Tummy separation after birth
Diastasis Recti (Abdominal Separation): Symptoms & Treatment
Overview
Diastasis recti happens when a person's abdomen stretches during pregnancy and creates a gap in the abdominal muscles.What is diastasis recti?
Diastasis recti (diastasis rectus abdominis or diastasis) is the separation of the rectus abdominis muscles during and after pregnancy. The rectus abdominis runs vertically along the front of your stomach. It's frequently referred to as someone's "six-pack abs." It's divided into left and right sides by a band of tissue called the linea alba that runs down the middle. As your uterus expands during pregnancy, the abdominals are stretched and the linea alba thins and pulls apart. This band of tissue gets wider as it's pushed outward.
Once you deliver your baby, the linea alba can heal and come back together. It's highly elastic and retracts backs (like a rubber band). When the tissue loses its elasticity from being overstretched, the gap in the abdominals will not close as much as it should. This is diastasis recti.
If you have diastasis, your belly may appear to stick out just above or below the belly button, making you appear pregnant months or years after giving birth.
Why does diastasis recti happen?
Pregnancy puts a lot of pressure on your abdomen (abs). The abdomen is made up of left and right ab muscles and a thin band of connective tissue (linea alba) in between. They are pushed outward and stretched to make room for the growing baby. Diastasis recti occurs when the linea alba is overstretched and doesn't come back together. The left and right sides of the abdominals stay separated. It's also referred to as an "ab gap" or abdominal separation.
Who gets diastasis recti?
Diastasis recti is most common in pregnant and postpartum women (it can also be seen in men and infants). Diastasis recti usually develops in the third trimester. There is increased pressure on the abdominal wall because the baby is growing quickly during this time. Most people don't notice diastasis recti until the postpartum period.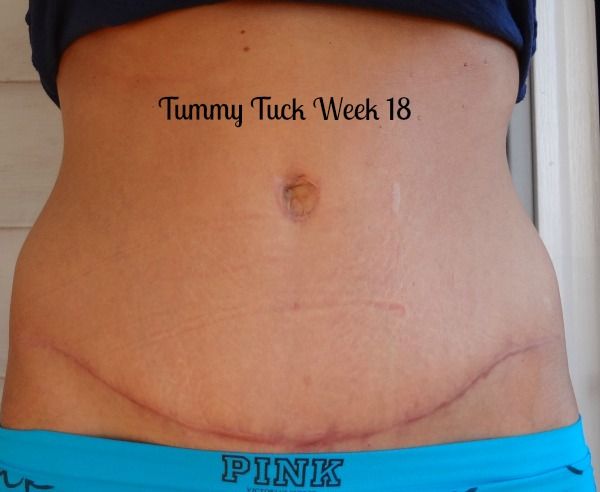
How common is diastasis recti?
Diastasis recti is extremely common in those who are pregnant and during the postpartum period. It affects 60% of people. It usually resolves itself within eight weeks of delivery. About 40% of those who have diastasis recti still have it by six months postpartum.
Symptoms and Causes
What are the symptoms of diastasis recti?
Most people don't notice signs of diastasis recti until they are postpartum. You can have diastasis recti during pregnancy, but it's hard to distinguish because your abdomen is stretched.
Common signs of diastasis recti during the postpartum period are:
- A visible bulge or "pooch" that protrudes just above or below the belly button.
- Softness or jelly-like feeling around your belly button.
- Coning or doming when you contract your ab muscles.
- Difficulty lifting objects, walking or performing everyday tasks.
- Pain during sex.
- Pelvic or hip pain.

- Low back pain.
- Poor posture.
- Urine leaking when you sneeze or cough.
- Constipation.
- Feeling weak in your abdominals.
What does diastasis recti feel like?
Diastasis recti is not painful. You may feel pain associated with some of the side effects of diastasis, but the ab separation itself doesn't hurt. You may feel weakness in your core when doing once easy tasks, like lifting a laundry basket. Some people feel a jelly-like texture in the space between the left and right abdominals when contracting the ab muscles.
How do I know if I have diastasis recti?
There are some common signs that can signal you have diastasis recti. One of the most common signs of diastasis recti is a bulge in your midsection that doesn't go away, even after exercising or losing weight gained during pregnancy. Another sign is that your belly cones or domes when you lean back on a chair or get up out of bed. You can check for diastasis recti on your own, but it is always a good idea to speak with your healthcare provider about your symptoms.
What are the risk factors for developing diastasis recti?
Several factors can increase your risk for developing diastasis recti:
- Having multiple pregnancies (especially back-to-back).
- Being over 35 years old.
- Having multiples (such as twins or triplets).
- Having a heavy or big baby.
- Being extremely petite.
- Vaginal delivery. Pushing can increase abdominal pressure.
Diagnosis and Tests
How is diastasis recti diagnosed?
Your healthcare provider will evaluate if diastasis is present, where it's located and how severe it is. Diastasis recti can occur above the belly button, below the belly button and at the belly button.
Your provider will use their hands and fingers to feel the abdominal area for gaps and muscle tone. Some providers may use ultrasound, measuring tape or a tool called a caliper for a more accurate measurement. This exam typically occurs at your postpartum appointment before being cleared for exercise.
An abdominal gap wider than 2 centimeters is considered diastasis recti. Diastasis recti is also measured in finger widths, for example, two or three fingers' separation.
Your healthcare provider may recommend movements for diastasis recti or they may refer you to a specialist for additional treatment.
How do I test myself for diastasis recti?
You can test yourself for diastasis recti:
- Lie on your back with your knees bent and feet flat on the floor.
- Lift your shoulders slightly off the ground, keeping one hand behind your head for support. Almost like you are doing a sit-up. Look down at your belly.
- Move your other hand above your belly button area, palms down and fingers towards your toes.
- Use your fingers to feel for a gap between the abs. See how many fingers can fit in the gap between your right and left abdominals.
If you feel a gap of two or more finger widths, discuss your concerns with your healthcare provider. They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
Management and Treatment
How can I fix diastasis recti?
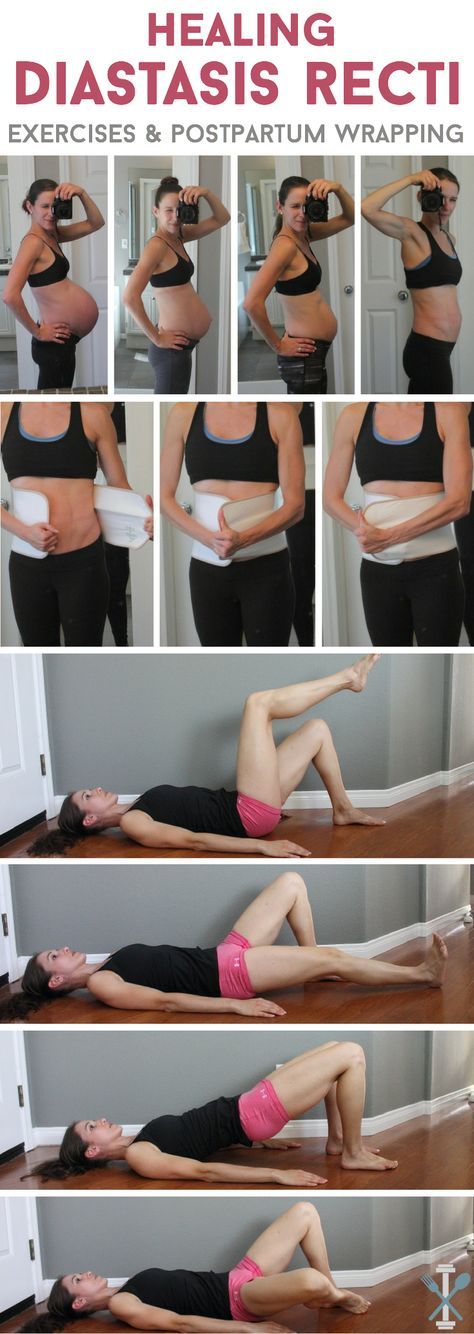
To fix diastasis recti, you'll need to perform gentle movements that engage the abdominal muscles. Before starting an exercise program, be sure it's safe for diastasis recti. Work with a fitness professional or physical therapist who has experience with diastasis recti. They can create a treatment plan to make sure you are performing the movements correctly and progressing to more challenging movements at the right time.
Certain movements will make abdominal separation worse. During the postpartum period, there are some modifications you should make:
- Avoid lifting anything heavier than your baby.
- Roll onto your side when getting out of bed or sitting up. Use your arms to push yourself up.
- Skip activities and movements that push your abdominals outward (like crunches and sit-ups).
Some people use binding devices (elastic belly bands) to help hold their belly in and support the lower back. Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Can you fix diastasis recti without surgery?
Yes, it's possible to fix diastasis recti without surgery. Surgery is rarely performed to fix diastasis recti. Healthcare providers will recommend physical therapy or at-home exercises to help heal diastasis before surgical methods. Surgery is performed in cases of hernia (when an organ pushes through the linea alba) or if a woman wants diastasis recti surgery (a tummy tuck).
What are the best exercises for diastasis recti?
The best exercises for diastasis recti are those that engage the deep abdominals. Most diastasis recti exercises involve deep breathing and slow, controlled movements. Unfortunately, many of the most common ab exercises (like crunches) can worsen your diastasis. Before starting abdominal exercises, ask your healthcare provider to check you for diastasis recti.
What movements make diastasis recti worse?
Any movement that bulges the abdominal wall forward can cause more damage to your diastasis recti. Everyday movements like getting out of bed or up off a chair can worsen diastasis. Try to be mindful about how you are using your abdominals as you go about your day.
These exercise movements should be avoided if you have diastasis recti:
- Crunches or sit-ups of any kind.
- Planks or push-ups (unless using modifications).
- Downward dog, boat pose and other yoga poses.
- Double leg lifts, scissors and other Pilates moves.
- Any exercise that causes your abdominals to bulge, cone or dome.
Prevention
How do I prevent diastasis recti?
Some abdominal separation is normal and expected with pregnancy. There are some things you can do to lower your risk for developing diastasis recti:
- Healthy weight gain during pregnancy: Exercising and eating healthy foods to keep weight gain within a healthy range.

- Proper posture and deep breathing: Stand up straight with your shoulders back. Take deep breaths that allow your ribs to expand and not just your belly.
- Safe core exercises: Avoid exercises like sit-ups and crunches that put pressure on your abdominals after 12 weeks of pregnancy and postpartum.
- Don't strain while lifting: Certain day-to-day activities like lifting grocery bags or your children can put undue strain on your abdominals.
- Log roll when getting out of bed: If you're pregnant or postpartum, roll to one side and use your arms to push up out of bed.
Outlook / Prognosis
How long will it take to heal my diastasis recti?
The amount of time it takes to heal diastasis recti depends on the amount of ab separation and how consistent you are with strengthening exercises. After several weeks postpartum, this gap will start to close as your muscles regain strength. If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
Can I get diastasis recti again?
Yes, you can heal your diastasis recti and get it again. Your risk for diastasis recti increases the more times you are pregnant. Think of the linea alba as a rubber band that is continuously stretched. Over time, the rubber band will lose its elasticity. The linea alba may not regain its original shape or form after being stretched through multiple pregnancies.
Is it too late to fix my diastasis recti?
It's never too late to repair your diastasis recti. With the proper exercises, you can fix your ab separation years after you've delivered your last baby.
Are there complications from diastasis recti?
If left untreated or in severe cases of diastasis recti, complications can include:
- Umbilical hernia.
- Increase in back pain.
- Pain during sex.
- Urinary incontinence.
- Pelvic and hip pain.
Living With
When should I see my healthcare provider?
Diastasis recti is a common and easily treated condition. If you have more than a two-finger gap between your abdominals or are experiencing pain, contact your healthcare provider for a diagnosis. They may want you to see a physical therapist or pelvic floor specialist to help strengthen your abdominal muscles.
A note from Cleveland Clinic:
Diastasis recti can make you appear pregnant years after your last baby. Discuss your concerns with your healthcare provider so they can diagnose and treat you. Getting treatment can help you feel more confident in your body and correct any pain you are experiencing.
Abdominal separation (diastasis recti) | Pregnancy Birth and Baby
Abdominal separation (diastasis recti) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is abdominal separation?
Some women find their stomach muscles weaken and separate during and after pregnancy. This is known as abdominal separation, ‘diastasis recti’ or ‘recti divarication’. It is a common condition and often gets better in the first 8 weeks after having your baby.
This is known as abdominal separation, ‘diastasis recti’ or ‘recti divarication’. It is a common condition and often gets better in the first 8 weeks after having your baby.
Abdominal separation occurs when the growing uterus causes the 2 long, parallel muscles of your stomach to separate from each other. These muscles run from your chest to your pelvis, just under the skin, down the middle of your belly.
Abdominal separation is partly due to the pressure of your growing baby, and partly due to the hormonal changes that take place during pregnancy. It usually starts in the second half of pregnancy.
Abdominal separation is more common in women who have had more than 1 child, are aged over 35 or who are having twins or triplets (or more). It can also occur in a small-statured woman who is having a larger-than-average baby.
It is sometimes known as ‘DRAM’ (diastasis of rectus abdominis muscle).
What are the signs and symptoms of abdominal separation?
If you have abdominal separation after the birth of your baby, you may be able to see a gap between the two bands of abdominal muscles. You can see this gap more clearly if you lie flat on your back and lift your head up.
You can see this gap more clearly if you lie flat on your back and lift your head up.
You might also notice a physical canoe-shaped bulge in the middle of your stomach, especially when your abdominal muscles are active.
Some women with abdominal separation also get lower back pain, as the separation prevents the stomach muscles from supporting the back.
How is abdominal separation diagnosed?
Your GP, midwife or physiotherapist can check how big your abdominal separation is by measuring it with their fingers or a measuring tape, or by doing an ultrasound.
Does abdominal separation go away by itself?
Abdominal separation usually goes away after the birth of the baby. That said, up to 1 in 3 women still report problems with abdominal separation 12 months after the birth.
How can abdominal separation be prevented during pregnancy?
Strengthening your core muscles before you get pregnant or in the early stages of pregnancy might help prevent abdominal separation.
It’s best to avoid putting excess strain on your abdominal muscles while pregnant. Avoid sit-ups or planks. Try to avoid constipation and if you have a cough, get it treated.
How is abdominal separation after the birth treated?
It’s important to stop the separation from getting worse. Try these tips:
- Avoid lifting anything heavier than your baby.
- Roll onto your side when getting out of bed or sitting up.
- Choose gentle exercises (rather than intense ones) that strengthen the deeper stomach muscles.
- Skip activities and movements that can make abdominal separation worse, such as sit-ups (crunches), oblique curls and some yoga poses (ask your GP, midwife or physiotherapist for advice).
You can also wear a supportive brace or compression underwear to help support your back and resolve the muscle separation.
There is a good chance that with time and care, the muscles will come back together. If that doesn’t work as well as you’d like, surgery after you’ve had your baby is an option.
Surgery often involves using stitches to repair the abdominal wall and reduce the gap between the muscles. This can improve quality of life and muscle strength, especially when separation is wider than 3cm.
Where to get help
If you notice anything unusual about your stomach muscles or experience any symptoms, see your GP, midwife or physiotherapist. You can find a physiotherapist near you using the healthdirect service finder.
You can also contact Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse.
Sources:
Royal Women’s Hospital (Abdominal muscle separation), Surgical Endoscopy (The general surgeon’s perspective of rectus diastasis), King Edward Memorial Hospital (Physiotherapy after childbirth), Pelvic Floor First (Re-thinking abdominal training in pregnant and postnatal women)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2020
Back To Top
Related pages
- Yoga and Pilates during pregnancy
- Looking after your body after having a baby
- Pelvic floor exercises
- Safe return to exercise after pregnancy
- Exercising during pregnancy
- Physiotherapy advice after pregnancy
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Diastasis of the abdominal muscles after childbirth in women in Moscow
Diastasis is a divergence to the side of the rectus abdominis muscles. At the same time, the white line of the abdomen becomes thinner and stretched - a connective tissue structure that connects the muscles that form the very desired "press cubes".
If its width is more than 20 mm, we are talking about the presence of rectus diastasis.
Diastasis itself is not a disease, but rather a physiological condition. This is not a hernia: there is no defect in the white line, so there is no risk of infringement of internal organs. At the same time, the expansion and thinning of the white line increases the potential risk of developing true hernias.
Causes of diastasis
Most often, diastasis appears in the third trimester of pregnancy. This is one of the manifestations of physiological changes in the connective tissue of a woman during this period under the influence of hormones - the anterior abdominal wall is stretched due to connective tissue structures (and primarily the white line) - otherwise the uterus with a growing child would simply not fit in the abdominal cavity. In this case, the center of gravity of the body shifts anteriorly, the bend of the spine increases, the pressure on the anterior abdominal wall increases. The second reason for the appearance and increase in diastasis is an increase in pressure in the abdominal cavity, including during certain physical exercises.
In the postpartum period, the distance between the muscles decreases, but this process takes about a year. A survey of 300 women conducted by our Norwegian colleagues showed that 6 weeks after birth, diastasis persists in 60% of women, and after 12 months - only in 33%. That is why we do not recommend considering the issue of surgical treatment of diastasis earlier than a year after childbirth.
Classification of diastasis
There are several classifications of diastasis. Back at 1990 Ranney proposed to define diastasis as small with a width of up to 3 cm, moderate - 3-5 cm and large - if the distance between the rectus muscles is 5 cm or more.
Today we most often use the classification of Reinpold et al. (2019), which is similar to the hernia classification of the European Society of Herniology. We also note the number of pregnancies, skin condition, clinical symptoms and a number of other parameters that help us to carefully describe the situation in each case and choose the best way to correct diastasis.
Symptoms of diastasis
Diastasis is often visible to the naked eye. For its clearer definition, we ask patients in the supine position to raise their heads and shoulders. At the same time, the rectus abdominis muscles contract and a protrusion becomes visible, or vice versa, a deepening along a line running from the sternum to the pubis. Palpation allows you to more accurately identify the presence and degree of diastasis.
Diastasis may also present with clinical symptoms. The loss of a strong “foothold” for the muscles of the anterior abdominal wall leads to a redistribution of the static load, which in turn can lead to pelvic and lumbar pain, and in some, fortunately rare, cases, dysfunction of the pelvic organs.
Diastasis Diagnosis
We routinely use ultrasound to accurately determine the presence, length and width of diastasis, white line defects and hernias. Ultrasound is included in the consultation and is performed by the surgeon, who determines the tactics of treatment. This approach, in our opinion, is optimal and allows you to obtain reliable additional information that affects the adoption of a tactical decision.
This approach, in our opinion, is optimal and allows you to obtain reliable additional information that affects the adoption of a tactical decision.
In some cases, usually with severe diastasis and the presence of a hernia, we perform computed tomography, which gives us an understanding of the state of the anterior abdominal wall and allows us to determine and model the optimal method of diastasis repair.
How can diastasis be treated?
As we said above, diastasis is not a disease, but rather a postpartum condition that leads to an aesthetic and functional defect of the anterior abdominal wall. Accordingly, we prefer to replace "treatment" with "correction".
A correctly selected set of exercises can often correct external manifestations. It must be remembered that not all exercises can be performed with diastasis. All types of exercises that can contribute to an increase in diastasis are prohibited - these are all basic exercises with weights (deadlift, squats), many exercises for the abdominal muscles - twisting, hanging leg raises, etc. The classic "bar" is also not recommended for patients with diastasis.
The classic "bar" is also not recommended for patients with diastasis.
What exercises do we recommend for diastasis? Anything that strengthens the “deep core muscles”: side plank, tummy tuck, cat, Kegel exercises.
They cannot reduce the width of the white line (we remember that this is not a muscle, but a connective tissue that cannot be "pumped up"), but they can often improve the appearance of the abdomen and the quality of life of its owner, as shown by a recent study by Thabet and Alshehri, although the level of evidence for this thesis is low. However, we recommend a training program for at least 6 months before considering diastasis surgery.
NB! This does not apply to situations where diastasis is combined with hernias - umbilical or white line. It is impossible to eliminate hernias with physical exercises, we immediately move on to the surgical treatment option (here, it is the treatment).
Surgical treatment of diastasis
Surgery for diastasis is a rather extensive topic: there are several options for operations: laparoscopic (at least three fundamentally different methods) and open (also at least three), with or without implants, various suture materials, etc. .d. We will devote a separate article to these features, and now we will only briefly dwell on the indications for surgical correction:
.d. We will devote a separate article to these features, and now we will only briefly dwell on the indications for surgical correction:
- Any diastasis associated with a hernia of the anterior abdominal wall or severe diastasis with a cosmetic defect and/or clinical symptoms
- Childbirth more than 12 months ago
- No effect after 6 months of training
- Not planning another pregnancy
If these four conditions are met, we can plan the surgical treatment of diastasis.
Prevention of diastasis
There are practically no evidence-based measures for the prevention of diastasis today. You can reduce pressure on the anterior abdominal wall by following these 5 principles:
- Don't slouch
- Before sitting or getting out of bed, roll onto your side to engage your lateral abdominal muscles when you get up
- Avoid heavy lifting during pregnancy, and if you have to, use proper lifting technique with a straight back
- A special supporting corset takes on part of the load, and in addition, physically pulls the rectus abdominis muscles together
- Don't forget about regular exercise during pregnancy to strengthen your core and pelvic floor muscles.

We will be happy to answer any questions on the topic of rectus diastasis by email [email protected] or +7(995)500-0324 (WhatsApp, Telegram).
what happens to the body after childbirth
A woman's body does not rejuvenate during pregnancy and after the birth of a child. We tell you what cardinal changes in the body lead to and what to do about it.
Pregnancy and childbirth are, without exaggeration, the most amazing stages in the life of every woman. Waiting for and meeting a new person can be both very easy and difficult. Everything is individual and often unpredictable. Being aware of what happens "after" will help to cope with possible difficulties, fears and excitement.
After childbirth, the body will not be the same, all women know about it. But, as a rule, most often they mean stretch marks, excess weight, a flabby stomach, severe hair loss during breastfeeding and the consequences after episiotomy (surgical dissection of the perineum and posterior wall of the vagina) during natural childbirth.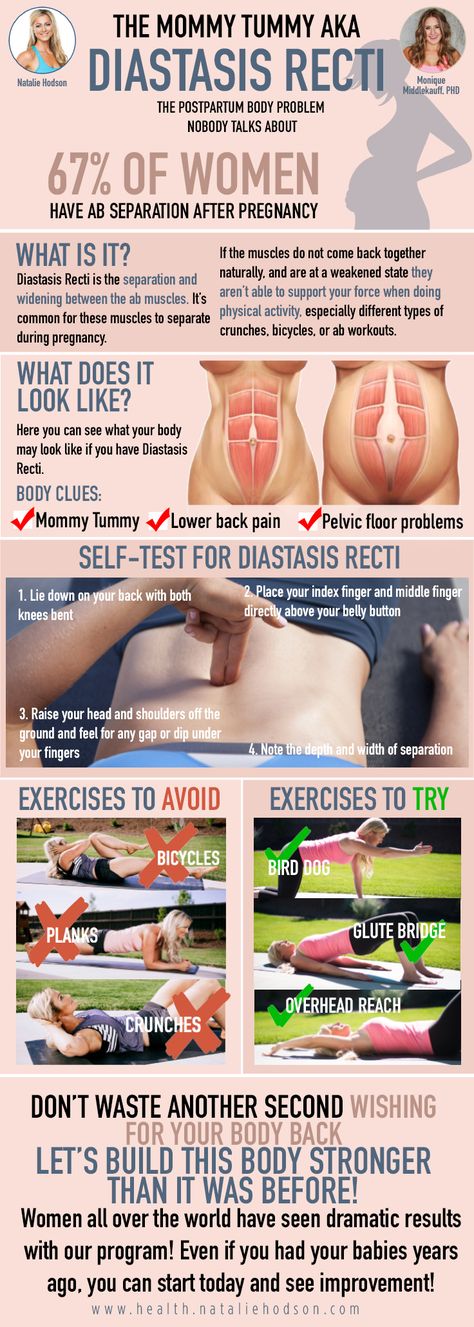 Less common are brittle teeth, an increase in the size of the foot, a change in the structure of the hair (wavy can become straight and vice versa), and a decrease in vision. Few people talk about urinary incontinence, umbilical hernia, severe dryness of intimate organs and pain in the chest.
Less common are brittle teeth, an increase in the size of the foot, a change in the structure of the hair (wavy can become straight and vice versa), and a decrease in vision. Few people talk about urinary incontinence, umbilical hernia, severe dryness of intimate organs and pain in the chest.
So that this does not become a cause for concern and one of the triggers for the development of postpartum depression, it makes sense to understand the physiology of pregnancy and study rehabilitation techniques.
Pregnancy is the strongest restructuring of the body and worldview.
Firstly, you should not worry, because pregnancy is the strongest restructuring of both the body and the worldview. And secondly, the notorious “get in shape after childbirth” is most often inappropriate in any of the situations. The main thing is to give yourself time and help the body recover calmly.
Why do some women recover easily and quickly after childbirth, while others face such serious problems as urinary incontinence, diastasis, hernias, posture disorders, varicose veins, hemorrhoids, dry mucous membranes and loss of vaginal sensitivity? All these consequences of pregnancy are associated with undifferentiated connective tissue dysplasia (CTD).
Candidate of Medical Sciences, obstetrician-gynecologist Inna Kondrashova says that DST is a genetic and autoimmune disorder of collagen synthesis. There are about 20 signs of CTD: tall stature and narrow shoulders, changes in posture and early signs of osteochondrosis, O- or X-shaped deformity of the lower extremities and flat feet, chronic migraines and frequent headaches, asthenia and a low hairline on the forehead, vascular diseases and visual disturbances, a tendency to allergies, and clear, thin, dry skin.
If a woman has more than five signs, then most likely she has undifferentiated CTD, and it is important to take this into account when preparing for and managing pregnancy. Timely diagnosis will help to avoid complications. It is important to start prevention in time, for example, taking the right vitamins (it is especially important to normalize iron levels), a balanced diet (a sufficient amount of protein is needed for the synthesis of collagen and elastin), the use of prenatal and postnatal bandage, exercises to strengthen the muscular frame.
Organ prolapse and urinary incontinence
During pregnancy, the load on the pelvic organs and kidneys increases due to the constant growth of the fetus and the pressure of the enlarged uterus. That is why urination becomes more frequent. Going to the toilet every two hours is not a cause for concern.
Stretched pelvic floor muscles during pregnancy can lead to pelvic organ prolapse, symptoms of which may include urinary incontinence, leakage when coughing or sneezing, pain during intercourse, a feeling of something foreign in the vagina, and as if the bladder is not emptying completely. These features may be slightly more common in women who have given birth vaginally.
As a self-help exercise, pelvic floor exercises work well. Although most women do them incorrectly, straining the auxiliary muscles, abs or buttocks. The easiest way is to imagine that you are stopping the process of urination. Repeat this exercise for several minutes, tensing and then relaxing the muscles.
Elena Lyubimkina, obstetrician-gynecologist, ultrasound and integrative medicine doctor:
“During pregnancy, you need to be especially careful about yourself if a woman has diseases that result in constantly increased pressure inside the abdomen. Most often, these are chronic diseases of the digestive system with persistent constipation or the respiratory system, accompanied by a constant cough.
Obesity significantly increases the load on the pelvic floor muscles. Also, prolapse of the pelvic organs can occur in case of complicated childbirth: large fetus, rapid labor, episiotomy, use of obstetric forceps, vacuum.
Diastasis and umbilical hernia
Another common problem that is not so easy to diagnose. Immediately after childbirth, as a rule, a woman’s belly remains soft, like a pillow, about the size of the fourth or fifth month of pregnancy (although everything is individual). There may also be a protruding navel.
During pregnancy, the abdominal muscles and connective tissues stretch due to the expanding uterus. Diastasis is the separation of the rectus abdominis muscles. According to a 2015 study, 100% of women who gave birth have this pathology.
A month or two after childbirth, you can do a test: lie on your back, bending your knees, and lift your upper body, placing your fingers on your navel. If the fingers fall inward a little, into a line along the abdomen, then this is diastasis. The width of the dip up to two and a half centimeters is the norm. Moreover, there is no need to hurry with the exercises, because, as a rule, the muscles converge on their own after six months.
With diastasis, in no case should you pump the press! It is necessary to use the oblique muscles of the abdomen: do side and reverse planks, pull-ups on all fours - and not earlier than two months after childbirth and a mandatory consultation with a doctor. You can get rid of severe diastasis with the help of abdominoplasty, that is, surgically.
“Do breathing exercises, abdominal massage, Kegel exercises and glute bridge already in the postpartum ward. Be sure to wear a bandage and be careful when lifting heavy weights, no more than four to five kilograms for six to eight weeks. It is also important to maintain an adequate drinking regimen and balance the diet with fiber to prevent constipation,” recommends Elena Lyubimkina.
Stoop and pain in the chest
During pregnancy, the center of gravity shifts, a deflection occurs in the lumbar region, because of this, the spine in the chest area is rounded, that is, kyphosis is formed. In the last stages of pregnancy, it can pull the lower back, and after childbirth, pain in the spine in the chest area is possible. In addition, many women feed the baby at first, hunched over, bending over him. It is better to use a special pillow and lean back to relax as much as possible.
Daily exercise with an emphasis on the upper body, swimming and massage can significantly improve the condition.