How do you have a miscarriage
Causes, Symptoms, Risks, Treatment & Prevention
Overview
What is a miscarriage?
A miscarriage (also called a spontaneous abortion) is the unexpected ending of a pregnancy in the first 20 weeks of gestation. Just because it’s called a “miscarriage” doesn’t mean you did something wrong in carrying the pregnancy. Most miscarriages are beyond your control and occur because the fetus stops growing.
Types of miscarriage
Your pregnancy care provider may diagnose you with the following types of miscarriage:
- Missed miscarriage: You’ve lost the pregnancy but are unaware it’s happened. There are no symptoms of miscarriage, but an ultrasound confirms the fetus has no heartbeat.
- Complete miscarriage: You’ve lost the pregnancy and your uterus is empty. You’ve experienced bleeding and passed fetal tissue. Your provider can confirm a complete miscarriage with an ultrasound.
- Recurrent miscarriage: Three consecutive miscarriages.
It affects about 1% of couples.
- Threatened miscarriage: Your cervix stays closed, but you’re bleeding and experiencing pelvic cramping. The pregnancy typically continues with no further issues. Your pregnancy care provider may monitor you more closely for the rest of your pregnancy.
- Inevitable miscarriage: You’re bleeding, cramping and your cervix has started to open (dilate). You may leak amniotic fluid. A complete miscarriage is likely.
How do I know if I’m having a miscarriage?
You may not be aware you’re having a miscarriage. In people who have symptoms of a miscarriage, the most common signs are:
- Bleeding that progresses from light to heavy. You may also pass grayish tissue or blood clots.
- Cramps and abdominal pain (usually worse than menstrual cramps).
- Low back ache that may range from mild to severe.
- A decrease in pregnancy symptoms.
Contact your pregnancy care provider right away if you’re experiencing any of these symptoms. They will tell you to come into the office or go to the emergency room.
They will tell you to come into the office or go to the emergency room.
Symptoms and Causes
What causes miscarriage?
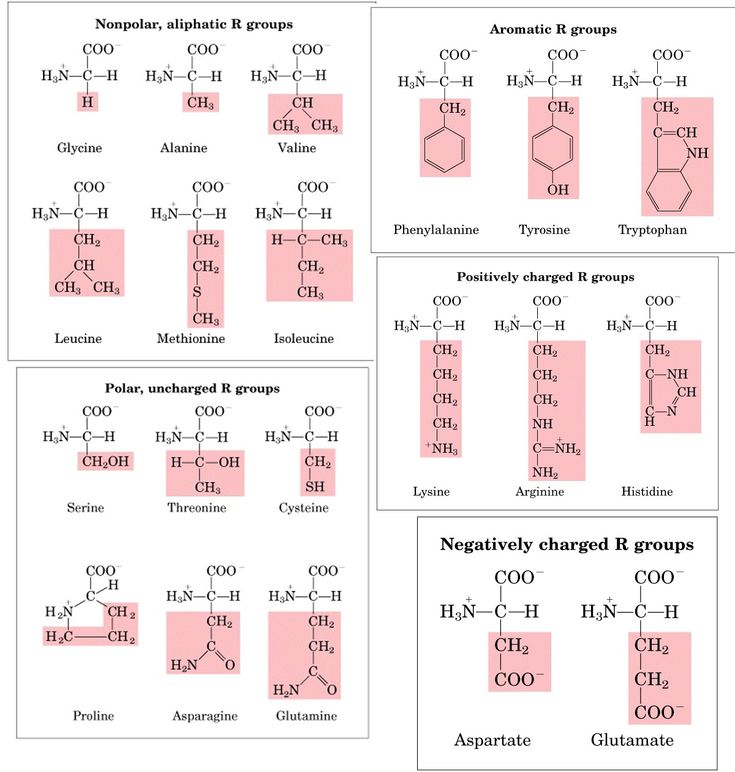
Chromosomal abnormalities cause about 50% of all miscarriages in the first trimester (up to 13 weeks) of pregnancy. Chromosomes are tiny structures inside the cells of your body that carry your genes. Genes determine all of a person’s physical attributes, such as assigned sex, hair and eye color and blood type.
During fertilization, when the egg and sperm join, two sets of chromosomes come together. If an egg or sperm has more or fewer chromosomes than normal, the fetus will have an abnormal number. As a fertilized egg grows into a fetus, its cells divide and multiply several times. Abnormalities during this process also leads to miscarriage.
Most chromosomal problems occur by chance. It’s not completely known why this happens.
Several factors may cause miscarriage:
- Infection.
- Exposure to TORCH diseases.
- Hormonal imbalances.
- Improper implantation of fertilized egg in your uterine lining.
- How old you are.
- Uterine abnormalities.
- Incompetent cervix (your cervix begins to open too early in pregnancy).
- Lifestyle factors such as smoking, drinking alcohol or using recreational drugs.
- Disorders of the immune system like lupus.
- Severe kidney disease.
- Congenital heart disease.
- Diabetes that isn't managed.
- Thyroid disease.
- Radiation.
- Certain medicines, such as the acne drug isotretinoin (Accutane®).
- Severe malnutrition.
There is no scientific proof that stress, exercise, sexual activity or prolonged use of birth control pills cause miscarriage. Whatever your situation is, it’s important to not blame yourself for having a miscarriage. Most miscarriages have nothing to do with something you did or didn’t do.
How painful is a miscarriage?
Miscarriages are different for every person. Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
What happens first during a miscarriage?
It’s hard to say what happens first during a miscarriage because everyone’s symptoms are different. Sometimes there are no signs of miscarriage, and you find out at a prenatal ultrasound that you’ve lost the pregnancy. Most people will experience some degree of cramping and bleeding, but what happens first varies.
How long does a miscarriage take?
It depends. Some people have painful cramping and heavy bleeding longer than others. Your pregnancy care provider can tell you what to expect and give you advice on how to manage pain and cramps during your miscarriage.
What are the risk factors for a miscarriage?
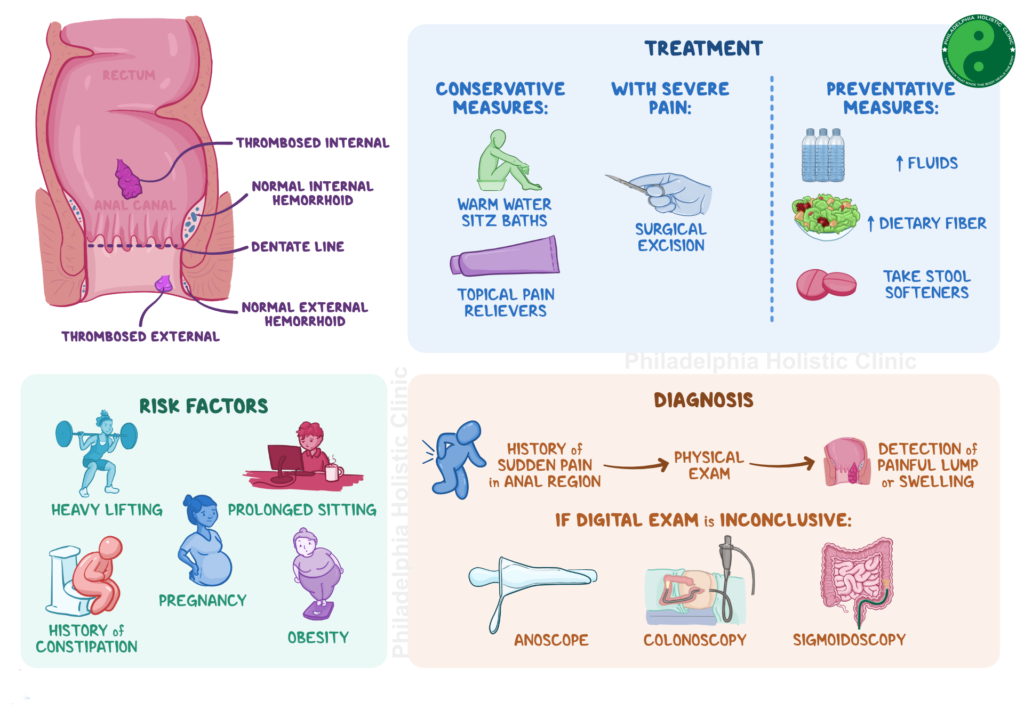
A risk factor is a trait or behavior that increases a person’s chance of developing a disease or condition. Risk factors for miscarriage include:
Risk factors for miscarriage include:
- Your age: Studies show that the risk of miscarriage is 12% to 15% for people in their 20s and rises to about 25% for people by age 40. Most age-related miscarriages happen because of a chromosomal abnormality (the fetus has missing or extra chromosomes).
- Previous miscarriage: You have a 25% chance of having another miscarriage (only slightly higher than someone who hasn’t had a miscarriage) if you’ve already had one.
- Health conditions: Certain health conditions like unmanaged diabetes, infections or issues with your uterus or cervix increase your chance of miscarriage.
Talk to your pregnancy care provider about the risk factors for miscarriage. They can discuss your risk after they’ve reviewed your medical history.
How many people have miscarriages?
Between 10% and 20% of all known pregnancies end in miscarriage. Most miscarriages (80%) happen within the first three months of pregnancy (up to 13 weeks of pregnancy). Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
What is my risk of miscarriage by week?
Your risk of pregnancy loss declines each week you’re pregnant. Around 15% of pregnancies end in miscarriage. Miscarriage risk in the second trimester (13 to 19 weeks) is between 1% and 5%. Many factors affect your risk of miscarriage such as your age and health. However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
Diagnosis and Tests
How is a miscarriage diagnosed?
Your pregnancy care provider will perform an ultrasound test to confirm a miscarriage. These tests check for fetal heartbeat or the presence of a yolk sac (one of the first fetal structures your provider can see on ultrasound).
You may also have a blood test to measure human chorionic gonadotropin (hCG), a hormone produced by the placenta. A low hCG level can confirm a miscarriage.
Finally, your provider may perform a pelvic exam to check if your cervix has opened.
Management and Treatment
What are the treatments for a miscarriage?
If you experience the loss of a pregnancy, the fetus must be removed from your uterus. If any parts of the pregnancy are left inside your body, you could experience infection, bleeding or other complications.
If the miscarriage is complete and your uterus expels all the fetal tissue, then no further treatment is usually needed. Your pregnancy care provider will conduct an ultrasound to make sure there’s nothing left in your uterus.
If your body doesn’t remove all the tissue on its own or you haven’t started to bleed, your pregnancy care provider will recommend removing the tissue with medication or surgery.
Nonsurgical treatment
Your pregnancy care provider may recommend waiting to see if you pass the pregnancy on your own. This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
If a miscarriage wasn’t confirmed, but you had symptoms of a miscarriage, your provider may prescribe bed rest for several days. You might be admitted to the hospital overnight for observation. When the bleeding stops, you may be able to continue with your normal activities. If your cervix is dilated, they may diagnose you with an incompetent cervix, and they may perform a procedure to close your cervix (cervical cerclage).
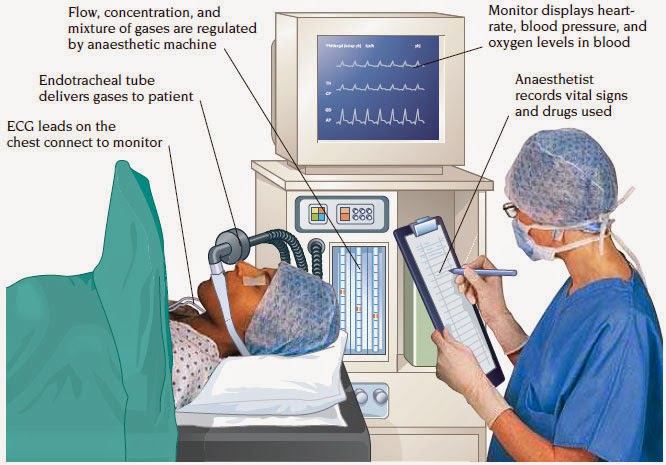
Surgical treatment
Your provider may perform a dilation and curettage (D&C) or dilation and evacuation (D&E) if your uterus hasn’t passed the pregnancy or if you’re bleeding heavily. Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
What are some of the symptoms after a miscarriage?
Spotting and mild discomfort are common symptoms after a miscarriage.
Contact your healthcare provider immediately if you have any of these symptoms as it could be signs of an infection:
- Heavy bleeding or worsening bleeding.
- Fever.
- Chills.
- Intense pain.
Don’t put anything inside your vagina for at least two weeks after a miscarriage. This includes tampons, sexual intercourse and fingers or sex toys. Your provider will schedule a follow-up appointment with you to discuss your recovery and any complications.
What tests should I have after repeat miscarriages?
Blood tests or genetic tests might be necessary if you’ve more than three miscarriages in a row (called repeated miscarriage). These include:
These include:
- Genetic tests: You and your partner can have blood tests, like karyotyping, to check for chromosome abnormalities. If tissue from the miscarriage is available, your provider may be able to test it for chromosome irregularities.
- Blood tests: You may have a blood test to check for autoimmune or hormone conditions that could be causing miscarriages.
Your provider may also look at your uterus using one of the following procedures:
- Hysterosalpingogram (an X-ray dye test of your uterus and fallopian tubes).
- Hysteroscopy (a test during which your provider views the inside of your uterus with a thin, telescope-like device).
- Laparoscopy (a procedure during which your provider views the pelvic organs with a lighted device).
Prevention
How can I prevent another miscarriage?
It’s usually not possible to prevent a miscarriage. If you have a miscarriage, it’s not because you did something to cause it. Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
- Attending all your prenatal care appointments.
- Maintaining a weight that's healthy for you.
- Avoiding risk factors for miscarriage like drinking alcohol and smoking cigarettes.
- Taking a prenatal vitamin.
- Getting regular exercise and eating a healthy diet.
Outlook / Prognosis
Can I get pregnant after I’ve had a miscarriage?
Yes. Most people (87%) who have miscarriages have subsequent normal pregnancies and births. Having a miscarriage doesn’t necessarily mean you have a fertility problem. Remember, most miscarriages occur because of a chromosomal abnormality, not because of something you did.
How soon can I get pregnant after a miscarriage?
The decision on when you should begin trying to get pregnant again is between you and your pregnancy care provider. Most people can get pregnant again after they’ve had one “normal” menstrual period.
Taking time to heal both physically and emotionally after a miscarriage is important. Counseling is available to help you cope with your loss. A pregnancy loss support group might also be a valuable resource to you and your partner. Ask your healthcare provider for more information about counseling and support groups. Above all, don’t blame yourself for the miscarriage. Take the time you need to grieve.
If you’ve had three miscarriages in a row, ask your provider about performing tests to figure out an underlying cause. You should use birth control until you receive the results. After your provider reviews the test results, they may suggest going off birth control and trying to conceive again.
Living With
How can I cope with my miscarriage?
Losing a pregnancy can be devastating and leave you with a range of emotions and lots of questions. Healing emotionally from a miscarriage is often harder and longer than the physical healing. Take the time you need to grieve your loss.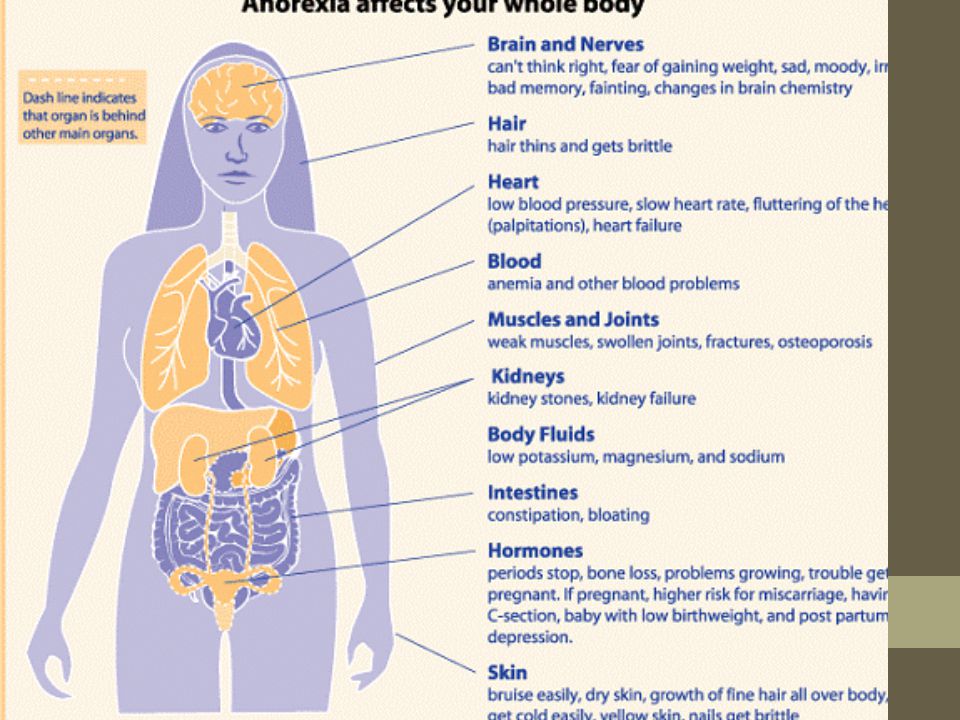 Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
A note from Cleveland Clinic
A miscarriage is a very emotional moment for expectant parents and it’s natural to grieve the loss. Remember that a miscarriage can’t be prevented, and it’s not caused by something you did wrong. It doesn’t mean that you can’t have children or that you’ll have another miscarriage. If you’re planning to become pregnant, reach out to your healthcare provider to discuss the timing of your next pregnancy and ask any questions you have. It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
Miscarriage - Causes - NHS
There are many reasons why a miscarriage may happen, although the cause is often not identified.
If a miscarriage happens during the first trimester of pregnancy (the first 3 months), it's usually caused by problems with the unborn baby (foetus).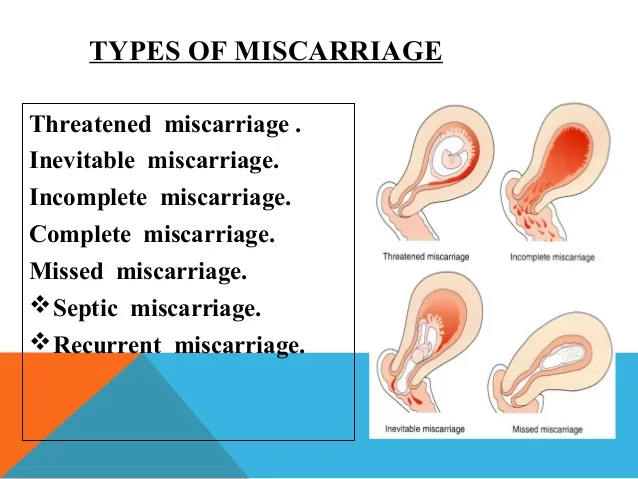 About 3 in every 4 miscarriages happen during this period.
About 3 in every 4 miscarriages happen during this period.
If a miscarriage happens after the first trimester of pregnancy, it may be the result of things like an underlying health condition in the mother.
These late miscarriages may also be caused by an infection around the baby, which leads to the bag of waters breaking before any pain or bleeding. Sometimes they can be caused by the neck of the womb opening too soon.
First trimester miscarriages
First trimester miscarriages are often caused by problems with the chromosomes of the foetus.
Chromosome problems
Chromosomes are blocks of DNA. They contain a detailed set of instructions that control a wide range of factors, from how the cells of the body develop to what colour eyes a baby will have.
Sometimes something can go wrong at the point of conception and the foetus receives too many or not enough chromosomes. The reasons for this are often unclear, but it means the foetus will not be able to develop normally, resulting in a miscarriage.
The reasons for this are often unclear, but it means the foetus will not be able to develop normally, resulting in a miscarriage.
This is very unlikely to recur. It does not necessarily mean there's any problem with you or your partner.
Placenta problems
The placenta is the organ linking your blood supply to your baby's. If there's a problem with the development of the placenta, it can also lead to a miscarriage.
Things that increase your risk
An early miscarriage may happen by chance. But there are several things known to increase your risk of problems happening.
Your age can also have an influence:
- in women under 30, 1 in 10 pregnancies will end in miscarriage
- in women aged 35 to 39, up to 2 in 10 pregnancies will end in miscarriage
- in women over 45, more than 5 in 10 pregnancies will end in miscarriage
A pregnancy may also be more likely to end in miscarriage if you:
- are obese
- smoke
- use drugs
- drink lots of caffeine
- drink alcohol
Second trimester miscarriages
Long-term health conditions
Several long-term (chronic) health conditions can increase your risk of having a miscarriage in the second trimester, especially if they're not treated or well controlled.
These include:
- diabetes (if it's poorly controlled)
- severe high blood pressure
- lupus
- kidney disease
- an overactive thyroid gland (hyperthyroidism)
- an underactive thyroid gland (hypothyroidism)
- antiphospholipid syndrome (APS)
Infections
The following infections may also increase your risk:
- rubella (german measles)
- cytomegalovirus (CMV)
- bacterial vaginosis
- HIV
- chlamydia
- gonorrhoea
- syphilis
- malaria
Food poisoning
Food poisoning, caused by eating contaminated food, can also increase the risk of miscarriage. For example:
For example:
- listeriosis – most commonly found in unpasteurised dairy products, such as blue cheese
- toxoplasmosis – which can be caught by eating raw or undercooked infected meat
- salmonella – most often caused by eating raw or partly cooked eggs
Read more about foods to avoid in pregnancy.
Medicines
Medicines that increase your risk include:
- misoprostol – used for stomach ulcers
- retinoids – used for eczema and acne
- methotrexate – used for conditions such as rheumatoid arthritis
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen; these are used for pain and inflammation
To be sure a medicine is safe in pregnancy, always check with your doctor, midwife or pharmacist before taking it.
Read more about medicines during pregnancy.
Womb structure
Problems and abnormalities with your womb can also lead to second trimester miscarriages. Possible problems include:
- non-cancerous growths in the womb called fibroids
- an abnormally shaped womb
Weakened cervix
In some cases, the muscles of the cervix (neck of the womb) are weaker than usual. This is known as a weakened cervix or cervical incompetence.
A weakened cervix may be caused by a previous injury to this area, usually after a surgical procedure. The muscle weakness can cause the cervix to open too early during pregnancy, leading to a miscarriage.
Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a condition where the ovaries are larger than normal.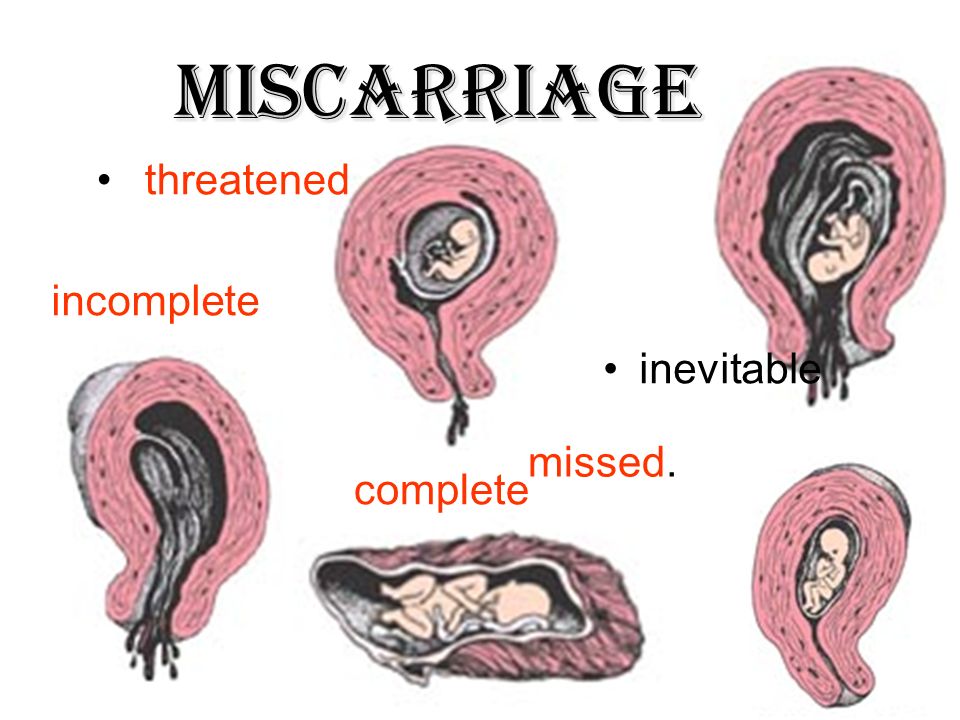 It's caused by hormonal changes in the ovaries.
It's caused by hormonal changes in the ovaries.
PCOS is known to be a leading cause of infertility as it can prevent the release of an egg (ovulation). There's some evidence to suggest it may also be linked to an increased risk of miscarriage.
Misconceptions about miscarriage
An increased risk of miscarriage is not linked to:
- your emotional state during pregnancy, such as being stressed or depressed
- having a shock or fright during pregnancy
- exercise during pregnancy – but discuss with your GP or midwife what type and amount of exercise is suitable for you during pregnancy
- lifting or straining during pregnancy
- working during pregnancy – or work that involves sitting or standing for long periods
- having sex during pregnancy
- travelling by air
- eating spicy food
Recurrent miscarriages
If you have had a miscarriage, it's natural to worry that you'll have another if you get pregnant again.![]() But most miscarriages are a one-off event.
But most miscarriages are a one-off event.
About 1 in 100 women experience recurrent miscarriages (3 or more in a row) and many of these women go on to have a successful pregnancy.
Page last reviewed: 09 March 2022
Next review due: 09 March 2025
Early miscarriage - symptoms and how to prevent it
The term "early miscarriage" refers to a spontaneous abortion that occurs in the first 6-8 weeks of pregnancy. It can occur before 20 weeks of pregnancy for reasons related to the natural states of the fair sex. According to statistics, the logical outcome of every fifth pregnancy is a miscarriage. However, quite often a woman does not even know that she was pregnant by the time the fetus is rejected by the body.
In addition, a curious pattern was revealed: more often than a natural one, a pregnancy induced artificially ends in a miscarriage. For example, in vitro fertilization, unfortunately, does not always lead to a successful pregnancy and the birth of a baby on time.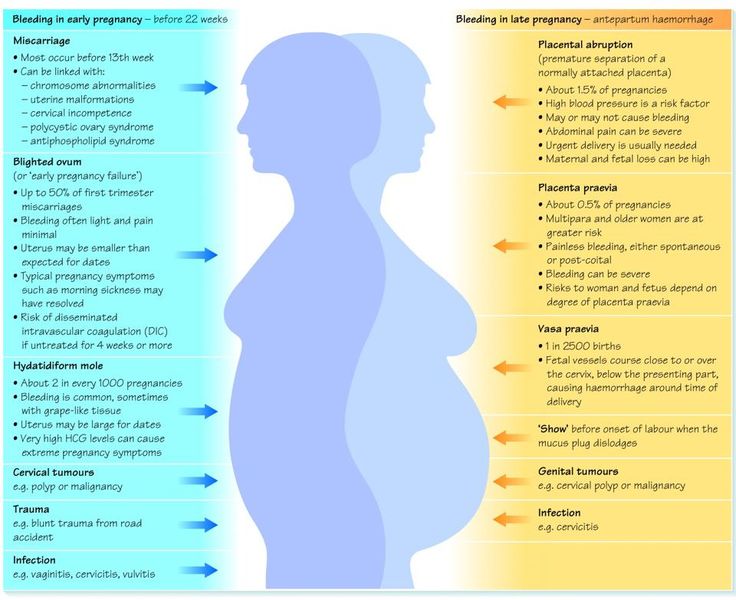
Why can an early miscarriage occur?
Here are the most common causes, each of which significantly increases the risk of miscarriage:
- the expectant mother has certain infectious diseases, as well as STDs;
- intoxication of a woman's body for various reasons, including as a result of her living in an ecologically unfavorable region;
- all kinds of metabolic disorders in the body;
- hormonal disruptions, including those caused by a malfunction of the thyroid gland;
- various neoplasms in the uterus and others, as well as the cervix, pathologies;
- maintenance by the future mother of a life far from a healthy lifestyle. May include drinking alcohol, smoking, taking psychotropic and narcotic drugs, as well as malnutrition;
- obesity;
- immune status disorders;
- cardiac diseases;
- diabetes mellitus;
- too early for pregnancy or, conversely, the patient's overly mature age at times increases the risk of miscarriage;
- all kinds of pathologies of chromosomes and genes;
- prolonged exposure to stress or severe psycho-emotional trauma in a woman.
The timing of a miscarriage may depend, among other things, on the patient's genetic predisposition to miscarriage. Finally, often its specific cause remains unexplained to the end.
Symptoms of miscarriage
A pregnant woman should urgently seek medical help if she has the following warning signs:
- bleeding from the vagina;
- spotting discharge from the genital tract. They can have both light pink and intense red or brownish tint;
- convulsions;
- severe pain in the lumbar region;
- abdominal pain, etc.
All of the above signs can be symptoms of a miscarriage. Timely provision of qualified medical care is the key to maintaining pregnancy.
Life after miscarriage
If a woman could not bear the pregnancy - an early miscarriage crossed out all her plans - then she needs to calm down and take all measures to prevent such complications in the future. Usually obstetricians-gynecologists recommend planning a new pregnancy no earlier than six months after a miscarriage. During this time, a woman needs to be examined and find out if she has any pathology in her body that could lead to an abortion. It can be various STDs and infectious diseases. In the presence of chronic diseases that can provoke spontaneous abortion, it is necessary to throw all your efforts into their treatment.
Gynecologists of the corresponding department of our private clinic in Ryazan will help you find out what could have caused the miscarriage, as well as make recommendations on how to prepare for pregnancy. They usually include a set of physical exercises suitable for a woman, a diet rich in everything necessary for bearing a healthy baby, no stress, and measures to maintain a normal body mass index. Can't recover or get pregnant after a miscarriage? Contact "ON CLINIC in Ryazan" - here you will definitely be helped!
miscarriage, symptoms - Health Clinic 365 G.
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnostics of miscarriage
Treatment and prevention of miscarriage
Peregiasis - this is spontaneous termination of pregnancy up to 20 weeks. According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy. Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Symptoms of miscarriage .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter. In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Call your doctor if:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can place a piece of tissue to be isolated in a clean container and take it to your doctor for examination.