Gestation period for chicken pox
Chickenpox (Varicella) for Healthcare Professionals
Varicella in Vaccinated Persons (Breakthrough Varicella)
Breakthrough varicella on the abdomen of a vaccinated child.
Breakthrough varicella is infection with wild-type varicella-zoster virus (VZV) occurring in a vaccinated person more than 42 days after varicella vaccination. Breakthrough varicella is usually mild. Patients typically are afebrile or have low fever and develop fewer than 50 skin lesions. They usually have a shorter illness compared to unvaccinated people who get varicella. The rash is more likely to be predominantly maculopapular rather than vesicular. However, 25% to 30% of people vaccinated with one dose who get breakthrough varicella will have clinical features similar to unvaccinated people with varicella.
Since the clinical features of breakthrough varicella are often mild, it can be difficult to make a diagnosis on clinical presentation alone. Laboratory testing is increasingly important for confirming varicella and appropriately managing the patients and their contacts. Breakthrough varicella occurs less frequently among those who have received two doses of vaccine compared with those who have received only one dose; disease may be even milder among two-dose vaccine recipients, although the information about this is limited.
Transmission
Varicella is highly contagious. The virus can be spread from person to person by direct contact, inhalation of aerosols from vesicular fluid of skin lesions of acute varicella or zoster, and possibly through infected respiratory secretions that also may be aerosolized. A person with varicella is considered contagious beginning one to two days before rash onset until all the chickenpox lesions have crusted. Vaccinated people may develop lesions that do not crust. These people are considered contagious until no new lesions have appeared for 24 hours.
It takes from 10 to 21 days after exposure to the virus for someone to develop varicella. Based on studies of transmission among household members, about 90% of susceptible close contacts will get varicella after exposure to a person with disease. Although limited data are available to assess the risk of VZV transmission from zoster, one household study found that the risk for VZV transmission from herpes zoster was approximately 20% of the risk for transmission from varicella.
Although limited data are available to assess the risk of VZV transmission from zoster, one household study found that the risk for VZV transmission from herpes zoster was approximately 20% of the risk for transmission from varicella.
People with breakthrough varicella are also contagious. One study of varicella transmission in household settings found that people with mild breakthrough varicella (<50 lesions) who were vaccinated with one dose of varicella vaccine were one-third as contagious as unvaccinated people with varicella. However, people with breakthrough varicella with 50 or more lesions were just as contagious as unvaccinated people with the disease.
Varicella is less contagious than measles, but more contagious than mumps and rubella.
Complications
X-ray of pneumonia caused by varicella.
The most common complications from varicella are:
- In children: Bacterial infections of the skin and soft tissues
- In adults: Pneumonia
Severe complications caused by the virus include cerebellar ataxia, encephalitis, viral pneumonia, and hemorrhagic conditions. Other severe complications are due to bacterial infections and include:
Other severe complications are due to bacterial infections and include:
- Septicemia
- Toxic shock syndrome
- Necrotizing fasciitis
- Osteomyelitis
- Bacterial pneumonia
- Septic arthritis
People at High Risk for Severe Varicella
People at risk for severe varicella include:
- Immunocompromised people without evidence of immunity to varicella, such as:
- People with leukemia or lymphoma
- People on medications that suppress the immune system, such as high-dose systemic steroids or chemotherapeutic agents
- People with cellular immune-deficiencies or other immune system problems
- Newborns whose mothers have varicella from five days before to two days after delivery
- Premature babies exposed to varicella or herpes zoster, specifically:
- Hospitalized premature infants born at ≥28 weeks of gestation whose mothers do not have evidence of immunity
- Hospitalized premature infants born at <28 weeks of gestation or who weigh ≤1,000 grams at birth regardless of their mothers’ varicella immunity status
- Pregnant women without evidence of immunity to varicella
Immunocompromised People
Immunocompromised people who get varicella are at risk of developing visceral dissemination (VZV infection of internal organs) leading to pneumonia, hepatitis, encephalitis, and disseminated intravascular coagulopathy. They can have an atypical varicella rash with more lesions, and they can be sick longer than immunocompetent people who get varicella. New lesions may continue to develop for more than 7 days, may appear on the palms and soles, and may be hemorrhagic.
They can have an atypical varicella rash with more lesions, and they can be sick longer than immunocompetent people who get varicella. New lesions may continue to develop for more than 7 days, may appear on the palms and soles, and may be hemorrhagic.
People with HIV or AIDS
Children with HIV infection tend to have atypical rash with new crops of lesions presenting for weeks or months. The lesions may initially be typical maculopapular vesicular but can later develop into non-healing ulcers that become necrotic, crusted, and hyperkeratotic. This is more likely to occur in HIV-infected children with low CD4 counts.
Some studies have found that VZV dissemination to the visceral organs is less common in children with HIV than in other immunocompromised people with VZV infection. The rate of complications may also be lower in HIV-infected children on antiretroviral therapy or HIV-infected people with higher CD4 counts at the time of varicella infection. Retinitis can occur among HIV-infected children and adolescents.
Retinitis can occur among HIV-infected children and adolescents.
Most adults, including those who are HIV-positive, have already had varicella and are VZV seropositive. As a result, varicella is relatively uncommon among HIV-infected adults.
For more information about vaccinating immunocompromised people, including some groups with HIV-infection, see Special Considerations for Vaccination (Vaccination of HIV Infected Persons) in Prevention of Varicella: Recommendations of the Advisory Committee on Immunization Practices (ACIP).
Pregnant Women
Pregnant women who get varicella are at risk for serious complications, primarily pneumonia, and in some cases, may die as a result of varicella. Some studies have suggested that both the frequency and severity of VZV pneumonia are higher when varicella is acquired during the third trimester, although other studies have not supported this observation.
If a pregnant woman gets varicella in her first or early second trimester, her baby has a small risk (0. 4 to 2.0%) of being born with congenital varicella syndrome. The baby may have scarring on the skin; abnormalities in limbs, brain, and eyes, and low birth weight.
4 to 2.0%) of being born with congenital varicella syndrome. The baby may have scarring on the skin; abnormalities in limbs, brain, and eyes, and low birth weight.
If a woman develops varicella rash from 5 days before to 2 days after delivery, the newborn will be at risk for neonatal varicella. Historically, the mortality rate for neonatal varicella was reported to be about 30%, but the availability of VZV immune globulin and intensive supportive care have reduced the mortality to about 7%.
The vaccine is contraindicated for pregnant women. See Guidelines for Vaccinating Pregnant Women: Varicella.
Top of Page
Managing People at High Risk for Severe Varicella
Varicella-Zoster Immune Globulin
For people exposed to varicella or herpes zoster who cannot receive varicella vaccine, varicella-zoster immune globulin can prevent varicella from developing or lessen the severity of the disease. Varicella-zoster immune globulin is recommended for people who cannot receive the vaccine and 1) who lack evidence of immunity to varicella, 2) whose exposure is likely to result in infection, and 3) are at high risk for severe varicella.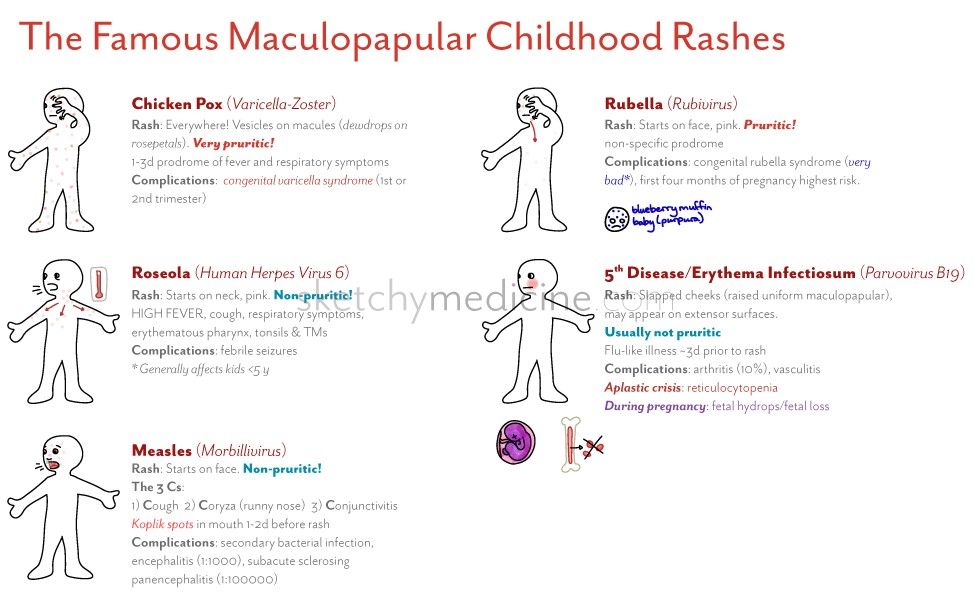
The varicella-zoster immune globulin product licensed for use in the United States is VariZIG™. VariZIG should be given as soon as possible after exposure to VZV; it can be given within 10 days of exposure. For more information on the recommendations for VariZIG use, see the Morbidity and Mortality Weekly Report article on Updated Recommendations for Use of VariZIG — United States, 2013. VariZIG is commercially available from a broad network of specialty distributors in the United States (list available at www.varizig.com).
Acyclovir Treatment
The American Academy of Pediatrics (AAP) recommends that certain groups at increased risk for moderate to severe varicella be considered for oral acyclovir or valacyclovir treatment. These high risk groups include:
- Healthy people older than 12 years of age
- People with chronic cutaneous or pulmonary disorders
- People receiving long-term salicylate therapy
- People receiving short, intermittent, or aerosolized courses of corticosteroids
Some healthcare providers may elect to use oral acyclovir or valacyclovir for secondary cases within a household.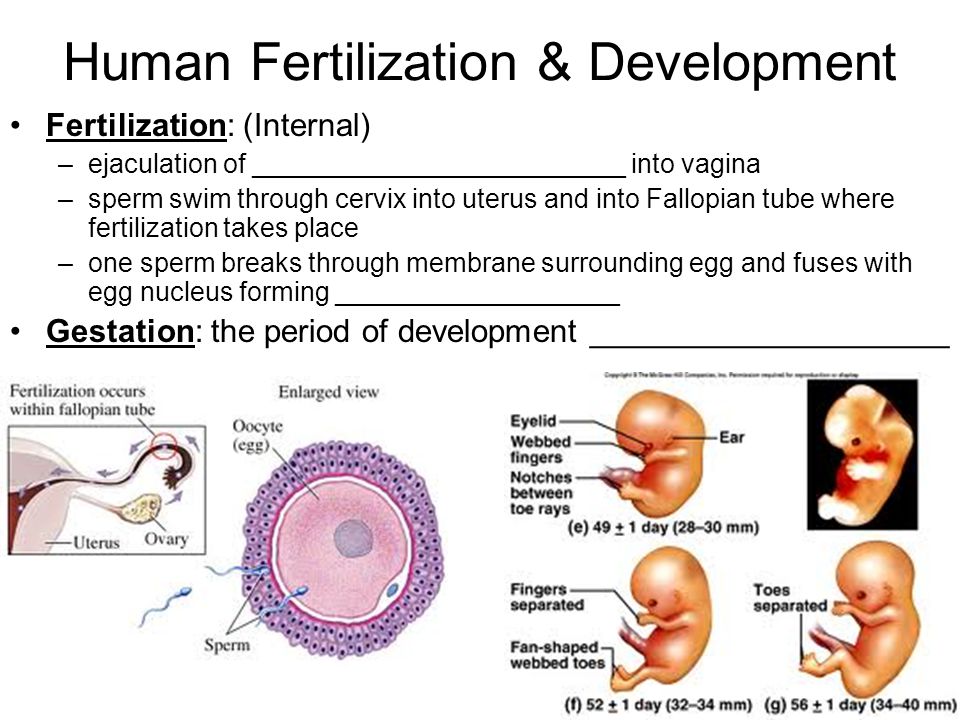 For maximum benefit, oral acyclovir or valacyclovir therapy should be given within the first 24 hours after the varicella rash starts.
For maximum benefit, oral acyclovir or valacyclovir therapy should be given within the first 24 hours after the varicella rash starts.
Oral acyclovir or valacyclovir therapy is not recommended by AAP for use in otherwise healthy children experiencing typical varicella without complications. Acyclovir is a category B drug based on the U.S. Food and Drug Administration’s Drug Risk Classification in pregnancy. Some experts recommend oral acyclovir or valacyclovir for pregnant women with varicella, especially during the second and third trimesters. Intravenous acyclovir is recommended for the pregnant patient with serious, viral-mediated complications of varicella, such as pneumonia.
Intravenous acyclovir therapy is recommended for severe disease (e.g., disseminated VZV such as pneumonia, encephalitis, thrombocytopenia, severe hepatitis) and for varicella in immunocompromised patients (including patients being treated with high-dose corticosteroid therapy for >14 days).
Famciclovir is available for treatment of VZV infections in adults, but its efficacy and safety have not been established for children. In cases of infections caused by acyclovir-resistant VZV strains, which usually occur in immunocompromised people, Foscarnet should be used to treat the VZV infection, but consultation with an infectious disease specialist is recommended.
In cases of infections caused by acyclovir-resistant VZV strains, which usually occur in immunocompromised people, Foscarnet should be used to treat the VZV infection, but consultation with an infectious disease specialist is recommended.
Assessing Immunity to Varicella
Two doses of varicella vaccine are recommended for all children, adolescents, and adults without evidence of immunity to varicella. Those who previously received one dose of varicella vaccine should receive their second dose for best protection against the disease.
Evidence of immunity to varicella includes any of the following:
- Documentation of age-appropriate varicella vaccination
- Preschool-age children (i.e., age 12 months through 3 years): one dose
- School-age children, adolescents, and adults: two doses
- Laboratory evidence of immunity or laboratory confirmation of disease*
- Birth in the United States before 1980 (should not be considered evidence of immunity for healthcare personnel, pregnant women, and immunocompromised people)
- Diagnosis or verification of a history of varicella or herpes zoster by a healthcare provider
*Commercial assays can be used to assess disease-induced immunity, but they lack sensitivity to detect vaccine-induced immunity (i. e., they might yield false-negative results).
e., they might yield false-negative results).
To verify a history of varicella, healthcare providers should inquire about:
- An epidemiologic link to another typical varicella case or to a laboratory confirmed case, or
- Evidence of laboratory confirmation, if testing was performed at the time of acute disease
People who have neither an epidemiologic link nor laboratory confirmation of varicella should not be considered as having a valid history of disease. For these people, a second dose of vaccine is recommended if they previously received only one dose. If a healthcare provider verifies the diagnosis based on the above criteria, then vaccination is not needed.
Routine testing for varicella immunity after two doses of vaccine is not recommended. Available commercial assays are not sensitive enough to detect antibodies after vaccination in all instances. Documented receipt of two doses of varicella vaccine supersedes results of subsequent serologic testing.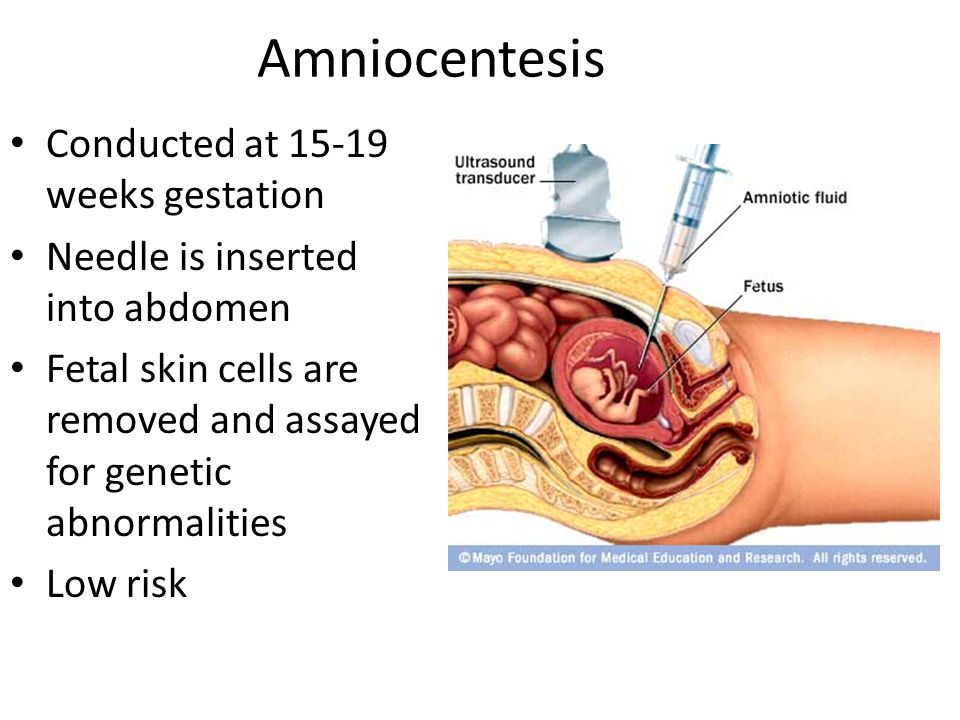
Preventing Varicella in Healthcare Settings
Nosocomial Transmission of VZV
Nosocomial transmission of VZV is well-recognized and can be life threatening to certain groups of patients. Reports of nosocomial transmission are uncommon in the United States since introduction of varicella vaccine.
Patients, healthcare providers, and visitors with varicella or herpes zoster can spread VZV to susceptible patients and healthcare providers in hospitals, long-term-care facilities, and other healthcare settings. In healthcare settings, transmissions have been attributed to delays in the diagnosis or reporting of varicella and herpes zoster and failures to implement control measures promptly.
Although all susceptible patients in healthcare settings are at risk for severe varicella and complications, certain patients without evidence of immunity are at increased risk:
- Premature infants born to susceptible mothers
- Infants born at less than 28 weeks gestation or who weigh ≤1000 grams, regardless of maternal immune status
- Immunocompromised people, including those who are undergoing immunosuppressive therapy, have malignant disease, or are immunodeficient
- Pregnant women
Management of Patients with Varicella
Healthcare providers should follow standard precautions plus airborne precautions (negative air-flow rooms) and contact precautions until lesions are dry and crusted.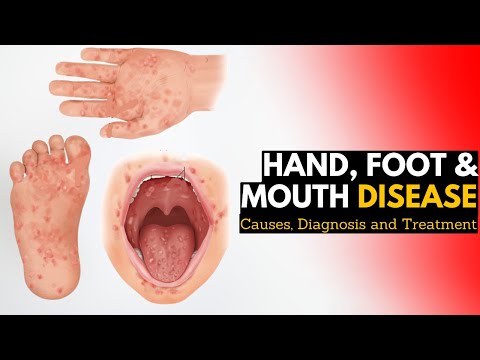 If negative air-flow rooms are not available, patients with varicella should be isolated in closed rooms with no contact with people without evidence of immunity. Patients with varicella should be cared for by staff with evidence of immunity.
If negative air-flow rooms are not available, patients with varicella should be isolated in closed rooms with no contact with people without evidence of immunity. Patients with varicella should be cared for by staff with evidence of immunity.
For more information, see:
- Preventing Varicella-Zoster Virus (VZV) Transmission from Zoster in Healthcare Settings
- Management of Patients with Herpes Zoster
- Management of Healthcare Personnel
- References and Resources
Top of Page
Impact of the U.S. Varicella Vaccination Program
Varicella used to be very common in the United States and contributed significantly to the burden of childhood disease. In the early 1990s each year, more than 4 million people got varicella,10,500 to 13,500 were hospitalized, and 100 to 150 died. More than 90% of cases, 70% of hospitalizations, and about half of the deaths occurred in children.
Main Findings from 1995-2019
- Varicella hospitalizations and deaths declined 94% and 97%, respectively, among people 50 years old and younger.
- The greatest decline in cases was among people 20 years old and younger who were born during the program, with 97% drop in hospitalizations and more than 99% drop in deaths.
- The risk of shingles is significantly lower among vaccinated children, including those who are immunocompromised.
- There is approximately an 80% lower risk of shingles among healthy vaccinated children compared to unvaccinated children who had wild-type varicella.
- The varicella vaccination is an effective and cost-saving public health intervention, both in terms of disease prevention and dollars saved. During the first 25 years:
- The U.S varicella vaccination program prevented an estimated 91 million cases, 238,000 hospitalizations, 1.1 million hospitalization days, and almost 2,000 deaths; and saved 118,000 life-years, at net societal savings of $23.4 billion.
- For every $1 spent, the estimated return on investment is $1.70; however, the benefits of the investment will continue to accrue beyond 2020.

Contagious Diseases | Pediatric Chickenpox
Chickenpox is a highly contagious disease, usually associated with childhood. By adulthood, more than 90 percent of Americans have had chickenpox.
The disease is caused by the varicella-zoster virus (VZV). Transmission occurs from person-to-person by direct contact or through the air.
Until 1995, chickenpox infection was a common occurrence, and almost everyone had been infected by the time he or she reached adulthood. However, the introduction of the chickenpox vaccine in 1995 has caused a decline in the incidence of chickenpox in all ages, particularly in ages one through four years.
What are the symptoms of chickenpox?
Symptoms are usually mild among children, but may be life threatening to adults and people with impaired immune systems. The following are the most common symptoms of chickenpox. However, each child may experience symptoms differently. Symptoms may include:
- fatigue and irritability one to two days before the rash begins
- itchy rash on the trunk, face, under the armpits, on the upper arms and legs, and inside the mouth
- feeling ill
- decreased appetite
The symptoms of chickenpox may resemble other skin problems. Always consult your child's physician for a diagnosis.
Always consult your child's physician for a diagnosis.
How is chickenpox spread?
Once exposed, the incubation period is typically 14 to 16 days, but it may take as few as 10 and as many as 21 for the chickenpox to develop. Chickenpox is contagious for one to two days before the appearance of the rash and until the blisters have dried and become scabs. The blisters usually dry and become scabs within four to five days of the onset of the rash. Children should stay home and away from other children until all of the blisters have scabbed over.
Family members who have never had chickenpox have a 90 percent chance of becoming infected when another family member in the household is infected.
How is chickenpox diagnosed?
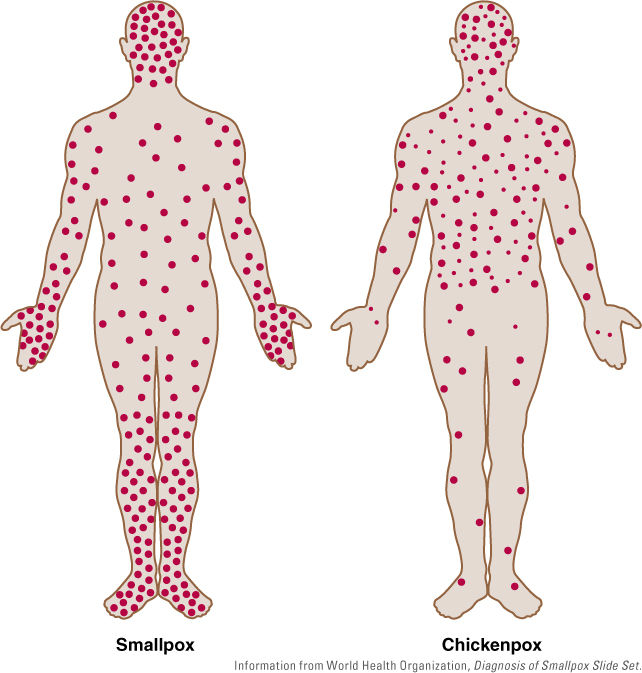
The rash of chickenpox is unique and therefore the diagnosis can usually be made on the appearance of the rash and a history of exposure.
Treatment for chickenpox:
Specific treatment for chickenpox will be determined by your child's physician based on:
- your child's age, overall health, and medical history
- extent of the condition
- your child's tolerance for specific medications, procedures, or therapies
- expectations for the course of the condition
- your opinion or preference
Treatment for chickenpox may include:
- acetaminophen or ibuprofen for fever (DO NOT GIVE ASPIRIN)
- antibiotics for treating bacterial infections
- calamine lotion (to relieve itching)
- antiviral drugs (for severe cases)
- bed rest
- increased fluid intake (to prevent dehydration)
- cool baths with baking soda or Aveeno (to relieve itching)
Children should not scratch the blisters, as this could lead to secondary bacterial infections. Keep your child's fingernails short to decrease the likelihood of scratching.
Keep your child's fingernails short to decrease the likelihood of scratching.
Immunity from chickenpox:
Most individuals who have had chickenpox will be immune to the disease for the rest of their lives. However, the virus remains dormant in nerve tissue and may reactivate, resulting in herpes zoster (shingles) later in life. Sometimes, a second case of chickenpox does occur. Blood tests can confirm immunity to chickenpox in people who are unsure if they have had the disease.
What complications are commonly associated with chickenpox?
Complications can occur from chickenpox. Those most susceptible to severe cases of chickenpox are adults and people with impaired immune systems. Complications may include:
- secondary bacterial infections
- pneumonia
- encephalitis (inflammation of the brain)
- cerebellar ataxia (defective muscular coordination)
- transverse myelitis (inflammation along the spinal cord)
- Reye syndrome (a serious condition which may affect all major systems or organs)
- death
Questions about chickenpox during pregnancy
How dangerous is chickenpox for a pregnant woman and is it necessary to be vaccinated? Doctors of medical clinics "Art-Med" answer questions about the danger of chickenpox for pregnant women.
Ask a Question
Pregnancy 22-23 weeks, 4-year-old daughter fell ill with chickenpox. I didn't get chicken pox. What are the consequences for the fetus?
Since you are constantly in contact with your daughter who is already ill, it makes little sense to isolate her from you - the infection could have already occurred. Chickenpox in the middle of pregnancy does not pose a great danger to the development of the fetus.
My wife has chickenpox, she is 12-13 weeks pregnant. She had chicken pox as a child. What consequences can be for the child, if so, how to determine?
Chickenpox in the early stages of pregnancy is not an absolute indication for abortion, the probability of any damage to the fetus is usually estimated at 2-3% (some authors up to 8%) - this is a low risk.
Is there a threat to the fetus if his mother (pregnancy 3 months) communicated with a person who is in the incubation period of chickenpox, although the mother herself had chickenpox in childhood? Is a carrier of infection a person who had chickenpox in childhood, but in this period of time is in daily contact with a sick chickenpox?
1. There is no threat to the fetus. 2. No, it is not.
There is no threat to the fetus. 2. No, it is not.
I am 24 years old, 22 weeks pregnant, I got chickenpox. How will this affect the child, what pathologies can there be?
If chickenpox occurs in mid-pregnancy, the risk of adverse effects on the fetus is low, to reduce the severity of the clinical manifestations of chickenpox, discuss with your doctor the possibility of using immunoglobulin.
My twins in the garden (their group) are in chickenpox quarantine. Two children fell ill in a week, my children did not get chickenpox. I am 38 weeks and 2 days pregnant. What should I do? How dangerous is this for an unborn baby? If there was contact, are the children already infected?
You have a very ambiguous situation. If you get sick, the chances that the unborn baby will suffer greatly is very high. Therefore, if possible, completely exclude contact with twins until the end of the incubation period, do not take them to the garden, because if someone else in the group gets sick, the incubation period will be extended. Then it will be dangerous for you to return home with a newborn. If the babies do not get sick within two days, consider that you and your baby in utero have happily avoided chickenpox.
Then it will be dangerous for you to return home with a newborn. If the babies do not get sick within two days, consider that you and your baby in utero have happily avoided chickenpox.
My pregnancy is 24-25 weeks. The windmill has started. No temperature yet. What is the danger to the child? What research needs to be done and when?
Chicken pox in mid-pregnancy does not lead to developmental defects in the fetus, since the main organ formation has already been completed. The risk of intrauterine infection of the fetus (pneumonia) is slightly increased. The situation does not require termination of pregnancy. Regarding the need for any therapeutic measures (introduction of immunoglobulin, etc.), consult with an infectious disease specialist. The most commonly used expectant tactics, symptomatic treatment. Be sure to observe quarantine so as not to infect others, refrain from visiting the antenatal clinic and other medical centers for the next 3 weeks.
My wife fell ill with chickenpox at the 11th week of pregnancy, before that she had been on sick leave for about a month. By the time she recovered, she was already 13 weeks old. They passed the necessary blood tests from an infectious disease specialist, the tests do not predict anything bad. All doctors say to give birth, but no one has ever said about possible pathologies. What is the risk?
Chickenpox transferred in the early stages of pregnancy is not an absolute indication for termination of pregnancy, the risk of adverse effects on the fetus is present, but not high - about 2-3%. Therefore, in your case, termination of pregnancy was not offered. To exclude gross anomalies in fetal development, a standard prenatal screening program is recommended - ultrasound - 3-4 times during pregnancy, blood tests for AFP, hCG, free estriol at 16-20 weeks.
My sister got chicken pox when she was four months pregnant.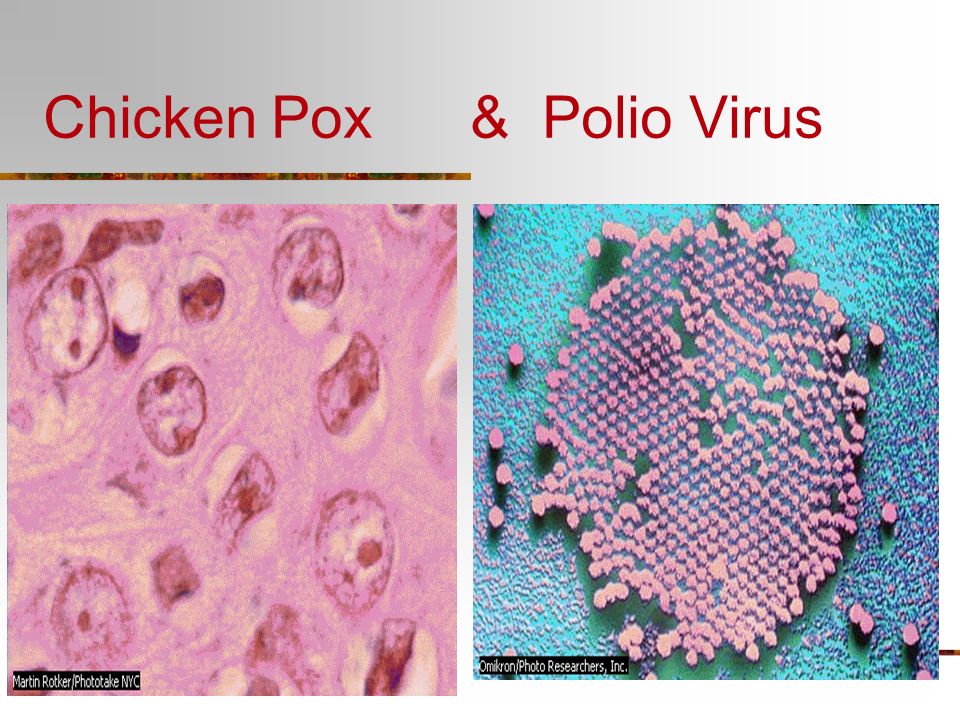 Is there a chance that the baby will be born healthy or not?
Is there a chance that the baby will be born healthy or not?
If you have had chicken pox in the second trimester of pregnancy, the likelihood of such an event remains low. Recommendations in such a situation are standard - to exclude gross anomalies in the development of the fetus, do a blood test for AFP, hCG and St. estriol at 16-20 weeks and ultrasound at 22-23 weeks of fundamental or expert level. In order not to create a threat of infecting other patients, you can contact the medical institution no earlier than 3-4 weeks after the onset of the rash.
At 17 weeks pregnant, I had contact with a recent chickenpox survivor with residual signs of the disease. I didn't get sick as a child. How big are the chances of getting sick? And is it worth it to vaccinate in this situation?
How likely you are to get chickenpox after exposure depends on your individual susceptibility to infections. Pregnant women should not be vaccinated against chickenpox. In order to prevent severe clinical manifestations, it is desirable to carry out treatment to support immunity - the introduction of specific immunoglobulin, immunocorrective drugs. To do this, I recommend contacting a virologist.
In order to prevent severe clinical manifestations, it is desirable to carry out treatment to support immunity - the introduction of specific immunoglobulin, immunocorrective drugs. To do this, I recommend contacting a virologist.
I am 32 years old, second pregnancy, 5-6 weeks. My son got chickenpox in the garden, we live together. As a child, I had chickenpox, how dangerous is it for the fetus?
Childhood varicella usually provides lifelong immunity, relapse is rare. That is, you are likely to have reliable protection against this infection. It makes no sense to carry out any quarantine measures to isolate the child - if infection were possible, then it would have already happened.
My daughter goes to kindergarten, a child in her group got chicken pox a week ago. One of these days we will go to Moscow and would like to meet our friend. She is pregnant - about 5 months. I don't know if she had chicken pox or not. My child did not have chickenpox. Do you think we can meet with our friend or is it better to wait?
My child did not have chickenpox. Do you think we can meet with our friend or is it better to wait?
If you can, please specify if your friend has had chicken pox. If not, then it is better to refrain from contact.
My wife (she is 36 years old) developed chickenpox at about the seventh week of pregnancy, she contracted it from her sick son. Information is very different both on the Internet and from doctors, including geneticists. What is the likelihood of fetal damage?
The probability of damage to the fetus is not very high - about 3.5%. A born baby may experience congenital pneumonia, and a child may also be born with a syndrome of congenital chickenpox (areas of skin scarring, hypoplasia of the bones and muscles of the limbs in the same places, neurological disorders, including mental retardation, rarely - eye damage).
Is chickenpox transmitted through objects, such as door handles, dishes? I live with my husband in the family, my husband's sister often comes to visit us, and she has one child seriously ill with chicken pox, and after 2 weeks the other fell ill. I am pregnant, the term is 6 weeks, my daughter (she is 3 years old) communicated with patients for only a couple of minutes. After that, I washed her hands and face with soap. I did not get sick in childhood, I did everything for myself and my daughter. What to do? How does chickenpox affect pregnancy?
I am pregnant, the term is 6 weeks, my daughter (she is 3 years old) communicated with patients for only a couple of minutes. After that, I washed her hands and face with soap. I did not get sick in childhood, I did everything for myself and my daughter. What to do? How does chickenpox affect pregnancy?
Chickenpox is an acute viral disease that is transmitted by airborne droplets (not through objects). The causative agent of chickenpox is unstable in the external environment and enters the body through the mucous membranes of the upper respiratory tract. The incubation period (from the moment of infection to the manifestation of the disease) lasts an average of 14 days (from 11 to 21 days). The patient is subject to isolation at home until the 5th day from the moment the last element of the rash appears. Disinfection is not carried out. Children under the age of 3 who have been in contact with a patient with chickenpox and who have not had it before are separated from the 11th to the 21st day, counting from the moment of contact. If your child did not get sick, then the infection probably did not pass on to you either. If you have any doubts, please contact your doctor for examination.
If your child did not get sick, then the infection probably did not pass on to you either. If you have any doubts, please contact your doctor for examination.
I am 17 weeks pregnant and 26 years old. At 14-15 weeks I had chicken pox. What does this mean for the child? What research needs to be done and which specialists to visit?
The varicella-zoster virus rarely causes harm to the fetus. You need to do an ultrasound at 18-24 weeks of pregnancy. Just tell the doctor about the infection, let him pay attention to the development of the bones of the skull and limbs. You can make an appointment with an obstetrician-gynecologist for a consultation and conduct examinations at the ART-MED clinic.
I am 34 weeks pregnant, I will have close contact with a child with chickenpox (rash, fever), I had chickenpox as a child, is this a threat to me and my child?
Cases of reinfection with varicella are rare, but nonetheless known. Intrauterine chickenpox transferred by the fetus can be complicated by pneumonia, neurological disorders, and even intrauterine death. Therefore, it is better not to take risks and exclude close contact with a sick child for at least 3-4 weeks.
Intrauterine chickenpox transferred by the fetus can be complicated by pneumonia, neurological disorders, and even intrauterine death. Therefore, it is better not to take risks and exclude close contact with a sick child for at least 3-4 weeks.
My wife had chickenpox when she was a child. She is pregnant at 24 weeks. Had contact with a child who has chickenpox. Can a fetus get chickenpox?
Chickenpox usually acquired during childhood provides lifelong immunity, although rare cases of recurrence are known. In your situation, short-term contact of the wife with a sick child is unlikely to lead to any adverse consequences.
I have a question for you. I am 28 weeks pregnant, I already had chickenpox as a child, an employee (we are in the same office) has a child with chickenpox at the moment. Can this affect my child, I heard that if I myself had been ill, then for me it is not dangerous, but dangerous for the fetus. Is it true? Goodbye.
Is it true? Goodbye.
Chickenpox usually acquired in childhood gives lifelong immunity; cases of recurrence are rare. Find out if your co-worker is immune to varicella—if so, the risk to your fetus seems negligible.
I am 22 years old, at 13 weeks I got chickenpox. No temperature, only dots covered. Doctors, without really explaining anything, sent me for interruption. But I want to keep the baby. What is the percentage that he will be born healthy and what tests can be done for pathology?
The risk of damage to the fetus in case of chickenpox in the first trimester of pregnancy is at least 8%. Methods of prenatal diagnostics (ultrasound, blood tests, invasive methods) may be powerless in the search for defects in the development of the central system of the fetus, vision, hearing, immune system, etc. Doctors' recommendations for termination of pregnancy in your case seem justified. I do not invite you to a face-to-face consultation in the near future, since chickenpox is a very contagious disease and can be dangerous for other pregnant patients. If pregnancy persists, I recommend ultrasound at 20-22 weeks, a triple test at 18-20 weeks.
If pregnancy persists, I recommend ultrasound at 20-22 weeks, a triple test at 18-20 weeks.
I am 25 years old. First pregnancy. Term 9 weeks. I got sick with chicken pox. What are the consequences of the disease?
Chicken pox at 9 weeks of pregnancy is a very unpleasant event. Although this infection is not an official indication for termination of pregnancy (as is the case with rubella), nevertheless, the risk of fetal abnormalities is estimated to be at least 8%. It is unrealistic to predict what specific problems with the development of the fetus may appear, the possibilities of prenatal diagnosis in this case are rather limited. If you are a healthy woman, and there were no problems with the onset of pregnancy, then in such a situation, you can discuss the possibility of terminating the pregnancy. I can’t invite you to a face-to-face consultation in the next month, because chickenpox is very contagious and can be dangerous for other pregnant patients. If the pregnancy persists, follow the standard screening program (“sieving”) for gross fetal developmental defects - ultrasound 3-4 times, a triple test at 16-20 weeks.
If the pregnancy persists, follow the standard screening program (“sieving”) for gross fetal developmental defects - ultrasound 3-4 times, a triple test at 16-20 weeks.
I had chickenpox as a child. Now my husband and I want to have a baby, and I'm not 100% sure that the pregnancy has not yet come, 10 more days before menstruation. Next week I will have contact with a child who has had chickenpox for a week. What is the risk of infection itself and the fetus (or complications?). Asking because I can avoid contact, but it's work.
It is generally accepted that chickenpox suffered in childhood gives a stable lifelong immunity. Although in practice rare cases of repeated infection are known. The risk of contracting chickenpox in the situation you describe is likely low. But if you are planning a pregnancy, then planned contacts with infectious patients, especially with viral infections, should be excluded. To find out about the presence of pregnancy for a period of 1-2 weeks, a blood test for hCG will help.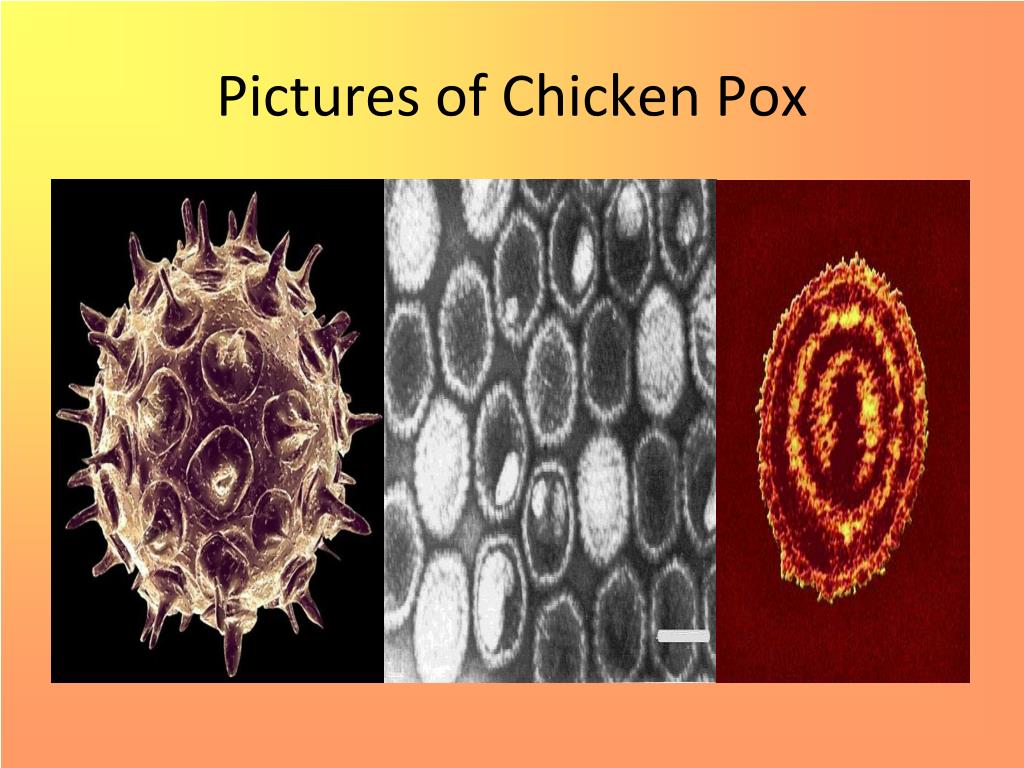
My wife is 40 weeks old and has contracted chickenpox. Characteristic Rash on the body, temperature, in general, all the symptoms of chickenpox. It is most likely that she is. Of course, we called the doctor, but I would like to know the following. What is the prognosis for chickenpox at this time, for the mother and for the fetus? What could be the consequences? What maternity hospitals with infectious diseases departments are there in Moscow? Which one is the best and what should you pay attention to when choosing such a maternity hospital?
First of all, you should finally make sure that your wife really has chicken pox. This requires consultation with an infectious disease specialist. Since the pregnancy is already full-term, it is advisable for the patient to deliver. The disease at this stage of pregnancy will most likely not have any effect on the child. It is important not to infect it after birth. In Moscow, there are only two maternity hospitals that accept patients with such infectious diseases for childbirth - the maternity hospital at the 2nd Clinical Infectious Diseases Hospital and at the 36th City Clinical Hospital. Both maternity hospitals are identical, and you should probably pay attention only to their location in relation to the location of your residence.
Both maternity hospitals are identical, and you should probably pay attention only to their location in relation to the location of your residence.
I am 30 years old, 4 weeks pregnant, diagnosed with chickenpox, temperature 38.5, itching. Is it possible to leave the fetus, what could be the consequences, if so, what medicines can be taken?
Chicken pox in such early stages of pregnancy is an unpleasant situation. Officially, this disease is not a reason for terminating a pregnancy, but the risk of fetal developmental defects, including those that are not amenable to any diagnostic methods, is usually estimated at at least 8%. To resolve this issue, it is necessary to compare the chances of being able to still have a pregnancy and the risk of anomalies in the fetus. Given that you have an infection that is dangerous for other patients, I do not invite you to a face-to-face consultation in the next month. If you keep the pregnancy, then do an ultrasound scan every 4 weeks, biochemical tests do not develop fetal defects at 10-14 weeks and 16-20 weeks.
Pregnancy 10 weeks, at 6-7 weeks she had a rotovirus infection. Is it possible to find out with the help of three-dimensional ultrasound whether the disease affected the child, that is, to identify malformations?
There are not enough observations about the possibility of the impact of rotavirus infection on the growing fetus. For viral infections in early pregnancy, only for one there is a categorical recommendation for termination of pregnancy - this is rubella. For other types of viral infections (respiratory, hepatitis, CMV, herpes, chicken pox, measles), there are no such unambiguous recommendations, pregnancy is usually continued, although some risk to the fetus remains. Probably, it is better for you to consult with an infectious disease specialist at the Research Institute of Epidemiology and Microbiology. G. N. Gabrichevsky. Given the significant uncertainty in the prognosis for the fetus and the lack of reliable diagnosis of intrauterine infection with rotovirus in a woman with intact childbearing function, the possibility of abortion can be discussed. Three-dimensional ultrasound cannot reveal the entire spectrum of developmental anomalies, including damage to the organs of hearing, vision, and the immune system.
Three-dimensional ultrasound cannot reveal the entire spectrum of developmental anomalies, including damage to the organs of hearing, vision, and the immune system.
May 26 will be 36 weeks pregnant (first day of last period September 16). From 18 weeks I take ginipral and up to 36 weeks (as prescribed in the antenatal clinic) due to cramping uterine contractions and tone, as well as a slightly open cervix by 1 finger. Almost the entire pregnancy I tried to lie down, because. any action causes petrification in the abdomen. And today (May 24), my eldest daughter was diagnosed with chickenpox, I was in contact with her and now I’m horrified (I didn’t get chickenpox as a child), I don’t know what to do, because if I cancel ginipral and childbirth can come soon and plus I I can get chickenpox and a newborn (which is very dangerous) from me. Maybe you need to do a caesarean without waiting for a natural birth?
First of all, don't panic, as it won't help anyway. You need to continue treatment aimed at maintaining pregnancy and not necessarily with the help of Ginepral. This treatment should be carried out only in a hospital setting, as the risk of preterm birth remains. The threat of premature birth and the risk of getting chickenpox are not indications for a caesarean section. It is not at all necessary that you will get this disease and, moreover, it is not necessary that the newborn will suffer from this. You should completely isolate yourself from the sick eldest daughter and go to the hospital under the supervision of doctors.
You need to continue treatment aimed at maintaining pregnancy and not necessarily with the help of Ginepral. This treatment should be carried out only in a hospital setting, as the risk of preterm birth remains. The threat of premature birth and the risk of getting chickenpox are not indications for a caesarean section. It is not at all necessary that you will get this disease and, moreover, it is not necessary that the newborn will suffer from this. You should completely isolate yourself from the sick eldest daughter and go to the hospital under the supervision of doctors.
The gestational age is 34-35 weeks, the oldest child in the garden, but not in his group, has chickenpox, my son was ill with it a year ago, but I myself did not get sick in childhood. I didn’t get sick even when my son was sick, although there was close contact (and kissed him, the bubbles burst when I smeared them and the liquid from the bubbles got into my eyes). Chickenpox was severe in my son with a temperature of 38. 5 and a severe rash. Is chickenpox dangerous for me and for my unborn child. To take the child to the garden or not? Can I get infected if I didn't get infected through closer contact?
5 and a severe rash. Is chickenpox dangerous for me and for my unborn child. To take the child to the garden or not? Can I get infected if I didn't get infected through closer contact?
Chicken pox poses a certain risk to pregnancy. Based on the situation you presented, the probability for you to get chickenpox is no greater than for everyone else, since there is no direct contact with a child who has fallen ill in another group of kindergarten. If you still have doubts, it is better not to take your child to the kindergarten for the period of quarantine.
Chickenpox ("chickenpox"): why is this "childhood" infection dangerous for pregnant women?
| Attention, chicken pox! How to protect a pregnant woman from infection if someone in the family gets sick |
| after the last rash appeared) If someone in your family had contact with a sick person and could potentially be infected. It may manifest the first manifestations of the disease in the period from 7 to 21 days from the moment of contact with the patient.  According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because in case of illness, there is a risk of infection. According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because in case of illness, there is a risk of infection. |
Varicella (chicken pox)
Pathogen - DNA-containing herpes virus type 3 Varicella-Zoster
Incubation period - from 7 to 17 days
Rash - appears simultaneously with an increase in temperature or several hours later. First, small spots form, which quickly turn into papules and vesicles. Vesicles are usually unicameral. Rashes are located on the skin of the trunk, face, limbs, scalp, less often on the mucous membranes of the mouth, respiratory tract, eyes, and external genital organs.
Rash may be accompanied by itching. On the mucous membranes, the elements of the rash quickly macerate with the formation of superficial erosions that heal within 1-2 days. On the skin, the bubbles gradually dry out and become covered with crusts. After exfoliation of the crusts, light pigmentation remains in their place for a long time, in rare cases - scars.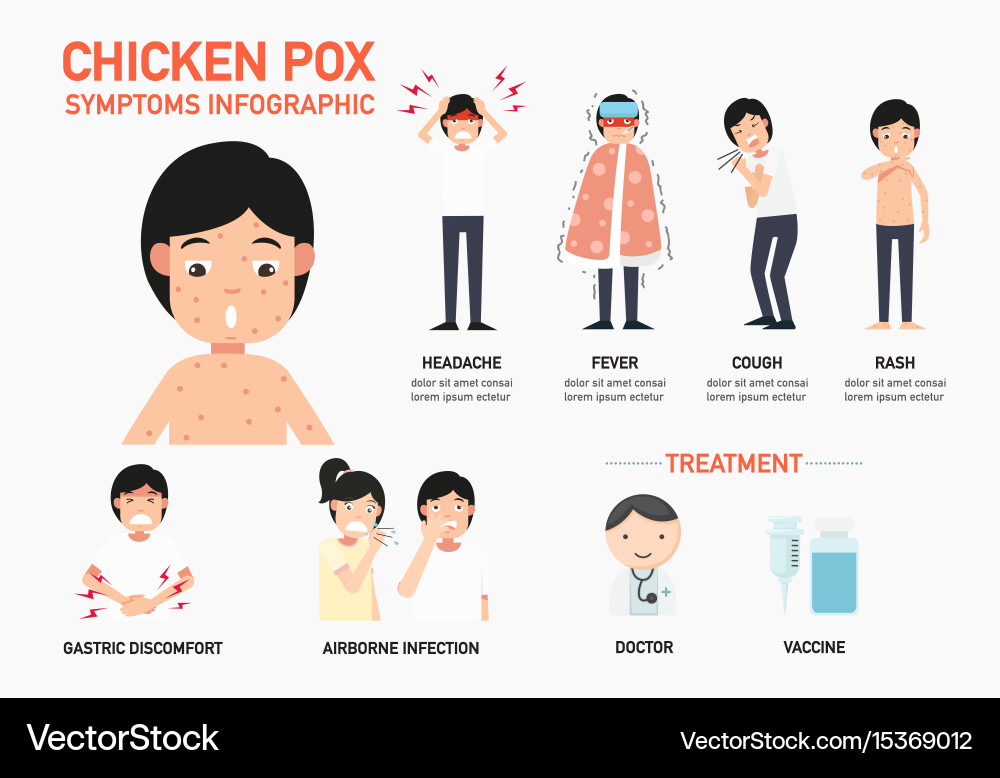 The process of rash occurs in jolts, with an interval of 1-2 days for 2-4 days, in rare cases up to 7 days or more.
The process of rash occurs in jolts, with an interval of 1-2 days for 2-4 days, in rare cases up to 7 days or more.
There is a false polymorphism of the rash.
Infectiousness period - 10-12 days 1-2 days before the appearance of the rash, the entire period of the rash, up to 5 days after the
appearance of the last rash (blister - vesicles).
Danger for pregnant women - the most unfavorable first trimester and the last week before delivery. Fetal risk is lowest between 20 and 35 weeks. Infection of a pregnant woman in the 1st trimester may result in the death of the embryo. When infected before the 20th week of pregnancy, there is a danger of the formation of congenital vitrine syndrome. This pathology is characterized by: a violation of the normal development of the limbs, brain, organs of vision, the formation of scars on the skin, as well as a general delay in intrauterine development. A pregnant woman, who fell ill on the eve of childbirth, may have a child with chickenpox of a newborn.
In general, the pathology of pregnancy is not common, so the disease is not a direct indication for termination of pregnancy. Pregnant women must undergo prenatal screening (double and triple tests), ultrasound (especially for a period of 20-22 weeks). In some cases, a study of amniotic fluid by PCR for the presence of virus DNA in them.
Prevention - isolation of the patient up to 5 days after the last rash. Contacts up to 3 years old, not sick, are isolated from 11 to 21 days from the moment of contact. Isolation of patients for 4 days from the onset of the disease, newborns with congenital rubella ─ up to 1 year. Contacts are not allowed in children's groups for 21 days (from the moment of isolation of the patient), monitoring of contacts.
Prophylactic vaccination available. The virus persists in the body for life, but recurrence after an illness is very rare. When the virus is activated, another form of infection develops - herpes zoster (zoster).
Emergency prophylaxis on contact (if the patient has not previously been ill and has no vaccination data) - passive immunization: donor immunoglobulin 0. 2-0.5 ml / kg in the first 2 days.
2-0.5 ml / kg in the first 2 days.
Conclusion: If you have a family member with chickenpox, they need to be isolated for 10 to 12 days: 12 days before the rash appears and up to 5 days after the rash appears. To avoid infecting others, especially pregnant women, stay at home and avoid contact with anyone for six days after the rash begins to appear.
3. Visipans are located on the trunk, face, limbs, less often on the mucous membranes of the mouth, eyes, and respiratory tract.
for pregnant women!
Pregnant women must undergo prenatal screening (double and triple tests) and ultrasound (especially at 20-22 weeks).
2. Emergency prophylaxis by contact (if the patient has not been ill before and has no data on vaccinations) - passive immunization: donor immunoglobulin in the first 2 days.

How to protect a pregnant woman from
infection if someone in the family gets sick
If someone in your family had contact with a sick person and could potentially be infected.
It may manifest the first manifestations of the disease in the period from 7 to 21 days from the moment of contact with the patient. According to such a person, during this period it is also not advisable to communicate with a pregnant woman, because in case of illness, the risk of infecting others occurs 1-2 days before the
rash appears. and then the entire period of rash. According to such a person, it is also not advisable to communicate with a pregnant woman during this period, because it is possible not to notice the early manifestations of the disease, and during this period the transmission of the infection is already potentially possible.