's called a uterine artery embolization, which limits blood flow to your uterus
- Use something called a Bakri balloon that's inflated inside your uterus and adds pressure to help slow the bleeding
Sitemap
|
|
What is the best drug to reduce excessive blood loss after childbirth?
What is the problem?
The aim of this Cochrane review was to find out which drug is most effective in preventing excessive blood loss in labor and has the fewest side effects.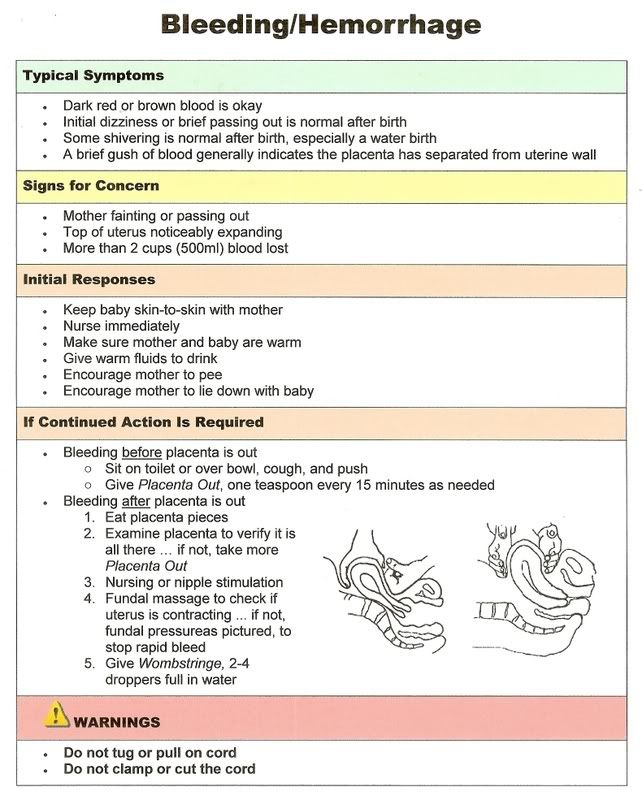 We collected and analyzed all relevant studies to answer this question (search date: May 24, 2018).
We collected and analyzed all relevant studies to answer this question (search date: May 24, 2018).
Why is this important?
Excessive blood loss after childbirth (postpartum haemorrhage) is a common cause of maternal death during childbirth worldwide. Although most women experience moderate blood loss during childbirth, some women may experience excessive blood loss and this can pose a serious risk to their health and life. To reduce excessive bleeding in childbirth, the administration of a uterine contraction agent (uterotonic) has become standard practice throughout the world.
Various medications are routinely used in childbirth to reduce excessive bleeding. These are oxytocin, misoprostol, ergometrine, carbetocin, injectable prostaglandins, and combinations of these drugs, each with varying efficacy and side effects. Some reported side effects include vomiting, high blood pressure, and fever. Oxytocin is currently recommended as the standard treatment for reducing excess bleeding. We reviewed all available evidence to compare the efficacy and side effect profile of each drug.
We reviewed all available evidence to compare the efficacy and side effect profile of each drug.
What evidence did we find?
We found 196 studies involving 135,559 women. We compared seven uterotonics with each other and with no uterotonic treatment. The studies were carried out in 53 countries. In most studies, women gave birth naturally in a hospital setting.
This analysis suggests that all drugs are effective in preventing blood loss equal to or greater than 500 ml compared to no standard uterotonic treatment. Compared with oxytocin (the standard recommended treatment), the top three treatments for this outcome were ergometrine plus oxytocin, carbetocin, and misoprostol plus oxytocin. We found that other drugs such as misoprostol, injectable prostaglandins, ergometrine may not (or only slightly) affect this outcome compared to oxytocin.
All drugs except ergometrine and injectable prostaglandins are effective in preventing blood loss equal to or greater than 1000 ml compared to no treatment. The combination of ergometrine with oxytocin and the combination of misoprostol with oxytocin do not (or only slightly) affect this outcome compared to oxytocin. Uncertainty remains as to whether carbetocin and ergometrine alone affect this outcome. However, misoprostol is less effective in preventing blood loss equal to or greater than 1000 ml compared to oxytocin.
The combination of ergometrine with oxytocin and the combination of misoprostol with oxytocin do not (or only slightly) affect this outcome compared to oxytocin. Uncertainty remains as to whether carbetocin and ergometrine alone affect this outcome. However, misoprostol is less effective in preventing blood loss equal to or greater than 1000 ml compared to oxytocin.
Misoprostol in combination with oxytocin reduces the use of additional uterotonics and probably reduces the risk of blood transfusion compared to oxytocin. Carbetocin, injectable prostaglandins, and the combination of ergometrine with oxytocin may also reduce the use of additional uterotonics, but the evidence is low-certainty. No significant differences were found between all agents in terms of maternal mortality or severe complications in childbirth, as these were rare in these studies.
Two drug combinations were associated with significant side effects. Compared with the oxytocin group, women who received misoprostol plus oxytocin were more likely to experience vomiting and fever. Women who received the combination of ergometrine and oxytocin were also more likely to vomit, and the combination may not (or only slightly) affect the risk of hypertension, but the evidence for this outcome was low-certainty.
Women who received the combination of ergometrine and oxytocin were also more likely to vomit, and the combination may not (or only slightly) affect the risk of hypertension, but the evidence for this outcome was low-certainty.
The analysis performed was similar whether women delivered vaginally or by caesarean section, in hospital or at home, at high or low risk of PPH, were receiving high or low dose misoprostol, and whether they received bolus or infusion of oxytocin, or both.
What does this mean?
All agents were generally effective in preventing excess bleeding compared with no treatment with uterotonic agents. The combination of ergometrine with oxytocin, carbetocin, and the combination of misoprostol with oxytocin may have additional benefits compared to standard administration of oxytocin. However, these two drug combinations are associated with significant side effects that may be worrisome for women when compared to oxytocin. Carbetocin may have some additional benefit over oxytocin, and does not appear to increase side effects.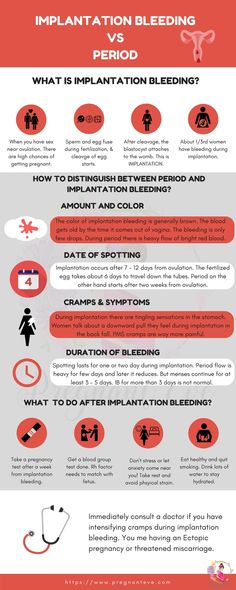
 Practice
Practice