Exposure to measles while pregnant
Measles and pregnancy | Pregnancy Birth and Baby
Measles and pregnancy | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is measles?
Measles is a highly contagious viral illness that can cause serious complications for anyone who becomes infected. The broad uptake of measles vaccination through the Australian National Immunisation Program means that the disease is now quite rare in Australia.
However, outbreaks still occur, with overseas visitors and returning residents bringing the virus into Australia. For this reason, it is important to make sure that everyone in your family is protected.
What are the symptoms of measles?
The most well-recognised symptom of measles is the characteristic rash, which appears after a few days of general illness with fever. The rash develops with flat discoloured skin and small bumps but is not itchy. It usually starts on the face or upper neck and then spreads over the body.
Some early signs and symptoms of measles include:
- fever
- conjunctivitis (sore, red eyes)
- cold symptoms (runny nose, sneezing, feeling tired and generally unwell)
- cough
You might start to show symptoms about 10 to 12 days after exposure to the measles virus, and these symptoms can last for up to 14 days.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
What are the complications of measles?
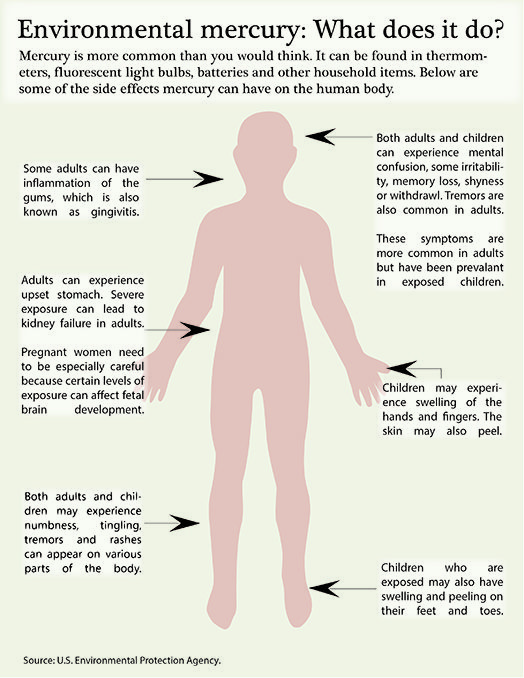
Common complications include middle ear infections and pneumonia. A rare but life-threatening complication of measles is inflammation of the brain.
Adults are at higher risk of developing complications.
If you are concerned, don’t hesitate to call your doctor. Measles can be a very serious illness, with some people needing to go to hospital.
Measles can be a very serious illness, with some people needing to go to hospital.
I’m pregnant — can measles affect my unborn baby?
A measles infection during pregnancy can cause miscarriage and premature birth. Having measles in pregnancy is not associated with an increased risk to your baby of birth defects.
If you are pregnant, you should not be vaccinated for measles until after you've had your baby.
Read more
Vaccinations and pregnancy
Some vaccinations are recommended before pregnancy, while others you can safely have during pregnancy.
How is measles spread?
Measles is one of the most contagious of all childhood illnesses. Being in the same room as an infected person is enough to spread the virus, and 9 out of 10 unvaccinated people who come into contact with an infected person will get measles.
A person who has the measles virus will be contagious from the day before they start to feel unwell until up to 4 days after the rash appears.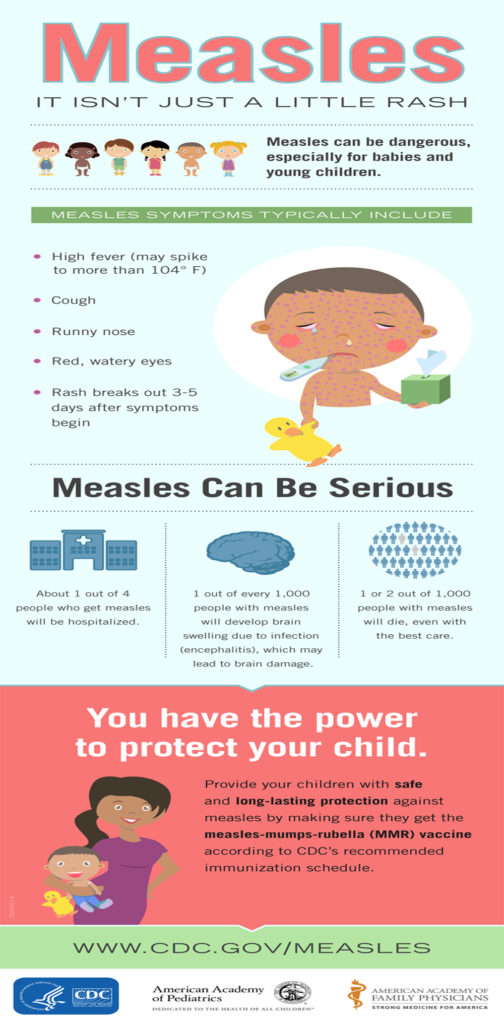
If you are pregnant and have been in contact with anyone with the measles virus you should call your doctor immediately. Do not go to the clinic since you don’t want to infect people in the waiting room. Staff will let you know the safest way to see the doctor. Be sure to tell them that you are pregnant.
It is also important to:
- stay away from others to prevent spread of the virus
- look out for any symptoms
- ask your doctor if family members need to be vaccinated
If your doctor thinks you may have measles, you may be asked to take a blood or urine test or for a sample from your nose or throat to check your immunity.
If you have measles, a public health unit staff member will interview you to try and find out where you caught measles and identify all your contacts to prevent further spread of the virus.
Make sure you let your doctor and the public health unit staff know if there is anyone in your home who may be at high-risk, for example people with an immune disease or on medications such chemotherapy. Other high risk groups include pregnant women who don’t know if they have been immunised and babies who haven’t yet had their vaccinations.
Other high risk groups include pregnant women who don’t know if they have been immunised and babies who haven’t yet had their vaccinations.
Is there any treatment for measles?
There is no specific treatment for measles. You should rest and drink plenty of fluids and you can also take paracetamol for fever — be sure to check the dosage instructions on the pack. It is important to note you may have to avoid other pain-relief medications during pregnancy. Contact your doctor or pharmacist before taking any medicine during pregnancy.
I’m planning a pregnancy — what can I do to avoid measles?
Any adult born during or after 1966 should make sure they have had 2 doses of the vaccine. Speak to your doctor if you are unsure. Vaccination before pregnancy is particularly important, but remember to use contraception to avoid pregnancy for at least 28 days after you get the vaccine. There is no risk to pregnant women from contact with people who have recently been vaccinated.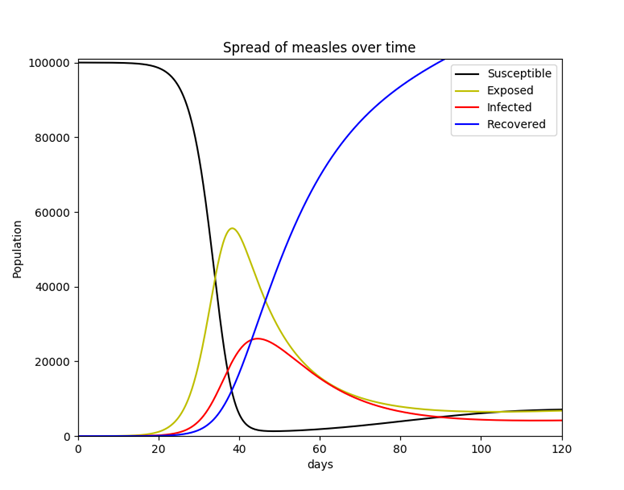
Measles in babies and children
Find out how babies and children can catch measles, how to treat your child at home, and when to have them vaccinated.
Sources:
NSW Health (Measles fact sheet), Communicable Diseases Network Australia (CDNA) (Measles), Department of Health (Measles), Australian Immunisation Handbook (Measles), NSW Government - Health (Measles: information for contacts)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Medicines during pregnancy
- Measles in babies and children
- Vaccinations and pregnancy
Need more information?
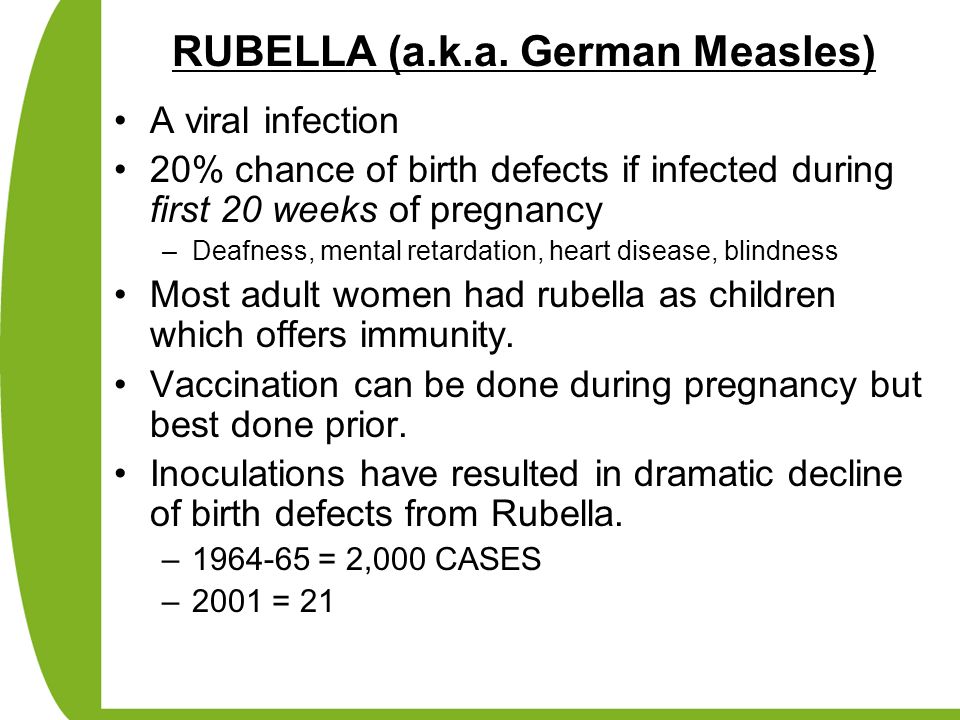
Rubella (German measles)
Rubella is a viral infection and is sometimes called German measles, although it is not related to measles itself.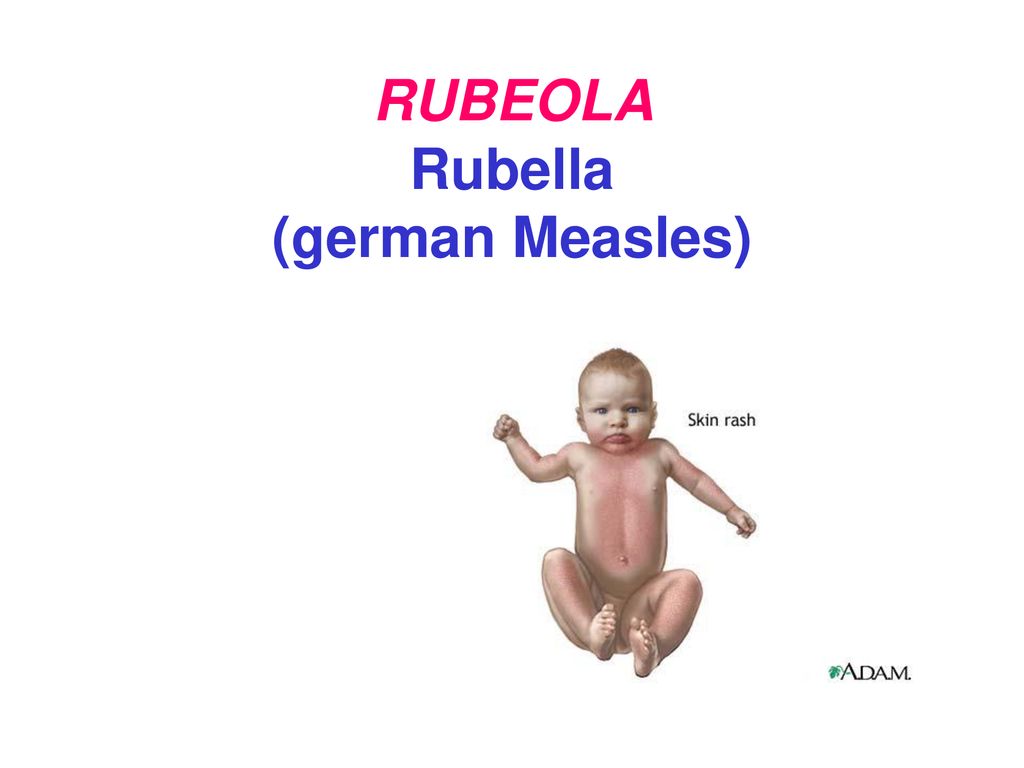 Most people with rubella experience a mild illness involving fever and rash. It is important as rubella illness during pregnancy may significantly affect the developing foetus.
Most people with rubella experience a mild illness involving fever and rash. It is important as rubella illness during pregnancy may significantly affect the developing foetus.
Read more on Queensland Health website
German measles (rubella)
German measles, also known as rubella, is a mild viral illness. It is a different disease to measles. Most people recover quickly from this infection.
Read more on WA Health website
Measles
Measles is an acute, highly infectious illness caused by the measles virus. Measles can cause serious complications such as pneumonia (lung infection) and encephalitis (inflammation of the brain). It may also cause middle ear infection.
Read more on Queensland Health website
Measles in babies and children
Find out about the symptoms of measles, how to help prevent your child catching the infection, and how to treat them at home if they get measles.
Read more on Pregnancy, Birth & Baby website
Measles, Mumps And Rubella (MMR) Vaccine | SA Health
Measles, mumps and rubella (MMR) vaccine recommendations, possible side effects and how to reduce the side effects
Read more on SA Health website
Measles - Better Health Channel
Measles can cause serious and sometimes fatal complications, including pneumonia and brain inflammation.
Read more on Better Health Channel website
Rubella or German measles in children | Raising Children Network
Rubella or German measles is a viral illness. Immunisation protects your child from rubella, but see your GP if you think your child has rubella symptoms.
Read more on raisingchildren.net.au website
Rubella in Australia
Rubella (also known German measles) is a viral disease. For most people, a rubella infection causes mild illness of fever, rash and swollen lymph glands.
Read more on AIHW – Australian Institute of Health and Welfare website
Rubella (German measles) | Australian Government Department of Health and Aged Care
Find out how we define and monitor cases of rubella, how you can get vaccinated, and where you can learn more about this disease.
Read more on Department of Health and Aged Care website
Rubella in babies and children
Find out more about the symptoms of rubella, when your child should see a doctor, how to care for a sick child at home, and how the disease spreads.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What women need to know about measles and pregnancy | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
July 2, 2019
Your Pregnancy Matters
Robyn Horsager-Boehrer, M.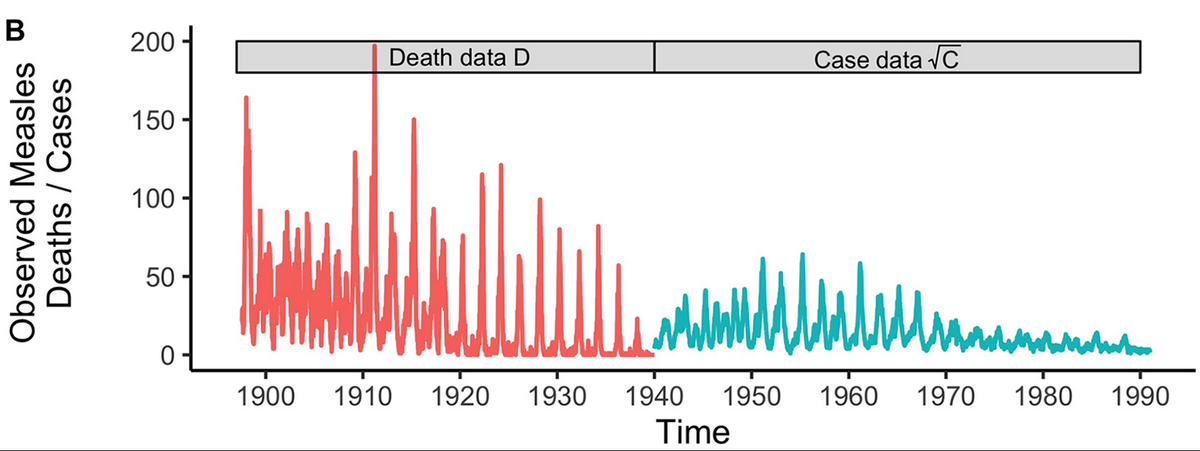 D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
In 2000, the government determined that measles had been eliminated in the U.S. But in 2019, we're seeing a resurgence of the disease that is putting pregnant women, babies, and other vulnerable populations across the country at risk.
As of June 13, 2019, more than 1,000 cases of measles have been confirmed in 28 states – up six states from the previous week. Texas has already had more cases in 2019 (15 confirmed to date) than in all of 2018 (nine total).
The rise in measles can be attributed to many factors, including:
- Travel between the U.S. and areas with high measles infection rates.
- Vaccine hesitancy – more than 90 percent of a community must be vaccinated to achieve "herd immunity," or protection for people who medically can't be vaccinated.
- Lack of education about vaccine boosters from providers to patients.
- The highly contagious nature of measles – it can stay in the air for two hours after an infected person leaves an area, and the virus is easily spread through breathing, talking, sneezing, or coughing. Infection requires very little exposure to the virus.
Nine out of 10 people who haven’t had the measles before or haven’t been vaccinated will come down with the illness when exposed. Even those who have been vaccinated can get measles, though symptoms might be less severe.
While measles in pregnant women has not been shown to cause birth defects in the developing fetus, research suggests that exposure to the virus can increase the risk of miscarriage and preterm birth. However, the measles vaccine is given as part of the measles, mumps, and rubella (MMR) vaccination and cannot be given during pregnancy.
The recent increase in confirmed cases of measles has led the American Congress of Obstetricians and Gynecologists (ACOG) and researchers from the University of Washington to update measles prevention guidelines for pregnant and reproductive-aged women at high risk of infection.
| Measles cases reported by year | U.S. | Primary outbreak state |
|---|---|---|
| 2014 | 667 | 338 cases in Ohio |
| 2015 | 188 | 147, California |
| 2016 | 86 | (no outbreaks) |
| 2017 | 120 | 75, Minnesota |
| 2018 | 372 | 82, New York |
| 2019 (as of June 27) | 1,095 | 275, New York |
| Source: CDC |

Women's health updates for measles risk
The revised guidelines include three main considerations for women:
If you are considering pregnancy, this is the perfect time to check your immunization record.
- If you are at average risk and have received one dose of the measles, mumps, and rubella (MMR) vaccine, you've done all you can to protect yourself.
- If you are at high risk, you should have two MMR vaccinations. The University of Washington is recommending this approach for certain individuals, including healthcare workers, college students, and international travelers.
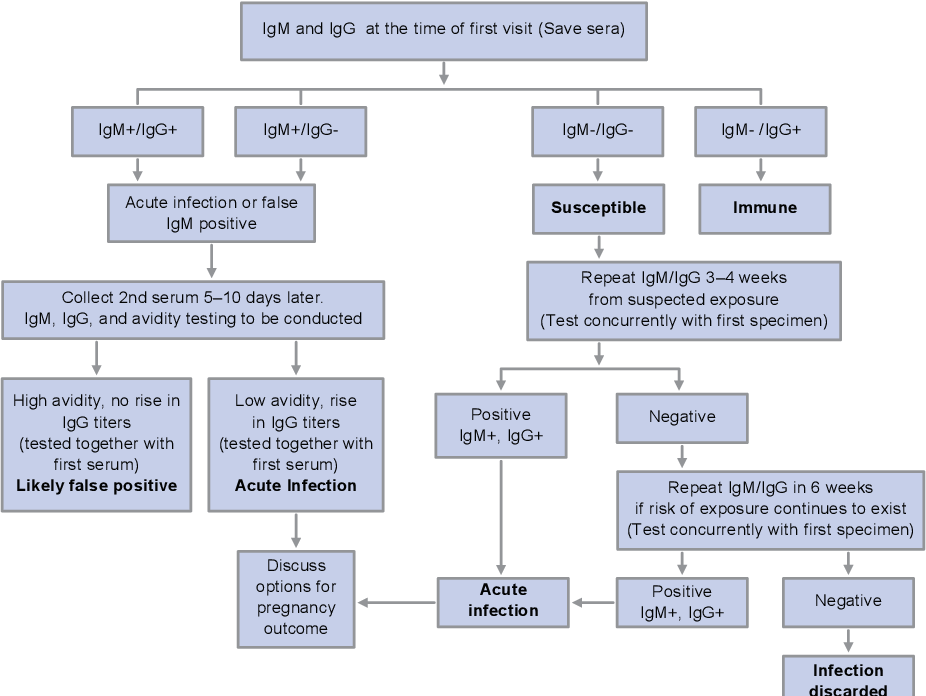
- If you can’t locate your records and are uncertain, the IgG ELISA blood test can help determine whether you received the measles vaccine or had measles as a child.
- For about four weeks after receiving an MMR vaccine, take additional precautions to avoid pregnancy.
If you are pregnant and you are exposed to measles, contact your doctor right away.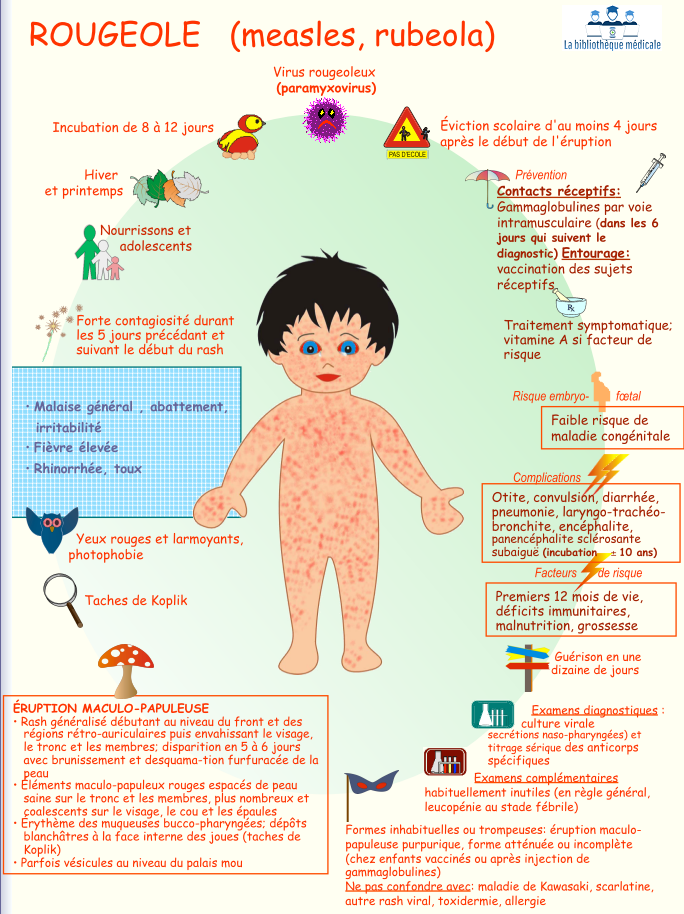 You might be able to receive a treatment to reduce the likelihood of infection.
You might be able to receive a treatment to reduce the likelihood of infection.
After pregnancy, consider getting an MMR vaccine if you aren’t immune. It is safe for breastfeeding women and babies.
Even if you have no desire to become pregnant, getting an MMR vaccine can help protect your health and the health of others in the community who are at risk for infection, including pregnant women, infants, and people with weakened immune systems.
Related reading: Beyond healthy babies: Why we discuss vaccines, maternal health during pregnancy
A few closing thoughts
Patients with measles are considered contagious as early as four days prior to breaking out with the signature measles rash. Early symptoms include fever, cough, and general weakness and fatigue. A red, bumpy rash follows, typically after 14 days of exposure.
We recommend that patients consider vaccination for themselves before pregnancy and discuss vaccination with family members and friends who will be around the baby.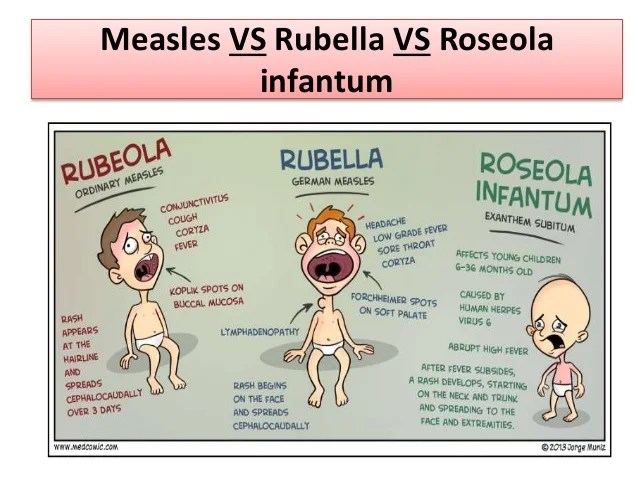
The health of women and babies is our utmost concern. If you're concerned that you've been exposed, call your doctor right away. If you aren't sure about your vaccination history or know that you need the MMR vaccine, call 214-645-8300 or request an appointment online.
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.D.
September 27, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
September 20, 2022
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
Your Pregnancy Matters
August 29, 2022
Your Pregnancy Matters
- Patricia Santiago-Munoz, M.
 D.
D.
August 23, 2022
Mental Health; Your Pregnancy Matters
August 11, 2022
Your Pregnancy Matters
- Emily Adhikari, M.D.
August 2, 2022
More Articles
Measles and pregnancy | Dr.
 Elena Berezovskaya
Elena Berezovskaya Since measles cases began to grow among the population of post-Soviet countries, where a huge number of children and adults are not vaccinated, vaccination certificates are bought, where measles is often diagnosed incorrectly, accurate statistics are untrue, I receive a lot of questions from women planning pregnancy, and already pregnant women about how to protect yourself from measles, whether this infection is terrible for a pregnant woman, how to avoid it, what to do in case of contact with a sick person. Since the questions are repeated, I have collected them together.
GENERAL
Is measles a viral or bacterial disease?
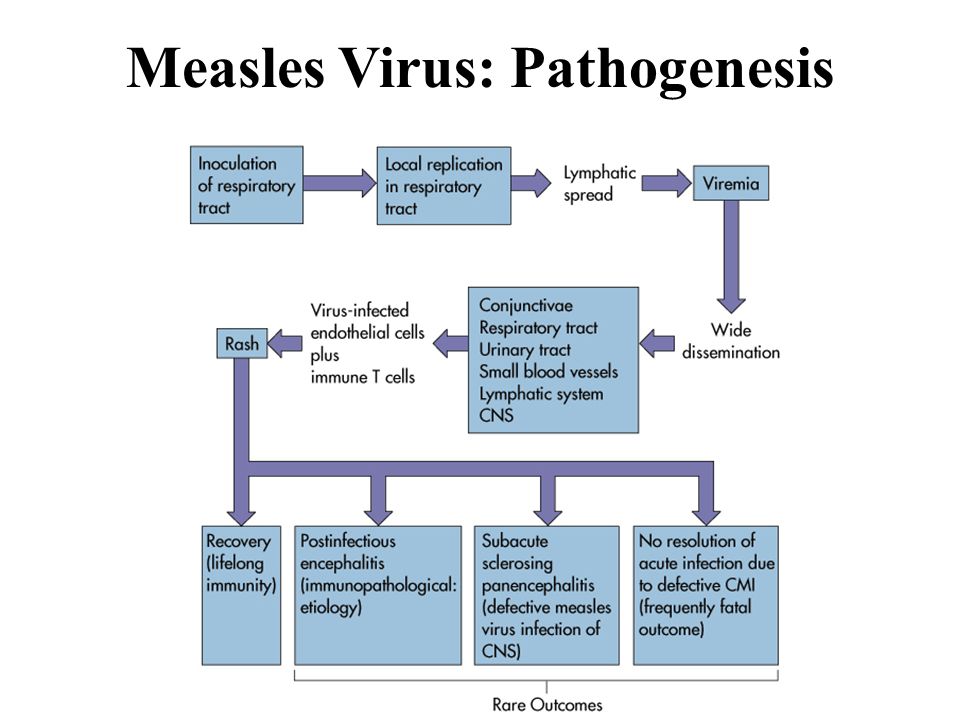
Measles is a viral disease. The causative agent is an RNA virus from the Paramyxoviridae family.
What is the difference between measles and rubella?
Rubella is caused by a completely different type of virus. It is sometimes referred to as German measles or 3-day measles, which can cause confusion in the correct interpretation of an infectious disease.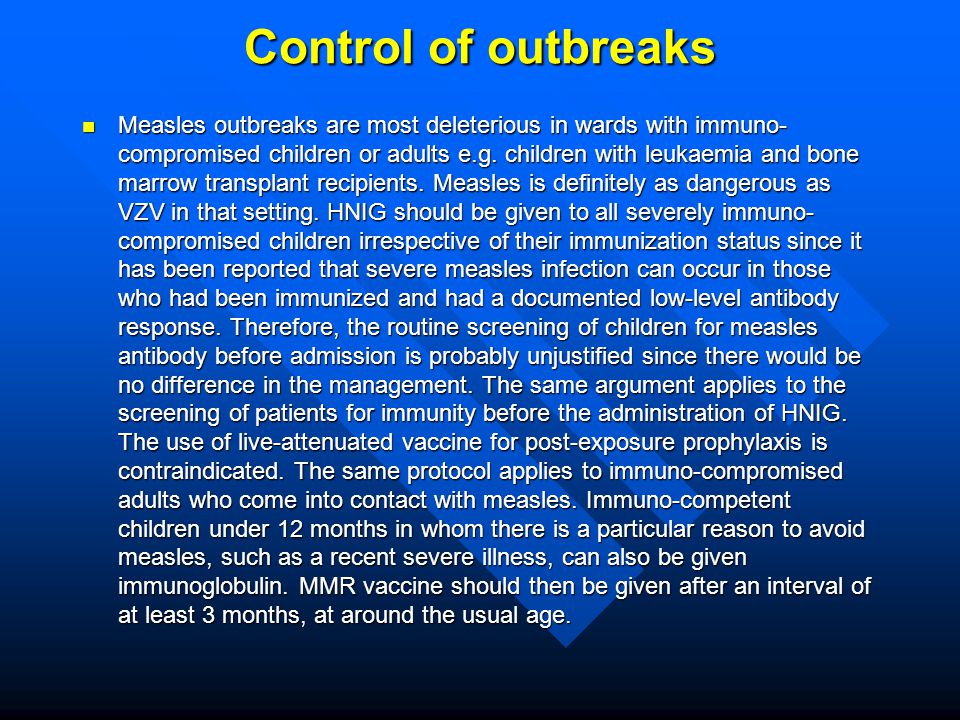 The clinical picture for measles and rubella is also different.
The clinical picture for measles and rubella is also different.
How long is the incubation period when you may not know about the disease?
On average, 10-12 days. Rashes appear most often on the 14th day after infection, although it may be earlier and later (7-21 days). This is a highly contagious disease - 90% of people get measles after being infected.
How long is a person contagious if they get measles?
A person can be contagious even in the absence of complaints and symptoms: 4 days before the onset of the rash and the next 4 days of rashes on the skin and mucous membranes.
How dangerous is it to be in a room where a person with measles has been?
The measles virus can survive on smooth surfaces and in the air for up to 2 hours. Therefore, the likelihood of infection also exists when a sick person is not in the room for a short period of time.
How does measles manifest itself?
In the classic course of the disease, there is a triad: cough, runny nose, conjunctivitis (in English 3 Cs cough, coryza, conjunctivitis) against the background of fever and general weakness.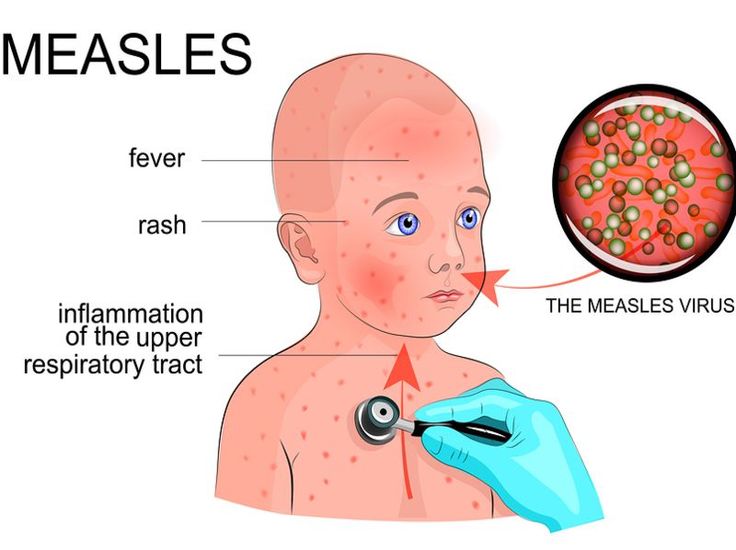 The rash appears on the 2-3rd day, in particular in the form of specific white spots with a red base (Koplik spots) on the mucosa of the soft and hard palate. Following them, spots appear on the skin of the head and body. Gradually, the rashes turn pale (usually from top to bottom).
The rash appears on the 2-3rd day, in particular in the form of specific white spots with a red base (Koplik spots) on the mucosa of the soft and hard palate. Following them, spots appear on the skin of the head and body. Gradually, the rashes turn pale (usually from top to bottom).
How is measles diagnosed?
The most reliable method for diagnosing measles is the detection of IgM antibodies and RNA of the virus by PCR in blood and secretions from the oral cavity (mucosal scraping).
How is measles treated?
There is no cure for measles. In severe cases, therapy is supportive. When a bacterial infection is attached, antibiotic treatment is performed.
Is it true that adults have a worse tolerance for measles than children?
Yes, measles is more severe in adults and may be accompanied by more serious complications than in children. Measles is very dangerous for the elderly, as well as for patients with serious chronic diseases and with suppressed immunity.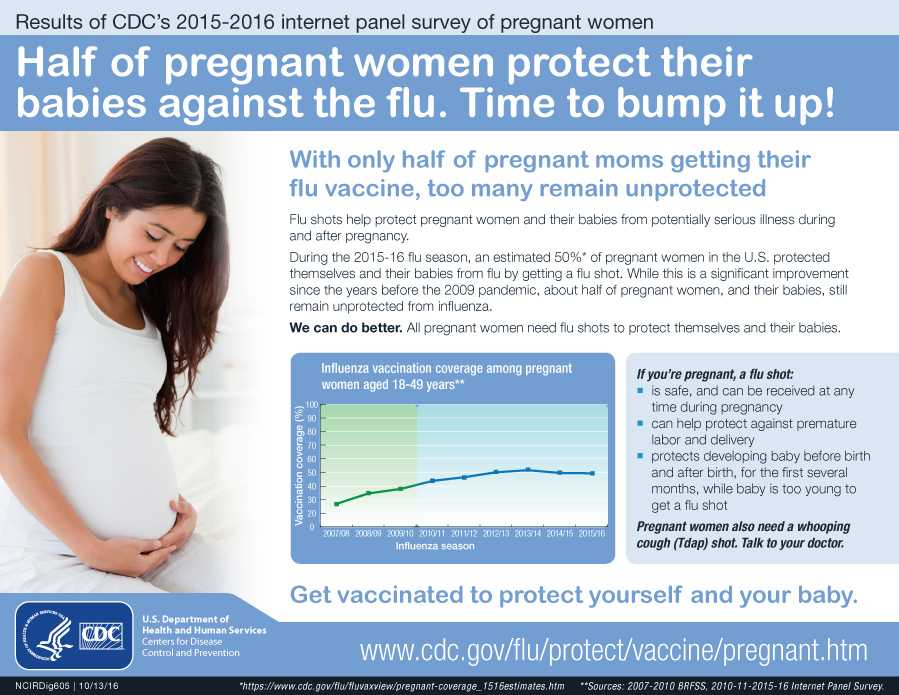
What are the most common complications of measles?
Relatively mild complications include bronchitis, pneumonia. Serious: encephalitis, subacute sclerosing panencephalitis, nervous system damage, death.
How common is measles?
In countries where vaccination has been regularly carried out for several years (mainly in developed countries), there are 3-11 cases of measles per 100,000 population per year. In countries where vaccination is low, the incidence of measles can increase by several times.
IMPACT OF MEASLES ON A PREGNANT WOMEN
Why is measles dangerous for a pregnant woman?
Pregnant women are more likely to develop complications of pneumonia, which also increases the mortality rate from complications of measles and pregnancy itself. Such women are more likely to end up in the hospital.
Although there are many publications on the topic of measles during pregnancy, most of them contain inaccurate data without taking into account many factors that determine the reliability of information. Also, the socio-economic status of pregnant women infected with measles affects the rate of complications during pregnancy. In developed countries, the number of pregnant women infected with measles is extremely small, which does not allow drawing conclusions characterizing the level of danger of this disease for the mother and fetus.
Also, the socio-economic status of pregnant women infected with measles affects the rate of complications during pregnancy. In developed countries, the number of pregnant women infected with measles is extremely small, which does not allow drawing conclusions characterizing the level of danger of this disease for the mother and fetus.
Should a pregnant woman be hospitalized if she has measles?
No, if her condition is satisfactory. However, the woman should be isolated from other family members and people who do not have measles immunity, that is, be in a separate room.
If a pregnant woman comes down with measles before giving birth, what should be done about her baby?
If the infection occurred 10 days before birth, it is advisable for the newborn to receive immunoglobulins (IM) during the first 5 days of life. Also, a protective dose of immunoglobulins is recommended for children under 12 months of age in case of measles infection of their mothers.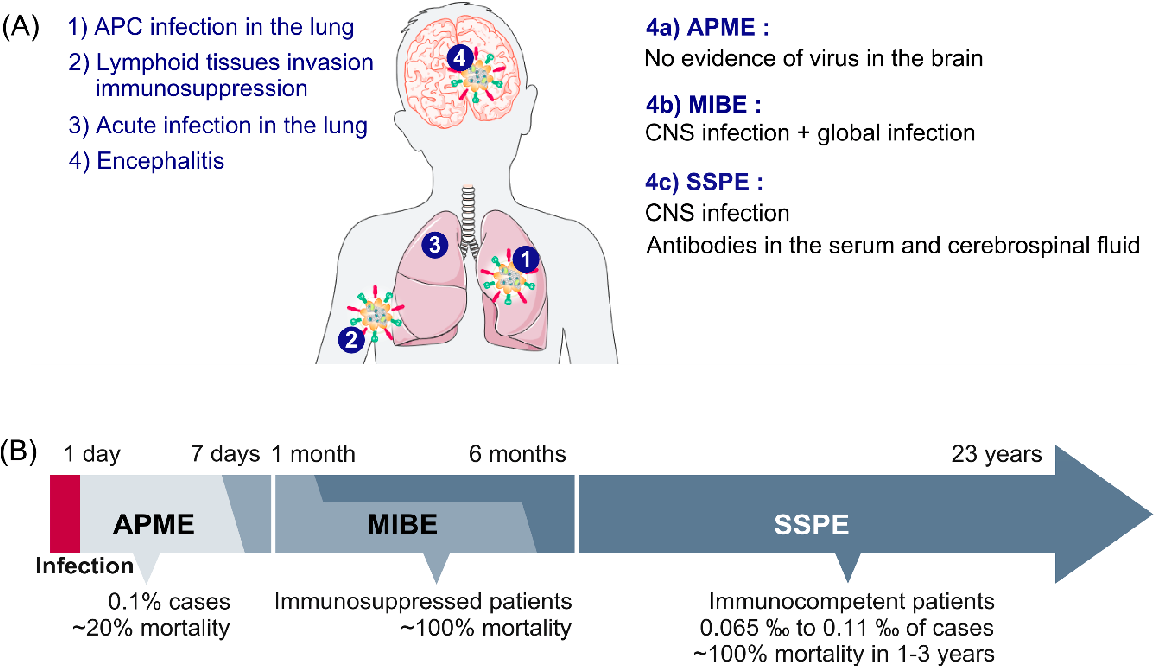
Should the newborn be isolated if the mother has measles?
There is very little evidence to support child isolation. Usually, the issue of isolation for 4 days after birth is decided on a case-by-case basis, taking into account the protection of other newborns.
EFFECT OF MEASLES ON THE FETUS
Is the measles virus transmitted to the fetus?
Transmission of the measles virus to the fetus has been described in several cases where women contracted the infection just a few days before delivery. Such children were born with congenital measles - they had a rash on the skin and mucous membranes, characteristic of measles, during the first 10 days of life. Of course, these children have an increased risk of developing other complications, but there is not enough information on this topic.
How dangerous is measles to the fetus?
Data on the effect of measles on the fetus in most publications are collected retrospectively by analyzing pregnancies many years ago, when vaccination was not or was not carried out regularly.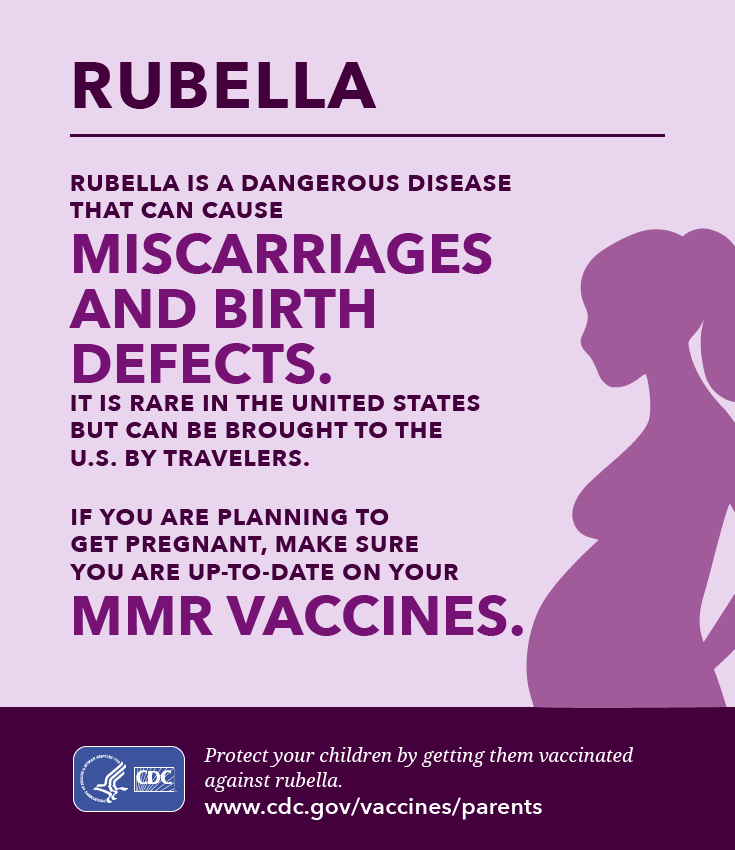 The most common complication is the low weight of the child (less than 2500 g) and premature birth.
The most common complication is the low weight of the child (less than 2500 g) and premature birth.
Does measles increase pregnancy loss?
The evidence that women who contract measles have an increased rate of miscarriage is controversial, as is information about higher rates of intrauterine fetal death and stillbirth.
The level of losses depends on the gestational age at which the infection occurred. According to some publications, if the infection occurred in the first trimester, then the probability of pregnancy loss is 50%, if in the second - 20%. But whether the cause is the direct effect of the virus on the fetus, or the serious condition of the mother, is unknown.
Does measles cause birth defects?
The measles virus does not increase the rate of birth defects. Several publications with isolated cases of measles in pregnant women do not deny the occurrence of malformations in the fetus. But high body temperature is a teratogenic factor and can lead to the death of the embryo or the development of defects, especially cardiovascular. A significant link between cases of measles and malformations has not yet been confirmed.
A significant link between cases of measles and malformations has not yet been confirmed.
What is the chance of fetal survival in a multiple pregnancy in a woman with measles?
Nobody knows the answer to this question. Only one case is described in the medical literature, when out of two fetuses in a woman who fell ill with measles at 19 weeks, one died in utero, the other was born healthy at term. Changes characteristic of intrauterine infection were found in the placenta.
IMMUNOLOGICAL STATUS
For example, US statistics show that over 16% of pregnant women are seronegative (unprotected) for measles. Many of them do not remember if they were vaccinated in childhood, whether they had one dose of vaccination or two. But even among vaccinated women (documented), the protective level of antibodies was only in 85-88% of cases. Therefore, many doctors recommend checking the level of IgG antibodies to the measles virus before planning a pregnancy and, in their absence or insufficient level, to re-vaccinate.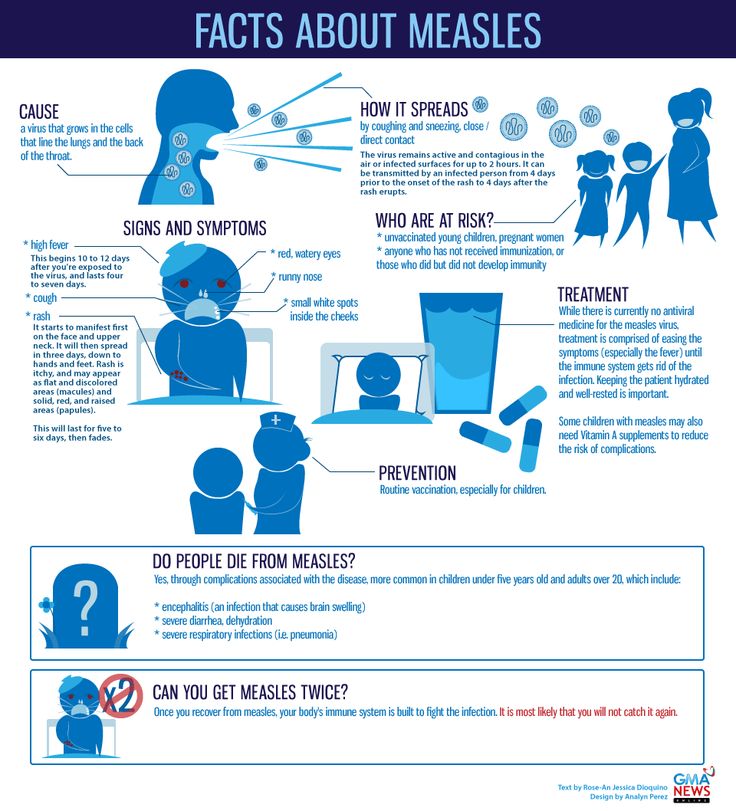
Is there a way to prevent this disease?
Yes, at 12-15 months of age, a vaccine is given that also protects against rubella and mumps, and in some countries against chickenpox. Re-vaccination is carried out at 4-6 years.
How effective is the measles vaccine?
The effectiveness of the vaccine depends on compliance with the vaccination schedule: after the first dose - 93%, after the second dose - 97%. However, with age, the protective response of the vaccine may decrease. In 80% of adults, immunity persists until old age.
Can measles be vaccinated during pregnancy?
The measles vaccine also includes suppressed rubella and mumps viruses. Although there is no evidence of harm to the embryo and fetus, it is still contraindicated during pregnancy.
When can pregnancy be planned after measles vaccination?
After 3-4 weeks. This time is enough to develop immunity and deactivate viruses.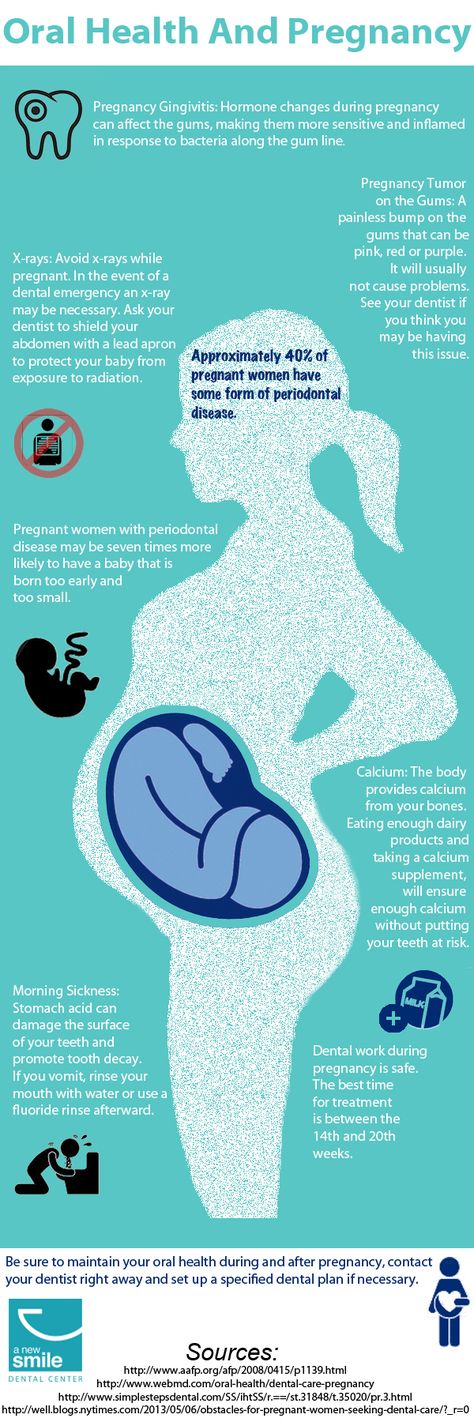
What if a woman did not know she was pregnant at the time of measles vaccination? Should this pregnancy be terminated?
No, a woman can safely carry a pregnancy. There is only a theoretical risk of possible harm from the vaccine, but no cases of pregnancy complications as a result of measles vaccination, including pregnancy loss, have been reported. On the contrary, there is a lot of data on the safety of this vaccination during pregnancy, when the vaccination was carried out without taking into account the presence of pregnancy. But traditionally, doctors do not recommend such vaccination for pregnant women.
Is it possible to vaccinate after childbirth? If yes, then when? Is it necessary to stop breastfeeding in this case?
Measles vaccine is recommended for women after childbirth, at almost any time. Most often it is carried out at the time of discharge from a medical institution. Breastfeeding does not need to be interrupted. On the contrary, the produced antibodies will be transmitted through breast milk, which to a certain extent will serve as protection for the newborn.
On the contrary, the produced antibodies will be transmitted through breast milk, which to a certain extent will serve as protection for the newborn.
If a pregnant woman has had contact with a person with measles, what should she do?
If a woman (whether she is pregnant or not) is vaccinated against measles or had the disease in childhood, she may not worry about the possible development of the disease.
If a woman is not immune to measles, it is advisable to give her intravenous IgG immunoglobulins within 5-6 days after infection. The antibodies will help neutralize the effects of the measles virus and protect the woman from developing the disease.
If a woman does not know her immunological status, she can either determine the level of IgG in the blood by a rapid method, or inject antibodies without prior analysis.
Rubella during pregnancy - maternity hospital "Leleka"
What is rubella?
Rubella is an infectious disease that is accompanied by high fever and skin rashes, as well as chills, redness of the face, pain in the throat and lymph nodes. Rubella is classified as a childhood disease: this highly contagious virus most often affects children of preschool and primary school age. The infection is transmitted only from person to person by airborne droplets, the peak incidence occurs in the spring. Sometimes adults get sick too. Subject to the regimen, the disease is easily tolerated and does not cause complications.
Rubella is classified as a childhood disease: this highly contagious virus most often affects children of preschool and primary school age. The infection is transmitted only from person to person by airborne droplets, the peak incidence occurs in the spring. Sometimes adults get sick too. Subject to the regimen, the disease is easily tolerated and does not cause complications.
Rubella during pregnancy
Rubella is considered a dangerous disease during pregnancy. In the first trimester, the transferred rubella increases the risk of miscarriage up to 40%, fading of pregnancy and the birth of a dead child - by 20%, the death of a baby in the first year of life - 10% higher. The virus inhibits the process of cell division. During the period of intensive development of the fetus, laying and formation of internal organs, the action of the virus can critically affect the viability of the fetus, as well as the ability of its organs to fully perform their functions.
The most dangerous period is up to the 14th week of pregnancy, when all the main organs are laid in the fetus. If a pregnant woman becomes ill, the virus can pass through the placenta to the fetus and cause congenital rubella syndrome. This syndrome causes pathologies of development: from 3 to 11 weeks of pregnancy - the brain, 4-7 weeks - pathologies of the eyes and heart, 7-13 - hearing impairment; during the same period, rubella can lead to the appearance of a cleft lip, as well as other pathologies and deformities in the fetus, up to its complete non-viability. Most often, the "Gregg triad" develops (cataract - 75% of cases, heart disease - 50%, deafness - 50%). Unfortunately, after suffering rubella, auto-abortion often occurs, or premature birth, in which the fetus is born unviable.
Congenital rubella syndrome
From about 16 weeks, the risk of dangerous pathologies due to congenital rubella syndrome decreases, the consequences of the disease are not so critical.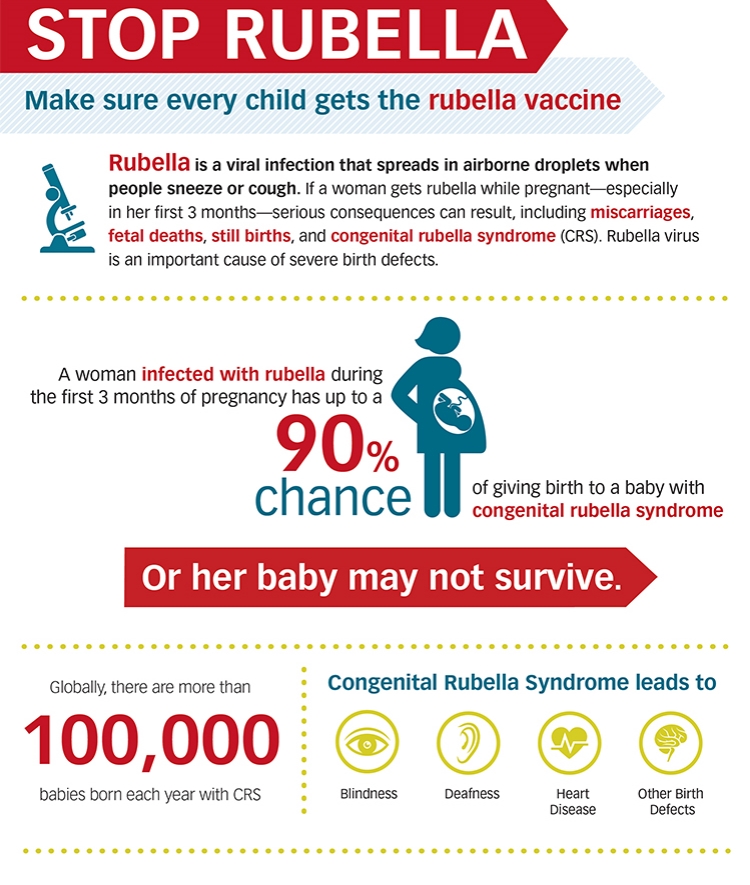 But if a pregnant woman has been ill with rubella before 14 weeks, this is the official reason for artificial termination of pregnancy. A woman should remember that the decision to terminate a pregnancy is not made by the doctor, but by herself. In such a situation, the doctor can only advise and advise. If a woman hesitates in making a decision, a consultation with a gynecologist can help her.
But if a pregnant woman has been ill with rubella before 14 weeks, this is the official reason for artificial termination of pregnancy. A woman should remember that the decision to terminate a pregnancy is not made by the doctor, but by herself. In such a situation, the doctor can only advise and advise. If a woman hesitates in making a decision, a consultation with a gynecologist can help her.
A special fetal blood test will help determine if the rubella virus has been able to cross the placenta and pose risks to the fetus. In addition, it is recommended to prescribe an additional ultrasound diagnostic session in order to examine the development of the baby's vital organs and exclude the development of pathologies.
Another danger of rubella is that it can be asymptomatic in adults. Thus, a woman can get rubella without noticing it. If cases of rubella are recorded in the region, pregnant women are offered to undergo a special analysis for antibodies. The presence in the blood of a pregnant woman of a large number of antibodies to the causative agent of this disease will show whether the woman was sick.
The presence in the blood of a pregnant woman of a large number of antibodies to the causative agent of this disease will show whether the woman was sick.
Vaccination against rubella
Rubella is included in the list of diseases against which babies in Ukraine are vaccinated at the age of one year. The incidence of rubella is low. If for some reason a pregnant woman has not been vaccinated against rubella, she should inform her doctor at the time of registration for pregnancy. However, even childhood vaccination does not provide 100% protection against the disease. Ideally, the rubella vaccine should be done additionally, a few months before the planned pregnancy. This is especially true for women who work in areas with an increased risk of disease - children's educational institutions, children's clinics, etc. If you are planning a pregnancy and there are cases of rubella in your area, you should consider additional vaccination. Studies show that women who have been vaccinated shortly before pregnancy do not develop fetal abnormalities caused by the rubella virus.