Father with depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.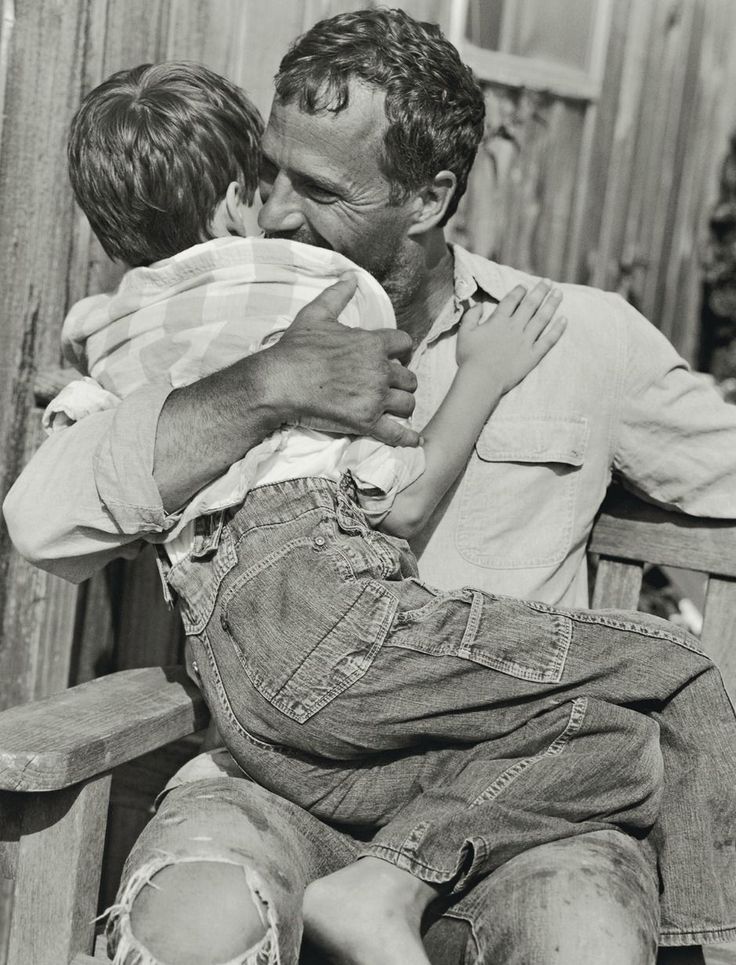 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
If a parent is depressed | GBUZ "CHOTSOZ MP"
(For mothers who believe that their dissatisfaction with life does not affect their children)
Normally a person is very adaptable. There are no conditions to which a person could not adapt if his psyche is not devoid of such a magical property as plasticity. Depression deprives this property. Even a small irritant, usually insignificant, takes on the scale of a trauma. For a child, the loss of plasticity may look like the fact that mom or dad became very angry at something that did not bother them before. The rules have changed, and the child must somehow learn to live in a new way. While he is trying to adapt to changes in the parental psyche, he no longer has time and energy for development.
The rules have changed, and the child must somehow learn to live in a new way. While he is trying to adapt to changes in the parental psyche, he no longer has time and energy for development.
“My mother used to have fun putting my toys away with me, but now she yells at me and demands that I put them away. Maybe give a slap. I'm afraid of her. I carefully monitor her mood, I'd rather play the same toy, although I really want to pull out the Lego and build a castle all over the room. But last time, my mother did not let me finish and kicked my parts with her feet. So I’d rather not build, I’ll drive a train, it can be quickly removed. ” So the kid sits and sluggishly rolls a train instead of an exciting construction, which, by the way, develops eye-hand coordination, dexterity and fine motor skills.
Depression causes feelings of incompetence. Parents, especially young ones, begin to believe that they don’t know anything, they don’t understand, they can’t, and they worry terribly because of this. Parents may feel that they cannot learn anything, that they are mediocre and stupid. In addition, depression deprives a person of the ability to respond emotionally to anything. Feelings become faded and dulled, and a person is deprived of the opportunity to empathize with others, including his child, share his sorrows and joys, and because of this, inevitably finds himself in a spiritual vacuum. This in itself adds suffering.
Parents may feel that they cannot learn anything, that they are mediocre and stupid. In addition, depression deprives a person of the ability to respond emotionally to anything. Feelings become faded and dulled, and a person is deprived of the opportunity to empathize with others, including his child, share his sorrows and joys, and because of this, inevitably finds himself in a spiritual vacuum. This in itself adds suffering.
Further, more. Man also suffers from his insensitivity. It is clear that in this state a person is focused on himself, natural egocentrism is practically his only property. He is immersed in his experiences, his sensitivity and vulnerability are exacerbated extremely. Any word of another person causes resentment and / or aggression, a depressed person remains “without skin”. And of course, there is no spiritual strength to see and hear what is happening with your own child. A depressed person is very acutely experiencing his uselessness, disunity with the world, rejection by everyone, including a child, even if it is a baby. What kind of adequacy is there ...
What kind of adequacy is there ...
The child does not receive an emotional response, the parent communicates with him formally, insufficiently and improperly cares, terribly tired, literally exhausted, from simple interaction with him. With a dead face, drooping, the mother is present at the game, or bathing, or feeding the child, while her thoughts are somewhere far away. The child has to solicit the attention of mom or dad by all available means. Babies cry, older children attract attention, mainly by bad behavior, illness and whims. Instead of developing, learning to walk, talk, eat with a spoon, etc., the child does his best to interest his depressed parent. All available forces and vital energy go to this. For a child, there is nothing worse than parental indifference. When parents are physically present, but they are not in communication, the child experiences severe anxiety, anxiety and, in turn, depression (in advanced cases). He began to speak, and then his mother fell ill with depression - and fell silent again, trying to return to the previous stage of development, when everything was still fine and his mother was with him.
The period of motherhood most vulnerable to depression is immediately after childbirth.
Whenever parents suffer from depression, the child feels rejected and abandoned. How harmful parental depression is to a child depends on the child's age. If maternal depression coincides with a developmental crisis, then this crisis will be worse. During periods of age crisis, behavior and ways of perceiving the real world change dramatically, a person must master new skills and really needs support, acceptance and understanding. And the mother herself needs help and is not able to provide it.
Can a father have postpartum depression?
Author: Claudia M. Elsig, MD
Having a baby is a life-changing event for all parents, and adjusting to parenting, whether it's the first or subsequent child, is an exciting and joyful time. But many of the challenges that come up in the early days of childcare can create additional stress in a relationship, and sometimes unexpected emotions can come up.
Postpartum depression is more common than you might think. When we talk about postpartum depression, we tend to focus on the woman. But studies show that about 1 in 10 men also go through a difficult psychological period in the early years of parenting. 1
Postpartum depression in men is usually not covered, so the figure is probably much higher. Men very often suffer in silence; some estimates say that every fourth man has postpartum depression! 3
There is a lot of research into the causes and consequences of postpartum depression in women 4 , but much less has been studied in men. This article explains the impact of having a baby on men's mental health.
What is depression after childbirth?
Many mothers experience depression for several weeks after giving birth. There is a significant decrease in the level of the hormones estradiol, progesterone and prolactin in the period after childbirth. 4 Bad mood and mild depressive symptoms are caused by these dramatic hormonal and chemical changes in the body.
Such mild depressive symptoms are commonly known as "postpartum depression". Symptoms usually develop on the second or third day after delivery, peak in the next few days, and then subside and disappear on their own within two weeks of onset. 4
Symptoms include sadness, crying, fatigue, irritability, anxiety, insomnia, inability to concentrate, hypersensitivity and mood swings.
What is postpartum depression and can men suffer from it?
Postpartum depression goes away on its own, has an immediate cause, and the symptoms are fairly mild. When mothers experience a longer and more severe depression, this is known as postpartum depression. Basically, it manifests itself in the form of constant depressive moods and feelings of depression. Fathers and partners may also suffer from this (a condition known as postpartum depression (PDP) or paternal depression).
Postpartum depression can result from several factors, and symptoms range from mild and relatively short-term to long-term and severe. In extreme cases, a person may feel "on edge" and unable to care for themselves or their child. At such times, a person may even experience psychotic episodes. Although postpartum psychosis in men is extremely rare, it is nevertheless possible. 5
In extreme cases, a person may feel "on edge" and unable to care for themselves or their child. At such times, a person may even experience psychotic episodes. Although postpartum psychosis in men is extremely rare, it is nevertheless possible. 5
Postpartum depression can start any time during the first year after the baby is born, but is most likely when the baby is 3 to 6 months old. PPD in men develops more slowly and gradually over the course of a year after the birth of a child, and this may be the reason why the problem does not receive sufficient coverage. 2
What causes postpartum depression in men?
There are many studies looking at postpartum depression (PPD) in women, but much less is known about the condition in men. The doctor's checklist and postpartum support tend to focus on the well-being of the mother.
Lack of sleep, new responsibilities and lack of “me time” can negatively affect the emotional and mental health of both new moms and dads.
The reasons why fathers or partners may experience depression after childbirth are often the same as for mothers. They include:
- Negative childbirth experience.
- Lack of sleep (circadian rhythm disorder).
- Excessive sense of responsibility.
- Difficulties in establishing communication with the child.
- Significant changes in daily routine and lifestyle.
- Stress in relationships.
- Financial pressure.
- Recovery of childhood trauma.
In addition, there are other reasons that are unique to men. A man is more likely to experience depressive feelings if his partner has postpartum depression. Studies show that about 50% of men whose partners are diagnosed with postpartum depression experience depression themselves. 6
Research also highlights a history of depression, family conflicts, and unintended pregnancy as other possible causes of postpartum depression in men.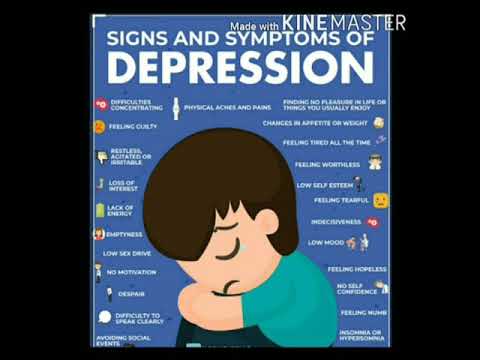 7
7
Surprisingly, not only women are subject to hormonal changes after childbirth. Kim and Swain argue that a father can experience hormonal changes during his wife's pregnancy and for several months after the baby is born. 2
Studies show that new fathers have increased levels of the hormones estrogen, oxytocin, prolactin and glucocorticoids. 8
What are the risk factors for postpartum depression in men?
There are many risk factors that can make paternal postpartum depression more likely. Lack of social support, difficulty adjusting to lifestyle changes, changes in marital/partner relationships, and feelings of exclusion due to mother-child bonding can all act as triggers for depressive episodes.
Men in high positions in business may feel unfit to be the new father.
Traumatic experiences during childbirth can also cause anxiety and mental health problems in men. In some cases, this leads to post-traumatic stress disorder (PTSD). A man may experience despair if the birth does not go according to plan. Even in situations of conventional birth, the sight of a partner in pain can make him feel helpless, especially when the man can't "fix" anything.
A man may experience despair if the birth does not go according to plan. Even in situations of conventional birth, the sight of a partner in pain can make him feel helpless, especially when the man can't "fix" anything.
A high association of paternal postpartum depression with other psychiatric disorders, such as anxiety and obsessive-compulsive disorder (OCD), has also been found. have anxiety problems. 9
What are the symptoms of postpartum depression in men?
Many of the symptoms of postpartum depression in men are similar to those of other forms of depression. Usually, they include:
- Fear, confusion and feelings of helplessness and uncertainty about the future.
- distraction from family life, work and social responsibilities
- Feelings of sadness, loneliness and hopelessness.
- Feeling guilty about not feeling happy.
- Decisiveness.

- Apathy.
- Despair, irritability and anger.
- Family conflicts.
- Partner violence.
- Negative attitude towards parental responsibilities.
- Alcohol and drug use.
- Insomnia.
- Physical symptoms such as indigestion, changes in appetite and weight, diarrhea, constipation, headaches and nausea.
How father's depression affects the child
As with mothers, depression in fathers can have a significant impact on the child (or children). A growing body of evidence suggests that father's depression is a major risk factor for difficulties in a child's life. A depressed parent is less empathetic towards their child and may exhibit inappropriate parental behavior in the form of neglect or over-responsibility.
Parenting can fluctuate between two extremes, from neglect followed by feelings of guilt where the parent may be overly engrossed in parenting. There is no sensitivity to the signals of the child.
There is no sensitivity to the signals of the child.
A study of 22,000 children from intact families found that father's depression increased the child's risk of emotional problems. 10
What are the treatments for postpartum depression in fathers?
When it comes to postpartum depression in men, it is more difficult for men to admit that there is a problem, and this can make treatment more difficult. A man's admission of postpartum depression can seem like a setback, and is taboo in many circles.
The good news is that postpartum depression can be cured. But this is an individual process for everyone. Psychotherapy is very effective, but each case must have its own approach.
At CALDA, we treat Dads with postpartum depression. Our highly individualized programs are based on comprehensive and detailed diagnostics. We conduct a detailed clinical and chemical analysis to determine the status of the disease. We treat the causes, not the symptoms.
Individualized treatment plans are developed by our team of experts, including therapists, world leading psychiatrists and nutritional experts.
We dedicate all our experience and time to each client individually. All clients are self-payers, which ensures the possibility of absolute secrecy. Clients stay in our luxury private residences overlooking Lake Zurich in a serene and sophisticated home environment. We provide a full range of premium services including butler, chef, chauffeur and limousine service.
We take care of everything so that you can recover quickly, return to your place in the family and enjoy fatherhood. If you have any questions, we will be happy to help you at any time. Just contact us.
Sources/Links
- National Childbirth Trust. Feb2018. Viewed 14 July 2022. Postnatal depression in dads: 10 things you should know.
- Kim P, Swain JE. Feb 2007. Sad dads: paternal postpartum depression. Psychiatry (Edgmont).;4(2):35-47.

- O'Hara, Michael & Swain, Annette. 2009. Rates and Risk of Postpartum Depression-a Meta-Analysis. International Review of Psychiatry. 8. 37-54.
- Balaram K, Marwaha R. Jan 2022. Postpartum Blues. [Updated Mar 9, 2022]
- Shahani L. 8 May 2012. A father with postpartum psychosis. BMJ Case Rep: bcr1120115176.
- Carberg, J (Medically fact checked by Langdon, K). Postpartum Depression Statistics. Postpartumdepression.org
- Scarff JR. May 1, 2019. Postpartum Depression in Men. Innovations in Clinical Neuroscience; 16(5-6):11-14.
- Gholipour, B. 14 Jun 2014. 5 Ways Fatherhood Changes a Man’s Brain. Website: livescience.com [accessed 16 July 2022]
- Matthey S, Barnett B, Howie P, Kavanagh DJ. Apr 2003. Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety? J Affect Discord. 74(2):139-47.
- Weitzman, M. Rosenthal, D.G. Ying-Hua, L. Dec 2011. Paternal Depressive Symptoms and Child Behavioral or Emotional Problems in the United States.