Fussy newborn after eating
Baby Cries After Feeding: What Should I Do?
Medically reviewed by Karen Gill, M.D. — By Chaunie Brusie on October 3, 2018
My daughter, the “crier”
My second daughter was what my oldest fondly referred to as a “crier.” Or, in other words, she cried. A lot. The crying with my baby girl seemed to intensify after every single feeding and particularly at night.
It was those hellish hours between darkness and dawn when my husband and I would take turns walking around the house with her in our arms, praying and, mostly in my case, sobbing because we couldn’t console our baby.
I didn’t know it then in my sleep-deprived state, but my daughter’s crying after feedings wasn’t that uncommon. In combination with her frequent spitting up, it was pretty much a classic textbook case of colic.
Colic
Colic, in technical terms, simply means a “crying, fussy baby that doctors can’t figure out.”
OK, so that’s not really the definition, but in essence, that’s what it boils down to. The British Medical Journal (BMJ) lists one criterion for colic: A baby that cries for at least three hours a day, three or more days a week, and is under 3 months old. Check, check, and check.
There isn’t one single known cause of colic. Even the actual clinical incidence of colic, estimated by BMJ to be around 20 percent of all babies, can be tricky.
Acid reflux
One of those causes of crying after feeding and spitting up in babies is actually acid reflux. This condition is known as gastroesophageal reflux disease (GERD) if it also causes significant symptoms such as poor weight gain.
When my “crier” daughter was 5, she frequently complained of her stomach hurting and as a result, had to undergo a series of testing with a gastroenterologist, a doctor that specializes in the GI system.
At our first appointment, the very first question he asked me was if she had colic as a baby and if she spit up a lot, to both of which I practically shouted, “Yes! How did you know?!”
He explained that acid reflux or GERD can manifest as symptoms similar to colic in babies, stomach pain in school-aged children, and later as actual heartburn pain in adolescents.
While many infants spit up, fewer have actual GERD, which can be caused by an underdeveloped flap between the esophagus and stomach or a higher-than-normal production of stomach acid.
In most cases, a diagnosis of infant reflux is simply based on your baby’s symptoms. If your doctor suspects a severe case however, there are several different tests that actually diagnose infant reflux.
Testing can involve taking a biopsy of your baby’s intestine or using a special type of X-ray to visualize any affected areas of obstruction.
Food sensitivities and allergies
Some babies, especially breastfed babies, may be allergic to certain food particles that their mothers are eating.
The Academy of Breastfeeding Medicine notes that the most common offender is cow’s milk protein in the mother’s milk, but even a true allergy is very rare. Only about 0.5 to 1 percent of exclusively breastfed babies are thought to be allergic to cow’s milk protein.
The other most common culprits, according to the ABM, are egg, corn, and soy, in that order.
If your baby is displaying symptoms of extreme irritability after feedings and has other symptoms, such as bloody stools (poop), you should speak with your healthcare provider about getting them tested for allergies.
Aside from a true allergy, there’s also been some evidence that following a low allergen diet while breastfeeding (essentially avoiding those top allergy foods, such as dairy, eggs, and corn) may be beneficial for infants with colic.
Strict elimination diets can have their own risks, so speak with your doctor before significantly changing your diet.
In our situation, I found that dairy, caffeine, and certain seeded fruit exacerbated my daughter’s crying and spitting up. By eliminating those foods and substances from my diet, I was able to help lessen her discomfort.
If you have a baby with colic, you might want to try anything at all to help ease your baby’s crying. If you’re curious to see if your diet has any effect, you can start by logging your food in a food journal and writing down your baby’s reactions after each meal.
Next, you can eliminate one food at a time and see if reducing your intake of certain foods seems to make a difference in your baby’s behavior. If you hit on one you feel helps your baby to cry less, this does not mean they will not be able to eat that food in the future.
Just be sure to keep in mind that a true allergy is rare. Also, be sure to monitor for any additional symptoms, such as blood in your baby’s poop.
Gas
If your baby is crying a lot after every feeding, it may simply be a buildup of air swallowed while eating. It’s thought that bottle-fed babes in particular may be more prone to swallowing a lot of air during a feeding. This can trap gas in their stomachs and be uncomfortable.
In general, breastfed babies swallow less air while eating simply due to the way they eat. But every baby is different and even breastfed babies may need to be burped after a feeding.
Trying keeping your baby upright after a feeding and burping gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out. Also check out this illustrated guide to burping a sleeping baby.
Also check out this illustrated guide to burping a sleeping baby.
Formula
If your baby is formula-fed, swapping out the formula you use may be a simple solution to a crying baby after feedings. Every formula is a little bit different and certain brands make formulas for more sensitive baby tummies.
If you decide to try this, talk to your baby’s pediatrician about whether an elemental formula would be a good choice to try for a week. If you try one different brand and you see no change in your baby’s fussiness, continuing to try different brands is unlikely to help.
Takeaway
Colic, along with a few other common conditions, might be the culprit if you too have a “crier” on your hands.
If your baby doesn’t find relief after dietary changes or additional burping, then make an appointment to see their doctor.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on October 3, 2018
- Parenthood
- Baby
- 06 Months
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ABM clinical protocol #24: Allergic proctocolitis in the exclusively breastfed infant. (2011). DOI:
10.1089/bfm.2011.9977 - Harrel MC, et al. (2015). Is there a correlation between maternal diet in breastfeeding mothers and infantile colic? DOI:
10.1097/01.EBP.0000541032.94135.ca - Mayo Clinic Staff. (2018). Infant reflux.
mayoclinic. org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412
org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412 - Rosen LD, et al. (2007). Complementary, holistic, and integrative medicine.
pedsinreview.aappublications.org/content/28/10/381 - Saavedra MA, et al. (2003). Infantile colic incidence and associated risk factors: A cohort study. .
ncbi.nlm.nih.gov/pubmed/14502331 - Sung V, et al. (2014). Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. DOI:
10.1136/bmj.g2107 - Symptoms & causes of GER and GERD in infants. (2015).
niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-infants/symptoms-causes
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Baby Cries After Feeding: What Should I Do?
Medically reviewed by Karen Gill, M. D. — By Chaunie Brusie on October 3, 2018
D. — By Chaunie Brusie on October 3, 2018
My daughter, the “crier”
My second daughter was what my oldest fondly referred to as a “crier.” Or, in other words, she cried. A lot. The crying with my baby girl seemed to intensify after every single feeding and particularly at night.
It was those hellish hours between darkness and dawn when my husband and I would take turns walking around the house with her in our arms, praying and, mostly in my case, sobbing because we couldn’t console our baby.
I didn’t know it then in my sleep-deprived state, but my daughter’s crying after feedings wasn’t that uncommon. In combination with her frequent spitting up, it was pretty much a classic textbook case of colic.
Colic
Colic, in technical terms, simply means a “crying, fussy baby that doctors can’t figure out.”
OK, so that’s not really the definition, but in essence, that’s what it boils down to. The British Medical Journal (BMJ) lists one criterion for colic: A baby that cries for at least three hours a day, three or more days a week, and is under 3 months old. Check, check, and check.
Check, check, and check.
There isn’t one single known cause of colic. Even the actual clinical incidence of colic, estimated by BMJ to be around 20 percent of all babies, can be tricky.
Acid reflux
One of those causes of crying after feeding and spitting up in babies is actually acid reflux. This condition is known as gastroesophageal reflux disease (GERD) if it also causes significant symptoms such as poor weight gain.
When my “crier” daughter was 5, she frequently complained of her stomach hurting and as a result, had to undergo a series of testing with a gastroenterologist, a doctor that specializes in the GI system.
At our first appointment, the very first question he asked me was if she had colic as a baby and if she spit up a lot, to both of which I practically shouted, “Yes! How did you know?!”
He explained that acid reflux or GERD can manifest as symptoms similar to colic in babies, stomach pain in school-aged children, and later as actual heartburn pain in adolescents.
While many infants spit up, fewer have actual GERD, which can be caused by an underdeveloped flap between the esophagus and stomach or a higher-than-normal production of stomach acid.
In most cases, a diagnosis of infant reflux is simply based on your baby’s symptoms. If your doctor suspects a severe case however, there are several different tests that actually diagnose infant reflux.
Testing can involve taking a biopsy of your baby’s intestine or using a special type of X-ray to visualize any affected areas of obstruction.
Food sensitivities and allergies
Some babies, especially breastfed babies, may be allergic to certain food particles that their mothers are eating.
The Academy of Breastfeeding Medicine notes that the most common offender is cow’s milk protein in the mother’s milk, but even a true allergy is very rare. Only about 0.5 to 1 percent of exclusively breastfed babies are thought to be allergic to cow’s milk protein.
The other most common culprits, according to the ABM, are egg, corn, and soy, in that order.
If your baby is displaying symptoms of extreme irritability after feedings and has other symptoms, such as bloody stools (poop), you should speak with your healthcare provider about getting them tested for allergies.
Aside from a true allergy, there’s also been some evidence that following a low allergen diet while breastfeeding (essentially avoiding those top allergy foods, such as dairy, eggs, and corn) may be beneficial for infants with colic.
Strict elimination diets can have their own risks, so speak with your doctor before significantly changing your diet.
In our situation, I found that dairy, caffeine, and certain seeded fruit exacerbated my daughter’s crying and spitting up. By eliminating those foods and substances from my diet, I was able to help lessen her discomfort.
If you have a baby with colic, you might want to try anything at all to help ease your baby’s crying. If you’re curious to see if your diet has any effect, you can start by logging your food in a food journal and writing down your baby’s reactions after each meal.
Next, you can eliminate one food at a time and see if reducing your intake of certain foods seems to make a difference in your baby’s behavior. If you hit on one you feel helps your baby to cry less, this does not mean they will not be able to eat that food in the future.
Just be sure to keep in mind that a true allergy is rare. Also, be sure to monitor for any additional symptoms, such as blood in your baby’s poop.
Gas
If your baby is crying a lot after every feeding, it may simply be a buildup of air swallowed while eating. It’s thought that bottle-fed babes in particular may be more prone to swallowing a lot of air during a feeding. This can trap gas in their stomachs and be uncomfortable.
In general, breastfed babies swallow less air while eating simply due to the way they eat. But every baby is different and even breastfed babies may need to be burped after a feeding.
Trying keeping your baby upright after a feeding and burping gently from the bottom of their back and up through the shoulders to work the gas bubbles up and out. Also check out this illustrated guide to burping a sleeping baby.
Also check out this illustrated guide to burping a sleeping baby.
Formula
If your baby is formula-fed, swapping out the formula you use may be a simple solution to a crying baby after feedings. Every formula is a little bit different and certain brands make formulas for more sensitive baby tummies.
If you decide to try this, talk to your baby’s pediatrician about whether an elemental formula would be a good choice to try for a week. If you try one different brand and you see no change in your baby’s fussiness, continuing to try different brands is unlikely to help.
Takeaway
Colic, along with a few other common conditions, might be the culprit if you too have a “crier” on your hands.
If your baby doesn’t find relief after dietary changes or additional burping, then make an appointment to see their doctor.
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on October 3, 2018
- Parenthood
- Baby
- 06 Months
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- ABM clinical protocol #24: Allergic proctocolitis in the exclusively breastfed infant. (2011). DOI:
10.1089/bfm.2011.9977 - Harrel MC, et al. (2015). Is there a correlation between maternal diet in breastfeeding mothers and infantile colic? DOI:
10.1097/01.EBP.0000541032.94135.ca - Mayo Clinic Staff. (2018). Infant reflux.
mayoclinic.org/diseases-conditions/infant-acid-reflux/diagnosis-treatment/drc-20351412
- Rosen LD, et al. (2007). Complementary, holistic, and integrative medicine.
pedsinreview.aappublications.org/content/28/10/381 - Saavedra MA, et al. (2003). Infantile colic incidence and associated risk factors: A cohort study. .
ncbi.nlm.nih.gov/pubmed/14502331 - Sung V, et al. (2014). Treating infant colic with the probiotic Lactobacillus reuteri: Double blind, placebo controlled randomised trial. DOI:
10.1136/bmj.g2107 - Symptoms & causes of GER and GERD in infants. (2015).
niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-infants/symptoms-causes
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Oct 3, 2018
By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Causes of hiccups in infants - GBUZ "Perinatal center of the city of Armavir" MH KK
The first year of a baby's life is a wonderful time full of love, tenderness and unexpected discoveries. But in this joyful period, alarming situations arise. For example, many parents are concerned about the fact that their baby often hiccups. Let's figure out why this happens and what to do.
But in this joyful period, alarming situations arise. For example, many parents are concerned about the fact that their baby often hiccups. Let's figure out why this happens and what to do.
Content
- Physiological phenomenon
- Overeating
- Extra air
- Flatulence
- Hypothermia and stress
- To drink or not?
- Warning signs
- Procedure
Physiological phenomenon
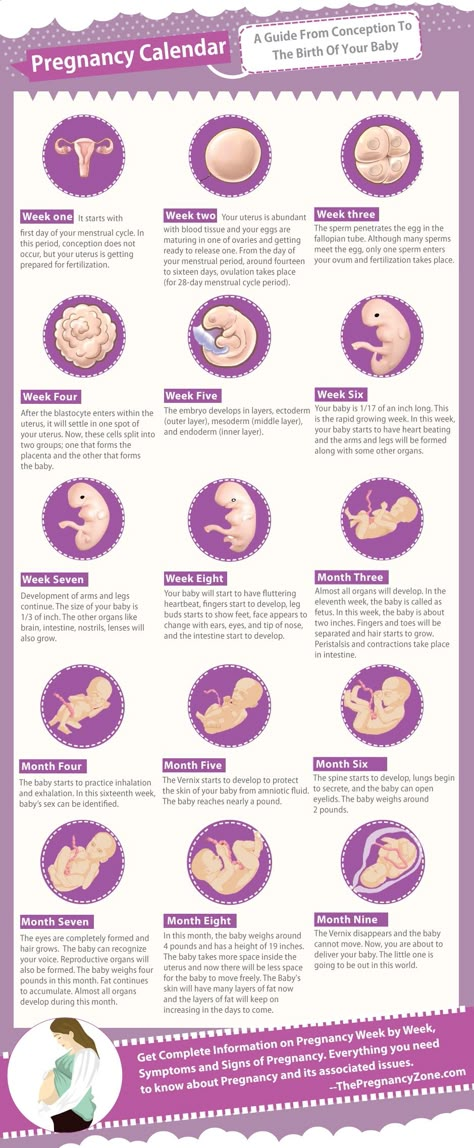
Hiccups are an absolutely normal phenomenon that accompanies a person throughout his life. Why does it arise? The mechanism is simple: under the influence of certain factors, the diaphragm contracts with a simultaneous sharp closure of the airways. A condition occurs that resembles short-term suffocation and is accompanied by a characteristic stifled sound. Such painless, but unpleasant convulsive tremors are repeated several times in a row.
Babies experience hiccups much more often than adults, because all their organs and systems are in the process of maturation. Normally, seizures can occur several times a day and last 10-30 minutes.
Normally, seizures can occur several times a day and last 10-30 minutes.
Why does the baby hiccup? The reasons are as follows:
- Feeding errors resulting in overeating, air swallowing (aerophagia) and flatulence
- hypothermia
- stress
Let's consider each factor in detail and find out what to do in order to help the baby.
Overeating
In infancy, hiccups often occur after meals: the stomach overflows with milk or formula, presses on the diaphragm, and it begins to contract. There is only one way to prevent this situation - to control the amount eaten by the crumbs.
When breastfeeding, pediatricians advise to keep intervals between meals at 1.5-2 hours and stop sucking if the baby eats for more than 15-20 minutes. With artificial nutrition, it is necessary to strictly observe the dosage of the mixture and the intervals between meals.
It is important not to go to the other extreme – to take too long breaks. In this case, the child will eagerly swallow milk during the long-awaited feeding and will definitely overeat. In addition, hunger and thirst can provoke hiccups as a result of reflex irritation of the walls of the stomach and diaphragm. In an infant older than 6 months who is already eating solid foods, cramps may be the result of eating too fast or eating dry foods.
In this case, the child will eagerly swallow milk during the long-awaited feeding and will definitely overeat. In addition, hunger and thirst can provoke hiccups as a result of reflex irritation of the walls of the stomach and diaphragm. In an infant older than 6 months who is already eating solid foods, cramps may be the result of eating too fast or eating dry foods.
Excess air
If the baby swallows a lot of air during sucking, then a bubble forms in the stomach, which gradually moves up and affects the respiratory muscles. For the prevention of aerophagia, it is recommended:
- Apply correctly to the chest. It is necessary that the child captures the entire areola of the nipple with his mouth. With abundant milk production, it can be expressed a little before feeding. The position of the crumbs during the meal should be almost vertical
- Choose your pacifier and bottle wisely. Swallowing air during formula feeding is possible if the nipple is made too wide a hole.
 Ideally, when the bottle is turned upside down, a few drops of milk per second should be released. During feeding, you need to hold it so that the nipple is constantly filled with liquid. It is advisable to use an anti-colic bottle
Ideally, when the bottle is turned upside down, a few drops of milk per second should be released. During feeding, you need to hold it so that the nipple is constantly filled with liquid. It is advisable to use an anti-colic bottle - After a meal, the child should be held upright for 5-10 minutes, pressing his tummy to your chest. Excess air bubbles will come out naturally. The same must be done with an attack of hiccups
Flatulence
Gases that accumulate in the upper intestines press on the stomach and displace the diaphragm. Prevention of flatulence in a baby is the diet of a nursing mother. Whole milk, corn, legumes, black bread, fresh pastries, carbonated drinks, fresh vegetables and fruits can cause increased gas formation. If the tummy swells after the mixture, then it should be changed after consulting with the pediatrician.
Flatulence is relieved by abdominal massage and herbal carminative preparations (with fennel, anise, dill, cumin) or simethicone.
Hypothermia and stress
Why does the baby still hiccup? Other reasons are related to the work of the nervous system. It's about hypothermia and stress. In these situations, there is irritation of the vagus nerve, passing from the thoracic region to the abdominal region, and spasm of the diaphragm.
The baby can freeze on a walk or in a cold room. It needs to be dressed warmer, covered with another blanket or picked up and warmed.
Sudden sounds, bright lights, strangers, sudden change of scenery, and so on can cause stress in a baby. What to do in this case? Remove the annoying factor, hug the child, stroke him, sing a song, attach to the chest. A grown-up baby can be occupied with an interesting game or a fairy tale.
Watch a short video about hiccups and how to deal with it. Do not forget to read the article to the end
To drink or not?
Drinking is an effective remedy for hiccups. But before 6 months, many breastfed babies receive only milk. It is believed that they do not need additional liquid. If the baby hiccups, then this rule can be broken and give him some warm water from a spoon. This is true if the attack occurred after feeding, because in this case, additional breastfeeding will only exacerbate the problem.
But before 6 months, many breastfed babies receive only milk. It is believed that they do not need additional liquid. If the baby hiccups, then this rule can be broken and give him some warm water from a spoon. This is true if the attack occurred after feeding, because in this case, additional breastfeeding will only exacerbate the problem.
Warning signs
Exhausting hiccups in an infant that does not subside for hours or days may indicate a pathology, especially if it is supplemented by:
- frequent and profuse regurgitation
- hyperthermia
- nervousness, fussiness
- crying
- persistent cough
Such symptoms should promptly seek medical attention. Why might they arise? There are a lot of serious diseases against which abnormal hiccups appear. Among them:
- infections that can provoke inflammation of the brain - measles, rubella, toxoplasmosis and others
- traumatic brain injury
- brain and lung tumors
- pneumonia
- gastroesophageal reflux
- neuritis - diaphragmatic affection etc.

Algorithm of actions
What should parents do if a baby hiccups? Do not panic and try to help him. Here are some tips:
- Hold baby upright after feeding
- Give him some warm water
- Breastfeed if the cause of the hiccups is not overeating
- Keep him warm in case of hypothermia
- Provide a calm environment, entertain with a game or book
- Seek medical attention if seizure persists for more than an hour and other signs of distress occur
Hiccups in a baby after a meal or as a result of fright is a physiological reflex. In the first months of life, the baby's body is actively developing, which is why it reacts so violently to external stimuli. With age, the frequency of seizures decreases markedly. Parents, on the other hand, should protect the peace of the baby, monitor his nutrition and respond in time to weather changes. The main thing during hiccups is not to create unnecessary fuss, because in fact, spasms of the diaphragm do not cause much discomfort to the child.
How to help the baby when regulating
Support Support iconKeywords for searching
Home Home ›!! How to help a child in spanning
Home ›!! how to help a child in regurgitation
↑ Verkh 9000 9000
Breastfeed - a very special time for a mother and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: Why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagy. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
- Holding a child upright on one's legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up while feeding.
 If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after. - When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.
Breastfeeding is a wonderful time to strengthen the bond between parent and baby. Every mom and every baby is different, so learning to help your newborn burp properly can take time and practice.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you.