How does cmv affect pregnancy
CMV Fact Sheet for Pregnant Women and Parents
Español (Spanish)
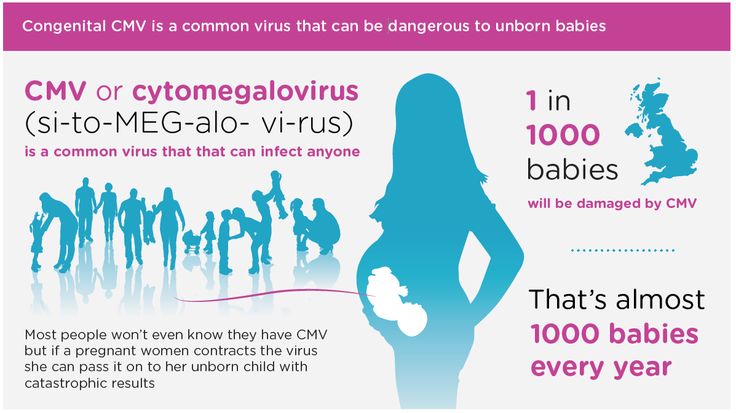
Most people have been infected with cytomegalovirus (CMV), but do not have symptoms. If a pregnant woman is infected with CMV, she can pass it to her developing baby. This is called congenital CMV, and it can cause birth defects and other health problems.
For pregnant women
You can pass CMV to your baby
If you are pregnant and have CMV, the virus in your blood can cross through your placenta and infect your developing baby. This is more likely to happen if you have a frst-time CMV infection while pregnant but can also happen if you have a subsequent infection during pregnancy.
You are not likely to be tested for CMV
It is not recommended that doctors routinely test pregnant women for CMV infection. This is because laboratory tests cannot predict which developing babies will become infected with CMV or have long-term health problems.
You may be able to reduce your risk
You may be able to lessen your risk of getting CMV by reducing contact with saliva and urine from babies and young children. The saliva and urine of children with CMV have high amounts of the virus. You can avoid getting a child’s saliva in your mouth by, for example, not sharing food, utensils, or cups with a child. Also, you should wash your hands after changing diapers. These cannot eliminate your risk of getting CMV, but may lessen the chances of getting it.
For parents
About 1 out of every 200 babies is born with congenital CMV. About 1 out of 5 of these babies will have birth defects or other long-term health problems.
Babies with congenital CMV may show signs at birth
Some signs that a baby might have congenital CMV infection when they are born are:
- Small head size
- Seizures
- Rash
- Liver, spleen, and lung problems
Tests on a baby’s saliva, urine, or blood done within two to three weeks after birth can confirm if the baby has congenital CMV.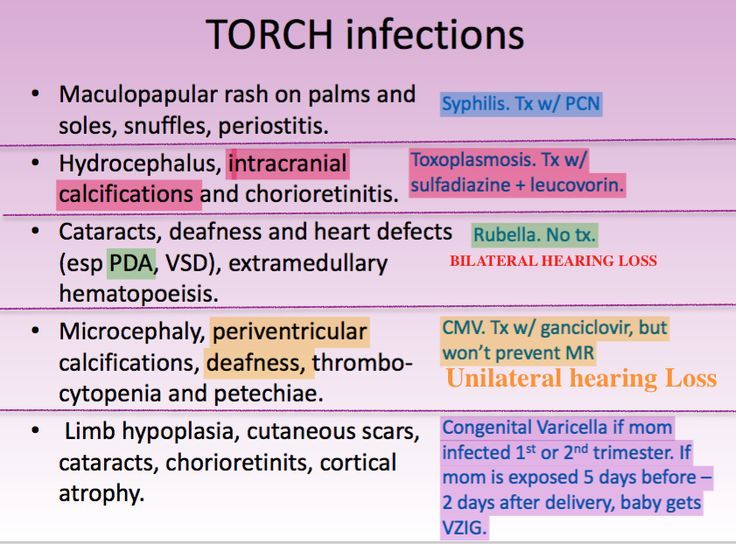
Early treatment may help
Babies who show signs of congenital CMV at birth may be treated with medicines called antivirals. Antivirals may decrease the severity of health problems and hearing loss but should be used with caution due to side effects.
Long-term health problems may occur
Babies with signs of congenital CMV at birth are more likely to have long-term health problems, such as:
- hearing loss
- intellectual disability
- vision loss
- seizures
- lack of coordination or weakness
Some babies with congenital CMV but without signs of disease at birth may still have or develop hearing loss. Hearing loss may be present at birth or may develop later in babies who passed their newborn hearing test. Sometimes, hearing loss worsens with age.
Hearing checks and therapies are recommended
Children with congenital CMV should have regular hearing checks. Children with hearing loss should receive services such as speech or occupational therapy.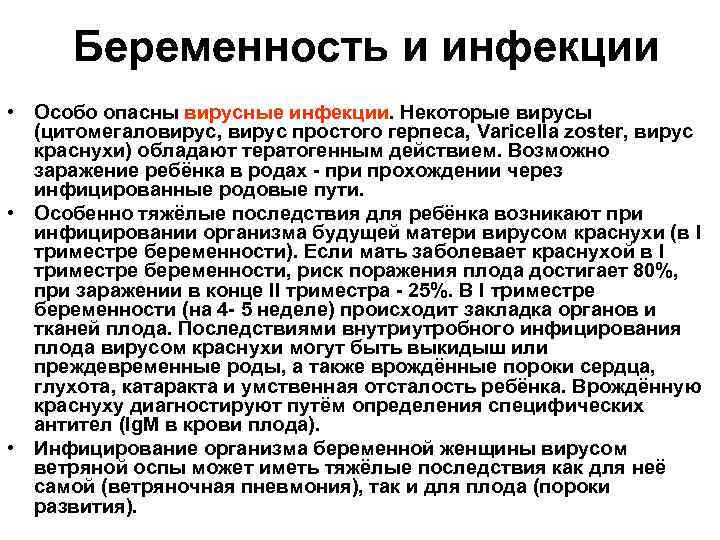 These services help ensure they develop language, social, and communication skills.
These services help ensure they develop language, social, and communication skills.
The earlier your child can get hearing checks and therapies, the more he or she can benefit from them.
Download the print version and share pdf icon[1 page]
Cytomegalovirus and pregnancy | March of Dimes
Cytomegalovirus (also called CMV) is the most common infection passed from pregnant people to babies during pregnancy.
More than half of adults have been infected with CMV by age 40 but most don’t know they’ve been infected.
Once you’re infected with CMV, it stays in your body for the rest of your life.
If you get infected with CMV during pregnancy, it may cause pregnancy loss or serious health problems in your baby, including preterm birth or low birthweight, or hearing loss at birth or later in life.
CMV is the leading cause of hearing loss in this country, causing 1 in 3 cases of hearing loss.
What is cytomegalovirus?
Cytomegalovirus (also called CMV) is a common virus that infects people of all ages. More than half of adults in the United States become infected with CMV by age 40. Once CMV is in your body, you have it for the rest of your life. The virus can reactivate and cause another infection. You can also be re-infected with a different strain (variety) of the virus.
More than half of adults in the United States become infected with CMV by age 40. Once CMV is in your body, you have it for the rest of your life. The virus can reactivate and cause another infection. You can also be re-infected with a different strain (variety) of the virus.
Most people with CMV infection have no symptoms and aren’t aware that they have been infected. CMV infection usually isn’t harmful in healthy adults or children because their immune system protects their bodies from infection. But CMV can cause serious health problems for some, including:
- Babies who get infected before birth
- Preterm babies (babies born before 37 weeks of pregnancy) or low birthweight babies (babies born weighing less than 5 pounds, 8 ounces)
- People with weakened immune systems. People with weak immune systems include people living with a serious illness, like HIV, people getting treatment for cancer and people who’ve had a bone marrow or organ transplant.
CMV is the most common infection passed from pregnant people to babies during pregnancy. One in 3 pregnant people passes the infection on to their babies. If you have CMV during pregnancy, the virus in your blood can pass through the placenta to your baby. The placenta supplies the baby with food and oxygen through the umbilical cord. It’s possible for CMV to cause the death of a baby during pregnancy (pregnancy loss).
One in 3 pregnant people passes the infection on to their babies. If you have CMV during pregnancy, the virus in your blood can pass through the placenta to your baby. The placenta supplies the baby with food and oxygen through the umbilical cord. It’s possible for CMV to cause the death of a baby during pregnancy (pregnancy loss).
When a baby gets CMV during pregnancy, it’s called congenital CMV. Congenital means that it’s present at birth. One in 200 babies in the U.S. is born with CMV. Most babies with congenital CMV don’t have problems, but some get sick or have long-term health problems. A baby also may get infected after birth if they come in contact with infected body fluids.
There’s no cure for CMV, but medicines can help treat CMV in newborns and people with weak immune systems.
CMV is part of the family of herpes viruses. It’s related to the viruses that cause chickenpox, herpes simplex (also called HSV) and mononucleosis (also called mono). Once you’re infected with CMV, it stays in your body for life. If you’re healthy, CMV usually stays inactive but it can become active again, especially if you get a disease or take medicine that weakens your immune system. You also can get infected again with a different strain of the virus.
If you’re healthy, CMV usually stays inactive but it can become active again, especially if you get a disease or take medicine that weakens your immune system. You also can get infected again with a different strain of the virus.
What are the signs and symptoms of CMV?
Most people with CMV don’t know they have the infection because they don’t have signs or symptoms. Signs and symptoms of CMV can be different in healthy people, babies and people with weak immune systems.
Signs and symptoms of CMV in healthy people may include:
- Chills and/or sweats
- Decreased appetite
- Fatigue (being very tired and having little energy)
- Fever
- Headache
- Muscle aches
- Sore throat
- Swollen glands
CMV sometimes can cause hepatitis and mononucleosis (mono). Hepatitis is a disease caused by a virus that attacks the liver. Mono is a disease that can cause extreme fatigue, head and body aches, sore throat, swollen lymph nodes and swollen spleen or liver.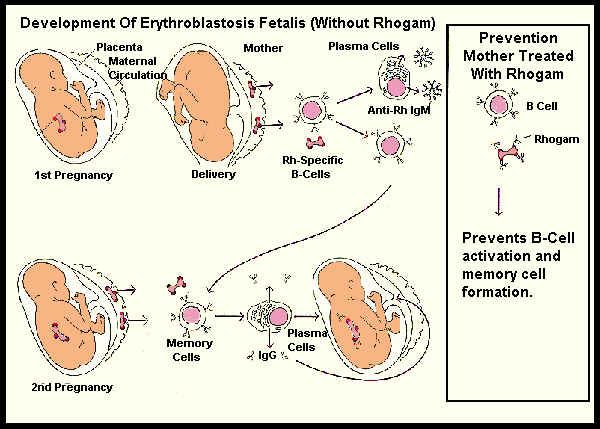
People with weakened immune systems who get CMV can have more serious problems that can affect the eyes, lungs, liver, esophagus, stomach and intestines. The esophagus is the tube that connects the mouth and stomach. The intestines are long tubes that help your body break down (digest) food.
People who are more likely to have the signs and symptoms of CMV include:
- Babies who became infected with CMV before they are born (congenital CMV).
- Babies who become infected during birth or shortly after (perinatal CMV). This group includes babies infected while nursing.
- People who have weakened immune systems, such as those who have had an organ, bone marrow or stem cell transplant, or those who are infected with HIV.
Contact your health care provider if you have the symptoms of mono while pregnant. These include:
- Extreme fatigue
- Head and body aches
- Sore throat
- Swollen lymph nodes
- Swollen spleen or liver.

How does CMV spread?
You get CMV by coming in direct contact with body fluids from a person who’s infected with CMV. Body fluids that can contain CMV include:
- Blood
- Breast milk
- Saliva
- Semen
- Tears
- Urine
- Vaginal fluids
CMV spreads in several ways:
- Passing it to your baby during pregnancy, labor, birth, or nursing
- Touching your eyes or the inside of your mouth or nose after direct contact with an infected person’s body fluids, including saliva, urine, blood, tears, semen and human milk.
- Having sexual contact or kissing an infected person
- Getting an organ, bone marrow or stem cell transplant or blood transfusion
Adults usually get CMV by having sex with someone who has CMV or by having contact with young children who have CMV.
You may be more likely than other people to get CMV if you:
- Have young children.
 CMV often spreads during diaper changes, bathing and other close contact with babies and young children. Children can get infected with CMV at child care or school and pass it on to their families, caregivers and other children.
CMV often spreads during diaper changes, bathing and other close contact with babies and young children. Children can get infected with CMV at child care or school and pass it on to their families, caregivers and other children. - Work with young children. For example, you’re a child care worker or a teacher. CMV spreads easily in child care centers or preschools where children share toys that may carry CMV.
- Have sex with someone who has CMV.
- Work in a health care setting, like a health care provider’s office or a laboratory, where you may have contact with infected body fluids
- Have a blood transfusion or organ transplant. A blood transfusion is when you have new blood put into your body. An organ transplant is when you have a new organ, like a heart or kidney, put into your body.
Can I give CMV to my baby?
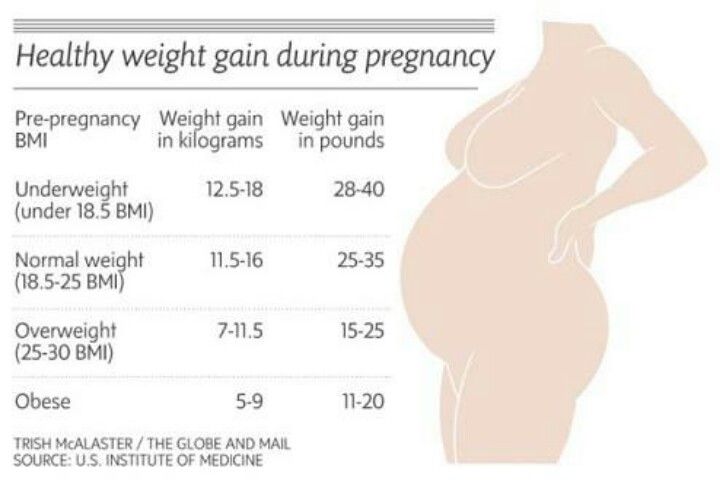
You’re more likely to pass CMV to your baby if you get infected during pregnancy than if you had an infection before you got pregnant. If you have a CMV infection during pregnancy, you have a 1-in-3 chance (33 percent) of passing it to your baby. If you were infected with CMV before you got pregnant, the chance of passing it to your baby drops to about 1 in 100.
If you have a CMV infection during pregnancy, you have a 1-in-3 chance (33 percent) of passing it to your baby. If you were infected with CMV before you got pregnant, the chance of passing it to your baby drops to about 1 in 100.
More than half of adults have had a CMV infection by the time they are 40 years old, and about 1 to 4 in 100 people (1 to 4 percent) get infected with CMV for the first time during pregnancy.
You can pass CMV to your baby at any time during pregnancy. But you are more likely to pass it on if you get infected for the first time during pregnancy or if a past CMV infection becomes active again, especially in the third trimester. You also can pass CMV to your baby during labor and birth, or while nursing. If your baby gets the virus during these times and was born at a healthy weight, they probably won’t have health problems. Preterm babies (babies born before 37 weeks of pregnancy) and low-birthweight babies (babies born weighing less than 5 pounds, 8 ounces) may get sick if they’re infected during birth or while you’re nursing.
If you had a CMV infection before you got pregnant, you can still pass it to your baby, but this is rare.
How does CMV affect babies?
Most babies born with CMV never show signs of the disease and don’t have health problems.
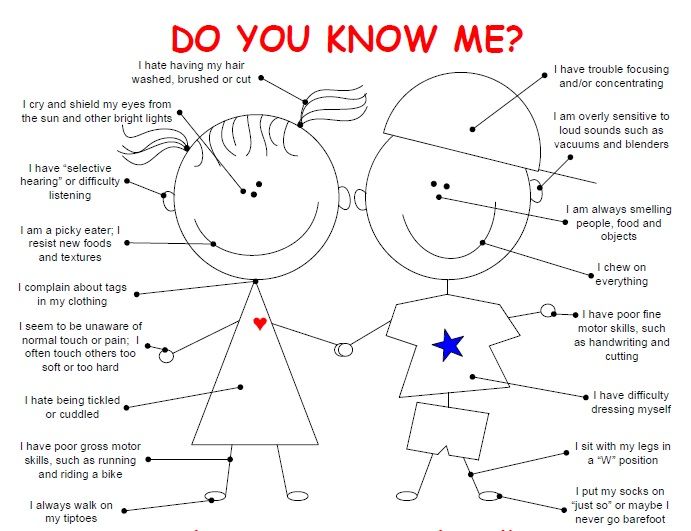
However, babies who are infected with CMV at birth may have long-term health problems, including:
- Hearing loss
- Intellectual and developmental disabilities. These are problems with how the brain works that can cause a person to have trouble or delays in physical development, learning, communicating, taking care of themselves or getting along with others.
- Coordination issues or muscle weakness
- Smaller than expected head (called microcephaly)
- Seizures or convulsions
- Vision loss
Some babies with congenital CMV who don’t show the signs of the disease at birth may still have or develop hearing loss. It may affect one ear or both ears. Sometimes hearing loss can get worse as a baby grows up.
How is CMV diagnosed during pregnancy?
You typically won’t be tested for CMV during prenatal testing. Tell your health care provider if you think you may have CMV or you think you may have been exposed to CMV. Your provider can give you a blood test or test other body fluids to see if you’re infected. Blood tests can help you know whether you have a new infection or if you had a past infection.
Can a baby get tested for CMV before birth?
Yes. If a blood test shows you have a new CMV infection during pregnancy, your provider may recommend testing your baby for the virus using amniocentesis (also called amnio). An amniocentesis is a test that takes some amniotic fluid from around your baby before they are born to check for birth defects and genetic conditions in your baby. You can get this test at 15 to 20 weeks of pregnancy. Your provider also may use ultrasound to check for physical signs that your baby has CMV. An ultrasound (also called sonogram) uses sound waves to show a picture of your baby before they are born. If your provider thinks that your baby may have CMV, your baby’s urine and saliva may be tested to check for the virus.
If your provider thinks that your baby may have CMV, your baby’s urine and saliva may be tested to check for the virus.
How is CMV treated during pregnancy?
There is no cure for CMV, but medications can control infections. Most healthy adults with CMV don’t need treatment. This includes during pregnancy.
People with weakened immune systems may need treatment with an antiviral medicine. These medicines kill infections caused by viruses. Medicines used to treat CMV include ganciclovir, valganciclovir, cidofovir and foscarnet.
How are babies diagnosed with CMV after birth?
About 1 in 200 babies (less than 1 percent) is born with congenital CMV in this country each year. Your baby’s provider can diagnose CMV infection by testing your newborn baby’s saliva, urine or blood. Testing should be done within 2 to 3 weeks after your baby is born to confirm that your baby has congenital CMV.
Most babies with congenital CMV don’t have health problems, but about 1 in 5 babies with congenital CMV can get sick from the virus or have long-term health problems.
Some babies born with CMV have signs and symptoms, including:
- Hearing loss. This is the most common health problem in babies born with CMV. A baby may have hearing loss at birth or it may develop later in childhood.
- Eye damage
- Problems with the spleen, liver or lungs. The spleen is an organ that filters blood in your body and fights infection.
- Jaundice. Jaundice is when a baby’s eyes and skin look yellow. A baby has jaundice when their liver isn’t fully developed or isn’t working well.
- Low birthweight (less than 5 pounds, 8 ounces)
- Smaller than expected head (called microcephaly)
- Neurologic problems, including seizures or convulsions
- Pneumonia
- Preterm birth
- Skin rash or purple splotches on the skin
- Swollen lymph nodes
How is CMV treated after birth?
Babies who show the signs of CMV at birth may be treated with antiviral medications. Antiviral medication may lower your baby’s risk of developing health problems and hearing loss.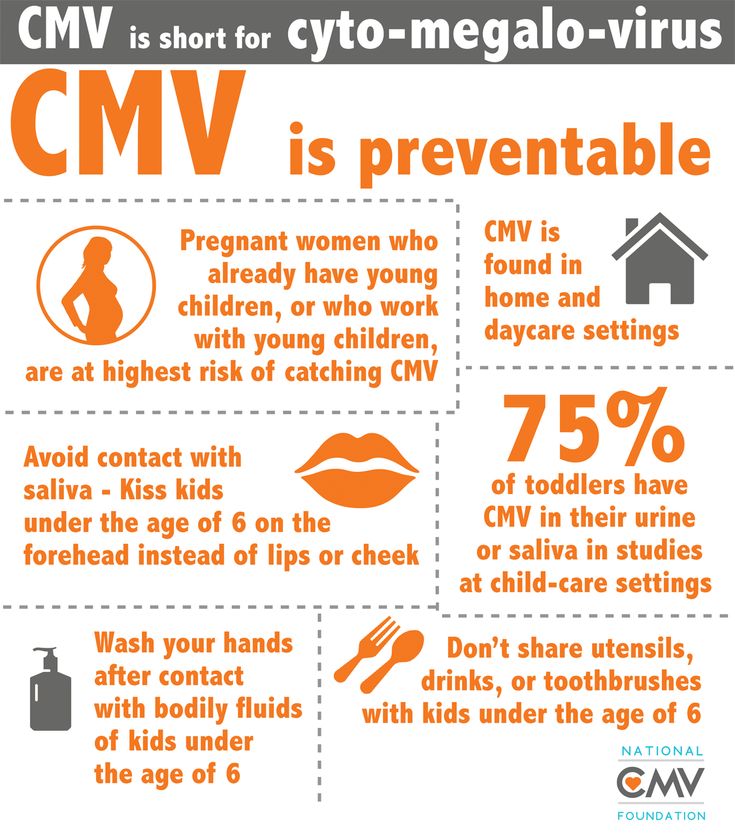 These medications can include ganciclovir or valganciclovir. However, both can cause serious side effects. More research about using antiviral medications on babies is needed.
These medications can include ganciclovir or valganciclovir. However, both can cause serious side effects. More research about using antiviral medications on babies is needed.
Using antivirals to treat babies with congenital CMV who have no signs at birth is not currently recommended.
Babies with congenital CMV, with or without signs at birth, should have regular hearing checks. If your baby has a hearing issue, the earlier it’s detected, the more your baby can benefit from treatment. You should also follow up regularly with your baby’s doctor to discuss any care or additional services that your baby may need. This may include speech services or occupational therapy.
Can I nurse my baby if I have CMV?
CMV can be transmitted to your baby through breast milk while nursing. If you have CMV, you can nurse your baby if they were full term at birth. However, if your baby was born before 30 weeks of pregnancy and weighs less than 3.3 pounds (1,500 grams), talk to your provider before nursing.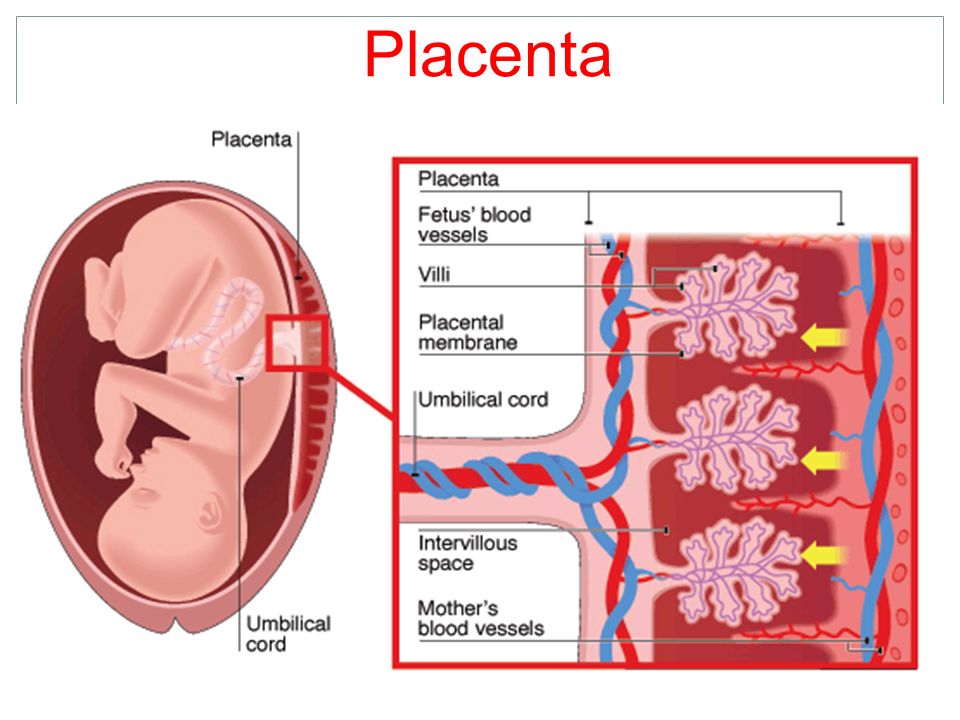 Some preterm and low birthweight babies can get sick from infected breast milk. Freezing and pasteurizing (heating) breast milk can decrease the risk of transmission. However, freezing does not make nursing completely safe for your baby
Some preterm and low birthweight babies can get sick from infected breast milk. Freezing and pasteurizing (heating) breast milk can decrease the risk of transmission. However, freezing does not make nursing completely safe for your baby
How can you protect yourself from CMV?
Here are some things you can do:
- Wash your hands often with soap and water, especially after being in contact with body fluids from babies or children. Carefully throw away used diapers and tissues. Wash your hands after changing diapers, feeding a child, wiping noses and picking up toys.
- Avoid contact with tears or saliva if you kiss a child, especially if you’re pregnant. Kiss babies and children on the cheek or head instead of on the lips.
- Don’t share toothbrushes, food, drinks, cups, straws, forks or other utensils with young children or with anyone who may have CMV. Don’t put a baby’s pacifier in your mouth.
- Clean toys and countertops often.

- If your partner has CMV, use a latex condom during sex..
- If you’re a health care worker in contact with people who have CMV, including newborns, follow workplace safety rules to protect yourself from infection. Wash your hands often and wear gloves.
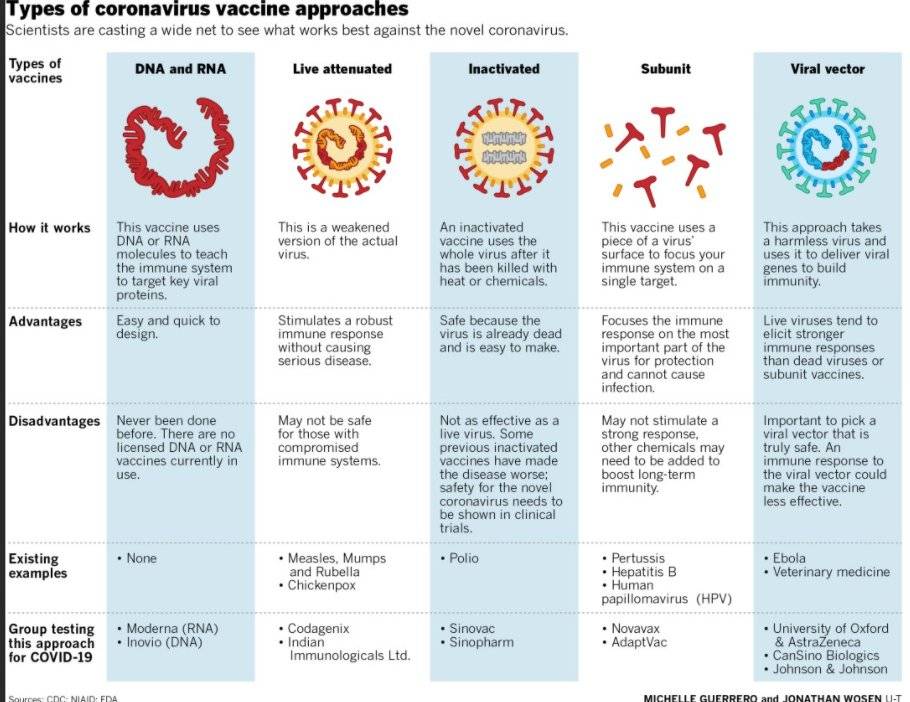
Scientists are working to develop vaccines for CMV. Vaccines make you immune to certain diseases. These vaccines may help prevent CMV infection in pregnant people and babies, and they may help reduce the chance that a baby born to an infected person will have health problems.
For more information
nationalcmv.org
CDC.gov
Last reviewed: August 2021
Diagnosis and treatment of cytomegalovirus during pregnancy H-Clinic blog CMV treatment
Diagnosis and treatment of cytomegalovirus during pregnancy H-Clinic blog CMV treatment
04/15/2020
Cytomegalovirus (CMV) is one of the members of the herpes virus family (it also includes the causative agents of herpes simplex, chickenpox, Epstein-Barr virus).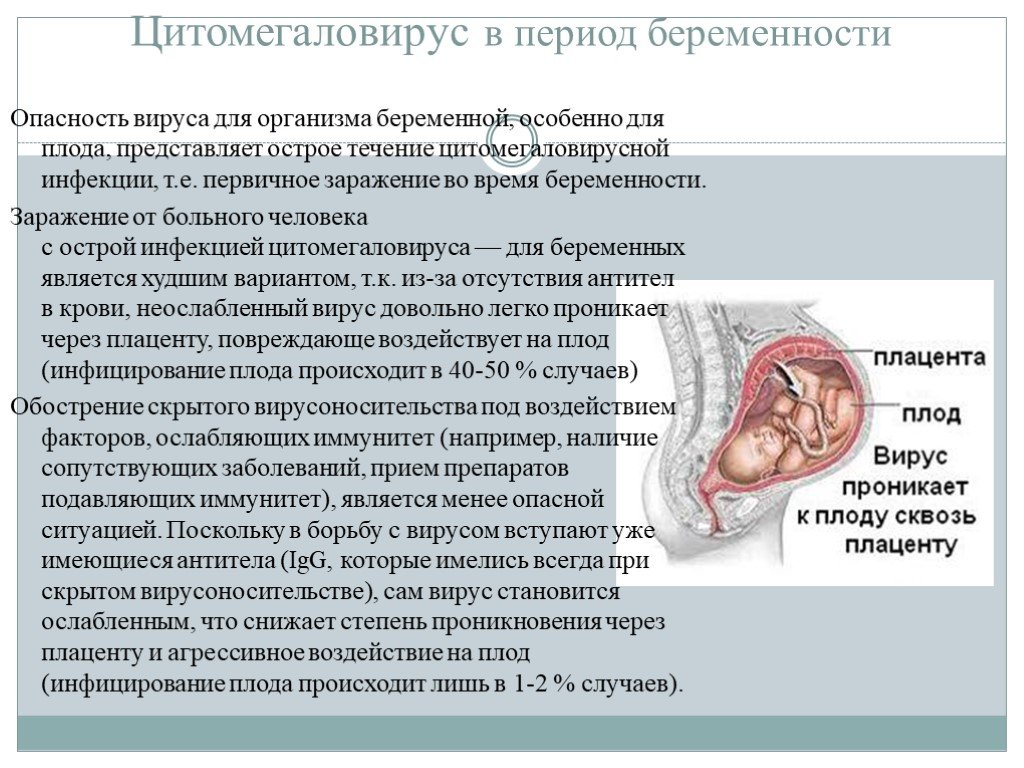 The first contact with the virus most often occurs in childhood, and most adults have antibodies to it. Like many viruses of this family, CMV has the ability to persist for life in the body's cellular reservoirs, usually without causing any symptoms, since the immune system does not allow the virus to multiply uncontrollably. However, cytomegalovirus during pregnancy can be reactivated from reservoir cells against the background of a physiological decrease in immune function in a pregnant woman. This can lead to serious fetal developmental disorders such as: nine0003
The first contact with the virus most often occurs in childhood, and most adults have antibodies to it. Like many viruses of this family, CMV has the ability to persist for life in the body's cellular reservoirs, usually without causing any symptoms, since the immune system does not allow the virus to multiply uncontrollably. However, cytomegalovirus during pregnancy can be reactivated from reservoir cells against the background of a physiological decrease in immune function in a pregnant woman. This can lead to serious fetal developmental disorders such as: nine0003
• lack of hearing;
• decreased vision or blindness;
• hepatitis and jaundice;
• microcephaly;
• decrease in the level of platelets;
• learning difficulties;
• epilepsy.
Cytomegalovirus in pregnant women is especially dangerous for the fetus if the woman has not previously been in contact with the virus, does not have immunity to it, and became infected with CMV during the current pregnancy or shortly before its onset. nine0003
nine0003
This can be checked by testing for antibodies to the virus. During pregnancy, monitoring is carried out for the so-called TORCH complex (this is an analysis for infections that can be transmitted from mother to fetus during pregnancy and cause developmental disorders in the child: toxoplasma, rubella, cytomegalovirus and herpes). It is optimal to pass this analysis even before the onset of the planned pregnancy to assess possible risks.
Upon contact of the body with any pathogen (be it a bacterium, virus or helminth), at least two types of antibodies can be produced in the blood: antibodies of the IgM class and antibodies of the IgG class. The former are an "immediate" reaction of the human immune system to the entry of a foreign organism and usually indicate a recent infection. The second type of antibodies is aimed at the final suppression of the disease and the maintenance of immunity for a long time (sometimes for life). nine0003
Thus, if IgG antibodies are detected before pregnancy, and IgM antibodies give a negative result, this indicates that your body has previously encountered the virus, has a certain level of immune protection, and the risk of re-infection is very small. If the test for IgG is negative, then additional precautions are necessary. In the practice of monitoring a pregnant woman, PCR tests of blood and urine for CMV infection are also widely used. All women are shown mandatory screening for cytomegalovirus during pregnancy. The timing and order of the examination are determined by the doctor. nine0003
If the test for IgG is negative, then additional precautions are necessary. In the practice of monitoring a pregnant woman, PCR tests of blood and urine for CMV infection are also widely used. All women are shown mandatory screening for cytomegalovirus during pregnancy. The timing and order of the examination are determined by the doctor. nine0003
How is CMV transmitted?
CMV is usually transmitted through close contact with a person who already has the virus in their body and sheds it into the environment. The virus can spread through saliva, blood, urine, seminal fluid, breastfeeding. CMV can only be transmitted from a person whose virus is in an "active" state and is excreted in bodily fluids. This happens, for example, if:
• a person contracted the virus for the first time: children often transmit the virus to each other through close contact in kindergarten;
• the virus "reactivated": began to multiply uncontrollably after a certain time after the initial infection.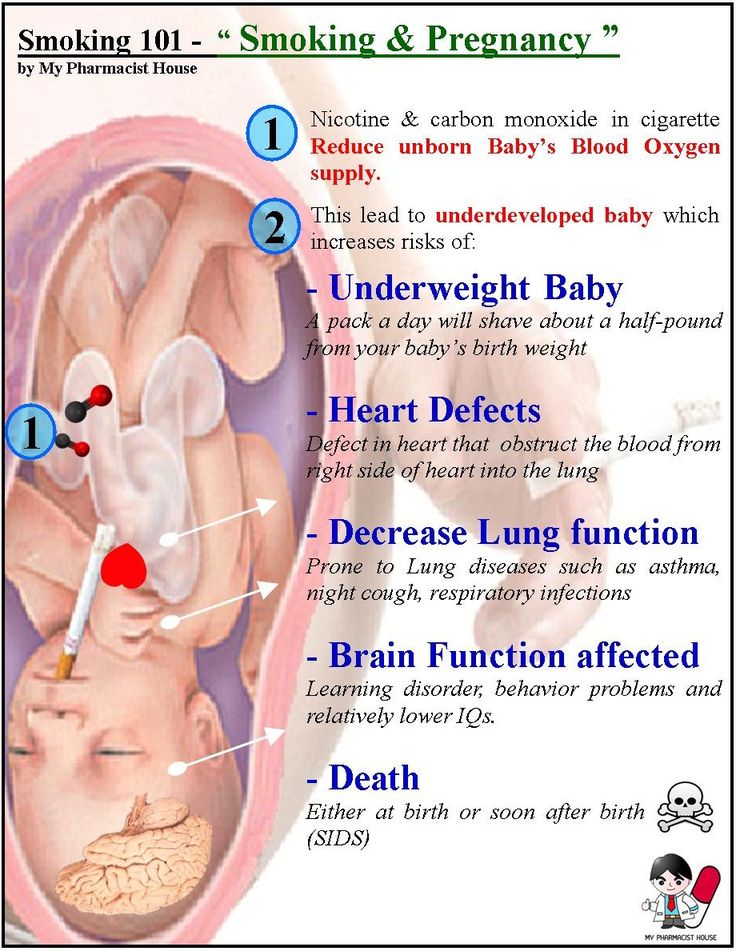 This occurs as a result of a significant weakening of the immune system;
This occurs as a result of a significant weakening of the immune system;
• if reinfection (re-infection) has occurred: the person has become infected with another subtype of CMV.
Thus, the source of infection can most often be children, in whom, after the first contact with the infection, the virus actively multiplies in the body for some time, sometimes causing symptoms like acute respiratory infections, and sometimes completely asymptomatic. In the "risk zone" are pregnant women who work with children or already have children. nine0003
How to prevent infection?
It is impossible to completely prevent infection: a CMV vaccine has not yet been developed. But during pregnancy, you can reduce your risk by doing the following:
• Wash your hands regularly with warm water and soap, especially if you've changed your baby's diapers or work in day care;
• do not kiss small children on the lips or cheek: it is better to kiss them on the top of their head or just hug them; nine0003
• do not finish eating after the child, do not use the same utensils with him;
• Do not lick baby's pacifiers.
How to cure an infection?
In the event that a planned screening examination nevertheless revealed signs of infection or reactivation of an infection in a pregnant woman, further tactics of treatment and management of pregnancy are determined by the doctor together with the woman, taking into account the risks of infection of the fetus. Sometimes invasive diagnostic interventions (such as amniocentesis) may be required. nine0003
The following drugs are registered in Russia for the treatment of cytomegalovirus infection: ganciclovir and valganciclovir. Foscarnet and cidofovir are also used abroad. All of these drugs have a direct antiviral effect. However, possible effects on the fetus limit the use of some of them during pregnancy. There are studies showing the efficacy and safety of hyperimmune globulin G (that is, a drug containing antibodies to the virus) in preventing transmission to the fetus. The choice of treatment tactics, therapy regimens is determined by the attending physician, based on a number of data: laboratory test results, gestational age, etc. As for drugs that indirectly affect the immune system (panavir, isoprinosine, viferon), their effectiveness in the prevention of congenital CMV infection has not been proven. nine0003
As for drugs that indirectly affect the immune system (panavir, isoprinosine, viferon), their effectiveness in the prevention of congenital CMV infection has not been proven. nine0003
Diagnosis and treatment of cytomegalovirus during pregnancy is a complex task, which usually requires the simultaneous participation of an experienced obstetrician-gynecologist and an infectious disease specialist.
Author: infectious disease specialist at the H-Clinic Degtyareva Svetlana Yurievna .
Medical editor: Head of the University Clinic, Candidate of Medical Sciences, infectious disease specialist Konnov Danila Sergeevich . nine0037
You can also read about cytomegalovirus in our article CYTOMEGALOVIRUS TREATMENT .
Return to the list
Cytomegalovirus infection and pregnancy (pregravid preparation and therapy) uMEDp
The article presents the results of studies aimed at studying cytomegalovirus infection in pregnant women, its pathogenesis, clinic, diagnosis, therapy.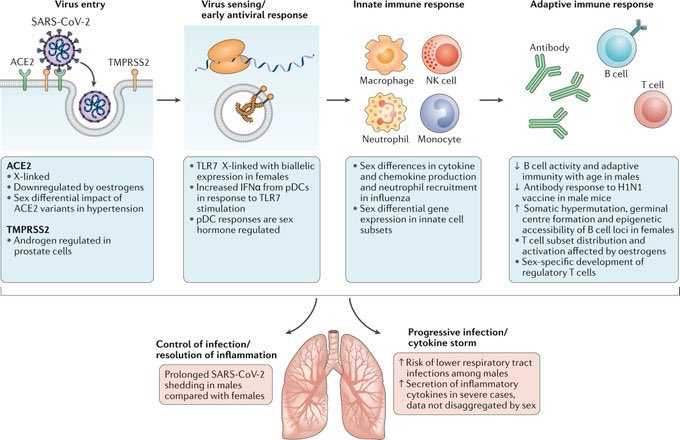 Recommendations are given for preconception preparation of women with cytomegalovirus infection. nine0007
Recommendations are given for preconception preparation of women with cytomegalovirus infection. nine0007
Table. Drugs used to treat active forms of CMVI in pregnant women
Cytomegalovirus infection and the immune system
The problem of cytomegalovirus infection (CMVI) remains relevant at the present time. The need to study CMVI is due to its wide distribution and the fact that CMV can cause various disorders in newborns and children whose mothers had CMVI during pregnancy. nine0003
The causative agent of CMVI is an opportunistic agent, a typical anthroponosis, belonging to the family Herpesviridae , subfamily Betaherpesvirinae - Human herpesvirus 5 (official name). The common name is Cytomegalovirus . CMV is different:
- the ability to infect almost all cells of the human body, which causes a variety of clinical manifestations;
- low tissue selectivity; nine0123
- slow replication;
- relatively low virulence;
- a high degree of dependence on the state of immunity and the ability to suppress cellular immunity;
- lifelong persistence in the host organism;
- periodic reactivation;
- the uncertainty of the moment and ways of infection.
Cytomegaly is coded according to ICD-10 as:
- B25. Cytomegalovirus disease; nine0123
- B25.0. cytomegalovirus pneumonia;
- B25.1. Cytomegalovirus hepatitis;
- B25.2. Cytomegalovirus pancreatitis;
- B25.8. Other cytomegalovirus diseases;
- Q25.9. unspecified cytomegalovirus disease;
- O35.3. Damage to the fetus (suspected) as a result of a viral illness of the mother, requiring the provision of medical care to the mother.
The immune system plays an important role in the pathogenesis of CMVI. The body's first antiviral defense line is innate immunity. However, unlike acquired immunity, it does not provide long-term and reliable protection to the host. During the primary interaction, viruses are opposed by protective barriers (skin epithelium and mucous membranes). An important innate way of protecting the body against viruses is RNA interference [1, 2]. The acquired immune system, when confronted with a virus, produces specific antibodies that attach to the virus and often make it harmless. The most important are two types of antibodies. The first is class M immunoglobulin (Ig), which is highly effective in neutralizing viruses, but is produced by the cells of the immune system only for a few weeks. Synthesis of the second - IgG continues indefinitely. The presence of IgM in the blood indicates an acute infection, IgG indicates an infection suffered in the past [3–6]. nine0003
The most important are two types of antibodies. The first is class M immunoglobulin (Ig), which is highly effective in neutralizing viruses, but is produced by the cells of the immune system only for a few weeks. Synthesis of the second - IgG continues indefinitely. The presence of IgM in the blood indicates an acute infection, IgG indicates an infection suffered in the past [3–6]. nine0003
The second protective antiviral mechanism is cellular immunity, which includes immune cells - T-lymphocytes. An important protective reaction is also the production of interferon, which is formed in the body in response to the presence of the virus. Interferons suppress the intracellular stages of viral reproduction in infected cells, provide immunity to viruses of surrounding healthy cells, prevent dissemination of viruses in the body, and stop the formation of new viruses by affected cells, killing them [2, 7, 8]. nine0003
Epidemiology
The incidence of CMVI is endemic and is not subject to seasonal fluctuations. In Europe, CMVI occupies a leading position among congenital viral infections. The prevalence of antibodies to CMV among women of childbearing age varies in regions of the world from 40 to 100% [3, 9–11]. In the Russian Federation, according to various authors, the frequency of detection of CMVI markers in women reaches 90%. Among women over 30, 98% are infected. The seropositive response rate among pregnant women in Japan is 95%, in China - 92%, in Israel - 84%, in Australia - 71%, in France - 50% [3, 4, 7, 11].
In Europe, CMVI occupies a leading position among congenital viral infections. The prevalence of antibodies to CMV among women of childbearing age varies in regions of the world from 40 to 100% [3, 9–11]. In the Russian Federation, according to various authors, the frequency of detection of CMVI markers in women reaches 90%. Among women over 30, 98% are infected. The seropositive response rate among pregnant women in Japan is 95%, in China - 92%, in Israel - 84%, in Australia - 71%, in France - 50% [3, 4, 7, 11].
In Western Europe, there are three to five cases of congenital CMVI per 1000 births [1, 12]. The frequency of transplacental infection of newborns in different countries, according to the literature, ranges from 0.2 to 14%. It should be especially noted that 0.2–2.2% of newborns are diagnosed with intrauterine CMVI infection with the development of severe psychomotor and somatic disorders in subsequent years [3, 13]. In case of primary infection during pregnancy, infection of the fetus occurs in 30-40% of cases, and according to some data, it can reach 75% [2, 10, 13].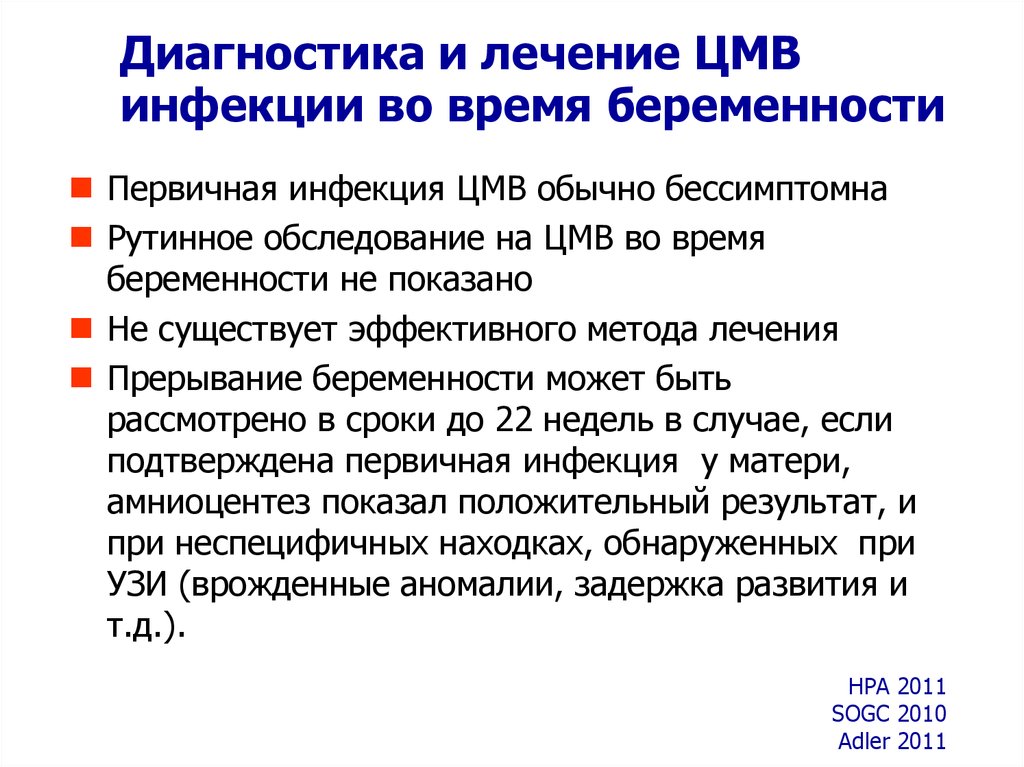 nine0003
nine0003
The frequency of CMVI is higher in developing countries among the population with a low socioeconomic level [1, 4, 7, 9].
High-risk groups for CMV infection include:
- pregnant;
- premature babies;
- newborns;
- young children;
- blood and organ recipients;
- cancer patients;
- hematological patients; nine0123
- AIDS patients and HIV-infected;
- patients with immunodeficiencies of various etiologies;
- homosexuals;
- medical workers.
Pathogenesis
The pathogenetic mechanisms of the development of CMVI depend on the dose of the virus, the routes of infection, the age of the patient, and genetic characteristics.
CMV is present in the blood of most people. The source of the virus can be urine, nasopharyngeal secretions, cervical mucus and vaginal secretions, semen, breast milk, tears, saliva, blood. In other words, CMV can be transmitted by feeding, transfusion of blood and its preparations, contact with secrets and excretions deposited on toys and household items, through all biological fluids and body secretions (saliva, urine, etc. ), coughing (contact-household route of infection), a sexually transmitted route of infection is also possible [12, 14]. nine0003
), coughing (contact-household route of infection), a sexually transmitted route of infection is also possible [12, 14]. nine0003
A distinctive feature of CMV is that, once it enters the body of a person with normal immunity, it invades cells that are sensitive to it and is preserved there for a long time. CMV can persist in blood leukocytes, vascular endothelium, salivary glands, kidneys, and other organs. The virus remains in an inactive state, since the normal state of the immune system is an insurmountable obstacle for it [2, 7, 12]. With a significant decrease in immunity, CMV is activated, destroys the nuclei of the cells in which it "hid" and other intracellular structures. As a result, the cell attracts liquid to itself, swells and acquires a characteristic appearance, which is why it was called "owl's eye" [1, 3, 9, 15, 16].
Clinical picture
As a rule, with CMVI there are no clinical manifestations or there is scanty nonspecific symptoms. The incubation period is 30-40 days, the minimum incubation period is two weeks, the maximum is three months. With clinically pronounced CMVI, a temperature reaction develops (38–40 ° C), which can last two to three weeks, hepatomegaly, splenomegaly, and adenopathy. Much less frequently, patients develop interstitial pneumonia, myocarditis, pericarditis, polyradiculoneuritis, myelitis, meningoencephalitis, hemolytic anemia, and thrombocytopenia. nine0003
The incubation period is 30-40 days, the minimum incubation period is two weeks, the maximum is three months. With clinically pronounced CMVI, a temperature reaction develops (38–40 ° C), which can last two to three weeks, hepatomegaly, splenomegaly, and adenopathy. Much less frequently, patients develop interstitial pneumonia, myocarditis, pericarditis, polyradiculoneuritis, myelitis, meningoencephalitis, hemolytic anemia, and thrombocytopenia. nine0003
In 1989, the staff of the Institute of Virology. DI. Ivanovsky developed a classification of CMVI manifestations depending on the route of infection, the most suitable for practical work.
1. Manifestations in perinatal infection:
- miscarriage, stillbirth;
- malformations;
- congenital CMVI.
2. Manifestations during intra- and postnatal infection: nine0003
- acute infectious disease;
- latent carriage, inapparent, subclinical forms of chronic infection;
- reactivation of infection.
3. Manifestations of infection through blood, saliva, urine, sexual contact:
- acute infectious disease;
- latent carriage, inapparent, subclinical forms;
- reactivation of infection. nine0138
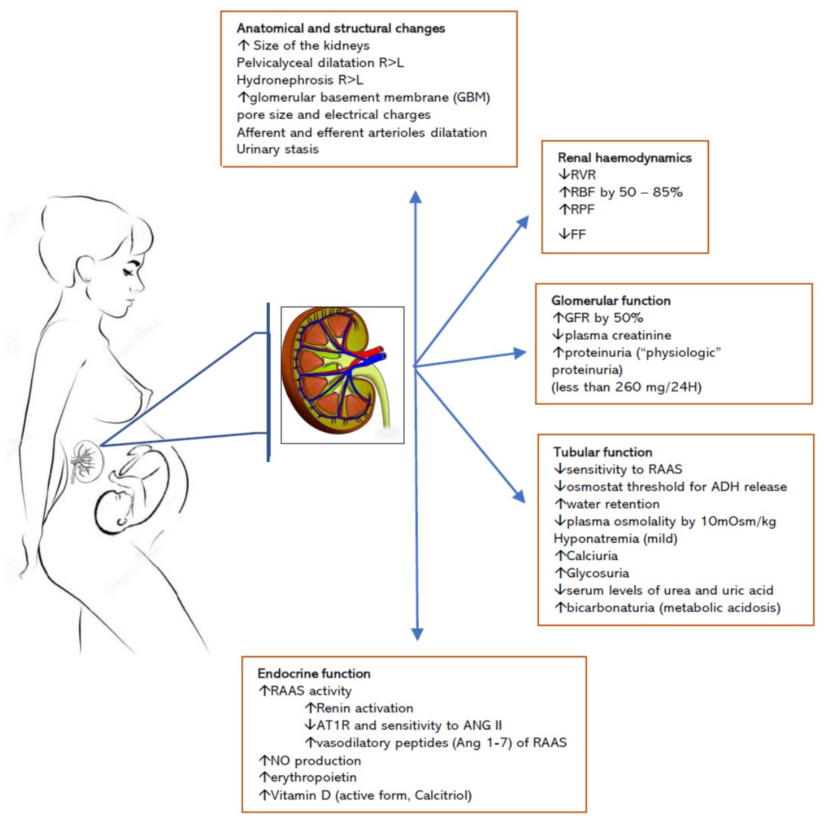
Cytomegalovirus infection and pregnancy. Consequences of transplacental infection
The physiological course of pregnancy is accompanied by a suppressive restructuring of the immune system, the purpose of which is the formation and maintenance of immunological tolerance to fetal alloantigens. Viral infections cause the development of inflammatory processes, affect intercellular interactions and lead to changes in the synthesis of regulatory proteins by cells of the immune system [1, 3, 9, eleven]. Due to the peculiarities of immune protection during pregnancy, the state of immunity at the time of infection, the nature of the interaction between the host's immune response and viral replication, as well as the state of the pregnant woman's cellular immunity system are of great importance [1, 3, 7, 15].
Women with recurrent miscarriage are significantly more likely than other pregnant women to be diagnosed with a persistent form of CMVI (41.9%, p
The frequency of transplacental infection in different countries, according to the literature, ranges from 0.2 to 14%. Risk factors for intrauterine infection of the fetus include the presence of active CMVI in the mother, a high level of viremia, an immunodeficient state of the mother, increased permeability of the fetoplacental barrier [1, 2, 3, 19].
In the presence of CMVI, an asymptomatic infection may develop without consequences for the health of the child. However, in some cases, the presence of CMVI increases the risk of impaired embryogenesis, intrauterine damage to the fetus, spontaneous abortion, placental insufficiency, congenital pathology of the fetus and newborn, and the formation of immunodeficiencies in the postnatal period. The risk of adverse effects is high in both severe and subclinical variants of cytomegaly. An analysis of the condition of newborns showed that in pregnant women with a burdened obstetric and gynecological history, the risk of giving birth to children in serious condition is 4.9times higher when CMVI is detected in the third trimester of pregnancy [9, 16].
An analysis of the condition of newborns showed that in pregnant women with a burdened obstetric and gynecological history, the risk of giving birth to children in serious condition is 4.9times higher when CMVI is detected in the third trimester of pregnancy [9, 16].
Congenital CMVI in the second - fifth year of a child's life can manifest itself as blindness, deafness, speech inhibition, lag in psychomotor and mental development. The risk group for the development of congenital CMVI includes children of patients who do not have basic immunity to CMV (absence of immunoglobulins to CMV in serum) [11, 14, 17].
Diagnostics
CMVI must be differentiated from acquired immunodeficiency syndrome, infectious mononucleosis, acute leukemia, lymphogranulomatosis, viral hepatitis, and sepsis. The congenital form of CMVI should be distinguished from such infectious embryopathies and fetopathy as rubella, listeriosis, toxoplasmosis, herpes infection, syphilis. Differential diagnosis is also carried out between CMVI and hemolytic disease of the newborn, birth injuries, and hereditary syndromes. At the same time, the anamnestic data of the woman and the results of instrumental examination methods are of great importance. An important role in establishing the causes of the disease is played by the pathomorphological examination of the placenta, umbilical cord and fetal membranes. In case of antenatal or intranatal death of the fetus, it is necessary to conduct a thorough histological, bacteriological and virological examination of the tissues of the deceased fetus and newborn [4, 15]. nine0003
Differential diagnosis is also carried out between CMVI and hemolytic disease of the newborn, birth injuries, and hereditary syndromes. At the same time, the anamnestic data of the woman and the results of instrumental examination methods are of great importance. An important role in establishing the causes of the disease is played by the pathomorphological examination of the placenta, umbilical cord and fetal membranes. In case of antenatal or intranatal death of the fetus, it is necessary to conduct a thorough histological, bacteriological and virological examination of the tissues of the deceased fetus and newborn [4, 15]. nine0003
Laboratory diagnosis of CMVI includes verification of the etiological agent (identification of the pathogen, its genome, antigen), detection of serological markers (serological antibodies), determination of the severity of the infectious process - the activity of virus replication (separate determination of anticytomegalovirus antibodies of the IgM and IgG classes) [4, 11].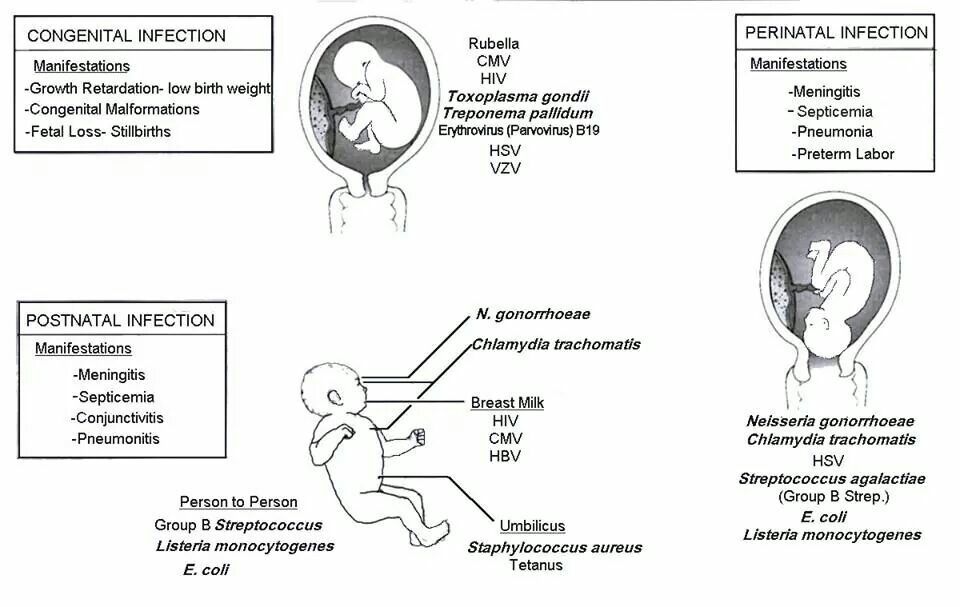
Laboratory criteria for CMVI activity include detection of a virus, CMV antigen (pp65, pp72) or CMV DNA, anti-CMV IgM class antibodies in the blood, multiple (4 times or more) increase in titers of anti-CMV IgG class antibodies in "paired sera" or the appearance of IgG class antibodies in previously seronegative women, the detection of IgG class antibodies in serum with a low avidity index. nine0003
To clarify the nature of the infection (primary or chronic), it is necessary to take into account the avidity index (the degree of strength of binding of an antibody molecule to an antigen molecule). The detection of IgG antibodies with an avidity index below 30–35% in the test serum indicates a fresh primary infection. An IgG antibody level with an avidity index of ≥ 40% indicates past infection. The presence of IgG antibodies with an avidity index of 31–39% indicates a late stage of primary infection or a recent infection when high concentrations of IgG antibodies are detected [2–4]. nine0003
nine0003
Optimal diagnosis of CMVI includes a combination of virological, serological and molecular biological methods, which allows not only to diagnose the infection, but also to determine its activity.
During pregnancy, the active form of CMVI is detected in 40–50% of seropositive women, while the infection can become active at any stage of pregnancy, which requires examination of pregnant women for CMVI markers. Recommended timing for virological monitoring: 8–12 weeks, 23–25 weeks, 33–35 weeks of gestation [2, 4, 9, 20].
Treatment
The objectives of the treatment of women with an active form of CMVI are the termination of viral excretion and the elimination of IgM CMV from the blood, the transformation of reactivated and persistent forms of infection into a latent one.
In the treatment of severe generalized forms of CMVI, antiviral agents are used: acyclovir, ganciclovir, valaciclovir, famciclovir, foscarnet, cidofovir, fomivirsen. However, they are highly toxic, which greatly limits their use in pregnant, lactating women, and newborns. They are also not recommended for patients planning pregnancy [11, 16]. The only safe alternative to etiotropic drugs is Neocytotect. nine0003
However, they are highly toxic, which greatly limits their use in pregnant, lactating women, and newborns. They are also not recommended for patients planning pregnancy [11, 16]. The only safe alternative to etiotropic drugs is Neocytotect. nine0003
The table shows the drugs used to treat active forms of CMVI in pregnant women. The active form or reactivation of CMVI in pregnant women may serve as an indication for the appointment of hyperimmune anticytomegalovirus immunoglobulin (Neocytotect, Biotest Pharma, Germany). Activation of CMVI occurs at a low titer of specific IgG. Neocytotec contains ten times more IgG antibodies to CMV than standard immunoglobulins, blocks CMV and limits its dissemination in the body. The introduction of Neocytotect to pregnant women reduces the risk of intrauterine infection of the fetus and the development of long-term consequences of congenital CMVI. According to many researchers, the use of Viferon in the complex therapy of CMVI during pregnancy makes it possible to reduce the concentration of interferon gamma and interleukin 8 in the blood serum by two to three times [9, 15, 16, 21].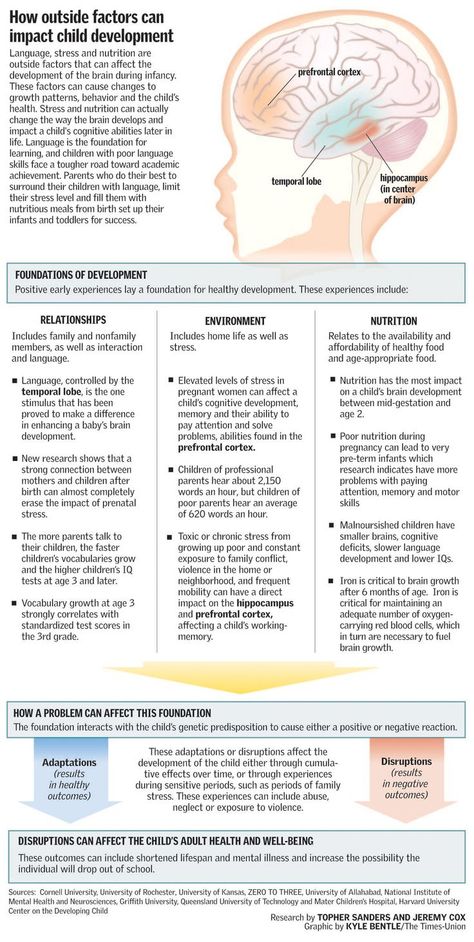 The composition of the drug Viferon, produced by Feron LLC (Moscow), in addition to recombinant human interferon-alpha-2b, includes antioxidants.
The composition of the drug Viferon, produced by Feron LLC (Moscow), in addition to recombinant human interferon-alpha-2b, includes antioxidants.
Women with an active form of CMVI are at risk of possible intrauterine transmission of the infection. Such women outside of pregnancy are recommended to carry out immunocorrective therapy using mainly Taktivin, Cycloferon, Panavir, Viferon. Pregnancy planning is allowed when the active infection is eliminated and the latent form of CMVI is established. Treatment of women with an active form of CMVI before pregnancy planning prevents the activation of CMVI in the most dangerous first trimester of pregnancy in 75% of cases. nine0003
Conclusion
CMVI is an important problem in obstetrics, gynecology and perinatology due to the negative consequences of the infection in relation to reproductive health. To date, CMVI therapy remains insufficiently effective, which necessitates the development of standardized methods for the prevention and treatment of this disease.