Extreme nausea and vomiting during pregnancy
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 16 to 20, although for some women it can last longer.
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- being dehydrated. Symptoms of dehydration include, feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
- low blood pressure (hypotension) when standing
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
Getting help early can help you avoid dehydration and weight loss.
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See the healthtalk.org website for videos and written interviews of women talking about their experiences of hyperemesis gravidarum and how they coped.
What causes hyperemesis gravidarum?
It's not known what causes HG, or why some women get it and others do not. Some experts believe it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, vitamins (B6 and B12) and steroids, or combinations of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given via a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
Other symptoms you may experience
Pregnancy Sickness Support is in touch with many women who have had HG, and who report having some or all of the following symptoms in addition to the main symptoms listed above:
- extremely heightened sense of smell
- excessive saliva production
- headaches and constipation from dehydration
If you experience these symptoms, you are not alone. Many women have them and they will go away when the HG stops or the baby is born.
Many women have them and they will go away when the HG stops or the baby is born.
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself. Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Severe Morning Sickness (Hyperemesis Gravidarum) (for Parents)
What's Morning Sickness?
During the first trimester of pregnancy, many women have the bouts of nausea and vomiting known as morning sickness.
Despite its name, morning sickness can happen day or night. It usually starts around the 6th week of pregnancy, is at its worst around week 9, and stops by weeks 16 to 18. Although unpleasant, morning sickness is considered a normal part of a healthy pregnancy.
What’s Severe Morning Sickness?
Severe morning sickness is when nausea and vomiting get so serious that a pregnant woman vomits several times a day, loses weight, and gets dehydrated or is at risk for dehydration.
If this rare pregnancy-related condition isn’t treated, it can affect a woman's health and her baby's ability to thrive.
The medical term for severe morning sickness is "hyperemesis gravidarum" (hi-per-EM-eh-sis grav-ih-DARE-um), which means "excessive vomiting during pregnancy." It usually follows a similar timeline to normal morning sickness. But it can go longer, sometimes lasting for the whole pregnancy. Often, the symptoms get less severe as the pregnancy continues.
Most cases of hyperemesis gravidarum affect a woman's first pregnancy. But women who have it in one pregnancy are more likely to have it in future pregnancies.
What Causes Severe Morning Sickness?
The cause of severe morning sickness isn’t known. But it might be related to the hormone changes of pregnancy. A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
Severe morning sickness also might run in families. It’s more common in women whose close family members (such as mothers and sisters) have had it.
Other things that can increase a woman's chances of having severe morning sickness include:
- carrying multiples (twins, triplets, etc.)
- history of motion sickness
- migraine headaches with nausea or vomiting
What Problems Can Happen?
The nausea and vomiting that happen in severe morning sickness are so extreme that they can harm the mother and the baby. Not being able to keep down food makes it hard for the mom to meet her nutritional needs. So she might lose weight. And a loss of fluids, combined with the loss of stomach acid from vomiting, can cause dehydration and electrolyte imbalances.
If severe morning sickness isn’t treated, it can cause many problems, including organ failure and the early birth of her baby.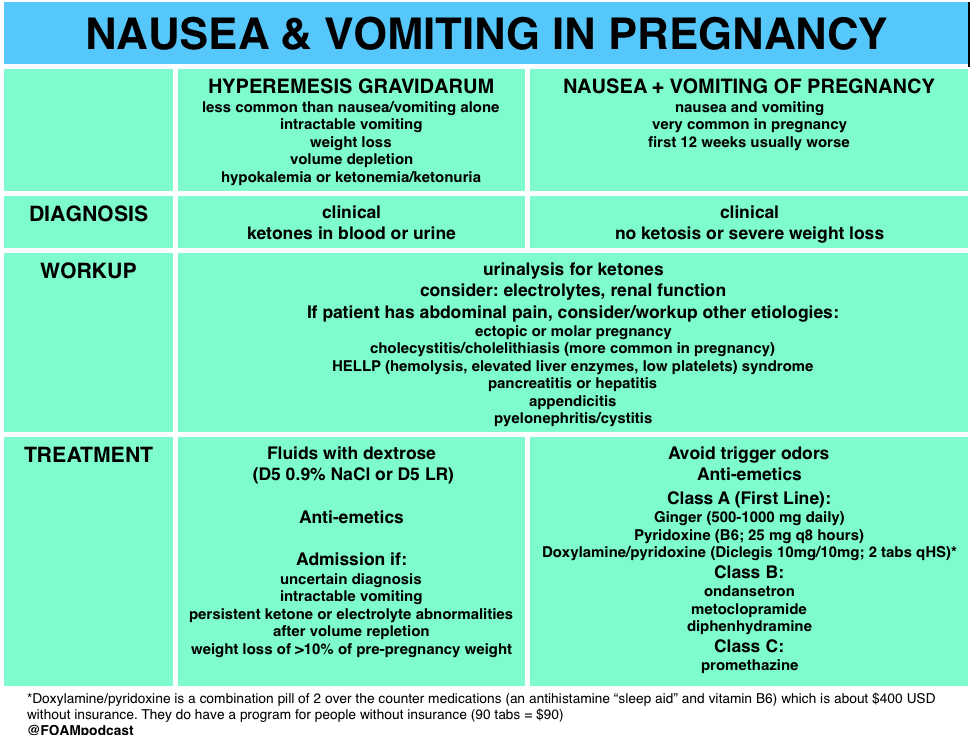
When Should I Call the Doctor?
Call the doctor right away if you’re pregnant and have any of these symptoms:
- nausea that lasts throughout the day, making it impossible to eat or drink
- vomiting three to four times per day or not being to keep anything in the stomach
- brownish vomit or vomit with blood or streaks of blood in it
- weight loss
- fainting or dizziness
- peeing less than usual
- a fast heart rate
- a lot of headaches
- unpleasant, fruity mouth or body odor
- extreme tiredness
- confusion
How Is Severe Morning Sickness Treated?
Treatments used for morning sickness, such as eating dry crackers in the morning or a bland diet, may be recommended for women with extreme morning sickness. But these might not help with severe symptoms.
Medical treatment can include:
- a short period of not eating to rest the gastrointestinal system
- intravenous (IV) fluids
- vitamin and nutritional supplements
Some women might get medicine to stop the vomiting, either by mouth or through an IV. The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
- Eat a bland diet.
- Eat frequent small meals.
- Drink plenty of liquids when not feeling nauseated.
- Avoid spicy and fatty foods.
- Eat high-protein snacks.
- Avoid sensory stimuli that can act as triggers (like specific smells or noises).
If a woman feels anxious or depressed about her condition, talking to a therapist or counselor might help her cope with her feelings.
What Else Should I Know?
With treatment, women with severe morning sickness can feel better and get the nourishment they need so they and their babies thrive. And lifestyle changes can help ease nausea and vomiting and make the pregnancy more enjoyable.
With time, symptoms usually do improve. And, of course, they stop by the time a woman's next journey starts: parenthood.
Early toxemia of pregnancy - causes and treatment
- When does early toxemia begin during pregnancy
- Manifestation of early toxicosis
- Causes of early toxicosis
- Severity of toxicosis during pregnancy
- How to manage morning sickness and relieve symptoms
- Principles of treatment of early toxicosis
Most women, having barely learned about the onset of pregnancy, expect to feel unwell, bouts of nausea and even vomiting. Indeed, early toxicosis often becomes a constant companion of many expectant mothers in the early stages of pregnancy. Is there any way to alleviate these unpleasant symptoms?
Indeed, early toxicosis often becomes a constant companion of many expectant mothers in the early stages of pregnancy. Is there any way to alleviate these unpleasant symptoms?
Toxicosis (and doctors call this condition gestosis) is a syndrome that is defined as a violation of a woman's adaptation to pregnancy. According to the time of occurrence, early preeclampsia is distinguished, which will be discussed in this article, and late preeclampsia, which appears in the last 2-3 months of pregnancy and is manifested by edema, increased blood pressure and the appearance of protein in the urine.
When early morning sickness begins in pregnancy
Early morning sickness usually occurs in the first half of pregnancy. As a rule, after the end of the formation of the placenta, that is, at 12-13 weeks of pregnancy, the phenomena of toxicosis stop. During a normal pregnancy, adaptive changes in the function of almost all organs and systems occur in a woman's body, which are regulated by the nervous system with the participation of endocrine glands. Toxicosis also occurs due to the impossibility of the adaptive mechanisms of the body of the expectant mother to adequately meet the needs of the developing fetus.
Toxicosis also occurs due to the impossibility of the adaptive mechanisms of the body of the expectant mother to adequately meet the needs of the developing fetus.
Manifestation of early toxicosis
The most common manifestation of toxicosis is vomiting. Other forms of early toxicosis are very rare:
- pregnancy dermatosis is a group of skin diseases that occur during pregnancy and disappear after it. When it occurs in early pregnancy, dermatosis is caused by immune disorders in the body of a pregnant woman, and is also most often found in patients with diseases of the digestive and endocrine systems. The most common form of dermatoses of pregnancy is pruritus gravidarum, which can be on a small area of the skin or spread throughout the body, including the feet and palms.
- tetany (chorea) of pregnant women. This condition occurs when the function of the parathyroid glands decreases, as a result of which calcium metabolism in the body is disturbed.
 Clinically, the disease is manifested by muscle cramps, more often cramps occur in the fingers, sometimes in the muscles of the face.
Clinically, the disease is manifested by muscle cramps, more often cramps occur in the fingers, sometimes in the muscles of the face. - salivation - increased secretion of saliva, in connection with which there is a large loss of fluid (up to 1 liter per day). Salivation can be an independent manifestation of toxicosis or accompany vomiting of pregnant women. In the development of salivation, not only changes in the central nervous system are important, but also local disturbances in the salivary glands and their ducts under the influence of hormonal changes.
- Pregnancy bronchial asthma is an extremely rare form of preeclampsia.
- osteomalacia of pregnancy - softening of the bones due to a violation of the metabolism of calcium and phosphorus, while the bones of the pelvis and spine are more often affected
- neuropathy and psychopathy of pregnant women.
Causes of toxicosis in the early stages
There are many theories trying to explain the causes and mechanisms of early toxicosis: the most recognized are the so-called neuro-reflex and immunological.
According to the neuro-reflex concept , vomiting occurs as a result of a violation of the relationship between the cerebral cortex and subcortical structures. During pregnancy, the subcortical centers of the brain begin to work more intensively than usual, which are responsible for most protective reflexes, including breathing and cardiac activity. In the same areas of the subcortical structures are the vomiting and salivary centers, the nuclei of the olfactory system of the brain. Excitation processes also capture them. Therefore, nausea and vomiting may be preceded by such phenomena as deepening of breathing, increased heart rate, an increase in the amount of saliva, pallor due to vasospasm, and a change in smell.
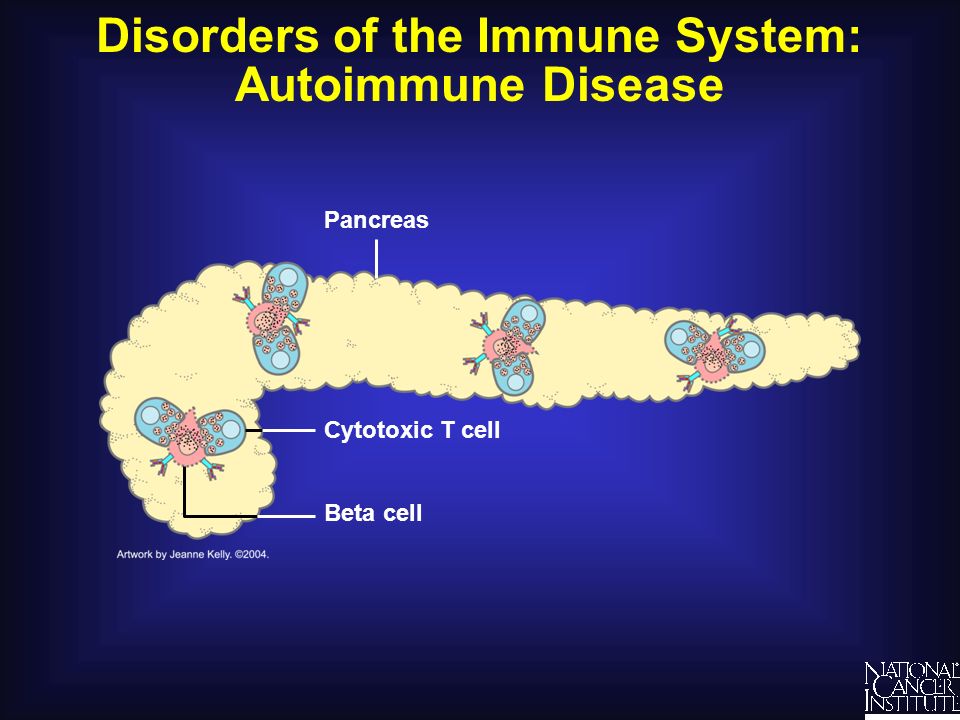
Immunological disorders play a certain role in the development of preeclampsia . The timing of the onset of vomiting usually coincides with the formation of blood circulation in the placenta, increased reproduction of white blood cells - lymphocytes, which are involved in immune reactions. The fetus is foreign to the mother's body, and her immune system reacts to it in this way. After the full maturation of the placenta, which accumulates all these immune cells, toxicosis usually disappears.
The fetus is foreign to the mother's body, and her immune system reacts to it in this way. After the full maturation of the placenta, which accumulates all these immune cells, toxicosis usually disappears.
Human chorionic gonadotropin (hCG) plays a certain role in the development of vomiting during pregnancy. This hormone is produced by the placenta during pregnancy. Its high concentration can provoke vomiting.
The severity of toxicosis during pregnancy
The main symptom of early toxicosis of pregnant women is vomiting. Depending on the frequency of its occurrence, as well as the degree of metabolic disorders in the body of the expectant mother, doctors distinguish three degrees of severity of vomiting during pregnancy.
How to manage morning sickness and relieve symptoms
Treatment for mild morning sickness is usually done at home. But, nevertheless, a pregnant woman should be under the supervision of doctors, take all the tests recommended by the doctor, and follow the appointments. This will allow the doctor to monitor the condition of the future mother's body and prevent possible complications in time. A woman needs to organize a normal sleep and rest regimen, walks in the fresh air, a calm atmosphere in the family are shown.
This will allow the doctor to monitor the condition of the future mother's body and prevent possible complications in time. A woman needs to organize a normal sleep and rest regimen, walks in the fresh air, a calm atmosphere in the family are shown.
Proper nutrition
You need to eat in small portions, fractionally, every 2-3 hours. Food should be easily digestible, high-calorie and fortified whenever possible. In connection with a decrease in appetite, they recommend varied and pleasant food for the expectant mother, that is, products are selected taking into account the desires of the pregnant woman, with the exception of spicy dishes and smoked meats. It is important to remember that very hot or very cold food often induces vomiting, so the dishes should be warm. Reception of alkaline mineral waters in small volumes 5-6 times a day is shown.
If nausea and vomiting occur in the morning, immediately after waking up, it is recommended to have breakfast while lying in bed without getting up. For breakfast, you can eat dry crackers, crackers, drink tea or water with lemon, light yogurt is allowed. It is better to put all this next to the bed in advance or ask someone to bring breakfast.
For breakfast, you can eat dry crackers, crackers, drink tea or water with lemon, light yogurt is allowed. It is better to put all this next to the bed in advance or ask someone to bring breakfast.
Every woman chooses for herself a remedy that helps to fight nausea. Someone helps a slice of orange, lemon or apple, some expectant mothers carry crackers or mint sweets with them to alleviate the symptoms of toxicosis. Pumpkin juice has a good antiemetic effect. Many pregnant women benefit from ginger tea. It is prepared very simply:
ginger root finely chopped or grated on a coarse grater is poured with boiling water and infused for 15-20 minutes. Tea can be drunk warm or chilled, adding lemon, mint or honey to it.
Fats and proteins of animal origin are recommended to be consumed in the morning, when pancreatic enzymes are more active. Dairy products are best eaten after dinner or before bed.
Do not use food with preservatives, broiler meat, fast food, fast food.
To maintain metabolic processes in the body, it is advisable to drink 2-2.5 liters of fluid per day. With increased vomiting, it is not recommended to consume solid and liquid food at the same time. Liquids should not be drunk 30 minutes before and within 1.5 hours after eating, as this provokes vomiting by stretching the walls of the stomach and affecting the receptors.
Decoctions and infusions
Oat broth
As an enveloping agent, that is, a substance that forms a mucous film and prevents irritation of receptors on the walls of the stomach and intestines, oat broth is recommended. It is prepared as follows: 2-3 tbsp. spoons of oat grains are washed, pour 500-700 ml of water, boil over low heat under a lid for 30 minutes. The broth is drained, the grains are crushed and poured with new water and boiled until fully cooked. The resulting mass is crushed with a blender. You need to use the decoction on an empty stomach and in the evening before going to bed, but not earlier than 2 hours after dinner, and also throughout the day in small portions.
It has a particularly good effect in combination with rosehip infusion.
Rosehip infusion
This infusion is a good source of vitamins and microelements - it contains vitamins C, K, P and PP, potassium, manganese, iron, and contributes to the normalization of the gallbladder function. To prepare it, you need 1 tbsp. pour a spoonful of crushed rose hips with 250 ml of boiling water and insist in a thermos for about 2 hours.
The following infusions and decoctions contribute to reducing nausea and improving the condition of the expectant mother.
Phytonast
Take equally: valerian root, common anise fruits, fireweed leaves, linden flowers, marigold flowers, common blueberry shoots, blood-red hawthorn fruits. 1 st. Pour 500 ml of boiling water over a spoonful of the mixture ground in a coffee grinder and insist in a thermos for 2 hours, then strain. Take the infusion as needed, up to 6 times a day in a heated form, 1/3 cup.
Benediktov's collection
To prepare this collection you will need: common yarrow (10 g), peppermint herb (20 g), shepherd's purse herb (20 g), valerian officinalis rhizomes (10 g), calendula officinalis inflorescences (20 g) and inflorescences of chamomile officinalis (20 g). Pour 10 g of the mixture with 400 ml of water, soak in a water bath for 30 minutes, strain. Take 50 ml 6 times a day for 25 days, three courses with 15-day breaks.
Pour 10 g of the mixture with 400 ml of water, soak in a water bath for 30 minutes, strain. Take 50 ml 6 times a day for 25 days, three courses with 15-day breaks.
Viburnum with honey
Grind 2 tbsp. tablespoons of fresh viburnum berries, pour 250 ml of boiling water over them, heat for 10 minutes in a water bath, strain, add a little honey. Take 1/3 cup of warm infusion before meals 3-4 times a day.
Cranberries with mint, honey and lemon
Squeeze the juice from 250 g of cranberries, cool it, boil the pulp in 1 liter of water, add 1 tbsp. a spoonful of mint leaves and leave for 15 minutes under the lid. Strain, dissolve in a hot broth 2-3 tbsp. tablespoons of honey, let cool to room temperature, add chilled cranberry juice and a slice of lemon. Drink 0.5 cup after meals or when nausea occurs.
Rose hips with apples
Crushed rose hips (about 1 tbsp) pour 250 ml of boiling water, add 0.5 tbsp. tablespoons of dried apples, heat in a water bath for 15-20 minutes. This drink can be consumed throughout the day instead of tea.
This drink can be consumed throughout the day instead of tea.
Rosehip with garden berries
To make a drink you will need: 1 tbsp. a spoonful of rose hips, 1 tbsp. spoon of raspberries, 1 tbsp. spoon of blackcurrant leaves, 1 tbsp. a spoonful of lingonberry leaves. 2 tbsp. spoons of the mixture pour 500 ml of boiling water, boil for 5 minutes, leave for 1 hour, strain. Take 100 ml of decoction 3 times a day.
Therapeutic exercise
Among non-drug treatments, exercise therapy has a good effect. The complex of exercises includes walking, deep breathing with stretching of the muscles of the trunk and limbs. It is necessary to exclude inclinations, they can increase nausea. The complex includes dynamic exercises for training the muscles of the arms, legs, relaxation exercises. Remedial gymnastics also includes training in breathing techniques. As a result, the body is saturated with oxygen, the excitability of the vomiting center decreases - toxicosis is relieved.
Physiotherapeutic procedures
Physiotherapeutic procedures for the treatment of early toxicosis include electrosleep, acupuncture, laser therapy . Electrosleep is a method that uses low frequency currents to induce sleep. The duration of the procedure is from 60 to 90 minutes, the course of treatment is 6-8 sessions.
Laser therapy
In the complex therapy of early toxicosis, blood is irradiated with a helium-neon laser through a light guide passed through a needle placed in the cubital vein. The procedure lasts 15-20 minutes. The therapeutic effect is achieved due to the influence of the laser on blood cells, changes in its properties, accumulation of biologically active substances in the blood. As a result, the metabolism in cells changes, the resistance of tissues and the body to adverse conditions increases, and the vitality increases.
Acupuncture, acupuncture
Treatment methods based on stimulation of biologically active points and zones on the body and face. With early toxicosis, such an effect changes the tone of the nervous system of a pregnant woman. A session of acupuncture is carried out 1-2 times a week and lasts 15-30 minutes.
With early toxicosis, such an effect changes the tone of the nervous system of a pregnant woman. A session of acupuncture is carried out 1-2 times a week and lasts 15-30 minutes.
Acupressure method is effective for morning sickness and vomiting of pregnant women. To do this, you need to press your finger on a point that is located on the inside of the wrist, in the middle, 3 transverse fingers above the palm.
Aromatherapy
The use of plant aromas has a positive effect on the expectant mother and baby. By inhaling pleasant aromas, you can achieve a good psychological effect, create a good mood, and reduce the effects of toxicosis. During pregnancy, aroma lamps, aroma medallions, pads - sachets are mainly used. To relieve nausea and vomiting, oils of noble laurel, lemon, lavender, cardamom present, dill, lemon balm, peppermint, anise, eucalyptus, ginger are suitable. To flavor the air, you can use the following mixture 0 3 drops of lavender oil, 1 drop of peppermint oil, 1 drop of eucalyptus oil.
Principles of treatment of early toxicosis
Even with a mild course of early toxicosis of pregnant women, the attending physician will definitely prescribe a number of tests - a general blood test, a general urinalysis, a biochemical blood test, a hemostasiogram. This is necessary to control the condition of a pregnant woman and to timely prescribe medications to correct the changes that occur in the body.
If non-drug remedies are ineffective, the doctor prescribes medications that help fight toxicosis. First of all, these are herbal sedatives, homeopathic medicines for nausea, vitamin B6 preparations, antiemetics.
If, despite all the therapy, vomiting increases, the doctor detects changes in blood and urine tests, and body weight continues to progressively decrease, hospitalization is indicated.
An intravenous infusion of medicines is carried out in the hospital, which restores the fluid, microelements and proteins lost by the body. A pregnant woman receives at least 2-2. 5 liters of fluid intravenously per day.
5 liters of fluid intravenously per day.
To improve blood flow through the placenta and improve oxygen supply to the fetus, oxygen therapy can be prescribed - inhalation of an oxygen-air mixture for 20-30 minutes twice a day.
Most often, the effects of toxicosis gradually decrease by 12-13 weeks of pregnancy.
Mild
Mild vomiting on an empty stomach or after meals occurs 3 to 5 times a day. Despite vomiting, part of the food is still retained and significant weight loss is not observed in such pregnant women. The general condition does not suffer significantly, there are no changes in blood and urine tests. Such vomiting is easily treatable with various non-drug means, and often resolves on its own after the normalization of the diet and rest.
Moderate vomiting
Moderate vomiting (or moderate vomiting) is expressed in the increase in vomiting up to 10 times a day, regardless of food intake. Characterized by persistent nausea. There comes dehydration of the body, a decrease in body weight by 3-5 kg (6% of the initial weight). The general condition of pregnant women worsens. Expectant mothers complain of weakness, apathy, tearfulness, sometimes depression. The skin is pale, dry, the tongue is covered with a white coating, yellowness of the skin may be noted.
The general condition of pregnant women worsens. Expectant mothers complain of weakness, apathy, tearfulness, sometimes depression. The skin is pale, dry, the tongue is covered with a white coating, yellowness of the skin may be noted.
Excessive vomiting
Severe (excessive pregnancy vomiting) is rare. The frequency of vomiting up to 20 times a day or more. Excessive vomiting is characterized by severe dehydration and intoxication. This condition can occur as a continuation of moderate vomiting of pregnant women or initially acquire a severe character. With excessive vomiting, body weight decreases rapidly, on average by 2-3 kg per week, the skin becomes dry and flabby, subcutaneous fat quickly disappears, the tongue and lips are dry, there is a smell of acetone from the mouth, body temperature can rise up to 38 degrees. Vomiting of moderate and severe degrees is treated in a hospital.
We fight against toxicosis - articles from the specialists of the clinic "Mother and Child"
Alexandrova Anna Evgenievna
Embryologist
Clinic "Mother and Child" South-West
rest more
Very often in the first trimester, the expectant mother feels weak, drowsy, she wants to lie down to rest, and sometimes she simply does not even have the strength to move. This, of course, is not toxicosis, but if such sensations arise, then they must be indulged so as not to inadvertently provoke another attack of nausea. Get plenty of rest and do not make any sudden movements, because even if you just fail to get up from a chair, you can provoke an attack of nausea.
This, of course, is not toxicosis, but if such sensations arise, then they must be indulged so as not to inadvertently provoke another attack of nausea. Get plenty of rest and do not make any sudden movements, because even if you just fail to get up from a chair, you can provoke an attack of nausea.
Sleep with the windows open: the air in the bedroom should be fresh and cool. Go to bed on time, do not sit at midnight in front of the TV or at the computer, eliminate all irritating factors: an uncomfortable mattress, blanket, pillow, hard bedding - lack of sleep can respond with morning sickness.
eat right
Eat small meals, 5-6 times a day, or more often. When you wake up, don't get out of bed right away. One of the most effective methods against toxicosis is breakfast in bed. In the evening, put crackers, yogurt, or any product that you can tolerate well next to your bed. Eat it before you get up, and then lie down for a while. Most likely, morning sickness will either not appear at all, or will be very weak.
Usually, in case of toxicosis, it is not recommended to eat fatty, smoked, salty, pickled, drink soda (the usual set of food hazards). But it is likely that some not very healthy product will now be well tolerated, and something from healthy food, on the contrary, will cause nausea. "Pregnant whims" - a cake with herring or pineapples at night - these are the requests of the body that it needs one or another component in food. For example, the desire to chew chalk is a sign of calcium deficiency. So eat what you like and what you want, within reason, of course. And if you don’t feel like something, even if this product is extremely useful and necessary, don’t eat it. If you feel sick from some dish, it means that the body signals you: I don’t need this now!
drink more often
Toxicosis may not be limited to nausea, some may also vomit. This means fluid is lost. Therefore, between meals, drink more often: a sip or two of mineral water or tea with lemon will help to cope with nausea and replenish lost fluids. But drink in small sips. Also, you should not drink food and you should give up soups for a while - a large amount of food drunk and eaten, on the contrary, only provokes nausea and vomiting.
But drink in small sips. Also, you should not drink food and you should give up soups for a while - a large amount of food drunk and eaten, on the contrary, only provokes nausea and vomiting.
breathe fresh air
Outdoor walks are good for everyone, but especially for toxicosis. Firstly, when walking, the blood of the expectant mother and baby is saturated with oxygen, which is very important for health, and secondly, walking calms the nervous system. Together, this helps to reduce the unpleasant symptoms of toxicosis. You need to walk at least two hours a day - but not just along the street, but in the place where the air is really fresh: in the forest, park, square, and best of all outside the city. Before you go out, think over the route: go away from gas-polluted highways, street cafes, food stalls and other "fragrant" places.
exclude fragrances
Taste and smell preferences change during the first trimester. Now even your favorite perfumes can cause nausea, headaches and allergic reactions. Therefore, put away all fragrant cosmetics that irritate you: perfumes, deodorants, creams, and so on. You will have to stop using your favorite perfume for both your husband and loved ones. Explain to others that this is not a whim, but a temporary measure, very soon everything will return to normal.
Therefore, put away all fragrant cosmetics that irritate you: perfumes, deodorants, creams, and so on. You will have to stop using your favorite perfume for both your husband and loved ones. Explain to others that this is not a whim, but a temporary measure, very soon everything will return to normal.
And do not worry that now you will be left without your usual beauty products. Both the cosmetic store and the pharmacy are full of different creams, tonics, shampoos without fragrance or with a minimal smell.
work with yourself
Psychologists believe that the cause of toxicosis is not only in hormonal changes, but also in the psychological state of a woman. The more a woman experiences, the more anxieties and fears she has, the more pronounced toxicosis can be. Ideally, it is better to limit yourself during pregnancy from any stress. Of course, it’s not always possible to eliminate nervous work or crowding in public transport, but watch less TV, don’t read negative news and various pregnant “horror stories” on the Internet, and don’t react to minor or even major everyday troubles everyone can do. Therefore, if you are worried about toxicosis, create your own comfortable world during pregnancy. If you can’t cope on your own, contact a specialist (psychologist). Toxicosis is really well treated with psychotherapy. The main thing is that the expectant mother should want to get rid of her own anxiety.
Therefore, if you are worried about toxicosis, create your own comfortable world during pregnancy. If you can’t cope on your own, contact a specialist (psychologist). Toxicosis is really well treated with psychotherapy. The main thing is that the expectant mother should want to get rid of her own anxiety.
No matter how unpleasant toxicosis is, it does not last forever. It is necessary to suffer until the beginning or (less often) the middle of the II trimester. And very soon all the unpleasant symptoms of toxicosis will remain in the past!
Make an appointment
to the doctor - Alexandrova Anna Evgenievna
Clinic "Mother and Child" South-West
IKSIECO
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic KG "Lapino" in Odintsovo (branch)Clinic "Mother and Child" Khodynskoye PoleClinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" Yugo-ZapadMother and Child Clinic NovogireyevoMother and Child Clinic Lefortovo
All directionsSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesTreatment roomTelemedicine for adultsTherapeutic studiesUltrasound examinations for adults
01.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg)